Abstract
Eveningness, a preference for later sleep and rise times, has been associated with a number of negative outcomes in terms of both physical and mental health. A large body of evidence links eveningness to Major Depressive Disorder (MDD). However, to date, evidence quantifying this association is limited. The current meta-analysis included 43 effect sizes from a total 27,996 participants. Using a random-effects model it was demonstrated that eveningness is associated with a small effect size (Fisher’s Z = − 2.4, 95% CI [− 0.27. − 0.21], p < 0.001). Substantial heterogeneity between studies was observed, with meta-regression analyses demonstrating a significant effect of mean age on the association between diurnal preference and depression. There was also evidence of potential publication bias as assessed by visual inspection of funnel plots and Egger’s test. The association between diurnal preference and depression is small in magnitude and heterogenous. A better understanding of the mechanistic underpinnings linking diurnal preference to depression and suitably powered prospective studies that allow causal inference are required.
Subject terms: Risk factors, Depression
Introduction
Circadian rhythms are endogenous processes that follow a near 24-h cycle. These rhythms are self-autonomous, and in humans are controlled by a central oscillator (or master clock) located in the suprachiasmatic nuclei (SCN) of the hypothalamus1. Individuals maintained under constant conditions isolated from external timing cues can maintain an endogenous period close to 24 h. However, because these cycles oscillate with periods that differ slightly from 24 h there is a loss of synchrony with the earth’s day-night cycle. To account for this, the central oscillator is adaptable and can be entrained to respond to external time-givers, or zeitgebers (e.g., light). The molecular mechanisms underlying the generation of circadian oscillations relies on multiple proteins generated by clock-related genes that interact to inhibit and activate gene expression in an inhibitory loop that oscillates to produce the near-24-h cycle.
Disruption of circadian rhythms are widely reported in depression. Patients may display a regular daily pattern of symptoms with increased symptom severity often reported in the morning2. In MDD there are dampened and phase-shifted rhythms of activity, temperature and hormones (with the exception of cortisol which is increased rather than reduced)3 which are correlated with depressive symptom severity4. Disrupting circadian rhythms through shift-work, long-distance travel (jet-lag) or misalignment between internal (biological) and social (external) time (referred to as social jet-lag) has been observed to increase depressive symptoms5–7. Poor entrainment of the SCN to light (as may occur in Major Depressive Disorder with Seasonal Pattern) and the subsequent disruptions of daily rhythms of hormones and neurotransmitters has been reported as an additional factor to develop depression8. In addition, treatments that target circadian rhythms (e.g. agomelatine, early morning bright-light therapy) may be effective in reducing depressive symptoms9.
Diurnal preference, or morningness/eveningness, reflects an individual’s preferred timings for sleep and activity and is an individual trait that arises through a combination of endogenous factors and external, environmental stimuli10. Evening-types (colloquially referred to as “night owls”) prefer to go to bed late, rise late and plan work and other activities (e.g., meetings, gym visits) for later in the day. By contrast, morning-types (“larks”) prefer to retire early, rise early and plan activities for earlier in the day.
Diurnal preference can be reliably estimated using subjective assessment, which has particular utility for large scale studies. A number of instruments have been developed to measure eveningness and among the most widely used are the Morningness–Eveningness Questionnaire (MEQ)11, the reduced version of the MEQ12 and the Composite Scale of Morningness (CSM)13. All three measures have been shown to have moderate to good reliability and construct validity14 and the MEQ has also been demonstrated to be a strong predictor of dim melatonin onset—which is considered the most reliable measure of circadian rhythm in humans15.
Twin studies indicate heritability estimates between 46 and 57% for diurnal preference16 and diurnal preference is considered a relatively stable trait in adulthood17. A better understanding of individual differences in sleep–wake behaviour and how these may relate to disease is becoming increasingly important as a large body of work now suggests that eveningness is associated with a number of negative physical18 and mental health outcomes19,20 particularly depression21,22. Current evidence suggests that eveningness is associated with greater depressive symptomatology7,22,23. Eveningness is also associated with having a current diagnosis of depression, treatment for depression or antidepressant use22,24,25, non-remission26 and suicidal thoughts27.
Despite the prevalence and debilitating nature of depression and the overwhelming body of evidence indicating an association between depression and diurnal preference8–17 synthesis of these data has been largely restricted to systematic reviews (e.g.19,20,28,29). To date, only one study has quantified this relationship in the form of a meta-analysis30. The aim of the current study was to extend this previous meta-analysis30 (which was limited to data published up to February 2016) to include recent literature published up to 31st December 2020. Based on previous work it is hypothesised that eveningness will be associated with greater depressive symptomatology.
Methods
The protocol for this meta-analysis was prospectively registered with PROSPERO (CRD4202122977). The raw data and fully reproducible code are available on the OSF (https://osf.io/wyjtx/).
Literature search
PubMed and Web of Science were searched for articles published between 1st January 2000 and 31st December 2020 using the search terms ("chronotype" OR "diurnal preference" OR "circadian preference" OR "morningness" OR "eveningness" OR "social jetlag") AND ("depression" OR "MDD" OR "Unipolar"). The titles and abstracts of articles returned using this search were initially screened before the full text was examined in greater detail.
To be included in the meta-analysis articles were required to meet the following criteria: (1) Diurnal preference quantified using either the Morning-Evening Questionnaire11 the Reduced Morningness–Eveningness Questionnaire12 or the Composite Scale of Morningness13; (2) Depressive symptomatology measured using either the Beck Depression Inventory (BDI)31, the Hospital Anxiety and Depression Scale (HADS)32, the Hamilton Rating Scale for Depression (HRSD)33, the Depression, Anxiety, Stress Scales (DASS)34, the Quick Inventory of Depressive Symptomatology–Self-report (QUIDS-SR)35, the Centre for Epidemiology Studies Depression (CES-D)36, the Self-Rating Depression Scale (SDS)37, the Montgomery-Asberg Depression Rating Scale–Self (MADRS-S)38, the Patient Health Questionnaire 9 (PHQ-9)39, the Patient Health Questionnaire 4 (PHQ-4)40, the Brief Symptom Rating Scale (BSRS)41, the Geriatric Depression Scale (GDS)42 and the Depressed Mood Scale (DMS)43; (3) Sufficient statistical information to estimate an effect size (correlation coefficient, mean and standard deviation or standard error, odds ratio); (4) Written in English; (5) Participants aged 18 or over; (6) For clinical samples, patients diagnosed with MDD; and (5) Published in a peer-reviewed journal. Exclusion criteria were: (1) Studies that included depressive disorders other than MDD (e.g., Seasonal Affective Disorder); and (2) Incomplete or modified versions of the MEQ/rMEQ/CSM (e.g. diurnal preference determined using a single question). Data selection is summarised in Fig. S1, Supplemental Data.
