Abstract
Social support and strain have been linked with many health outcomes. However, less is known about whether these psychosocial factors are associated with Type 2 diabetes risk. This study uses the Midlife in the United States (MIDUS) dataset to examine the relationship between social support and strain from friends, family members, and spouse/partners and blood hemoglobin A1c levels in married/cohabiting adults who have not been diagnosed with diabetes. In addition, health locus of control is examined as a possible mediator. The study’s findings suggest that support from friends is negatively associated with HbA1c levels, indicating a relationship between better glycemic control and social support from friends, and an indirect association for spouse/partner support. A direct effect for internal health locus of control was also found.
Keywords: health, Type 2 diabetes risk, relationships, social support, social strain
More than 415 million people worldwide are affected by diabetes and the impact is expected to increase over the next few decades (IDF, 2017). Type 2 diabetes (T2D) typically begins in adulthood and is the most common form of the disease. This diagnosis brings a barrage of suggested lifestyle changes, such as modifying diet and exercise to help manage the disease in addition to medications (Inzucchi et al., 2015). Due to its prevalence and association with modifiable risk factors, such as improving diet and physical activity—compared with Type 1, an autoimmune disease that cannot be prevented, and gestational diabetes that occurs during pregnancy—the present study focuses on T2D risk and its relationship with social support and strain from three different sources.
Social support is typically conceptualized as an individual’s perception of receiving comfort, care, and assistance from others (Wallston, Alagna, DeVellis, & DeVellis, 1983). Although types and sources of social support vary, it is often a product of close relationships, such as one’s significant other, family members, and friends (Fingerman, Hay, & Birditt, 2004). The effect of social support on individuals’ health has been studied in various contexts, including diabetes self-management (Wardian & Sun, 2014), HIV treatment adherence (Simoni, Frick, & Huang, 2006), and loneliness (Chen & Feeley, 2014). Overall, social support typically relates to positive health outcomes (e.g., Wallston et al., 1983).
Negative social interactions—referred to as social strain—may also affect one’s health (e.g., Uchino Holt-Lunstad, Uno, & Flinders, 2001). This strain may come through critical comments, lack of emotional availability, or giving unsolicited advice (Coty & Wallston, 2010). Negative health outcomes may come as a result of not receiving needed support due to avoiding straining interactions (e.g., Uchino et al., 2001). For instance, social strain stemming from negative interactions has been shown to have a deleterious effect on health; outcomes include higher levels of depression and heart disease (de Guzman, Jurado, & Juson, 2015; Uchino, 2013). Previous research has shown that social support and strain may come from many sources, including family, friends, and spouses or partners (Chen & Feeley, 2014). In addition, the importance of those relationships may shift throughout one’s lifetime (de Guzman et al., 2015; Thomas, 2015).
Finally, health locus of control (HLC) reflects the perceived extent to which one can influence his or her health. This concept was established to address health-related issues and is often divided into two categories: internal and external (Lindström & Rosvall, 2012). Specifically, those who possess a higher internal HLC are more likely to believe they can personally influence their health outcomes. Conversely, those who exhibit higher external ratings tend to believe that other sources hold more influence over their health outcomes (Wallston, Wallston, Kaplan, & Maides, 1976). This is important because social support has been shown to buffer the effects of stress, which may in turn relate to HLC. Seminal work from Fusilier and colleagues (1987) suggested that responses to stress are hinged upon both social support and locus of control. Specifically, individuals with an external locus of control tended to have more pronounced reactions to stress than those with an internal locus of control (Fusilier et al., 1987).
This has also been seen in relation to HbA1c levels. Specifically, prior work suggests that decreased social support can relate to worsened glycemic control over time for individuals who have an external HLC (Schwartz, Coulson, Toovy, Lyons, & Flaherty, 1991). Conversely, internal locus of control has been linked with lower HbA1c levels (O’hea et al., 2005) and better health outcomes (Náfrádi, Nakamoto, & Schulz, 2017). Additionally, HLC has been shown to have a mediating relationship with social support and a number of health outcomes (e.g., Marr & Wilcox, 2015; Náfrádi et al., 2017).
The present study has two aims. First is to further examine the association between social support and social strain with blood glycemic control as an indicator of T2D risk. The second is to examine whether HLC serves as a mediator between the social support and strain variables included in the analysis and blood glucose control as indicated by hemoglobin A1c (HbA1c) levels.
Review of Literature
An overview of the study’s main outcome variable is presented first. This is followed by an overarching review of the main independent variables, social support and social strain. A summary of relevant research on the potential mediating variable, health locus of control, is presented as the final section of the literature review.
Glycemic Control
Diabetes is a chronic health condition in which the body is not able to produce sufficient insulin to regulate blood glucose (Global Diabetes Community, n.d.). The cause of T2D is not fully understood, although several factors such as age, obesity, and lack of physical activity may contribute (IDF, 2017). Prediabetes is a condition in which individuals have elevated blood glucose levels that have not risen high enough to be classified as diabetic; left untreated, it often becomes T2D (Global Diabetes Community, n.d.). Glycated hemoglobin (HbA1c) has been shown as a reliable measure of both prediabetes and diabetes management (Tankoya, Chakarova, Dakovsk & Atanassova, 2012).
HbA1c is formed when hemoglobin—a protein in red blood cells—bonds with glucose in the blood. Because red blood cells survive for eight to 12 weeks between renewal cycles, HbA1c gives a more complete picture of glycemic control than blood glucose levels (Global Diabetes Community, n.d.). Specifically, this measure provides a general indicator of an individual’s glycemic control over the past two to three months (O’Sullivan et al., 2006). In addition, HbA1c has been shown to function as a predictor for developing T2D and assessing prediabetes risk (Edelman, Olsen, Dudley, Harris, & Oddone, 2004). Along with having good reliability if testing is conducted properly, HbA1c tests are preferred because they can be taken at any point in the day and do not require fasting to obtain an accurate reading (Global Diabetes Community, n.d.).
Social Support
Social support is generally conceptualized as the perception of positive interactions, advice, care, or esteem coming from others when it is needed (Lindström & Rosvall, 2012). It is important to note that the sources and type of support may vary, with differences seen in impact as well. For instance, emotional and instrumental support from family and friends were found to be significantly related to diabetes self-care (Toljamo & Hentinen, 2001). This aligns with findings from other research that suggests friends and family members provide different types of social support to adolescents who have diabetes (LaGreca et al., 1995). Perceived social support has been shown as a predictor of health behaviors and positive health outcomes, both within the general population and for individuals with chronic illnesses such as diabetes (Ng & Jeffery, 2003). As an example, Birditt and Antonucci (2008) examined relationship qualities from three sources—spouse, children, and family/friends. This longitudinal study’s findings showed a mix of results. For instance, positive spousal relationship qualities that were consistent across time-points were associated with decreased mortality. Yet, negative spousal relationship qualities at baseline were less deleterious for health outcomes than relationships initially rated positively that declined over time (Birditt & Antonucci, 2008).
Importantly, social support is also frequently linked with stress management. Within the diabetes resilience model (Hilliard, Harris & Weissberg-Benchell, 2012), support from friends and family was linked with improved outcomes for adolescent diabetes patients as measured by HbA1c levels as well as blood glucose levels. This is relevant to the present study due to the connection from support to stress, which in turn was associated with improved HbA1c levels (Hilliard et al., 2012).
Overall, there is a void in the literature regarding social support and T2D risk. However, there is increasing evidence for an association between social factors and T2D risk. For instance, in examining social relationship variables and T2D risk among postmenopausal women, Hendryx and colleagues (2019) found that women who had the highest levels of social support had a lower risk of developing T2D. Likewise, in a population-based study in Sweden, Norberg and colleagues (2007) found that low emotional support may contribute to T2D risk in women. Finally, an examination of a nationally representative sample of adults in the U.S. reported an inverse relationship between satisfaction with spouse/partners’ daily interactions and elevated HbA1c levels (Maki, 2018). Together, these findings suggest that social support may have a protective association with glycemic control. Based on these findings that relate to the role of social support in glycemic control, the first hypothesis is posed:
H1: Social support from friends (H1a), family members (H1b), and one’s spouse/partner (H1c) will be negatively related to HbA1c levels (therefore indicating better glycemic control).
