Key Points
Question
What is the risk of fracture subsequent to traumatic fractures vs nontraumatic fractures among postmenopausal women?
Findings
In this large prospective cohort study of 66 874 postmenopausal women, future fracture risk after initial traumatic fracture was similar to that after nontraumatic fracture.
Meaning
Clinical osteoporosis assessment of postmenopausal women should include high-trauma as well as low-trauma fractures.
Abstract
Importance
The burden of fractures among postmenopausal women is high. Although nontraumatic fractures are strong risk factors for future fracture, current clinical guidelines do not address traumatic fractures.
Objective
To determine how future fracture risk varies according to whether an initial fracture is traumatic or nontraumatic.
Design, Setting, and Participants
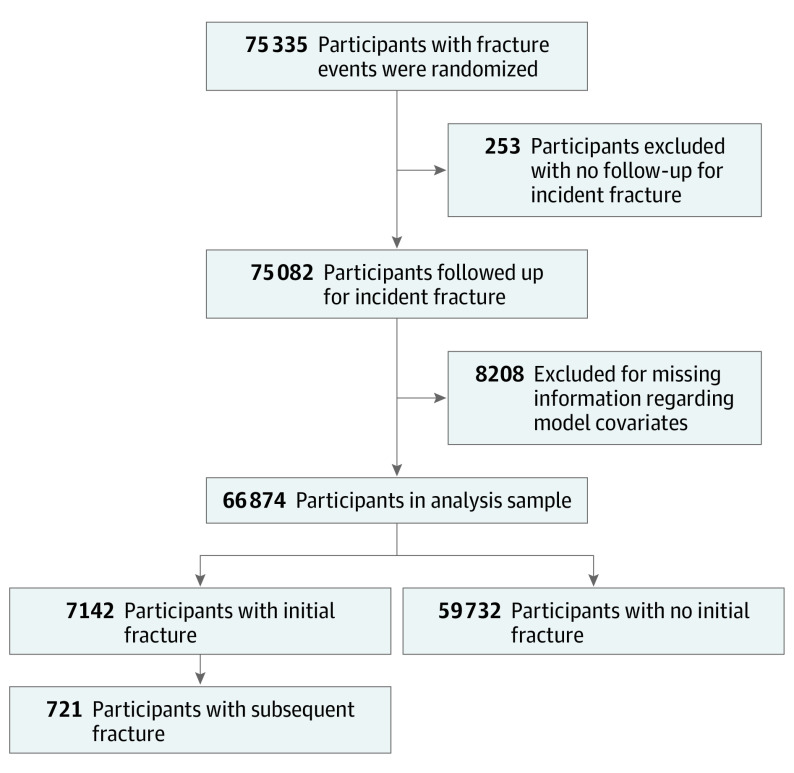
We conducted a prospective observational study using data from the Women’s Health Initiative Study (WHI) (enrollment, September 1994-December 1998; data analysis, September 2020 to March 2021), which enrolled postmenopausal women aged 50 to 79 years at baseline at 40 US clinical centers. The WHI Clinical Trials and WHI Bone Density Substudy, conducted at 3 of the clinical centers, asked participants to report the mechanism of incident fractures. Of 75 335 participants, information regarding incident fracture and covariates was available for 66 874 participants (88.8%), who comprised the analytic sample of this study. Mean (SD) follow-up was 8.1 (1.6) years.
Interventions
None.
Main Outcomes and Measures
Incident clinical fractures were self-reported at least annually and confirmed using medical records. Participants reported the mechanism of incident fracture as traumatic or nontraumatic.
Results
Among the 66 874 participants in the analytic sample (mean [SD] age, 63.1 [7.0] years and 65.3 [7.2] years among women without and with clinical fracture, respectively), 7142 participants (10.7%) experienced incident fracture during the study follow-up period. The adjusted hazard ratio (aHR) of subsequent fracture after initial fracture was 1.49 (95% CI, 1.38-1.61). Among women whose initial fracture was traumatic, the association between initial fracture and subsequent fracture was significantly increased (aHR, 1.25; 95% CI, 1.06-1.48). Among women whose initial fracture was nontraumatic, the association between initial fracture and subsequent fracture was also increased (aHR, 1.52; 95% CI, 1.37-1.68). Confidence intervals for associations between initial fracture and subsequent fracture were overlapping for traumatic and nontraumatic initial fracture strata.
Conclusions and Relevance
In this cohort study, among postmenopausal women older than 50 years, fracture was associated with a greater risk of subsequent fracture regardless of whether the fracture was traumatic or nontraumatic. These findings suggest that clinical osteoporosis assessment should include high-trauma as well as low-trauma fractures.
This cohort study examines how future fracture risk in postmenopausal women varies according to whether an initial fracture is traumatic or nontraumatic.
Introduction
One in 2 postmenopausal women will have an osteoporosis-related fracture during their remaining lifetimes.1 Fractures can result in loss of independence, chronic pain and disability, decreased quality of life, and increased mortality.2 Nontraumatic, or fragility fractures, are strong risk factors for future fracture. However, it is unclear whether traumatic fractures are associated with increased risk of subsequent fractures, particularly among younger postmenopausal women (age 50-64 years). Moreover, clinical osteoporosis guidelines do not mention traumatic fractures. For example, to our knowledge, clinical guidelines recommend considering pharmacologic therapy for postmenopausal women and men 50 years or older who have experienced fragility fractures3 or certain types of fragility fractures (ie, vertebral or hip fragility fractures),4 but do not provide guidance regarding traumatic fractures.