Study quality was evaluated using the McMaster critical review tool for quantitative studies44. Data extracted from the included studies was: (1) Authorship; (2) Year of publication; (3) Sample size; (4) Mean age; (5) Age range; (6) Measure of diurnal preference (e.g., MEQ); (7) Depression measure (e.g. BDI); (8) Gender breakdown (e.g. percentage of female participants); and (9) Clinical or non-clinical samples.
Statistical analyses
All statistical analyses were performed using R version 3.6.145 including the following packages: esc; effectsize; meta; metafor; dmetar: DiagrammeR; DiagrammeRsvg; and ggplot2. Individual effect sizes were obtained from each study. As most studies (52%) reported correlation coefficients, Fisher’s Z transformed correlation coefficient was used as the summary effect size. Odds ratios and standardised mean differences were transformed to Fisher’s Z scores for inclusion in the analysis. The corresponding pooled effect size and its 95% confidence intervals (CI) were calculated from a random-effects model with a Sidik–Jonkman estimator for τ2 with Hartung–Knapp adjustment. This method was adopted as a conservative approach in the presence of sample heterogeneity46. A pooled effect size of 0.1–0.3 was considered small, 0.3–0.5 medium and 0.5–1 considered a large effect47,48. Study heterogeneity was assessed with Q statistics and the I2 index. Outlier analysis (studies were considered outliers if the 95% CI was outside the pooled effect size 95% CI) were also performed and the random-effects model refitted after excluding any such study. To assess the potential impact of publication bias, funnel plots were visually inspected, and an Egger’s test conducted to quantify asymmetry with a p value of < 0.05 considered evidence of asymmetry that may reflect publication bias. Based on the outcome of the Egger’s test, a trim and fill procedure was conducted to impute potential missing studies into the funnel plot to achieve symmetry. Categorial moderators (clinical vs. non-clinical, diurnal preference measure, clinical measure and published in 2020 vs any other year (this latter analysis was included as studies published in 2020 overlap with the COVID-19 outbreak and may therefore include data collected during the pandemic) were investigated uses subgroup analyses. Continuous variables (age, year of publication, sample size and percentage of female participants) were explored using meta-regression.
Results
The initial literature search returned 864 articles (PubMed = 318, Web of Science = 546, see Supplemental S1 for a graphical overview). Following article screening, a total of 51 studies were entered into the initial random effects model. Outlier analyses identified a total of ten studies49–58 and these were subsequently excluded from the analysis (See Supplemental S2 for details of these studies including the 95% CI for each excluded effect size). Heterogeneity was reduced after excluding these studies (prior to exclusion I2 = 77.9%, Q(52) = 235.11, p < 0.001, after exclusion I2 = 60.2%, Q(42) = 105.5, p < 0.001) but remained substantial and significant. The final sample included 43 effect sizes from a total 27,996 participants with a mean age of 32 years. The predominant measure of eveningness was the MEQ (59% of included studies), CES-D and BDI where the most common measures of depressive symptomatology (respectively, 26% and 19%) and non-clinical samples made up 86% of effect sizes. Details of the included studies are shown in Table 1.
Table 1.
Study characteristics. For abbreviations please see main text.
| Author | Chronotype | Age | N | Females (%) | Sample | Depression measure |
|---|---|---|---|---|---|---|
| Akram et al.59 | MEQ | 24 | 453 | 75 | Non-clinical | HADS—depression subscale |
| Asarnow et al.60 | CSM | 43 | 139 | 66 | Clinical | HRSD |
| Aydin et al.61 | MEQ | 22 | 209 | 49 | Non-clinical | DASS-21 depression subscale |
| Bakotic et al.62 | CSM | 21 | 1052 | 62 | Non-clinical | HADS—depression subscale |
| Berdynaj et al.63 | MEQ | 21 | 86 | 78 | Non-clinical | DMS |
| Chan et al.26 | MEQ | 51 | 253 | 84 | Clinical | BDI |
| Coleman and Cain64 | rMEQ | 46 | 424 | 73 | Clinical | HRSD |
| Furusawa et al.65 | MEQ | 41 | 362 | 0 | Non-clinical | SDS |
| Gaspar-Barba et al.27 | MEQ | 32 | 82 | 37 | Clinical | BDI |
| Haraszti et al.66 | MEQ | 38 | 44 | 100 | Non-clinical | PHQ-9 |
| Hidalgo et al.23 | MEQ | 31 | 142 | 61 | Non-clinical | QUIDS-SR |
| Hirata et al.67 | MEQ | 22 | 33 | 52 | Non-clinical | SDS |
| Horne et al.53 | rMEQ | 24 | 167 | 77 | Non-clinical | CES-D |
| Hou et al.68 | MEQ | 37 | 884 | 63 | Non-clinical | CES-D |
| Hsu et al.69 | MEQ | 20 | 790 | 53 | Non-clinical | MADRS |
| Inomata et al.70 | MEQ | 21 | 27 | 48 | Non-clinical | CES-D |
| Jankowski and Dmitrzak-Weglarz71 | CSM | 32 | 338 | 51 | Non-clinical | HADS—depression subscale |
| Jankowski72 | CSM | 22 | 974 | 70 | Non-clinical | PHQ-4—depression subscale |
| Jeon et al.73 | MEQ | 32 | 700 | 91 | Non-clinical | CES-D |
| Kang et al.74 | rMEQ | 19 | 940 | 63 | Non-clinical | DASS-21 depression subscale |
| Khan et al.75 | MEQ | 40 | 59 | 54 | Non-clinical | BSRS |
| Lau et al.76 | CSM | 21 | 230 | 66 | Non-clinical | CES-D |
| Lester77 | MEQ | 22 | 194 | 72 | Non-clinical | CES-D |
| Liberman et al.78 | MEQ | 19 | 242 | 64 | Non-clinical | CES-D |
| Lin et al.79 | rMEQ | 27 | 1791 | 70 | Non-clinical | CES-D |
| Markarian et al.80 | MEQ | 38 | 296 | 60 | Non-clinical | HADS—depression subscale |
| Müller et al.81 | MEQ | 42 | 64 | 61 | Clinical | BDI |
| Ong et al.82 | CSM | 49 | 156 | NR | Non-clinical | BDI-short form |
| Park et al.83 | CSM | 19 | 5632 | 51 | Non-clinical | DASS-21 depression subscale |
| Park84 | CSM | 37 | 29 | 72 | Clinical | BDI |
| Przepiorka et al.85 | CSM | 20 | 398 | 71 | Non-clinical | BDI |
| Randler et al.86 | CSM | 22 | 277 | 100 | Non-clinical | HADS—depression subscale |
| Selvi et al.55* | MEQ | 31 | 80 | 55 | Non-clinical | BDI-II |
| Smagula et al.87 | CSM | 70 | 54 | 70 | Non-clinical | PHQ-9 |
| Sun et al.88 | rMEQ | 48 | 629 | NR | Non-clinical | CES-D |
| Togo et al.89 | MEQ | 41 | 2669 | 97 | Non-clinical | CES-D |
| Toomey et al.90 | MEQ | 55 | 1231 | NR | Non-clinical | BDI |
| Türkoglu and Selvi91 | MEQ | 42 | 70 | 83 | Non-clinical | CES-D |
| Üzer and Yücens58 * | MEQ | 65 | 70 | 50 | Non-clinical | PHQ-9 |
| Üzer and Yücens92 | MEQ | 22 | 339 | 54 | Non-clinical | BDI |
| Watts and Norbury93 | rMEQ | 26 | 240 | 79 | Non-clinical | BDI |
| Zhang et al.94 | MEQ | 19 | 616 | 65 | Non-clinical | PHQ-9 |
| Zhou et al.95 | MEQ | 19 | 4531 | 30 | Non-clinical | HADS—depression subscale |
*Two effect sizes were initially estimated for each of these studies two of which were subsequently identified outliers and excluded from the main random effects model.
