Abstract
Injuries to the knee involving multiple ligaments occur in a variety of circumstances and require careful assessment and planning. A wide constellation of injuries can occur with causes sufficiently traumatic to produce bicruciate ligament deficiency, and this technical report will describe diagnosis, treatment and rehabilitation for a knee dislocation with lateral injury (KD-III-L on the Schenk classification). Reconstruction in the acute setting is preferred, with anatomic-based, single-bundle anterior cruciate ligament reconstruction, double-bundle posterior cruciate ligament reconstruction, and anatomic reconstruction of the posterolateral corner using two grafts for the 3 primary posterolateral corner stabilizers. Tunnel orientation to prevent convergence and sequence of graft tensioning and fixation are discussed as well. Successful outcomes have been achieved using these anatomic-based reconstruction techniques along with appropriate rehabilitation and bracing.
Technique Video
Repair of bicruciate ligament injury with grade III posterolateral corner tear. Examination under anesthesia is consistent with KD-III-L injury. Dissection of biceps femoris tendon (BFT) and common peroneal nerve (CPN) is performed through a lateral hockey stick incision. A fibular tunnel is drilled first, then a tibial tunnel for the popliteus tendon (PLT) and popliteofibular ligament (PLT). Femoral tunnels for the PLT and fibular collateral ligament (FCL) are drilled, oriented 35°anteromedially. Bone-patellar tendon-bone autograft is then harvested. After diagnostic arthroscopy, the PCL anterolateral bundle (ALB) and posteromedial bundle (PMB) tunnels are drilled, then the anterior cruciate ligament (ACL) femoral tunnel. A tibial guide pin is placed, confirmed with fluoroscopy, then a tunnel reamed and a large smoother passed. The ACL tibial tunnel is then reamed. The PMB graft of the PCL is passed first and secured, then the ALB. The ends of both bundles are passed down the tibial tunnel using the smoother. The ACL femoral graft is pulled into place and secured. The femoral ends of the FCL and PLT grafts are then secured. The FCL graft is passed under the iliotibial band (ITB) and through the fibular head tunnel. PCL grafts are then fixed on the anterior tibial cortex with screws and washers; ALB in 90° flexion and PMB in extension. This eliminated the posterior drawer. The ACL graft is then secured on the anterior tibia. The FCL graft is then secured in the fibular head tunnel with a screw at the anterior aperture. The PLT and PFL grafts are then passed from posterior to anterior through the tibial PLC tunnel and secured with a screw. Suture anchors are used to repair the lateral capsule and biceps femoris tendon, and the ITB repaired. Closure completes the procedure.
Multiple ligament knee injuries often occur in the setting of knee dislocation with disruption of one or both cruciate ligaments (anterior cruciate ligament [ACL] and posterior cruciate ligament [PCL]) and one or both of the fibular collateral ligaments (FCL) and medial collateral ligaments. Injuries to the posterolateral corner (PLC) or posteromedial corner (PMC) structures, and to associated structures like the biceps femoris and common peroneal nerve, are also common. Multiligament knee injuries may also occur without concomitant knee dislocation, which typically involves tear of one or both cruciate ligaments (Table 1).1,2
Table 1.
The Schenck Knee Dislocation Classification System (Medial Sided)1
| Schenck Knee Dislocation Classification (KD) |
| KD-I |
| KD-II |
| KD-III-M |
| KD-III-L |
| KD-IV |
| KD-V |
| Description of Injury |
| Multiligament injury with single cruciate ligament injury (ACL or PCL) |
| ACL and PCL involvement |
| Injury to both ACL and PCL with additional medial injury (medial collateral ligament) |
| Injury to both ACL and PCL with additional lateral injury (fibular collateral ligament) |
| ACL + PCL and MCL + FCL injury (both cruciate ligaments and both collaterals) |
| Same as KD-IV with peri-articular fracture |
ACL, anterior cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
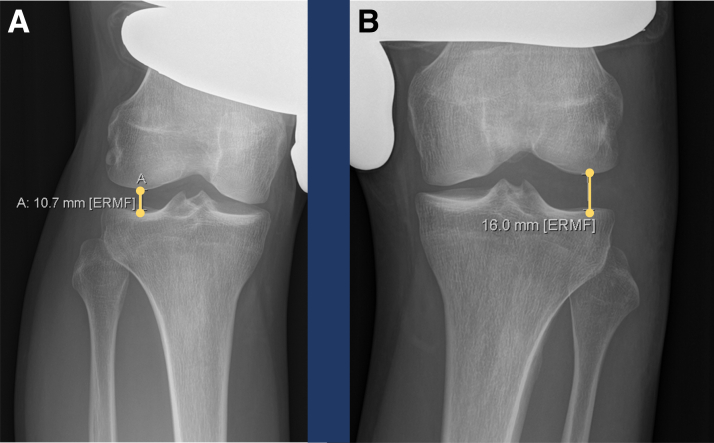
Multiple ligament knee injuries may occur with knee dislocations in high-energy traumatic causes, low-energy mechanisms like athletic injuries, or in ultra-low velocity injuries, seen in the severely obese.1, 2, 3 These are complicated conditions to assess and treat, because diverse combinations of injury may be seen to the ligaments, tendons, and neurovascular structures of the knee. Advanced trauma and life support and assessment of vascular status may be necessary because of the frequency of vascular injuries in knee dislocation and the traumatic etiology of many of these injuries.1,2 A thorough physical examination and multimodal imaging evaluation is required. Lachman, posterior-drawer, varus, valgus and rotational testing are useful to determine the nature and scope of injuries, and supplementation with posterior, varus, and valgus stress radiographs provides an accurate picture of the integrity of major stabilizing ligaments (Figs 1 and 2).4, 5, 6 A foot-drop indicates common peroneal nerve involvement. Magnetic resonance imaging is additionally used to detect concomitant meniscal, nervous, muscular, or other injuries and bony edema and cartilage damage (Fig 3).2
Fig 1.