To our knowledge, no published studies have prospectively examined whether subsequent fracture risk differs according to whether an initial fracture is traumatic or nontraumatic among younger postmenopausal women in the US. A comparison of traumatic fractures and nontraumatic fractures in association with risk of subsequent fracture has the potential to affect clinical counseling and future clinical practice guidelines. The goal of this study was to determine how future fracture risk varies according to whether an initial fracture is traumatic or nontraumatic.
Methods
The Women’s Health Initiative Study Design
Between 1993 and 1998, the Women’s Health Initiative (WHI) study enrolled 161 808 postmenopausal women aged 50 to 79 years who were recruited at 40 US clinical sites.5 The WHI Observational Study (WHI-OS) examined risk factors for, and the course of, important causes of morbidity and mortality in postmenopausal women. Women with serious cardiac, pulmonary, kidney, and liver conditions were excluded from the study. The WHI Clinical Trials (WHI-CT) tested 3 interventions: menopausal hormone therapy, calcium plus vitamin D supplementation, and dietary modification (low-fat eating pattern). The current study is focused on data collected during the main study period (September 1994-December 1998; baseline through annual visit 9).
Institutional review board approval was obtained by each participating institution. Written informed consent was provided by all participants. At baseline, weight and height were measured, and body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) was calculated.
WHI Medical Record–Confirmed Fracture Cohort
The analytic sample included women for whom self-reported fractures were confirmed by medical records as well as the WHI Bone Density Substudy and the WHI-CT. In the WHI Bone Density Substudy, participants at 3 of the 40 clinical centers (Tucson/Phoenix, Arizona; Pittsburgh, Pennsylvania; and Birmingham, Alabama) were invited to undergo bone mineral density (BMD) measurement. Similarly, WHI conducted medical record confirmation of self-reported fractures in the WHI-CT participants using the same protocol. Together, the WHI Bone Density Substudy and the WHI-CTs provide medical record confirmation of incident fractures for 75 335 WHI participants during the main study.
Of the 75 335 participants, we excluded data from participants who did not provide follow-up information regarding incident fractures (253 [0.3%]) and participants for whom we lacked covariate information (8208 [10.9%]), resulting in analytic sample of 66 874 participants (Figure).
Figure. Strengthening the Reporting of Observational Studies in Epidemiology Analytic Sample Flow Diagram.
Fracture Ascertainment
Annually (and semiannually in the WHI-CT), participants were asked about incident fracture with the following question: “Has a doctor told you for the first time that you have a new broken, crushed, or fractured bone?” Participants who answered affirmatively were asked to report which bone was fractured. Response choices included hip, upper leg (not hip), pelvis, knee (patella), lower leg or ankle, foot (not toe), tailbone (coccyx), spine or back (vertebra), lower arm or wrist, hand (not finger), elbow, upper arm or shoulder, or other. Fractures of the jaw, nose, face, skull, finger, toe, ribs, and sternum were excluded from this analysis.
Self-reported fractures (the first fracture at a given anatomical location) were confirmed by medical record review. Fracture confirmation was confirmed centrally by WHI study physicians. Hip fracture was confirmed by review of written reports of radiographic studies; if written reports by a radiologist mentioned possible”, probable”, or suspected” hip fractures, hip fractures were confirmed by the University of California, San Francisco Bone Density Center radiologist. Nonhip fractures were confirmed by review of written radiography reports, clinic notes, emergency department notes, and operative reports stating that a new, acute, or healing fracture of a bone was clearly present based on a review of a radiograph. In the case of uncertain or equivocal results on an initial radiography report, confirmation of fracture required clear diagnosis of the fracture or healing fracture on a subsequent report. The following phrases were required for confirmation of a fracture using radiographic reports: fracture, definite fracture, break, hairline fracture, or healing fracture.
For this analysis, each incident fracture was classified into 1 of the following categories of body region: lower extremity (ankle, hip, patella, pelvis, shaft of femur, tibia/fibula, tibial plateau), upper extremity (carpal, elbow, lower end of humerus, radius/ulna, upper end of humerus, shaft of humerus, upper radius/ulna), or spine (lumbar spine and/or thoracic spine). In addition, we defined any clinical fracture as a fracture of the upper extremity, lower extremity, or clinical spine. We excluded the following types of fractures: foot (not toes), tailbone (sacrum and/or coccyx), hand (metacarpal bone(s), and collarbone (clavicular and scapular).
In addition to asking about incident fracture events, a questionnaire item assessed the mechanism of the fracture. Response choices included a car crash or being hit by a car, falling downstairs, a fall from a height (eg, fall while standing on a ladder or chair), other fall or trip (eg, while walking or getting out of bed), sports activity (eg, snow- or water-skiing, horse riding, or climbing), or other. We defined traumatic fractures as fractures that resulted from motor vehicle collisions, falls downstairs, falls from a height, or a sports activity. Fractures resulting from an other fall or trip were considered nontraumatic, and responses of other were defined as unknown mechanism.