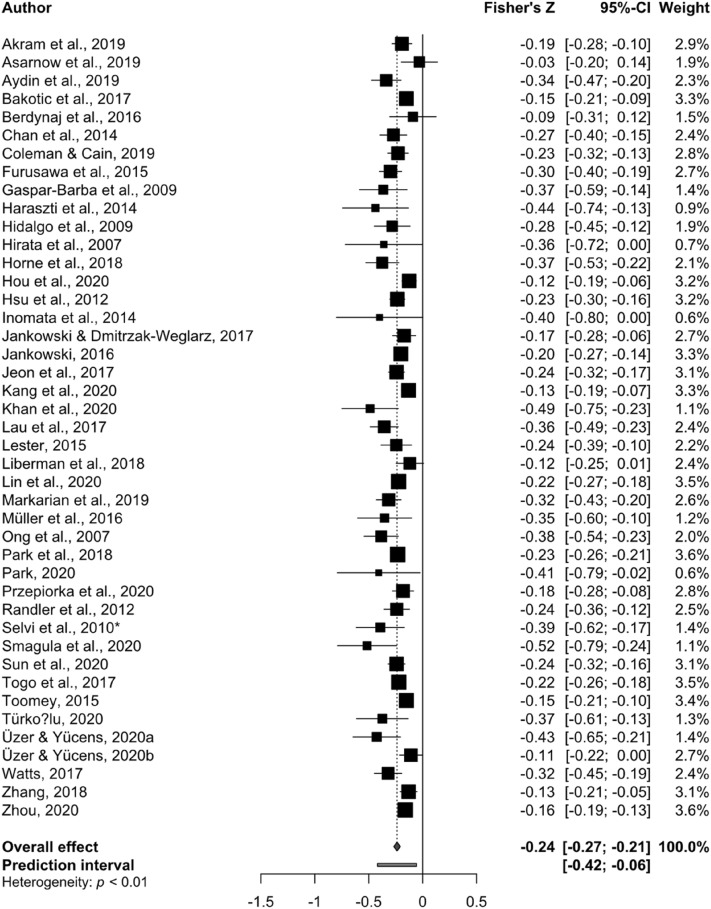
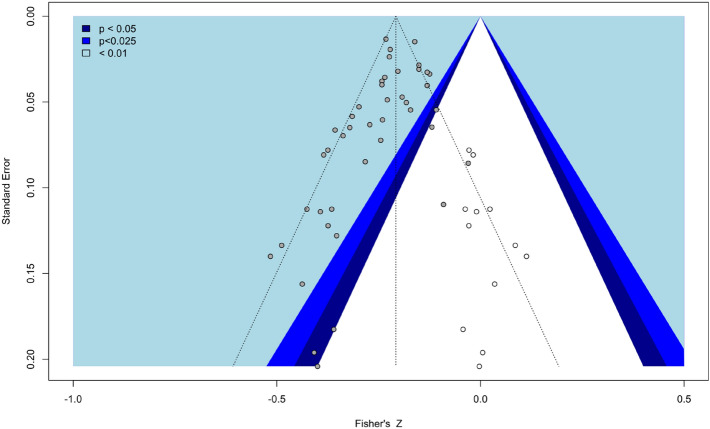
The effect size estimated from the random-effects model was Fisher’s Z = − 0.24, 95% CI [− 0.27. − 0.21], p < 0.001, demonstrating a small, but significant, association between eveningness and depression symptomatology (Fig. 1). Visual inspection of the funnel plot (Fig. 2) and the result of the Egger’s test of the intercept (− 1.135, 95% CI [− 1.86, − 0.41], p = 0.004) suggest publication bias should be taken into consideration when interpreting the results and the trim and fill adjusted estimate was − 0.21, 95% CI [− 0.2438; − 0.1715], p < 0.0001 with twelve adjusted studies.
Figure 1.
Forest plot of standardised effect sizes from each study. The overall effect is indicated in blue, prediction interval in red.
Figure 2.
Contour funnel plot indicating potential risk of publication bias. Open dots represent the 12 studies imputed to achieve symmetry.