Kneeling posterior stress x-rays: Posterior stress x-rays are a validated method for examining posterior translation of the tibia. The patient is instructed to kneel on some surface with the tibial portion of the joint line at an edge. Posterior displacement is measured by drawing a line along the posterior tibial cortex (from a point roughly 8 cm distal to the joint line) through the intercondylar notch. The point from this line to the posterior-most point of Blumensaat’s line is measured to assess laxity. A 0 to 4 mm side-to-side difference is expected in a normal patient. Isolated posterior cruciate ligament (PCL) injuries may display 5 to 12 mm increased posterior displacement compared to the uninjured contralateral knee. Patients with >12 mm posterior displacement of the injured knee compared to the contralateral side may have combined injuries to the PCL, posterolateral corner (PLC), or posteromedial structures. In the above patient, the increase in posterior displacement between the injured left knee in (B) and the uninjured right knee (A) is 4.6 mm.
Fig 2.
Varus stress radiographs are a validated method to assess for fibular collateral ligament (FCL) and posterolateral corner (PLC) injuries. Proper technique in taking the radiograph is essential. Increased side-to-side difference with clinician-applied varus gapping of 2.2 to 2.7 mm should raise suspicion of a complete FCL tear or grade III posterolateral corner injury if gapping is increased more than 4.0 mm on the injured side compared to the uninjured side. In the above images, 16.0 mm gapping is measured with varus stress on the injured left knee (A), whereas 10.7 mm is measured on the uninjured right side (B). This difference of 5.3 mm may indicate complete (grade III) posterolateral corner injury.
Fig 3.
Preoperative magnetic resonance imaging (MRI) demonstrates extensive injuries around a patient’s left knee. Multiple ligamentous injuries around the knee often occur in the setting of knee dislocation, either in sports or trauma, and may entail damage to ligaments, tendons, capsular structures, and nervous and vascular structures. When life-threatening injuries and vascular compromise have been ruled out, MRI is performed in addition to x-radiography to fully assess the extent of the damage. Images (A) and (B) are sagittal proton dense (PD) views of the left knee, demonstrating acute disruption of the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) [yellow arrows]. The PCL tibial facet is indicated by “CGD,” for the champagne glass drop-off. Images (C) and (D) are axial PD images from the same left knee. (C) Capsular and popliteus tendon (PLT) disruption in the posterolateral corner with a yellow arrow. (D) PLT rupture at the popliteus sulcus attachment on the lateral femoral condyle. (E) A coronal T2 PD fat-suppressed (FS) image, which shows increased signal intensity around the posterolateral corner (arrow) and tear/avulsion of the biceps femoris tendon (BFT). (F) A coronal PD image demonstrating complete fibular collateral ligament disruption (yellow arrow).
This Technical Note will describe an anatomic reconstruction of a knee dislocation with multiple ligamentous injuries and posterolateral corner involvement (KD-III-L on the Schenk classification) (Table 1). Reconstruction has been reported to be superior to repair in addressing these injuries, with improved outcomes for surgical intervention in the acute stage.7 Although there has been some past controversy regarding whether to reconstruct the popliteofibular ligament (PFL), improved outcomes have been reported with PFL reconstruction, using 2 grafts for the 3 chief PLC stabilizers (FCL, popliteus tendon [PLT], and PFL).8
Graft Preparation
A bone-patellar tendon-bone ACL autograft is preferred,9,10 with 2 passing sutures for each bone plug, and the grafts sized for 10 mm reconstruction tunnels. Double-bundle PCL reconstruction is performed with an 11 mm Achilles tendon allograft for the anterolateral bundle (ALB), and a 7 mm tibialis anterior allograft for the posteromedial bundle (PMB).11 The ALB Achilles tendon graft has a proximal 11 × 20 mm bone plug and distal tubularized end. The PMB tibialis anterior allograft is whipstitched at each end. The FCL, PLT, and PFL are reconstructed with a split Achilles tendon autograft, each piece with a 9 × 20 mm bone plug.12
Tunnel Orientation
Three-dimensional modeling studies have been performed to determine optimal orientations of femoral bone tunnels to avoid convergence.13, 14, 15 For lateral-sided multiligament reconstructions, the FCL and PLT tunnels are most at risk of convergence with the single ACL tunnel. Both the FCL and PLT tunnels should be aimed 35° to 40° anteriorly, parallel with one another to avoid convergence with the ACL tunnel.
Surgical Technique
A narrated walkthrough of the procedure is given in Video 1. The patient is brought into the operating room, placed supine, and induced with general anesthesia, and a high thigh tourniquet is applied. Examination with the patient under anesthesia should compare heel height/hyperextension, range of flexion, posterior and posterolateral drawer, Lachman’s, pivot shift, and dial tests, both in extension and at 30° of flexion, as well as assessment of the proximal tibiofibular joint.
Open procedures are recommended to better assess the extent of damage; the posterolateral approach with a standard hockey-stick incision is performed first to visualize the structures before fluid extravasation. A very meticulous dissection over the superficial layer of the iliotibial band (ITB) and along the inferior aspect of the biceps femoris tendon should be performed, with caution during the approach for the peroneal nerve. The nerve should be dissected proximally and distally and carefully retracted from the operative field (Fig 4).
Fig 4.
Dissection of the biceps femoris tendon (BFT). In multiligament and posterolateral corner (PLC) injuries, the distal aspect of the biceps femoris tendon must be carefully dissected out. The common peroneal nerve (CPN) can slip proximally if the BFT is avulsed, and scar tissue can obscure its location. In the above left knee KD-III-L injury, the CPN has previously been dissected and lies beneath the BFT. A split portion of the iliotibial band (ITB) is retracted; forceps are being used to elevate a torn portion of the lateral capsule (Lat Caps). Under the elevated capsular flap, an instrument is being used to point to the underside of the lateral meniscus (LM), which has suffered avulsion off of the lateral tibial plateau.