Other Covariates
Information regarding age, race/ethnicity, education, income levels, cigarette smoking, supplemental calcium and vitamin D intake, alcohol intake, frequency of falls in the past year, medical history (including diabetes and previous fractures), and medication use was assessed on the baseline self-report questionnaire. Dietary calcium and vitamin D intakes were assessed by a food frequency questionnaire.6 We calculated the RAND 36-item health survey physical functioning construct (range, 0-100, in which a higher score indicates a more favorable health state).7,8,9 Using the WHI validated physical activity questionnaire,10,11,12 we quantified physical activity level as total metabolic equivalent task hours per week.
Statistical Analysis
We compared baseline characteristics among women who did and did not experience any initial (incident) fracture of the lower extremity, upper extremity, or spine. We calculated fracture event rates for initial fracture and subsequent fractures overall, and then stratified by age group (<55, 55-59, 60-64, 65-69, 70-74, or ≥75 years old) and racial/ethnic group (White, African American, Hispanic, other/unknown) as reported by the participant.
We used an extension of the Cox proportional hazards model for repeated failures to estimate the associations of a fracture during the study, by type, with a subsequent clinical fracture. Occurrence of a fracture was initially classified at study entry as none for all participants and then reclassified at the time of the first fracture during the study according to whether this fracture was traumatic, nontraumatic, or of unknown trauma status. This time-dependent categorical exposure allowed us to make head-to-head comparisons of the adjusted fracture rates that were associated with history of traumatic vs nontraumatic fractures as well as comparisons of each with no history of fracture, the reference condition. Participants were censored at time of death, loss to follow-up, or the end of the follow-up period. We adjusted for age, race/ethnicity, BMI, treated diabetes, frequency of falls (none, once, twice, 3 times, or more during the previous year), and physical function and activity. The baseline hazard was jointly stratified on use of hormone therapy (trial assigned or self-initiated), WHI Calcium + Vitamin D trial assignment, previous fracture (before study entry), and the WHI study component (WHI-CT or WHI-OS). Analyses were conducted using SAS, version 9.4 (SAS Institute), and statistical significance was set at P < .05.
Results
The mean (SD) follow-up time between the initial fracture and the subsequent clinical fracture or last follow-up date (whichever occurred first) was 8.1 (1.6) years; the median follow-up time (interquartile range) was 8.2 (7.4-9.1) years. Among the 66 874 participants in the analytic sample, 7142 participants (10.7%) experienced incident fracture during the study follow-up period (13.9 per 1000 person-years) (Table 1). Of those 7142 participants, 721 participants (10.1%) experienced a second fracture after the initial incident fracture.
Table 1. Frequencies, Events, and Event Rates per 1000 Person-Years of Initial and Subsequent Clinical Fracture,a Stratified by Age and Race/Ethnicity.
| Characteristic | Fracture outcome | |||||
|---|---|---|---|---|---|---|
| Initial fracture | Subsequent fracture | |||||
| No. (%) | Events | Rate per 1000 (95% CI) | No. (%) | Events | Rate per 1000 (95% CI) | |
| All participants | 66 874 (100) | 7142 | 13.9 (13.6-14.3) | 7142 (100) | 721 | 26.1 (24.3-28.1) |
| Age, y | ||||||
| <55 | 7713 (11.5) | 574 | 9.0 (8.3-9.7) | 574 (8.0) | 33 | 13.2 (9.4-18.5) |
| 55-59 | 13 695 (20.5) | 1101 | 10.0 (9.4-10.6) | 1101 (15.4) | 63 | 13.8 (10.8-17.7) |
| 60-64 | 16 440 (24.6) | 1498 | 11.9 (11.3-12.6) | 1498 (21.0) | 115 | 19.5 (16.2-23.4) |
| 65-69 | 14 876 (22.2) | 1781 | 16.0 (15.3-16.8) | 1781 | 182 | 26.7 (23.1-30.9) |
| 70-74 | 9859 (14.7) | 1403 | 19.6 (18.6-20.6) | 1403 (19.6) | 179 | 34.9 (30.1-40.4) |
| ≥75 | 4291 (6.4) | 785 | 26.6 (24.8-28.6) | 785 (11.0) | 149 | 54.7 (46.6-64.2) |
| Race/ethnicity | ||||||
| White | 54 131 (80.9) | 6392 | 15.4 (15.1-15.8) | 6392 (89.5) | 678 | 27.5 (25.5-29.7) |
| African American | 7111 (10.6) | 331 | 5.9 (5.3-6.6) | 331 (4.6) | 14 | 10.6 (6.3-17.9) |
| Hispanic | 2900 (4.3) | 191 | 8.8 (7.6-10.1) | 191 (2.7) | 14 | 19.0 (11.2-32.0) |
| Other/unknown | 2732 (4.1) | 228 | 11.1 (9.7-12.6) | 228 (3.2) | 15 | 16.2 (9.8-26.9) |
| American Indian/Alaska Native | 370 (0.6) | 29 | 10.6 (7.3-15.2) | 29 (0.4) | 2 | 16.7 (4.2-66.8) |
| Asian/Pacific Islander | 1469 (2.2) | 106 | 9.5 (7.8-11.5) | 106 (1.5) | 7 | 15.0 (7.1-31.4) |
| Unknown | 893 (1.3) | 93 | 14.1 (11.5-17.2) | 93 (1.3) | 6 | 17.8 (8.0-39.6) |
Fracture sites included lower extremity (ankle, hip, patella, pelvis, shaft of femur, tibia/fibula, tibial plateau), upper extremity (carpal, elbow, lower end of humerus, radius/ulna, upper end of humerus, shaft of humerus, upper radius/ulna), and spine (lumbar spine, thoracic spine) fractures.
