Abstract
Rotator cuff repairs are associated with suboptimal outcomes and possibly greater incidence of retears if the biological healing environment is compromised. Strategies to optimize tendon–bone healing include the use of bioinductive scaffolds and regenerative stem cell therapy. The subacromial bursa has been shown to have significant pluripotent stem cell potency for tendon healing and has the advantage of easy accessibility and no added cost. However, a reproducible surgical technique for bursal mobilization, harvest, and vascularity preservation has not been described. We describe our technique for vasculature-preserving bursal mobilization and harvest of the entire posterosuperior and lateral subacromial bursa, and its use in rotator cuff repair augmentation is presented. The technique involves mobilization of the bursa as a continuous layer by maintain its medial and lateral vascularity. The bursa is advanced laterally, and the “vascular bursal duvet” and cuff tendons are repaired together as a tendon–bursa unit.
Technique Video
The surgical technique is demonstrated in a left shoulder in the beach-chair position. The subacromial space is accessed via the posterior portal and the subacromial bursa is dissected and mobilized as a continuous layer. The medial and lateral attachments of the bursal layer are preserved and the bursa is mobilized. A high posterolateral portal is created and used for visualization throughout the procedure. Three to four all-suture anchors are inserted in a single-row configuration, and sutures are passed through the tendon and bursa either together or in separate passes. Sliding knots are used to secure “vascular bursal duvet” to the tendon and tuberosity. Dynamic flexion–extension and rotational assessment is finally performed to ensure correct tension on the tendon–bursa composite repair.
Rotator cuff tears are common, and arthroscopic repair often is performed routinely to restore structural integrity and symptomatic relief. Longstanding partial and complete tears are often atrophic and retracted, and associated factors (e.g. smoking, failed repairs, multiple steroid injections, etc.) add to the poor healing environment after repair. Bioinductive scaffolds have been used to provide a superior healing environment in partial rotator cuff tears, and encouraging results have been reported.1 The use of subacromial bursa as a biological augmentation tissue has been proposed and evaluated in several basic science studies; bursal tissue has been shown to have significant pluripotent stem cell potency for tendon healing and has the advantage of easy accessibility and no added cost.2,3 However, the surgical procedure has not been standardized, and a reproducible method of bursal mobilization, harvest, and vascularity preservation has not been described.
The purpose of this report is to present a surgical technique for vasculature-preserving bursal mobilization and harvest of the entire posterosuperior and lateral subacromial bursa, and its use in rotator cuff repair augmentation. The technique uses the bursal layer as a continuous sheet with intact vascular attachments, and the “vascular bursal duvet” and cuff tendons are repaired together as a tendon–bursa unit.
Surgical Technique (With Video Illustration)
Arthroscopic bursa-augmented repair is useful in high-grade partial- and full-thickness supraspinatus and infraspinatus tears, especially chronic degenerative and atrophic tears (Fig 1). The procedure is performed with the patient in standard beach-chair position, and the arm is supported by an upper-limb positioner. A 30° arthroscope (ConMed Linvatec, Largo, FL) is used via the posterior portal for diagnostic arthroscopy, the key steps and surgical pearls of the technique are summarized in Tables 1 and 2, respectively, and the steps are demonstrated in Video 1.
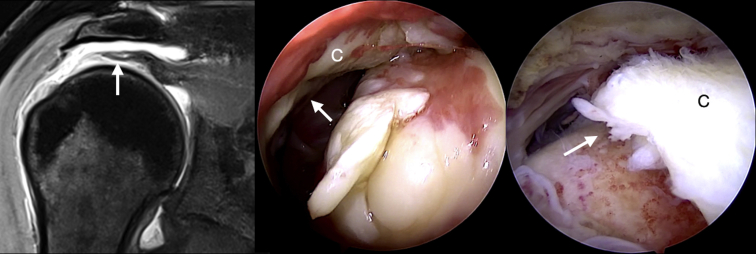
Fig 1.
Magnetic resonance image and arthroscopic view (posterior portal) of a full-thickness rotator cuff tear in a left shoulder (arrow) is shown. The torn tendon (C) is atrophic and retracted.
Table 1.