Social Strain
Social strain is often conceptualized as a lack of support when it is needed, criticism directed toward a behavior or situation, or offering unsolicited advice (Coty & Wallston, 2010). These types of negative interactions not only undermine one’s sense of autonomy but may also relate to feelings of social isolation and depression (e.g., Blom, Janszky, Balog, Orth-Gomér, & Wamala, 2003). It is possible for a relationship to possess both negative and positive characteristics, making it difficult for individuals to address negative issues or acknowledge positive attributes (e.g., Uchino et al., 2001).
In contrast to the findings for social support, social strain has been shown as a significant predictor of various health ailments such as depression (Teo, Choi, & Valenstein, 2013) and coronary heart disease (e.g., Lett et al., 2005). These are both noteworthy in the context of diabetes risk because there are many shared risk factors for diabetes and cardiovascular disease (Kumari, Head & Marmot, 2004). Moreover, social strain has been found to significantly relate to many other health issues (Walen & Lachman, 2000).
For instance, Mayberry and Osborn (2012) found that diabetes patients with non-supportive family members felt as though their care regimens were being sabotaged. As a result, those with non-supportive family members had poorer medication adherence as well as worse glycemic control (Mayberry & Osborn, 2012). Similarly, higher levels of stress have been shown to have a positive association with HbA1c levels throughout the lifespan (Hilliard et al., 2016), thus indicating a higher likelihood of developing T2D associated with stress. In addition, Kumari and colleagues (2004) found an increased likelihood of T2D among men with more work stress operationalized as effort-reward imbalance. Work-related stress has also been linked with T2D risk in women (Norberg et al., 2007). Similarly, a 12-year longitudinal study that utilized causal modeling found an increased risk of T2D due to stress (Harris et al., 2017). This is also reflected in findings from a study of postmenopausal women. Specifically, social strain was associated with an increased risk of developing T2D (Hendryx et al., 2019). Finally, a review of social determinants of T2D showed links with stress, unmet personal needs due to attention to spousal needs, and the potential difficulty of managing self-care within social networks (Clark & Utz, 2014). Thus, based on these findings, the second hypothesis is posed:
H2: Social strain from friends (H2a), family members (H2b), and one’s spouse/partner (H2c) will be positively related to HbA1c, indicating glycemic control.
Health Locus of Control
The locus of control framework is centered on perceptions of being able to influence one’s own health. Typically, HLC is considered in the context of an internal or external orientation. Although there is a void in literature regarding HLC and T2D risk, better health outcomes are often associated with an internal HLC orientation in the context of diabetes management. For instance, in a study on the effects of HLC on diabetes treatment adherence, Morowatisharifabad and colleagues (2009) found that patients with internalized HLC ratings were more likely to adhere to their diabetes treatments. Similarly, findings from a study examining health outcomes of T2D patients showed an association between internal HLC and HbA1c levels, along with a number of interactions indicating poorer glycemic control among individuals who reported high external HLC related to “chance” along with low internal HLC beliefs (O’hea et al., 2005). This finding aligns with other work that suggests an external HLC orientation is associated with poorer health outcomes (e.g., Náfrádi et al., 2017; Roddenberry & Renk, 2010).
Additionally, a relationship between social support and HLC has been suggested by prior work. Within the context of stress and illness, Rodenberry and Renk (2010) found a mediating relationship between stress and illness among college students. Scholars have also shown similar associations for patient populations. For instance, in a mixed-methods study with diabetes patients, Juárez-Ramírez and colleagues (2015) found that perceived social support helped patients feel more capable of handling their treatment. Another study found that individuals with an internal locus of control were proactive in managing T2D risk, whereas those with an external locus of control tended to believe that T2D is due to fate or other non-modifiable reasons (Macaden & Clarke, 2010). Further, a systematic review of patient empowerment and treatment adherence showed that HLC has been shown to mediate the relationship between a number of factors, including social support, and treatment outcomes (Náfrádi et al., 2017). In addition, an analysis of social support and patient-provider communication among diabetes patients found that patient empowerment served as a mediator between these variables (Oh & Lee, 2012).
Building from these findings, it is expected that HLC would also relate to HbA1c levels due to the link between glycemic control and behavioral factors. For instance, individuals reporting both external HLC and decreases in social support showed reduced glycemic control over time; this suggests a link between these factors and HbA1c levels (Schwartz et al., 1991). Indeed, health locus of control has been shown to mediate social support and healthy eating habits in college students (Marr & Wilcox, 2015). Likewise, an analysis of young adults from 18 European countries found that internal locus of control was associated with a greater likelihood of health behaviors including exercise, consuming less salt, and having a lower fat diet with a more than 40% increase in odds of engaging in healthy behavior for those in the highest quartile of internal control ratings compared to the lowest quartile (Steptoe & Wardle, 2001). Based on these findings, the final hypotheses are posed along with a research question regarding to association between HLC and HbA1c levels.
H3: Internalized HLC will be negatively related to HbA1c levels, thus indicating better glycemic control and lower risk of developing T2D.
H4: External HLC will be positively related to HbA1c levels, indicating worse glycemic Control and higher risk of developing T2D.
RQ: Do internal and external HLC mediate social support and strain’s relationship to HbA1c?
Method
Data for this study came from the Midlife in the United States (MIDUS) survey, collected from 2004 through 2006. MIDUS provides nationally-representative data examining social, psychological, and behavioral factors in conjunction with physical and mental health data from adults (Ryff et al., 2007). This sample is based on a random-digit-dial sample of noninstitutionalized English-speaking adults who were chosen from working telephone banks in the U.S. The second wave of MIDUS is a 10-year follow-up from the first wave, which was conducted in 1995 to 1996. A third wave of data collection was started in 2013 with additional projects, such as biomarker sampling, still underway (MIDUS, n.d.). Only data from the second wave were included in this cross-sectional analysis. This decision was made because MIDUS 1 did not collect biomarker data and MIDUS 3 biomarker data have not been released as of the January 2020 writing of this manuscript (MIDUS, n.d.).
In terms of demographics, the majority of respondents reported being married (70.91%) and most had either a high school diploma or less education (33.1%) or had completed at least some college (20.9%). In order to account for the spouse/partner measurement, only participants who indicated they were married/cohabiting were included in the present study. Most were White (88.96%) and about one-third of participants were female (36.5%). The ages ranged from 33 to 83 years old (M = 55.16, SD = 11.54). The MIDUS project included twins and sibling data. In order to account for this, a dummy variable was created to control for potential non-independence of data (participants who were not part of the twin or sibling subsamples serve as the reference group for this variable). Within the present analysis, approximately 25% of participants were within the twin or sibling subsample. For this study’s analysis, the participants’ socioeconomic index was used to capture education, income, and prestige; missing values for this variable were imputed using multiple imputation with five iterations in SPSS. The MIDUS II post-stratum weight-9 variable was applied for this study’s cross-sectional analysis in order to align the sample with the general U.S. population’s characteristics (please see Ryff et al., 2007 for a more detailed explanation of the weighting process). Additionally, because the present study is examining social support and strain in relation to T2D risk, individuals who had previously been diagnosed with diabetes were excluded. As mentioned above, due to the large proportion of married participants and the nature of the spouse/partner support measures used as independent variables, the present analysis only included individuals who indicated they were married or cohabiting. The final sample for this study included 926 participants.