At baseline, the mean (SD) age of participants was 63.1 (7.0) years among women without clinical fracture during study follow-up and 65.3 (7.2) years among participants who experienced incident fracture (Table 2). Compared with participants who did not experience fracture, a higher proportion of participants who experienced fracture were White, had ≥1 fall in the past year, and had never used hormone therapy before enrollment in WHI. Compared with women who experienced traumatic fractures or fractures with unknown trauma status, more women who experienced nontraumatic fractures had a BMI of 30 or greater and had never received estrogen therapy.
Table 2. Baseline Characteristics by Initial Fracture Locationa for 66 874 Participants.
| Characteristic | No. (%) | P value | ||||
|---|---|---|---|---|---|---|
| No fracture (n = 59 732) | Traumatic (n = 1624) | Nontraumatic (n = 3891) | Unknown trauma (n = 1627) | Fracture vs no fracture | Traumatic vs nontraumatic vs unknown trauma | |
| Age at enrollment, mean (SD), y | 63.1 (7.0) | 64.0 (7.0) | 65.6 (7.2) | 65.8 (7.2) | ||
| <55 | 7139 (12.0) | 147 (9.1) | 311 (8.0) | 116 (7.1) | <.001 | <.001 |
| 55 to <60 | 12 594 (21.1) | 327 (20.1) | 552 (14.2) | 222 (13.6) | ||
| 60 to <65 | 14 942 (25.0) | 384 (23.6) | 768 (19.7) | 346 (21.3) | ||
| 65 to <69 | 13 095 (21.9) | 377 (23.2) | 993 (25.5) | 411 (25.3) | ||
| 70 to <75 | 8456 (14.2) | 258 (15.9) | 809 (20.8) | 336 (20.7) | ||
| ≥75 | 3506 (5.9) | 131 (8.1) | 458 (11.8) | 196 (12.0) | ||
| Race/ethnicity | ||||||
| White | 47 739 (79.9) | 1436 (88.4) | 3490 (89.7) | 1466 (90.1) | <.001 | .69 |
| African American | 6780 (11.4) | 84 (5.2) | 176 (4.5) | 71 (4.4) | ||
| Hispanic | 2709 (4.5) | 49 (3.0) | 107 (2.7) | 35 (2.2) | ||
| American Indian/Alaska Native | 341 (0.6) | 4 (0.2) | 18 (0.5) | 7 (0.4) | ||
| Asian/Pacific Islander | 1363 (2.3) | 27 (1.7) | 55 (1.4) | 24 (1.5) | ||
| Unknown | 800 (1.3) | 24 (1.5) | 45 (1.2) | 24 (1.5) | ||
| Education | ||||||
| ≤High school/GED | 14 638 (24.5) | 363 (22.4) | 969 (24.9) | 362 (22.2) | .28 | .08 |
| School after high school | 23 468 (39.3) | 621 (38.2) | 1500 (38.6) | 675 (41.5) | ||
| ≥College graduate | 21 208 (35.5) | 631 (38.9) | 1397 (35.9) | 579 (35.6) | ||
| BMI, mean (SD) | 28.9 (6.0) | 27.9 (5.3) | 28.6 (5.7) | 28.2 (5.7) | ||
| <25 | 16 811 (28.1) | 521 (32.1) | 1139 (29.3) | 517 (31.8) | <.001 | <.001 |
| 25 to <30 | 20 978 (35.1) | 613 (37.7) | 1426 (36.6) | 593 (36.4) | ||
| ≥30 | 21 943 (36.7) | 490 (30.2) | 1326 (34.1) | 517 (31.8) | ||
| ≥1 Fall during the past year | ||||||
| Yes | 18 251 (30.6) | 600 (36.9) | 1491 (38.3) | 580 (35.6) | <.001 | .19 |
| No | 41 037 (68.7) | 1011 (62.3) | 2376 (61.1) | 1030 (63.3) | ||
| Unknown | 444 (0.7) | 13 (0.8) | 24 (0.6) | 17 (1.0) | ||
| Fracture at age 55 y or older | ||||||
| Yes | 4903 (8.2) | 219 (13.5) | 613 (15.8) | 284 (17.5) | <.001 | <.001 |
| No | 54 354 (91.0) | 1396 (86.0) | 3249 (83.5) | 1320 (81.1) | ||
| Unknown | 475 (0.8) | 9 (0.6) | 29 (0.7) | 23 (1.4) | ||
| Smoking | ||||||
| Never | 30 424 (50.9) | 802 (49.4) | 1973 (50.7) | 822 (50.5) | .51 | .32 |
| Past | 24 041 (40.2) | 690 (42.5) | 1582 (40.7) | 654 (40.2) | ||
| Current | 4681 (7.8) | 119 (7.3) | 286 (7.4) | 137 (8.4) | ||