Key Steps of the Procedure
| A Thorough Diagnostic Assessment is Necessary to Assess associated Pathology. Subscapularis Tears and Biceps Lesions Necessitate Surgical Repair and Tenodesis Using Standard Techniques. |
| Subacromial space is accessed via posterior portal and subacromial bursa is preserved. |
| The subacromial bursa is dissected carefully as a thick layer from the posterior and posterolateral deltoid fascia. Medial and lateral continuity of the bursal layer is preserved, and vascular sheet along the tendon aspect (deep bursal layer) is left undisturbed. |
| Bursal layer mobility is assessed to determine best sites for suture passage for adequate bursal advancement and coverage. |
| The tuberosity and frayed edges of the torn tendons are debrided and prepared for repair. |
| Three or four all-suture anchors are used in a single-row configuration. |
| Sutures are passed from anterior to posterior through the tendons and posterior and posterolateral bursal aspects, either in a single pass or separate passes through the 2 tissues. The lateral bursal layer is left undisturbed to prevent disruption of its continuity with deltoid fascia. |
| Sutures are tied using sliding locking knots and these are then tensioned laterally. Bursal advancement and adequate tendon coverage are confirmed while sutures are tied. |
| Static and dynamic assessment of the repair is performed to confirm adequacy of repair and bursal augmentation, and to ensure that the bursal tissue is not under undue stresses that may result in bursal disruption with physiological movements in the healing period. |
Table 2.
Technical Pearls and Pitfalls
| Pearls |
| Bursal dissection should begin from medial acromial aspect and should be continued laterally. |
| The plane between the bursa and posterior deltoid fascia is used to separate and mobilize bursal tissue as a thick sheet. |
| The deep layer of bursal sheet is left undisturbed to preserve vascularity. |
| Bursal layer is tested for adequate mobility and advancement and suture passage sites are identified. |
| All-suture anchors can be inserted via a 3-mm entry hole and add to the preservation of tuberosity bone and healing environment. |
| Sutures are passed through tendon and bursa together or as separate passes at predetermined points to ensure that the bursal tissue is not under undue tension. |
| The lateral bursal continuation into deltoid fascia is left undisturbed. This aspect of the bursa is thinner and is away from the repair site. Suturing the lateral aspect may result in bursal tissue disruption. |
| Pitfalls |
| Failure to identify and treat associated lesions may result in suboptimal outcomes. |
| Aggressive subacromial resection will result in damage to the vascularity and continuity of the thicker posterior bursa. |
| Incorrect initial plane of bursal dissection may result in bursal tissue damage and bleeding. |
| Inadequate bursal mobilization or incorrect bursal suture passage results in tearing of the bursal tissue and/or inadequate tendon coverage. |
Step 1: Diagnostic Assessment and Associated Lesions
Arthroscopic evaluation is performed to identify the rotator cuff tear pattern and to assess tendon quality and reparability. Associated subscapularis tears are repaired using standard techniques, and significant biceps lesions are treated with a tenodesis procedure.
Step 2: Subacromial Space Access and Initial Bursectomy
The subacromial space is accessed via the posterior portal. Gentle debridement is performed to clear the space, and only the acromial aspect of the anterolateral bursa is excised. Care is taken to ensure that the medial, posterior, and posterolateral bursal aspects are preserved.
Step 3: Subacromial Bursal Preparation
Subacromial bursa is harvested for augmentation and mobilized to prevent restriction of range. Bursal dissection begins medially along the scapular spine and medial acromion. A radiofrequency device (Edge; ConMed Linvatec) is used at a reduced setting via a lateral portal to gently harvest the bursal tissue. The correct tissue plane is relatively avascular and dissection is extended posterolaterally. The most lateral aspect of the bursa cannot be visualized via the posterior portal and a high posterolateral portal is necessary.