Measures
The present study utilized six main independent variables: support from friends, family, and spouse/partner; and strain from friends, family, and spouse/partner. In addition, two HLC variables (internal and external) were included as potential mediators, along with the final outcome variable of HbA1c level. Control variables included the following demographics: age, gender, persons of color (due to a lack of diversity in this sample, all participants who identified with non-White racial groups were grouped together), and the socio-economic index variable that is measured by MIDUS to reflect individuals’ income, prestige, and education in relation to occupation (full sample range: 9.56-80.53, M = 42.08, SD = 14.29). Additionally, physiological (BMI and high blood pressure diagnosis), and behavioral (current smoking status) measures were included due to their association with T2D risk (Gonzalez-Zacarias, Mavarez-Martinez, Arias-Morales, Stoicea, & Rogers, 2016).
Social support.
Given the secondary nature of this study, the variables used for support from friends and family members are both a scale constructed of four items with Likert-type responses: “How much do your friends really care about you?”, “How much do they understand the way you feel about things?”, “How much can you rely on them for help if you have a serious problem?”, and “How much can you open up to them if you need to talk about your worries?”. Possible responses for each item ranges from one (“a lot”) to four (“not at all”). The scale items were reverse coded so that higher values represent higher levels of social support. The internal consistency of the scale is strong (α = 0.88, M = 3.28, SD = 0.66). The variable used for support from family is an identical scale that also shows good internal consistency (α = 0.84, M = 3.52, SD = 0.58).
Support from participants’ spouses/partners was measured by a scale constructed of six items with Likert-type responses. These include: “How much does your spouse or partner really care about you?”, “How much does he or she understand the way you feel about things?”, “How much does he or she appreciate you?”, “How much do you rely on him or her for help if you have a serious problem?”, “How much can you open up to him or her if you need to talk about your worries?”, and “How much can you relax and be yourself around him or her?”. The possible responses for each of these items ranges from one (“a lot”) to four (“not at all”). The items were reverse coded so that higher values indicate higher levels of support. The scale showed good internal consistency (α = 0.90, M = 3.64, SD = 0.53). It is noteworthy that some of these variables overlap—and have been used—with other constructs such as perceived responsiveness (Slatcher, Selcuk, & Ong, 2015; Selcuk & Ong, 2013). However, their use as an indicator of social support also has precedent (Chen & Feeley, 2014; Yang, Schorpp, & Harris, 2014). The decision to use these measures as an indicator of social support, rather than perceived responsiveness, for the present study was made due to the inclusion of family and friends in addition to marital relationships.
Social strain.
The variable used for strain from friends is a scale constructed with four items, including: “How often do your friends make too many demands on you?”, “How often do they criticize you?”, “How often do they let you down when you are counting on them?”, and “How often do they get on your nerves?” Each item was answered with a four-point Likert-type scale, ranging from one (“often”) to four (“never). The items were reverse coded so that higher values indicate higher levels of strain. The scale showed acceptable internal consistency (α = 0.79, M = 1.84, SD = 0.50). Family members’ strain is measured with an identical scale, which also exhibits good internal consistency (α = 0.79, M = 2.04, SD = .60).
Strain from spouses/partners was measured with a six-item scale. The items include: “How often does your spouse or partner make too many demands on you?”, and “How often does he or she argue with you?”, “How often does he or she make you feel tense?”, “How often does he or she criticize you?”, “How often does he or she let you down when you are counting on him or her?”, and “How often does he or she get on your nerves?”. Each item is answered with a Likert-type scale, anchored at one (“often”) and four (“never”). The items were reverse coded so that higher values indicate higher levels of strain. The internal consistency of the scale is good (α = 0.87, M = 2.14, SD = 0.61).
Health locus of control.
Two indicators of HLC were included in the analysis. First, internal HLC was measured with a scale constructed of four items. These Likert-type questions include: “Keeping healthy depends on things that I can do”, “There are certain things I can do for myself to reduce the risk of a heart attack”, “There are certain things I can do for myself to reduce the risk of getting cancer”, and “I work hard at trying to stay healthy”. The possible responses ranged from one (“strongly agree”) to seven (“strongly disagree”). The items were reverse coded so that higher values reflect a higher internal HLC. The internal reliability of the scale is good (α = 0.74, M = 6.07, SD = 0.87).
Second, external HLC was measured with one item: “When I am sick, getting better is in the doctor’s hand”. This item used Likert-type responses, ranging from one (“strongly agree”) to seven (“strongly disagree”), and was reverse coded so that higher values reflect higher external HLC ratings (M = 4.25, SD = 1.80).
Hemoglobin A1c.
The HbA1c measure was derived from a blood test obtained from participants. The biomarker data collection was completed at three general clinical research centers by clinicians or trained staff, following procedures specified in the study protocol (Ryff, Seeman, Weinstein, 2019). The assays were performed using a validated method for measuring HbA1c that may be read about in detail through MIDUS documentation (MIDUS, n.d.).
Analysis.
The hypothesized model (Figure 1) was tested using a path analysis using Lisrel software (version 10.2) and maximum likelihood estimation. Figure 1 shows eight direct effect and six indirect effect paths, but omits covariances specified between each pair of exogenous variables for visual clarity. The direct and indirect effects of the three sources of support and strain on HbA1c were estimated, along with direct effects of the exogenous variables on HLC (the mediators), as well as the direct effects of internal and external HLC on HbA1c.
Figure 1.
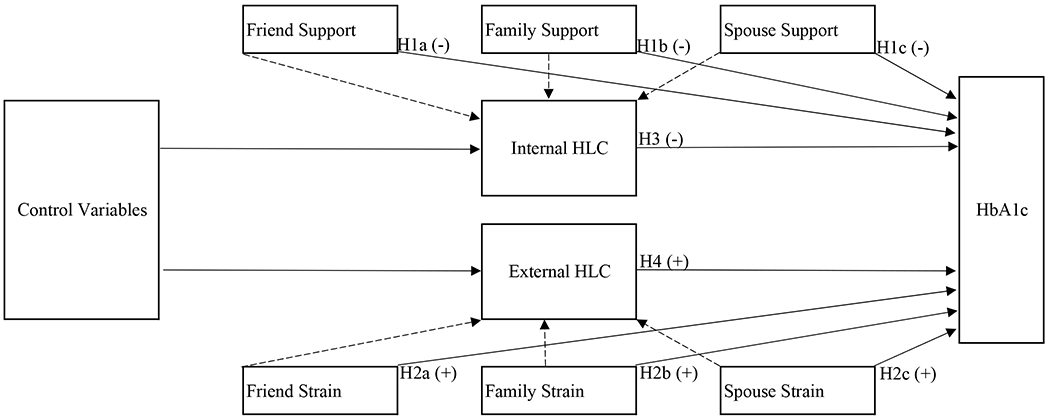
Hypothesized model showing indirect and direct paths for HbA1c
Because the χ2 statistic is often significant with large samples (Schumacker & Lomax, 2010), three alternative fit indices were examined to examine the model’s fit. The alternative indices include the root mean square error of approximation (RMSEA), comparative fit index (CFI), goodness of fit index (GFI), and normed fit index (NFI). For the CFI, GFI, and NFI, values larger than 0.90 are considered as indicators of good fit, and RMSEA values smaller than 0.05 and 0.08 are considered a close fit and good fit (Schumacker & Lomax, 2010). This study was approved as exempt from [university] IRB.
Results
Descriptive statistics and a correlation matrix of the variables are provided in Table 1. In the initial SEM analysis, a path from each of the exogenous control variables, including age, race/ethnicity, and gender, to each endogenous variable was included. In order to account for measurement error due to using similar instruments, the error for HLC internal and HLC external was allowed to correlate in the model based on the modification indices. Other modifications were not made based on these results.
Table 1.
