Abstract
While proximal hamstring tears at the myotendinous junction are common sports-related injuries that are often successfully treated nonoperatively, complete avulsions from the origin on the ischial tuberosity are less common and better treated with surgical repair to prevent significant functional limitations and ongoing weakness. The diagnosis can be easily missed, leading patients to present several months after the initial injury. In addition, some patients decide on nonoperative management initially but later present requesting surgical intervention. The delayed cases are challenging due to often significant tendon retraction, making direct repair difficult if not impossible. Techniques using allograft and autograft reconstruction have been described for this clinical situation. This Technical Note describes the use of 2 Achilles tendon allografts fixed via 5 suture anchors to reconstruct a chronic complete avulsion injury of the proximal hamstring with >5-cm retraction.
Technique Video
Simulation of proximal hamstring reconstruction using the aforementioned technique via a sawbones model. The sawbones pelvis is positioned prone. A model graft is shown representing the Achilles allograft with demonstration of the suture technique used. The video then demonstrates placement of the suture anchors into the ischium with tensioning of the graft.
Acute strains of the hamstring muscle group are relatively common sports injuries that often respond well to nonoperative management. Complete tears are less common, most often occurring at the myotendinous junction. Complete avulsion injuries of the proximal hamstring from their origin on the ischial tuberosity result in significant weakness and functional limitations.1 As many as 12% of hamstring injuries involve an avulsion tear at the origin of the tendons on the ischial tuberosity, which often undergo primary repair.2,3 When not treated acutely, chronic avulsions can lead patients to have ongoing weakness, with few able to return to preinjury sport and recreational activity levels.4 Advanced imaging usually demonstrates significant retraction of the hamstring tendon, at which point primary open repair may no longer be feasible. In these challenging cases, the use of allografts to augment the repair of the hamstring tendon is often needed.5,6 In this Technical Note, we present a surgical technique employing 2 Achilles tendon allografts to augment the repair of a chronic proximal hamstring tear.
Patient Presentation and Physical Examination
Proximal hamstring injuries often occur as a result of an eccentric contraction with the hip flexed and knee extended.3 Patients often report a loud pop with pain in the buttock region. They may also complain of paresthesia or symptoms of sciatic nerve irritation.7 In cases of delayed presentation due to missed initial injuries or failed nonoperative management, ecchymosis (which may be observed in acute cases) is absent on inspection.
Most patients will present with a “stiff-legged” gait as they try to avoid concomitant hip flexion and knee extension.1 Palpation is performed to evaluate presence of tenderness over the ischial tuberosity and a palpable defect; however, this may be absent due to overlying soft tissue. Bilateral active and passive range of motion is performed to assess for asymmetry. Muscle strength in the lower extremities, with a focus on knee flexion strength, also should be evaluated. In addition, there are several provocative tests that can aid in diagnosis of proximal hamstring injuries. These include the active standing hamstring stretch (Puranen–Orava), bent-knee, and modified-bent-knee stretch test. It is key to also perform a thorough neurovascular examination and document any peroneal nerve sensory or motor deficits.1
Plain radiographs are often negative in avulsion injuries unless an avulsion fracture of the ischial tuberosity is present. Ultrasound can sometimes be useful; however, this imaging modality is indicated for acute injuries at the musculotendinous junction rather than in chronic tears. Magnetic resonance imaging (MRI) tends to be more sensitive and specific in detecting both acute and chronic avulsion injuries with tendon retraction. MRI is the imaging modality of choice, especially for those presenting with chronic injuries. In contrast to ultrasound, MRI allows for better determining the extent of the injury and the amount of tendon retraction, if present.8 MRI allows for identifying the location of the tear (avulsion off the ischial tuberosity, tear at myotendinous junction, muscle belly tear), number of tendons involved, and extent of retraction, all of which influence the decision of whether to treat the injury operatively and aid in surgical planning.1
Surgical Technique
Patient Positioning
The patient is brought to the operating room and placed in the prone position after induction of general anesthesia. A nonsterile clear self-adhesive impermeable drape is then placed around the proximal hip. A second drape is then placed around the superior aspect of the hip, ensuring maintenance of exposure of the posterior gluteal fold. Sterile prepping and draping are then completed with impervious drapes. The surgical field is then sealed with Ioban (3M, St. Paul, MN) to ensure no drape peel off. The entire extremity is draped in to allow manipulation of the leg and knee during surgery to allow assessment of hamstring tendon excursion, confirmation of anatomic structures, and proper graft tensioning.
