Introduction:
Patients with advanced incurable cancer do not make important health decisions in isolation. Rather, medical decisions typically are based on information, perspectives, stories, and advice from multiple sources. With the patient and health care professionals, these sources also interact, forming a dynamic relational process between the patient, his/her social networks, and health care professionals (1). However, patients rarely mention these sources to clinicians.
The influence of social networks is particularly important when it comes to discussions of prognosis. Patients unaware of their prognosis are at risk for receiving burdensome treatments with little prospect of improving quality of life (QoL). Because clinicians tend to prioritize discussions of test results and treatment recommendations, defer discussions of patients’ illness beliefs, information sources, and prognosis (2), and use vague language when describing risks, benefits and outcomes, patients are left unaware or uncertain of their prognosis. Unsurprisingly, patients often seek counsel from social network members who might provide information that is both helpful and accurate, or might also augment misconceptions about prognosis and treatment intent (curative versus palliative) (3), leading patients to pursue cancer treatments that ultimately result in lower QoL and delay in initiating palliative measures (4).
Older adults with advanced cancer are particularly vulnerable to harms due to lack of prognostic understanding. With adequate prognostic understanding, older patients more often communicate a preference for comfort-oriented approaches and palliative care (5). Yet, in addition to reluctance to discuss prognosis, communication is further hampered by the paucity of clinical trials that include older patients and those with aging-related conditions (i.e., disability, comorbidity) (6) and high symptom burden (7), resulting in optimistically-biased discussions about the benefits and risks of treatments (8).
Older adults with aging-related conditions are more likely to depend on social networks for instrumental support and communication with clinicians, and are more likely to be accompanied at office visits, especially those with low health literacy, higher symptom burden and with functionally limitations (9). Caregivers typically accompany older patients when important information is divulged (1); they were present in 86% of oncology visits when “bad news” was delivered about prognosis or lack of treatment options (1). As health and function declines, older patients increasingly defer decision-making to caregivers (10). While caregivers can be strong advocates, ensuring the accuracy of information exchange and understanding (11), sometimes they selectively filter information, overshadow patients’ perspectives (12), or act as spokespersons for a larger social network (13).
The nature of social networks:
Older patients’ networks are diverse and complex, including friends and family, cancer survivors, and other groups (such as clergy and acquaintances), all of whom might provide some kind of medical advice. Frequency of contact or length of relationship are not necessarily associated with influence on understanding and decision-making (14). While close relatives might be expected to provide support (15) they might be sources of tension and hinder communication and self-management of the disease (16), leading older patients to rely primarily on weaker social connections and anonymous online networks (17). Those weaker connections may also be important, for example, by raising issues that close relatives are reluctant to discuss.
Social networks evolve dynamically over time. In response to a stressful life event (e.g. diagnosis of a severe disease) older patients activate relationships within their networks that they perceive as best supporting their particular needs at the time, selecting from among a larger group of potential network members taking into account availability and potential costs (18). On the other hand, unprecedented medical conditions may result in shrinkage of social networks, as individuals’ roles and expectations and the older patient’s capabilities for social interactions change (19). Older patients may change the network compositions, for example, preferentially affiliating with those who reinforce over-optimistic prognoses (20), and those who are less likely to stigmatize their illness (19).
Studying social networks:
A common approach to study social networks, particularly in the field of social support is assessing the change in the size of personal networks (21), or individuals’ assessment of social support (22). Existing tools, such as the Berkman Syme Social Network Index (23), typically aggregate the number of individuals in particular social groups (family, friends, colleagues, etc.) into a single score to study associations between these indices and important health outcomes. Yet, this approach may not take into account the context-dependent nature of these relationships (24). Here, we describe a methodologic approach that lends insight into these diverse and nuanced structures, content and processes that characterize social networks of older patients with advanced cancer.