Correlation matrix and descriptive statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. HbA1c | 1 | ||||||||||||||||
| 2. Age | 19** | 1 | |||||||||||||||
| 3. Twin/Sibling | .02 | .15** | 1 | ||||||||||||||
| 4. Female | −.20** | −.07* | .12** | 1 | |||||||||||||
| 5. Persons of color | .08* | −.27** | −.04 | −.16** | 1 | ||||||||||||
| 6. Socioeconomic index | −.03 | .07* | .07* | −.04 | −.03 | 1 | |||||||||||
| 7. High blood pressure | .11** | .11** | .06 | −.07* | .08* | .07* | 1 | ||||||||||
| 8. BMI | .24** | −.13** | −.06 | −.16** | 23** | .03 | 23** | 1 | |||||||||
| 10. Smoke currently | .02 | −.30** | −.19** | −.13** | .12** | −.15** | .04 | .05 | 1 | ||||||||
| 11. Spouse/partner support | .04 | 23** | −.09** | .01 | .00 | −.03 | .00 | −.17** | −.04 | 1 | |||||||
| 12. Spouse/partner strain | −.06 | −.18** | .08* | −.10** | .10** | .02 | −.00 | .14** | −.06 | −.72** | 1 | ||||||
| 13. Friend support | −.06 | .12** | .13** | .18** | −.15** | .06 | −.05 | −.06 | −.15** | 23** | −.26** | 1 | |||||
| 14. Friend strain | −.04 | −.30** | −.15** | −.08* | .16** | −.10** | .18** | .25** | .15** | −.21** | .31** | −.30** | 1 | ||||
| 15. Family support | .03 | .14** | −.07* | .06 | −.04 | −.00 | −.06 | −.07* | −.10** | .25** | −.23** | .46** | −.20** | 1 | |||
| 16. Family Strain | −.06 | −.41** | −.13** | .01 | .25** | −.15** | .11** | .28** | .15** | −.15** | .25** | −.30** | .63** | −.41** | 1 | ||
| 17. HLC external | −.07* | −.09** | −.03 | .06 | −.08* | .08* | −.04 | −.02 | .02 | −.04 | .01 | −.01 | −.01 | −.02 | .06 | 1 | |
| 18. HLC internal | −.17** | .09** | −.04 | .10** | −.08* | .02 | .10** | −.20** | −.26** | .20** | −.01 | .13** | .01 | .10** | −.07* | −.16** | 1 |
| Mean (n for binary variable) | 5.84 | 55.16 | 232 | 338 | 102 | 40 | 241 | 28.60 | 253 | 3.57 | 2.25 | 3.18 | 1.89 | 3.50 | 2.10 | 4.08 | 6.04 |
| Standard Deviaion (or %) | 0.45 | 11.54 | 25% | 37% | 11% | 12.44 | 26% | 4.99 | 27% | 0.56 | 0.71 | 0.66 | 0.52 | 0.62 | 0.63 | 1.80 | 0.89 |
Note:
p < .05
p < .01
N = 926
Results of the final analysis for the proposed model (Figure 1) show good fit. In specific, the RMSEA indicates an acceptable model fit (RMSEA = 0.09). Likewise, the other fit indices show strong model fit (NFI = 0.99; CFI = 0.99; and GFI = 0.99). As anticipated due to the sample size, the χ2 statistic is significant (χ2 = 50.40, p < .001).
The standardized path coefficients with indirect and direct effects are shown in Table 2. As shown in Table 2, social support from family members and spouses/partners did not have a direct association with HbA1c. However, social support from friends had a negative direct relationship (β = −0.05, SE = 0.03, p = .047). None of the sources of strain had a statistically significant direct relationship with HbA1c. Thus, hypothesis one (H1a) was partially supported and hypothesis two was not supported.
Table 2.
Direct and indirect effects of path coefficients for key variables, hypothesized model
| HLC Internal | HLC External | HbA1c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Direct | Indirect | Total | Direct | Indirect | Total | Direct | Indirect | Total | |
| Control variables | |||||||||
| Age | −0.01 | ----- | −0.01 | −0.01* | ----- | −0.01 | 0.01*** | 0.00* | 0.01*** |
| Twin/Sibling | −0.20** | ----- | −0.20* | −0.11 | ----- | −0.11 | 0.03 | 0.02** | 0.04 |
| Female | 0.07 | ----- | 0.07 | 0.13 | ----- | 0.13 | −0.12*** | −0.01 | −0.12*** |
| Persons of Color | −.0.07* | ----- | 0.08* | 0.66** | ----- | 0.66** | −0.07 | −0.01* | −0.09* |
| Smoke (1=yes) | −0.54*** | ----- | −0.54*** | 0.07 | ----- | 0.07 | 0.01 | 0.04** | 0.044 |
| SEI | −0.00 | ----- | −0.00 | 0.01** | ----- | 0.01** | −0.00 | 0.00 | −0.00 |
| High BP | 0.36*** | ----- | 0.36*** | −0.10 | ----- | −0.10 | 0.05 | −0.02** | 0.03 |
| BMI | −0.04*** | ----- | −0.04*** | −0.01 | ----- | −0.01 | 0.02*** | 0.00** | 0.02*** |
| Internal HLC | −0.07*** | −0.07*** | −0.07*** | ||||||
| Friend Support | 0.08 | ----- | 0.08 | ----- | ----- | ----- | −0.05* | −0.01 | −0.06* |
| Family Support | 0.02 | ----- | 0.02 | ----- | ----- | ----- | 0.03 | −0.00 | −0.03 |
| Spouse Support | 0.22** = | ----- | 0.22*** | ----- | ----- | ----- | 0.02 | −0.02** | 0.00 |
| External HLC | −0.01 | −0.01 | −0.01 | ||||||
| Friend Strain | ----- | ----- | ----- | −0.19 | ----- | −0.19 | −0.02 | −0.00 | −0.02 |
| Family Strain | ----- | ----- | ----- | 0.30* | ----- | 0.30* | −0.03 | −0.00 | −0.04 |
| Spouse Strain | ----- | ----- | ----- | 0.06 | ----- | 0.06 | −0.03 | −0.00 | −0.03 |
| HbA1c | |||||||||
Note:
= p < .05
= p < .01
= p < .001
The path coefficient to HbA1c from internal HLC was statistically significant in the anticipated direction (β = −0.07, SE = 0.02, p < .001), thus the third hypothesis was supported. Finally, the path from external HLC was not statistically significant. Thus, the fourth hypothesis was not supported.
To address the research question, the path coefficients for friends’ support, (β = 0.08, SE, 0.05, p = .08), family support (β = 0.02, SE = 0.05, p = .75), and spouse support (β = 0.22, SE = 0.05, p < .001) going to internal HLC were examined. Likewise, the path coefficients for friends’ strain (β = −0.19, SE = 0.15, p = .21), family strain (β = 0.30, SE = 0.13, p = .02), and spouse strain (β = 0.06, SE = 0.09, p = .53) going to external HLC were examined. Along with family strain, the following control variables were significantly associated with external HLC: age (β = −0.01, SE = 0.01, p = .03), race (β = −0.66, SE = 0.20, p = .001). SEI (β = 0.01, SE = 0.00, p = .005) with external HLC. As evidenced above, spouse/partner’s support were associated with higher internal HLC ratings, while support from friends and family members was not.
To further examine the possible mediating role of HLC, the indirect effects of the support and strain variables were examined. As shown in Table 2, spouse/partner support (β = −0.02, SE = 0.01, p < .01) is indirectly related to HbA1c. However, none of the other support and strain sources were statistically significant. It appears that support from partners is mediated by internal HLC, but the same effect is not seen for family members’ support. Likewise, the sources of strain are not significantly related to HbA1c or mediated by external HLC.
