Abstract
Attention-Deficit/Hyperactivity Disorder (ADHD) is highly prevalent among adolescent clinical populations and associated with myriad deficits in school functioning. Yet, behavior therapists have few developmentally appropriate tools for addressing school problems in this group. This article introduces a behavioral protocol designed to fill the gap: Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA). CASH-AA is a family-based intervention that targets home environment, adolescent skills, and family-school partnership characteristics in order to improve school performance. Protocol components are derived from three evidence-based approaches for adolescent behavior problems: family psychoeducation, clinical family interventions to heighten adolescent and caregiver motivation to change, and training interventions for homework planning and organization skills. CASH-AA contains four treatment modules: (1) Psychoeducation: ADHD and Academic Functioning; (2) Motivation & Preparation: Home Academic Environment; (3) Behavior Change: School Attendance and Homework Plan; (4) Collaboration: Therapist-Family-School Partnership. The protocol can be implemented as a stand-alone intervention for ADHD or an adjunct to other behavioral interventions for co-occurring disorders. Two case examples with markedly different treatment profiles are presented to illustrate the utility and flexibility of the protocol.
Keywords: adolescent ADHD, family-based treatment, psychoeducation, training interventions
Introduction
As described below, Attention-Deficit/Hyperactivity Disorder (ADHD) is highly prevalent among adolescent clinical populations as both a primary reason for referral and a co-occurring disorder among teenagers presenting with conduct, anxiety and depression, and substance use problems. Adolescents with ADHD often present with myriad school problems in the domains of school achievement, learning difficulties, and behavioral infractions, all of which complicate treatment planning efforts. The most common treatment option, pharmacological intervention, has proven generally effective in reducing ADHD behavioral symptoms. However, medications have not demonstrated strong or consistent impacts on academic functioning. Moreover, most behavioral interventions1 that strengthen school outcomes in younger children with ADHD are either developmentally inappropriate or unproven for adolescents. Thus behavior therapists have few viable options for treating ADHD-related school problems in their teenage clients.
This paper addresses the need for academic interventions for adolescents with ADHD by introducing a behavioral treatment protocol designed to be implemented in clinical settings: Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA). CASH-AA is a family-based protocol that in intended to improve school performance by targeting home environment, adolescent skills, and family-school partnership characteristics that directly support academic success. CASH-AA contains intervention components derived from three evidence-based approaches for adolescents with ADHD and co-occurring disorders: ADHD psychoeducation, family-based treatment engagement and motivational techniques, and training interventions for homework planning and organizational skills. These three approaches are integrated into the four CASH-AA treatment modules presented below. Two case studies are presented to illustrate the utility of the protocol in routine clinical settings.
Rationale for Developing a Family-Based Clinical Protocol to Improve School Functioning in Adolescents with ADHD
ADHD Prevalence in General and Clinical Adolescent Populations
Knowledge about the prevalence of ADHD in adolescent populations has grown enormously over the past decade. There is now consensus that ADHD is a chronic childhood mental health condition that persists across the developmental span of adolescence and into young adulthood (Taylor, 2009). The newest national prevalence data on ADHD in adolescents gathered by the National Survey of Children’s Health (Visser et al., 2014) indicate that 14% of children aged 11-17 have received an ADHD diagnosis at some point in their lives. Based on these and similar data (e.g., Merikangas et al., 2011; Schwarz & Cohen, 2013), ADHD affects almost one in 5 teen boys and 1 and 10 teen girls. These rates confirm its status as the most prevalent behavioral disorder among teenagers (Merikangas et al., 2011).
With regard to youth seeking behavioral treatment, ADHD is a leading reason for referral among children age 3-12 (Yeh et al., 2002). It is also highly prevalent among adolescents, affecting between 18-48% of those enrolled in outpatient mental health and substance use services (Tims et al., 2002; Turner et al., 2004; Wu et al., 2011). These are conservative estimates of clinical prevalence given that ADHD has been traditionally underdiagnosed in adolescent clinical samples, due in large part to deficiencies in the developmental sensitivity of diagnostic criteria (Sibley et al., 2012; Todd, Huang, & Henderson, 2008)2. Also it is frequently undetected when co-occurring with other chronic psychiatric disorders for which teens are typically referred: oppositional defiant and conduct disorder, anxiety, depression, and substance use (see Merikangas et al., 2011). Rates of ADHD comorbidity for disruptive behavior disorders and substance use problems among teenagers enrolled in outpatient treatment typically exceed 70% (e.g., Chan, Dennis, & Funk, 2008; Thompson, Whitmore, Raymond, & Crowley, 2006). Based on these estimates, of the 2.8 million adolescents enrolled annually in outpatient mental health care (SAMHSA, 2009), combined with 125,000 in outpatient substance use treatment (SAMHSA, 2007) and tens of thousands more receiving behavioral services in nonspecialty settings (e.g., school mental health, juvenile justice, child welfare; Jones, Foster, & CPPRG, 2009), approximately 20-50% meet diagnostic criteria for ADHD. These data suggest that the outpatient behavioral care system contains between 750,000 and 1.5 million teenagers with ADHD on a yearly basis.
ADHD in Adolescents is Linked to Impaired School Functioning
Adolescents who meet full diagnostic criteria for ADHD present well-documented behavioral deficits in attention, self-regulation, and social competence (Barkley, 2006). These behavioral symptoms typically precipitate school behavior problems that include inconsistent attendance, poor grades, disruptive classroom behavior, time management and planning deficits, and a disorganized approach to academics (Kent et al., 2011; Kuriyan et al., 2013). Youth with ADHD also suffer a high rate of learning difficulties of several kinds (Cutting & Denckla, 2003) that create an additional barrier to academic achievement (Bussing et al., 2012). Like ADHD, learning disabilities are considered chronic conditions that require intensive intervention and ongoing management (Fletcher, Lyon, Fuchs, & Barnes, 2007). These ADHD-related behavioral and learning problems together lead to greater incidence of grade retention and dropout and incur enormous costs in educational support services (Robb et al., 2011).
Additionally, clinical neuroscience has begun to map neurocognitive risk factors associated with childhood ADHD that routinely persist into adolescence, particularly executive functioning deficits in planning, cognitive flexibility, working memory, and processing speed (e.g., Coolidge, Thede, & Young, 2000). Executive dysfunction exacerbates, and may underlie, behavioral and learning problems experienced by youth with ADHD (Barkley, 2006), and it affects social as well as academic functioning (Langberg, Dvorsky, & Evans, 2013). Thus the confluence of poor attention and self-regulation, learning difficulties, and for many, executive functioning deficits creates a profile of compounded impairment that compromises school performance and complicates treatment planning for adolescents with ADHD.
Medication is Not (Usually) Sufficient to Address School Problems for Adolescents with ADHD
Stimulant medication is recommended by many as the first-line treatment option for ADHD in adolescents (Faraone & Buitelaar, 2010). There is solid evidence that rapid-acting stimulants such as methylphenidate (Ritalin) are effective in reducing ADHD symptoms and improving social functioning in teens (Sibley, Kuriyan, Evans, Waxmonsky, & Smith, 2014). Recent data suggest that extended-release stimulants such as OROS-MPH (Concerta) are also safe, well tolerated, and effective in reducing ADHD symptoms for this age group (e.g., McGough et al., 2006). Effect sizes for OROS-MPH (e.g., Wilens et al., 2006) and other once-daily medications are in the medium-to-large range for symptom reduction among teenagers, which is consistent with meta-analytic findings for immediate-release medication (Sibley, Kuriyan, et al., 2014).
However, stimulant medications are not a panacea for treating adolescents with ADHD. ADHD medication compliance declines precipitously from childhood through adolescence (Sanchez et al., 2005). This is likely due to the inconvenience, stigma, and side effects of medication, combined with decreases in adult monitoring and increases in adolescent autonomy and self-care (Sanchez et al., 2005). In addition, parents tend to prefer behavioral interventions to medication as a treatment option (e.g., Johnston, Hommersen, & Seipp, 2008; Waschbusch et al., 2011). A recent study found that adolescents could not reliably discern whether they were taking active ADHD medication or placebo and rarely attributed behavioral effects to the given pill (Pelham et al., 2013), suggesting that teens may not be generally disposed to advocate for their own medication. Also, due to widespread fragmentation of pharmacological versus behavioral services in usual care (Institute of Medicine, 2006), adolescents with ADHD often have trouble accessing medication interventions in behavioral care settings.
Most importantly there is little consistent evidence that, beyond symptom reduction, ADHD medications improve school functioning in teens. Whereas some research shows that medication improves academic performance and classroom behavior in analogue settings (Evans et al., 2001), other studies indicate that these benefits may not extend to actual school settings. For example, the landmark Multimodal Treatment of ADHD study found that children assigned to a stimulant medication regimen who were still taking medication 6 to 8 years later showed virtually no advantages in academic functioning over study youth who were no longer taking medication, with the exception of math achievement scores (Molina et al., 2009). A recent meta-analysis of longitudinal studies found that ADHD medication produced minimal gains in standard scores and negligible effects on school grades and retention rates across the age span (Langberg & Becker, 2012). Thus for teenagers with ADHD, medications alone have not proven to be reliably acceptable, accessible, and effective enough to boost academic outcomes.
ADHD Behavioral Management Interventions Do Not (Readily) Translate to Adolescent Populations
Psychosocial interventions for childhood ADHD can be separated into two broad treatment approaches: behavior management, and training interventions (Evans, Owens, & Bunford, in press). Behavior management (BM) is intended to lead to behavior change by manipulating contingencies in the target environment. Once targeted behaviors are changed, then generalization and maintenance of behavior change can be achieved by fading the modified contingencies and connecting the child to naturally occurring contingencies (Stokes & Baer, 1977). BM has been a well-established approach for childhood ADHD for over two decades and includes strong empirical support for several BM models, notably behavioral parent training, behavioral classroom management, and behavioral peer interventions (usually in the form of intensive summer programs) (Evans et al., in press). By definition, behavioral classroom management targets school problems in school settings. Behavioral parent training and behavioral peer interventions also routinely target school-related issues as either primary or secondary treatment goals.