| Alcohol drinks/wk, mean (SD) | 2.1 (4.4) | 2.4 (4.4) | 2.4 (5.0) | 2.1 (4.7) | ||
| 0 | 26 261 (44.0) | 655 (40.3) | 1669 (42.9) | 727 (44.7) | <.001 | .13 |
| >0 to <7 | 27 200 (45.5) | 783 (48.2) | 1759 (45.2) | 740 (45.5) | ||
| ≥7 | 6108 (10.2) | 181 (11.1) | 451 (11.6) | 155 (9.5) | ||
| Physical activity (total MET h/wk), mean (SD) | 10.8 (12.8) | 12.0 (12.9) | 10.4 (12.0) | 10.6 (12.6) | ||
| 0 | 11 377 (19.0) | 264 (16.3) | 721 (18.5) | 295 (18.1) | .84 | <.001 |
| >0 to <5 | 14 125 (23.6) | 357 (22.0) | 902 (23.2) | 419 (25.8) | ||
| 5 to <12 | 14 321 (24.0) | 388 (23.9) | 1004 (25.8) | 379 (23.3) | ||
| ≥12 | 19 909 (33.3) | 615 (37.9) | 1264 (32.5) | 534 (32.8) | ||
| Estrogen therapy use (pill or transdermal patch)b | <.001 | .004 | ||||
| Never | 21 140 (35.4) | 642 (39.5) | 1691 (43.5) | 634 (39.0) | <.001 | .004 |
| Past | 8368 (14.0) | 245 (15.1) | 608 (15.6) | 270 (16.6) | ||
| Current | 30 224 (50.6) | 737 (45.4) | 1592 (40.9) | 723 (44.4) | ||
| Calcium intake,c mg/d, mean (SD) | 1132.2 (685.5) | 1182.7 (698.1) | 1145.0 (668.0) | 1176.5 (673.1) | ||
| <400 | 4984 (8.3) | 110 (6.8) | 266 (6.8) | 117 (7.2) | <.001 | .10 |
| 400 to <800 | 16 468 (27.6) | 456 (28.1) | 1119 (28.8) | 411 (25.3) | ||
| 800 to <1200 | 15 003 (25.1) | 384 (23.6) | 978 (25.1) | 419 (25.8) | ||
| ≥1200 | 22 049 (36.9) | 642 (39.5) | 1444 (37.1) | 644 (39.6) | ||
| Vitamin D intake,d IU/d, mean (SD) | 351.6 (266.9) | 359.9 (271.9) | 356.5 (259.2) | 374.9 (264.4) | ||
| <200 | 23 693 (39.7) | 633 (39.0) | 1480 (38.0) | 575 (35.3) | .004 | .06 |
| 200 to <400 | 11 184 (18.7) | 313 (19.3) | 745 (19.1) | 302 (18.6) | ||
| 400 to <600 | 13 643 (22.8) | 353 (21.7) | 907 (23.3) | 401 (24.6) | ||
| ≥600 | 9984 (16.7) | 293 (18.0) | 675 (17.3) | 313 (19.2) | ||
| Physical Function Score,e mean (SD) | 80.7 (19.8) | 82.2 (18.5) | 78.3 (20.6) | 77.1 (21.5) | ||
| ≤60 | 9788 (16.4) | 227 (14.0) | 736 (18.9) | 369 (22.7) | <.001 | <.001 |
| 60 to <90 | 20 402 (34.2) | 555 (34.2) | 1474 (37.9) | 573 (35.2) | ||
| ≥90 | 29 542 (49.5) | 842 (51.8) | 1681 (43.2) | 685 (42.1) | ||
| History of treated diabetes | ||||||
| Yes | 2953 (4.9 | 79 (4.9) | 218 (5.6) | 96 (5.9) | .04 | .04 |
| No | 56 779 (95.1) | 1545 (95.1) | 3673 (94.4) | 1531 (94.1) | ||
| History of cancer | ||||||
| Yes | 2808 (4.7) | 88 (5.4) | 205 (5.3) | 87 (5.3) | .07 | .80 |
| No | 56 593 (94.7) | 1524 (93.8) | 3668 (94.3) | 1531 (94.1) | ||
| WHI component | ||||||
| Clinical trial | 53 603 (89.7) | 1480 (91.1) | 3527 (90.6) | 1447 (88.9) | .10 | NA |
| Observational study | 6129 (10.3 | 144 (8.9) | 364 (9.4) | 180 (11.1) | ||
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); GED, general educational developmental certificate; MET, metabolic equivalent task; WHI, Women’s Health Initiative.
Fracture sites included lower extremity (ankle, hip, patella, pelvis, shaft of femur, tibia/fibula, tibial plateau), upper extremity (carpal, elbow, lower end of humerus, radius/ulna, upper end of humerus, shaft of humerus, upper radius/ulna), and spine (lumbar spine, thoracic spine) fractures. Individual fracture site columns do not include 89 participants who had initial fractures at multiple body areas.
