Abstract
Vertebral hemangiomas are an incidental and relatively common radiological finding and a benign tumor of vascular origin. VH are the most common spine tumors with an estimated incidence of 1.9-27% in the general population. Rarely, vertebral hemangiomas can exhibit extraosseous expansion with resulting compression of the spinal cord. Such lesions are termed aggressive or atypical vertebral hemangiomas (AVH) and account for less than 1% of spinal hemangiomas. A 68-year-old female was referred with progressive walking difficulty and sensory disturbances in her lower extremities. MRI imaging of the thoracic spine revealed a T1- and T2-weighted hyperintense lesion involving the T10 vertebra. Additionally, there was extraosseous extension of the tumor into the spinal canal, located both anterior and posterior to the spinal cord, causing severe spinal cord compression. A combined endovascular and surgical approach (arterial coil embolization and en bloc resection) for treatment was decided. Although vertebral hemangiomas are an incidental and relatively common radiological finding, the findings of our case were consistent with an aggressive hemangioma with atypical MRI and clinical prognostic characteristics. In summary, the present case highlights the need for multidisciplinary approach and in-depth knowledge of this rare pathologic entity.
Keywords: Αggressive Vertebral Hemangiomas, En Bloc Resection, Endovascular Embolization, Prognosis, Recurrence
Introduction
Vertebral hemangiomas (VH) are an incidental and relatively common radiological finding and a benign tumor of vascular origin. VH are the most common spine tumors (3% of all spine tumors) with an estimated incidence of 1.9-27% in the general population. They were first described in 1863 by Virchow, Perman (1926) and Bailey/Bucy (1929). Bucy and Capp (1930) first described the radiological features of hemangiomas[1]. The vast majority of VH is asymptomatic (Enneking 1, S1) or present with pain as the only symptom (Enneking 2, S2). VH are characterized as latent, aggressive and recurrent and can be also classified as cavernous, capillary and mixed types with various degree of fat content[2]. Rarely, VH can exhibit extraosseous expansion with resulting compression of the spinal cord. Such lesions are termed aggressive or atypical vertebral hemangiomas (AVH) and account for less than 1 % of spinal hemangiomas (Enneking 3, S3).
Case presentation
A 68-year-old female was referred with progressive walking difficulty and sensory disturbances in her lower extremities. Symptoms began 12 months prior to referral as radicular pain in her legs, followed by a slowed and mildly unsteady gait a few weeks later. Over the following months, the patient gradually developed significant restrictions to her mobility. On clinical examination, motor examination was normal (MRC Grade 5/5) while decreased light touch sensation with a mid-thoracic sensory level as well as lower extremity hyperreflexia and increased tone were observed. Her gait was broad-based, and she was not able to tandem gait. She used a cane for support.
MRI imaging of the thoracic spine revealed a T1- and T2-weighted hyperintense lesion involving the T10 vertebral body, both pedicles, both transverse processes, the lamina, and the spinous process. Additionally, there was extraosseous extension of the tumor into the spinal canal, located both anterior and posterior to the spinal cord, causing severe spinal cord compression. The subarachnoid space was effaced and spinal cord signal change was observed, consistent with cord edema or myelomalacia. The findings were consistent with an aggressive hemangioma (Enneking S3/Weinstein-Boriani- Biagnini D-E) (Figures 1-4).
Figure 1.
MRI Sagittal T1- weighted hyperintense lesion involving the T10 vertebral body.