The wealth of evidence demonstrating BM effectiveness for ADHD symptom reduction and improved social and school functioning is restricted to elementary-school aged children between 4 and 12 years of age. No randomized trials of the various BM models have focused on adolescents, and few have included adolescent participants (Evans et al., in press). Given the manifold developmental changes occurring within children as they progress through puberty and transition into young adulthood, it is imprudent to generalize the effectiveness of BM to adolescent populations in the absence of adolescent-specific research. Moreover, BM interventions for adolescents face steep implementation barriers in both home and school settings. Teens are monitored by adults less closely than younger children; identifying salient behavioral rewards for adolescents is challenging; and numerous teachers interact with teens throughout the school day, with individual teachers seeing students for relatively brief amounts of time. It therefore appears doubtful that BM can be readily adapted to address school functioning in the older group (see Fabiano et al., 2009).
ADHD Training Interventions are a Promising Approach for Treating School Problems in Adolescents
The second category of psychosocial interventions for ADHD is training interventions (TIs). TIs induce change by improving the skill set of the child and, in some cases, providing reinforcement and punishment in the training setting for behavior change that occurs outside of that setting. The TI category includes social skills training programs, which have been tested in various formats for decades, as well as emerging interventions in the form of neurofeedback (Gevensleben et al., 2009), cognitive enhancement (Beck, Hanson, Puffenberger, Benninger, & Benninger, 2010), and organization skills training (e.g., Abikoff et al., 2013; Langberg, Epstein, Becker, Girio-Herrera, & Vaughn, 2012). The addition of TI models to the relatively modest arsenal of psychosocial interventions for ADHD has been an important shift in the focus of treatment development for this disorder. Whereas early efforts at social skills training were not generally successful for ADHD youth, recent TI models aimed at enhancing cognitive competencies and organization habits show promise among elementary school children, though only organization skills training can be considered well-established (see Chacko et al., in press; Evans et al., in press).
Unlike BM, TIs are individual skills-based interventions that do not rely on adults in the home and school environments to reliably implement modified contingencies. This represents an obvious advantage in implementation feasibility and flexibility for adolescent populations in various care settings, making TIs a logical focus of treatment development efforts for this age group. Still, although there is an assumption that TIs produce change in competencies that persist over time and across settings, this potential generalization advantage has not yet been demonstrated for any group.
TIs have been used in a few studies focused specifically on adolescents, with promising results for social and organizational skills training (Evans et al., in press; Sibley, Kuriyan, et al., 2014) but no evidence yet supporting cognitive enhancement training (Sibley, Kuriyan, et al., 2014). Almost all TI studies have occurred in school settings, a natural choice given that adolescents are difficult to engage in outpatient settings (Merikangas et al., 2011) and benefit substantially from having services in easy reach as school-day or after-school programming (Schultz, Storer, Watabe, Sadler, & Evans, 2011). For example Langberg and colleagues (2012) evaluated an 11-week intervention provided by school mental health professionals in middle schools that involved training students to organize their school materials, track and monitor assignments, and plan evening homework completion. The intervention improved organization, homework, and family conflict based on parent (but not teacher) report. Similarly, the Challenging Horizons Program (CHP; Evans et al., 2011) is a multimodal school-based program for adolescents with ADHD that targets impairment related to organization, academic skills, and social functioning. CHP has been implemented as both an in-school and after-school program in middle and high schools, demonstrating significant improvements in academic and social functioning (e.g., Evans et al., 2007, 2011; Molina et al., 2008; Schultz et al., 2009).
Need for a Family-Based Clinical Protocol to Improve School Outcomes for Adolescents with ADHD
As stated above, TI programs located in school settings enjoy great leverage for targeting academic and behavioral outcomes among students with ADHD. Yet, school-based TIs cannot satisfy the full marketplace demand for academic interventions among adolescents presenting for behavioral services outside the school setting. For one thing, it is usually impractical for clinicians working in other systems to refer their adolescent clients to school-located programs, and school-based TIs currently exist in few school districts. Also, clinically referred families may be unprepared to benefit from school-based TIs. Many have elevated levels of disorganization and stress (Repetti, Taylor, & Seeman, 2002) that can disrupt the generalization of school-trained academic skills into the home setting, and many have ambivalent or contentious relationships with school personnel that can undermine efforts to enroll and sustain teens in school services. Moreover, clinical adolescent populations are often disengaged or truant from school (Armstrong & Costello, 2002) or otherwise deemed ineligible for interventions in school settings. In such cases, outpatient treatment usually focuses on re-engaging youths in school or educational alternatives.
For all these reasons, behavior therapists working outside school settings need to have effective tools to address school performance deficits in adolescent clients with ADHD. Some exploratory research on cognitive-behavioral (Antshel, Faraone, & Gordon, 2012) and family-focused (Sibley, Altszuler, et al., 2014) clinic-based approaches have been reported, as well as preliminary evidence supporting the STAND program (Sibley et al., 2013). This article introduces another such tool, a modular protocol that combines evidence-based family interventions, ADHD psychoeducation, and TIs for adolescents with ADHD: Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA). A family-based approach to academic interventions is well suited for overcoming limitations in the clinical reach of school-based TIs (Orr, Miller, & Polson, 2007). First, clinical family interventions can directly target parent and youth motivation for school involvement among teens who are enrolled in outpatient care but disconnected from school (Hogue & Liddle, 2009). Second, they are an appropriate vehicle for intervening in the family processes and home ecology of teens with ADHD in order to engineer more productive homework routines and stronger family-school connections (Robin, 2006). This includes incorporation of selected BM interventions (e.g., behavior contracting) as needed to promote school attendance among truant teens. In this manner, clinical family interventions can help prepare the home soil so that TIs take proper root among adolescents with ADHD.
Evidence Base for the Three Primary Components of the CASH-AA Protocol
CASH-AA integrates components from three evidence-based behavioral approaches: family psychoeducation in ADHD, family therapy models for adolescent conduct and substance use problems, and TIs for adolescents with ADHD. Figure 1 depicts a conceptual model of the CASH-AA protocol, including evidence-based intervention components, hypothesized mechanisms of change, and targeted clinical outcomes. As described below, the protocol is intended to (a) enhance clinician confidence and technical knowledge in treating ADHD as either a primary or co-occurring disorder for adolescent cases and (b) supply research-proven behavioral tools for addressing school-related impairments that are highly prevalent among youth with ADHD and often resistant to pharmacological intervention (Sibley, Kuriyan, et al., 2014). Similar “family-school” interventions exist for improving academic outcomes in youth with ADHD, including programs for younger children that feature parent training sessions (e.g., Habboushe et al., 2001; Pfiffner et al., 2007) and two models for adolescents that feature ADHD psychoeducation and joint parent-adolescent interventions to support academic achievement (Raggi et al., 2009; Sibley et al., 2013). CASH-AA is unique in featuring clinical family interventions to heighten adolescent and caregiver motivation to change, as well as behavioral interventions that specifically target school attendance, both of which appear essential for treating ADHD in high-risk, clinically referred teens.
Figure 1.
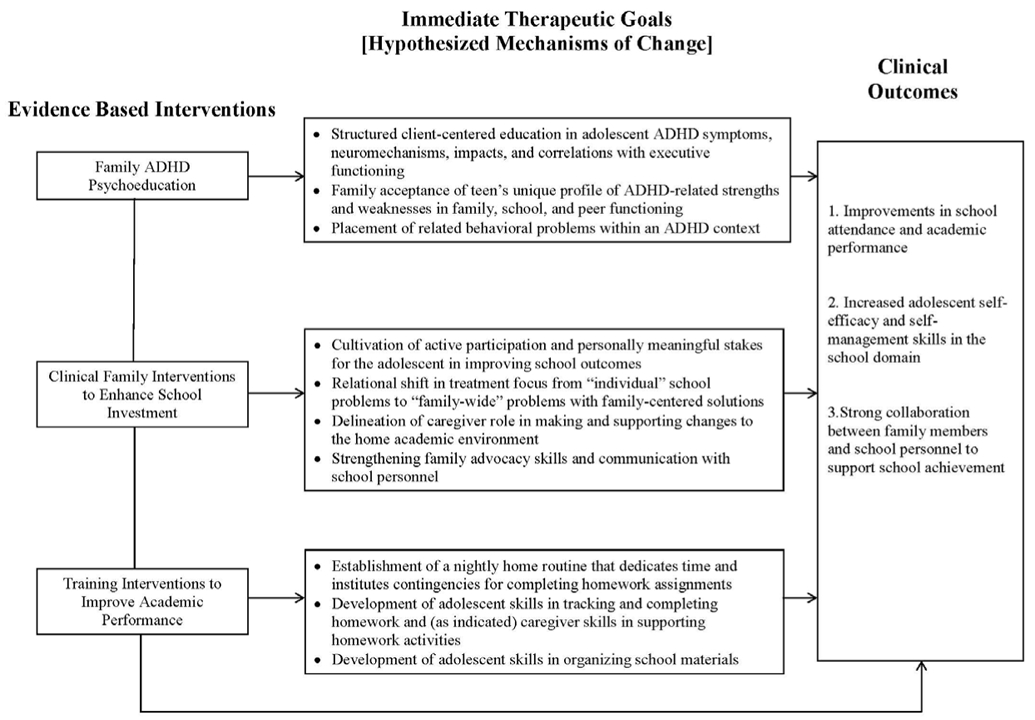
Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA) Conceptual Model: Interventions, Mechanisms, and Outcomes.