Additional Analyses
In order to further test the model, external HLC and other non-significant paths were removed one at a time, as recommended, for model testing (Schumacker & Lomax, 2010). Paths from significant control variables remained in the model. Based on modification indices and past work examining potential interactions between locus of control and support/strain relationships (e.g., Noor, 1995), a path from spouse strain was added going to internal HLC. The modified model showed overall excellent fit. Specifically, its χ2 statistic is no longer significant (χ2 = 8.03, df = 7, p = .33). The additional fit indices also suggest good model fit (RMSEA = 0.01, NFI = 1.00, CFI = 1.00).
The path coefficients are presented in Table 3 and also shown in Figure 2. Interestingly, spousal strain was negatively associated with HbA1c (β = −0.04, p =.02) and positively associated with internal HLC (β = 0.35, p < .001), with an indirect relationship also seen with HbA1c (β = −0.02, p < .001). One reason for this finding may be buffering from potentially beneficial aspects of negative relationship qualities (e.g., Birditt & Antonucci, 2008). Likewise, spousal support had a significant direct association with internal HLC (β = 0.51, p < .001) and an indirect association with HbA1c (β = −0.03, p < .001). Friend support (β = 0.13, SE = 0.04, p = .002) was positively associated with internal HLC. Finally, internal HLC was negatively associated with HbA1c, as would be expected (β = −0.06, SE = 0.02, p < .001). As can be seen in Figure 2, this model is a great deal more parsimonious than the hypothesized model (Figure 1).
Table 3.
Direct and indirect effects of path coefficients for modified model
| HLC Internal | HbA1c | R2 | |||||
|---|---|---|---|---|---|---|---|
| Direct | Indirect | Total | Direct | Indirect | Total | ||
| Control variables | |||||||
| Age | ----- | ----- | ----- | 0.01*** | ----- | 0.01*** | |
| Twin/Sibling | −0.24*** | ----- | −0.24*** | ----- | 0.02** | 0.02** | |
| Female | 0.13* | 0.13* | −0.13*** | −0.01* | −0.13*** | ||
| Persons of ColorBlack | ----- | ----- | ----- | 0.09* | ----- | −0.09* | |
| Smoke (1=yes) | −0.44*** | ----- | −0.44*** | ----- | 0.03*** | 0.03*** | |
| SEI | ----- | ----- | ----- | ----- | ----- | ----- | |
| High BP | 0.35*** | ----- | 0.35*** | ----- | −0.02** | −0.02** | |
| BMI | −0.04*** | ----- | −0.04*** | 0.02*** | 0.00*** | 0.02*** | |
| Internal HLC | −0.06*** | −0.06*** | ----- | 0.20 | |||
| Friend Support | 0.13** | ----- | 0.13** | ----- | −0.01** | −0.01* | |
| Spouse Support | 0.51*** | ----- | 0.51*** | ----- | −0.03*** | −0.03*** | |
| Spouse Strain | 0.35*** | ----- | 0.35*** | −0.05* | −0.02*** | −0.07** | |
| HbA1c | 0.15 | ||||||
Note:
= p < .05
= p < .01
= p < .001
Figure 2.
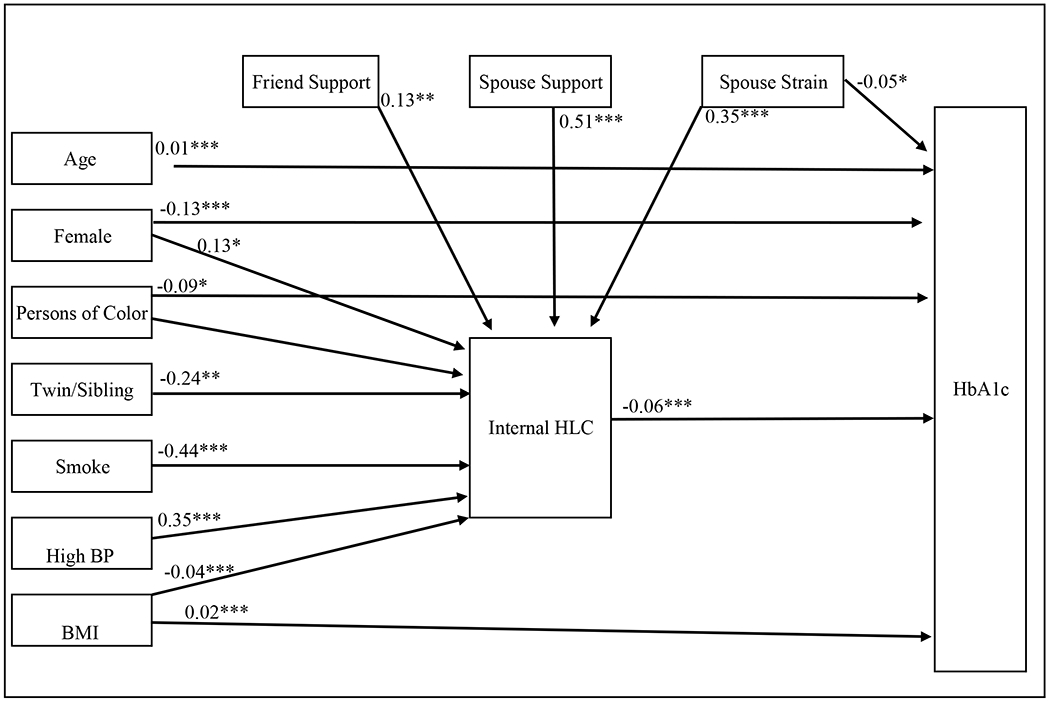
Modified model showing direct paths for HbA1c and Internal HLC
Discussion
This study examined the effects of various sources of social support and strain on HbA1c levels with a national sample of married or cohabiting adults who have not previously been diagnosed with diabetes. Results indicated that social support from friends was associated with lower HbA1c levels, indicating better glycemic control. Meanwhile, the findings regarding other sources of social support and strain were mixed. Specifically, social support from one’s spouse or partner is indirectly related to HbA1c levels, through internal HLC. However, social support from family members is neither mediated by internal HLC nor related to HbA1c in this study.
There are a number of factors that help explain this finding. First, this outcome may be due to the differential importance of relationships throughout the lifespan with varied roles and relative importance shifting throughout one’s life. For instance, prior work suggests that friends and family members may play different roles in adults’ well-being as support networks shift over time (Huxhold, Miche & Schüz, 2013). Similarly, a study of college students found that friends’ support was most impactful on personal growth when family support was low and as impacts from negative life events increased, students reported lower perceived family support (Secor, Limke-McLean, & Wright, 2017). These findings suggest that sources of support shift over time with relative importance waxing and waning with life cycles. Second, the lack of significance among family and friends’ support in the present analysis may be partly due to the sample being limited to only married or cohabiting individuals. Specifically, for married/cohabiting adults, family relationships may be less important (Heinze, Kruger, Reischl, Cupal, & Zimmerman, 2015). Finally, in terms of mortality outcomes, prior longitudinal work has shown that martial relationships and relationships with children are more important than relationships with friends and other family members for adults in midlife and beyond (Birditt & Antonucci, 2008). Overall, the present study’s results suggest that there is a difference in health outcomes relating to social support based on its source (e.g., spouse/partner versus friend).
Additionally, the indirect effect of internal HLC on HbA1c is noteworthy. As noted above, this study’s findings suggest a mediation from spouse/partner support to HbA1c through internal HLC. This aligns with previous findings suggesting a link between social support and locus of control. For instance, prior work has shown a negative association between social support and HLC in preventive health behaviors such as breast self-examination (Holroyd, Molassiotis, & Taylor-Pilliae, 2001), and a joint impact between social support and locus of control on individual outcomes (Fusilier et al., 1987). Grafting into this literature, the present study’s findings suggest that social support’s positive effects may be seen for those who are closest to an individual through a mediation of HLC. Speculatively, having social support from a spouse/partner likely enables individuals to feel as though they have agency to alter their health outcomes, though a threshold effect may be at play here. Specifically, the finding of spouse/partner strain contributing to internal HLC and negatively associating with HbA1c in the supplemental analyses may aid in uncovering layers in the complex association between social support and HLC noted by scholars over the years. For instance, Krause (1987) suggests a threshold for the beneficial outcomes related to social support in relation to locus of control; after that is crossed, additional social support may wash out feelings of internal control. Thus, the association of spouse/partner strain with internal HLC may result from a similar mechanism whereby low levels of strain (or nagging behaviors) may be associated with higher levels of internal HLC.