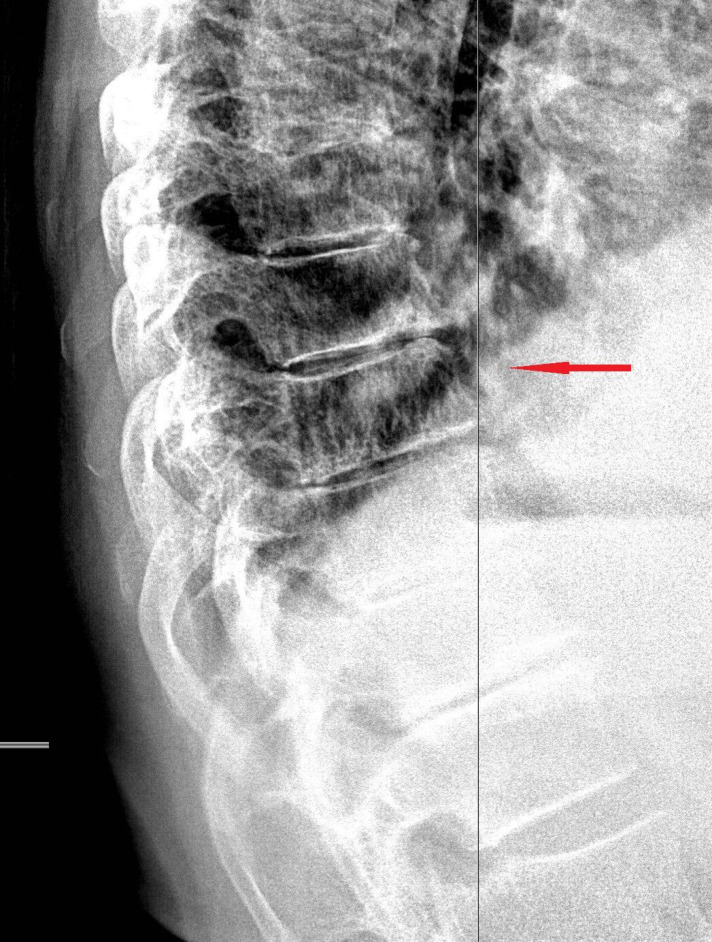
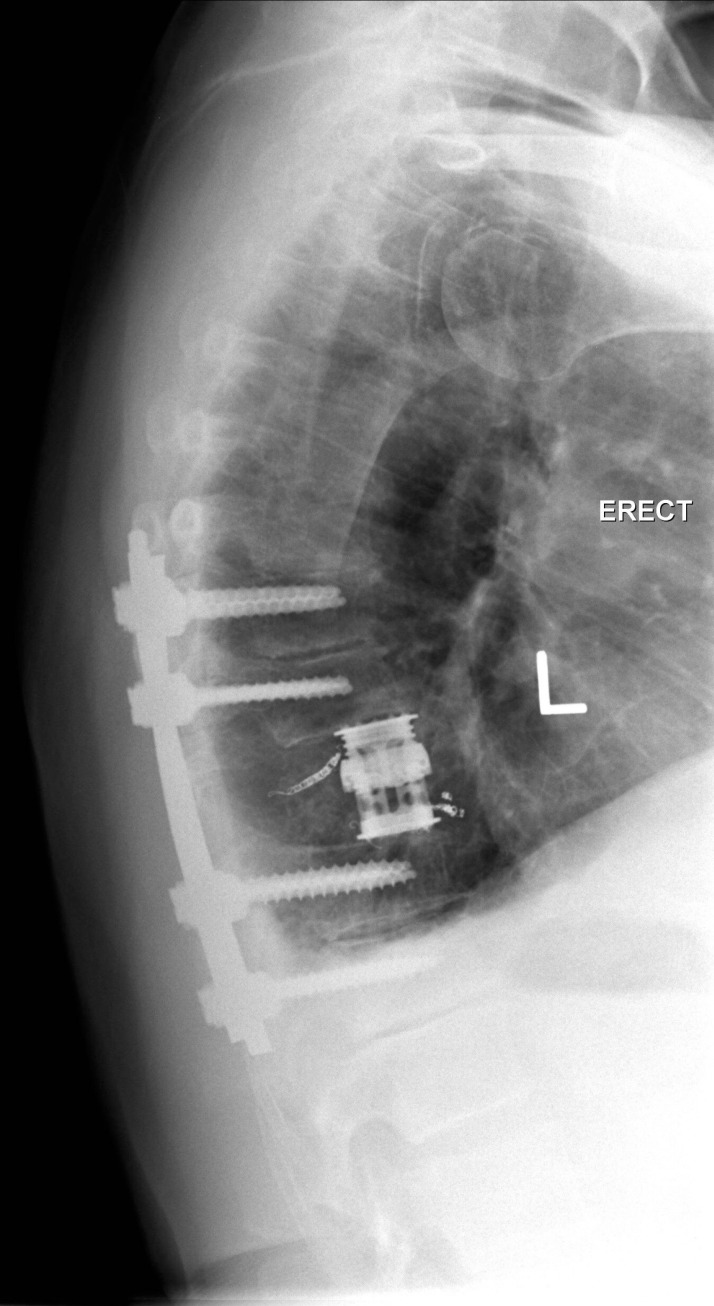
Figure 4.