The status of structures about the fibular head should then be assessed after developing an interval between the lateral gastrocnemius head and soleus. A collateral drill guide (Extra-Articular Reconstruction [EAR] fibular set; Smith & Nephew) is used to place a guide pin from the anatomic FCL attachment to the posteromedial aspect of the fibular head and overreamed with a 7 mm reamer. A passing stitch is then placed.
A tibial drill guide (EAR Set; Smith & Nephew) is used to place a guide pin for the tibial PLC tunnel, starting from the flat spot distal and medial to Gerdy’s tubercle and emerging 1 cm medial and 1 cm proximal to the posteromedial opening of the fibular head tunnel (Table 2). A passing stitch is placed after the pin is overreamed with a 9 mm reamer while a large Chandler retractor protects the neurovascular structures.
Table 2.
Pearls and Pitfalls
| Pearls |
| Perform Posterolateral approach first to visualize the anatomy before fluid extravasation |
| If the peroneal nerve is damaged, do not completely dissect to avoid further neuropraxia |
| When drilling the tibial tunnel, place a probe inside the fibular head tunnel to serve as a guide for the posterolateral emergence of the drill from the tibia |
| Use a large Chandler retractor with a finger behind it to protect the neurovascular bundle when drilling tunnels around the PLC |
| A small sulcus can be palpated at the anatomic FCL attachment on the fibular head, located within the BF bursa |
| Make sure to reduce the biceps tendon for repair in full extension—this may require releasing some of the short head from the capsule |
| A “drive-through sign,” or interval between the lateral femoral condyle and PLT, indicates femoral avulsion of the PLT |
| Ream the last 40% of the tibial PCL tunnel by hand to ensure it emerges correctly, and use a large curette to protect the joint |
| Repair BF Tendon after PLC reconstruction to avoid convergence between suture anchors and PLT/PFL tunnel |
| Pitfalls |
| Scarring and an avulsed BF tendon can make the location of the common peroneal nerve unpredictable |
| Normal landmarks may not be palpable depending on the extent of damage |
| Reaming the fibular head tunnel too proximally risks fracture or blowout |
| Graft preparation should begin before the case, otherwise it may take significantly longer |
| Avoid blowout by maintaining a 2 mm backwall when reaming the femoral ACL tunnel |
| Continuously check softness of calf to ensure fluid extravasates out of joint and not into leg compartments |
| The tourniquet should be let down at 2 hours |
| Hematoma at the head of the fibula can put pressure on the common peroneal nerve and lead to foot drop; postoperative cryotherapy can help prevent excessive swelling. |
| If the PLC tibial guide pin is too lateral, it can enter the anterior compartment musculature or the PTFJ, particularly if the patient is obese |
ACL, anterior cruciate ligament; BF, biceps femoris; FCL, fibular collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner; PLT, popliteus tendon; PTFJ, proximal tibiofibular joint.
The ITB is then split in line with its fibers, 4 cm anterior to the femoral FCL attachment (Table 3). A Z-retractor is used to locate the PLT attachment through this interval. A collateral instrument guide (EAR; Smith & Nephew) is used to drill a guide pin anteromedial through the center of the attachment. The femoral FCL attachment is located 18.5 mm posterior to the PLT attachment, and a guide pin is drilled parallel to the PLT attachment. A 9 mm reamer is used to overream both of these to a depth of 25 mm, and passing sutures are placed (Fig 5).
Table 3.
Anatomic Attachments and Landmarks
| Ligament/Tendons | Anatomic Attachment |
|---|---|
| FCL | Femoral: 1.4 mm proximal and 3.1 mm posterior to lateral epicondyle Fibular: 8.2 mm posterior to anterior margin of the fibular head, 28.4 mm distal to the tip of the fibular styloid |
| PLT | Femoral: tendon attaches 18.5 mm anterior to FCL in anterior 1/5 of popliteal sulcus |
| BF Tendon | Tendon has direct attachments of long and short heads on fibular head. Common BF tendon attaches to posterolateral aspect of fibular styloid |
| ACL | Femoral: 8.5 mm anterior to posterior cartilage margin, 1.7 mm proximal to the bifurcate ridge, 14.7 mm proximal to the distal cartilage margin, 6.1 mm posterior to the lateral intercondylar ridge Tibial: 7.5 mm medial to the anterior horn of the lateral meniscus |
| PCL | Femoral: ALB: Between trochlear arch and medial arch point PMB: 8-9 mm posterior to articular cartilage Tibial: 6-7 mm above champagne glass drop-off. Avoid shiny white fibers of posterior medial meniscus root. Aligned with medial border of lateral tibial eminence |
ACL, anterior cruciate ligament; BF, biceps femoris; FCL, fibular collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner; PLT, popliteus tendon.
Fig 5.
Lateral femoral condyle tunnels in reconstruction of posterolateral corner (PLC) structures are created by drilling two guide pins through the femur to mark the anatomic locations of the fibular collateral ligament (FCL) and popliteus tendon (PLT). Anatomic reconstructions of multiple ligamentous injuries and PLC injuries result in more normal knee kinematics and faster recovery of range of motion and muscle strength. (A) The iliotibial band (ITB) is split, and a z-retractor used to expose the anatomic PLT attachment and drill a guide pin. (B) A collateral ligament guide is used to drill a guide pin for the femoral FCL tunnel. (C) Measurement demonstrating 18.5 mm distance between the anatomic PLT and FCL lateral femoral condyle attachments.
The patellar tendon autograft is then harvested. An anterior incision from the proximal patella to the medial tibial tubercle is made and the paratenon is dissected off medially and laterally for a later repair. A central third tendon autograft with a 10 × 20 mm patellar bone plug and 10 × 25 mm tibial bone block is harvested and prepared as described earlier. The tendon is closed, and the patellar defect is bone-grafted later in the case.
