Abstract
Purpose:
To characterize clinician-scientists in ophthalmology and identify factors associated with successful research funding, income, and career satisfaction.
Design:
Cross-sectional study
Methods:
We conducted a survey of clinician-scientists in ophthalmology at U.S. academic institutions between April 17, 2019 and May 19, 2019. We collected information including 1) demographic data, 2) amount, type, and source of startup funding, first extramural grant, and first R01-equivalent independent grant, 3) starting and current salaries, and 4) Likert-scale measures of career satisfaction were analyzed using multivariate regression.
Results:
98 clinician-scientists in ophthalmology were surveyed across different ages (mean 48±11 years), research categories, institutional types, geographic regions, and academic ranks. Median startup funding was $50–99k, and median starting salary was $150–199k. Most investigators (67%) received their first extramural award from the National Eye Institute, mostly through K-award mechanisms (82%). The median time to receiving their first independent grant was 8 years, mostly through an R01 award (70%). Greater institutional startup support (P=0.027) and earlier extramural grant success (P=0.022) were associated with earlier independent funding. Male gender (P = 0.001) and MD degree (P=0.008) were associated with higher current salaries, but not starting salaries. Overall career satisfaction increased with career duration (P=0.011), but not with earlier independent funding (P=0.746) or higher income (P=0.300).
Conclusions:
Success in research funding by clinician-scientists in ophthalmology may be linked to institutional support and earlier acquisition of extramural grants, but does not impact academic salaries. Nevertheless, career satisfaction among clinician-scientists improves with time, which is not necessarily influenced by research or financial success.
Clinician-Scientist Table of Contents
Clinician-scientists in ophthalmology are valuable yet endangered professionals. Their success in research funding may be linked to institutional support and earlier acquisition of extramural grants, but independent grant success does not appear to impact academic salaries. Career satisfaction among clinician-scientists improves with time and is not necessarily influenced by research or financial success.
Introduction
Bridging the gap between bench and bedside, clinician-scientists form the cornerstone of biomedical research. As medical providers, they are intimately aware of the unmet clinical needs of patients. As researchers, they are empowered to tackle these needs by engaging in basic, translational, and clinical research. Yet, the pathway to becoming a successful clinician-scientist is arduous, often requiring prolonged periods of training and multiple academic degrees that result in greater debt accumulation from medical or other graduate education, reduced start-up packages compared to Ph.D. scientists1, as well as delayed entry into academic faculty positions. Many experts have commented on the shortage and endangerment of clinician-scientists2–4, especially those in ophthalmology.5–9 The ongoing COVID-19 pandemic are exacerbating these issues, with models predicting a research output decrease between 20 and 40%.10 In particular, scientists in earlier career stages, women, and underrepresented groups are most impacted, and the lasting consequences of this crisis have yet to be determined.11–12
Prior reports have also underscored the critical role of the National Institutes of Health (NIH) and National Eye Institute (NEI) in maintaining the viability of the clinician-scientist career path.13 Undergraduate medical training can be supplemented with biomedical research through NIH-supported research immersion programs such as the Medical Research Scholars Program, or through dual MD-PhD degree programs such as the Medical Scientist Training Program. After graduation, NIH K-award mechanisms support early career clinician-scientists with research and salary support under mentorship from more established investigators. However, among ophthalmologists who received K08 or K23 funding, only 48% of these individuals successfully secured an R01 grant,14–15 which is often considered an indicator of research funding success as an independent investigator. A recently published study showed that of ophthalmology or optometry clinician-scientists who obtain their first R01 grant, less than 4% will secure a second R01 (renewal of first R01 or new second R01) 5 years following initiation of funding of the first R01.16 Beyond extramural funding, institutional or departmental support, startup funding, and salary all contribute to job satisfaction. In this study, we conducted an anonymous survey of current clinician-scientists in ophthalmology to investigate factors that may be associated with research funding, income, and career satisfaction.