Study Contributions
Despite the disparate findings, this study makes several contributions that warrant further discussion. First, social support and strain from a variety of sources—friends, family members, and spouse/partner—were included, allowing effects from each to be examined. The present findings indicated that friends and spouses or partners were more influential in glycemic control than family members within the context of married/cohabiting adults who had not been diagnosed with T2D. Although the majority of work relating to social support and T2D centers on its management rather than prevention, these findings are consistent with related research. Specifically, Thomas (2015) found, the relative importance of social support sources tends to vary over the course of a lifetime, with friends playing a more important role for younger and older individuals. Likewise, different types of support may be received from varied sources. For instance, friends may offer more emotional support, whereas family members may provide higher levels of instrumental or informational support (LaGreca et al., 1995). Importantly, prior work has shown that both positive and negative qualities may influence mortality outcomes among adults with chronic illnesses (Birditt & Antonucci, 2008). Within the present study, this may be seen with additional analysis results that showed a direct negative path going from spouse strain to HbA1c. Future research may help shed light on this finding. Yet one potential explanation is that some spousal strain may be due to reminders for healthy lifestyle factors—such as engaging in exercise, eating a healthier diet, or actively addressing other issues—that may be perceived as nagging (e.g., Sandberg, Trief, Greenberg, Graff, & Weinstock, 2006).
The second contribution is the simultaneous examination of effects for social support and social strain. The present study’s findings suggest indirect effects on HbA1c from social support, but not strain. These findings are partially consistent with previous studies, which have reported that social support is related to improved diabetes care (e.g., Tang, Brown, Funnell, & Anderson, 2008), and social strain is related to many negative health outcomes (e.g., Walen & Lachman, 2000). Part of the discrepancy may be that the sample for the present study includes only individuals who have not been diagnosed with diabetes in order to avoid biasing the study’s focus on T2D risk. However, the brunt of research on social strain has examined its effects among individuals who have already been diagnosed with an illness or other chronic health condition (e.g., Orth-Gomér et al., 2000).
Finally, this study contributes to the literature by including internal and external HLC as a possible mediator between social support/strain and HbA1c levels. There are likely many channels through which HbA1c is influenced, but by including psychosocial variables such as social support and HLC, our understanding of factors that may be modified is increased. The present study’s findings point to a mediating effect of internal HLC for social support from a spouse or partner to HbA1c.
Theoretical Implications
There are two main implications from the present study for future theoretical development. First, this study’s findings suggest that social support from one’s spouse or partner is indirectly associated with lower levels of HbA1c, but support from family members did not achieve statistical significance when examining direct effects. In addition, the role of support from friends appears to remain important for health outcomes such as lower HbA1c levels. Prior work has suggested that friendship networks may become smaller as couples enter marriage or cohabitation (Kalmijn, 2003), and that friendships are relatively less important in mortality outcomes compared with marital relationships or relationships with children (Birditt & Antonucci, 2008). Yet, support from friends appears to be associated with a lower risk of T2D within this study, indicating a continued importance for friendships among married/cohabiting adults. Thus, it appears necessary for future research to develop and test theories of social support to further parse out which types of social support are most beneficial from specific sources.
Second, more detailed operationalization of social support and strain constructs may provide more fine-grained distinctions for future researchers. For instance, including items that deal more directly with specific communicative behaviors may provide more fruitful results, compared to asking participants how often their family members get on their nerves or are there when needed (e.g., LaGreca et al., 1995). In addition to providing participants with more clarity for responding, including specific supportive or straining actions would allow a more parsimonious theory to be developed (du Pré, 2005).
Practical Implications
Building upon the theoretical contributions, the current study’s findings have important implications for developing intervention strategies for mitigating Type 2 diabetes risk in adults. Specifically, because spouse or partner support was found to have a significant indirect impact on HbA1c levels, health interventions targeting adults should focus on both improving relationships and increasing internal HLC beliefs. In addition, the finding that shows a negative association between support from friends and HbA1c could allow for additional work to examine other positive outcomes of maintaining supportive friendships for individuals within committed relationships. Further, these interventions may be fruitful at both interpersonal and group levels due to the many factors that are involved with both interpersonal relationships and HLC beliefs.
Specifically, at an interpersonal level, intervention programs may focus on maintaining positive interactions with one’s spouse or other close social contacts. This may come through sharing daily activities, enhancing communication skills, or learning new activities together. Additionally, interventions geared toward making health lifestyle changes may also be fruitful, as was seen with Gorin et al.’s (2008) study on intervention efforts for adults with diabetes. In addition, by aiming intervention efforts at an interpersonal level, many other positive health outcomes may ensue such as increased well-being (e.g., Chen & Feeley, 2014).
Limitations
Despite the contributions of this study, some limitations must be considered when interpreting the findings. First, this study included social support and strain as provided with constructed scales from the MIDUS dataset. Although these scales show acceptable internal consistency, they do not separate different types of social support. Overall, these scales tend to reflect emotional support. Previous research has shown that emotional support may be most beneficial for treatment outcomes (e.g., Helgeson, & Cohen, 1996). However, including all types would be more optimal as different types of social support may be more useful than others, depending on the context in which they are perceived or given (diMatteo, 2004). In addition, these measures have overlapping use for other constructs, such as perceived responsiveness (e.g., Slatcher et al., 2015), which raises questions regarding their validity for all chosen applications. Likewise, social strain was measured in the present study by the constructed scales provided in the MIDUS dataset. Although these scales include items that reflect some unsupportive behaviors, an instrument that addresses various types of strain—such as failing to provide instrumental support, offering bad advice, or sabotaging efforts for healthier outcomes should be included in future research (Mayberry & Osborn, 2012; Newsom, Nishishiba, Morgan, & Rook, 2003). Also of note is the fact that HbA1c levels reflect glycemic variability over a time of two to three months. However, the social support and strain items are not linked to a specific amount of time in which participants are considering while responding. Thus, this measure could be further improved by a closer time link in both the item wording and data collection for the questionnaire and biomarker data.
Second, external HLC was measured with one item. Although the decision to include this measure was made based on what was available within the dataset, it would be more ideal to utilize a stronger instrument. Additionally, both HLC scales were relatively specialized in their scope. Although they were based on a shortened form of the HLC scale, future research should try to include a broader measure of this construct.
Finally, it should be noted that the causal relationships among social support/strain, HLC, and HbA1c cannot be inferred as this is a correlational, cross-sectional study. In order to prevent biasing the results, the present study used a sample of married or cohabiting adults who had not been diagnosed with diabetes. Although this decision was made in order to reduce the risk of bias, it would be beneficial for future primary research to collect data in a manner that would allow greater flexibility and inclusiveness for assessing relational support among all adults. Future research would also benefit from including a longitudinal analysis when the biomarker data are released from MIDUS 3 or other longitudinal studies in order to examine the effects over time and establish a causal order.
Conclusion
This study contributes to the literature through highlighting associations between social support, HLC beliefs, and glycemic control. Among this sample of married or cohabiting adults who have not been diagnosed with diabetes, support from friends is negatively associated with HbA1c levels. In addition, the present study’s findings suggest that spousal support is indirectly related to better glycemic control, and in turn, reduced likelihood of being diagnosed with Type 2 diabetes. This relationship appears to be mediated by internal HLC, suggesting that those who feel as though they can alter their health outcomes are indeed less likely to develop Type 2 diabetes in the near future. Future research may benefit from analyzing other types of social support and strain, as well as differentiating between perceived and received support.