Step 4: High Posterolateral Portal (HPL)
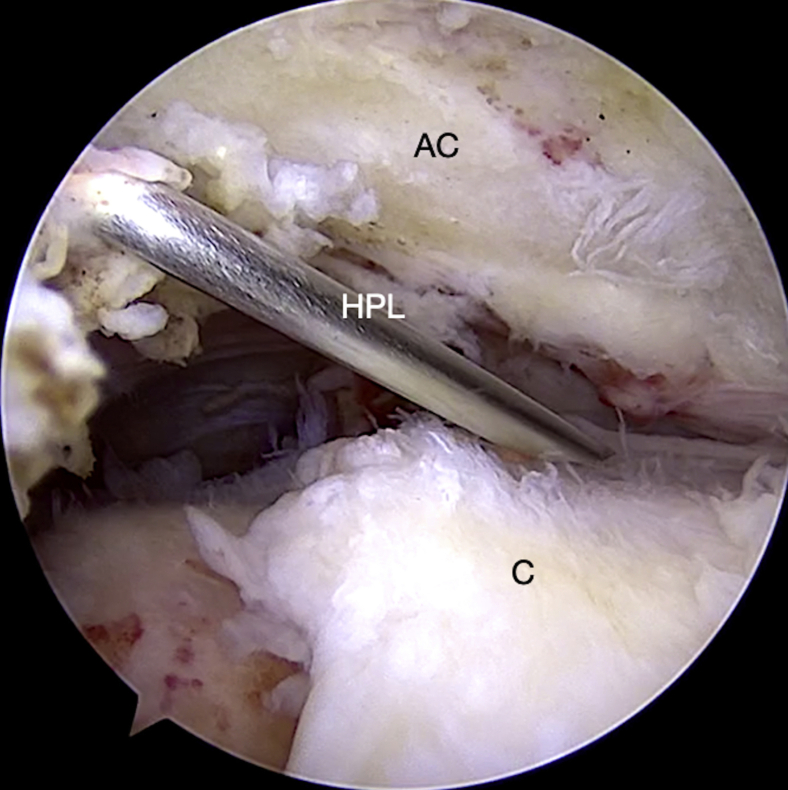
An HPL portal is created approximately 1 cm anterior to the posterolateral corner of the acromion. An outside-in technique is used and the needle should be seen passing superior to the upper border of the posterolateral bursal layer. The HPL portal facilitates further bursal mobilization and provides and unobstructed view of the rotator cuff tear for further repair (Fig 2).
Fig 2.
An HPL is created using an outside-in technique and the needle should be seen passing obliquely in a superolateral–inferomedial direction. This angulation preserves the lateral bursal attachment and provides an unobstructed view of the rotator cuff tear (C) and bursa for further repair. (AC, acromion, left shoulder; HPL, high posterolateral portal.)
Step 5: Lateral Bursal Dissection
The arthroscope is placed in the HPL portal, and dissection is continued further lateral until the bursal tissue is seen attaching to the deltoid fascia. The deep layer is visualized separately from the rotator cuff, and the vascularity on the deeper aspect can be appreciated.
Step 6: Assessment of Bursal Tissue Harvest
It is crucial to assess the bursal tissue before suture passage to ensure correct tension on the tissue; this is necessary to prevent tissue and vascular layer disruption and helps in adequate advancement of bursa for tendon coverage. The prerequisites for bursal tissue advancement include: (1) structural integrity of bursal tissue with preservation of medial and lateral attachments, (2) visualization of vascularity along the deep layer of the bursa, and (3) mobility of the bursal tissue in a posterior to anterior direction with gentle traction using an atraumatic grasper (Fig 3 and 4).
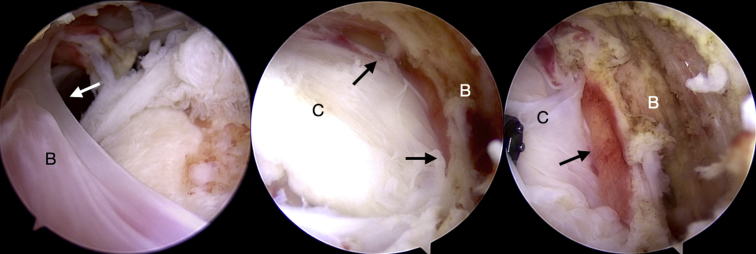
Fig 3.
Arthroscopic view through the high posterolateral portal (left shoulder) demonstrates the entire extent of the subacromial bursal layer (B) and the rotator cuff (C). The lateral attachment of B to deltoid fascia (left image) and medial attachments (middle image) are preserved (arrows). The deep vascularity (right image, arrow) along the bursal layer can be visualized.
Fig 4.
