INTRODUCTION
Irritability and temper outbursts lead to significant impairment in family and peer relationships as well as academic performance.1,2 Irritability, which is commonly defined as a tendency to react to stimuli with the experience of negative affective states (eg, an increased proneness to anger) compared with peers at the same developmental level,3 is observed across multiple psychiatric disorders, and puts youth with one disorder (eg, attention deficit with hyperactivity [ADHD]) at risk for other disorders (eg, depression)4 and high-risk behaviors like suicidal ideation and self-harming behaviors.5 Like irritability, temper outbursts are defined as aggressive or nonaggressive behaviors that occur in response to frustration,6 occur transdiagnostically, and have associated interpersonal and academic impairment. Irritability and temper outbursts are widely accepted examples of dysregulated emotion, although their representation within and beyond mood disorders signal the need for broad-based preventive interventions that should be applicable to a diverse group of youth and across many settings.
The frequency, severity, and intensity of irritability and temper outbursts along with age of onset, persistence and episodicity are key parameters for treatment planning. For example, early onset, persistent, and chronic irritability may suggest a neurodevelopmental or ADHD-like phenotype, whereas a later-onset irritability may be indicative of a mood disorder phenotype.7 Further, episodic versus chronic and persistent irritability may distinguish adolescents who are at risk for mania versus those who are at risk for depression.8 With different presentations that portend multifinal outcomes, the developmental context of irritability and temper outbursts have implications for how they are conceptualized, and how and when we treat them.9
Irritability and temper outbursts are not only features of multiple disorders and symptom constellations, but they may also be unstable over the course of development, calling into question the usefulness of singular or unifying diagnoses such as the new diagnosis added to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, disruptive mood dysregulation disorder (DMDD), that aimed to distinguish nonepisodic from episodic emotion dysregulation.10 Despite controversy surrounding the validity of DMDD, evidence points to a clinically significant number of children who are characterized by nonepisodic, chronic, and severe irritability and temper outbursts.11
After an initial evaluation of safety considerations and acute stabilization, existing interventions for irritability and temper outbursts are broadly framed around symptom reduction (ie, in frequency and in intensity) and relapse prevention (preventing the undesired behavior from recurring). Importantly, if a behavior can be predicted through early identification and tracking of precursor emotions, behaviors, or triggers, perhaps it can also be prevented. This review summarizes the literature on primary, secondary, and tertiary relapse prevention strategies, with a focus on strategies that promote resilience in youth to prevent the onset and recurrence of irritability and temper outbursts (Fig. 1). Although the urgency to treat the frequency and severity of outbursts is self-evident, highlighting interventions in the context of prevention and a resilience framework can enhance our understanding of treatments in terms of causal mechanisms, and illuminate interventions that could be adapted early and transdiagnostically rather than focusing on treating a single disorder. This is principally why more research is needed to guide clinicians on effective treatments to decrease the impact of stress, adversity,12 and other risk factors, as well as the consequences of common manifestations of emotion dysregulation.
Fig 1.
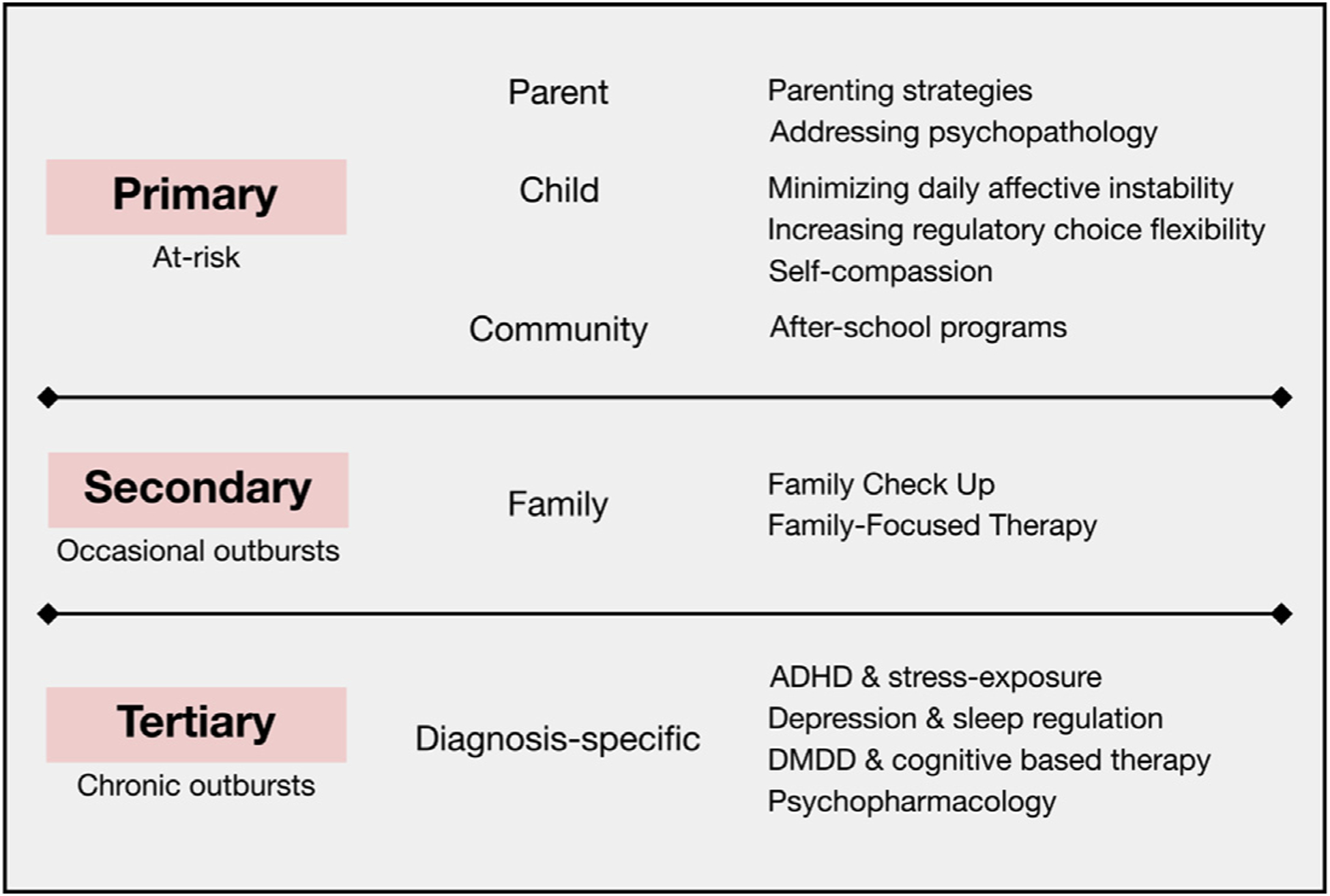
Summary of the available evidence for primary, secondary, and tertiary prevention strategies for irritability and temper outbursts. Primary prevention aims to decrease the risk for disorder onset in susceptible populations through parent, child, or community interventions. Secondary prevention strategies, targeting children with occasional outbursts, are currently predominantly family oriented. Tertiary prevention is diagnosis specific because children with chronic outbursts often are already diagnosed with mental illness. ADHD, attention deficit hyperactivity disorder; DMDD, disruptive mood dysregulation disorder.