Mixed-Methods Social Network Analysis (MMSNA) can be particularly useful in shedding light into the complexity of older patients’ networks. MMSNA is an approach to study the patterns of relationships between “actors” in a network by integrating quantitative information about network structures with qualitative insights about perspectives of network actors (25). MMSNA addresses structure (e.g., How well connected is the patient?; Who are the influential actors?; Are there clusters or structural gaps?) and process (e.g., What information, advice and stories are shared?; What information is withheld?; When and with whom are decisions made?). In a fully-integrated MMSNA, quantitative and qualitative data are collected and analyzed simultaneously (in contrast to conventional mixed methods approaches that collect and analyze quantitative and qualitative data in parallel or sequentially) (26). In semi-structured interviews, respondents provide data about members of their social network, display inter-relationships among network members graphically, and comment on the nature, meaning and impact of those relationships. Interviews also reveal important information about targets for intervention by illuminating how older patients reconcile competing perspectives on their illness (e.g. when family’s beliefs conflict with doctors’, or when patients hesitate to communicate in burdensome family networks).
An application of MMSNA:
In this paper we use the experience of a pilot study of social networks of older patients with advanced cancer to introduce an integrated mixed-methods approach to study personal networks of older patients with advanced cancer. In this study, we sought to clarify ways in which social network members informed older patients’ understanding of their disease, prognosis, and treatment choices.
After ethics approval and informed consent, we interviewed 16 older patients, collecting quantitative and qualitative network data simultaneously using network maps (27). The patient (ego) lists social contacts (alters) with whom they have discussed health-related issues, and marks the strength of their relationships on a chart comprised of concentric circles with ego at the center and radial sections representing various social categories (Figure 1a). After placing all alters on the map, the older patient draws lines connecting alters to show connections between pairs. The older patients then elaborate on the quality, content, and dynamics of each social relation.
Figure 1: An example of network chart developed in social network interview of patients #24. 1a: the chart that was completed in the interview. 1b: a force-directed map created based on 1a.
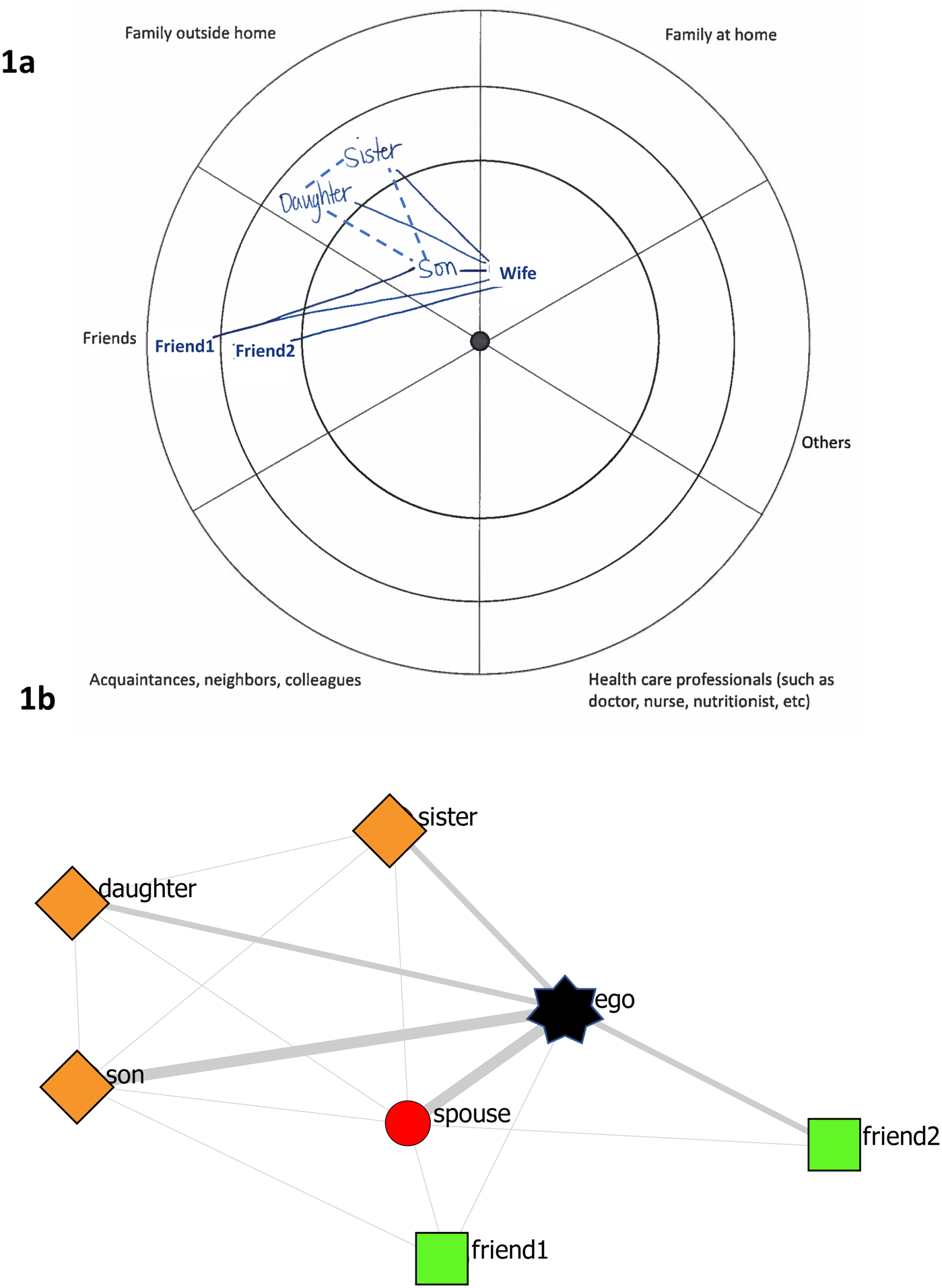
1a: Solid lines were drawn by the patient. Dashed lines were added after reading the transcript. Some names were masked to preserve patient’s identity. 1b: line thickness represents the actor’s place on inner, middle, or outer circles. Actors are distributed using Spring embedding algorithm force-directed algorithm. Star: ego, circle: family at home, diamond: family outside home, square: friends.
