Abstract
Purpose:
Postural tachycardia syndrome (POTS) and vasovagal syncope (VVS) are two disorders of orthostatic intolerance which are often misdiagnosed as the other. In each case, patients experience a reduced health-related quality of life (HRQoL) compared to healthy populations. This study was conducted to test the hypothesis that HRQoL is worse in POTS.
Methods:
POTS patients were recruited from the Dysautonomia International Annual Patient and Caregiver Conference. VVS patient data came from those enrolled in the Second Prevention of Syncope Trial. Participants ≥18 years (177 POTS and 72 VVS) completed the RAND 36-Item Health Survey, a generic and coherent health-related quality of life survey.
Results:
POTS patients reported reduced HRQoL compared to VVS patients in physical functioning (42.5±1.7 vs. 76.5±2.9, p<0.001), role limitations due to physical health (11.4±1.9 vs. 33.0±5.0, p<0.001), energy and fatigue (27.2±1.3 vs. 50.7±2.6, p<0.001), social functioning (45.2±1.8 vs 71.2±2.9, p<0.001), pain (48.8±1.9 vs. 67.7±2.9, p<0.001), and general health (31.2±1.5 vs. 60.5±2.6, p<0.001) domains. Scores did not differ significantly in the role limitations due to emotional health (p=0.052) and emotional well-being (p=0.271) domains. Physical and general health composite scores were lower in the POTS population, while mental health composite scores were not different.
Conclusion:
Differences in HRQoL exist between these patient populations. POTS patients report lower scores in physical and general health domains than VVS patients, but emotional health domains do not differ significantly. Targeting physical functioning in these patients may help improve quality of life.
Keywords: Vasovagal syncope, postural tachycardia syndrome, quality of life, physical function, emotional health
INTRODUCTION:
Postural Tachycardia Syndrome (POTS) and vasovagal syncope (VVS) are two common autonomic disorders which are recognized to have reduced health-related quality of life (HRQoL) compared to healthy populations.[1–3] However, the relative differences in HRQoL between POTS and VVS have not yet been evaluated.
POTS is defined by the presence of chronic, disabling symptoms of orthostatic intolerance in addition to a heart rate increase of at least 30 bpm within 10 minutes of standing, in the absence of a significant drop in blood pressure (≥20/10mmHg).[4] POTS is a heterogeneous disorder with varying levels of morbidity, often accompanied by symptoms of light-headedness, brain fog, and palpitations.[4] Additionally, POTS patients report high levels of daytime fatigue and difficulty sleeping, which have been found to contribute to the diminished quality of life seen in this population.[3]
Syncope is defined as a transient loss of consciousness and postural tone, with an abrupt and sudden onset, followed by a relatively rapid recovery.[5] Syncopal episodes are the result of cerebral hypoperfusion.[6] VVS, a form of reflex fainting, is the most common form of syncope in the general population.[7]
Studies have previously found that both POTS and VVS patients experience a reduced quality of life across many aspects of their lives.[1, 2] In both cases, the reduction in quality of life is comparable to that of chronic conditions such as rheumatoid arthritis and end-stage renal disease. [3, 8] The similarities in patient profiles between these disorders has resulted in the two disorders often being misdiagnosed.[9] However, based on our clinical experience, we hypothesized that HRQoL would be worse in POTS patients than in those with VVS. A better understanding of the relative impacts on HRQoL in these disorders may allow for a better understanding of these disorders, and inform treatment strategies optimized to the different patient populations.
METHODS:
Participants
All POTS patients in the study self-reported a physician diagnosis of POTS. Patients with POTS were recruited for participation in the conference research study at the Dysautonomia International Annual Patient and Caregiver Conference (2014 or 2016). These studies were approved by the Institutional Review Boards of Vanderbilt University (IRB#140671) and the University of Texas Southwestern Medical Center (IRB#042016). Each participant gave written informed consent. These studies enrolled both POTS patients and participants without POTS. However, this analysis included only participants with a physician diagnosis of POTS who were ≥18 years at the time of consent and provided answers for at least some of the HRQoL questions (see Figure 1). Participants completed questionnaires related to symptoms and medical history, as well as standardized tests of fatigue, symptom burden and HRQoL. Patients in the POTS group may have experienced one or more syncopal episodes; however, due to the nature of the survey design, we were unable to exclude POTS patients with co-morbid syncope. These data were collected using secure Research Electronic Data Capture (REDCap) database.[10] Twentyfour participants were in both the 2014 and 2016 cohorts. In order to avoid counting their data twice, their responses from the 2016 survey were excluded.
Fig. 1.