Medial and lateral portals are made and diagnostic arthroscopy is performed. The anatomic center of the PCL ALB is found 7.4 mm from the trochlear point and 11.0 mm from the medial arch point. The PMB center is 12 mm from the ALB center in a line parallel to the medial intercondylar ridge. An 11 mm reamer is used for the PCL ALB and a 7 mm reamer for the PMB, with passing sutures placed. An ACL femoral tunnel is reamed using a 10 mm reamer, 25 mm deep, while the knee is held in 120° of flexion, keeping at least a 2 mm backwall.1 The anatomic center of the ACL is 1.7 mm proximal to the bifurcate ridge and 6.1 mm posterior to the lateral intercondylar ridge (Fig 6).
Fig 6.
Anatomic single bundle anterior cruciate ligament (ACL) reconstruction and double bundle posterior cruciate ligament (PCL) reconstruction is shown via arthroscope in a left knee in this image. Single-bundle ACL reconstruction restores normal kinematics to the knee, but double bundle PCL reconstruction is required for normal joint function. The femoral ACL tunnel is placed through the lateral aspect of the intercondylar notch, in between the anatomic attachments of the anteromedial and posterolateral bundles. A guide pin is placed first, then overreamed to a depth of 25 mm with a 10 mm reamer, maintaining a 2 mm backwall. In this image, an arthroscopic shaver is being used to hold the passing sutures in the PCL tunnels to protect them from the ACL reamer.
A posteromedial arthroscopic portal is then made and the PCL footprint outlined. The aid of a 70° arthroscope may be helpful. A PCL tibial guide pin is drilled using a cruciate instrument guide (Arthrex) from 6 cm distal to the anteromedial joint line, emerging at the PCL facet, and its placement is confirmed fluoroscopically (Fig 7). The pin is overreamed with a 12 mm reamer 60% of the transtibial distance, with the remaining distance reamed by hand. A large curette is held posteriorly to protect against overpenetration (Table 2). A large smoother (Gore Smoother Crucial Tool; Smith & Nephew) is passed through the tibial PCL tunnel to ease graft passage and then the end of the smoother is passed out of the anterolateral arthroscopic portal. The ACL tibial footprint is then identified, and a tibial ACL guide (Arthrex) is used to drill a guide pin in the center of the footprint, adjacent to the anterior root of the lateral meniscus, and then overreamed with a 10 mm acorn reamer (Arthrex).
Fig 7.
Intraoperative fluoroscopy during posterior cruciate ligament (PCL) reconstruction is used to ensure proper placement of the PCL tibial tunnel. Double-bundle PCL reconstruction has been demonstrated to be superior in restoring native knee kinematics over single bundle reconstruction. The anterolateral bundle and posteromedial bundle (ALB and PMB) grafts are secured in two femoral tunnels, but both grafts are attached to the tibia through one transtibial tunnel. The tibial PCL tunnel is drilled from the anterior aspect of the tibia (midway between the anterior tibial crest and the medial border of the tibia) and emerges between the anatomic ALB and PMB centers on the tibial PCL facet, just superior to the champagne glass drop-off. As indicated, a 7 mm back wall should be maintained. The tibial tunnel is drilled at roughly a 45° angle with the long axis of the tibia, often determined using a two line method (dashed lines).
Graft Passage
The PMB PCL allograft is passed first into its femoral tunnel using the passing stitch through the anterolateral portal and secured with a 7 × 20 mm bioabsorbable screw (Biosure; Smith & Nephew). The bone plug for the ALB is then passed and secured in the femoral tunnel with a 7 × 20 mm titanium screw (Softsilk; Smith & Nephew). The PMB and ALB suture ends are then passed into the end of the Gore smoother and passed down the tibial tunnel (Fig 8). The sutures prepared through the ACL femoral graft bone block are passed through the loop of the passing suture in the femoral tunnel, which is pulled out from the lateral thigh. The femoral bone plug suture ends are pulled to advance the graft into the femoral tunnel. The ACL graft is then secured in the femoral tunnel with a 7 × 20 mm titanium screw (Smith & Nephew). The bone plugs for the FCL and PLT grafts are then pulled into their femoral tunnels by looping the sutures left in the bone plugs through passing sutures left through the tunnels. The grafts are then secured in the femoral tunnels with 7 × 20 mm cannulated titanium screws (Smith & Nephew) threaded over a guide pin aimed between the surface of the plugs and the tunnel margin. The FCL graft is passed under the ITB and then through the fibular head tunnel using the passing suture left in place. The PCL grafts are then secured on the tibia with 6.5 mm titanium screws and washers (Arthrex) after cycling the knee to remove slack: the ALB first at 90° of flexion and then the PMB in extension. The posterior drawer sign should now be absent, and the ACL graft should not have any slack when viewed arthroscopically. The ACL tibial graft is then secured with a 9 × 20 mm titanium screw in full extension. Verify intraarticular bicruciate fixation arthroscopically, with no graft bunching or roof impingement. Next the distal FCL graft is secured in the fibular head (exiting the posteromedial fibular tunnel) with the knee flexed to 20°, a slight varus force and traction on the graft with a 7 × 20 mm bioabsorbable screw. The PLT and PFL grafts are now passed from posterior to anterior through the tibia, with caution to avoid the common peroneal nerve, and secured with a 9 × 20 mm bioabsorbable screw anteriorly (Figs 9 and 10).1,16
Fig 8.
Distal posterior cruciate ligament (PCL) graft passage using a smoothing tool (Sm) in a left knee. During double bundle PCL reconstruction, the anterolateral bundle (ALB) and posteromedial bundle (PMB) are separately reconstructed to better restore native joint mechanics. A smoothing tool is passed up a tibial tunnel from the anterior tibial cortex from 6 cm distal to the anteromedial joint line to the PCL facet posteriorly, and out the anterolateral portal. (A) Sutures through the distal ends of the ALB and PMB grafts are first passed through the looped end of the smoother tool (Loop) while held exterior to the anterolateral portal. The grafts are then pulled back into the joint by traction on the smoother (B), then pulled from posterior to anterior through the tibial tunnel and out the tibial tunnel anteriorly (C). Dashed lines indicate direction of motion.
Fig 9.