Methods
Survey Administration
A 38-item survey was developed using Qualtrics survey software (Qualtrics, Provo, UT) and digitally administered to clinician-scientists in ophthalmology between April 17 to May 19, 2019 (Supplemental Figure). Invitations for the survey were sent via electronic mail to a list of approximately 300 self-identified clinician-scientists compiled from an Association for Research in Vision and Ophthalmology (ARVO) annual meeting mailing list as well as clinician-scientists known by the authors to have obtained NIH funding through search of projectreporter.nih.gov. Questions were multiple-choice with the option for free-text responses. Because the survey did not collect personal identifiable information, multiple responses from single internet protocol (IP) addresses were blocked to ensure that each entry was unique. Entries without complete research funding, income, or satisfaction data were excluded from the analysis. Subjects who have not yet received an academic appointment were also excluded. E-mail reminders were sent to encourage participation, but no additional incentives were provided. This survey study was not considered to be human subject research and was exempted by the Institutional Review Board at the University of California, Davis. All study procedures adhered to the tenets set forth in the Declaration of Helsinki.
Survey Details
The survey collected demographic data including age and gender, as well as academic factors such as professional degree, primary research type (basic science, clinical science, or both), self-reported career stage (early, mid, or senior career), current academic rank (assistant, associate, or full professor), institution type (private or public), and U.S. geographic region (Northeast, Midwest, South, or West). We also requested the year of the most recent academic degree, terminal training position, and first academic appointment. Career duration was defined as years from first academic appointment to present. Research funding information included institutional startup funding amount, source and year of first extramural grant (any non-institutional support) and first independent (R01-equivalent) grant, years of continuous extramural funding, and alternative support during funding lapse if applicable. Income data included starting and current salary, and along with funding data were recorded in $50,000 category increments. The United States Bureau of Labor Statistics Consumer Price Index for all Urban Consumers (CPI-U) was used to calculate the annual rate of inflation to adjust institutional startup funding amount and starting salary. Career satisfaction was assessed using a series of 5-point Likert scale questions to address burnout, salary, research progress, clinical impact, work-life balance, grant support, university contribution, teaching, and overall satisfaction, which are summed to produce a composite satisfaction score with a maximum of 45 points. The survey is included in Supplemental Materials.
Statistical Analyses
Multivariate Cox semi-parametric regression and linear regression analyses with time adjustments were used to identify factors associated with time from first academic appointment to first independent grant, and duration of funding lapse. Multivariate regression analyses with time and inflation adjustments were used to evaluate factors associated with amount of startup research funding, starting salary, and current salary. Multivariate linear regressions were used to determine factors associated with composite career satisfaction score. Predetermined sets of factors were included as covariates in each multivariate regression model, with each analysis adjusting for all other covariates. Statistical analyses were performed using SPSS software version 27.0 (IBM Corp., Armonk, NY).
Results
Demographics & Academic Factors
Ninety-eight clinician-scientist respondents were included in the analysis (33% response rate). Median respondent age was 44 years (range: 31–78; Figure 1A), and consisted of more males than females (68% vs. 32%; Figure 1B). Most of the individuals held dual MD-PhD (52%) or MD (43%) degrees (Figure 1C), with a median time of 14 years since their last academic degree at the time of this survey. Most respondents identified as engaging in both clinical and basic science research (46%), followed by basic science (34%) and clinical research (20%) (Figure 1D), and were roughly evenly employed by public and private institutions (Figure 1E) that included slightly more individuals from Western states (Figure 1F). The median time since first academic appointment was 4 years for Assistant Professors, 8.5 years for Associate Professors, and 25 years for Full Professors, while a small subset of individuals held other academic positions such as “Instructor” (Figure 1G). Most respondents considered themselves to be in an early-career stage (46%) versus mid (29%) and senior career (25%), with median time since first academic appointment of 4 years for early-career, 12 years for mid-career, and 26 years for senior clinician-scientists (Figure 1H).
Fig 1.

Characteristics of 98 clinician-scientists in Ophthalmology. Charts showing (A) age distribution, (B) gender, (C) highest academic degrees, (D) research category, (E) institution type, and (F) regional distribution. (G-H) Bar-and-whisker plots comparing average time from first academic appointment of clinician-scientists by academic rank (G), and self-reported career stage (H).