Family Psychoeducation in ADHD among Adolescents
Family ADHD psychoeducation refers to a set of interactive educational interventions that provide structured information about symptoms, course of the disorder, impacts on multiple domains of functioning (family, school, peers), and individual differences associated with ADHD in adolescents. This information is packaged in an easy-to-digest format and sets the stage for developing a unique family profile of ADHD symptoms and related behavioral characteristics for each client (e.g., Lopez, Toprac, Crimson, Boemer, & Baumgartner, 2005; McCleary & Ridley, 1999). Psychoeducation in mental health disorders has been shown to enhance behavioral treatment effects (e.g., Fristad, 2006) and improve treatment adherence (Vieta, 2005) as well as medication compliance (Cummings & Fristad, 2007) for a variety of behavioral problems. Several family psychoeducation protocols have been tested as adjunctive treatment components in behavioral care for childhood disorders other than ADHD, including depression (Sanford et al., 2006), bipolar disorder (Fristad, 2006), and eating disorders (Geist, Heinmaa, Stephens, Davis, & Katzman, 2000).
Clinical Family Interventions to Enhance School Investment
Previous research on family-based treatments to reduce parent-child conflict among families of adolescents with ADHD (Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001; Barkley, Guevremont, Anastopoulos, & Fletcher, 1992) generated modest evidence of reliable treatment effects. Rather than targeting family conflict, CASH-AA clinical family interventions are designed to increase family motivation to make meaningful changes in school functioning. These interventions are drawn from two empirically supported family therapy models for adolescent behavior problems. First, adolescent engagement interventions are derived from Multidimensional Family Therapy (MDFT), which has proven effective in treating adolescent substance use and conduct problems (e.g., Liddle et al., 2008; Rigter et al., 2013) and also boosting school attendance, behavior, and grades (Liddle et al., 2001, 2009). Adolescent engagement interventions specifically address adolescent investment in working on school-related issues in therapy by (a) developing a personally meaningful treatment agenda for school functioning in which teens can be motivated participants and (b) (re)moralizing teens by generating hope that school-related problems can and will improve (Diamond, Liddle, Hogue, & Dakof, 1999; Liddle, 1995).
Second, interventions for relabeling ADHD behaviors and reframing individual problems as family problems are derived from Functional Family Therapy (FFT), a model designed to alter dysfunctional family patterns that contribute to adolescent delinquency and substance use (Alexander, Robbins, & Sexton, 2000; Sexton & Alexander, 2003). FFT family motivation and change planning interventions are used to link adolescent school problems to family processes and create positive expectations for change (e.g., Robbins, Turner, Alexander, & Perez, 2003). Specifically, FFT relabeling and reframing techniques (Alexander, Waldron, Barton, & Mas, 1989; Robbins, Alexander, Newell, & Turner, 1996; Robbins, Alexander, & Turner, 2000) launch an ongoing therapy dialogue on connections among ADHD symptoms, family involvement in school performance, and family commitment to improve school outcomes. Finally, FFT case management interventions facilitate stronger connections between family members and key social institutions (e.g., schools, religious and/or recreational organizations, juvenile justice) to augment in-session interventions and foster prosocial adolescent development (Sexton & Alexander, 2003).
Training Interventions to Improve Academic Performance in Adolescents with ADHD
CASH-AA training interventions derive from the Challenging Horizons Program (CHP), a multimodal school-based intervention for adolescents with ADHD described above. The specific TIs adapted from CHP have two foci: homework planning skills (Evans, Pelham, & Grudberg, 1994; Evans et al., 2006; Gureasko-Moore, DuPaul, & White, 2006) and organizational interventions for managing school materials (Evans, Axelrod, & Langberg, 2004; Sadler, Evans, Schultz, & Zoromski, 2011). Controlled studies of CHP across multiple school settings have demonstrated long-term program benefits in non-academic outcomes such as ADHD symptom reduction (Evans et al., 2011; Evans, Serpell, Schultz, & Pastor, 2007) and enhanced social functioning (Evans et al., 2007; Sadler et al., 2011). CHP studies also report academic benefits such as improved organization of materials that predicted improved classroom performance (Evans et al., 2009) and promising trends for raised grade point averages (Evans et al., 2007; Schultz, Evans, & Serpell, 2009) and lessened academic impairment (Evans et al., 2011). Although many CHP techniques were designed for implementation in schools, some (such as those incorporated into CASH-AA) can be modified for use in a clinic setting.
CASH-AA Protocol: Treatment Modules and Interventions
CASH-AA (Hogue, Bobek, Evans, & Dendy, 2014) is a family-based clinical protocol intended for use with adolescents diagnosed with ADHD as either a primary or secondary disorder. It can be delivered in conjunction with family-based treatment or with individual-based treatment that can include caregivers in multiple sessions. It consists of four treatment modules, described briefly below, that can be initiated and completed at any point based on individualized treatment planning and case progress (Chorpita, Daleiden, & Weisz, 2005). Each CASH-AA module contains specific treatment aims and behavioral interventions that might be implemented in a single session or as a continuous intervention sequence across multiple sessions (typically 2-4 sessions, depending on how much time is devoted to working on the protocol in each session). It follows that the length of time needed to complete each module will vary greatly depending on the profile of the given family, practice habits of the provider team, and progress of the case. Figure 2 depicts the CASH-AA fidelity monitoring checklist, which lists the four treatment modules and their respective interventions components.
Figure 2.
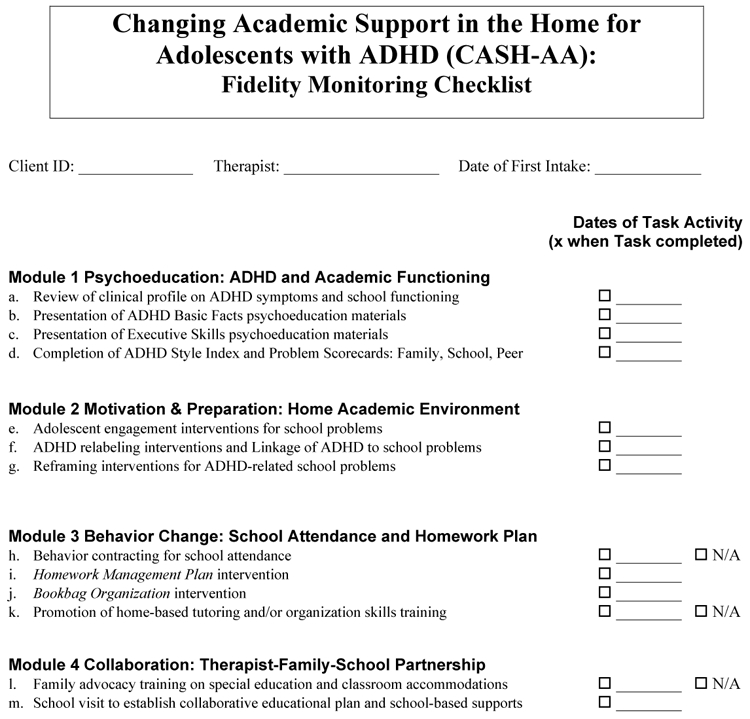
CASH-AA Fidelity Monitoring Checklist.
Module 1 Psychoeducation: ADHD and Academic Functioning
Module 1 is intended to assess family educational background and current adolescent school functioning, educate family members about links between ADHD and academic performance, and collaboratively identify the adolescent’s unique profile of ADHD-related behavioral problems and other personality characteristics.
Review of Clinical Profile of ADHD Symptoms and School Functioning.
Standard or customized intake evaluations determine whether adolescents meet diagnostic criteria for ADHD, taking into account the assessment challenges associated with (a) divergent reporter perspectives on the presence and severity of symptoms, (b) developmental changes in symptom expression, and (c) incomplete or skewed knowledge about symptom expression in school and other settings. The protocol also requires clinicians to gather assessment data directly from school personnel in order to make a confident and specific diagnosis, obtain reliable data on the history and current standing of school performance indicators (including enrollment in educational support services), and set the stage for assessing clinically significant improvements in school functioning and conducting Module 4 activities aimed at developing a therapist-family-school partnership. Clinicians also learn about the educational experiences of caregivers and others who live in the home in order to contextualize teens’ current school performance and illuminate the degree to which caregivers are prepared to support changes in the home that are needed to improve school functioning.
Presentation of Psychoeducation Materials: ADHD Basic Facts.
Colorful slides (contained in the CASH-AA treatment manual; Hogue et al., 2014) are used as educational materials and therapeutic prompts for interactive discussions about several issues pertaining to ADHD among adolescents. Several slides present ADHD prevalence rates, behavioral symptoms, and common impacts on developmental functioning. Others deliver a strong anti-stigma message while encouraging teens to take ownership of ADHD-related characteristics. Slides also educate families about the neurobiology of ADHD (using accessible metaphors) in order to promote family acceptance, defuse moral attributions, and establish practical expectations for change. Potential benefits of medication are also briefly described, and when possible, medication consultation is offered to interested families.
Presentation of Psychoeducation Materials: Executive Skills.
Slides are also used to define components of executive functioning (EF), including working memory, behavioral inhibition, emotional control, planning and organization, and analytic skills. Another set of slides elaborates the relations among three main influences on academic achievement for teens with ADHD: intelligence, EF skills, and ADHD behavioral symptoms (especially inattention and impulsivity). Others present prevalence rates for learning disabilities and prompt discussion of any history of learning delays, setting the stage for home-based tutoring activities in Module 3 as indicated.
Completion of ADHD Style Index and Problem Scorecards: Family, School, Peer.