Mobility of the bursal layer (B) is assessed by applying traction at the superior edge (arrow) and assessing coverage obtained. This helps to determine suture passage points for optimal coverage of the repaired tendon. (C, torn cuff tendon, left shoulder, high posterolateral portal.)
Step 7: Tuberosity and Tendon Preparation
The greater tuberosity and frayed tendon edges are gently debrided to healthy tissue. Decortication of the tuberosity is avoided. The bursal tissue may obstruct visualization of posterior tuberosity and a Wissinger rod may be used via the posterior portal to carefully retract the bursa.
Step 8: Suture Anchor Insertion
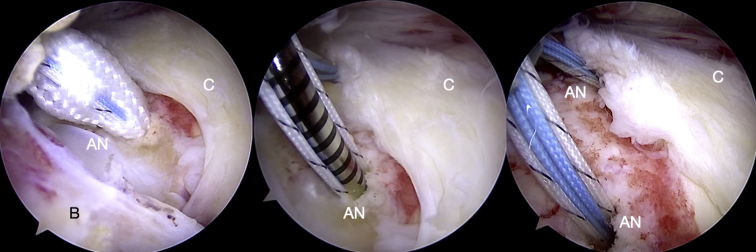
Self-punching all-suture anchors (Y-Knot RC; ConMed Linvatec) are used to minimize the insertion area (3-mm aperture) along the tuberosity. Three or four double-loaded anchors are inserted in a single-row configuration along the medial aspect of the tuberosity. The posterior anchor insertion is facilitated by retracting the bursa as described previously (Fig 5).
Fig 5.
All-suture anchors (AN) are passed along the medial aspect of the tuberosity in a single row configuration (left to right images). The 3-mm self-punching anchors help in preservation of the lateral bursal attachment (B, left image), and a small aperture is necessary thereby preserving more tuberosity bone. (C, torn cuff tendon, left shoulder, high posterolateral portal view.)
Step 9: Suture Passage Through Tendon and Bursa
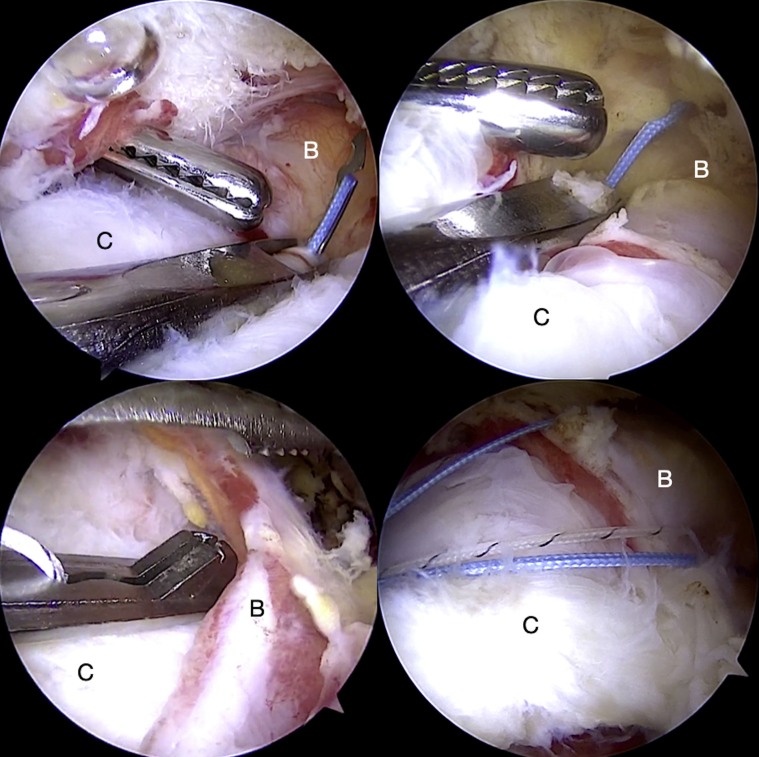
An antegrade suture-passing device is used to pass one strand of each suture through the tendon and bursa from anterior to posterior. The most anterior suture is passed through the anterior aspect of the supraspinatus tendon alone. The subsequent sutures are passed via tendon and bursal tissue in a single pass, or further posterolateral via separate passes. The bursal passage points are predetermined using mobility assessment with traction as described previously (Fig 6).