Research Funding
Most surveyed clinician-scientists in our study reported <$50k of institutional startup funding, with a median of $50–99k, which is equivalent to $100–149k when adjusted for inflation (Figure 2A). Higher startup funding was given to males, but was not impacted by age, year of first appointment, degree, research type, institution type, or geographic location on multivariate regression (Supplemental Table).
Fig 2.
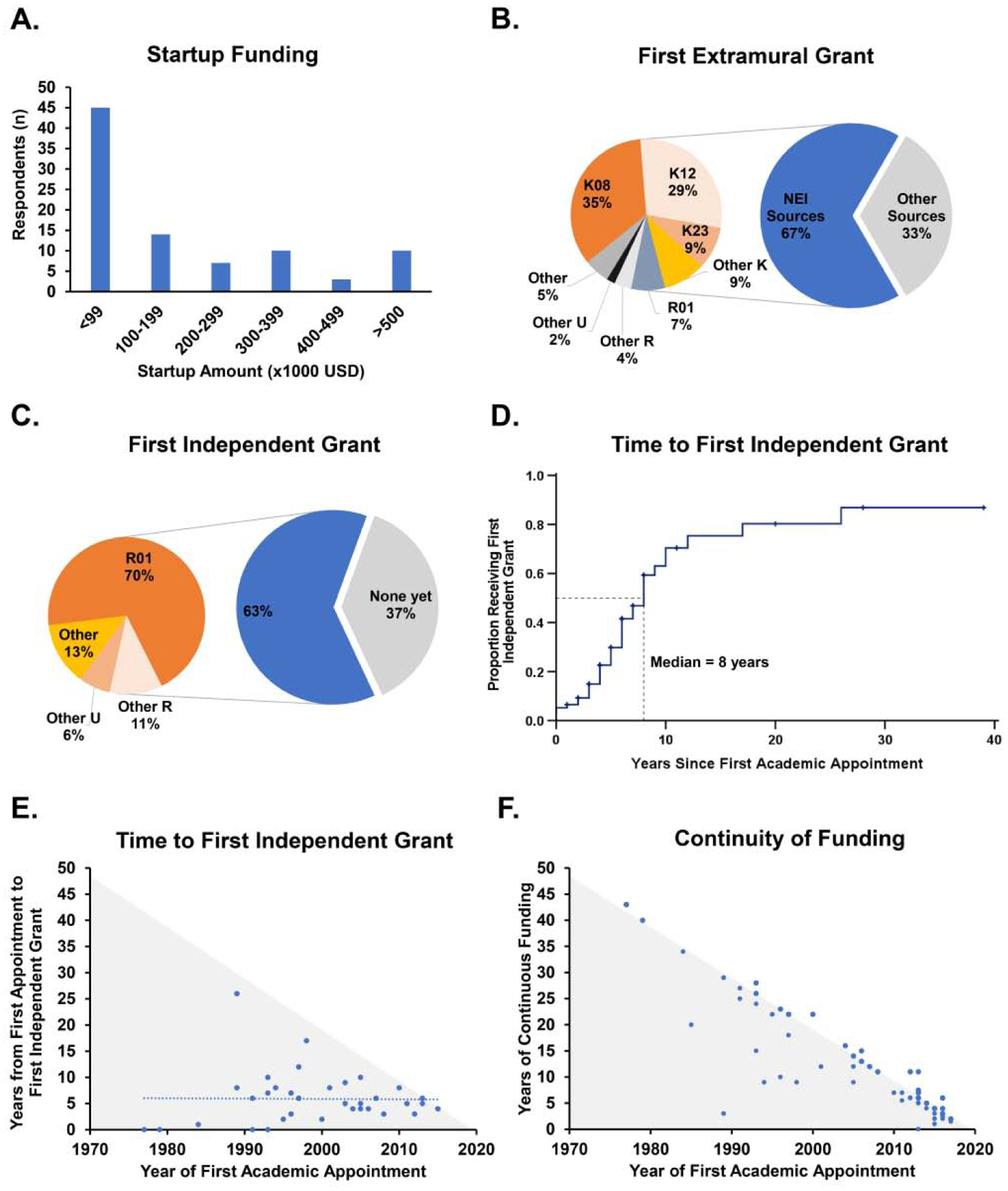
Research funding among clinician-scientists in Ophthalmology. (A) Bar graph showing distribution of institutional startup funding. (B-C) Charts showing distribution of first extramural (B) and R01-equivalent independent awards (C) and sources. (D) Kaplan-Meier survival analysis showing time to first independent grant. (E-F) Scatterplots showing time to first independent grant (E) and respondents with continuous funding (F) over the past 50 years. The gray-shaded area represents the maximum duration based on the year of first academic appointment.