Conjointly with caregivers and teens, clinicians administer and discuss a checklist of positive and negative personality and social characteristics associated with ADHD (ADHD Style Index) and three checklists of common ADHD-related impairments in the family, school, and peer domains (Problem Scorecards). These materials anchor generic psychoeducation about ADHD symptoms and EF deficits to client-specific characteristics and priorities identified by families. They also encourage further teen ownership and family acceptance of the ADHD condition, including identification of desirable social traits, while instilling a non-blaming explanatory narrative for difficulties experienced in everyday functioning. Finally, they help clinicians and families identify the most troublesome problems that then form the core of family-endorsed treatment goals.
Module 2 Motivation & Preparation: Home Academic Environment
Module 2 in intended to engage adolescents as active participants in therapeutic activities focused on improving school performance, link ADHD traits to school functioning, reframe the adolescent’s school problems as family problems with family solutions, assess characteristics of the home environment that support or impede school success, and determine caregiver and adolescent readiness to make changes in the home academic setting.
Adolescent Engagement Interventions for School Problems.
Adolescents with ADHD typically enter treatment having experienced a (long) history of school difficulties and disappointments of varying degrees. This can cause them to feel hopeless about achieving success, being recognized as talented or hard-working, or gaining personal satisfaction. For such youths a primary therapeutic task is school (re)moralization: Generate hope that school problems can and will improve. Clinicians approach this task via a two-step engagement process: (1) Use a given teen’s stated problems and complaints to craft school-related treatment goals that are personally meaningful to the teen. Clinicians help teens perceive therapy as a context in which their unique concerns can be met, in addition to caregivers’ treatment agenda. (2) Build and maintain teen commitment to working on personal goals by making those goals a collaborative venture equally shared between clinician and teen. This can be accomplished by presenting the enhanced value of a “team” effort and fostering a joint vision of problem-solving strategies. Often clinicians will first meet alone with teens to develop a “we” bond for pursuing goals, then meet conjointly with caregivers to cement teen investment and negotiate a mutually agreeable treatment agenda.
ADHD Relabeling Interventions and Linkage of ADHD to School Problems.
Family members often enter therapy with strong negative attributions about ADHD-related school deficits. Clinicians can facilitate more constructive family engagement in school problems by using the cognitive intervention relabeling: Altering negative attributions about a given behavior by emphasizing an unrecognized or mislabeled cause, thereby casting it in a more benign light. One kind of relabeling, “ADHD Acquittal”, moves families away from a negative attribution—ascribing personal/moral blame to an ADHD-related behavior presumed to be under teen control—and toward a benign attribution—accepting a common ADHD characteristic that arises from a neurobiological condition. For example, “lazy” is recast as inattentive or distractible, “irresponsible” as having a poor sense of time, “disruptive” as impulsive, and so on. A second kind of relabeling, “ADHD Rewards”, introduces rewarding or adaptive aspects of ADHD characteristics. For example, the “flip side” of distractibility is alertness, of immaturity is youthful exuberance, of impulsivity is spontaneity, and so forth. Both relabeling interventions are primed by the psychoeducation activities in Module 1. Relabeling also supports development of school-related treatment goals by linking ADHD characteristics directly to school problems. This linking process facilitates: (1) reduced negativity and blame surrounding the school issues, similar to the reattribution effect of ADHD Acquittal; and (2) increased motivation to participate in ADHD-targeted interventions to improve school performance, such as those in Module 3.
Reframing Interventions for ADHD-Related School Problems.
Reframing interventions are used to change the focus of discussion about ADHD-related school deficits from “individual” adolescent problems to “family” problems that affect, and are affected by, the larger family environment. To accomplish this, clinicians engage families in describing (1) how school problems affect the emotional valence and everyday functioning of the home and (2) how families respond to (and perhaps exacerbate) these problems on a regular basis. When successful, reframing helps relieve teens from bearing the exclusive burden of the problems, lowers defensiveness and reduces the likelihood of hostile exchanges or escalating negativity in session, and prompts renewed investment from all members in changing how families support school achievement. This can lead to adoption of family-centered solutions to enhance the home academic environment, such as those contained in Module 3.
Reframing school deficits as family-wide problems with family-centered solutions also creates the opportunity to collaboratively assess the capacity of caregivers to participate in reconfiguring the home academic environment. This includes a realistic appraisal of the routine availability and commitment of caregivers to support and monitor their adolescents’ academic activities, along with caregiver capacity to be involved in restructuring the environment as needed. Note that the two TIs contained in Module 3—Homework Management Plan, Bookbag Organization—were originally designed as individual or group interventions delivered in school settings. Thus, whereas a family-based clinical approach confers certain advantages for delivering TIs to clinical populations, extensive caregiver involvement is not required for TIs to be effective. The TIs incorporated in CASH-AA can be adjusted ad hoc for delivery to adolescents alone (or with minimal family involvement), assuming teens are sufficiently self-motivated to participate consistently. This adjustment may be needed when caregivers prove to be unhelpful monitors at home and/or unreliable participants in treatment, or when school attendance and performance are not a priority in the family.
Module 3 Behavior Change: School Attendance & Homework Plan
Module 3 in intended to implement family-centered interventions designed to boost school attendance (as needed) and homework quality. For adolescents with lateness or truancy issues, clinicians and families design a developmentally calibrated behavior contract featuring incentives for regular school attendance. For all cases, two training interventions adapted from CHP, Homework Management Plan and Bookbag Organization, are implemented to improve homework completion and organization habits over the course of several weeks.
Behavior Contracting for School Attendance.
For those adolescents with school attendance problems, behavior contracting begins with augmenting motivation to attend school via adolescent engagement interventions (see Module 2). To construct the contract itself, clinicians follow three basic principles that enhance the success of behavior contracts in adolescent populations: (1) Teens should be physically present during all phases of construction, whether as active participants or silent/contrarian witnesses (allowing for pre-contract preparation meetings with caregivers or teens alone to augment the productivity of contract negotiations); (2) Contract language and contingencies should be simple (versus legalistic or multiply conditional) and couched in purely behavioral terms (e.g., “She will leave the house by 7:40 am”) rather than terms that evoke cognitive/emotional states (e.g., “She will try harder to arrive at school on time”); (3) Contracts should contain a mix of positive incentives (rewards/privileges) and negative incentives plus punishments (current privileges revoked, new restrictions incurred) that are selected for moderate impact and retain personal value to a given teen. When teens are active participants in the contracting, they can be invited to share what changes at home could make it easier or more manageable to attend school, for example, shifting morning chores to after-school hours. For teens subject to external consequences for absenteeism imposed by the school or juvenile justice system, these consequences can be balanced with voluntary rewards/privileges that do not compromise the salience of external strictures.
Homework Management Plan Intervention.
This intervention is used to train adolescents to develop good study habits while decreasing family anxiety and conflict over homework completion. The foundation of the plan involves helping caregivers accept things they can no longer control (e.g., knowing the homework assignments each day, understanding all of the content of the academic subjects) and making a renewed effort to influence things they can (e.g., ensuring teens spend time on schoolwork each evening). Helping caregivers accept new limits on how much they can assist with schoolwork may be quite difficult for those who were able to boost their child in elementary school by being very involved in daily assignments. In contrast, for caregivers who have been minimally or uninvolved in homework routines, the initial stages of the plan focus on establishing the motivation and basic monitoring habits needed to support homework scheduling and completion. For all families, initial sessions involve meeting with caregivers to discuss this new approach, identifying the parameters of what is negotiable, and determining how homework sessions can best fit within the routine evening schedule.
The ultimate goal of the plan is to increase the amount of time teens spend on schoolwork each evening. Caregivers and teens negotiate a fixed amount of time and establish contingencies for adherence. A common framework for this plan is that teens are allowed full privileges until a certain point in the evening (e.g., dinner). After this point, they have no privileges until they spend the negotiated time on schoolwork. The privileges withheld should be as comprehensive as possible, including computer time, video games, cell phone use, leaving home, having friends at the house, and television (unless one of these is needed for completion of homework, e.g., computer). As soon as the full amount of time allotted for schoolwork is completed, all privileges are returned. If teens claim to have no schoolwork, then caregivers assign “busy work” such as writing a summary of a book chapter. Because middle and high school students always have assignments or test preparation, there is always a schoolwork related task that they could choose to complete. Although adolescents may complain about the assignment of busy work, if this procedure is made clear in the negotiated plan agreed to by parents and adolescents, the conflict at the point of assignment is usually brief and leads to adolescents finding schoolwork to complete.
Parents are encouraged to loosely monitor their teens during homework time. In other words, parents should be confident that teens are doing something related to school (e.g., reading, completing assignments), but not be involved to the degree of checking accuracy or debating which work teens should complete. The behavior being targeted is time spent on schoolwork; decisions about which schoolwork to complete are left to the students themselves. This distinction is made to support the developing autonomy of the adolescent regarding self-reliance and making one’s own decisions, while using parents to enforce the allocation of time to schoolwork. Clinicians should review the progress of the plan each week in session, with the goal of settling on a fixed routine that allows teens to complete all assigned homework on a daily basis. When useful, worksheets are available for tracking when homework should be completed, with what contingencies, and under what working arrangements. It is often useful to renegotiate the amount of time spent on schoolwork at each grading period based on the grades received. Of course a variety of problems can arise when implementing this plan; there are established procedures for responding to most of them (see Evans et al., 2011; Hogue et al., 2014) that can be referenced as helpful.
Bookbag Organization Intervention.