Our integrated mixed-method analysis was exploratory, inductive, and iterative, aiming to identify and score main dimensions that distinguished networks from one another. The analytic procedure included:
Framing:
In order to find a graphical presentation that represent the complexities and patterns of social relations in personal networks, we restructured the interview maps using force-directed algorithms (28) (Figure 1b), to redistribute the nodes based on their connection patterns.
Pattern Detection:
This process involved identification of network dimensions, and then sorting the maps. The multi-step qualitative coding process (29) included: holistic coding (exploring the overall shapes of network maps; such as resemblance to star network, segregated clusters, etc; see table 1 for results), structural coding (using conventional network analysis measures such as density, reciprocity, centralization etc (30)), attribute coding (using compositional and personal attributes as codes, such as position of health care professionals, main caregiver or other significant social roles in the network), and exploratory coding (identifying emergent non-a priori features). After identification of main dimensions, we sorted the maps, and identified extreme cases (two ends of the continuum) and typical cases (middle of the continuum). Team members worked independently, then reconciled their differing insights in regular consensus meetings.
Table 1:
Structural and membership dimensions identified through analysis
| Domain | Definition |
|---|---|
| Structural dimensions | |
| Cohesive Circle | existence of a densely connected circle/cluster in the network (most people are connected to each other) usually family and friends |
| Segregated | existence of separate (weakly connected) clusters, usually identified by different social roles: family, friends, colleagues, etc. |
| Star | a network resembling a central actor (ego), with most people connected to it, with no (rare) connections between those partners. A network that looks like a cartwheel |
| Membership dimensions | |
| Core | one (or more) central actor who is connected to almost everybody that ego is connected. The main caregiver. Often the spouse |
| Health Care professional’s inclusion /embeddedness | your judgment of how strongly/frequently health care professionals are connected to ego and other network members |
| Others’ embeddedness | your judgment of how strongly/frequently members of OTHERS group (e.g. religious figures, patient experts, etc.) are connected to ego and other network members |
| Family Dominance | the overall picture of network, how dominantly the network is shaped by the family (number, strength of ties to ego, connections with each other) in comparison to other groups |
| Role Diversity | the overall picture of network, how diverse the network is in terms of multiplicity of social roles. The extreme low is a network that is only made of family |
Labeling:
In consensus meetings, we discussed the meaningful labels for identified dimensions. This process resembles mixed methods ‘qualitization’ (31), a set of procedures aiming to transform patterns and numbers into words and narrative profiles.