WHY IS PROACTIVELY PROMOTING RESILIENCE AN INTRIGUING SOLUTION TO PREVENTING REACTIVE EMOTION DYSREGULATION?
Resilience is a complex process that is defined as the ability of a system to adapt successfully to challenges that threaten the function, viability, or future development of the system.13 Resilience is dynamic, falls along its own continuum, and can be cultivated with the potential for change across the lifespan to proactively bring about positive outcomes or help avoid or reduce the impact of the negative outcomes of adversity.14 Resilience has been measured using a variety of scales. The Strength and Difficulties Questonnaire15 is among the most common metric and evaluates psychopathology risk and resilient factors among youth using emotional, conduct, hyperactive–inattentive, peer, and prosocial factors. The prosocial factor (eg, voluntary actions intended to benefit others) is the single construct of resilience in the Strength and Difficulties Questionnaire, reflecting a key cross-species characteristic that centers on the evolutionarily adaptive drive to be social to promote survival.16 Several studies have demonstrated a bidirectional inverse relation between prosocial behavior and aggression or delinquency over the course of childhood and adolescence,17 suggesting the potential for prosociality to be an antidote to various forms of aggression.18 Thus, resilience, conceptualized in terms of prosociality, could be framed as a preventive intervention, such that skills that encourage prosocial behaviors have the effect of intervening to decrease aggression.
Other studies consistently find that promoting resilience encourages other positive outcomes in the face of adversity by increasing emotion regulation (ability to respond appropriately to situational demands), encouraging life satisfaction, or decreasing depressive symptoms.19,20 Thus, key factors associated with resilience include prosociality with peers and caregivers, enhancing skills in emotion regulation, and academic engagement.21
Novel interventions that enhance resilience for emotionally dysregulated youth could be implemented as primary or adjunctive strategies along the entire continuum of prevention. However, primary and secondary prevention approaches that enhance resilience may yield more enduring effects than tertiary relapse prevention strategies, such as complex psychotherapeutic interventions or poly-psychopharmacology.22,23 Resilience-based interventions also have the potential to be implemented early in life to prevent the onset and development of myriad future problem behaviors.24,25 Further, research on the neurobiological mechanisms underlying resilience may open doors to novel understanding of treatment effects for interventions for irritability and temper outbursts. Reliable biomarkers may also increase our ability to identify the most vulnerable, treatment refractory, or treatment responsive youth before symptom onset. Accelerating discovery toward personalized treatments for subtypes of emotion dysregulation that are particularly difficult to treat are critical because the currently available treatments have modest effect sizes and offer nonspecific benefits.26
WHAT ARE THE RISK FACTORS FOR IRRITABILITY AND TEMPER OUTBURSTS?
Studies have shown that the risks for irritability and temper outbursts include both environmental and genetic factors. Some known risk factors for irritability include growing up in poverty, homelessness, exposure to violence or abuse, and being the offspring of parents with psychopathology.19,27–29 When using child self-report measures, twin studies report the heritability of irritability to be around 0.30.30 Based on parent reports, heritability seems to be higher.31 Irritability may also be linked to perturbations of the prefrontal cortex that impair emotion regulation.32 Irritable youth also show abnormalities in neural circuits related to threat and reward processing.33 Further understanding the neurodevelopmental features of irritability may elucidate novel primary, secondary, and tertiary preventive interventions.34
PRIMARY PREVENTION
Primary prevention refers to strategies to prevent disease onset among susceptible populations.35 Here, we refer to children at risk for developing irritability or temper outbursts as our susceptible population. These sections leverage studies on this at-risk population to highlight targets for interventions that attempt to prevent the development of irritability and temper outbursts. We classify these studies as parent, child, and community focused. Fig. 2 summarizes the key findings.
Fig. 2.
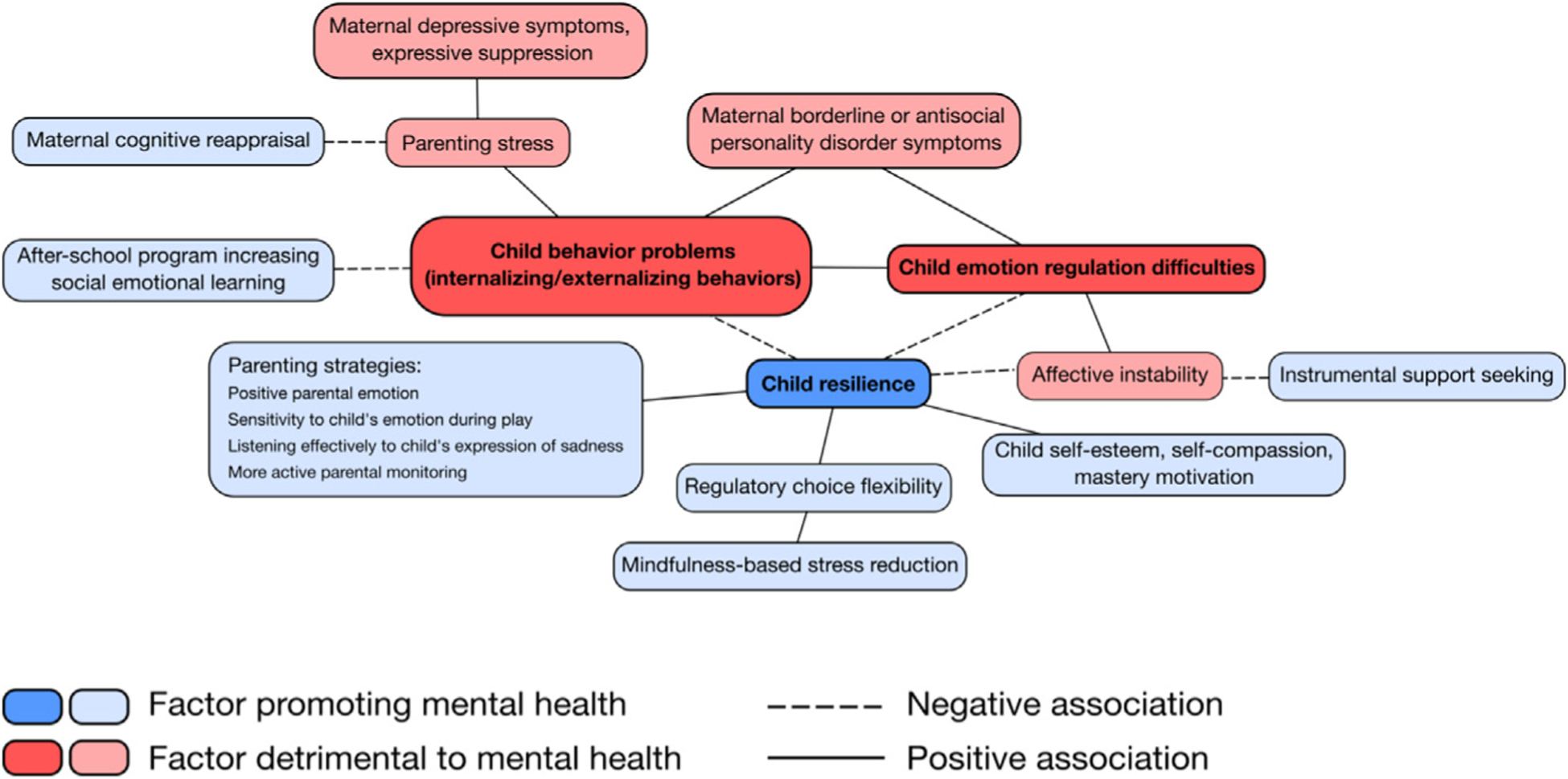
Summary of the interplay of moderators and targets of primary prevention strategies for irritability and temper outbursts. The main outcome measures are highlighted in the darker color shades (child behavior problems, resilience, emotion regulation difficulties). Key Terms: Affective instability, Shifts in emotional intensity over a relatively brief period of time within an individual; Cognitive reappraisal, Reinterpretation of an emotion-eliciting situation in a way that changes its emotional impact; Emotion regulation, Ability to respond appropriately to situational demands and manage the experience and expression of emotions; Expressive suppression, Inhibition of emotional expression; Externalizing behaviors, Actions in the external world, such as aggression, impulsivity, control problems; Instrumental support seeking, Soliciting advice and assistance with planning, decision-making and problem solving; Internalizing behaviors, Characterized by processes within the self, such as anxiety, depression, withdrawal; Mastery motivation, Drive to control and master challenges independently and persistently; Mindfulness-based stress reduction, Developed by Dr. Jon Kabat-Zinn in 1979, an 8-week program teaching mindfulness meditation exercises, initially targeting stress management; Positive parental emotion, Experience of positive emotions by parents; Regulatory choice flexibility, Ability to deploy different emotion regulation strategies based on context; Resilience, Capacity of a system to successfully adapt to threats to its function, viability, or development; Self-compassion, Ability to be kind and nonjudgmental toward the self during stress and failure; Self-esteem, Affectively laden evaluation of one’s worth.