Of the 84 respondents who received extramural funding, the majority (67%) received their first extramural grant from the NEI, with the most common mechanism being K08 (35%), followed by K12 (29%), K23 (9%), and other K-mechanisms such as K11 and KL2 (9%). Other funding sources included other NIH institutes (n = 3), the Department of Defense (n = 1), as well as various nonprofit foundations or commercial entities including Fight for Sight (n = 9), Research to Prevent Blindness (n = 3), Foundation Fighting Blindness (n = 3), Knights Templar (n = 2), International Retinal Research Foundation (n = 1), BrightFocus Foundation (n = 1), American Diabetes Association (n = 1), American Glaucoma Society (n = 1), Burroughs Wellcome Fund (n = 1), Lowry Medical Research Institute (n = 1), Bayer (n = 1), or other local medical foundation (n = 1) (Figure 2B).
Among the 50 of these individuals (63%) who received their first major independent grant (R01-equivalent) at the time of the survey, most were awarded by the NEI (80%), and consisted primarily of R01 (70%), followed by other R- (11%) or U- (6%) mechanisms (Figure 2C). Other independent grants (R01-equivalent) were awarded by the Department of Defense (n = 5), other NIH institutes (n = 2), Veterans Affairs (n = 1), or other unidentified sources (n = 2). Kaplan-Meier survival analysis showed that the median time from first academic appointment to first independent grant was 8 years (range: 0–26) among respondents (Figure 2D), which remained generally stable over the past 40 years, albeit with less variability in the past decade (Figure 2E). Earlier independent research funding was associated with earlier time to first extramural career award (Estimate = 0.842, P = 0.022) and inflation-adjusted startup funding amount (Estimate = 1.017, P = 0.027), while age and year of first appointment, gender, academic degree, research type, and first extramural grant source and type showed no significant association on multivariate analyses (Table 1).
Table 1.
Factors associated with research funding success, income, and career satisfaction.
| Time to Independent Grant | Current Salary | Career Satisfaction Composite Score | |||||
|---|---|---|---|---|---|---|---|
| Category or Increment | Hazard Ratio | P- Valuea | Estimate | P- Valueb | Estimate | P- Valueb | |
| 1 Year | .927 | .410 | −.909 | .185 | .185 | .185 | |
| 1 Year | 1.009 | .087 | .294 | .091 | .245 | .011* | |
| Male | Reference | - | Reference | - | Reference | - | |
| Female | .960 | .935 | -9.108 | .001* | −.372 | .788 | |
| MD | Reference | - | Reference | - | Reference | - | |
| MD/PhD | .515 | .156 | -8.540 | .008* | −.249 | .858 | |
| Professor | - | - | Reference | - | Reference | - | |
| Assistant Professor | - | - | −.689 | .872 | .146 | .949 | |
| Associate Professor | - | - | 4.096 | .345 | −.067 | .975 | |
| Other | - | - | −4.808 | .375 | 4.243 | .122 | |
| Clinical | Reference | - | Reference | - | Reference | - | |
| Basic Science | .747 | .607 | −6.811 | .082 | 2.712 | .110 | |
| Both | 1.074 | .874 | 1.758 | .562 | .426 | .745 | |
| $10,000 | 1.017 | .027* | - | - | - | - | |
| 1 Year | .842 | .022* | - | - | - | - | |
| K-Award | Reference | - | - | - | - | - | |
| Other | .589 | .283 | - | - | - | - | |
| 1 Year | - | - | 1.997 | .541 | .036 | .746 | |
| $10,000 | - | - | .059 | .596 | - | - | |
| Current Salary | $10,000 | - | - | - | - | .060 | .300 |
Multivariate Cox semi-parametric regression
Multivariate linear regression
Indicates statistical significance. Multivariate regression performed with all factors in models.