As shown in Table 1, we identified three structural dimensions and 5 membership dimensions. The four networks in Figure 2 are organized around the structural dimensions, while also presenting membership dimensions; dimensions are not mutually exclusive. Figure 2a shows a network with a prominent Core member (here the spouse) who is connected to the majority of the ego’s network, and also to some extent resembling a star network of unconnected network members. Figure 2b presents a cohesive circle of tightly-knit family and friends, characterized by family dominance. Figure 2c shows segregated clusters with weak connections across clusters. Figure 2d exemplifies embeddedness of healthcare professionals (pink), embeddedness of other social contacts (blue; neighbors and co-workers), and role diversity.
Figure 2: Four examples of networks prominently present the structural and membership dimensions.
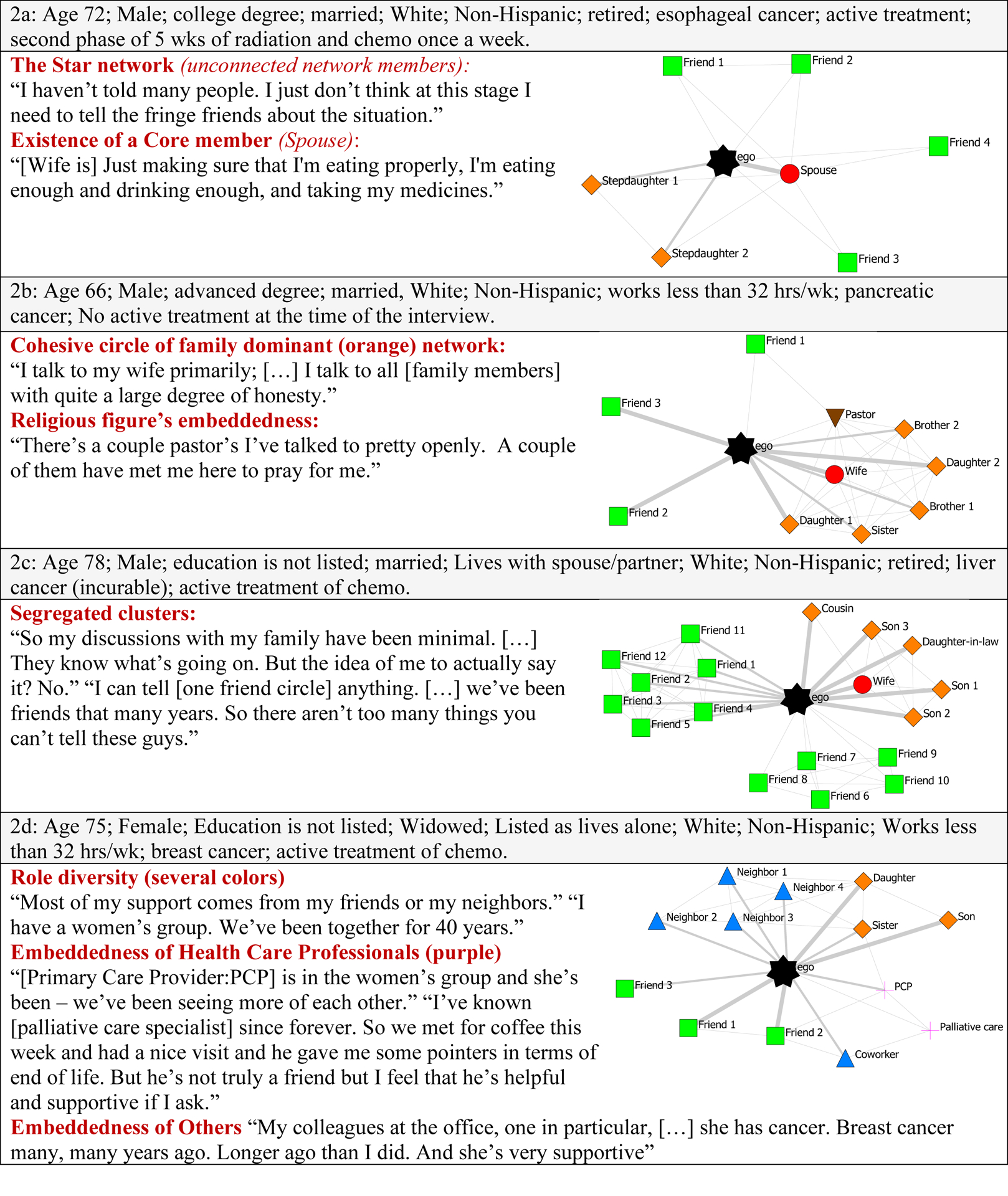
Star: ego, circle: family at home, diamond: family outside home, square: friends, up triangle: neighbors and acquaintances, down triangle: others, plus: healthcare professionals
Next steps of the analysis will include further integration of quantitative and qualitative data. Networks could be scored along the dimensions and resulting variables could be used in statistical models to assess the relationship between dimensional scores and clinical and prognostic variables. The network dimensions can also inform further purposeful sampling for qualitative assessments to learn about specific social dynamics that happen in each network type.
Discussion:
Even with our small sample size in this pilot study, we identified three thematic structural dimensions, corresponding to: a) segregated clusters, b) star-shaped, and c) core. While linking network structure and care outcomes is premature from our data, others have showed important associations between network structures and important outcomes, such as self-management in long-term illness (32), physical functioning following stroke (33), injurious falls and functional decline (34). For example, among older cancer survivors, adding two new relationships exhibited protective effects against functional decline, and declines in frequency of contacts were associated with greater functional impairment (35).