Parent-Focused Studies
As discussed elsewhere in this article, resilience is associated with individual intrinsic (eg, problem-solving skills, self-regulation) and relational or prosocial (eg, capacity to form secure attachments) characteristics.13 The expression and regulation of emotions occur in interpersonal contexts and begin as early as in infancy.36 Thus, it is not surprising that parenting plays a central role in a child’s ability to regulate emotions.
Parental psychopathology has been identified as a risk factor for child internalizing and externalizing behaviors through multiple mechanisms, including increased parenting stress.37 In their study on mothers with homelessness and problems with substance use disorders, Wu and colleagues26 found that maternal depressive symptoms and “expressive suppression,” defined as the attempt to inhibit emotional expression, were associated with increased parenting stress regarding young children (ages 0–6). In contrast, cognitive reappraisal, or an attempt to reinterpret an emotion-eliciting situation in a way that changes its emotional impact, was associated with decreased parenting stress.37 Borderline and antisocial personality disorder symptoms in mothers have been associated with child behavior problems, a relation partially mediated by emotion dysregulation in youth.29 Maternal irritable depression has also been associated with offspring disruptive behavioral disorders, whereas the remission of maternal depression after 3 months of antidepressant treatment was associated with decreases in psychiatric diagnoses and symptoms in the offspring.38 Further, the effect of maternal remission on her children may have been mediated by an improvement in maternal symptoms of high anxious distress and irritability.39 Thus, treating psychopathology and personality pathology among parents should be considered as potential targets for the prevention of psychopathology in children. Dialectical behavior therapy, which targets emotion dysregulation, has been studied extensively as a therapeutic intervention for borderline personality disorder, but its use to improve parenting quality merits evaluation, given that a parent’s ability to regulate emotions is critical for effective parenting.40
Parental strategies like encouraging positive parental emotion (ie, parents expressing positive emotions toward a child, as measured by the Positive Affect Scale41), sensitivity to children’s emotions during play, listening effectively to children’s expression of sadness, and active monitoring of the child may be particularly helpful to families living in poverty or exposed to violence.19,28,42 Future studies should address whether such parental strategies can be harnessed to prevent the onset of irritability and temper outbursts in at-risk youth.
Child-Focused Studies
Targeting child risk factors for emotion dysregulation is also a primary prevention strategy. For example, dysregulated temperament43 may be an early risk factor for mood disorders.44 Difficult childhood temperaments, with traits like behavioral inhibition, irritability, a high activity level, and poor adaptability are associated with subsequent mood disorders, ADHD, and substance abuse.45–47 However, these associations have been cross-sectionally determined and merit longitudinal observation to evaluate the predictive validity of early temperament characteristics on developing emotion dysregulation. In 1 longitudinal study, parental temperament of fearfulness moderated the link between childhood fearfulness and their subsequent development of anxiety disorders.48 This finding may be rooted in either genetics, overprotective parenting practices, or the modeling of avoidant behavior, which could all increase susceptibility to anxiety in children.48 Thus, intervening on fear-based parenting practices may be a point of intervention in children with temperament vulnerabilities to emotion dysregulation.
Transient mood state changes have also been implicated in persistent emotion dysregulation. A longitudinal study spanning 6 years of adolescence found that day-to-day teen affective instability predicted difficulties in emotion regulation over time, suggesting a process by which mood variability becomes consolidated into enduring patterns of response.49 Targeting day-to-day affective instability through behavioral or pharmacologic interventions may interrupt the consolidation process that leads to chronic emotion dysregulation. Further, in a national sample of 100 US adolescents, greater trait resilience and support seeking by soliciting advice and assistance with planning, decision-making and problem solving have been associated with lower levels of negative affect instability.50 An insecure attachment style accounted for the unexpected relation between emotional support seeking and negative affect instability, such that adolescents, and more likely girls, with an insecure–anxious attachment style were more prone to seeking reassurance. It is worth investigating whether interventions that promote instrumental support seeking over emotional support seeking (eg, asking for solutions rather than comfort or validation) are helpful in preventing emotion dysregulation in youth. Indeed, gender differences may moderate the effects of such interventions and should be considered for personalized treatment matching.