Most respondents (63%) reported sustained extramural research funding since their first academic appointment, although a notable portion (37%) indicated a lapse in funding with a median of 2 years (range 0.25–27; Figure 2F). Among the 29 clinician-scientists who reported funding lapses, 17 received departmental research funding, 10 received institutional funding, 9 obtained salary support, and 4 had personnel support (e.g. laboratory technician). Five researchers (17%) reported no ancillary support during their funding lapse. Those who received departmental or institutional support had shorter duration of funding lapse than those who did not (median 2 vs. 3 years), although this difference did not reach statistical significance (P = 0.746).
Income
The median starting salary for clinician-scientists was $150–199k, corresponding to $200–249k when adjusted for inflation, and appeared to increase slightly over the past 40 years (Figure 3A). A cross-sectional analysis of current salaries of respondents shows a linear rate of salary increase of approximately $43k per decade (Figure 3B). On multivariate analyses, both male gender and MD degree were independently associated with higher current salary, compared with their female and MD-PhD counterparts (Table 1, Fig 3C–3D). Other factors such as age, year of first appointment, academic rank, research type, time to first independent grant, and inflation-adjusted starting salary did not appear to be associated with clinician-scientist salaries in our surveyed cohort.
Fig 3.

Income of clinician-scientists in Ophthalmology. (A) Scatterplot showing change in inflation-adjusted starting salary over the past 40 years. (B) Scatterplot of the relationship between current salary and career duration. (C-E) Bar plots showing mean salaries based on academic rank (C), gender (D), and highest academic degree (E). Error bars represent standard error. *P<0.05, statistically significant.
Career Satisfaction
Career satisfaction was generally high among respondents, with a majority reporting a score of 5 (completely satisfied) or 4 (generally satisfied) across most categories, with the highest level of satisfaction seen in items related to burnout levels as well as impact of research and clinical work, followed by institutional contribution and teaching, while the lowest satisfaction was associated with work/life balance, grant support, and salary (Fig 4A). When asked if the individual would choose the clinician-scientist career path again, however, the response was very positive (Fig 4A). Multivariate regression analysis showed longer career duration (year of first appointment) was independently associated with greater composite career satisfaction score (Estimate 0.245, P = 0.011; Fig 4B). Other factors such as age, gender, degree, academic rank, research type, time to first independent grant, or current salary did not influence overall career satisfaction (Table 1). Additionally, actual current salary was not associated with satisfaction scores related to salary (OR 1.003, P = 0.410).
Fig 4.

Career satisfaction among clinician-scientists in Ophthalmology. (A) Bar plots showing distribution of scores based on a 5-point Likert scale survey to address clinical work impact, level of burnout, research impact, teaching, institutional contribution, salary, grant funding, and work/life balance. (B) Scatterplot of composite satisfaction score based on sum of Likert-scale scores from 9 survey questions on career satisfaction (maximum 45 points).