In our sample, health care professionals were rarely included in older patients’ networks, suggesting reasons why older patients often do not understand, accept, or heed information that they receive from clinicians. Recognizing that the clinician is only a node in a more complex and dynamic information-sharing network (36) can enable them to intervene to enhance communication and strengthen relationships by engaging influential network members (with patient consent) to provide information and facilitate decision-making (36). Providing older patients’ personal care maps to health care providers may help them better understand the “person-in-context” (37), enabling more productive and effective communication about treatment choices and prognosis, and ultimate foster shared mind between older patients and health care professionals (38).
Network maps are graphical representations of social worlds that influence health care, and are particularly useful when older patients are seriously ill, symptomatic, and facing uncertainty and seeking information to guide important decisions regarding their care. Our approach to MMSNA is a novel analytic method that can help us simultaneously analyze graphical representations of older patients’ social worlds (network maps), and rich personal stories about illness experiences and perspectives obtained through qualitative inquiry with older patients and their key network members, yielding insights not possible by considering these data sources separately. These insights can help health professionals engage older patients’ social networks in ways that ultimately improve older patient understanding, agency, and QoL.
Acknowledgements:
That authors are grateful to Ms Chandrika Sanapala, Ms Lee A Kehoe, Ms Grace DiGiovanni, and Dr Melissa Loh for their assistance in data collection and analysis.
Financial support:
The work was funded through a K24 AG056589 (Mohile), pilot funds from the Wilmot Cancer Institute and philanthropy to the Wilmot Cancer Institute geriatric oncology program. All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the official views of the funding agencies.
Footnotes
Conflict of interest: All authors have declared no conflicts of interest.
Contributor Information
Reza Yousefi Nooraie, Department of Public Health Sciences, School of Medicine & Dentistry, University of Rochester, 265 Crittenden Blvd., CU 420644, Rochester, New York 14642.
Supriya G. Mohile, James P Wilmot Cancer Institute, School of Medicine & Dentistry, University of Rochester, 90 Crittenden Blvd, Rochester, NY 14642, Rochester, NY, USA.
Sule Yilmaz, Geriatric Oncology Research. University of Rochester, 265 Crittenden Blvd, Rochester, NY 14620.
Jessica Bauer, School of Medicine & Dentistry, University of Rochester, 90 Crittenden Blvd, Rochester, NY 14642, Rochester, NY, USA.