Lateral x-ray at presentation. Arrow on the T10 vertebra.
Figure 2.
MRI Sagittal T2- weighted hyperintense lesion involving the T10 vertebral body.
Figure 3.
MRI Axial T2- weighted image of the T10 vertebra.
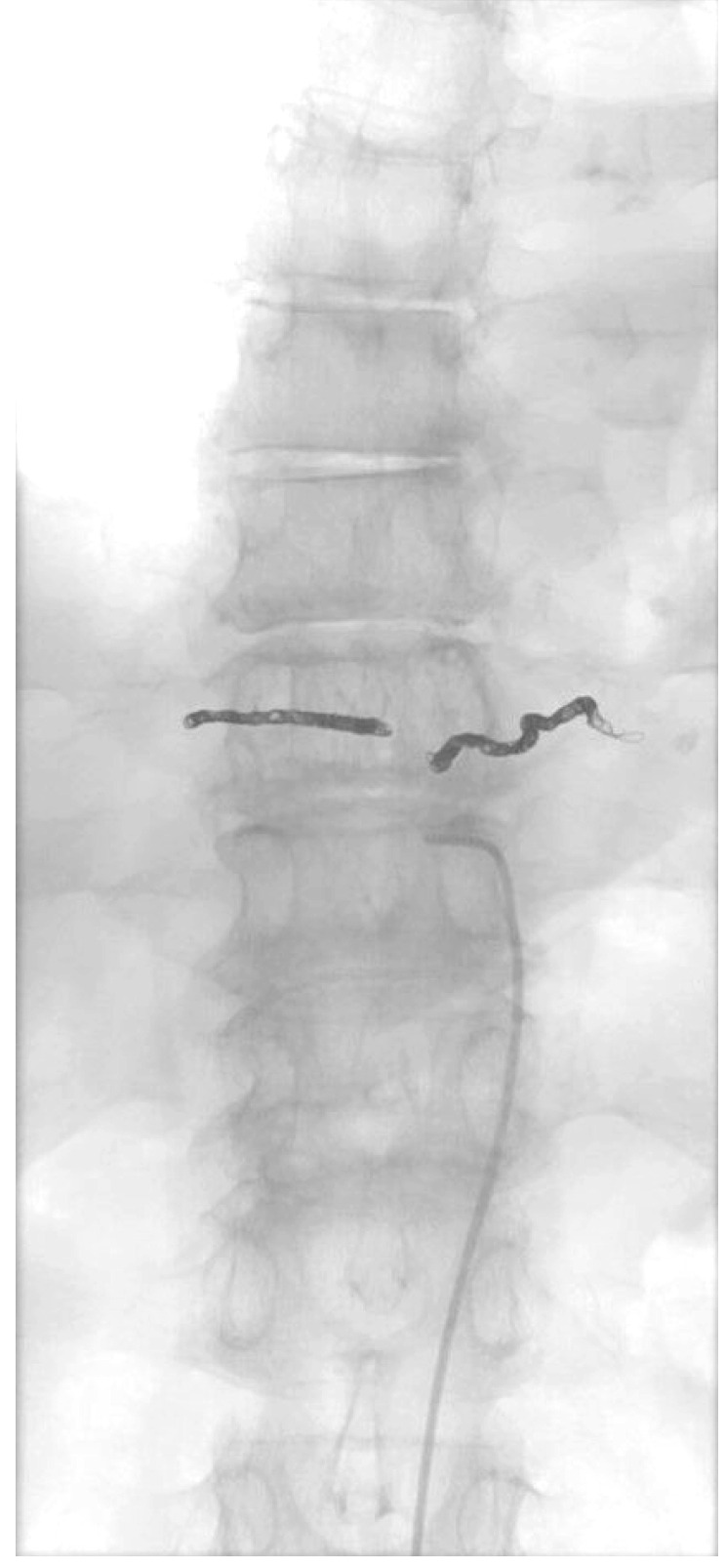
A combined endovascular and surgical approach for treatment was decided. The angiographic images demonstrated a T10 hemangioma with obvious blush within the T10 vertebral body which was supplied from bilateral segmental arteries. Arterial coil embolization was performed. Two