Discussion
In this study, we surveyed 98 self-declared clinician-scientists in academic ophthalmology to explore characteristics that affect starting salary and institutional startup funding, as well as factors that may contribute to research success (based on time to R01-equivalent independent funding), financial success (based on income), and career satisfaction. We found that greater institutional startup support and earlier attainment of extramural funding (any non-institutional awards) were associated with earlier acquisition of independent funding, while male gender and MD degree had higher salaries. Neither earlier research funding nor higher salary appeared to be associated with overall career satisfaction. Our study cohort spanned all career stages with similar proportions of assistant professors and full professors, basic and clinical researchers, and drew from diverse geographic regions across the United States. The median age was 44 years, with nearly half (46%) of respondents considering themselves in their early career, suggesting a selection bias toward more junior investigators, which may be due greater interest and relevance of the survey topic, more time to complete the survey, or greater proficiency with navigating the online survey among younger individuals. While there are no precise definition of “early”, “mid-career”, or “senior” investigators, the median time from first academic appointment for these three categories were 4, 12, and 26 years, respectively, with significant overlap in range.
Our study found that median inflation-adjusted startup funds for ophthalmic clinician-scientists was $100–149k, which are much lower than the average startup costs for newly-hired Assistant Professors in the biological sciences which ranged from $308,201 at public institutions to $403,071 at private institutions based on a survey on start-up costs and laboratory allocation rules at 222 U.S. academic institutions by the Cornell Higher Education Research Institute in 2002, even before adjustment for inflation.17 Another study, which analyzed newly-hired tenure-track assistant professors who received Burroughs Wellcome Trust Career Awards in Biomedical Sciences in 2004 found that median start-up package was $675,000 for Ph.D. scientists (n=21) and $480,000 for physician-scientists (n=11).1 This discrepancy may be based on the notion that clinician-scientists spend only part of their efforts conducting research, although it is arguable that these investigators require more institutional support given their clinical demands and time constraints. In fact, our study found that higher startup funds and earlier extramural award achievement were associated with earlier acquisition of an R01-equivalent independent award, suggesting that efforts should be made by institutional leadership to bolster support of clinician-scientists in the earliest, most vulnerable time of their careers.
Prior reports have been published describing the important role of the NIH and NEI in supporting the development of clinician-scientists, and our study confirmed that a majority of clinician-scientists received their first extramural grant from the NEI through K-award mechanisms (68%), and their first independent award from the NEI mostly in the form of an R01 (70%). Interestingly, our survival analysis found that the median time to receiving this first independent grant was 8 years, consistent with a prior study of K awardees where their mean time to an R01 was 2.8 years after completing their K grant, which are between 2–7 years in duration.15 This finding emphasizes the importance of “bridge funding” to support clinician-scientists who are very likely to experience a gap in funding during this period. The same prior report found that only 48% of clinician-scientists in ophthalmology who had received K awards were able to successfully secure R01 funding,15 which comports with a recent NIH-wide data release reporting that 42% of K-awardees later served as PI on an R01 equivalent award.18 These values are lower than the 63% R01 achievement rate among our surveyed cohort, but may be due to a selection bias in our study for clinician-scientists who may have been more successful at securing research funding. Our survey found that 37% of respondents experienced a funding lapse with a median duration of 2 years, during which time most investigators (83%) received some institutional or department support in the form of research funding, salary support, or personnel cost-sharing. We noted that those who received support during their funding lapse achieved independent funding earlier, although this did not reach statistical significance due to the small size of this cohort. Interestingly, only 62.8% of ophthalmology and optometry clinician-scientists who obtained their first R01 successfully obtained a second R01, and only 3.9% attained the second R01 within 5 years.16 Together, our results emphasize the vulnerability of clinician-scientists in obtaining initial and sustained independent research support in today’s competitive funding environment, and the important role of departments and institutions in supporting these researchers during their career.