Anterior and lateral aspects of a left knee after graft passage during posterolateral corner (PLC) reconstruction. Anatomic posterolateral corner reconstruction is accomplished by restoring all 3 stabilizers of the posterolateral corner of the knee; the fibular collateral ligament (FCL), popliteus tendon (PLT), which functions as a ligament in the knee, and the popliteofibular ligament (PFL). Two split Achilles tendon grafts are used, with 2 femoral tunnels, 1 fibular head (FH) tunnel, and 1 tibial (Tib) tunnel. The FCL and PLT grafts are secured on the femur with interference screws. The FCL graft is secured in the fibular head with an interference screw as it passes through the fibular head tunnel and becomes the PFL graft. The PFL and PLT grafts are then passed posterior to anterior through the tibial tunnel, and can be seen emerging anteriorly (PLC, PLT, PFL). The portion of the PLT graft secured to the femur is not visible 18.5 mm anterior to the FCL attachment to the femur. The tibial ends of a double bundle PCL graft can also be seen emerging anteriorly (Achilles tendon graft for anterolateral bundle, tibialis anterior graft for the anteromedial bundle). The lateral meniscus (LM) can also be seen through a rent in the lateral capsule (Lat Caps). The common peroneal nerve (CPN) can displace significantly in PLC injuries, partly because of avulsion of the biceps femoris tendon (BFT).
Fig 10.
Order of graft fixation. When performing reconstruction of extensive injuries around the knee involving both cruciate ligaments and lateral-sided structures, fixation and tensioning of grafts should follow the general order: posterior cruciate ligament (PCL), then anterior cruciate ligament (ACL), and then posterolateral corner (PLC). A more in-depth look at when to secure grafts in femoral tunnels, pass through transosseous tunnels, and secure grafts in their respective tibial fixation points is given in this flow-chart. The heading boxes indicate ACL, PCL, or PLC, and the text boxes indicate what part of those structures and what fixation or graft passages are performed.
If lateral meniscus or capsular pathology is present, 2 suture anchors in the lateral capsule can now be used at this stage to repair these injuries. The biceps femoris tendon is now repaired in full extension to the fibular head and styloid process with 2 suture anchors (Q-Fix; Smith & Nephew). The ITB is then repaired in a manner dependent on the injury with side-to-side sutures or suture anchors.
Physical examination maneuvers should now be normal, without excessive graft or suture tension, and excess grafts and passing sutures are now removed. Deep tissues are closed after hemostasis with 0 and 2-0 Vicryl sutures, followed by Monocryl skin stitch. Steri-Strips are loosely applied, then sterile dressing and a knee immobilizer.
Rehabilitation
Patients remain nonweightbearing after surgery for 6 weeks with a knee immobilizer. With PCL involvement, a dynamic PCL rebound brace should replace the immobilizer when swelling has resolved enough for proper fit, ideally by postoperative day 3 to 5.17 Physical therapy begins on postoperative day 1. Baseline lateral and anteroposterior radiographs are obtained at that time as well and deep venous thrombosis prophylaxis is followed for 2 weeks with enoxaparin before transitioning to aspirin and thrombo-embolic deterrent (TED) hose until initiation of full weightbearing at 6 weeks after surgery (Fig 11). Patients perform routine cryotherapy immediately after surgery to manage pain and swelling. Early therapy focuses on patient education, pain and swelling control, patellar mobilizations, protected range of motion (ROM), and quadriceps muscle activation. LaPrade et al.18 demonstrated that knee stability was restored in a large cohort of patients after single-stage multiple-ligament reconstruction using a protocol that initiated ROM immediately after surgery. With PCL involvement, ROM is initiated passively with the patient in the prone position to minimize posterior tibial translation. Knee flexion is limited to 90° for the first 2 weeks with all procedure types and knee hyperextension is avoided with PLC and PCL involvement to minimize early strain on the grafts. Patellofemoral joint mobilizations and peripatellar soft tissue mobilizations along with frequent quadriceps contractions, which create proximal patellar translation, help minimize postoperative stiffness, which is a critical first step for maximizing recovery and long-term joint health.19, 20, 21 In the case of biceps femoris repair, hamstring muscle strengthening should be delayed for the first 8 weeks to minimize disruption of initial tendon healing at the attachment site, then gentle isometrics may begin, followed by graduated loading progressions to stimulate the healing process. Resisted hamstring curling into knee flexion is prohibited until 4 months after surgery with PCL and PLC reconstructions to avoid excessive posterior tibial translation.22,23 A thoughtful approach with early quadriceps strengthening should be followed per the involved ligaments, respecting that quadriceps activation in deeper flexion (>60°) induces slight posterior tibial translation and activation into terminal knee extension (30° to 0°) induces more pronounced anterior translation.22, 23, 24, 25 Later progressions with therapy are individualized per patient and generally address muscle strength, joint proprioception and postural stability, cardiovascular fitness, and athletic function. The use of neuromuscular electrical stimulation and blood flow restriction therapy are advocated to facilitate maximal recovery of muscular strength and reverse any potential loss of bone density after an extensive period of restricted weightbearing and reduced physical activity in the immediate postoperative period.26, 27, 28, 29, 30, 31 Serial physical performance testing is useful on 3- to 4-month intervals after surgery to assess patient recovery in all domains and guide decision making for return to activity and sport.
Fig 11.
Left knee radiographs, (A) anteroposterior, (B) lateral. Postoperative radiographs after reconstruction of anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), fibular collateral ligament (FCL), popliteus tendon (PLT), and popliteofibular ligament (PFL). Single-bundle ACL reconstruction restores normal joint function, and bone-patellar-tendon bone autograft is preferred in healthy, active adults. Double-bundle PCL reconstruction is performed to better restore the normal functioning of the posteromedial and anterolateral PCL bundles. Anatomic posterolateral corner reconstruction. In the above image, the titanium screws and washers of ACL and PCL reconstruction can be easily visualized, as well as the titanium femoral fixation screws of the FCL and PLT. Bioabsorbable screws are used for fibular head tunnels, and these are more difficult to distinguish for the distal posterolateral corner (PLC) points of fixation. ACL screws = green letters and arrows, PCL screws = blue letters and arrows, PLC screws = yellow letters and arrows.