days later, the patient underwent a T10 modified en bloc resection of the tumor with a T8-T12 stabilization/fusion. Histopathological examination revealed a soft tissue lesion composed of dilated and congested thin-walled capillaries with no wall thickening or muscular component as well as fatty replacement of vertebral bone marrow. The radiological and histological features were diagnostic of an aggressive hemangioma (Figures 5-8).
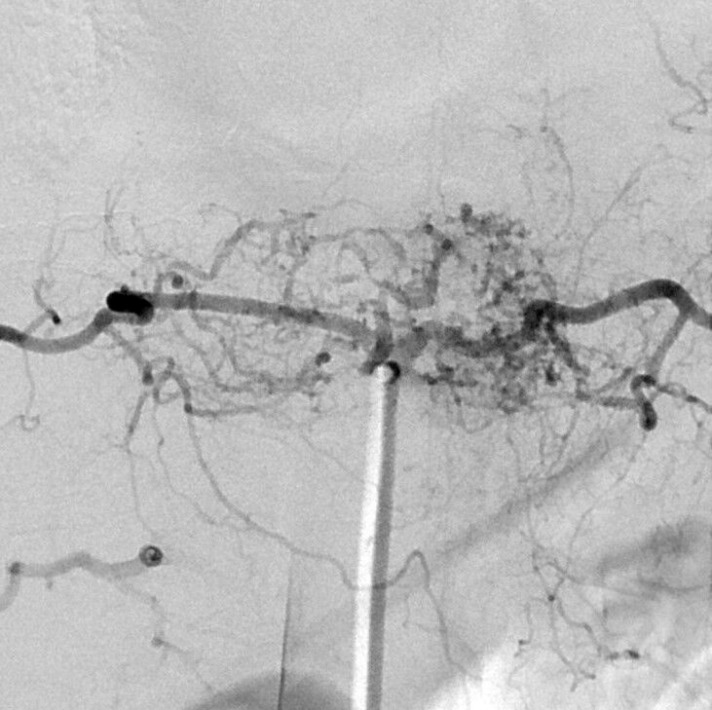
Figure 5.
Angiographic image of the lesion.