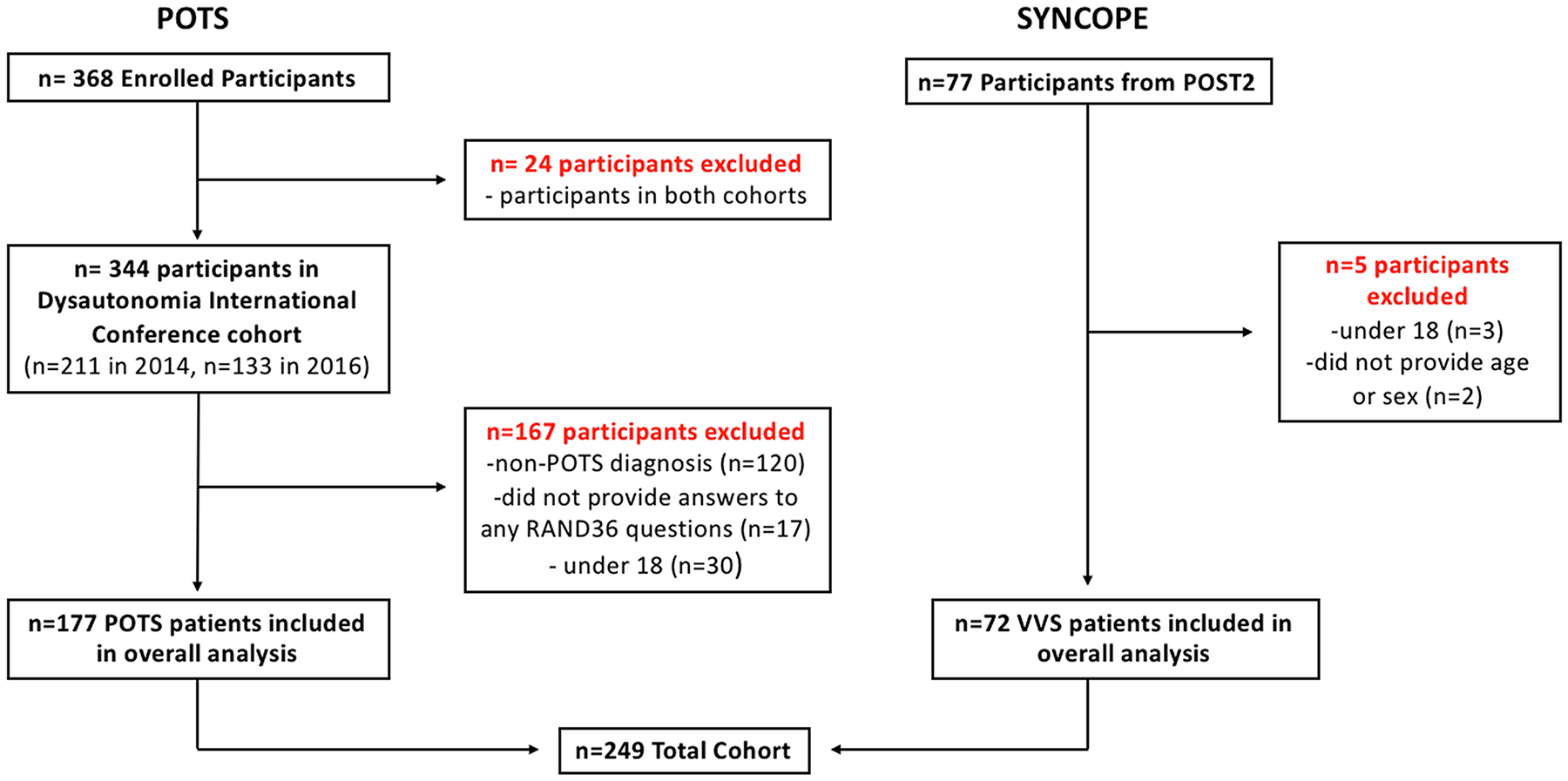
Flow diagram indicating inclusion and exclusion of participants. A total of 177 participants with Postural Tachycardia Syndrome (POTS), and 72 participants with vasovagal syncope (VVS) were included in this analysis.
VVS data for this study came from patients enrolled in the Second Prevention of Syncope Trial (POST2): a multicenter, longitudinal, randomized, placebo-controlled trial of fludrocortisone for VVS patients, which began in 2005 and concluded in 2010. [11, 12] These patients were recruited from syncope and arrhythmia clinics and were included in POST2 if they were 14 years or older, had a score ≥−2 on the Calgary Syncope Symptom Score, and had 3 or more lifetime syncopal episodes prior to enrollment. [11, 12] Patients were excluded from this study if they could not provide informed consent, had other causes of syncope, had other significant diseases, a permanent pacemaker, glaucoma, diabetes mellitus, hepatic or renal disease, a seizure disorder, hypertension, or had an opposition to fludrocortisone treatment for syncope. [11, 12] Importantly, patients were also excluded if, during a 5-minute stand test, they had postural tachycardia or orthostatic hypotension.[11, 12] Postural tachycardia was defined as a heart rate increase greater than 30 bpm, and orthostatic hypotension as a systolic blood pressure decrease greater than 20 mmHg. [11, 12] Of the patients who participated in POST2, we only included those who were 18 and over, had filled out the RAND36 survey, and provided sex. POST2 was approved by the Calgary Conjoint Health Research Ethics Board and the local ethics boards for each participating site. [11, 12] POST2 was registered with www.clinicaltrials.gov (NCT00118482).
Study Design
We chose to compare HRQoL in POTS and VVS patient populations since they are both disorders of orthostatic intolerance. All participants completed a number of surveys, including the RAND 36-Item Health Survey (RAND36). [13] This is a generic and easily-administered quality-of-life survey which assesses eight health-related domains: physical functioning, role limitations due to physical health, role limitations due to emotional health, social functioning, emotional well-being, energy and fatigue, pain, and general health. Each domain score ranges from 0–100, with higher scores representing greater levels of functioning and a preferable health-related quality of life. Scores from the eight domains were used to determine composite scores for general health, physical health and mental health.[13]
Missing Data
Participants with some missing answers were still included in the analysis of domains for which they had provided full answers. This was possible because each domain score is calculated from a subset of the 36 questions in the survey. As such, if someone left one question blank, seven out of eight of their domain scores would be unaffected. Importantly, no more than three participants scores were missing in each diagnosis, suggesting the effect of missing data was likely minimal on overall results. Participants who did not report sex were not included in the analyses.