Discussion
Historically, there was some debate over whether to address MLI knee injuries in the acute phase or wait for subsidence of swelling. Multiple systematic reviews have reported significantly improved outcomes with acute surgical intervention, less than 3 weeks from injury, along with 1-stage surgery and commencement of early range of motion after surgery.7,18,32,33
For PCL-reconstructions, the double-bundle method is reported to restore native kinematics of the knee with faster quadriceps recovery time and superior outcomes in comparison of side-to-side posterior translation and International Knee Documentation Committee scores when contrasted to single-bundle reconstruction techniques (Table 4).11 In ACL reconstruction, no significant differences have been shown by biomechanical studies to exist for single bundle versus double bundle reconstruction techniques in anterior tibial translation or tibial rotation during pivoting or loading.34
Table 4.
Advantages and Disadvantages
| Advantages |
| Anatomic multiligament reconstruction in one stage leads to faster strength recovery, better knee kinematics, and a lower rate of progression to osteoarthritis |
| Open incisions allow for better tissue visualization and may decrease operative time because of greater ease of access |
| Addressing the PLC before arthroscopy allows for better visualization before fluid extravasation; this can interfere with landmark and structure identification |
| Single-stage surgery in the acute setting decreases risk of arthrofibrosis as a complication |
| Disadvantages |
| Single-stage procedures may necessitate a longer operative time than multiple staged procedures |
| Open incisions may prolong recovery time compared to arthroscopic-only (unless arthroscopic fluid extravasation causes significant problems) |
| Risk of fluid extravasation into lower limb compartments; ensure calf remains soft throughout |
| Requires autografts and allografts due in part to the number of grafts needed |
PLC, posterolateral corner.
Finally, the anatomic reconstruction technique presented here for PLC reconstruction has been reported to result in significant improvements to International Knee Documentation Committee and Cincinnati objective scores, improved measurements on side-to-side varus stress testing, pivot-shift testing and external tibial rotation, and quantitative improvements in varus stress radiography at more than 2 years after surgery.1,7,12 Successful outcomes have been reported for both medial and lateral-sided multiligament knee injuries with consistent surgical approaches, with care taken to avoid tunnel convergence, passing and securing grafts in optimized order with correct positioning of the joint and appropriate rehabilitation.35 The importance of a systematic and biomechanically and clinically validated approach to multiligament knee reconstruction cannot be understated; revision multiligament procedures frequently must contend with extensive scarring and osteolysis, loss of autograft because of previous harvest, arthrofibrosis, and a significant quantity of retained hardware.36
Appropriate graft tensioning sequence is important to avoid overconstraint of the joint. If the ACL is tensioned first, posterior displacement of the tibia may result, whereas early PLC graft tensioning may result in increased internal tibial rotation. Tibial step-off, referring to the anterior position of the medial plateau relative to the medial femoral condyle, can be restored with anteriorly directed force during PCL ALB fixation with the knee at 90°.37 Failure to do so may result in posterior constraint of the knee during fixation of other grafts.1 The recommended order of fixation then should be PCL and then ACL, with the PLC grafts tensioned last.16
Multiple ligament injuries to the knee are difficult to treat and challenging in their array of damage to many knee structures. However, with early surgical intervention, appropriate surgical technique, anatomic reconstruction methods, avoidance of tunnel convergence, optimized sequence of graft fixation, and a rigorous rehabilitation regimen, these patients can achieve satisfactory outcomes with minimal morbidity.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L is a consultant for Arthrex, Ossur, Smith and Nephew, and Linvatec, receives royalties from Arthrex, Ossur, and Smith and Nephew and research grants from Smith and Nephew and Ossur, and is on the editorial boards for AOSSM, JEO, and KSSTA. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Repair of bicruciate ligament injury with grade III posterolateral corner tear. Examination under anesthesia is consistent with KD-III-L injury. Dissection of biceps femoris tendon (BFT) and common peroneal nerve (CPN) is performed through a lateral hockey stick incision. A fibular tunnel is drilled first, then a tibial tunnel for the popliteus tendon (PLT) and popliteofibular ligament (PLT). Femoral tunnels for the PLT and fibular collateral ligament (FCL) are drilled, oriented 35°anteromedially. Bone-patellar tendon-bone autograft is then harvested. After diagnostic arthroscopy, the PCL anterolateral bundle (ALB) and posteromedial bundle (PMB) tunnels are drilled, then the anterior cruciate ligament (ACL) femoral tunnel. A tibial guide pin is placed, confirmed with fluoroscopy, then a tunnel reamed and a large smoother passed. The ACL tibial tunnel is then reamed. The PMB graft of the PCL is passed first and secured, then the ALB. The ends of both bundles are passed down the tibial tunnel using the smoother. The ACL femoral graft is pulled into place and secured. The femoral ends of the FCL and PLT grafts are then secured. The FCL graft is passed under the iliotibial band (ITB) and through the fibular head tunnel. PCL grafts are then fixed on the anterior tibial cortex with screws and washers; ALB in 90° flexion and PMB in extension. This eliminated the posterior drawer. The ACL graft is then secured on the anterior tibia. The FCL graft is then secured in the fibular head tunnel with a screw at the anterior aperture. The PLT and PFL grafts are then passed from posterior to anterior through the tibial PLC tunnel and secured with a screw. Suture anchors are used to repair the lateral capsule and biceps femoris tendon, and the ITB repaired. Closure completes the procedure.