Ronald M. Epstein, Department of Family Medicine Research, 1381 South Ave, Rochester, NY 14620.
References:
- 1.Eggly S, Penner LA, Greene M, Harper FWK, Ruckdeschel JC, Albrecht TL. Information seeking during “bad news” oncology interactions: Question asking by patients and their companions. Social Science & Medicine. 2006;63(11):2974–85. [DOI] [PubMed] [Google Scholar]
- 2.Shields CG, Coker CJ, Poulsen SS, Doyle JM, Fiscella K, Epstein RM, et al. Patient-centered communication and prognosis discussions with cancer patients. Patient education and counseling. 2009;77(3):437–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loh KP, Mohile SG, Lund JL, Epstein R, Lei L, Culakova E, et al. Beliefs About Advanced Cancer Curability in Older Patients, Their Caregivers, and Oncologists. Oncologist. 2019;24(6):e292–e302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norton SA, Wittink MN, Duberstein PR, Prigerson HG, Stanek S, Epstein RM. Family caregiver descriptions of stopping chemotherapy and end-of-life transitions. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2019;27(2):669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loh KP, Mohile SG, Epstein RM, McHugh C, Flannery M, Culakova E, et al. Willingness to bear adversity and beliefs about the curability of advanced cancer in older adults. Cancer. 2019;125(14):2506–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohile SG, Dale W, Somerfield MR, Schonberg MA, Boyd CM, Burhenn PS, et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2018;36(22):2326–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandya C, Magnuson A, Flannery M, Zittel J, Duberstein P, Loh KP, et al. Association Between Symptom Burden and Physical Function in Older Patients with Cancer. Journal of the American Geriatrics Society. 2019;67(5):998–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lowenstein LM, Volk RJ, Street R, Flannery M, Magnuson A, Epstein R, et al. Communication about geriatric assessment domains in advanced cancer settings: “Missed opportunities”. Journal of geriatric oncology. 2019;10(1):68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riffin C, Van Ness PH, Wolff JL, Fried T. Family and Other Unpaid Caregivers and Older Adults with and without Dementia and Disability. Journal of the American Geriatrics Society. 2017;65(8):1821–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holroyd-Leduc J, Resin J, Ashley L, Barwich D, Elliott J, Huras P, et al. Giving voice to older adults living with frailty and their family caregivers: engagement of older adults living with frailty in research, health care decision making, and in health policy. Res Involv Engagem. 2016;2:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vick JB, Amjad H, Smith KC, Boyd CM, Gitlin LN, Roth DL, et al. “Let him speak:” a descriptive qualitative study of the roles and behaviors of family companions in primary care visits among older adults with cognitive impairment. Int J Geriatr Psychiatry. 2018;33(1):e103–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazer BL, Cameron RA, DeLuca JM, Mohile SG, Epstein RM. “Speaking-for” and “speaking-as”: pseudo-surrogacy in physician-patient-companion medical encounters about advanced cancer. Patient education and counseling. 2014;96(1):36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolff JL, Feder J, Schulz R. Supporting Family Caregivers of Older Americans. The New England journal of medicine. 2016;375(26):2513–5. [DOI] [PubMed] [Google Scholar]
- 14.Edwards M, Wood F, Davies M, Edwards A. ‘Distributed health literacy’: longitudinal qualitative analysis of the roles of health literacy mediators and social networks of people living with a long-term health condition. Health Expectations. 2015;18(5):1180–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agneessens F, Waege H, Lievens J. Diversity in social support by role relations: A typology. Social Networks. 2006;28(4):427–41. [Google Scholar]
- 16.Gallant MP, Spitze GD, Prohaska TR. Help or hindrance? How family and friends influence chronic illness self-management among older adults. Sage PublicationsSage CA: Los Angeles, CA; 2007. p. 375–409. [Google Scholar]