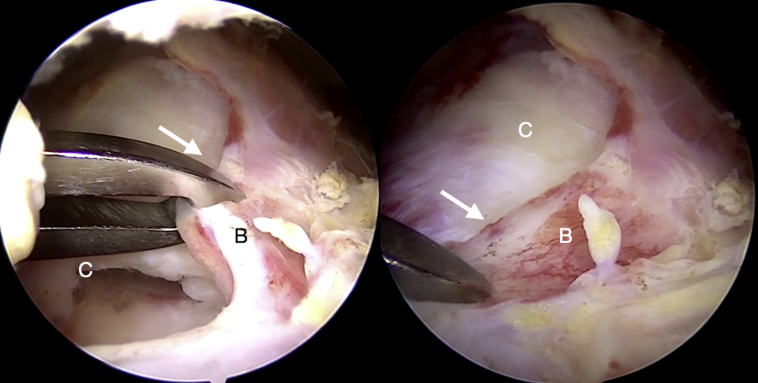
Fig 6.
Sutures are seen passing through the cuff tendon (C) and bursa (B) together as a composite (top images), and separately through the bursa alone (bottom left). Final view after passing sutures is demonstrated (bottom right, left shoulder, high posterolateral portal view).
Step 10: Knot-Tying and Bursal Advancement
Sliding locking knots (Nicky's knot) are used to secure the tendon-bursa composite to the tuberosity. The knots are shifted laterally as shown in Video 1, and this further advances the bursal tissue over the tendon.
Step 11: Final Repair Assessment
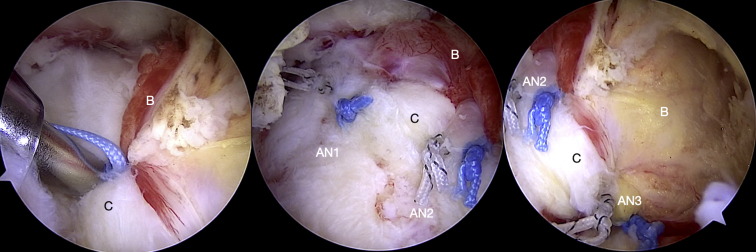
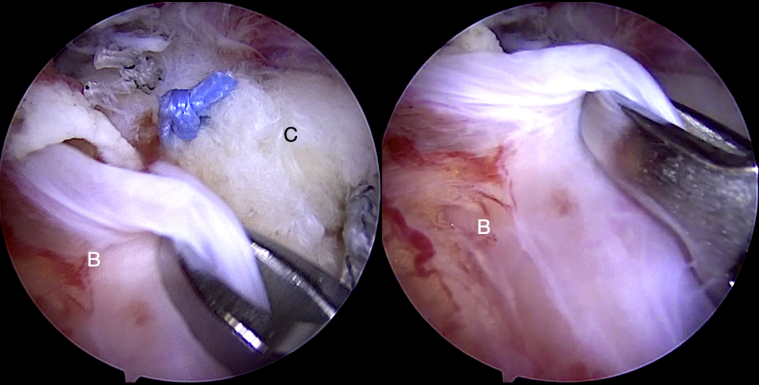
The repair integrity is visualized and probed to ensure secure fixation. The bursal tissue should be seen covering the supraspinatus and infraspinatus tendons (vascular bursal duvet) (Fig 7). Dynamic flexion–extension and rotational assessment should be performed to ensure correct tension on the tendon-bursa composite repair. The lateral bursal layer can be used to further cover the tuberosity and knots; however, this is best avoided as this lateral tissue is thinner as compared with the posterior bursa, and often results in disruption of the lateral attachment with dynamic movements (Fig 8).
Fig 7.
Sliding knots are used to advance the bursa (B) laterally over the repaired tendon (C) at its edge (left image). The final view shows the anterior (middle image) and posterior aspects (right image) of the repaired and augmented cuff tendons. The “vascular bursal duvet” is seen adequately covering the repaired tendons. (AN1, anterior anchor; AN2, middle anchor; AN3, posterior anchor, left shoulder, high posterolateral portal view.)
Fig 8.