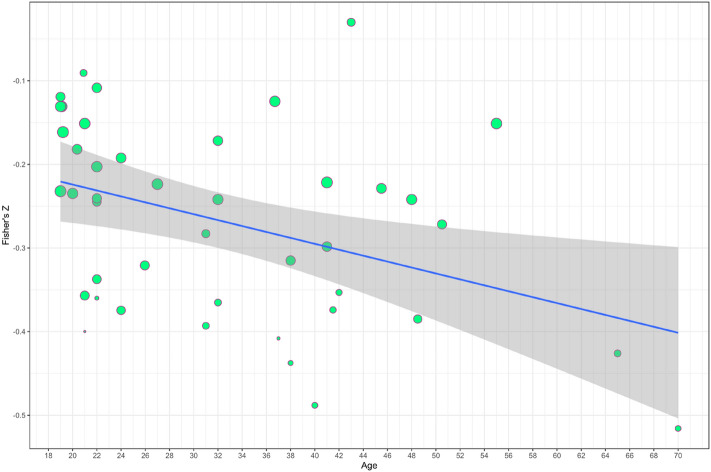
The substantial heterogeneity between studies suggests a potential impact of moderator variables on the reported association between eveningness and depressive symptomatology. To explore this a series of sub-group meta-analyses were conducted based on four potential confounders: Sample composition (clinical vs. non-clinical); Publication year (2020 vs. other year); Eveningness measure (MEQ vs. CSM vs. rMEQ) and Depression measure (BDI vs. CES-D vs. other). None of the included categorical moderators significantly explained heterogeneity in effect size. A summary of subgroup analyses is presented in Table 2. Meta-regression demonstrated that age was negatively associated with depression symptomatology (β = − 0.003, p = 0.03, 95% CI [− 0.005, − 0.0003], R2 = 10.63, Fig. 3). Neither sample size (β = 0.00, p = 0.12, 95% CI [− 0.00, 0.00], R2 = 4.44), year of publication (β = − 0.02, p = 0.56, 95% CI [− 0.09, 0.05], R2 = 0) or percentage of female participants (β = 0.00, p = 0.95, 95% CI [− 0.002, 0.002], R2 = 0) were related to the observed association between diurnal preference and depressive symptomatology.
Table 2.
Subgroup analysis.
| Subgroup analyses | Description | Contributing effect sizes | Fishers Z | 95% CI | Q | p value | |
|---|---|---|---|---|---|---|---|
| Sample composition | Clinical | 7 | − 0.27 | − 0.37 | − 0.17 | ||
| Non-clinical | 36 | − 0.23 | − 0.26 | − 0.20 | 0.52 | 0.47 | |
| Publication year | 2020 | 12 | − 0.24 | − 0.31 | − 0.16 | ||
| Other year& | 31 | − 0.24 | − 0.27 | − 0.21 | 0.00 | 0.94 | |
| Eveningness measure | CSM | 11 | − 0.24 | − 0.31 | − 0.17 | ||
| MEQ | 26 | − 0.24 | − 0.28 | − 0.20 | |||
| rMEQ | 6 | − 0.24 | − 0.30 | − 0.17 | 0.00 | 0.99 | |
| Depression measure | BDI | 12 | − 0.25 | − 0.32 | − 0.18 | ||
| CES-D | 10 | − 0.23 | − 0.28 | − 0.18 | |||
| Other&& | 21 | − 0.24 | − 0.28 | − 0.20 | 0.13 | 0.94 | |
Other year& = publication year other than 2020; Other&& = any depression measure other than BDI or CES-D (see text for details). Q-test for between study heterogeneity, p value for subgroup differences.
Figure 3.
Regression of effect size (Fisher’s Z) on age. Line of best fit plus confidence interval, bubbles show study weight.
Discussion
The current findings demonstrate a small but significant association between diurnal preference and depressive symptomatology. All of the reported studies indicated a positive association between eveningness and depression, ranging between − 0.52 and − 0.03. The summary effect size for the random effects model was − 0.24 which is largely consistent with an earlier meta-analysis30 that reported an effect size of − 0.2 and together these data suggest a small but reliable association between eveningness and depression. Contrary to the findings of Au and Reece, in the current analysis evidence of a potential publication bias (i.e. statistically significant or favourable results being more likely to be published than studies with non-significant or unfavourable results) was observed. The adjusted effect size (Fishers Z = − 0.21), however, remained significant. Subgroup analyses demonstrated no moderating effect of sample characteristics, eveningness or depression measure, or studies published in 2020 vs. any other year. Meta-regression showed a significant effect of age on the association between eveningness and depression symptomatology, but no evidence for a moderating effect of sample size, gender ratio, or year of publication.
A long-standing question in the literature is one of directionality; does eveningness cause depression or is eveningness a consequence of the disorder? The cross-sectional studies quantified here cannot speak directly to this question. However, the current results demonstrated no significant difference between clinical and non-clinical samples, a finding consistent with Au and Reece30. Eveningness may therefore represent a risk-factor for depression rather than a consequence of the depressed state. The vulnerability-stress hypothesis of depression96,97 proposes that depression emerges through an interaction between psychological vulnerability factors (e.g., negative biases/preferential processing of negative material) and an environmental stressor (e.g., bereavement, financial insecurity). Importantly, previous work suggests that eveningness is associated with aspects of negative thinking (i.e. psychological vulnerability factors) in never-depressed individuals. For example, eveningness has been associated with greater recall for negative personality trait words, greater recognition of sad facial expressions63,98 and maladaptive emotion regulation strategies93,99. Similarly, high neuroticism (i.e. individuals who are emotionally reactive and tend to experience more negative emotions and depression) has also been associated with eveningness100. Converging evidence, therefore, suggests that in healthy, never-depressed individuals, eveningness is associated with depressogenic personality types, negative biases in emotional processing and impaired emotion regulation which, if combined with adversity, may lead to depression. These findings also suggest modifiable markers that could be therapeutically targeted to prevent the onset of depression in evening type individuals.
Of the moderators tested here only age was significantly associated with effect size. This contrasts with the findings of Au and Reece (2017) who did not observe a similar relationship. The mean age range in the current study was 19–70, which is broader than included by Au and Reece (19–55, MDD sample only) which may account for the discrepancy. Although it should be noted that for the majority of studies included here (~ 50%) the mean age was less than 30 years of age. Of note, Kim et al. recently reported no difference in prevalence rates for depression in late chronotypes vs. neither types in a population of Korean adults stratified by age (19–40, 41–59 and 60–80 years). However, although the total sample size was large (N = 6382) the number of participants in the older 60–80 years group classified as evening-type was small (N = 22) which may limit interoperability101. Counter to this, eveningness has been associated with increased odds for reporting depression in a large sample of older adults (age range 40–70 years) taken from the UK Biobank102. Similarly, here increasing age was associated with increased depressive symptomatology but the factors underpinning this effect remain to be elucidated. Older individuals that remain more evening-type may gradually lose friendship networks and group allegiances as peers gravitate to a social schedule in synchrony with their changing circadian typology, potentially leaving evening-prone individuals more isolated and potentially more prone to depression. This notion, however, is purely speculative and requires further investigation with suitably powered, prospective studies to determine the potential impact of age on the association between eveningness and depression.