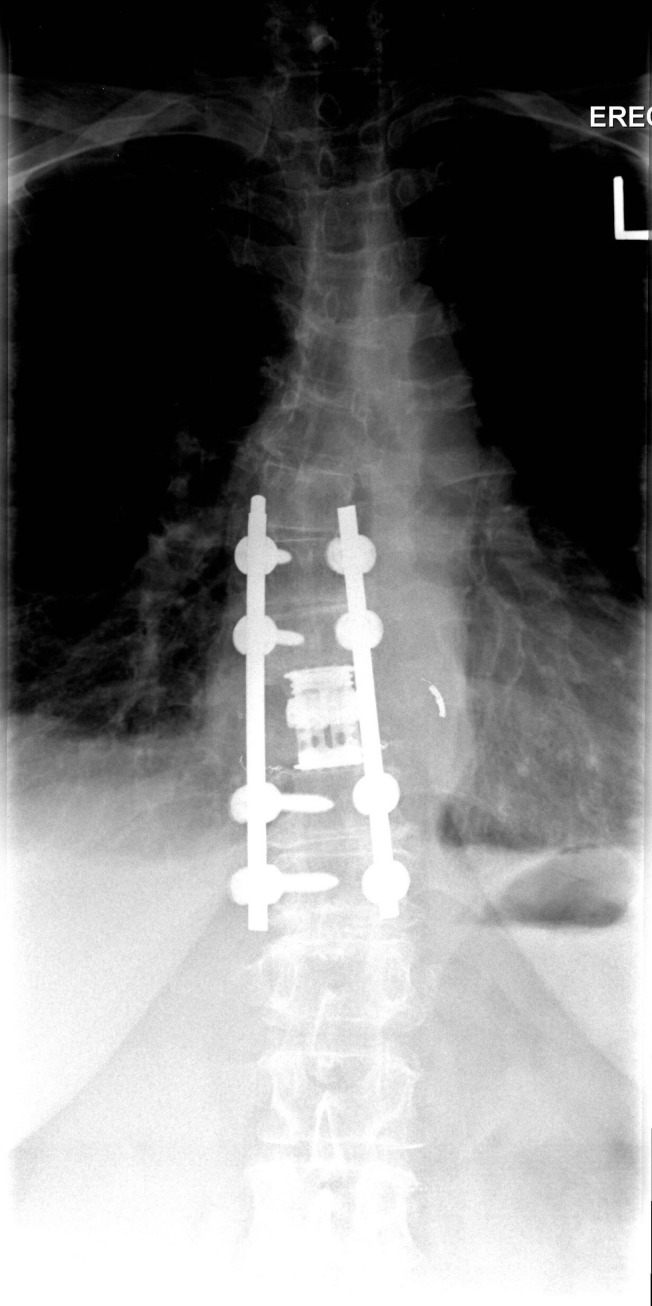
Figure 8.
Post-operative x-ray of the thoracic spine. The patient underwent a T10 en bloc resection with a T8-T12 fusion.
Figure 6.
Final result of the pre-operative embolization of the T10 vertebra.
Figure 7.
Post-operative x-ray of the thoracic spine. The patient underwent a T10 en bloc resection with a T8-T12 fusion.
Postoperatively, the patient noted a slow improvement in neurological status and at a 6-month follow-up was noted to have normal gait and balance and return of normal lower extremity sensation.
Discussion
Radiographically, VH typically present with a characteristic vertical pattern of trabecular thickening often described as jailhouse striation. In their aggressive form the entire vertebral body and neural arch is involved, with honeycomb appearance, thin vertebral cortex and soft tissue swelling. On computed tomography, the vertebral trabeculae are thickened and typically have a polka dot or salt and pepper appearance on axial imaging. On MRI, the typical forms appear hyperintense on T1- and T2-weighted images and enhance intensely on post-contrast T1-weighted, fat suppressed images while some atypical forms are hypointense on T1-weighted images but retain the T2-weighted and fat-suppressed post-contrast appearance. It should be emphasized that the typical radiological characteristics of VH and AVH may be absent in 35%, 20% and 48% of plain films, CTs and MRIs, respectively[3].
The differential diagnosis of AVH includes: metastases, solitary spine plasmacytoma, multiple myeloma, lymphoma, aneurysmal bone cyst, osteosarcoma, Paget’s disease and malignant vascular tumors such as epithelioid hemangioendothelioma and angiosarcoma. Their diagnosis can be challenging and requires a high level of suspicion and specialization and at the same time detailed work up to elucidate any primary or secondary malignancy[3]. Biopsy is a diagnostic tool in rare selected cases, but it should noted that needle biopsy carries the risk of sampling error because of the cystic nature of the lesion and adds significant risk of hemorrhage or spinal epidural hematoma.