Socioemotional functioning and emotion regulation, including self-compassion, self-esteem, and mastery motivation,25,27,42 may promote resilience against irritability and temper outbursts. In maltreated youth or youth living in poverty, self-esteem51 plays a protective role against emotional and behavioral problems52,53 and is associated with greater resilience. Here, resilience was defined as good adaptive functioning and the absence of any significant psychiatric symptomatology based on measures of global functioning (eg, Children’s Global Assessment Scale), behavioral disturbance (eg, Child Behavioral Checklist), or depression severity (eg, Childhood Depression Inventory).24,36 Similarly, in youth experiencing homelessness, higher mastery motivation (the drive to control and master challenges independently and persistently) is associated with better social and emotional functioning.27
Self-compassion is a relatively new concept in Western psychology and is the ability to be kind and nonjudgmental toward the self during stress and failure, recognizing that one’s suffering is common to the human experience.54 As such, self-compassion has been theorized to protect against the activation of psychopathological schema after negative affective experiences,25 that is, a defining feature of irritability. Consequently, interventions that attempt to enhance self-esteem, mastery motivation, and self-compassion may have preventive effects on the onset of irritability. These interventions may benefit both children and parents. For example, in elementary school children, emotion dysregulation has been associated with increased anxiety and decreased prosocial behaviors, and these associations are buffered by maternal agreeableness.55 Agreeableness is a core trait from the 5-factor model of personality that reflects the degree of expression of empathy, kindness, and consideration toward others.56 Thus, among children struggling with emotion dysregulation, an early intervention targeting maternal agreeableness or prosociality may decrease a child’s risk for irritability and temper outbursts.
Interventions to Promote Emotion Regulation
There are few interventions that encourage emotion regulation skill enhancement. Whether a specific emotion regulation strategy proves adaptive or maladaptive depends on the context in which it is applied. For example, it is adaptive to choose disengagement–distraction for high-intensity emotional stimuli versus engaging–reappraisal for low-intensity stimuli.57,58 Mindfulness-based practices may increase regulatory choice flexibility through an increased awareness of one’s thoughts, sensations, and feelings and decreasing automatic reactivity to emotional experiences. In addition, mindfulness training in the context of family therapy may enhance a family’s capacity for emotion regulation.36 Studies that promote understanding of these and other specific nuances that leverage emotion regulation skills in a family context may lead to additional points of intervention. Outside of the family context, in college students ages 21 to 40 years, Mindfulness-Based Stress Reduction was effective in cultivating “regulatory choice flexibility,” or the ability to deploy different emotion regulation strategies based on context to encourage resilience.59
Community-level interventions for children at risk for emotional dysregulation are limited.60 In 1 open trial of an after-school program for urban, middle school African American youth living in poverty, Frazier and colleagues22 found that encouraging recreational activities that enhance social–emotional learning (ie, problem solving, emotion regulation, effective communication) led to improvements in social skills and decreases in problem behaviors. The specificity of and degree to which such programs lead to long-term changes in problem behaviors in high-risk populations deserves exploration.
SECONDARY PREVENTION
Secondary prevention focuses on addressing subclinical forms of disease as early as possible to prevent progression to full-blown disease states. How can we help youth who have occasional outbursts from developing chronic patterns of emotion dysregulation that will impact their psychosocial functioning or develop into full-blown psychopathology? Lessons can be learned from findings across a number of psychiatric disorders, as well as from interventions developed for specific diagnoses. Indeed, understanding that early alliance in treatment can promote engagement and favorable outcomes underscores the importance of forging a working relationship with a child from intervention outset.61
The benefits of early family-based interventions are illustrated by a recent randomized controlled trial assessing the effects of the Family Check Up on dysregulated irritability in early childhood. The Family Check Up, which was designed to improve a child’s adjustment by motivating positive behavior support and other family management practices, was composed of a 2-session intervention that was individually tailored to the needs of the family. The sessions typically included an initial contact session, followed by a home-based ecological assessment, and finally a feedback session emphasizing parenting strengths as well as possible areas of change. A total of 8 opportunities for feedback sessions were offered over the 8 years of the study. After feedback sessions each year, families were offered individualized parent training sessions, with 82.8% of families receiving an annual average of less than 3 hours of follow-up intervention services. The authors found intervention effects of Family Check Up on irritability at age 4 years, compared with baseline at age 2, which predicted lower externalizing and internalizing symptoms at 10.5 years of age.62 Decreases in irritability at age 4 predicted long-term improvements in oppositional defiant disorder (ODD), generalized anxiety, and major depression at 10.5 years of age. These findings confirm that irritability in early childhood is a transdiagnostic risk indicator that can be used to identify children and families in need of intervention, and the Family Check Up may have salutary effects on long-term functional outcomes.62
Studies of youth at familial risk for bipolar disorder—who often present with depression, irritability, anxiety, and subthreshold manic states—indicate the benefits of early intervention in delaying progression to full-blown mood disorders. In a pilot randomized controlled trial of 40 high-risk youth, family-focused therapy for youth at high risk for bipolar disorder (FFT-HR), given during 12 sessions over 4 months, was found to hasten time to recovery from depressive symptoms and improve 1-year symptom trajectories compared with a brief educational control. In a more definitive 3-site trial of 127 high-risk youth, FFT-HR was associated with longer time to mood episodes, and specifically, longer well intervals before depressive episodes and lower levels of suicidal ideation and behavior when compared with standard psychoeducation of equal duration.63–65 Youth who received FFT-HR also showed increased ventrolateral prefrontal and anterior default mode brain network connectivity from baseline to end of treatment compared with youth who received standard psychoeducation, demonstrating improved functional connectivity in emotion regulatory neural networks.66 That neural plasticity in these networks preceded any observable mood outcome differences between treatment groups raises the intriguing possibility of neurobiological targeting to prevent mood progression. Time to conversion to bipolar I or II disorder over an average of 2 years of follow-up did not differ between FFT-HR and standard psychoeducation. Larger samples and longer follow-up might more definitively confirm the preventative potential of FFT-HR for mania onset or recurrence.64
In youth with depressive spectrum disorders and transient manic symptoms, Nadkarni and Fristad67 found that immediate treatment with multifamily psychoeducation groups was associated with lower rates of conversion to subthreshold and full threshold bipolar spectrum disorders than a waitlist control. Further research is necessary to clarify the relation between changes in family functioning and changes in the course of illness among high-risk youth, who often present with multiple comorbid disorders and myriad subthreshold mood symptoms.
TERTIARY PREVENTION
For youth already struggling with significant and functionally impairing irritability and temper outbursts, tertiary prevention measures aim to reduce symptom severity and enhance psychosocial functioning. These children are commonly diagnosed with psychiatric disorders such as depression, ADHD, autism, DMDD, or other disruptive behavioral disorders (eg, conduct disorder or ODD). Given the variable contexts in which irritability and temper outbursts occur in these youth, the question arises as to whether emotion dysregulation is a manifestation of the same or distinct psychopathologies. Will the same intervention for chronic emotion dysregulation be efficacious across disorders despite differences in underlying etiologies, or should interventions be tailored to a specific disorder? The answers to these questions are not yet clear; therefore, we provide a cursory review of extant literature on tertiary prevention in the context of specific disorders. We focus on depression, ADHD, autism, and DMDD owing to their common association with irritability or temper outbursts, and defer to other articles in this volume for details.