There are several limitations associated with this work which should be considered when interpreting the results. A general limitation of meta-analyses is that by creating a summary of outcomes, important between-study differences are ignored. To formally address this here study inclusion was restricted to adults, for clinical samples mood disorders other than MDD were excluded and only studies that used validated instruments to measure depressive symptomatology and diurnal preference were included. In addition, moderator analysis and meta-regression were employed to explore study heterogeneity. More specifically, the current analysis was unable to account for important factors that may impact the results. Sleep duration and/or sleep quality, for example, were not taking into consideration (zero-order correlations or unadjusted odds-ratios/mean differences were reported). Similarly, social jet-lag, the difference between internal rhythm and external demands (e.g. work or university), which may be more pronounced in evening-types and is associated with increased likelihood of reporting depressive symptoms103,104 was not included in this meta-analysis. The current report, therefore, cannot directly assess the potential impact of social jetlag on the association between eveningness and depressive symptoms. Further, the terms chronotype and diurnal preference are frequently used interchangeably in the literature but reflect different aspects of the same phenomenon. Here, the focus was diurnal preference and the questionnaires included limited to the MEQ, rMEQ and CSM which determine morningness/eveningness preferences based on self-reported preferences for times of activity and rest. These measures, therefore, reflect a personality trait. By contrast, instruments such as the Munich Chronotype Questionnaire (MCTQ)105 measure behaviour (mid-point of sleep on free days) which can be viewed as an indicator of state106. The focus of the current report was unipolar depression, but increasing evidence links eveningness with other affective disorders such as bipolar disorder107 and Major Depressive Disorder with Seasonal Pattern108 and anxiety109. Future meta-analyses that review and synthesise the recent literature related to these disorders is warranted. Finally, it should also be noted that all phases of this review and analyses were conducted solely by the author.
In summary, the current meta-analysis demonstrated that eveningness is associated with depressive symptoms. These data are largely consistent with a previous meta-analysis30 and the extant literature. The underlying causes that lead to depression are likely multifactorial and progress in understanding the links between diurnal preference and depression is predicated on a better understanding of the mechanistic underpinnings and suitably powered prospective studies that allow causal inference.
Supplementary Information
Author contributions
R.N. was responsible for reviewing the included studies, statistical analysis and manuscript preperation.
Funding
The author received no financial support for research or authorship. Funding to support publication fees was provided by Brunel University, London.
Competing interests
The author declares no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-91205-3.
References
- 1.Logan RW, McClung CA. Rhythms of life: Circadian disruption and brain disorders across the lifespan. Nat. Rev. Neurosci. 2019;20:49–65. doi: 10.1038/s41583-018-0088-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum. Psychopharmacol. 2008;23:571–585. doi: 10.1002/hup.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendoza J. Circadian insights into the biology of depression: Symptoms, treatments and animal models. Behav. Brain Res. 2019;376:112186. doi: 10.1016/j.bbr.2019.112186. [DOI] [PubMed] [Google Scholar]
- 4.Souêtre E, et al. Circadian rhythms in depression and recovery: Evidence for blunted amplitude as the main chronobiological abnormality. Psychiatry Res. 1989;28:263–278. doi: 10.1016/0165-1781(89)90207-2. [DOI] [PubMed] [Google Scholar]
- 5.Torquati L, Mielke GI, Brown WJ, Burton NW, Kolbe-Alexander TL. Shift work and poor mental health: A meta-analysis of longitudinal studies. Am. J. Public Health. 2019;109:e13–e20. doi: 10.2105/AJPH.2019.305278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz G, Knobler HY, Laibel Z, Strauss Z, Durst R. Time zone change and major psychiatric morbidity: The results of a 6-year study in Jerusalem. Comp. Psychiatry. 2002;43:37–40. doi: 10.1053/comp.2002.29849. [DOI] [PubMed] [Google Scholar]
- 7.Levandovski R, et al. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol. Int. 2011;28:771–778. doi: 10.3109/07420528.2011.602445. [DOI] [PubMed] [Google Scholar]
- 8.Graw P, Kräuchi K, Wirz-Justice A, Pöldinger W. Diurnal variation of symptoms in seasonal affective disorder. Psychiatry Res. 1991;37:105–111. doi: 10.1016/0165-1781(91)90110-B. [DOI] [PubMed] [Google Scholar]
- 9.Vadnie CA, McClung CA. Circadian rhythm disturbances in mood disorders: Insights into the role of the suprachiasmatic nucleus. Neural Plast. 2017;2017:1–28. doi: 10.1155/2017/1504507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrante A, et al. Diurnal preference predicts phase differences in expression of human peripheral circadian clock genes. J. Circadian Rhythms. 2015;13:5334. doi: 10.5334/jcr.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness–eveningness in human circadian rhythms. Int. J. Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 12.Adan A, Almirall H. Horne & Östberg morningness-eveningness questionnaire: A reduced scale. Personal. Individ. Differ. 1991;12:241–253. doi: 10.1016/0191-8869(91)90110-W. [DOI] [Google Scholar]
- 13.Smith CS, Reilly C, Midkiff K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J. Appl. Psychol. 1989;74:728–738. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- 14.Di Milia L, Adan A, Natale V, Randler C. Reviewing the psychometric properties of contemporary circadian typology measures. Chronobiol. Int. 2013;30:1261–1271. doi: 10.3109/07420528.2013.817415. [DOI] [PubMed] [Google Scholar]
- 15.Kantermann T, Sung H, Burgess HJ. Comparing the morningnes-–seveningness questionnaire and munich chronotype questionnaire to the dim light melatonin onset. J. Biol. Rhythms. 2015;30:449–453. doi: 10.1177/0748730415597520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barclay NL, Watson NF, Buchwald D, Goldberg J. Moderation of genetic and environmental influences on diurnal preference by age in adult twins. Chronobiol. Int. 2014;31:222–231. doi: 10.3109/07420528.2013.842924. [DOI] [PubMed] [Google Scholar]