- 17.Seeman N. Web 2.0 and chronic illness: new horizons, new opportunities. Healthcare quarterly (Toronto, Ont). 2008;11(1):4, 104,–8, 10. [PubMed] [Google Scholar]
- 18.Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Soc Sci Med. 2015;125:116–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perry BL. Symptoms, stigma, or secondary social disruption: Three mechanisms of network dynamics in severe mental illness. Journal of Social and Personal Relationships. 2014;31(1):32–53. [Google Scholar]
- 20.Burke B, Martens A, Faucher E. Two decades of terror management theory: A meta-analysis of mortality salience research. Personal Soc Psychol Rev. 2020;4:155–95. [DOI] [PubMed] [Google Scholar]
- 21.Anderson K, Laxhman N, Priebe S. Can mental health interventions change social networks? A systematic review. BMC Psychiatry. 2015;15:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma R, Mann F, J W, al. e. The effectiveness of interventions for reducing subjective and objective social isolation among people with mental health problems: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2019: 10.1007/s00127-019-1800-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. American journal of Epidemiology. 1979;109(2):186–204. [DOI] [PubMed] [Google Scholar]
- 24.Smith KP, Christakis NA. Social Networks and Health. https://doiorg/101146/annurevsoc34040507134601. 2008. [Google Scholar]
- 25.Williams TA, Sheperd DA. Mixed method social network analysis: Combining inductive concept development, content analysis, and secondary data for quantitative analysis. Organizational Research Methods. 2017;20(2):268–98. [Google Scholar]
- 26.Yousefi-Nooraie R, Sale JE, Marin A, Ross LE. Social network analysis: An example of fusion between quantitative and qualitative methods. Journal of Mixed Methods Research. 2020;14:110–24. [Google Scholar]
- 27.Hollstein B, Töpfer T, Pfeffer J. Collecting egocentric network data with visual tools: A comparative study. Network Science. 2020:1–28. [Google Scholar]
- 28.Venturini T, Jacomy M, Jensen P. What Do We See When We Look at Networks. An Introduction to Visual Network Analysis and Force-Directed Layouts: SSRN; 2019. [Available from: 10.2139/ssrn.3378438.. [DOI]
- 29.Saldaña J The coding manual for qualitative researchers: Sage; 2016. [Google Scholar]
- 30.Oliveira M, Gama J. An overview of social network analysis. Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery. 2012;2(2):99–115. [Google Scholar]
- 31.Teddlie C, Tashakkori A. Foundations of mixed methods research: Integrating quantitative and qualitative approaches in the social and behavioral sciences: Sage; 2009. [Google Scholar]
- 32.Morris RL, Kennedy A, Sanders C. Evolving ‘self’‐management: exploring the role of social network typologies on individual long‐term condition management. Health Expectations. 2016;19(5):1044–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dhand A, Luke D, Lang C, Tsiaklides M, Feske S, Lee JM. Social networks and risk of delayed hospital arrival after acute stroke. Nat Commun. 2019;10(1):1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trevisan C, Rizzuto D, Maggi S, Sergi G, Wang HX, Fratiglioni L, et al. Impact of Social Network on the Risk and Consequences of Injurious Falls in Older Adults. Journal of the American Geriatrics Society. 2019;67(9):1851–8. [DOI] [PubMed] [Google Scholar]
- 35.Guida JL, Holt CL, Dallal CM, He X, Gold R, Liu H. Social Relationships and Functional Impairment in Aging Cancer Survivors: A Longitudinal Social Network Study. The Gerontologist. 2020;60(4):607–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nimmon L, Regehr G. The Complexity of Patients’ Health Communication Social Networks: A Broadening of Physician Communication. Teaching and Learning in Medicine 2018;30:352–66. [DOI] [PubMed] [Google Scholar]
- 37.Young J, Poole U, Mohamed F, Jian S, Williamson M, Ross J, et al. Exploring the value of social network “care maps” in the provision of long-term conditions care. Chronic Illness. 2019: 10.1177/1742395319836463. [DOI] [PubMed] [Google Scholar]
- 38.Epstein RM, Gramling RE. What is shared in shared decision making? Complex decisions when the evidence is unclear. Med Care Res Rev. 2013;70(1 Suppl):94S–112S. [DOI] [PubMed] [Google Scholar]