References
- 1.Ferrari M.B., Chahla J., Mitchell J.J., et al. Multiligament reconstruction of the knee in the setting of knee dislocation with a medial-sided injury. Arthrosc Tech. 2017;6:e341–e350. doi: 10.1016/j.eats.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moatshe G., Chahla J., LaPrade R.F., Engebretsen L. Diagnosis and treatment of multiligament knee injury: State of the art. J ISAKOS. 2017;2:152–161. [Google Scholar]
- 3.Azar F.M., Brandt J.C., Miller R.H., 3rd, Phillips B.B. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39:2170–2174. doi: 10.1177/0363546511414855. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 5.Laprade R.F., Bernhardson A.S., Griffith C.J., Macalena J.A., Wijdicks C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am J Sports Med. 2010;38:330–338. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 6.Kane P.W., Cinque M.E., Moatshe G., et al. Fibular collateral ligament: Varus stress radiographic analysis using 3 different clinical techniques. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118770170. 2325967118770170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geeslin A.G., Moulton S.G., LaPrade R.F. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: Surgical treatment of acute injuries. Am J Sports Med. 2016;44:1336–1342. doi: 10.1177/0363546515592828. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy M., Camarda L., Wijdicks C.A., Johansen S., Engebretsen L., Laprade R.F. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38:1674–1681. doi: 10.1177/0363546510361220. [DOI] [PubMed] [Google Scholar]
- 9.Persson A., Fjeldsgaard K., Gjertsen J.E., et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: A study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 10.Chahla J., Moatshe G., Cinque M.E., Godin J., Mannava S., LaPrade R.F. Arthroscopic Anatomic single-bundle anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft: Pearls for an accurate reconstruction. Arthrosc Tech. 2017;6:e1159–e1167. doi: 10.1016/j.eats.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chahla J., Nitri M., Civitarese D., Dean C.S., Moulton S.G., LaPrade R.F. Anatomic double-bundle posterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e149–156. doi: 10.1016/j.eats.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Serra Cruz R., Mitchell J.J., Dean C.S., Chahla J., Moatshe G., LaPrade R.F. Anatomic posterolateral corner reconstruction. Arthrosc Tech. 2016;5:e563–572. doi: 10.1016/j.eats.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moatshe G., Brady A.W., Slette E.L., et al. Multiple Ligament reconstruction femoral tunnels: intertunnel relationships and guidelines to avoid convergence. Am J Sports Med. 2017;45:563–569. doi: 10.1177/0363546516673616. [DOI] [PubMed] [Google Scholar]
- 14.Moatshe G., LaPrade R.F., Engebretsen L. How to avoid tunnel convergence in a multiligament injured knee. Ann Joint. 2018;3 93-93. [Google Scholar]
- 15.Moatshe G., Slette E.L., Engebretsen L., LaPrade R.F. Intertunnel relationships in the tibia during reconstruction of multiple knee ligaments: How to avoid tunnel convergence. Am J Sports Med. 2016;44:2864–2869. doi: 10.1177/0363546516656371. [DOI] [PubMed] [Google Scholar]
- 16.Moatshe G., Chahla J., Brady A.W., et al. The influence of graft tensioning sequence on tibiofemoral orientation during bicruciate and posterolateral corner knee ligament reconstruction: A biomechanical study. Am J Sports Med. 2018;46:1863–1869. doi: 10.1177/0363546517751917. [DOI] [PubMed] [Google Scholar]
- 17.LaPrade R.F., Smith S.D., Wilson K.J., Wijdicks C.A. Quantification of functional brace forces for posterior cruciate ligament injuries on the knee joint: An in vivo investigation. Knee Surg Sports Traumatol Arthrosc. 2015;23:3070–3076. doi: 10.1007/s00167-014-3238-4. [DOI] [PubMed] [Google Scholar]
- 18.LaPrade R.F., Chahla J., DePhillipo N.N., et al. Single-stage multiple-ligament knee reconstructions for sports-related injuries: Outcomes in 194 patients. Am J Sports Med. 2019;47:2563–2571. doi: 10.1177/0363546519864539. [DOI] [PubMed] [Google Scholar]
- 19.Sit R.W.S., Chan K.K.W., Zou D., et al. Clinic-based patellar mobilization therapy for knee osteoarthritis: A randomized clinical trial. Ann Fam Med. 2018;16:521–529. doi: 10.1370/afm.2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shelbourne K.D., Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: How the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471–480. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 21.Shelbourne K.D., Urch S.E., Gray T., Freeman H. Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. Am J Sports Med. 2012;40:108–113. doi: 10.1177/0363546511423639. [DOI] [PubMed] [Google Scholar]
- 22.Markolf K.L., O'Neill G., Jackson S.R., McAllister D.R. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32:1144–1149. doi: 10.1177/0363546503262198. [DOI] [PubMed] [Google Scholar]
- 23.Kim J.G., Lee Y.S., Yang B.S., Oh S.J., Yang S.J. Rehabilitation after posterior cruciate ligament reconstruction: A review of the literature and theoretical support. Arch Orthop Trauma Surg. 2013;133:1687–1695. doi: 10.1007/s00402-013-1854-y. [DOI] [PubMed] [Google Scholar]
- 24.Escamilla R.F., Macleod T.D., Wilk K.E., Paulos L., Andrews J.R. Cruciate ligament loading during common knee rehabilitation exercises. Proc Inst Mech Eng H. 2012;226:670–680. doi: 10.1177/0954411912451839. [DOI] [PubMed] [Google Scholar]
- 25.Wilk K.E., Escamilla R.F., Fleisig G.S., Barrentine S.W., Andrews J.R., Boyd M.L. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med. 1996;24:518–527. doi: 10.1177/036354659602400418. [DOI] [PubMed] [Google Scholar]
- 26.DePhillipo N.N., Kennedy M.I., Aman Z.S., Bernhardson A.S., O'Brien L., LaPrade R.F. Blood flow restriction therapy after knee surgery: indications, safety considerations, and postoperative protocol. Arthrosc Tech. 2018;7:e1037–e1043. doi: 10.1016/j.eats.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hughes L., Paton B., Rosenblatt B., Gissane C., Patterson S.D. Blood flow restriction training in clinical musculoskeletal rehabilitation: A systematic review and meta-analysis. Br J Sports Med. 2017;51:1003–1011. doi: 10.1136/bjsports-2016-097071. [DOI] [PubMed] [Google Scholar]