This intervention helps adolescents take relatively small steps to create a more efficient and reliable organization of school materials. It takes place in the clinic office, follows a series of detailed checklists, and requires a few inexpensive school supplies. It is usually preferable to conduct these activities with teens alone to avoid negative remarks or intrusions from caregivers. The four intervention steps can be initiated during 10-20 minutes at the beginning or end of several consecutive sessions: (1) Discuss the current organizational system (if any) for school materials, how it is working/failing, and how it can be enhanced or revamped; (2) Investigate bookbag contents to view current organizational system, plan to install the new system, and consult checklist to identify needed supplies; (3) Organize a new master binder according to a detailed checklist that prescribes a system of binder divisions, subject folders, and common school supplies; and (4) Organize the bookbag itself according to a detailed checklist. Once installed, the new organizational system should be regularly monitored and tweaked as needed over the course of treatment.
Promotion of Home-Based Tutoring and/or Organization Skills Training.
The TIs described above may not be sufficient to boost academic achievement for some teens, especially those with significant executive functioning deficits and/or learning problems. Educational supports can often be found in the schools (see Module 4). Additionally, families may seek home-based supports in the form of (a) tutoring services that provide didactic instruction and practice in specific areas of academic weakness or (b) additional TIs that focus more intensely on time management and other study skills and are beyond the expertise and/or availability of most behavior therapists. Clinicians can assist families in determining the potential benefits and costs of appropriate services and evaluating their ongoing effectiveness.
Module 4 Collaboration: Therapist-Family-School Partnership
Module 4 is intended to establish and maintain a partnership among clinicians, families, and school personnel to serve the educational interests of teens, in line with evidence-based principles of family-school collaboration for youth with ADHD (Mautone, Lefler, & Power, 2011; Power et al., 2012). The first aim is to provide the family with education and advocacy training on special education rights and school-based services available to adolescents with ADHD. There are three kinds of services (see Harrison, Bunford, Evans, & Owens, 2013 for a review): (1) Modifications: changes to school practices that alter, lower, or reduce expectations to compensate for a disability (e.g., fewer/shorter homework assignments); (2) Accommodations: changes to school practices that hold a student to equivalent expectations but provide a differential boost to mediate the impact of a disability (e.g., extra time to take a test); (3) Interventions: changes made through a systematic process to improve knowledge, skills, behaviors, cognitions, or emotions (e.g., remedial instruction). Several professional resources have been compiled to guide clinicians in educating families about school policies for students with behavioral challenges (e.g., Individuals with Disabilities Education Improvement Act of 2004) and helping families secure appropriate services for youths diagnosed with ADHD (e.g., Dendy, 2000, 2006). Services are often available even for students with passing grades.
It is important for clinicians to help families understand the differences between interventions versus accommodations/modifications (A/Ms). First, to date no A/Ms for children with ADHD or other emotional and behavioral disorders have achieved strong empirical support (Harrison et al., 2013). Second, the goal of interventions is to improve the competencies and skills of students so they can meet age-appropriate expectations at school and in the community. In contrast, the goal of most A/Ms is to reduce the expectations or requirements of students so that they can succeed without the full set of skills or competencies. A/Ms are not designed to improve functioning on the core academic deficits that lead to school impairment. For example, having extended time on tests, or having teachers provide notes for students, is not likely to improve student ability to take tests or take notes in class. Thus, A/Ms do not assist or prepare students to function academically in a manner consistent with peers (see Evans, Owens, Mautone, DuPaul, & Power, 2014). For this reason, many recommend that A/Ms be provided for students with ADHD only when all available interventions (including medication) have failed.
The second aim is for clinicians to complete at least one school visit (when feasible) to solidify partnerships with appropriate school advocates and, if needed, construct a mutually determined plan for tailored educational services. Clinicians then assist caregivers in developing the skills required to work in conjunction with school staff to monitor and revise the educational plan over the course of the school experience. Clinicians can also provide case information to caregivers and schools throughout treatment (as consented) and troubleshoot caregiver advocacy efforts once they are underway.
Case Example 1: Michael
Case Presentation
Michael was a 14-year-old African American male living with his mother, younger brother and older sister. The family was referred for services by Michael’s high school guidance counselor based on concerns about his school performance, both academics and behavior. Michael was completing ninth grade and had passed few of his courses due to missing work and also attendance issues caused by chronic lateness.
Assessment
At intake Michael met diagnostic criteria for ADHD Combined Type (youth and caregiver report) and Oppositional Defiance Disorder (caregiver report). During the assessment process, Michael’s mother emphasized her belief in Michael’s strong intelligence and academic abilities, and her feelings of frustration at his difficulty utilizing these strengths and the subsequent lack of success in school. She also shared deep concern and frustration over Michael’s impulsive anger at home, with small arguments frequently escalating into destructive action on Michael’s part (e.g., punching a hole in a wall, tearing a door off its hinges), in contrast to his typically affable and polite demeanor. Michael expressed concerns about his low frustration tolerance and his recent decline in school performance, given that his grades in elementary and middle school were always above average. Nevertheless Michael eschewed homework, declaring it was “not necessary and a waste of time.”
Case Conceptualization
Case planning focused on addressing complex clinical and educational needs. Although ADHD symptoms had been present throughout his life, they created significant problems at school only within the past year. This demonstrates how youth with both ADHD and high intelligence sometimes do not experience academic problems until their secondary school years, when schoolwork requires greater levels of organization and long-term planning. At intake Michael and his mother had a general sense of what ADHD is, but neither had given thought to Michael’s unique ADHD profile and how the disorder had impacted daily family and school functioning. Both were averse to medication as a treatment option but interested to hear professional recommendations. The often contentious relationship between Michael and his mother constituted a barrier to school success, as frequent conflict erupted at home over grades, behavior reports, and disinterest in schoolwork. By the same token, their strong affective bond, and the mother’s high level of investment in Michael’s school performance, presented an opportunity to formulate family-centered interventions intended to (1) enhance Michael’s motivation to improve his school performance, (2) develop new schoolwork monitoring structures at home, and (3) encourage more communication and positive interactions between his mother and the school system.
Course of Treatment
The CASH-AA interventions described below were combined with family therapy interventions to reduce oppositional behavior, increase positive family communication, and promote adolescent individuation.
Module 1.
For Michael and his mother, psychoeducation on ADHD and its impact on academic functioning was central to the treatment plan. They wanted to understand the facts and myths about ADHD and to place his current struggles at school in proper context of the disorder. Understanding his unique ADHD profile as it emerged from completion of the ADHD Style Index and Problem Scorecards was important for increasing his acceptance of ADHD as a lifelong condition that created problems at school and home (though not with peers), but also a condition that could be meaningfully addressed with the help of his mother, school, and therapy.
Module 2.
Michael and his mother found relabeling to be a useful exercise for increasing their confidence in effectively managing the “problem” of his ADHD. They were able to develop a matter-of-fact perspective about his struggles while also acknowledging his many positive attributes (e.g., creativity, charisma) commonly associated with the disorder. As a result of these conversations about ADHD and ways to address it, the family became more curious and open to trying medication. After consulting a psychiatrist about the most effective methods to reduce ADHD symptomatology, both family members agreed that he would start taking stimulant medication. The therapeutic frame for the psychopharmacology was that it was not meant to solve all problems, but instead constituted an important part of a multicomponent approach that included behavioral ADHD interventions and ongoing family therapy. Also, Michael struggled with motivation to address his school problems in an energetic manner. He “accepted” his ADHD but still had difficulty identifying himself as a key player in making things better, instead locating blame in his mother, teachers, or unfair expectations. By engaging Michael as an active participant in treatment and elevating his role as an agent of change, the therapist obtained his endorsement for developing an evening routine that would dedicate time to completing school assignments. Family-based interventions focused on encouraging his mother to provide developmentally appropriate structure for Michael’s evenings, while allowing him to be the chief architect of the schedule and judge of the family’s daily adherence to it.
Module 3.
Although attendance and homework issues were central to his struggles at school, they were also issues around which Michael was continually working to assert familial independence. Behavior contracting with Michael for school attendance, in particular being on time for the first few periods of school, effectively eliminated almost daily power struggles with his mother. Also, the therapist emphasized Michael’s autonomy as much as possible during both the Homework Management Plan and Bookbag Organization interventions. He was able to formulate goals for himself regarding school performance, including passing grades and avoiding summer school. The therapist and mother reinforced these concrete goals whenever he voiced reservations or complaints about completing homework or organizing his materials. The home academic routines developed and codified in therapy were continually discussed and reinforced in subsequent sessions and during between-session conversations.
Module 4.
As Michael was asserting his independence through managing his ADHD and school performance, with the support and guidance of his mother, it remained critical to develop a working partnership among school staff, family, and therapist. The school’s ongoing report was essential for accurately assessing Michael’s difficulties and the impacts of interventions, including medication along with homework and organization skills-building. His mother was an active participant in all aspects of Michael’s treatment, and counseling her on becoming an advocate for him at school was an important opportunity to channel her concern and energy in a useful, role-specific manner. In particular, after accepting his ADHD diagnosis in the clinical setting and learning about the range of special education services for which he might be eligible, Michael’s mother asked the school convene an educational planning meeting for her son. She attended this and subsequent meetings on site and was instrumental in acquiring school-located tutoring services for him.
Michael’s treatment was successful insofar as it led to a meaningful understanding of the origin of his challenges in the home and school settings. With the help of his mother, the therapy, and his school, Michael was able to make important progress in several areas of school and family functioning, with periodic lapses and moments of difficulty.
Case Example 2: Jenny
Case Presentation
Jenny was a 17-year-old Hispanic female of Puerto Rican descent living with her grandmother. She was referred by a school guidance counselor based on reports of inability to focus in class and difficulties in emotional regulation that compromised her capacity for schoolwork. Jenny was starting her senior year of high school and maintained a part-time job as well as extensive involvement in extracurricular activities, particularly music and theater.