Hormone use incorporates self-report and Women’s Health Initiative Hormone Therapy Trial assignment.
From dietary intake and supplement use.
From dietary intake and supplement use.
RAND 36-item physical function score. Range is 0 to100, in which a higher score indicates a more favorable health state.
Absolute unadjusted rates of subsequent fracture were similar after initial traumatic and initial nontraumatic fractures (Table 3). After initial traumatic and nontraumatic fractures, rates of subsequent fracture were higher among older women.
Table 3. Frequencies, Events, and Event Rates per 1000 Person-Years of Subsequent Clinical Fracture,a Stratified by Whether the Initial Fracture Was Traumatic or Nontraumatic and Baseline Age.
| Characteristic | Subsequent fracture by initial fracture trauma | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Traumatic | Nontraumatic | Unknown traumatic | |||||||
| No. (%) | Events | Rate per 1000 (95% CI) | No. | Events | Rate per 1000 (95% CI) | No. (%) | Events | Rate per 1000 (95% CI) | |
| All participants | 1624 (100.0) | 137 | 20.3 (17.2-24.0) | 3891 (100.1) | 398 | 27.0 (24.5-29.8) | 1627 (100.0) | 186 | 30.2 (26.2-34.9) |
| Age, y | |||||||||
| <55 | 147 (9.1) | 8 | 11.9 (5.9-23.8) | 311 (8.0) | 15 | 11.6 (7.0-19.3) | 116 (7.1) | 10 | 18.5 (9.1-34.4) |
| 55-59 | 327 (20.1) | 14 | 9.9 (5.9-16.8) | 552 (14.2) | 38 | 17.08 (12.3-23.3) | 220 (13.6) | 11 | 12.1 (6.7-21.9) |
| 60-64 | 384 (23.7) | 26 | 16.3 (11.1-23.9) | 768 (19.7) | 58 | 19.3 (14.9-25.0) | 346 (21.3) | 31 | 23.9 (16.8-34.0) |
| 65-69 | 377 (23.2) | 38 | 23.7 (17.2-32.5) | 993 (25.5) | 95 | 25.9 (21.2-31.7) | 411 (25.1) | 49 | 32.0 (24.2-42.3) |
| 70-74 | 258 (15.9) | 34 | 35.2 (25.2-49.3) | 809 (20.8) | 104 | 34.9 (28.8-42.3) | 336 (20.7) | 41 | 34.4 (25.3-46.7) |
| ≥75 | 131 (8.1) | 17 | 34.2 (21.2-55.0) | 458 (11.8) | 88 | 57.2 (46.4-70.5) | 196 (12.1) | 44 | 63.9 (47.5-95.9) |
Fracture sites included lower extremity (ankle, hip, patella, pelvis, shaft of femur, tibia/fibula, tibial plateau), upper extremity (carpal, elbow, lower end of humerus, radius/ulna, upper end of humerus, shaft of humerus, upper radius/ulna), and spine (lumbar spine, thoracic spine) fractures.
Overall, the hazard ratio (HR) of subsequent fracture after initial fracture was 1.70 (95% CI, 1.57-1.84) (Table 4). After adjustment for covariates, the association between initial fracture and subsequent fracture remained statistically significant (adjusted HR, 1.49; 95% CI, 1.38-1.61; P < .001). In fully adjusted models, among women whose initial fracture was traumatic, the association between initial fracture and subsequent fracture was statistically significant, although of slightly lower magnitude (adjusted HR, 1.25; 95% CI, 1.06-1.48). For participants who experienced a nontraumatic initial fracture, the risk of subsequent fracture was comparable with that of the overall group (adjusted HR, 1.52; 95% CI, 1.37-1.68). The risk of subsequent fracture among women whose initial mechanism of fracture was unknown was also comparable with that of the overall group (adjusted HR, 1.67; 95% CI, 1.44-1.93). The adjusted HR for subsequent fracture after traumatic fracture vs nontraumatic fracture was 0.82 (95% CI, 0.68-1.00; P = .05).
Table 4. Associations between Initial Clinical Fracture,a Overall and by Traumatic vs Nontraumatic Mechanism, and Subsequent Clinical Fracture.
| Initial fracture mechanism | Unadjusted | Age/race adjusted | Multivariate adjustedb | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | |
| All fracture | 1.70 (1.57-1.84) | <.001 | 1.53 (1.42-1.66) | <.001 | 1.49 (1.38-1.61) | <.001 |
| By trauma | ||||||
| Traumatic vs no initial fracture | 1.36 (1.15-1.62) | <.001 | 1.28 (1.08-1.51) | .01 | 1.25 (1.06-1.48) | .01 |
| Nontraumatic vs no initial fracture | 1.75 (1.58-1.94) | <.001 | 1.56 (1.41-1.72) | <.001 | 1.52 (1.37-1.68) | <.001 |
| Unknown traumatic vs no initial fracture | 1.94 (1.68-2.25) | <.001 | 1.72 (1.49-2.00) | <.001 | 1.67 (1.44-1.93) | <.001 |
| Traumatic vs nontraumatic initial fracture | 0.78 (0.64-0.95) | .01 | 0.82 (0.67-1.00) | .04 | 0.82 (0.68-1.00) | .05 |
Abbreviations: HR: hazard ratio; WHI, Women’s Health Initiative.