The lateral aspect of the subacromial bursal layer (B) is thin and structurally weak (left image). This aspect of the bursa may be used to cover the repaired cuff if necessary (right image), however, there is a risk of potential disruption of this fragile layer. (C, torn cuff tendon, left shoulder, high posterolateral portal view.)
Discussion
The technique presented here describes a reproducible vasculature-preserving procedure for subacromial bursal harvest and rotator cuff tendon augmentation. The procedure involves standard instruments and anchors, and no additional implants or sutures are needed. The advantages and disadvantages of the procedure are listed in Table 3.
Table 3.
Advantages and Disadvantages
| Advantages |
| Subacromial bursa is readily available in rotator cuff repairs. |
| Standard rotator cuff repair techniques can be used for repair. |
| No special instruments or additional sutures like PDS are necessary in the repair. |
| The regenerative potential of subacromial bursa has been proven in several basic science studies. Use of subacromial bursa for augmentation provides added vascularity and structural strength to the repair. |
| Bursa-augmented cuff repair is a low-cost alternative to commercially available patches and scaffolds. |
| Disadvantages |
| Consistency of bursal tissue cannot be predicted. |
| Open rotator cuff repair techniques may not provide an adequate view of the dissection region and correct bursal harvest may be difficult. |
| Long-term benefits as compared with other augmentation tissues are not known need to be studied in a randomized control trial. |
PDS, polydioxanone.
The subacromial bursa is a consistent and readily harvestable tissue in rotator cuff repair surgery. Traditionally, arthroscopic rotator cuff repair involves a subtotal bursectomy and this was hypothesized to result in better outcomes and pain relief.4 This hypothesis has been contradicted in other studies, and a recent level 1 study has reported better outcomes with limited bursectomy.5, 6, 7, 8 The regenerative potential of subacromial bursal cells has been evaluated in basic science studies and the possible advantages of increased healing potential and better incorporation of the cuff at the tendon–bone interface have been suggested.2,3,9
The subacromial bursa extends from medial to lateral across the posterosuperior rotator cuff and is relatively thicker and structurally stronger medially and posteriorly. Bursal tissue harvest should be performed in a medial–lateral direction to avoid damage to the thinner lateral layer. The vascularity of the bursal layer is derived from the suprascapular vessels medially, and the deltoid vasculature posteriorly and laterally. Arthroscopically, the deep aspect of this layer can be observed to consist of a vascular sheet, and any use of instrumentation here results in disruption and bleeding. In addition, bursal continuity should be maintained at its medial (acromial, scapular spine, and musculotendinous) and lateral (deltoid) attachments for preserving vascularity. The entire sheet can be mobilized as a single structure and sutured to the tendon during cuff repair. Freislederer et al.10 have described a technique that involves suturing only the lateral aspect (subdeltoid) of the bursa to the cuff repair edge with PDS sutures for footprint coverage. In our experience, this lateral layer is thin and fragile as compared with the thicker posterior and posterolateral bursa and cannot be mobilized adequately for coverage of a larger area. This results in excessive stress at the bursal attachment site, as observed with dynamic testing, and bursal disruption is possible. Moreover, the fragile lateral bursa sutured to the repaired cuff edge does not contribute to the structural strength of the repair.
The technique described here has utility in partial- and full-thickness tears. In addition, bursal augmentation may also be useful as a source of vascularity and regenerative cells in reconstructive surgery for massive irreparable tears. The author has used this bursal-augmentation technique in irreparable tears in combination with partial repairs, biceps autografts, and superior capsular reconstructions. A possible disadvantage with this technique may be the inability to predict the thickness and ability to dissect an intact vascular bursal layer; however, in a large series of cases, the author has found consistent and adequate bursal tissue that can be harvested in every single case.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The surgical technique is demonstrated in a left shoulder in the beach-chair position. The subacromial space is accessed via the posterior portal and the subacromial bursa is dissected and mobilized as a continuous layer. The medial and lateral attachments of the bursal layer are preserved and the bursa is mobilized. A high posterolateral portal is created and used for visualization throughout the procedure. Three to four all-suture anchors are inserted in a single-row configuration, and sutures are passed through the tendon and bursa either together or in separate passes. Sliding knots are used to secure “vascular bursal duvet” to the tendon and tuberosity. Dynamic flexion–extension and rotational assessment is finally performed to ensure correct tension on the tendon–bursa composite repair.