The available literature regarding the natural history, prognosis, recurrence rates and optimal oncological and surgical treatment of AVH is very limited, although, the first description of a vertebral hemangioma with neurologic deficit was published in the 1930s[1]. Goldstein et al. in a recent multicenter study reported a local recurrence rate of 2.9%. Previous studies raised the recurrence rate up to 27.3 %[4]. Fat predominant VHs with high T1W signal/high T2W signal are generally considered inactive with good prognosis whereas those with low T1W signal/high T2W signal have a tendency to produce symptoms[3]. There are several case reports and case series described in the literature confirming these findings. In our case, although the MRI characteristics were that of a typical, benign VH (i.e. high T1W/high T2W signal), our patient presented with a severe and progressive thoracic myelopathy. To our knowledge, this case is one of the very few described where the specific MRI characteristics did not align with the clinical presentation.
The optimal treatment strategy for AVH remains controversial. Treatment options include: radiotherapy, vertebroplasty/kyphoplasty, ethanol ablation, endovascular embolization, decompressive surgery without tumor resection, subtotal or en bloc resection with various approaches and stabilization or a combination of the above. Due to the rich vascularization of the tumor the risk of surgical intervention and uncontrollable intraoperative hemorrhage is extremely high. Case reports and series in the available literature describe intraoperative blood loss of 4-5 L with or without preoperative embolization. It is generally agreed that surgical intervention through a multimodality approach with preoperative embolization offers greater efficacy with almost 100% recovery rate and extremely low mortality rate[4,5]. En bloc resection techniques that minimize or completely negate the need for intralesional resection dramatically decrease intraoperative blood loss and is our preferred surgical resection strategy.
The rarity of these cases and the fact that the literature includes small cases series with relative heterogeneity of clinical and radiological characteristics without a standardized tumor classification is the main reason that there are no well established recurrence rates or specific guidelines for treatment. This heterogeneity is further highlighted by our case, given the disparity between the MR imaging characteristics and the clinical course and emphasizes that, at present, optimal treatment of AVH should be determined on a case by case basis.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Edwin F, Lang Jr. Luigi Peserico. Neurologic and Surgical Aspects of Vertebral Hemangiomas. Surg Clin North Am. 1960;40:817–23. doi: 10.1016/s0039-6109(16)36106-0. [DOI] [PubMed] [Google Scholar]
- 2.Ben Wang, Song Bo Han, Liang Jiang, Xiao Guang Liu, Shao Min Yang, Na Meng, Feng Wei, Zhong Jun Liu. Intraoperative vertebroplasty during surgical decompression and instrumentation for aggressive vertebral hemangiomas:a retrospective study of 39 patients and review of the literature. Spine J. 2018;18(7):1128–1135. doi: 10.1016/j.spinee.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Jiang L, Liu XG, Yuan HS, Yang SM, Li J, Wei F, Liu C, Dang L, Liu ZJ. Diagnosis and treatment of vertebral hemangiomas with neurologic deficit:A report of 29 cases and literature review. Spine J. 2014;14(6):944–54. doi: 10.1016/j.spinee.2013.07.450. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein CL, Varga PP, Gokaslan ZL, Boriani S, Luzzati A, Rhines L, Fisher CG, Chou D, Williams RP, Dekutoski MB, Quraishi NA, Bettegowda C, Kawahara N, Fehlings MG. Spinal hemangiomas:results of surgical management for local recurrence and mortality in a multicenter study. Spine (Phila Pa 1976) 2015;40(9):656–64. doi: 10.1097/BRS.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 5.Viren S, Vasudeva, John H, Chi Michael W. Groff. Surgical treatment of aggressive vertebral hemangiomas. Neurosurg Focus. 2016;41(2):E7. doi: 10.3171/2016.5.FOCUS16169. [DOI] [PubMed] [Google Scholar]