Statistical Analysis
Demographic information and RAND36 scores are expressed as mean ± standard error of the mean (SEM). Demographic variables and RAND36 scores were assessed for normality using a Shapiro-Wilk test. Overall mean RAND36 scores, scores stratified by sex, and scores stratified by diagnosis were analyzed using a Mann-Whitney U test. The interaction between sex and diagnosis was determined using a two-factor ANOVA test. All p-values were two-tailed and the statistical significance was set at p<0.05. Statistical analyses were performed using IBM SPSS Statistics version 26 (IBM Corp., Armonk, N.Y., USA). Figures were made using GraphPad Prism version 8.42 (GraphPad Software, La Jolla, CA, USA).
RESULTS:
VVS vs POTS
In total, 177 POTS patients (12 male, 165 female) and 72 VVS patients (24 male, 48 female) were included in this analysis (Figure 1). VVS and POTS patients were similar in age (34.3±1.6 vs. 30.5±0.8 yr; p=0.09) and BMI (25.7±0.5 24.8±0.4 kg/m2; p=0.12). HRQoL was reduced in POTS compared to VVS patients in physical functioning (42.5±1.7 vs. 76.5±2.9, p<0.001), role limitations due to physical health (11.4±1.9 vs. 33.0±5.0, p<0.001), energy and fatigue (27.2±1.3 vs. 50.7±2.6, p<0.001), social functioning (45.2±1.8 vs 71.2±2.9, p<0.001), pain (48.8±1.9 vs. 67.7±2.9, p<0.001), and general health (31.2±1.5 vs. 60.5±2.6, p<0.001) domains. RAND36 scores did not differ significantly between the two groups in psychological/emotional domains: role limitations due to emotional health (p=0.052) and emotional well-being (p=0.271). These mean RAND36 scores are presented in Table 1. POTS patients also had significantly lower scores in two of the three composite dimensions: physical health (38.1±1.5 vs. 53.1±1.1, p<0.001), and general health (57.5±1.4 vs. 61.5±1.3, p=0.030). Of note, mental health composite scores were higher in POTS than in VVS patients (62.4±1.5 vs. 56.1±1.3, p=0.005).
Table 1.
RAND36 Scores for each patient population (overall)
| RAND36 DOMAIN | VVS Patients (n=72) | POTS Patients (n=177) | p |
|---|---|---|---|
| Physical Functioning | 76.5±2.9 | 42.5±1.7* | <0.001 |
| Role Limitations (Physical Health) | 33.0±5.0 | 11.4±1.9 | <0.001 |
| Role Limitations (Emotional Health) | 55.6±5.2 | 65.7±3.2* | 0.052 |
| Energy/Fatigue | 50.7±2.6 | 27.2±1.3 | <0.001 |
| Emotional Well-Being | 68.9±2.4** | 67.4±1.3* | 0.271 |
| Social Functioning | 71.2±2.9 | 45.2±1.8 | <0.001 |
| Pain | 67.7±2.9 | 48.8±1.9 | <0.001 |
| General Health | 60.5±2.6 | 31.2±1.5 | <0.001 |
| Composite Scores | |||
| Physical Health | 53.1±1.1 | 38.1±1.5* | <0.001 |
| Mental Health | 56.1±1.3** | 62.4±1.5*** | 0.005 |
| General Health | 61.5±1.3** | 57.5±1.4**** | 0.030 |
Data are presented as mean ± SEM. P Values are from Mann-Whitney U nonparametric tests.
n=176 respondents;
n=71 respondents;
n=175 respondents;
n=174 respondents
Sex Differences
Analysis of HRQoL based on sex, pooled across both diagnoses, revealed that males report higher HRQoL than females across a number of domains including physical functioning (66.9±5.4 vs. 49.9±1.8, p=0.003), social functioning (68.6±5.1 vs, 50.0±1.7, p<0.001), and general health (51.4±4.9 vs. 37.7±1.6, p=0.012) (Table 2). Similar to when HRQoL was compared between the two conditions, role limitations due to emotional health (61.1±7.5 vs 63.1±2.9, p=0.782) and emotional well-being (68.6±3.3 vs. 67.6±1.3, p=0.615) were the only domains where no significant differences found between all male and female participants, regardless of diagnosis. This translated into a difference only in the composite score for physical health, where male participants reported higher scores than female participants (48.8±2.7 vs 41.4±1.3; p=0.008).
Table 2.
RAND36 Scores by Sex (VVS and POTS patients pooled)
| RAND36 Domain | MALE (n=36) | FEMALE (n=213) | p |
|---|---|---|---|
| Physical Functioning | 66.9±5.4 | 49.9±1.8* | 0.003 |
| Role Limitations (Physical Health) | 36.8±7.5 | 14.4±2.0 | 0.006 |
| Role Limitations (Emotional Health) | 61.1±7.5 | 63.1±2.9* | 0.782 |
| Energy/Fatigue | 43.2±4.6 | 32.4±1.4 | 0.037 |
| Emotional Well-Being | 68.8±3.3 | 67.6±1.3** | 0.615 |
| Social Functioning | 68.8±5.1 | 50.0±1.7 | <0.001 |
| Pain | 68.7±4.3 | 51.9±1.8 | 0.002 |
| General Health | 51.4±4.9 | 37.7±1.6 | 0.012 |
Data are presented as mean ± SEM. P values are from Mann-Whitney U tests.
n=212
n=211
Mean RAND36 scores based on sex within each condition can be found in Table 3. When comparing HRQoL between male and female VVS patients, males reported higher HRQoL than females. Significant differences were observed in the RAND36 domain physical functioning (83.3±5.2 vs. 73.1±3.4, p=0.014), role limitations due to physical health (54.2±9.4 vs. 22.4±5.2, p=0.005), social functioning (83.3±4.7 vs. 65.1±3.3, p=0.002), and pain (76.0±4.9 vs. 63.6±3.6, p=0.040). There were also significant sex differences in all three composite scores in VVS patients: physical health (57.4±2.2 vs. 51.0±1.2, p=0.005), mental health (59.7±2.5 vs. 54.3±1.5, p=0.027), and general health (65.6±2.5 vs. 59.4±1.5, p=0.015).