Fracture sites included lower extremity (ankle, hip, patella, pelvis, shaft of femur, tibia/fibula, tibial plateau), upper extremity (carpal, elbow, lower end of humerus, radius/ulna, upper end of humerus, shaft of humerus, upper radius/ulna), and spine (lumbar spine, thoracic spine) fractures.
Multivariate models were adjusted for age, race, body mass index (calculated as weight in kilograms divided by height in meters squared), previous fracture, diabetes, physical function, physical activity, and frequency of falls in the past year. All models were stratified within the model to allow the baseline hazard to vary by hormone therapy use, WHI Calcium + Vitamin D intervention trial assignment, and WHI study component (WHI-CT or WHI-OS).
Discussion
In this large prospective study of postmenopausal women, the risk of subsequent fracture after an initial fracture was significantly elevated among women whose initial fracture was traumatic (HR, 1.25; 95% CI, 1.06-1.48) as well as women whose initial fracture was nontraumatic (HR 1.52; 95% CI, 1.37-1.68). The confidence intervals of these 2 estimates overlap, indicating that nontraumatic and traumatic initial fractures are similarly associated with risk of subsequent fracture.
To our knowledge, previously published studies have not prospectively compared the risk of subsequent fractures after traumatic and nontraumatic fractures among young postmenopausal women (younger than 65 years) in the US. However, our results are generally consistent with a study of older US women. A population-based study of women in Rochester, Minnesota (mean age at initial fracture, 66 years, 1975-1994) focused on initial forearm fracture; it found that there was no statistically significant difference in the risk of subsequent fractures at any site comparing those whose index forearm fracture was “due to severe vs moderate trauma” (except for greater risk of a subsequent vertebral fracture followed by distal forearm fractures that were caused by severe trauma).13 While the Study of Osteoporotic Fractures did not include women younger than 65 years (postmenopausal women who had a mean age of 73 years), it demonstrated that the increased risk of subsequent fracture was similar for initial low-trauma fractures (31% higher risk) and initial high-trauma fractures (34% higher risk) during 9-year the follow-up period.14 Leslie et al15 demonstrated associations between high-trauma fractures and subsequent fracture risk among women in Canada (mean age, approximately 65 years). Ensrud and colleagues16 demonstrated the importance of high-trauma fractures among older men in the MrOS study. Although these previous studies did not focus on younger postmenopausal women in the US, they are important in highlighting the importance of considering high-trauma fractures in association with subsequent fracture risk.
Our study’s results are clinically important because, in contrast to a nontraumatic fracture, a fracture that is considered traumatic often does not trigger further evaluation for osteoporosis or counseling regarding increased subsequent fracture risk, which could lead to underevaluation and undertreatment of at-risk women. High-trauma and low-trauma fractures show similar associations with low BMD.15 This suggests that osteoporosis intervention trials and future observational studies should include traumatic fractures as important outcomes14 and clinical osteoporosis assessment should include assessment for high-trauma as well as low-trauma fractures.
These study results will also help to inform future clinical guidelines regarding osteoporosis. Current guidelines do not focus on traumatic fractures. Regarding osteoporosis diagnosis, some guidelines consider previous fragility fracture to be diagnostic of osteoporosis3,4 but do not specifically mention traumatic fracture. Other clinical guidelines consider hip or vertebral fractures in the absence of major trauma to be diagnostic of osteoporosis but do not specifically mention other fracture types, or traumatic fracture, as being diagnostic of osteoporosis.17 Similarly, regarding treatment, some clinical guidelines recommend that women with hip fracture or vertebral fracture initiate pharmacologic therapy (regardless of bone density level), but women with other types of fracture, including traumatic fracture, would not automatically qualify for pharmacologic treatment unless they had bone density levels in the osteoporotic range.4,17 Other treatment guidelines recommend treatment for any type of previous fragility fracture, but, again, do not include specific guidance regarding traumatic fractures.3
This study highlights the high prevalence with which women do not specify whether their fracture mechanism was traumatic or nontraumatic fractures, as reflected by the many women with fractures who selected other (ie, designated a mechanism other than nontraumatic or traumatic) as the mechanism of fracture. Future studies that ascertain fracture incidence should work toward characterizing the specific reasons for this, because it presents a barrier to understanding how the degree of trauma that causes the initial fracture affects subsequent fracture risk. Such information will be important for clinicians when they perform patient counseling regarding the risk of subsequent fracture after an initial fracture. Our study’s results also underscore the issue of difficulty in assessing whether fractures are traumatic or nontraumatic. Information regarding the optimal way for clinicians to perform such assessment is needed to inform high-quality clinical practice.