Acknowledgments
This work was conducted while the author was completing a doctoral program at University at Buffalo, The State University of New York. A previous version of this paper was presented at the National Communication Association conference. The completion of this research was supported, in part, by a cancer prevention fellowship for Kristin Maki, supported by the Cancer Prevention and Research Institute of Texas grant award, RP170259, Shine Chang, PhD, Principal Investigator, and by the MD Anderson Cancer Center Support Grant, CA016672, funded by the National Cancer Institute.
This study uses the public-use MIDUS dataset. The MIDUS dataset is supported by John D. and Catherine T. MacArthur Foundation Research Network, National Institute on Aging (P01-AG020166), National institute on Aging (U19-AG051426). Biomarker data collection was further supported by the NIH National Center for Advancing Translational Sciences (NCATS) Clinical and Translational Science Award (CTSA) program as follows: UL1TR001409 (Georgetown); UL1TR001881 (UCLA); 1UL1RR025011 (UW)
Footnotes
As part of IARR’s encouragement of open research practices, the author has provided the following information: This research was not pre-registered.
The data used in the research are available. The data can be obtained at: https://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/4652?archive=ICPSR&q=MIDUS+ The materials used in the research are available. The materials can be obtained at: https://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/4652?archive=ICPSR&q=MIDUS+
References
- Birditt K & Antonucci TC, (2008). Life sustaining irritations? Relationship quality and mortality in the context of chronic illness. Social Science & Medicine, 67(8), 1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blom M, Janszky I, Balog P, Orth-Gomér K, & Wamala SP (2003). Social relations in women with coronary heart disease: the effects of work and marital stress. European Journal of Cardiovascular Risk, 10(3), 201–206. [DOI] [PubMed] [Google Scholar]
- Chen Y, & Feeley TH (2014). Social support, social strain, loneliness, and well-being among older adults: An analysis of the Health and Retirement Study*. Journal of Social and Personal Relationships, 31(2), 141–161. [Google Scholar]
- Clark ML & Utz SW (2014). Social determinants of type 2 diabetes and health in the United States. World Journal of Diabetes, 5(3), 296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coty MB, & Wallston KA (2010). Problematic social support, family functioning, and subjective well-being in women with rheumatoid arthritis. Women & Health, 50(1), 53–70. [DOI] [PubMed] [Google Scholar]
- de Guzman AB, Jurado JBN, & Juson AJA (2015). Examining the structural relationship of chronic illness, physical function, life satisfaction, and social support in the development of depression among Filipino elderly in institutionalized settings. Educational Gerontology, 41(3), 193–206. [Google Scholar]
- DiMatteo MR (2004). Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology, 23(2), 207–218. [DOI] [PubMed] [Google Scholar]
- du Pré A (2005). Communicating about health: Current issues and perspectives (2nd ed.). New York: Oxford University Press. [Google Scholar]
- Edelman D, Olsen MK, Dudley TK, Harris AC, & Oddone EZ (2004). Utility of hemoglobin A1c in predicting diabetes risk. Journal of General Internal Medicine, 19(12), 1175–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman KL, Hay EL, & Birditt KS (2004). The best of ties, the worst of ties: Close, problematic, and ambivalent social relationships. Journal of Marriage and Family, 66(3), 792–808. [Google Scholar]
- Fusilier MR, Ganster DC, & Mayes BT (1987). Effects of social support, role stress, and locus of control on health. Journal of Management 13(3), 517–528. [Google Scholar]
- Global Diabetes Community. (n.d.). Guide to HbA1c. Retrieved June 25, 2019, from http://www.diabetes.co.uk/what-is-hba1c.html [Google Scholar]
- Gonzalez-Zacarias AA, Mavarez-Martinez A, Arias-Morales CE, Stoicea N & Rogers B (2016). Impact of demographic, socioeconomic, and psychological factors on glycemic self-management in adults with Type 2 diabetes mellitus. Frontiers in Public Health, 4, 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, … & DiLillo VG (2008). Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. International Journal of Obesity, 32(11), 1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris ML, Oldmeadow C, Hure A, Luu J, Loxton D, & Attia J (2017). Stress increases the risk of type 2 diabetes onset in women: A 12-year longitudinal study using causal modeling. PLoS One, 12(2), e0172126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze JE, Kruger DJ, Reischl TM, Cupal S, & Zimmerman MA (2015). Relationships among disease, social support, and perceived health: A lifespan approach. American Journal of Community Psychology, 56(3–4), 268–279. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, & Cohen S (1996). Social support and adjustment to cancer: Reconciling descriptive, correlational, and intervention research. Health Psychology, 15(2), 135. [DOI] [PubMed] [Google Scholar]
- Hendryx M, Nicholson W, Manson JE, Kroenke CH, Lee J, Weitlauf JC, Garcia L, Jonasson JM, Wactawski-Wende J, & Luo J (2019). Journal of Gerontology Series B, Psychological Social Sciences, 1–12, doi: 10.1093/geronb.gbz047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Harris MA, & Weissberg-Benchell J (2012). Diabetes resilience: A model of risk and protection in type 1 diabetes. Current Diabetes Reports, 12(6), 739–748. [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Yi-Frasier JP, Hessler D, Butler AM, Anderson BJ, & Jaser S (2016). Stress and A1c among people with diabetes across the lifespan. Current Diabetes Reports, 16(8), 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holroyd EA, Molassiotis A, & Taylor-Pilliae RE (2001). Filipino domestic workers in Hong Kong: Health related behaviors, health locus of control and social support. Women & Health, 33(1–2), 181–205, doi: 10.1300/J013v33n01_11 [DOI] [PubMed] [Google Scholar]
- Huxhold O, Miche M, & Schüz B (2013). Benefits of having friends in older ages: Differential effects of informal social activities on well-being in middle-aged and older adults. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(3), 366–375, doi: 10.1093/geronb/gbt029. [DOI] [PubMed] [Google Scholar]
- IDF. (2017). IDF Diabetes Atlas 8th Edition Revision 2017. International Diabetes Federation. Available at: http://www.idf.org/diabetesatlas (accessed June 27, 2019). [Google Scholar]
- Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, … & Matthews DR (2015). Management of hyperglycemia in type 2 diabetes, 2015: A patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care, 38(1), 140–149. [DOI] [PubMed] [Google Scholar]
- Juárez-Ramírez C, Théodore FL, Villalobos A, Jiménez-Corona A, Lerin S, Nigenda G, & Lewis S (2015). Social support of patients with Type 2 diabetes in marginalized contexts in Mexico and its relation to compliance with treatment: A sociocultural approach. PloS one, 10(11), e0141766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn M (2003). Shared friendship networks and the life course: An analysis of survey data on married and cohabiting couples. Social Networks, 25(3), 231–249. [Google Scholar]
- Krause N (1987). Understanding the stress process: Linking social support with locus of control beliefs. Journal of Gerontology, 42(6), 589–593. [DOI] [PubMed] [Google Scholar]
- Kumari M, Head J, & Marmot M (2004). Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Archives of Internal Medicine, 164(17), 1873–1880. [DOI] [PubMed] [Google Scholar]
- LaGreca AM, Auslander WF, Greco P, Spetter D, Fisher Eb Jr., & Santiago JV (1995). I get a little help from my family and friends: Adolescents’ support for diabetes care. Journal of Pediatric Psychology, 20, 449–476. [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, & Sherwood A (2005). Social support and coronary heart disease: Epidemiologic evidence and implications for treatment. Psychosomatic Medicine, 67(6), 869–878. [DOI] [PubMed] [Google Scholar]