- 17.Barclay NL, Rowe R, O’Leary R, Bream D, Gregory AM. Longitudinal stability of genetic and environmental influences on the association between diurnal preference and sleep quality in young adult twins and siblings. J. Biol. Rhythms. 2016;31:375–386. doi: 10.1177/0748730416653533. [DOI] [PubMed] [Google Scholar]
- 18.Fabbian F, et al. Chronotype, gender and general health. Chronobiol. Int. 2016;33:864. doi: 10.1080/07420528.2016.1176927. [DOI] [PubMed] [Google Scholar]
- 19.Kivelä L, Papadopoulos MR, Antypa N. Chronotype and psychiatric disorders. Curr. Sleep Med. Rep. 2018 doi: 10.1007/s40675-018-0113-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor BJ, Hasler BP. Chronotype and mental health: Recent advances. Curr. Psychiatry Rep. 2018;20:59. doi: 10.1007/s11920-018-0925-8. [DOI] [PubMed] [Google Scholar]
- 21.Kitamura S, et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol. Int. 2010;27:1797–1812. doi: 10.3109/07420528.2010.516705. [DOI] [PubMed] [Google Scholar]
- 22.Merikanto I, et al. Evening types are prone to depression. Chronobiol. Int. 2013;30:719–725. doi: 10.3109/07420528.2013.784770. [DOI] [PubMed] [Google Scholar]
- 23.Hidalgo MP, et al. Relationship between depressive mood and chronotype in healthy subjects. Psychiatry Clin. Neurosci. 2009;63:283–290. doi: 10.1111/j.1440-1819.2009.01965.x. [DOI] [PubMed] [Google Scholar]
- 24.Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BWJH. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress. Anxiety. 2015 doi: 10.1002/da.22422. [DOI] [PubMed] [Google Scholar]
- 25.Merikanto I, et al. Circadian preference links to depression in general adult population. J. Affect. Disord. 2015;188:143–148. doi: 10.1016/j.jad.2015.08.061. [DOI] [PubMed] [Google Scholar]
- 26.Chan JWY, et al. Eveningness and insomnia: Independent Risk factors of nonremission in major depressive disorder. Sleep. 2014 doi: 10.5665/sleep.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaspar-Barba E, et al. Depressive symptomatology is influenced by chronotypes. J. Affect. Disord. 2009;119:100–106. doi: 10.1016/j.jad.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 28.Bauducco S, Richardson C, Gradisar M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 2020;34:77–83. doi: 10.1016/j.copsyc.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Taillard J, Sagaspe P, Philip P, Bioulac S. Sleep timing, chronotype and social jetlag: Impact on cognitive abilities and psychiatric disorders. Biochem. Pharmacol. 2021;1:114438. doi: 10.1016/j.bcp.2021.114438. [DOI] [PubMed] [Google Scholar]
- 30.Au J, Reece J. The relationship between chronotype and depressive symptoms: A meta-analysis. J. Affect. Disord. 2017;218:93–104. doi: 10.1016/j.jad.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 32.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 33.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Psychology Foundation of Australa; 1995. [Google Scholar]
- 35.Brown ES, et al. The Quick Inventory of Depressive Symptomatology–Self-report: A psychometric evaluation in patients with asthma and major depressive disorder. Ann. Allergy Asthma Immunol. 2008;100:433–438. doi: 10.1016/S1081-1206(10)60467-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 37.Zung WK. A self-rating depression scale. Arch. Gen. Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 38.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry J. Ment. Sci. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 41.Lee MB, Lee YJ, Yen LL, Lin MH, Lue BH. Reliability and validity of using a Brief psychiatric symptom rating scale in clinical practice. J. Formos. Med. Assoc. 1990;89:1081–1087. [PubMed] [Google Scholar]
- 42.Yesavage JA, et al. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 43.Roane BM, et al. Reliability of a scale assessing depressed mood in the context of sleep. TPM Test. Psychom. Methodol. Appl. Psychol. 2013;20:3–11. doi: 10.4473/TPM20.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Law M, et al. Critical review form: Quantitative studies. J. Psychiatr. Res. 1995;3:1–10. [Google Scholar]
- 45.R Core Team. (R Foundation for Statistical Computing, 2020).
- 46.Makambi KH. The effect of the heterogeneity variance estimator on some tests of treatment efficacy. J. Biopharm. Stat. 2004;14:439–449. doi: 10.1081/BIP-120037191. [DOI] [PubMed] [Google Scholar]
- 47.Statistical Power Analysis for the Behavioral Sciences. (Erlbaum, 1988).
- 48.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic Press; 2013. [Google Scholar]
- 49.Bacaro V, et al. Insomnia in the Italian population during covid-19 outbreak: A snapshot on one major risk factor for depression and anxiety. Front. Psychiatry. 2020;11:579107. doi: 10.3389/fpsyt.2020.579107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choi HJ, Lee YJ, Yoo YJ, Cho YW, Moon H-J. The effects of chronotype and social jetlag on medical students. Sleep Biol. Rhythms. 2019;17:269–276. doi: 10.1007/s41105-018-00198-6. [DOI] [Google Scholar]
- 51.Corruble E, et al. Morningness: Eveningness and treatment response in major depressive disorder. Chronobiol. Int. 2014;31:283–289. doi: 10.3109/07420528.2013.834924. [DOI] [PubMed] [Google Scholar]
- 52.Hogben AL, Ellis J, Archer SN, von Schantz M. Conscientiousness is a predictor of diurnal preference. Chronobiol. Int. 2007;24:1249–1254. doi: 10.1080/07420520701791596. [DOI] [PubMed] [Google Scholar]
- 53.Horne CM, Norbury R. Late chronotype is associated with enhanced amygdala reactivity and reduced fronto-limbic functional connectivity to fearful versus happy facial expressions. Neuroimage. 2018;171:355–363. doi: 10.1016/j.neuroimage.2018.01.025. [DOI] [PubMed] [Google Scholar]
- 54.Hwang JY, Kang S-G, Gwak AR, Park J, Lee YJ. The associations of morningness–eveningness with anger and impulsivity in the general population. Chronobiol. Int. 2016;33:200–209. doi: 10.3109/07420528.2015.1128947. [DOI] [PubMed] [Google Scholar]
- 55.Selvi Y, et al. Associations between chronotype, sleep quality, suicidality, and depressive symptoms in patients with major depression and healthy controls. Chronobiol. Int. 2010;27:1813–1828. doi: 10.3109/07420528.2010.516380. [DOI] [PubMed] [Google Scholar]