- 28.Hart J.M., Pietrosimone B., Hertel J., Ingersoll C.D. Quadriceps activation following knee injuries: A systematic review. J Athl Train. 2010;45:87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park S.H., Silva M. Neuromuscular electrical stimulation enhances fracture healing: Results of an animal model. J Orthop Res. 2004;22:382–387. doi: 10.1016/j.orthres.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 30.Toth M.J., Tourville T.W., Voigt T.B., et al. Utility of neuromuscular electrical stimulation to preserve quadriceps muscle fiber size and contractility after anterior cruciate ligament injuries and reconstruction: A randomized, sham-controlled, blinded trial. Am J Sports Med. 2020;48:2429–2437. doi: 10.1177/0363546520933622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nyland J., Fisher B., Brand E., Krupp R., Caborn D.N. Osseous deficits after anterior cruciate ligament injury and reconstruction: A systematic literature review with suggestions to improve osseous homeostasis. Arthroscopy. 2010;26:1248–1257. doi: 10.1016/j.arthro.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 32.Sheth U., Sniderman J., Whelan D.B. Early surgery of multiligament knee injuries may yield better results than delayed surgery: A systematic review. J ISAKOS. 2019;4:26–32. [Google Scholar]
- 33.Hohmann E., Glatt V., Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: A systematic review and meta-analysis. Knee. 2017;24:909–916. doi: 10.1016/j.knee.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 34.Goldsmith M.T., Jansson K.S., Smith S.D., Engebretsen L., LaPrade R.F., Wijdicks C.A. Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: an in vitro study. Am J Sports Med. 2013;41:1595–1604. doi: 10.1177/0363546513487065. [DOI] [PubMed] [Google Scholar]
- 35.Moatshe G., Vap A.R., Getgood A., LaPrade R.F., Engebretsen L. Medial-sided injuries in the multiple ligament knee injury. J Knee Surg. 2020;33:431–439. doi: 10.1055/s-0039-3402768. [DOI] [PubMed] [Google Scholar]
- 36.Stuart M.B., Woodmass J.M., Krych A.J., Levy B.A., Stuart M.J. Revision multiligament knee reconstruction surgery. J Knee Surg. 2020;33:346–350. doi: 10.1055/s-0039-3402791. [DOI] [PubMed] [Google Scholar]
- 37.Pache S., Aman Z.S., Kennedy M., et al. Posterior cruciate ligament: Current concepts review. Arch Bone Jt Surg. 2018;6:8–18. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Repair of bicruciate ligament injury with grade III posterolateral corner tear. Examination under anesthesia is consistent with KD-III-L injury. Dissection of biceps femoris tendon (BFT) and common peroneal nerve (CPN) is performed through a lateral hockey stick incision. A fibular tunnel is drilled first, then a tibial tunnel for the popliteus tendon (PLT) and popliteofibular ligament (PLT). Femoral tunnels for the PLT and fibular collateral ligament (FCL) are drilled, oriented 35°anteromedially. Bone-patellar tendon-bone autograft is then harvested. After diagnostic arthroscopy, the PCL anterolateral bundle (ALB) and posteromedial bundle (PMB) tunnels are drilled, then the anterior cruciate ligament (ACL) femoral tunnel. A tibial guide pin is placed, confirmed with fluoroscopy, then a tunnel reamed and a large smoother passed. The ACL tibial tunnel is then reamed. The PMB graft of the PCL is passed first and secured, then the ALB. The ends of both bundles are passed down the tibial tunnel using the smoother. The ACL femoral graft is pulled into place and secured. The femoral ends of the FCL and PLT grafts are then secured. The FCL graft is passed under the iliotibial band (ITB) and through the fibular head tunnel. PCL grafts are then fixed on the anterior tibial cortex with screws and washers; ALB in 90° flexion and PMB in extension. This eliminated the posterior drawer. The ACL graft is then secured on the anterior tibia. The FCL graft is then secured in the fibular head tunnel with a screw at the anterior aperture. The PLT and PFL grafts are then passed from posterior to anterior through the tibial PLC tunnel and secured with a screw. Suture anchors are used to repair the lateral capsule and biceps femoris tendon, and the ITB repaired. Closure completes the procedure.
Repair of bicruciate ligament injury with grade III posterolateral corner tear. Examination under anesthesia is consistent with KD-III-L injury. Dissection of biceps femoris tendon (BFT) and common peroneal nerve (CPN) is performed through a lateral hockey stick incision. A fibular tunnel is drilled first, then a tibial tunnel for the popliteus tendon (PLT) and popliteofibular ligament (PLT). Femoral tunnels for the PLT and fibular collateral ligament (FCL) are drilled, oriented 35°anteromedially. Bone-patellar tendon-bone autograft is then harvested. After diagnostic arthroscopy, the PCL anterolateral bundle (ALB) and posteromedial bundle (PMB) tunnels are drilled, then the anterior cruciate ligament (ACL) femoral tunnel. A tibial guide pin is placed, confirmed with fluoroscopy, then a tunnel reamed and a large smoother passed. The ACL tibial tunnel is then reamed. The PMB graft of the PCL is passed first and secured, then the ALB. The ends of both bundles are passed down the tibial tunnel using the smoother. The ACL femoral graft is pulled into place and secured. The femoral ends of the FCL and PLT grafts are then secured. The FCL graft is passed under the iliotibial band (ITB) and through the fibular head tunnel. PCL grafts are then fixed on the anterior tibial cortex with screws and washers; ALB in 90° flexion and PMB in extension. This eliminated the posterior drawer. The ACL graft is then secured on the anterior tibia. The FCL graft is then secured in the fibular head tunnel with a screw at the anterior aperture. The PLT and PFL grafts are then passed from posterior to anterior through the tibial PLC tunnel and secured with a screw. Suture anchors are used to repair the lateral capsule and biceps femoris tendon, and the ITB repaired. Closure completes the procedure.