Depression
Worsening irritability while on antidepressant treatment is associated with poorer outcomes and a decreased likelihood of remission.68 Indeed, youth with depression and a family history of bipolar disorder may be particularly predisposed to antidepressant-related adverse events that include irritability and temper outbursts, underscoring the importance of assessing illness risk factors when weighing treatment benefits against risks.69 In a study on depressed youth in remission after acute treatment with fluoxetine (12 weeks), higher levels of residual irritability, as well as insomnia were associated with increased odds of depressive relapse.70 In contrast, higher levels of resilience, and in particular positive affectivity, were related to a lesser occurrence of residual symptoms after remission from depression.71 Thus, targeting both risk factors for worsening irritability and predictors of residual symptoms early in treatment may decrease relapse rates or clinical worsening.
Attention Deficit Hyperactivity Disorder
Stimulants and behavioral treatment can improve irritability in ADHD.72,73 However, even with optimally titrated first-line stimulant treatment, a subset of youth have persistent aggressive behavior, indicating disability beyond that of ADHD alone.74 Indeed, emotion dysregulation is as much a feature of ADHD as of mood disorders.75 Mood disorders comorbid with ADHD, ODD, or conduct disorder and with high levels of anger or irritability may benefit from risperidone or divalproex sodium augmentation.74,76 The choice of agents is critical here77,78: recent meta-analyses of psychostimulant trials indicate that methylphenidate derivatives (eg, methylphenidate hydrochloride [Ritalin]) may be associated with decreased risk of irritability, whereas amphetamine derivatives (eg, amphetamine/dextroamphetamine [Adderall]) seem to be associated with increased risk of irritability.77,78
Aside from pharmacologic approaches, Hartman and colleagues54 emphasize that assessing stressful conditions in a child’s home should be integral to the diagnosis and treatment of ADHD. Specifically, cumulative high-stress exposure, including chronic illnesses in the child or immediate family member(s), academic pressure, problems at home or the neighborhood, unemployment, financial difficulties, having fewer friendships, being bullied, and having enduring conflicts, related strongly to a persistent course of ADHD with worsening irritability, anxiety, and depression.12 The literature on specific interventions targeting irritability and temper outbursts in children exposed to early life stress or trauma is sparse, but may be benefited by effective treatment of a primary disruptive behavioral disorder.
Autism
Extensive literature has demonstrated the efficacy of pharmacologic treatment for irritability and aggression in autism, which may manifest as temper outbursts and self-injurious behaviors.79 However, pharmacologic interventions do not address the underlying causes of irritability and temper outbursts in autism. Rather, contextual reasons for irritability in autism should be explored so that an appropriate evidence-based nonpharmacologic intervention can target those reasons. If this search strategy fails or if the magnitude of the irritability needs more urgent treatment, psychopharmacologic intervention may prove helpful. To clarify the stepwise guidelines for youth with autism and temper outbursts, a multidisciplinary workgroup has developed a practice pathway for pediatric primary care providers. This pathway emphasizes assessing contextual risk factors (eg, medical, functional communication challenges, psychosocial stressors, maladaptive reinforcement patterns, co-occurring psychiatric conditions) in each patient.80 Appropriate treatment is then based on such contextual factors. For instance, irritability or temper outbursts arising from difficulties using functional communication should be followed up with speech and language evaluations, with the inclusion of a communication component in a behavior treatment plan. In contrast, irritability arising from psychosocial stressors, such as poor adjustment to classroom or program characteristics, would warrant communication with the school to address potential changes to the classroom or curriculum. If co-occurring psychiatric disorders are present, treatment with medications may then be considered.
Disruptive Mood Dysregulation Disorder
DMDD is characterized by recurrent temper outbursts in the context of ongoing depressed, anxious, or irritable moods. The current literature has primarily focused on psychopharmacologic treatments for DMDD. Open-label studies of methylphenidate with or without aripiprazole and combined with parent training have shown efficacy in improving irritability and other clinical symptoms (eg, emotional lability, negative affect, and anger) in DMDD and its related precursor severe mood dysregulation.81,82 Exposure-based cognitive behavioral therapy in which youth with DMDD are exposed to frustrating situations is currently being evaluated. This treatment is theorized to engage cognitive control and top-down regulation of frustration to interrupt symptom reinforcement.83 How to integrate and personalize pharmacologic and psychosocial treatments beyond treating readily identifiable psychiatric comorbidities is an unmet need in our field.
Given the high rates of comorbid psychopathology associated with DMDD (eg, ODD, ADHD, anxiety disorders),84 other symptom dimensions often need intervention. One study in children with DMDD (with and without ADHD) found that an association between DMDD and sleep problems is mediated by their shared association with oppositional behaviors.85 Thus, oppositional behaviors may need targeting before other symptoms such as sleep dysregulation are addressed. Building resiliencethrough teaching emotion regulation skills, classically included in dialectical behavioral therapy (DBT), may decrease the frequency of temper outbursts and associated psychosocial impairments. A pilot randomized controlled trial of 43 children with DMDD (7–12 years old) demonstrated the feasibility and preliminary efficacy of DBT (adapted for preadolescents in 32 weekly 90-minute sessions) compared with a comparison group receiving individual therapy and medication management.86 Notably, the DBT versus comparison group had higher response rates (90.4% vs 45.5%, respectively). Importantly, the improvements from DBT were achieved without a need to start new psychiatric medications. The efficacy of DBT for decreasing DMDD behaviors should be further tested in randomized controlled trials that include manualized, equally intensive comparison treatments.
SUMMARY
Chronic irritability and temper outbursts—both indicators of emotional dysregulation—are transdiagnostic constructs that can significantly disrupt achievement of typical developmental milestones and result in psychopathology and impairment. An evidence base for early interventions is scarce, but the need to identify at-risk children and intervene early to promote positive neurodevelopmental outcomes cannot be un-derstated. Wakschlag and colleagues,87 in their translational road map entitled Mental Health, Earlier, recommend primary care screening of irritability as a risk factor for lifelong mental health problems, and low intensity interventions to promote self-regulation within an implementation science framework.
More research is needed to determine whether irritability and temper outbursts are disorder specific or share common neurobiological underpinnings. Primary prevention strategies can intervene at the level of the parent (eg, targeting parental mental health and parenting skills), the child (eg, targeting affective instability, self-esteem and self-compassion), and the community (eg, after school programs for at-risk youth to promote socioemotional learning, gun control, and violence prevention programs). Secondary prevention strategies might focus on intervening on family systems and effecting positive changes in the course of high-risk syndromes. Accelerating biomarker discovery and investigating clinically meaningful treatment targets and mechanisms would support the development of novel tertiary prevention strategies to reduce symptom burden and impairment. A research agenda focused on identifying interventions in the context of primary, secondary, and tertiary prevention of chronic irritability and temper outbursts will be essential to promoting resilience and reducing risks of lifelong psychopathology.