- 56.Sultan A, Taj S, Choudhary V, Parganiha A. Predictive role of socio-demographic and chronotype on health-related quality of life of cancer patients from southeastern India. Biol. Rhythm Res. 2020;1:1–16. doi: 10.1080/09291016.2020.1816050. [DOI] [Google Scholar]
- 57.Thapa N, et al. The relationship between chronotype, physical activity and the estimated risk of dementia in community-dwelling older adults. Int. J. Environ. Res. Public. Health. 2020;17:3701. doi: 10.3390/ijerph17103701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Üzer A, Yücens B. The effect of circadian preferences on insomnia severity and depressive symptoms via sleep hygiene in older adults with depression and healthy controls. Psychogeriatrics. 2020;20:871–879. doi: 10.1111/psyg.12610. [DOI] [PubMed] [Google Scholar]
- 59.Akram U, Stevenson JC, Gardani M, Akram A, Allen S. Psychopathy and chronotype disposition: The mediating role of depression. Heliyon. 2019;5:e2854. doi: 10.1016/j.heliyon.2019.e02894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Asarnow LD, et al. Circadian preference as a moderator of depression outcome following cognitive behavioral therapy for insomnia plus antidepressant medications: A report from the TRIAD study. J. Clin. Sleep Med. 2019;15:573–580. doi: 10.5664/jcsm.7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aydin D, Selvi Y, Kandeger A, Boysan M. The relationship of consumers’ compulsive buying behavior with biological rhythm, impulsivity, and fear of missing out. Biol. Rhythm Res. 2019;1:1–9. doi: 10.1080/09291016.2019.1654203. [DOI] [Google Scholar]
- 62.Bakotic M, Radosevic-Vidacek B, Bjelajac AK. Morningness–eveningness and daytime functioning in university students: The mediating role of sleep characteristics. J. Sleep Res. 2017;26:210–218. doi: 10.1111/jsr.12467. [DOI] [PubMed] [Google Scholar]
- 63.Berdynaj D, et al. Effect of chronotype on emotional processing and risk taking. Chronobiol. Int. 2016;1:1–13. doi: 10.3109/07420528.2016.1146739. [DOI] [PubMed] [Google Scholar]
- 64.Coleman MY, Cain SW. Eveningness is associated with greater subjective cognitive impairment in individuals with self-reported symptoms of unipolar depression. J. Affect. Disord. 2019;256:404–415. doi: 10.1016/j.jad.2019.05.054. [DOI] [PubMed] [Google Scholar]
- 65.Furusawa M, et al. Relationship between morningness–eveningness typology and cumulative fatigue or depression among Japanese male workers. Ind. Health. 2015;53:361–367. doi: 10.2486/indhealth.2013-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Haraszti RÁ, et al. Morningness–eveningness interferes with perceived health, physical activity, diet and stress levels in working women: A cross-sectional study. Chronobiol. Int. 2014;31:829–837. doi: 10.3109/07420528.2014.911188. [DOI] [PubMed] [Google Scholar]
- 67.Hirata FC, et al. Depression in medical school: The Influence of morningness–eveningness. Chronobiol. Int. 2007;24:939–946. doi: 10.1080/07420520701657730. [DOI] [PubMed] [Google Scholar]
- 68.Hou T, Zhang F, Mao X, Deng G. Chronotype and psychological distress among Chinese rural population: A moderated mediation model of sleep quality and age. PLoS ONE. 2020;15:0241351. doi: 10.1371/journal.pone.0241301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hsu C-Y, Gau SS-F, Shang C-Y, Chiu Y-N, Lee M-B. Associations between chronotypes, psychopathology, and personality among incoming college students. Chronobiol. Int. 2012;29:491–501. doi: 10.3109/07420528.2012.668995. [DOI] [PubMed] [Google Scholar]
- 70.Inomata Y, Echizenya M, Takeshima M, Shimizu K, Shimizu T. Validity and reliability of the Japanese version of the morningness–eveningness questionnaire evaluated from actigraphy. Sleep Biol. Rhythms. 2014;12:289–296. doi: 10.1111/sbr.12073. [DOI] [Google Scholar]
- 71.Jankowski KS, Dmitrzak-Weglarz M. ARNTL, CLOCK and PER3 polymorphisms: Links with chronotype and affective dimensions. Chronobiol. Int. 2017;34:1105–1113. doi: 10.1080/07420528.2017.1343341. [DOI] [PubMed] [Google Scholar]
- 72.Jankowski KS. Morningness-eveningness and depressive symptoms: Test on the components level with CES-D in Polish students. J. Affect. Disord. 2016;196:47–53. doi: 10.1016/j.jad.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 73.Jeon HJ, Bang YR, Park HY, Kim SA, Yoon I-Y. Differential effects of circadian typology on sleep-related symptoms, physical fatigue and psychological well-being in relation to resilience. Chronobiol. Int. 2017;34:677–686. doi: 10.1080/07420528.2017.1309425. [DOI] [PubMed] [Google Scholar]
- 74.Kang Y, et al. Testing the bidirectional associations of mobile phone addiction behaviors with mental distress, sleep disturbances, and sleep patterns: A one-year prospective study among Chinese College students. Front. Psychiatry. 2020;11:10. doi: 10.3389/fpsyt.2020.00634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Khan WAA, Conduit R, Kennedy GA, Jackson ML. The relationship between shift-work, sleep, and mental health among paramedics in Australia. Sleep Health. 2020;6:330–337. doi: 10.1016/j.sleh.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 76.Lau EYY, Hui CH, Lam J, Cheung S-F. Sleep and optimism: A longitudinal study of bidirectional causal relationship and its mediating and moderating variables in a Chinese student sample. Chronobiol. Int. 2017;34:360–372. doi: 10.1080/07420528.2016.1276071. [DOI] [PubMed] [Google Scholar]
- 77.Lester D. Morningness–eveningness, current depression, and past suicidality. Psychol. Rep. 2015;116:331–336. doi: 10.2466/16.02.PR0.116k18w5. [DOI] [PubMed] [Google Scholar]
- 78.Liberman AR, Halitjaha L, Ay A, Ingram KK. Modeling strengthens molecular link between circadian polymorphisms and major mood disorders. J. Biol. Rhythms. 2018;33:318–336. doi: 10.1177/0748730418764540. [DOI] [PubMed] [Google Scholar]
- 79.Lin C-Y, et al. Temporal associations between morningness/eveningness, problematic social media use, psychological distress and daytime sleepiness: Mediated roles of sleep quality and insomnia among young adults. J. Sleep Res. 2020;1:e13076. doi: 10.1111/jsr.13076. [DOI] [PubMed] [Google Scholar]
- 80.Markarian SA, Gildner DJ, Pickett SM, Warnke AS. Morningness-eveningness and social anxiety symptoms: The influence of depression symptoms on the indirect effect through punishment sensitivity and experiential avoidance. Chronobiol. Int. 2019;36:214–224. doi: 10.1080/07420528.2018.1529679. [DOI] [PubMed] [Google Scholar]