Strengths and Limitations
Our study has several potential limitations. We only captured the first initial fracture at each anatomic location. For example, if a participant had a lower arm/wrist fracture, a subsequent lower arm/wrist fracture would not be captured. As a result, our results may be conservative (ie, underestimate the associations of initial traumatic and nontraumatic fracture with subsequent fracture). Because BMD was only measured in 3 of the 40 WHI clinical centers, there were low numbers of events within BMD T score strata, limiting the statistical power to examine differences in associations across T score categories. Finally, although we adjusted for numerous potential confounders, residual confounding is possible, as in all observational studies. Our study also has several strengths, including the prospective study design, the large number of study participants from across the US (including 37 848 women aged between 50 and 64 years) who were not the focus of previous studies, medical record confirmation of fractures, information regarding the events (mechanisms) leading to the fractures, and detailed information regarding potential confounders. Moreover, this study contains many younger postmenopausal women who were not examined in previous prospective studies that compared traumatic and nontraumatic fractures among women in the US.
Conclusions
Future fracture risk is similar among postmenopausal women with initial traumatic fracture and women with initial nontraumatic fracture. Currently, nontraumatic fractures are characterized as osteoporotic. This study’s findings suggest that all fractures, whether traumatic or nontraumatic, should warrant evaluation for osteoporosis (including BMD testing) and counseling regarding subsequent increased fracture risk. These results advance our understanding of the burden of potentially preventable fractures, which is higher in women with initial traumatic fractures as well as those with initial nontraumatic fractures. Fracture in postmenopausal women older than 50 years is associated with a greater risk of subsequent fracture, regardless of mechanism (traumatic or nontraumatic). This information will inform the development of targeted secondary prevention strategies and future clinical guidelines.
References
- 1.U.S. Preventive Services Task Force . Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med. 2011;154(5):356-364. doi: 10.7326/0003-4819-154-5-201103010-00307 [DOI] [PubMed] [Google Scholar]
- 2.Curry SJ, Krist AH, Owens DK, et al. ; US Preventive Services Task Force . Screening for osteoporosis to prevent fractures: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(24):2521-2531. doi: 10.1001/jama.2018.7498 [DOI] [PubMed] [Google Scholar]
- 3.Qaseem A, Forciea MA, McLean RM, Denberg TD; Clinical Guidelines Committee of the American College of Physicians . Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818-839. doi: 10.7326/M15-1361 [DOI] [PubMed] [Google Scholar]
- 4.Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract. 2020;26(suppl 1):1-46. doi: 10.4158/GL-2020-0524SUPPL [DOI] [PubMed] [Google Scholar]
- 5.The Women’s Health Initiative Study Group . Design of the Women’s Health Initiative clinical trial and observational study. Control Clin Trials. 1998;19(1):61-109. doi: 10.1016/S0197-2456(97)00078-0 [DOI] [PubMed] [Google Scholar]
- 6.Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T. Measurement characteristics of the Women’s Health Initiative food frequency questionnaire. Ann Epidemiol. 1999;9(3):178-187. doi: 10.1016/S1047-2797(98)00055-6 [DOI] [PubMed] [Google Scholar]
- 7.Andresen EM, Bowley N, Rothenberg BM, Panzer R, Katz P. Test-retest performance of a mailed version of the Medical Outcomes Study 36-Item Short-Form Health Survey among older adults. Med Care. 1996;34(12):1165-1170. doi: 10.1097/00005650-199612000-00001 [DOI] [PubMed] [Google Scholar]
- 8.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care. 1992;30(6):473-483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 9.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ. 1993;2(3):217-227. doi: 10.1002/hec.4730020305 [DOI] [PubMed] [Google Scholar]
- 10.Pettee Gabriel K, McClain JJ, Lee CD, et al. Evaluation of physical activity measures used in middle-aged women. Med Sci Sports Exerc. 2009;41(7):1403-1412. doi: 10.1249/MSS.0b013e31819b2482 [DOI] [PubMed] [Google Scholar]
- 11.Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the Women’s Health Initiative physical activity questionnaire. Med Sci Sports Exerc. 2009;41(3):530-538. doi: 10.1249/MSS.0b013e31818ace55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716-725. doi: 10.1056/NEJMoa021067 [DOI] [PubMed] [Google Scholar]
- 13.Cuddihy MT, Gabriel SE, Crowson CS, O’Fallon WM, Melton LJ III. Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int. 1999;9(6):469-475. doi: 10.1007/s001980050172 [DOI] [PubMed] [Google Scholar]
- 14.Mackey DC, Lui LY, Cawthon PM, et al. ; Study of Osteoporotic Fractures and Osteoporotic Fractures in Men Study Research Groups . High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298(20):2381-2388. doi: 10.1001/jama.298.20.2381 [DOI] [PubMed] [Google Scholar]
- 15.Leslie WD, Schousboe JT, Morin SN, et al. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int. 2020;31(6):1059-1067. doi: 10.1007/s00198-019-05274-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ensrud KE, Blackwell TL, Cawthon PM, et al. ; Osteoporotic Fractures in Men (MrOS) Study of Osteoporotic Fractures (SOF) Research Groups . Degree of trauma differs for major osteoporotic fracture events in older men versus older women. J Bone Miner Res. 2016;31(1):204-207. doi: 10.1002/jbmr.2589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Osteoporosis Foundation . Clinician's Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]