Table 3.
RAND36 Scores by Diagnosis and Sex
| VVS | POTS | ||||||
|---|---|---|---|---|---|---|---|
| Male (n=24) | Female (n=48) | p | Male (n=12) | Female (n=165) | p | ||
| Physical Functioning | 83.3±5.2 | 73.1±3.4 | 0.014 | 34.2±4.6 | 43.1±1.8** | 0.224 | |
| Role Limitations (Physical Health) | 54.2±9.4 | 22.4±5.2 | 0.005 | 2.1±2.1 | 12.1±2.0 | 0.165 | |
| Role Limitations (Emotional Health) | 68.1±9.3 | 49.3±6.1 | 0.062 | 47.3±12.0 | 67.1±3.3** | 0.071 | |
| Energy/Fatigue | 56.3±4.7 | 47.9±3.1 | 0.147 | 17.1±4.5 | 27.9±1.4 | 0.024 | |
| Emotional Well-Being | 71.0±4.6 | 67.8±2.9* | 0.277 | 64.3±3.7 | 67.6±1.4** | 0.289 | |
| Social Functioning | 83.3±4.7 | 65.1±3.3 | 0.002 | 39.8±6.1 | 45.7±1.9 | 0.482 | |
| Pain | 76.0±4.9 | 63.6±3.6 | 0.040 | 54.0±7.1 | 48.4±2.0 | 0.594 | |
| General Health | 65.6±4.9 | 57.9±3.0 | 0.088 | 22.9±3.9 | 31.9±1.5 | 0.119 | |
Data are presented as mean ± SEM. P values are from Mann-Whitney U nonparametric tests.
n=47
n=164
The same comparison was made for males versus females diagnosed with POTS. In this population, male patients scored significantly lower than their female counterparts in some of the RAND36 domains: energy/fatigue (17.1±4.5 vs. 27.9±1.4, p=0.024), in addition to the mental health (53.3±3.5 vs. 63.0±1.6, p=0.038) and