KEY POINTS.
Chronic irritability and temper outbursts are transdiagnostic constructs that can disrupt achievement of typical developmental milestones and result in psychopathology and lifelong impairment.
An evidence base for preventive interventions is limited and more research is needed to determine whether irritability and temper outbursts are disorder-specific or share common neurobiological underpinnings.
Parent, child, and community-based approaches have empirical support.
Secondary prevention studies on the relations between changes in family functioning - for example, from family-focused therapy - and changes in the course of high-risk syndromes can help clarify treatment targets and mechanisms.
Tertiary prevention aims to reduce symptom severity and enhance psychosocial functioning.
DISCLOSURE
Dr M.K. Singh has received research support from Stanford’s Maternal Child Health Research Institute and the Department of Psychiatry, National Institute of Mental Health, National Institute on Aging, Johnson and Johnson, Allergan, and the Brain and Behavior Foundation. She is on the advisory board for Sunovion, has been a consultant for X: The moonshot factory (Alphabet Inc), and Limbix, and receives royalties from the American Psychiatric Association Publishing. Dr D.J. Miklowitz has received grant funding from the National Institute of Mental Health (NIMH), the Danny Alberts Foundation, the Attias Family Foundation, the Carl and Roberta Deutsch Foundation, the Kayne Family Foundation, the Jewish Foundation of Los Angeles, AIM for Youth Mental Health, and the Max Gray Fund; and book royalties from Guilford Press and John Wiley and Sons.
Abbreviations
- ADHD
attention deficit with hyperactivity
- DBT
dialectical behavioral therapy
- DMDD
disruptive mood dysregulation disorder
- FFT-HR
family-focused therapy for youth at high risk for bipolar disorder
- ODD
oppositional defiant disorder
REFERENCES
- 1.Dougherty LR, Smith VC, Bufferd SJ, et al. Disruptive mood dysregulation disorder at the age of 6 years and clinical and functional outcomes 3 years later. Psychol Med 2016;46(5):1103–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wesselhoeft R, Stringaris A, Sibbersen C, et al. Dimensions and subtypes of oppositionality and their relation to comorbidity and psychosocial characteristics. Eur Child Adolesc Psychiatry 2019;28(3):351–65. [DOI] [PubMed] [Google Scholar]
- 3.Stringaris A, Vidal-Ribas P, Brotman MA, et al. Practitioner review: definition, recognition, and treatment challenges of irritability in young people. J Child Psychol Psychiatry 2018;59(7):721–39. [DOI] [PubMed] [Google Scholar]
- 4.Eyre O, Riglin L, Leibenluft E, et al. Irritability in ADHD: association with later depression symptoms. Eur Child Adolesc Psychiatry 2019;28(10):1375–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benarous X, Consoli A, Cohen D, et al. Suicidal behaviors and irritability in children and adolescents: a systematic review of the nature and mechanisms of the association. Eur Child Adolesc Psychiatry 2019;28(5):667–83. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edition. Arlington (VA): American Psychiatric Association; 2013. [Google Scholar]
- 7.Riglin L, Eyre O, Thapar AK, et al. Identifying novel types of irritability using a developmental genetic approach. Am J Psychiatry 2019;176(8):635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leibenluft E, Cohen P, Gorrindo T, et al. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol 2006;16(4):456–66. [DOI] [PubMed] [Google Scholar]
- 9.Blader JC, Pliszka SR, Kafantaris V, et al. Prevalence and treatment outcomes of persistent negative mood among children with attention-deficit/hyperactivity disorder and aggressive behavior. J Child Adolesc Psychopharmacol 2016;26(2): 164–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayes SD, Mathiowetz C, Kokotovich C, et al. Stability of disruptive mood dysregulation disorder symptoms (irritable-angry mood and temper outbursts) throughout childhood and adolescence in a general population sample. J Abnorm Child Psychol 2015;43(8):1543–9. [DOI] [PubMed] [Google Scholar]
- 11.Evans SC, Burke JD, Roberts MC, et al. Irritability in child and adolescent psychopathology: an integrative review for ICD-11. Clin Psychol Rev 2017;53:29–45. [DOI] [PubMed] [Google Scholar]
- 12.Hartman CA, Rommelse N, van der Klugt CL, et al. Stress exposure and the course of ADHD from childhood to young adulthood: comorbid severe emotion dysregulation or mood and anxiety problems. J Clin Med 2019;8(11):1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masten AS. Resilience theory and research on children and families: past, present, and promise. J Fam Theory Rev 2018;10(1):12–31. [Google Scholar]
- 14.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health 2005;26: 399–419. [DOI] [PubMed] [Google Scholar]
- 15.Goodman R Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40(11):1337–45. [DOI] [PubMed] [Google Scholar]
- 16.Wilson DS, O’Brien DT, Sesma A. Human prosociality from an evolutionary perspective: variation and correlations at a city-wide scale. Evol Hum Behav 2009;30(3):190–200. [Google Scholar]
- 17.Padilla-Walker LM, Memmott-Elison MK, Coyne SM. Associations between prosocial and problem behavior from early to late adolescence. J Youth Adolesc 2018; 47(5):961–75. [DOI] [PubMed] [Google Scholar]
- 18.Jung J, Schröder-Abé M. Prosocial behavior as a protective factor against peers’ acceptance of aggression in the development of aggressive behavior in childhood and adolescence. J Adolesc 2019;74:146–53. [DOI] [PubMed] [Google Scholar]
- 19.Huang S, Han M, Sun L, et al. Family socioeconomic status and emotional adaptation among rural-to-urban migrant adolescents in China: the moderating roles of adolescent’s resilience and parental positive emotion. Int J Psychol 2019;54(5): 573–81. [DOI] [PubMed] [Google Scholar]
- 20.Poole JC, Dobson KS, Pusch D. Anxiety among adults with a history of childhood adversity: psychological resilience moderates the indirect effect of emotion dysregulation. J Affect Disord 2017;217:144–52. [DOI] [PubMed] [Google Scholar]
- 21.Gartland D, Riggs E, Muyeen S, et al. What factors are associated with resilient outcomes in children exposed to social adversity? A systematic review. BMJ Open 2019;9(4):e024870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frazier SL, Dinizulu SM, Rusch D, et al. Building Resilience After School for Early Adolescents in Urban Poverty: Open Trial of Leaders @ Play. Adm Policy Ment Health 2015;42:723–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carlson GA, Chua J, Pan K, et al. Behavior modification is associated with reduced psychotropic medication use in children with aggression in inpatient treatment: a retrospective cohort study. J Am Acad Child Adolesc Psychiatry 2020;59(5):632–41.e4. [DOI] [PubMed] [Google Scholar]
- 24.Schäfer JÖ, Naumann E, Holmes EA, et al. Emotion regulation strategies in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc 2017;46(2):261–76. [DOI] [PubMed] [Google Scholar]