- 81.Müller MJ, Olschinski C, Kundermann B, Cabanel N. Patterns of self-reported depressive symptoms in relation to morningness–eveningness in inpatients with a depressive disorder. Psychiatry Res. 2016;239:163–168. doi: 10.1016/j.psychres.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 82.Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J. Clin. Sleep Med. 2007;3:289–294. doi: 10.5664/jcsm.26801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Park H, Lee H-K, Lee K. Chronotype and suicide: The mediating effect of depressive symptoms. Psychiatry Res. 2018;269:316–320. doi: 10.1016/j.psychres.2018.08.046. [DOI] [PubMed] [Google Scholar]
- 84.Park Y-M. Relationship between auditory evoked potentials and circadian preference in patients with major depressive episodes. Brain Sci. 2020;10:370. doi: 10.3390/brainsci10060370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Przepiorka A, Blachnio A, Cudo A. Relationships between morningness, Big Five personality traits, and problematic Internet use in young adult university students: Mediating role of depression. Chronobiol. Int. 2020;38:248–259. doi: 10.1080/07420528.2020.1851703. [DOI] [PubMed] [Google Scholar]
- 86.Randler C, Stadler L, Vollmer C, Diaz-Morales JF. Relationship between depressive symptoms and sleep duration/chronotype in women. J. Individ. Differ. 2012;33:186–191. doi: 10.1027/1614-0001/a000089. [DOI] [Google Scholar]
- 87.Smagula SF, et al. Resting-state function connectivity associated with being a “morning-type” dementia caregiver and having lower depression symptom severity. J. Gerontol. 2020;6:115. doi: 10.1093/geronb/gbaa115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sun X, Gustat J, Bertisch S, Redline S, Bazzano L. The association between sleep chronotype and obesity among black and white participants of the Bogalusa Heart Study. Chronobiol. Int. 2020;37:123–134. doi: 10.1080/07420528.2019.1689398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Togo F, Yoshizaki T, Komatsu T. Association between depressive symptoms and morningness–eveningness, sleep duration and rotating shift work in Japanese nurses. Chronobiol. Int. 2017;34:349–359. doi: 10.1080/07420528.2016.1273942. [DOI] [PubMed] [Google Scholar]
- 90.Toomey R, Panizzon MS, Kremen WS, Franz CE, Lyons MJ. A twin-study of genetic contributions to morningness–eveningness and depression. Chronobiol. Int. 2015;32:303–309. doi: 10.3109/07420528.2014.971366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Türkoğlu G, Selvi Y. The relationship between chronotype, sleep disturbance, severity of fibromyalgia, and quality of life in patients with fibromyalgia. Chronobiol. Int. 2020;37:68–81. doi: 10.1080/07420528.2019.1684314. [DOI] [PubMed] [Google Scholar]
- 92.Üzer A, Yücens B. Chronotype and depressive symptoms in healthy subjects: The mediating role of hopelessness and subjective sleep quality. Chronobiol. Int. 2020;37:1173–1180. doi: 10.1080/07420528.2020.1775629. [DOI] [PubMed] [Google Scholar]
- 93.Watts AL, Norbury R. Reduced effective emotion regulation in night owls. J. Biol. Rhythms. 2017;32:369–375. doi: 10.1177/0748730417709111. [DOI] [PubMed] [Google Scholar]
- 94.Zhang Y, et al. Caffeinated drinks intake, late chronotype, and increased body mass index among medical students in Chongqing, China: A multiple mediation model. Int. J. Environ. Res. Public. Health. 2018;15:1–10. doi: 10.3390/ijerph15081721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhou J, et al. Chronotype and depressive symptoms: A moderated mediation model of sleep quality and resilience in the 1st-year college students. J. Clin. Psychol. 2021;77:340–355. doi: 10.1002/jclp.23037. [DOI] [PubMed] [Google Scholar]
- 96.Hankin BL, Abramson LY, Miller N, Haeffel GJ. Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cogn. Ther. Res. 2004;28:309–345. doi: 10.1023/B:COTR.0000031805.60529.0d. [DOI] [Google Scholar]
- 97.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Theory of Depression. Guildford; 1979. [Google Scholar]
- 98.Horne C, Marr-Phillips SDM, Jawaid R, Gibson EL, Norbury R. Negative emotional biases in late chronotypes. Biol. Rhythm Res. 2017;48:151–155. doi: 10.1080/09291016.2016.1236461. [DOI] [Google Scholar]
- 99.Antypa N, et al. Associations between chronotypes and psychological vulnerability factors of depression. Chronobiol. Int. 2017;34:1134. doi: 10.1080/07420528.2017.1345932. [DOI] [PubMed] [Google Scholar]
- 100.Duggan KA, Friedman HS, McDevitt EA, Mednick SC. Personality and healthy sleep: The importance of conscientiousness and neuroticism. PLoS ONE. 2014;9:e90628. doi: 10.1371/journal.pone.0090628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kim KM, Han SM, Heo K, Kim W-J, Chu MK. Sex differences in the association between chronotype and risk of depression. Sci. Rep. 2020;10:18512. doi: 10.1038/s41598-020-75724-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Norbury R, et al. Chronotype, depression and hippocampal volume: Cross-sectional associations from the UK Biobank. Chronobiol. Int. 2019;36:709–716. doi: 10.1080/07420528.2019.1578229. [DOI] [PubMed] [Google Scholar]
- 103.Islam Z, et al. Social jetlag is associated with an increased likelihood of having depressive symptoms among the Japanese working population: The Furukawa Nutrition and Health Study. Sleep. 2020;43:10. doi: 10.1093/sleep/zsz204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006;23:497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 105.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 106.Levandovski R, Sasso E, Hidalgo MP. Chronotype: a review of the advances, limits and applicability of the main instruments used in the literature to assess human phenotype. Trends Psychiatry Psychother. 2013;35:3–11. doi: 10.1590/S2237-60892013000100002. [DOI] [PubMed] [Google Scholar]
- 107.Kanagarajan K, et al. Morningness–eveningness questionnaire in bipolar disorder. Psychiatry Res. 2018;262:102–107. doi: 10.1016/j.psychres.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 108.Jankowski KS. Morningness–eveningness and seasonality. Biol. Rhythm Res. 2017;48:331–342. doi: 10.1080/09291016.2016.1263001. [DOI] [Google Scholar]
- 109.Alvaro PK, Roberts RM, Harris JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. 2014;15:934–941. doi: 10.1016/j.sleep.2014.03.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.