general health (48.7±2.7 vs. 58.1±1.5, p=0.036) composite scores. Physical functioning, role limitations due to emotional and physical health, emotional well-being, social functioning, pain, general health and the composite score for physical health were not significantly different between sexes in POTS. The eight RAND36 domain scores and composite scores within each diagnosis, split by sex, are found in Figure 2 for the VVS group, and Figure 3 for the POTS group.
Fig. 2.
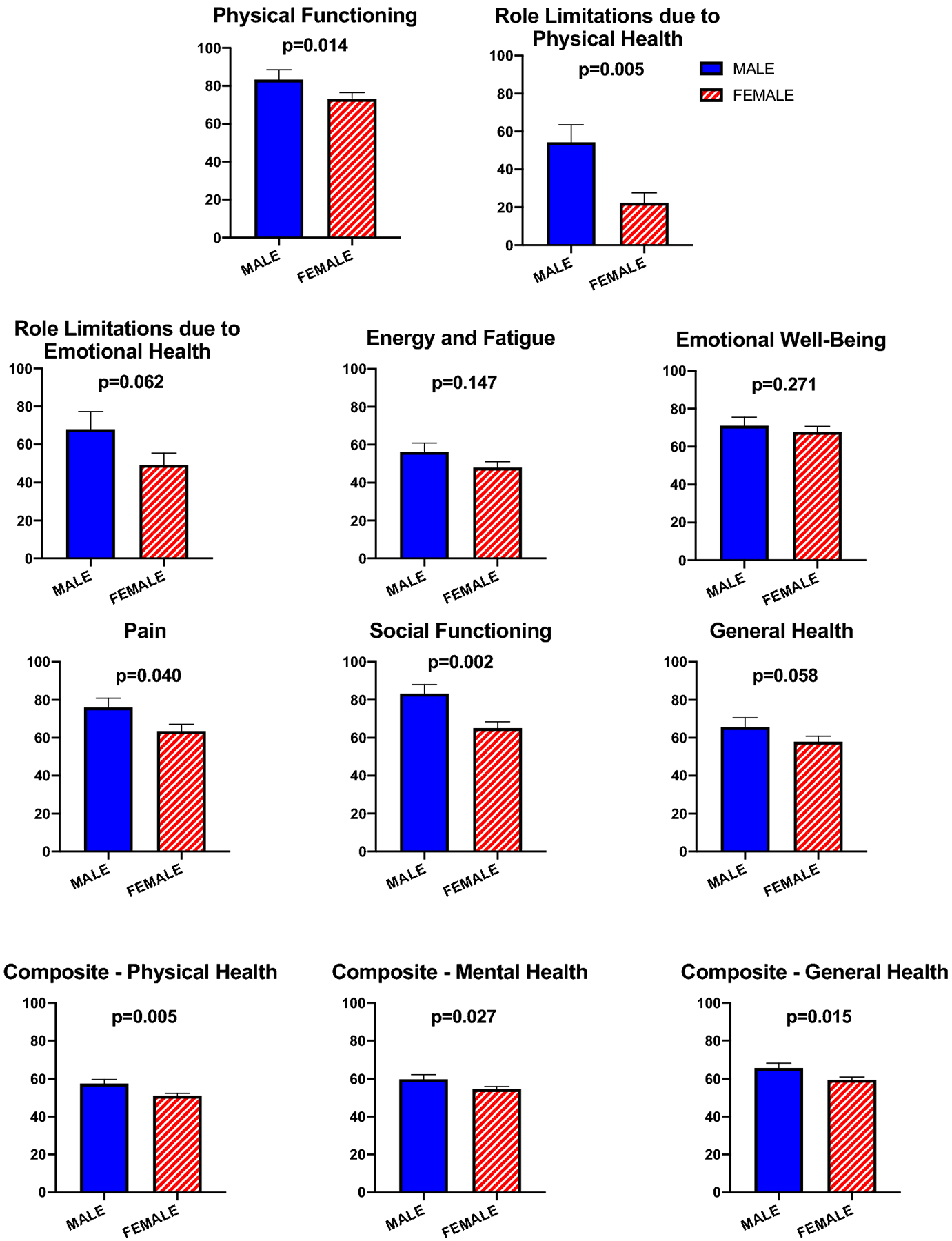
RAND36 health related quality of life (HRQoL) scores for the 8 RAND36 domains and 3 RAND36 composite scores, split by sex (male and female), among VVS patients. Data are plotted as mean ± SEM. Lower scores indicate a worse HRQoL. The P-value above each pair of bars is representative of the difference between sex within VVS. VVS: vasovagal syncope.
Fig. 3.
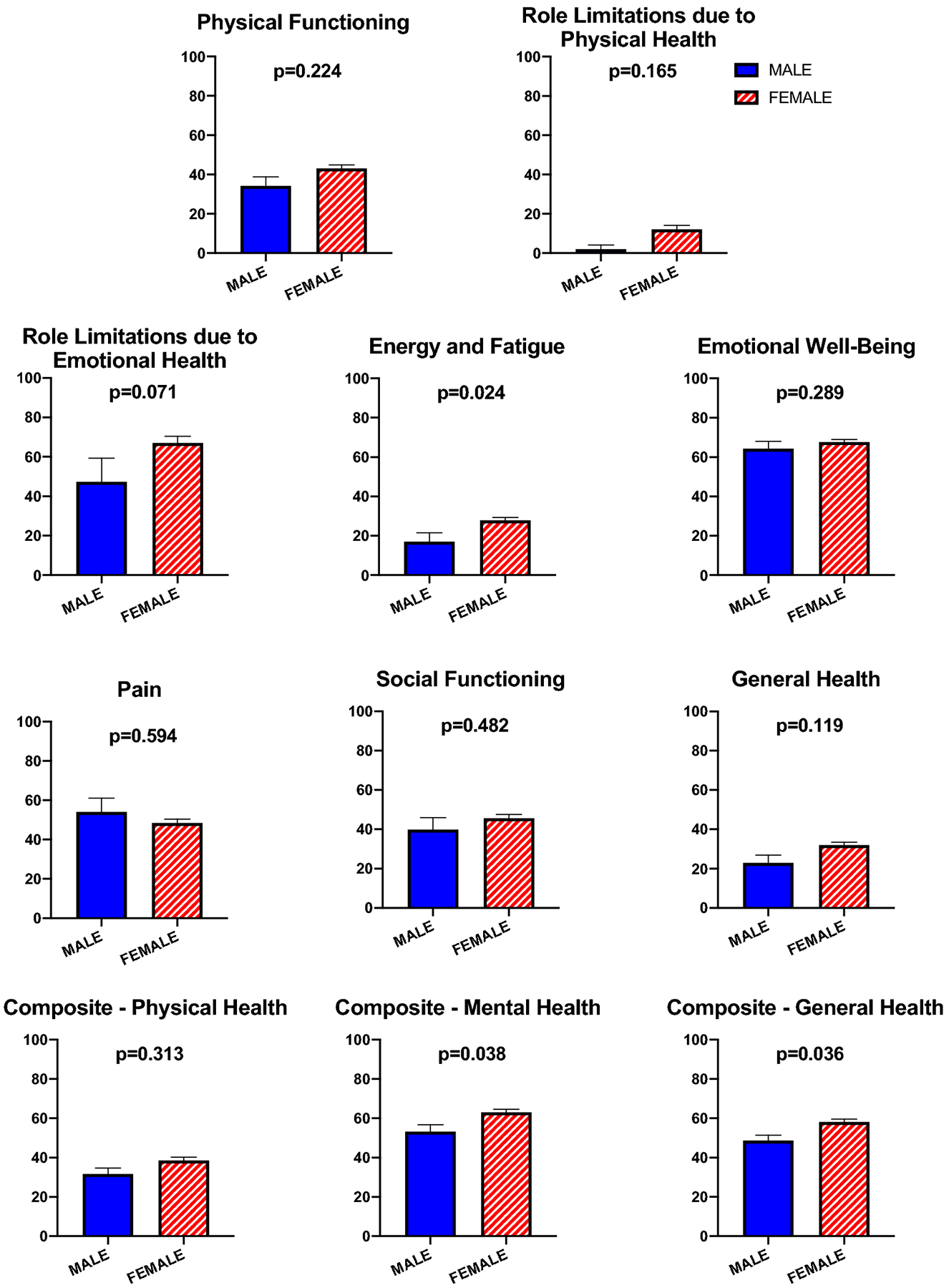
RAND36 health related quality of life (HRQoL) scores for the 8 RAND36 domains and 3 RAND36 composite scores, split by sex (male and female), among POTS patients. Data are plotted as mean ± SEM. Lower scores indicate a worse HRQoL. The P-value above each pair of bars is representative of the difference between sex within POTS. POTS: Postural Tachycardia Syndrome.