- 25.Trompetter HR, de Kleine E, Bohlmeijer ET. Why does positive mental health buffer against psychopathology? An exploratory study on self-compassion as a resilience mechanism and adaptive emotion regulation strategy. Cognit Ther Res 2017;41(3):459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu Q, Slesnick N, Murnan A, et al. Understanding parenting stress and children’s behavior problems among homeless, substance-abusing mothers. Infant Ment Health 2018;39:423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramakrishnan JL, Masten AS. Mastery motivation and school readiness among young children experiencing homelessness. Am J Orthopsychiatry 2020;90(2): 223–35. [DOI] [PubMed] [Google Scholar]
- 28.Caiozzo CN, Yule K, Grych J. Caregiver behaviors associated with emotion regulation in high-risk preschoolers. J Fam Psychol 2018;32(5):565–74. [DOI] [PubMed] [Google Scholar]
- 29.Kaufman EA, Puzia ME, Mead HK, et al. Children’s emotion regulation difficulties mediate the association between maternal borderline and antisocial symptoms and youth behavior problems over 1 year. J Pers Disord 2017;31(2):170–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rappaport LM, Carney DM, Brotman MA, et al. A population-based twin study of childhood irritability and internalizing syndromes. J Clin Child Adolesc Psychol 2020;49(4):524–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roberson-Nay R, Leibenluft E, Brotman MA, et al. Longitudinal stability of genetic and environmental influences on irritability: from childhood to young adulthood. Am J Psychiatry 2015;172(7):657–64. [DOI] [PubMed] [Google Scholar]
- 32.Blair C, Zelazo PD, Greenberg MT. The measurement of executive function in early childhood. Dev Neuropsychol 2005;28(2):561–71. [DOI] [PubMed] [Google Scholar]
- 33.Leibenluft E Pediatric irritability: a systems neuroscience approach. Trends Cogn Sci 2017;21(4):277–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wakschlag LS, Perlman SB, Blair RJ, et al. The neurodevelopmental basis of early childhood disruptive behavior: irritable and callous phenotypes as exemplars. Am J Psychiatry 2018;175(2):114–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kisling LA, Das JM. Prevention strategies. In: StatPearls. StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 36.Brody JL, Scherer DG, Turner CW, et al. A conceptual model and clinical framework for integrating mindfulness into family therapy with adolescents. Fam Process 2018;57(2):510–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu Q, Slesnick N, Murnan A. Understanding parenting stress and children’s behavior problems among homeless, substance-abusing mothers. Infant Ment Health J 2018;39(4):423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weissman MM, Pilowsky DJ, Wickramaratne PJ, et al. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA 2006; 295(12):1389–98. [DOI] [PubMed] [Google Scholar]
- 39.Weissman MM, Wickramaratne P, Pilowsky DJ, et al. Treatment of maternal depression in a medication clinical trial and its effect on children. Am J Psychiatry 2015;172(5):450–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zalewski M, Lewis JK, Martin CG. Identifying novel applications of dialectical behavior therapy: considering emotion regulation and parenting. Curr Opin Psychol 2018;21:122–6. [DOI] [PubMed] [Google Scholar]
- 41.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54(6): 1063–70. [DOI] [PubMed] [Google Scholar]
- 42.Buckner JC, Mezzacappa E, Beardslee WR. Characteristics of resilient youths living in poverty: the role of self-regulatory processes. Dev Psychopathol 2003; 15(1):139–62. [DOI] [PubMed] [Google Scholar]
- 43.West AE, Schenkel LS, Pavuluri MN. Early childhood temperament in pediatric bipolar disorder and attention deficit hyperactivity disorder. J Clin Psychol 2008; 64(4):402–21. [DOI] [PubMed] [Google Scholar]
- 44.Akiskal HS, Hirschfeld RMA, Yerevanian BI. The relationship of personality to affective disorders: a critical review. Arch Gen Psychiatry 1983;40(7):801–10. [DOI] [PubMed] [Google Scholar]
- 45.Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, et al. Further evidence of association between behavioral inhibition and social anxiety in children. Am J Psychiatry 2001;158(10):1673–9. [DOI] [PubMed] [Google Scholar]
- 46.Krueger RF, Hicks BM, Patrick CJ, et al. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol 2002;111(3):411–24. [PubMed] [Google Scholar]
- 47.Pisecco S, Baker DB, Silva PA, et al. Boys with reading disabilities and/or ADHD: distinctions in early childhood. J Learn Disabil 2001;34(2):98–106. [DOI] [PubMed] [Google Scholar]
- 48.Klein DN, Finsaas MC. The stony brook temperament study: early antecedents and pathways to emotional disorders. Child Dev Perspect 2017;11(4):257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Lissa CJ, Hawk ST, Koot HM, et al. The cost of empathy: parent-adolescent conflict predicts emotion dysregulation for highly empathic youth. Dev Psychol 2017;53(9):1722–37. [DOI] [PubMed] [Google Scholar]
- 50.Vannucci A, Finan L, Ohannessian CM, et al. Protective factors associated with daily affective reactivity and instability during adolescence. J Youth Adolesc 2019;48(4):771–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leary MR, Baumeister RF. The nature and function of self-esteem: sociometer theory. In: Zanna MP, editor. Advances in experimental social psychology, vol. 32. Cambridge (MA): Academic Press; 2000. p. 1–62. [Google Scholar]
- 52.Arslan G Psychological maltreatment, emotional and behavioral problems in adolescents: the mediating role of resilience and self-esteem. Child Abuse Negl 2016;52:200–9. [DOI] [PubMed] [Google Scholar]
- 53.Dang MT. Social connectedness and self-esteem: predictors of resilience in mental health among maltreated homeless youth. Issues Ment Health Nurs 2014;35(3):212–9. [DOI] [PubMed] [Google Scholar]
- 54.Hartman CA, Rommelse N, van der Klugt CL, et al. Stress Exposure and the Course of ADHD from Childhood to Young Adulthood: Comorbid Severe Emotion Dysregulation or Mood and Anxiety Problems. J Clin Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hipson WE, Gardiner SL, Coplan RJ, et al. Maternal agreeableness moderates associations between young children’s emotion dysregulation and socioemotional functioning at school. J Genet Psychol 2017;178(2):102–7. [DOI] [PubMed] [Google Scholar]
- 56.McCrae RR, Costa PT. Validation of the five-factor model of personality across instruments and observers. J Pers Soc Psychol 1987;52(1):81–90. [DOI] [PubMed] [Google Scholar]
- 57.Schönfelder S, Kanske P, Heissler J, et al. Time course of emotion-related responding during distraction and reappraisal. Soc Cogn Affect Neurosci 2014; 9(9):1310–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sheppes G, Scheibe S, Suri G, et al. Emotion regulation choice: a conceptual framework and supporting evidence. J Exp Psychol Gen 2014;143(1):163–81. [DOI] [PubMed] [Google Scholar]
- 59.Alkoby A, Pliskin R, Halperin E, et al. An eight-week mindfulness-based stress reduction (MBSR) workshop increases regulatory choice flexibility. Emotion 2019;19(4):593–604. [DOI] [PubMed] [Google Scholar]