References
- 1.Schlegel T.F., Abrams J.S., Bushnell B.D., Brock J.L., Ho C.P. Radiologic and clinical evaluation of a bioabsorbable collagen implant to treat partial-thickness tears: A prospective multicenter study. J Shoulder Elbow Surg. 2018;27:242–251. doi: 10.1016/j.jse.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Morikawa D., Muench L.N., Baldino J.B., et al. Comparison of preparation techniques for isolating subacromial bursa-derived cells as a potential augment for rotator cuff repair. Arthroscopy. 2020;36:80–85. doi: 10.1016/j.arthro.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 3.Dyrna F., Zakko P., Pauzenberger L., McCarthy M.B., Mazzocca A.D., Dyment N.A. Human subacromial bursal cells display superior engraftment versus bone marrow stromal cells in murine tendon repair. Am J Sports Med. 2018;46:3511–3520. doi: 10.1177/0363546518802842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chillemi C., Petrozza V., Franceschini V., et al. The role of tendon and subacromial bursa in rotator cuff tear pain: A clinical and histopathological study. Knee Surg Sports Traumatol Arthrosc. 2016;24:3779–3786. doi: 10.1007/s00167-015-3650-4. [DOI] [PubMed] [Google Scholar]
- 5.Uhthoff H.K., Sarkar K. Surgical repair of rotator cuff ruptures. The importance of the subacromial bursa. J Bone Joint Surg Br. 1991;73:399–401. doi: 10.1302/0301-620X.73B3.1670436. [DOI] [PubMed] [Google Scholar]
- 6.Põldoja E., Rahu M., Kask K., et al. Blood supply of the subacromial bursa and rotator cuff tendons on the bursal side. Knee Surg Sports Traumatol Arthrosc. 2017;25:2041–2046. doi: 10.1007/s00167-016-4379-4. [DOI] [PubMed] [Google Scholar]
- 7.Nam J.H., Park S., Lee H.R., Kim S.H. Outcomes after limited or extensive bursectomy during rotator cuff repair: Randomized control trial. Arthroscopy. 2018;34:3167–3174. doi: 10.1016/j.arthro.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 8.Feldman M.D. Editorial Commentary: When less is more-the benefits of limiting bursectomy in arthroscopic rotator cuff repair. Arthroscopy. 2018;34:3175–3176. doi: 10.1016/j.arthro.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Steinert A.F., Gohlke F. Editorial Commentary: Subacromial bursa-friend or foe within the shoulder? An old debate with new insights. Arthroscopy. 2019;35:2989–2991. doi: 10.1016/j.arthro.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Freislederer F., Dittrich M., Scheibel M. Biological augmentation with subacromial bursa in arthroscopic rotator cuff repair. Arthrosc Tech. 2019;8:e741–e747. doi: 10.1016/j.eats.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The surgical technique is demonstrated in a left shoulder in the beach-chair position. The subacromial space is accessed via the posterior portal and the subacromial bursa is dissected and mobilized as a continuous layer. The medial and lateral attachments of the bursal layer are preserved and the bursa is mobilized. A high posterolateral portal is created and used for visualization throughout the procedure. Three to four all-suture anchors are inserted in a single-row configuration, and sutures are passed through the tendon and bursa either together or in separate passes. Sliding knots are used to secure “vascular bursal duvet” to the tendon and tuberosity. Dynamic flexion–extension and rotational assessment is finally performed to ensure correct tension on the tendon–bursa composite repair.
The surgical technique is demonstrated in a left shoulder in the beach-chair position. The subacromial space is accessed via the posterior portal and the subacromial bursa is dissected and mobilized as a continuous layer. The medial and lateral attachments of the bursal layer are preserved and the bursa is mobilized. A high posterolateral portal is created and used for visualization throughout the procedure. Three to four all-suture anchors are inserted in a single-row configuration, and sutures are passed through the tendon and bursa either together or in separate passes. Sliding knots are used to secure “vascular bursal duvet” to the tendon and tuberosity. Dynamic flexion–extension and rotational assessment is finally performed to ensure correct tension on the tendon–bursa composite repair.