Interaction between Sex and Diagnosis on HRQoL
The effect of diagnosis, sex, and interaction between these two variables on HRQoL can be visualized in Figure 4. Of note, six of the eight domain scores are influenced by the interplay between these variables, as demonstrated by the ANOVA interaction (Pint.) term. Physical functioning (Pint. = 0.036), role limitations due to physical health (Pint. <0.001), role limitations due to emotional health (Pint. = 0.020), energy and fatigue (Pint. = 0.010), social functioning (Pint. = 0.010) and general health (Pint. = 0.035) were significant. The same can be said of the composite score in mental health (Pint. = 0.029) and general health (Pint. = 0.019), while the physical health composite score was not significantly different (Pint. = 0.058).
Fig. 4.
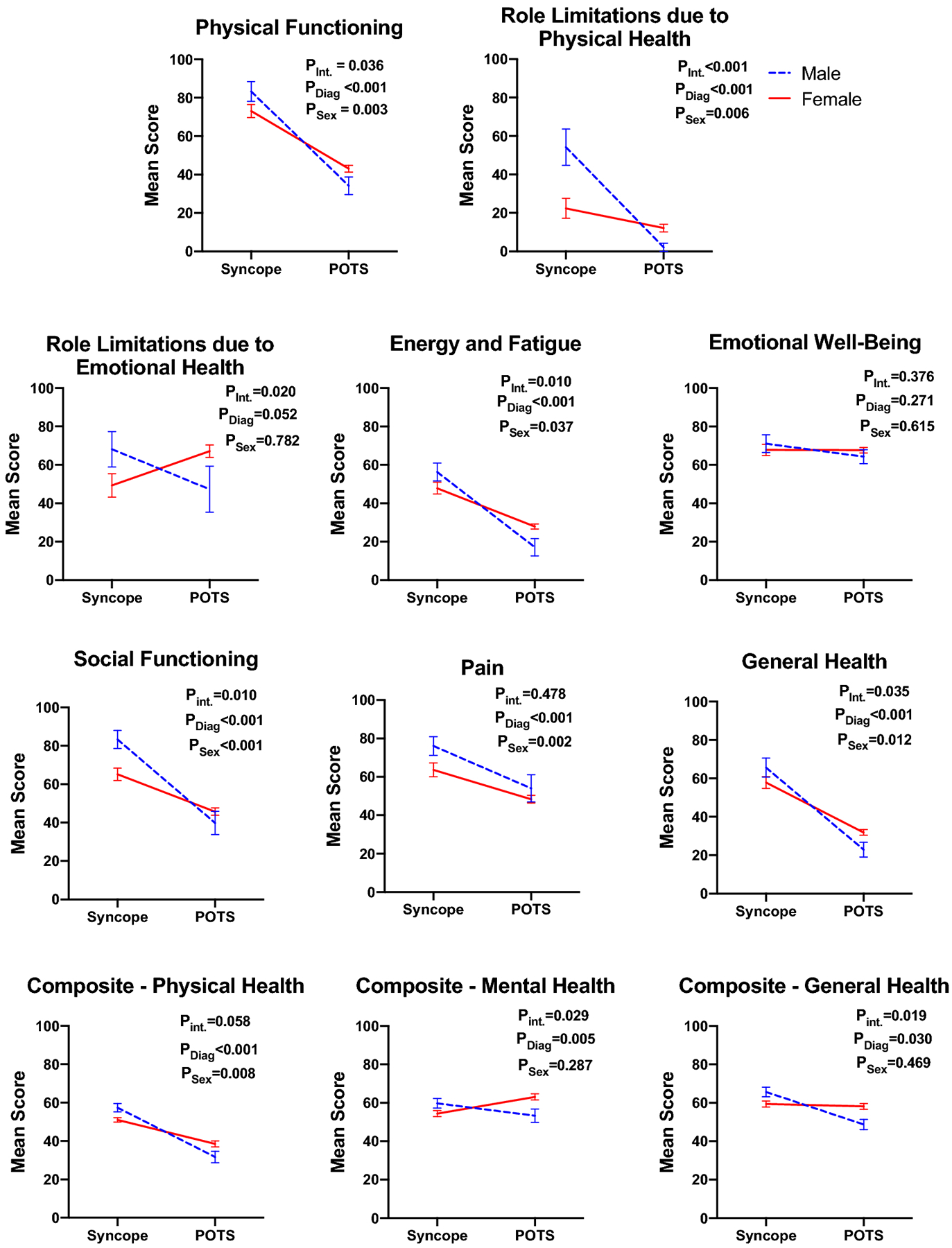
Interactions between Diagnosis (POTS and VVS) and Sex (male and female) on RAND36 Health Related Quality of Life scores. Diagnosis plotted against mean ± SEM RAND36 score. Plotted lines represent sex: the solid red line for female and the segmented blue line for male. Each diagnosis is distinct. Data were analyzed via two-factor ANOVA to examine main effects of POTS versus VVS diagnosis (PDiag) and male versus female regardless of diagnosis (Psex), and their interaction (Pint.). POTS: Postural Tachycardia Syndrome; VVS: vasovagal syncope.