Overall, the salaries of the clinician-scientists in our study were similar to the median salaries of academic faculty in ophthalmology as reported by the American Association of Medical Colleges (AAMC).19 The assistant, associate, and full professors we surveyed reported median salaries (male/female) of $275/275k, $425/325k, and $425/275k, respectively, as compared to AAMC median salaries of $288/242k, $357/283k, and $375/326k.19 Interestingly, clinician-scientists who have dual MD-PhD degrees earned lower income than their MD counterparts, even after adjusting for age, career duration, academic rank, and research type (basic vs. clinical research). While our study did not adjust for subspecialty, work hours, operating time, or clinical efforts, we hypothesize that MDs are more likely to maintain a larger portion of clinical efforts or perform more surgeries, which could account for the higher salaries. We also found that male gender was independently associated with higher startup funding and current salary, despite no difference in academic or research performance such as time to independent funding. This gender disparity reflects earlier studies showing similar gender differences in salaries of NIH K-awardees20, and size of NIH awards to primary investigators in ophthalmology departments.21 A recent study of academic pediatric ophthalmologists showed despite similar proportions of men and women across all academic ranks, women had a lower median h-index and lower NIH grant funding, which could be attributed to a shorter career duration in that subspecialty.22 Some progress has been made to improve female representation on editorial boards in ophthalmology, for example, but greater efforts are needed to achieve gender parity in both research funding and salaries in academic medicine.23
Our cohort of clinician-scientists expressed overall satisfaction with their career, with most expressing the greatest degree of satisfaction with the impact of their clinical work, research, and teaching, and less with salary, funding, and work/life balance. Interestingly, the degree of satisfaction did not appear to be associated with research performance (earlier independent funding) or financial success (current salary). The only factor associated with greater career satisfaction appeared to be the duration of their clinician-scientist career, although this is likely attributable to the selection bias of this voluntary survey, as those who were dissatisfied with their careers may no longer be pursuing the clinician-scientist career track. Other likely biases include the large proportion of younger respondents and possible under-representation of K-awardees who have yet to receive their first R01-equivalent grant. Key limitations of our study include the lack of confounders such as cost of living, clinical subspecialty, operating time, and research productivity as well as the inherent shortcomings associated with a voluntary survey and modest sample size. The survey anonymity also limited our ability to re-identify respondents to request additional information. Further research is needed to assess interventions such as bridge funding or increased startup packages and their effects on R01 success, income, and career satisfaction. Despite the issues our data raised surrounding the clinician-scientist pipeline, our survey respondents showed a steady improvement in job satisfaction over their career timeline, providing some optimism for young investigators who may seek to embark on the path of a clinician-scientist in ophthalmology.
Supplementary Material
Acknowledgements
A). Funding/Support:
None. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
B). Financial Disclosures:
A.M.R.: No financial disclosures.
N.J.P.: No financial disclosures.
R.C.R.: Research support: A. Alfred Taubman Medical Research Institute (Leslie and Abigail Wexner Emerging Scholar Award), Research to Prevent Blindness (Unrestricted Departmental Grant), The Leonard G. Miller Professorship and Ophthalmic Research Fund at the Kellogg Eye Center, Marek and Maria Spatz Endowment, Grossman, Greenspon, Dunn, Avers, Boustikakis, Sweiden and Terauchi Research Funds, and Beatrice & Reymont Paul Foundation all outside of the submitted work.
D.L.C.: Employee: Janssen Research and Development, Equity: Visgenx, DTx Pharma, and RecensMedical all outside of the submitted work.
G.C.Y.: Grants and personal fees: Alimera, Allergan, Carl Zeiss Meditec, Genentech, Intergalactic Therapeutics, Iridex, Regeneron, Topcon, and Verily all outside of the submitted work.
Biography

Alexander Rusakevich was selected as a 2020 J. William Kohl Scholar at the University of California, Davis, Department of Ophthalmology and Vision Sciences, where he assisted with studies investigating imaging of retinal vascular diseases. He has presented research internationally at large-scale ophthalmology meetings and co-authored multiple peer-reviewed publications. Alexander is currently a second-year medical student at Touro University-California and plans to pursue a career in ophthalmology.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental Material available at AJO.com.