- Lindström M, & Rosvall M (2012). Marital status, social capital and health locus of control: A population-based study. Public Health, 126(9), 790–795. [DOI] [PubMed] [Google Scholar]
- Macaden L & Clarke CL (2010). The influence of locus of control on risk perception in older South Asian people with Type 2 diabetes in the UK. Journal of Nursing and Healthcare of Chronic Illness, 2(2), 144–152. [Google Scholar]
- Maki KG (2018). The relationship between social support and Type 2 Diabetes risk. Communication Research Reports, 35(1), 12–21. [Google Scholar]
- Marr J & Wilcox S (2015). Self-efficacy and social support mediate the relationship between internal health locus of control and health behaviors in college students. American Journal of Health Education, 46(3), 122–131. [Google Scholar]
- Mayberry LS, & Osborn CY (2012). Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care, 35(6), 1239–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MIDUS. (n.d.). MIDUS - Midlife in the United States, A national longitudinal study of health and well-being. Retrieved January 14, 2020, from http://www.midus.wisc.edu/data/timeline.php [Google Scholar]
- Morowatisharifabad M, Mazloomy Mahmoodabad S, Baghianimoghadam M, & Rouhani Tonekaboni N (2009). Relationships between locus of control and adherence to diabetes regimen. Journal of Research in Health Sciences, 9(1), 37–44. [PubMed] [Google Scholar]
- Náfrádi L, Nakamoto K, & Schulz PJ (2017). Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS ONE, 12(10):e0186458. doi: 10.1371/journal.pone.0186458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsom JT, Nishishiba M, Morgan DL, & Rook KS (2003). The relative importance of three domains of positive and negative social exchanges: A longitudinal model with comparable measures. Psychology and aging, 18(4), 746. [DOI] [PubMed] [Google Scholar]
- Ng DM, & Jeffery RW (2003). Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology, 22(6), 638. [DOI] [PubMed] [Google Scholar]
- Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson, & Weinehall L (2007). Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diabetes Research and Clinical Practice, 76(3), 368–377. [DOI] [PubMed] [Google Scholar]
- Noor NM (1995). Job-role quality and women’s psychological well-being: Locus of control and social support as moderators. Journal of Community & Applied Social Psychology, 5(4), 259–272. [Google Scholar]
- Oh HJ & Lee B (2012). The effect of computer-mediated social support communities on patient empowerment and doctor-patient communication. Health Communication, 27, 30–41. Doi: 10.1080/10410236.2011.567449 [DOI] [PubMed] [Google Scholar]
- O’hea EL, Grothe KB, Bodenlos JS, Boudreaux ED, White MA, Brantley PJ (2005). Predicting medical regimen adherence: The interactions of health locus of control beliefs. Journal of Health Psychology, 10(5), 705–717. doi: 10.1177/1359105305055330 [DOI] [PubMed] [Google Scholar]
- Orth-Gomér K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, & Mittleman MA (2000). Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. Jama, 284(23), 3008–3014. [DOI] [PubMed] [Google Scholar]
- O’Sullivan CJ, Hynes N, Mahendran B, Andrews EJ, Avalos G, Tawfik S, … & Sultan S (2006). Haemoglobin A1c (HbA1C) in non-diabetic and diabetic vascular patients: Is HbA1C an independent risk factor and predictor of adverse outcome?. European Journal of Vascular and Endovascular Surgery, 32(2), 188–197. [DOI] [PubMed] [Google Scholar]
- Roddenberry A, & Renk K (2010). Locus of control and self-efficacy: potential mediators of stress, illness, and utilization of health services in college students. Child Psychiatry & Human Development, 41(4), 353–370. [DOI] [PubMed] [Google Scholar]
- Ryff R, Almeida DM, Ayanian JS, Carr DS, Cleary PD, Coe C, … Williams D (2007). Midlife Development in the United States (MIDUS II), 2004-2006 [Computer file]. ICPSR040652-v1. Ann Arbor, MI: Inter-University Consortium for Political and Social Research; [distributor]. [Google Scholar]
- Ryff CD, Seeman T & Weinstein M Midlife in the United States (MIDUS 2): Biomarker Project, 2004-2009. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [distributor], 2019-March-27. 10.3886/ICPSR29282.v9 [DOI] [Google Scholar]
- Sandberg J, Trief PM, Greenberg RP, Graff K, & Weinstock RS (2006). He said, she said: The impact of gender on spousal support in diabetes management. Journal of Couple & Relationship Therapy, 5(2), 23–42. [Google Scholar]
- Schumacker RE, & Lomax RG (2010). A Beginner’s Guide to Structural Equation Modeling (3rd ed.). New York, NY: Routledge. [Google Scholar]
- Schwartz LS, Coulson LR, Toovy D, Lyons JS, & Flaherty JA (1991). A biopsychosocial treatment approach to the management of Diabetes Mellitus. General Hospital Psychiatry, 13, 19–26. [DOI] [PubMed] [Google Scholar]
- Secor SP, Limke-McLean A, & Wright RW (2017). Whose support matters? Support of friends (but not family) may predict affect and wellbeing of adults faced with negative life events. Journal of Relationships Research, 8(e10), 1–10, doi: 10.1017/jrr2017.10 [DOI] [Google Scholar]
- Selcuk E, & Ong AD (2013). Perceived partner responsiveness moderates the association between received emotional support and all-cause mortality. Health Psychology, 32, 231–235. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, & Huang B (2006). A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychology, 25(1), 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher RB, Selcuk E, & Ong AD (2015). Perceived partner responsiveness predicts diurnal cortisol profiles 10 years later. Psychological Science, 26(7), 972–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A & Wardle J (2001). Locus of control and health behavior revisited: A multivariate analysis of young adults from 18 countries. British Journal of Psychology, 92, 659–672. [DOI] [PubMed] [Google Scholar]
- Tang TS, Brown MB, Funnell MM, & Anderson RM (2008). Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. The Diabetes Educator, 34(2), 266–276. [DOI] [PubMed] [Google Scholar]
- Tankova T, Chakarova N, Dakovska L, & Atanassova I (2012). Assessment of HbA1c as a diagnostic tool in diabetes and prediabetes. Acta Diabetologica, 49, 317–378. [DOI] [PubMed] [Google Scholar]
- Teo AR, Choi H, & Valenstein M (2013). Social relationships and depression: Ten-year follow-up from a nationally representative study. PloS One, 8(4), e62396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas PA (2015). The impact of relationship-specific support and strain on depressive symptoms across the life course. Journal of Aging and Health, 0898264315591004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toljamo M, & Hentinen M (2001). Adherence to self-care and social support. Journal of Clinical Nursing, 10(5), 618–627. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Holt-Lunstad J, Uno D, & Flinders JB (2001). Heterogeneity in the social networks of young and older adults: Prediction of mental health and cardiovascular reactivity during acute stress. Journal of Behavioral Medicine, 24(4), 361–382. [DOI] [PubMed] [Google Scholar]
- Uchino BN (2013). Understanding the links between social ties and health: On building stronger bridges with relationship science. Journal of Social and Personal Relationships, 30(2), 155–162. [Google Scholar]
- Walen HR, & Lachman ME (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17(1), 5–30. [Google Scholar]
- Wallston BS, Alagna SW, DeVellis BM, & DeVellis RF (1983). Social support and physical health. Health Psychology, 2(4), 367. [Google Scholar]
- Wallston BS, Wallston KA, Kaplan GD, & Maides SA (1976). Development and validation of the health locus of control (HLC) scale. Journal of Consulting and Clinical Psychology, 44(4), 580. [DOI] [PubMed] [Google Scholar]
- Wardian J, & Sun F (2014). Factors associated with diabetes-related distress: Implications for diabetes self-management. Social Work in Health Care, 53(4), 364–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YC, Schorpp K, & Harris KM (2014). Social support, social strain and inflammation: Evidence from a national longitudinal study of U.S. adults. Social Science & Medicine, 107, 124–135. [DOI] [PMC free article] [PubMed] [Google Scholar]