DISCUSSION:
Overall, the findings from this study demonstrate that POTS patients have a reduced HRQoL compared to VVS patients. Although both conditions report significantly reduced scores across a number of HRQoL domains when compared to healthy individuals [2, 3], POTS patients experience significantly greater impairment across multiple HRQoL domains compared to VVS patients.
POTS patients as a whole had significantly lower scores in six of the eight health domains assessed by the RAND36, notably in the physical and general health dimensions. The finding that HRQoL in psychological domains is less affected among POTS patients is consistent with prior studies that have assessed HRQoL in POTS patients.[3, 14] POTS is a chronic multisystem disorder that is often diagnosed along with a number of comorbidities.[4] This can lead to a significant symptom burden that may contribute to the reduced physical quality of life.[15] These findings suggest that physiological factors, rather than psychological factors, may play a larger role in the diminished quality of life seen in POTS. Consistent with this finding, POTS patients are no more likely than the general population to be diagnosed with major depression or anxiety disorders.[14]
The same cannot be said of VVS patients. Previous studies have found that this patient population has reduced scores in all 8 domains of the RAND36 survey compared to healthy controls.[2] In addition, these patients experience greater psychological distress in the form of anxiety and depression.[2] Other studies have found that, unlike POTS, the prevalence of psychiatric disorders is higher among VVS patients than controls.[16]. That being said, in our study, the role limitations due to emotional health and emotional well-being domain scores did not differ significantly between POTS and VVS patients. This suggests that, compared to healthy populations, both of these conditions are met with some degree of reduced psychological HRQoL. However, POTS patients were significantly more impaired in other domains than in psychological domains, suggesting that psychological effects are less detrimental to HRQoL than physical ones.
When looking at sex differences in HRQoL within each diagnosis, a similar trend appeared among patients with VVS. In this population, female participants had significantly lower scores than did their male counterparts in five of the eight RAND36 domains, and all three composite scores. The scores that did not differ between the two were the psychological domains (role limitations due to emotional health, emotional well-being), in addition to energy/fatigue. Previous studies on sex differences in VVS are limited, but suggest that presentation and outcomes are different between male and female patients.[17] For example, female patients tend to experience their first syncopal episode younger than males, and are more likely to have recurrent syncope.[17] Additionally, these more frequent syncopal episodes are met with a greater symptom burden than in males.[17] Such factors may contribute to the diminished HRQoL in female patients with VVS compared to male patients.
There were fewer sex-based differences in HRQoL in the POTS population, with differences existing only in the energy/fatigue domain, the mental composite, and general health composite scores. In contrast to the finding among the VVS patients, the male POTS patients reported lower HRQoL than the female patients in these specific domains. That being said, over 90% of POTS patients are female.[4] This was reflected in our POTS patient sample, which was composed primarily of females. As such, a larger male sample may be needed to properly assess the negative impacts of POTS on HRQoL in the male patient population. However, it should be noted that, overall, a number of HRQoL scores were influenced by the interaction between sex and diagnosis. Thus, these data suggest that sex-differences exist in how each disorder affects patient quality of life.
Although previous studies have looked at the extent to which HRQoL is reduced in POTS and VVS patient populations, to our knowledge, this is the first study to compare the two conditions. Overall, we found that differences exist between these disorders, which may be relevant to the treatment methods used for each condition. Notably, physical health domains appear to be more significantly affected in the POTS population than in the VVS population. Moreover, sex-differences may exist in the extent to which HRQoL is reduced in POTS and VVS.
Clinical Implications:
In order to decrease the burden of disease associated with VVS and POTS, it is crucial that the differences in quality of life, both among and between these disorders, be recognized by clinicians and by patients. For example, targeting physical symptoms and limitations may be more relevant to the treatment of POTS than it is for the treatment of VVS. It is not clear if targeting the physical symptoms will also improve the mental health domains.
Study Limitations
A significant limitation of this study is that the quality of life data used for analysis were collected using self-reported measures, which are vulnerable to subjective interpretation. The reliability of these results, however, are supported by the use of a widely used and externally validated HRQoL tool.
The female-dominant sex distribution of our POTS patient population is representative of the true sex distribution of POTS patients.[15] This led to a smaller sample of male POTS patients, which could make those findings more unstable. This analysis should ideally be re-addressed in follow-up studies.
The POTS patient sample in this study may be influenced by sampling bias and may therefore not be representative of the general patient population. It is also important to consider that we did not control for potential effects of hemodynamic, psychiatric conditions, or pain medications in this population. These factors could have impacted symptoms and quality of life.
Finally, POTS diagnoses were based on patients self-reporting a physician diagnosis of POTS. This diagnosis was not confirmed with medical records.
Conclusions:
Differences in HRQoL between POTS and VVS patients exist primarily in the physical and general health domains, while mental health domains are reportedly similar between the two conditions. There are sex differences in the extent to which HRQoL is reduced in each condition. Decreasing symptom burden and addressing the psychological and physiological roles played in each condition may be a key step to improving overall HRQoL.
ACKNOWLEDGEMENTS:
The authors would like to express our gratitude to the patients who participated in these studies.