References
- 1.Franko M, Ionescu-Pioggia M. Making the right moves: a practical guide to scientific management for postdocs and new faculty. Burroughs Wellcome Fund; 2006. [Google Scholar]
- 2.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;23:1254–9. [DOI] [PubMed] [Google Scholar]
- 3.Schafer AI, editor. The vanishing physician-scientist? Ithaca, New York: Cornell University Press; 2009. [Google Scholar]
- 4.Ley TJ, Rosenberg LE. The physician scientist career pipeline in 2005. JAMA. 2005;294:1343–51. [DOI] [PubMed] [Google Scholar]
- 5.Ambati BK, Cahoon J. Rejuvenating clinician-scientist training. Invest Ophthalmol Vis Sci. 2014;55(3):1853–1855. [DOI] [PubMed] [Google Scholar]
- 6.Culican SM, Rupp JD, Margolis TP. Retaining clinician-scientists: nature versus nurture. Invest Ophthalmol Vis Sci. 2014;55(5):3219–3222. [DOI] [PubMed] [Google Scholar]
- 7.Dana R, Miller JW. On the edge: the clinician-scientist in ophthalmology. JAMA Ophthalmol. 2013;131(11):1401–1402. [DOI] [PubMed] [Google Scholar]
- 8.Weinreb RN, Goldberg JL. Clinician-scientists in ophthalmology revisited. Ophthalmology. 2013;120(10):1949–1950. [DOI] [PubMed] [Google Scholar]
- 9.Van Gelder RN. The Clinician-Scientist in Vision Science: A Rare and Endangered Species. Trans Vis Sci Tech. 2020;9(12):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Council on Governmental Relations, August 2020. Research Impact under COVID-19: Financial Crisis and the “Pandemic Normal”.
- 11.Gewin V The career cost of COVID-19 to female researchers, and how science should respond. Nature. 2020. July;583(7818):867–869. [DOI] [PubMed] [Google Scholar]
- 12.Woolston C ‘It’s like we’re going back 30 years’: how the coronavirus is gutting diversity in science. Nature. 2020. July 31. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Gottesman MM. The role of the NIH in nurturing clinician-scientists. N Engl J Med. 2013. June 13;368(24):2249–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chao DL, Schiffman JC, Gedde SJ. Characterization of a clinician-scientist cohort in ophthalmology: a demographic analysis of K grant awardees in ophthalmology. Ophthalmology. 2013;120(10):2146–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Protopsaltis NJ, Chen AJ, Hwang V, Gedde SJ, Chao DL. Success in Attaining Independent Funding Among National Institutes of Health K Grant Awardees in Ophthalmology: An Extended Follow-up. JAMA Ophthalmol. 2018;136(12):1335–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu EA, Wang SY, Rao RC. Sustaining independent careers in vision research: demographics and success in second R01 attainment among clinician-scientists from 1985 to 2019. Trans Vis Sci Tech. 2020; 9(12): 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed Science Group Academic Sourcebook, November 2005; Cornell Higher Education Research Institute, Survey of Startup Costs and Laboratory Space Allocation Rules.
- 18.Lauer MS. NIH R01 Grant Outcomes of T32 Postdoctoral Participants: Associations with Demographics, Cohort, Degree, and Career Development (K) Awards. Available at https://nexus.od.nih.gov/. Accessed February 23, 2021.
- 19.Association of American Medical Colleges, April 2019. Report on Medical School Faculty Salaries. Washington DC: Association of American Medical Colleges. [Google Scholar]
- 20.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in salary in a recent cohort of early-career physician-researchers. Acad Med. 2013. November;88(11):1689–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Svider PF, D’Aguillo CM, White PE, Pashkova AA, Bhagat N, Langer PD, Eloy JA. Gender differences in successful National Institutes of Health funding in ophthalmology. J Surg Educ. 2014. Sep-Oct;71(5):680–8. [DOI] [PubMed] [Google Scholar]
- 22.Camacci ML, Ikpoh B, Lehman EB, Bowie E, Scott IU, Pantanelli SM, Ely A. Gender disparities among United States academic pediatric ophthalmologists: an analysis of publication productivity, academic rank, and NIH funding. J AAPOS. 2020. October 10:S1091–8531(20)30211–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bressler NM. JAMA Ophthalmology-The Year in Review, 2019: Striving for Sex Parity in Leadership and Excellence in Publications. JAMA Ophthalmol. 2020. May 1;138(5):437–438. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