Assessment
Jenny and her grandmother completed an intake assessment, though her grandmother’s report was compromised by her limited understanding of Jenny’s history, as she was not always the custodial caregiver and had little previous involvement in Jenny’s day-to-day life. Jenny met diagnostic criteria for ADHD Inattentive Type (youth and caregiver report) and Generalized Anxiety Disorder (youth report). Her grandmother stated concerns over Jenny’s anxiety symptoms and the disruptions in family life caused by her emotional outbursts. She conceptualized this behavior as Jenny seeking attention and provided little insight into Jenny’s schoolwork problems. Jenny felt confused about the cause of her emotional difficulties and her inability to complete schoolwork despite her general motivation to perform well. The grandmother did not wish to participate regularly in treatment sessions.
Case Conceptualization
For Jenny, the combination of ADHD and an anxiety disorder was greater than the sum of their parts. Symptoms from the two disorders interacted to make small tasks seem insurmountable and small changes overwhelming. Also, although Jenny already demonstrated a good deal of independence and responsibility, she was frustrated over her constant failures to reach her own schoolwork goals. During childhood her ADHD symptoms were often overlooked or misunderstood; as a result, a primary treatment goal was helping Jenny understand and accept her unique ADHD profile as a first step toward greater confidence in the school context. Similarly, given the lifelong absence of a consistent caregiver presence, treatment goals included acquisition of emotional coping skills as well as organization skills. Jenny was open to complying with treatment recommendations and utilizing therapy as an opportunity to make changes.
Course of Treatment
The CASH-AA interventions described below were combined with individual cognitive-behavioral interventions to reduce symptoms of anxiety and depression and enhance emotional regulation and coping skills.
Module 1.
ADHD psychoeducation was important for supporting Jenny’s motivation to reach educational and vocational goals. She could be easily overwhelmed by diagnostic labels and discussion of multiple symptoms, so that anchoring her ADHD treatment in science-based facts about the disorder was a significant palliative measure. In the same vein, helping her differentiate difficulties related to ADHD versus those related to her anxieties, temperament characteristics, and external life stressors was an important intervention. She generated many questions about ADHD and her own symptoms, and reviewing psychoeducation materials provided an anchor for this phase of treatment. The therapist identified several cognitive distortions Jenny was experiencing regarding her ADHD (“Having ADHD means I’m defective and crazy”) and addressed them via cognitive restructuring techniques. Jenny and her grandmother were opposed to medication interventions and declined psychiatric consultation.
Module 2.
Jenny entered treatment feeling ineffective and somewhat hopeless about positive change in the school domain after years of marginal performance. Thus Module 2 work began with remoralization: generating hope that she could be a success in school on her own merits, and that hard work could produce concrete payoffs. Jenny had specific interests in school extracurriculars for which a baseline level of academic performance was required. By reframing school success as an opportunity to pursue activities she enjoyed, Jenny was able to articulate for herself the merits of completing homework and ultimately improving her grades. Jenny kept a busy schedule filled with activities and employment, which she managed independently and for the most part effectively. Although she often complained of having “no time” for schoolwork, she agreed to reserve time segments to complete homework each school night.
Module 3.
After committing to a homework routine in Module 2, Jenny was more prepared to engage in formulating a homework management plan during the next phase of therapy; this plan became increasingly differentiated as treatment progressed. Because of her independence, Jenny and her therapist created “self-delivered incentives” that allowed Jenny to reward herself for adhering to the homework plan. She also adopted the bookbag organization system to upgrade her existing organization habits.
Module 4.
During the last phase of the protocol, Jenny was encouraged to become her own advocate at school. The therapist coached Jenny on communicating her learning needs to individual teachers and helped her craft requests for specific support, for example, emailing a teacher to obtain clarification on an assignment. The therapist also remained in frequent communication with Jenny’s guidance counselor and spent time helping Jenny learn to interpret and utilize school performance feedback, including grades, to assess and update personal goals.
While Jenny continued to have some struggles with emotional regulation and distractibility, treatment produced a prominent advance in Jenny’s coping and self-management skills along with objective improvements in school performance. Jenny remains somewhat isolated in motivating herself for academic and vocational success, but she is able to identify for herself realistic and meaningful goals for her future.
Implications for Practicing Behavioral Therapists
The CASH-AA protocol is designed to fill a troublesome gap in clinic-based psychosocial interventions for adolescents with ADHD. ADHD and its related school functioning deficits are highly prevalent in teens referred for outpatient behavioral services, yet few effective treatment options are available. Pharmacological interventions have demonstrated modest impact on school outcomes, and behavior management models are developmentally ill-suited for this age group. Whereas school-located training interventions focused on organization skills have shown promise, they have limited reach as a stand-alone approach for adolescents enrolled in specialty care (e.g., mental health centers, substance abuse clinics) and nonspecialty care (e.g., juvenile justice, child welfare) outside the school setting. CASH-AA is designed to be a new behavioral resource for this difficult-to-treat population that packages research-proven clinical family interventions, ADHD psychoeducation, and training interventions that can be readily implemented in a variety of care settings. Moreover, as with any behavioral intervention for ADHD, it can be combined with medication to maximize effects (see Hogue, Bobek, Tau, & Levin [in press] for a behavioral model that integrates medication decision-making interventions into outpatient behavioral treatment for adolescents with ADHD). Therapists are encouraged to consult emerging evidence-informed guidelines for selecting among behavioral, medication, and combined approaches for treating ADHD in adolescents (e.g., Sibley, Kuriyan, et al., 2014).
Promptly and systematically addressing ADHD concerns can provide compelling motivation for troubled and/or discouraged families to engage and remain in outpatient treatment. CASH-AA contains several features intended to heighten its compatibility and sustainability within the everyday working conditions of behavioral care. It can be utilized as a stand-alone intervention for ADHD or as an adjunct to other behavioral interventions for co-occurring disorders. It can be delivered in conjunction with family-based treatments (see Case Example 1) or with individual-based treatments that allow inclusion of caregivers in multiple sessions (Case Example 2). It contains four treatment modules that can be initiated and completed at any point based on individualized treatment planning. The protocol does not require clinical resources or training beyond what is contained in the treatment manual (Hogue et al., 2014) or otherwise widely available to line clinicians. And because CASH-AA interventions are fundamentally behavioral in nature (e.g., they do not target academic content or learning skills), they are easy to adopt and implement by most behavior therapists who are experienced with adolescent clients.
The basic principles of CASH-AA are also applicable for supporting non-traditional educational pursuits such as equivalency diplomas or vocational training among older adolescents. However, the protocol is not suitable for all adolescent clients with ADHD. Some may already be attending structured after-school programs that provide homework assistance and tutoring services; CASH-AA may be redundant for them. At the opposite end of the spectrum, teens who have dropped out of school altogether will have little incentive to participate. More broadly, adolescent motivation is the cornerstone for protocol success. Just as parents cannot “force a pill down the throat” of teens who refuse to take medication, therapists and families cannot effectively support academic functioning in teens who have no investment in school. For this reason the protocol asks therapists to assess, cultivate, and reinforce academic motivation throughout treatment. Finally, although CASH-AA is grounded in research-proven interventions for this clinical group, the full protocol has been implemented with only a handful of families and awaits formal piloting in a controlled research study to reliably ascertain its effectiveness, strengths, and limitations.
Acknowledgments
Preparation of this article was supported by the National Institute on Drug Abuse (K02 DA026538). The authors would like to thank Chris A. Ziegler Dendy for her invaluable contributions to CASH-AA model development.
Footnotes
This article uses the terms “behavioral intervention” and “behavior therapist” generically to reference psychosocial treatments of all kinds (behavioral, cognitive-behavioral, relational, etc.) and to contrast with pharmacological interventions.
A comprehensive review of national trends in ADHD diagnosis concluded that recent spikes in ADHD prevalence rates among youth are correlated with states’ passage of educational accountability laws that incentivize performance on standardized testing (Hinshaw & Scheffler, 2014)”.
Contributor Information
Aaron Hogue, The National Center on Addiction and Substance Abuse at Columbia University.
Molly Bobek, The National Center on Addiction and Substance Abuse at Columbia University.