Funding:
This work was supported in part by research grants from Dysautonomia International (East Moriches, NY, USA), the National Center for Advancing Translational Sciences Award UL1 TR000445 (Bethesda, MD, USA), and the Canadian Institutes of Health Research (Ottawa, ON, Canada).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
ETHICAL OVERSIGHT:
These studies were approved by the Institutional Review Boards of Vanderbilt University (IRB#140671) and the University of Texas Southwestern Medical Center (IRB#042016). Each participant gave written informed consent.
Conflicts of Interest
JH – None
KB – None
RSS – Medical Advisory Board of Dysautonomia International and PoTS UK, both without financial compensation.
SV – Consultant for Sage Therapeutics, Roche, and Catalyst Pharmaceuticals. Research Support from Dysautonomia International, Grifols, Genentech, BioHaven Pharmaceuticals. President, American Autonomic Society, without compensation. Medical Advisory Board of Dysautonomia International, without financial compensation.
VR – None
JN - None
LO – None
ACA – Consultant for Vaccine Injury Compensation Program, Department of Health and Human Services.
MB – Served on an Advisory Board for Biohaven Pharmaceuticals
LP – Consultant for ACI Clinical Endpoint Adjudication
SP – None
SR- Consultant for Lundbeck NA Ltd. and Theravance Biopharma; Chair, Data Safety and monitoring Board for Arena Pharmaceuticals; Research Grants from Dysautonomia International; Past-President, American Autonomic Society, without compensation; Medical Advisory Board of Dysautonomia International and PoTS UK, both without financial compensation.
REFERENCES
- 1.Benrud-Larson LM, Dewar MS, Sandroni P, et al. (2002) Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 77:531–537. 10.4065/77.6.531 [DOI] [PubMed] [Google Scholar]
- 2.Ng J, Sheldon RS, Ritchie D, et al. (2019) Reduced quality of life and greater psychological distress in vasovagal syncope patients compared to healthy individuals. PACE - Pacing Clin Electrophysiol 42:180–188. 10.1111/pace.13559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bagai K, Song Y, Ling JF, et al. (2011) Sleep disturbances and diminished quality of life in postural tachycardia syndrome. J Clin Sleep Med 7:204–210. 10.5664/jcsm.28110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raj SR, Guzman JC, Harvey P, et al. (2020) Canadian Cardiovascular Society Position Statement on Postural Orthostatic Tachycardia Syndrome (POTS) and Related Disorders of Chronic Orthostatic Intolerance. Can J Cardiol 36:357–372. 10.1016/j.cjca.2019.12.024 [DOI] [PubMed] [Google Scholar]
- 5.Shen WK, Sheldon RS, Benditt DG, et al. (2017) 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: A report of the American college of cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society [DOI] [PubMed]
- 6.Freeman R, Wieling W, Axelrod FB, et al. (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21:69–72. 10.1007/s10286-011-0119-5 [DOI] [PubMed] [Google Scholar]
- 7.Colman N, Nahm K, Ganzeboom KS, et al. (2004) Epidemiology of reflex syncope. Clin Auton Res 14:i9–i17. 10.1007/s10286-004-1003-3 [DOI] [PubMed] [Google Scholar]
- 8.McCarthy K, Ward M, Romero Ortuño R, Kenny RA (2020) Syncope, Fear of Falling and Quality of Life Among Older Adults: Findings From the Irish Longitudinal Study on Aging (TILDA). Front Cardiovasc Med 7:. 10.3389/fcvm.2020.00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nwazue VC, Raj SR (2013) Confounders of vasovagal syncope: Postural tachycardia syndrome. Cardiol Clin 31:101–109. 10.1016/j.ccl.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, et al. (2009) Research electronic data capture (REDCap)-Ametadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheldon R, Raj SR, Rose MS, et al. (2016) Fludrocortisone for the Prevention of Vasovagal Syncope A Randomized, Placebo-Controlled Trial. J Am Coll Cardiol 68:1–9. 10.1016/j.jacc.2016.04.030 [DOI] [PubMed] [Google Scholar]
- 12.Raj SR, Rose S, Ritchie D, Sheldon RS (2006) The Second Prevention of Syncope Trial (POST II)-a randomized clinical trial of fludrocortisone for the prevention of neurally mediated syncope: Rationale and study design. Am Heart J 151:1186.e11–1186.e17. 10.1016/j.ahj.2006.03.013 [DOI] [PubMed] [Google Scholar]
- 13.Hays RD, Sherbourne CD, Mazel RM (1993) The rand 36-item health survey 1.0. Health Econ 2:217–227. 10.1002/hec.4730020305 [DOI] [PubMed] [Google Scholar]
- 14.Raj V, Haman KL, Raj SR, et al. (2009) Psychiatric profile and attention deficits in postural tachycardia syndrome. J Neurol Neurosurg Psychiatry 80:339–344. 10.1136/jnnp.2008.144360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw BH, Stiles LE, Bourne K, et al. (2019) The face of postural tachycardia syndrome – insights from a large cross-sectional online community-based survey. J Intern Med 286:438–448. 10.1111/joim.12895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giada F, Silvestri I, Rossillo A, et al. (2005) Psychiatric profile, quality of life and risk of syncopal recurrence in patients with tilt-induced vasovagal syncope. Europace 7:465–471. 10.1016/j.eupc.2005.05.008 [DOI] [PubMed] [Google Scholar]
- 17.Deveau AP, Sheldon R, Maxey C, et al. (2020) Sex Differences in Vasovagal Syncope: A Post Hoc Analysis of the Prevention of Syncope Trials (POST) I and II. Can J Cardiol 36:79–83. 10.1016/j.cjca.2019.10.008 [DOI] [PubMed] [Google Scholar]