- 60.Biglan A The nurture effect: how the science of human behavior can improve our lives and our world. Oakland (CA): New Harbinger Publications; 2015. p. xii, 253. [Google Scholar]
- 61.Flückiger C, Rubel J, Del Re AC, et al. The reciprocal relationship between alliance and early treatment symptoms: a two-stage individual participant data meta-analysis. J Consult Clin Psychol 2020;88(9):829–43. [DOI] [PubMed] [Google Scholar]
- 62.Smith JD, Wakschlag L, Krogh-Jespersen S, et al. Dysregulated irritability as a window on young children’s psychiatric risk: transdiagnostic effects via the family check-up. Dev Psychopathol 2019;31(5):1887–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miklowitz DJ, Schneck CD, Singh MK, et al. Early intervention for symptomatic youth at risk for bipolar disorder: a randomized trial of family-focused therapy. J Am Acad Child Adolesc Psychiatry 2013;52(2):121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miklowitz DJ, Schneck CD, Walshaw PD, et al. Effects of family-focused therapy vs enhanced usual care for symptomatic youths at high risk for bipolar disorder: a randomized clinical trial. JAMA Psychiatry 2020;77(5):455–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miklowitz DJ, Merranko JA, Weintraub MJ, et al. Effects of family-focused therapy on suicidal ideation and behavior in youth at high risk for bipolar disorder. J Affect Disord 2020;275:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singh MK, Nimarko AF, Garrett AS, et al. Changes in intrinsic brain connectivity in family-focused therapy versus standard psychoeducation among youths at high risk for bipolar disorder. J Am Acad Child Adolesc Psychiatry 2021;60(4):458–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nadkarni RB, Fristad MA. Clinical course of children with a depressive spectrum disorder and transient manic symptoms. Bipolar Disord 2010;12(5):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jha MK, Minhajuddin A, South C, et al. Worsening anxiety, irritability, insomnia, or panic predicts poorer antidepressant treatment outcomes: clinical utility and validation of the concise associated symptom tracking (CAST) scale. Int J Neuropsy-chopharmacol 2018;21(4):325–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Angal S, DelBello M, Zalpuri I, et al. Clinical conundrum: how do you treat youth with depression and a family history of bipolar disorder? Bipolar Disord 2019; 21(4):383–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kennard BD, Mayes TL, Chahal Z, et al. Predictors and moderators of relapse in children and adolescents with major depressive disorder. J Clin Psychiatry 2018; 79(2):15m10330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hoorelbeke K, Van den Bergh N, Wichers M, et al. Between vulnerability and resilience: a network analysis of fluctuations in cognitive risk and protective factors following remission from depression. Behav Res Ther 2019;116:1–9. [DOI] [PubMed] [Google Scholar]
- 72.Fernández de la Cruz L, Simonoff E, McGough JJ, et al. Treatment of children with attention-deficit/hyperactivity disorder (ADHD) and irritability: results from the multimodal treatment study of children with ADHD (MTA). J Am Acad Child Adolesc Psychiatry 2015;54(1):62–70.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Galanter CA, Pagar DL, Davies M, et al. ADHD and manic symptoms: diagnostic and treatment implications. Clin Neurosci Res 2005;5(5):283–94. [Google Scholar]
- 74.Blader JC, Pliszka SR, Kafantaris V, et al. Stepped treatment for attention-deficit/hyperactivity disorder and aggressive behavior: a randomized, controlled trial of adjunctive risperidone, divalproex sodium, or placebo after stimulant medication optimization. J Am Acad Child Adolesc Psychiatry 2021;60(2):236–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Marwaha S, He Z, Broome M, et al. How is affective instability defined and measured? A systematic review. Psychol Med 2014;44(9):1793–808. [DOI] [PubMed] [Google Scholar]
- 76.Farmer CA, Brown NV, Gadow KD, et al. Comorbid symptomatology moderates response to risperidone, stimulant, and parent training in children with severe aggression, disruptive behavior disorder, and attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2015;25(3):213–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pozzi M, Carnovale C, Peeters GGAM, et al. Adverse drug events related to mood and emotion in paediatric patients treated for ADHD: a meta-analysis. J Affect Disord 2018;238:161–78. [DOI] [PubMed] [Google Scholar]
- 78.Stuckelman ZD, Mulqueen JM, Ferracioli-Oda E, et al. Risk of irritability with psychostimulant treatment in children with ADHD: a meta-analysis. J Clin Psychiatry 2017;78(6):e648–55. [DOI] [PubMed] [Google Scholar]
- 79.Fung LK, Mahajan R, Nozzolillo A, et al. Pharmacologic treatment of severe irritability and problem behaviors in autism: a systematic review and meta-analysis. Pediatrics 2016;137(Suppl 2):S124–35. [DOI] [PubMed] [Google Scholar]
- 80.McGuire K, Fung LK, Hagopian L, et al. Irritability and problem behavior in autism spectrum disorder: a practice pathway for pediatric primary care. Pediatrics 2016;137(Suppl 2):S136–48. [DOI] [PubMed] [Google Scholar]
- 81.Winters DE, Fukui S, Leibenluft E, et al. Improvements in irritability with open-label methylphenidate treatment in youth with comorbid attention deficit/hyperactivity disorder and disruptive mood dysregulation disorder. J Child Adolesc Psychopharmacol 2018;28(5):298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pan P-Y, Fu A-T, Yeh C-B. Aripiprazole/methylphenidate combination in children and adolescents with disruptive mood dysregulation disorder and attention-deficit/hyperactivity disorder: an open-label study. J Child Adolesc Psychopharmacol 2018;28(10):682–9. [DOI] [PubMed] [Google Scholar]
- 83.Kircanski K, Craske MG, Averbeck BB, et al. Exposure therapy for pediatric irritability: theory and potential mechanisms. Behav Res Ther 2019;118:141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leibenluft E Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry 2011;168(2):129–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Waxmonsky JG, Mayes SD, Calhoun SL, et al. The association between disruptive mood dysregulation disorder symptoms and sleep problems in children with and without ADHD. Sleep Med 2017;37:180–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Perepletchikova F, Nathanson D, Axelrod SR, et al. Randomized clinical trial of dialectical behavior therapy for preadolescent children with disruptive mood dysregulation disorder: feasibility and outcomes. J Am Acad Child Adolesc Psychiatry 2017;56(10):832–40. [DOI] [PubMed] [Google Scholar]
- 87.Wakschlag LS, Roberts MY, Flynn RM, et al. Future directions for early childhood prevention of mental disorders: a road map to mental health, earlier. J Clin Child Adolesc Psychol 2019;48(3):539–54. [DOI] [PMC free article] [PubMed] [Google Scholar]