Steven W. Evans, Ohio University
References
- Abikoff HB, Gallagher R, Wells K, Murray DW, Huang L, Lu F, & Petkova E (2013). Remediating organizational functioning in children with ADHD: Immediate and long-term effects from a randomized controlled trial. Journal of Consulting and Clinical Psychology, 81, 113–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander JF, Robbins MS, & Sexton TL (2000). Family-based interventions with older, at-risk youth: From promise to proof to practice. Journal of Primary Prevention, 21, 185–205 [Google Scholar]
- Alexander JF, Waldron HB, Barton C, & Mas CH (1989). The minimizing of blaming attributions and behaviors in delinquent families. Journal of Consulting and Clinical Psychology, 57, 19–24. [DOI] [PubMed] [Google Scholar]
- Antshel KM, Faraone SV, & Gordon M (2012). Cognitive behavioral treatment outcomes in adolescent ADHD. FOCUS: The Journal of Lifelong Learning in Psychiatry, 10(3), 334–345. [Google Scholar]
- Armstrong TD, & Costello EJ (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology, 70, 1224–1239 [DOI] [PubMed] [Google Scholar]
- Barkley R (2006). Associated cognitive, developmental, and health problems. In Barkley R (Ed.), Attention Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment (3rd ed., pp. 122–183). New York: Guilford. [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, & Metevia L (2001). The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology, 69, 926–941. [PubMed] [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, & Fletcher KE (1992). A comparison of three family therapy programs for treating family conflicts in adolescents with Attention-Deficit Hyperactivity Disorder. Journal of Consulting and Clinical Psychology, 60, 450–462. [DOI] [PubMed] [Google Scholar]
- Beck SJ, Hanson CA, Puffenberger SS, Benninger KL, & Benninger WB (2010). A controlled trial of working memory training for children and adolescents with ADHD. Journal of Clinical Child and Adolescent Psychology, 39, 825–836. [DOI] [PubMed] [Google Scholar]
- Bussing R, Porter P, Zima BT, Mason D, Garvan C, & Reid R (2012). Academic outcome trajectories of students with ADHD: Does exceptional education status matter? Journal of Emotional and Behavioral Disorders, 20, 131–143. [Google Scholar]
- Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, … & Ramon M (in press). A randomized clinical trial of Cogmed Working Memory Training in school-age children with ADHD: A replication in a diverse sample using a control condition. Journal of Child Psychology and Psychiatry. DOI: 10.1111/jccp.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Y, Dennis ML, & Funk RR (2008). Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment, 34, 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Weisz JR (2005). Modularity in the design and application of therapeutic interventions. Applied & Preventive Psychology, 11, 141–56. [Google Scholar]
- Coolidge FL, Thede LL, & Young SE (2000). Heritability and the comorbidity of attention deficit hyperactivity disorder with behavioral disorders and executive function deficits: A preliminary investigation. Developmental Neuropsychology, 17, 273–287. [DOI] [PubMed] [Google Scholar]
- Cummings CM, & Fristad MA (2007). Medications prescribed for children with mood disorders: Effects of a family-based psychoeducation program. Experimental and Clinical Psychopharmacology, 15, 555–562. [DOI] [PubMed] [Google Scholar]
- Cutting L, & Denckla M (2003). Attention: Relationships between attention deficit hyperactivity disorder and learning disabilities. In Swanson H, Harris K, & Graham S (eds.), Handbook of Learning Disabilities (pp. 125–139). New York: Guilford. [Google Scholar]
- Dendy CAZ (2000). Teaching Teens with ADD and ADHD: A Quick Reference Guide for Teachers and Parents. Bethesda, MD: Woodbine House. [Google Scholar]
- Dendy CAZ (2006). Teenagers with ADD and ADHD: A Guide for Parents and Professionals (2ndEdition). Bethesda, MD: Woodbine House. [Google Scholar]
- Diamond GM, Liddle HA, Hogue A, & Dakof GA (1999). Alliance-building interventions with adolescents in family therapy: A process study. Psychotherapy: Theory, Research, Practice, & Training, 36, 355–368. [Google Scholar]
- Evans SW, Axelrod J, & Langberg JM (2004). Efficacy of a school-based treatment program for middle school youth with ADHD. Behavior Modification, 28, 528–547. [DOI] [PubMed] [Google Scholar]
- Evans SW, Owens JS, & Bunford N (in press). Evidence-based psychosocial treatments for children and adolescents with Attention-Deficit/Hyperactivity Disorder. Journal of Clinical Child and Adolescent Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Owens JS, Mautone JA, DuPaul GJ, & Power TJ (2014). Toward a comprehensive life-course model of care for youth with Attention-Deficit/Hyperactivity Disorder. In Handbook of School Mental Health (pp. 413–426). United States: Springer. [Google Scholar]
- Evans SW, Pelham W, & Grudberg MV (1994). The efficacy of note-taking to improve behavior and comprehension of adolescents with Attention-Deficit/Hyperactivity Disorder. Exceptionality, 5, 1–17. [Google Scholar]
- Evans SW, Pelham WE, Smith BH, Bukstein O, Gnagy EM, Greiner AR, … & Baron-Myak C (2001). Dose–response effects of methylphenidate on ecologically valid measures of academic performance and classroom behavior in adolescents with ADHD. Experimental and Clinical Psychopharmacology, 9, 163–175. [DOI] [PubMed] [Google Scholar]
- Evans SW, Schultz BK, DeMars CE & Davis H (2011). Effectiveness of the Challenging Horizons after-school program for young adolescents with ADHD. Behavior Therapy, 42, 462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Schultz BK, White LC, Brady C, Sibley MH, & Van Eck K (2009). A school-based organization intervention for young adolescents with Attention-Deficit/Hyperactivity Disorder. School Mental Health, 1, 78–88. [Google Scholar]
- Evans SW, Serpell ZN, Schultz BK, & Pastor DA (2007). Cumulative benefits of secondary school-based treatment of students with Attention-Deficit/Hyperactivity Disorder. School Psychology Review, 36, 256–273. [Google Scholar]
- Evans SW, Timmins B, Sibley M, White LC, Serpell ZN, & Schultz B (2006). Developing coordinated, multimodal, school-based treatment for young adolescents with ADHD. Education and Treatment of Children, 29, 359–378. [Google Scholar]
- Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, & O'Connor BC (2009). A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review, 29, 129–140. [DOI] [PubMed] [Google Scholar]
- Faraone SV, & Buitelaar J (2010). Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. European Child & Adolescent Psychiatry, 19, 353–364. [DOI] [PubMed] [Google Scholar]
- Fletcher JM, Lyon G, Fuchs L, & Barnes M (2007). Learning disabilities: From identification to intervention. New York: Guilford. [Google Scholar]
- Fristad MA (2006). Psychoeducational treatment for school-aged children with bipolar disorder. Development and Psychopathology, 18, 1289–1306. [DOI] [PubMed] [Google Scholar]
- Geist R, Heinmaa M, Stephens D, Davis R, & Katzman DK (2000). Comparison of family therapy and family group psychoeducation in adolescents with anorexia nervosa. Canadian Journal of Psychiatry, 45, 173–178. [DOI] [PubMed] [Google Scholar]
- Gevensleben H, Holl B, Albrecht B, Schlamp D, Kratz O, Studer P, … & Heinrich H (2009). Distinct EEG effects related to neurofeedback training in children with ADHD: A randomized controlled trial. International Journal of Psychophysiology, 74, 149–157. [DOI] [PubMed] [Google Scholar]
- Gureasko-Moore S, DuPaul GJ, & White GP (2006). The effects of self-management in general education classrooms on the organizational skills of adolescents with ADHD. Behavior Modification, 30, 159–183. [DOI] [PubMed] [Google Scholar]
- Habboushe DF, Daniel-Crotty S, Karustis JL, Leff SS, …& Power TJ (2001). A family-school homework intervention program for children with Attention-Deficit/Hyperactivity Disorder. Cognitive and Behavioral Practice, 8, 123–136. [Google Scholar]
- Harrison JR, Bunford N, Evans SW, & Owens JS (2013). Educational accommodations for students with behavioral challenges: A systematic review of the literature. Review of Educational Research, 83, 551–597. [Google Scholar]
- Hinshaw SP, & Scheffler RM (2014). The ADHD Explosion: Myths, Medication, Money, and Today's Push for Performance. New York: Oxford University Press. [Google Scholar]
- Hogue A, Bobek M, Evans SW, & Dendy CAZ (2014). Changing Academic Support in the Home for Adolescents with ADHD (CASH-AA): Provider Manual. The National Center on Addiction and Substance Abuse at Columbia University, New York, NY. Available from the first author upon request: ahogue@casacolumbia.org. [Google Scholar]
- Hogue A, Bobek M, Tau GZ, & Levin FR (in press). Clinical strategies for integrating medication interventions into behavioral treatment for adolescent ADHD: The Medication Integration Protocol. Child & Family Behavior Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, & Liddle HA (2009). Family-based treatment for adolescent substance abuse: Controlled trials and new horizons in services research. Journal of Family Therapy, 31, 126–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2006). Improving the quality of healthcare for mental and substance use conditions. Washington, DC: National Academies Press. [Google Scholar]
- Johnston C, Hommersen P, & Seipp C (2008). Acceptability of behavioral and pharmacological treatments for Attention-Deficit/Hyperactivity Disorder: Relations to child and parent characteristics. Behavior Therapy, 39, 22–32. [DOI] [PubMed] [Google Scholar]
- Jones DE, Foster EM, & Conduct Problems Prevention Research Group (2009). Service use patterns for adolescents with ADHD and comorbid conduct disorder. The Journal of Behavioral Health Services & Research, 36, 436–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent KM, Pelham WE, Molina BSG, Sibley MH, Waschbusch DA, Yu J, … & Karch KM (2011). The academic experience of male high school students with ADHD. Journal of Abnormal Child Psychology, 39, 451–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyan AB, Pelham WE, Molina BSG, Waschbusch DA, Gnagy EM, Sibley MH, … & Kent KM (2013). Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology, 41, 27–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, & Becker SP (2012). Does long-term medication use improve the academic outcomes of youth with Attention-Deficit/Hyperactivity Disorder? Clinical Child and Family Psychology Review, 1–19. [DOI] [PubMed] [Google Scholar]
- Langberg JM, Dvorsky MR, & Evans SW (2013). What specific facets of executive function are associated with academic functioning in youth with attention-deficit/hyperactivity disorder? Journal of Abnormal Child Psychology, 41, 1145–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, Epstein JN, Becker SP, Girio-Herrera E, & Vaughn AJ (2012). Evaluation of the homework, organization, and planning skills (HOPS) intervention for middle school students with attention deficits hyperactivity disorder as implemented by school mental health providers. School Psychology Review, 41, 342–364. [PMC free article] [PubMed] [Google Scholar]
- Liddle HA (1995). Conceptual and clinical dimensions of a multidimensional, multisystems engagement strategy in family-based adolescent treatment. Psychotherapy: Theory, Research, Practice, & Training, 32, 39–58. [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, & Tejeda M (2001). Multidimensional Family Therapy for adolescent substance abuse: Results of a randomized clinical trial. American Journal of Drug and Alcohol Abuse, 27, 651–687. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Rowe CR, Henderson C, & Greenbaum P (2009). Multidimensional family therapy for early adolescent substance abusers: Twelve month outcomes of a randomized controlled trial. Journal of Consulting and Clinical Psychology, 77, 12–25. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Turner RM, Henderson CE, & Greenbaum PE (2008). Treating adolescent drug abuse: A randomized trial comparing multidimensional family gtherapy and cognitive behavior therapy. Addiction, 103, 1660–1670. [DOI] [PubMed] [Google Scholar]
- Lopez M, Toprac M, Crimson M, Boemer B, & Baumgartner J (2005). A psychoeducational program for children with ADHD or depression and their families: Results from the CMAP feasibility study. Community Mental Health Journal, 41, 51–66. [DOI] [PubMed] [Google Scholar]
- Mautone JA, Lefler EK, & Power TJ (2011). Promoting family and school success for children with ADHD: Strengthening relationships while building skills. Theory into Practice, 50, 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCleary L, & Ridley T (1999). Parenting adolescents with ADHD: Evaluation of a psychoeducation group. Patient Education and Counseling, 38, 3–10. [DOI] [PubMed] [Google Scholar]
- McGough JJ, McBurnett K, Bukstein O, Wilens TE, Greenhill L, Lerner M, & Stein M (2006). Once-daily OROS methylphenidate is safe and well tolerated in adolescents with Attention-Deficit/Hyperactivity Disorder. Journal of Child and Adolescent Psychopharmacology, 16, 351–356. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swendsen J, Avenevoli S, Case B, … & Olfson M (2011). Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Flory K, Bukstein OG, Greiner AR, Baker JL, Krug V, & Evans SW (2008). Feasibility and preliminary efficacy of an after-school program for middle schoolers with ADHD: A randomized trial in a large public middle school. Journal of Attention Disorders, 12, 207–217. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, …& the MTA Cooperative Group. (2009). MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 484–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr JM, Miller RB, & Polson DM (2007). Toward a standard of care for child ADHD: Implications for marriage and family therapists. Journal of Marital and Family Therapy, 31, 191–205 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EN, Sibley MH, Kipp HL, Smith BH, Evans SE, & Bukstein O (2013). Attributions and perception of methylphenidate effects in adolescents with ADHD. Journal of Attention Disorders. DOI: 10.1177/1087054713493320. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, Yee MA, Huang-Pollock C, Easterlin B, Zalecki C, & McBurnett K (2007). A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly Inattentive type. Journal of the American Academy of Child & Adolescent Psychiatry, 46, 1041–1050. [DOI] [PubMed] [Google Scholar]
- Power TJ, Mautone JA, Soffer SL, Clarke AT, Marshall SA, …& Jawad AF (2012). A family-school intervention for children with ADHD: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 80, 611–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raggi VL, Chronis-Tuscano A, Fishbein H, & Groomes A (2009). Development of a brief, behavioral homework intervention for middle school students with Attention-Deficit/Hyperactivity Disorder. School Mental Health, 1, 61–77. [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330–366. [PubMed] [Google Scholar]
- Rigter H, Henderson CE, Pelc I, Tossmann P, Phan O, Hendriks V, Schaub M, & Rowe CL (2013). Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: A randomised controlled trial in Western European outpatient settings. Drug and Alcohol Dependence, 130, 85–93. [DOI] [PubMed] [Google Scholar]
- Robb JA, Sibley MH, Pelham WE, Foster E, Molina BSG, Gnagy EM, & Kuriyan AB (2011). The estimated annual Cost of ADHD to the US education system. School Mental Health, 3, 169–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins MS, Alexander JF, Newell RM, & Turner C, W. (1996). The immediate effect of reframing on client attitude in family therapy. Journal of Family Psychology, 10, 28–34. [Google Scholar]
- Robbins MS, Alexander JF, & Turner CW (2000). Disrupting defensive family interactions in family therapy with delinquent adolescents. Journal of Family Psychology, 14, 688–701. [DOI] [PubMed] [Google Scholar]
- Robbins M, Turner CW, Alexander J, & Perez G (2003). Alliance and dropout in family therapy for adolescents with behavior problems: Individual and systemic effects. Journal of Family Psychology, 17, 534–544. [DOI] [PubMed] [Google Scholar]
- Robin A (2006). Training families with adolescents with ADHD. In Barkley R (ed.). Attention Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment (3rd ed., pp. 499–546). New York: Guilford. [Google Scholar]
- Sadler JM, Evans SW, Schultz BK, & Zoromski AK (2011). Potential mechanisms of action in the treatment of social impairment and disorganization in adolescents with ADHD. School Mental Health, 20, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2007). Substance Abuse and Mental Health Services Administration, Office of Applied Studies: The OAS Report: A day in the life of American adolescents: Substance use facts. Rockville, MD. [PubMed] [Google Scholar]
- SAMHSA. (2009). Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The NSDUH Report: Adolescent Mental Health: Service Settings and Reasons for Receiving Care. Rockville, MD. [Google Scholar]
- Sanchez R, Crismon M, Barner J, Bettinger T, & Wilson J (2005). Assessment of adherence measures with different stimulants among children and adolescents. Pharmacotherapy, 25, 909–917. [DOI] [PubMed] [Google Scholar]
- Sanford M, Boyle M, McCleary L, Miller J, Steele M, Duku E, & Offord D (2006). A pilot study of adjunctive family psychoeducation in adolescent major depression: Feasibility and treatment effect. Journal of the American Academy of Child & Adolescent Psychiatry, 45, 386–395. [DOI] [PubMed] [Google Scholar]
- Schultz BK, Evans SW, & Serpell ZN (2009). Preventing failure among middle school students with Attention-Deficit/Hyperactivity Disorder: A survival analysis. School Psychology Review, 38, 14–27. [Google Scholar]
- Schultz BK, Storer J, Watabe Y, Sadler J, & Evans SW (2011). School-based treatment of Attention-Deficit/Hyperactivity Disorder. Psychology in the Schools, 48, 254–262. [Google Scholar]
- Schwarz A, & Cohen S (2013). More diagnoses of hyperactivity in new C.D.C. data: A rapid rise in rates, The New York Times. Retrieved from http://www.nytimes.com/2013/04/01/health/more-diagnoses-of-hyperactivity-causing-concern.html?pagewanted=all&_r=0 [Google Scholar]
- Sexton TL, & Alexander JF (2003). Functional family therapy: A mature clinical model. In: Sexton T, Weeks G, & Robbins MS, (eds), Handbook of family therapy. New York: Brummer/Routledge. [Google Scholar]
- Sibley MH, Altszuler AR, Ross JM, Sanchez F, Pelham WE, & Gnagy EM (2014). A parent-teen collaborative treatment model for academically impaired high school students with ADHD. Cognitive and Behavioral Practice, 21, 32–42. [Google Scholar]
- Sibley MH, Kuriyan AB, Evans SW, Waxmonsky JG, & Smith BH (2014). Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical Psychology Review, 34, 218–232. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Derefinko KD, Kuriyan AB, Sanchez F, & Graziano PA (2013). A pilot trial of Supporting Teens’ Academic Needs Daily (STAND): A parent-adolescent collaborative intervention for ADHD. Journal of Psychopathology and Behavioral Assessment, 35, 436–449. [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Garefino AC, … & Karch KM (2012). Diagnosing ADHD in adolescence. Journal of Consulting and Clinical Psychology, 80, 139–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes TF, & Baer DM (1977). An implicit technology of generalization. Journal of Applied Behavior Analysis, 10, 349–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor E (2009). Developing ADHD. Journal of Child Psychology & Psychiatry, 50, 126–132. [DOI] [PubMed] [Google Scholar]
- Thompson LL, Whitmore EA, Raymond K, & Crowley TJ (2006). Measuring impulsivity in adolescents with serious substance and conduct problems. Assessment, 13, 3–15. [DOI] [PubMed] [Google Scholar]
- Tims FM, Dennis ML, Hamilton N, J Buchan B, Diamond G, Funk R, & Brantley LB (2002). Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction, P7(s1), 46–57. [DOI] [PubMed] [Google Scholar]
- Todd RD, Huang H, & Henderson CA (2008). Poor utility of the age of onset criterion for DSM-IV attention deficit/hyperactivity disorder: Recommendations for DSM-V and ICD-11. Journal of Child Psychology and Psychiatry, 49, 942–949. [DOI] [PubMed] [Google Scholar]
- Turner WC, Muck RD, Muck RJ, Stephens RL, & Sukumar B (2004). Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs, 36, 455–462. [DOI] [PubMed] [Google Scholar]
- Vieta E (2005). Improving treatment adherence in bipolar disorder through psychoeducation. Journal of Clinical Psychiatry, 66(Suppl 1), 24–29. [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, … & Blumberg SJ (2014). Trends in the Parent-Report of Health Care Provider-Diagnosed and Medicated Attention-Deficit/Hyperactivity Disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry, 53, 34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Cunningham CE, Pelham WE Jr., Rimas HL, Greiner AR, Gnagy EM, …& Hoffman MT (2011). A discrete choice conjoint experiment to evaluate parent preferences for treatment of young, medication naive children with ADHD. Journal of Clinical Child and Adolescent Psychology, 40, 546–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE, McBurnett K, Bukstein O, McGough J, Greenhill L, Lerner M … & Lynch JM (2006). Multisite controlled study of OROS methylphenidate in the treatment of adolescents with attention-deficit/hyperactivity disorder. Archives of Pediatrics & Adolescent Medicine, 160, 82–90. [DOI] [PubMed] [Google Scholar]
- Wu LT, Gersing K, Burchett B, Woody GE, & Blazer DG (2011). Substance use disorders and comorbid Axis I and II psychiatric disorders among young psychiatric patients: Findings from a large electronic health records database. Journal of Psychiatric Research, 45, 1453–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hurlburt MS, Hough RL, Hazen A, Culver S, … & Landsverk JA (2002). Referral sources, diagnoses, and service types of youth in public outpatient mental health care: A focus on ethnic minorities. Journal of Behavioral Health Services & Research, 29, 45–60. [DOI] [PubMed] [Google Scholar]