Surgical Approach and Repair (With Video Illustration)
The ischial tuberosity is palpated just proximal to the gluteal fold followed by palpation of the retracted musculotendinous complex. A vertical incision is made in line with these structures traversing the gluteal fold. A longitudinal/vertical incision is used to provide adequate exposure proximally and distally, given the extent of tendon retraction seen in chronic injuries. Furthermore, it is important to have adequate exposure to release scar tissue and avoid iatrogenic injury to the sciatic nerve. The gluteus maximus fascia is identified proximally along with the fascia overlying the hamstring tendon and retracted stump. This is opened. The sciatic nerve is identified and freed laterally from the hamstring bundle and associated fibrous scar tissue. Then adhesions surrounding the retracted proximal hamstring tendon are released to allow for maximal excursion, as seen in Figs 1 and 2. Once fully released, the remaining gap is measured between the ischial tuberosity and mobilized hamstring bundle to plan for graft size.
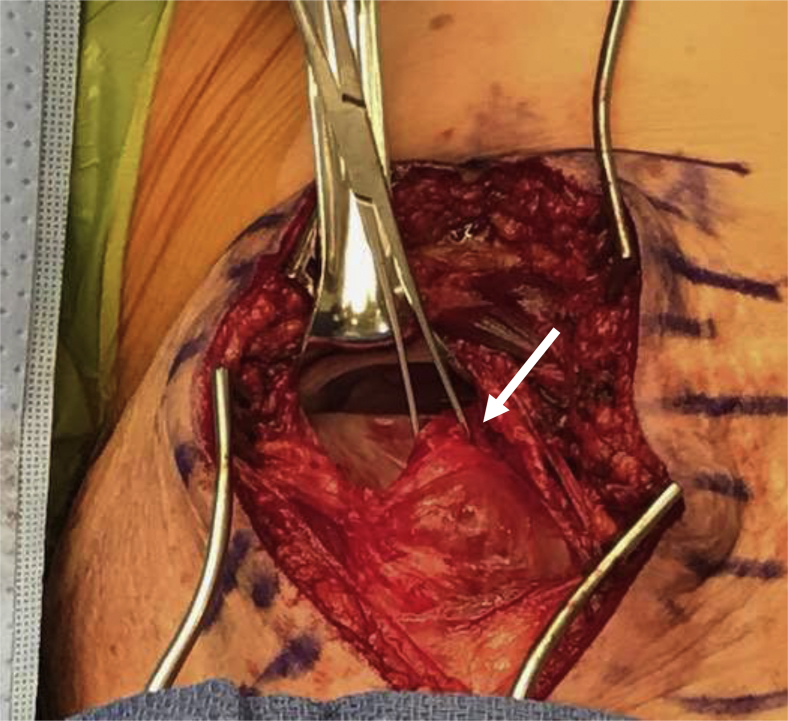
Fig 1.
Intraoperative image of right ischium with the patient in the prone position. A longitudinal incision is made and the hamstring tendon bundle is dissected out after the sciatic nerve has been identified and neurolysis performed.
Fig 2.
Intraoperative image of right ischium with the patient in prone position. The knee is flexed to 90° to aid mobilization of the tendon. The proximal hamstring tendon stump is identified and a tag stich is placed on the tendon stump (arrow). The gap between the tendon stump and the ischium is measured to determine the length of the graft needed.
The first Achilles tendon allograft is passed through the tendon stump in a Pulvertaft weave fashion. The graft is then secured back to itself and the hamstring tendon bundle using #5 FiberWire (Arthrex, Naples, FL) interrupted figure-of-8 sutures. Three #5 FiberWire sutures are then placed in a running locking fashion through the free end of the graft, as demonstrated in Fig 3. The second Achilles graft is then wrapped around this graft/native hamstring bundle, and interrupted 0 VICRYL sutures (Ethicon, Somerville, NJ) are used to secure the graft as a biologic covering, as shown in Fig 4.
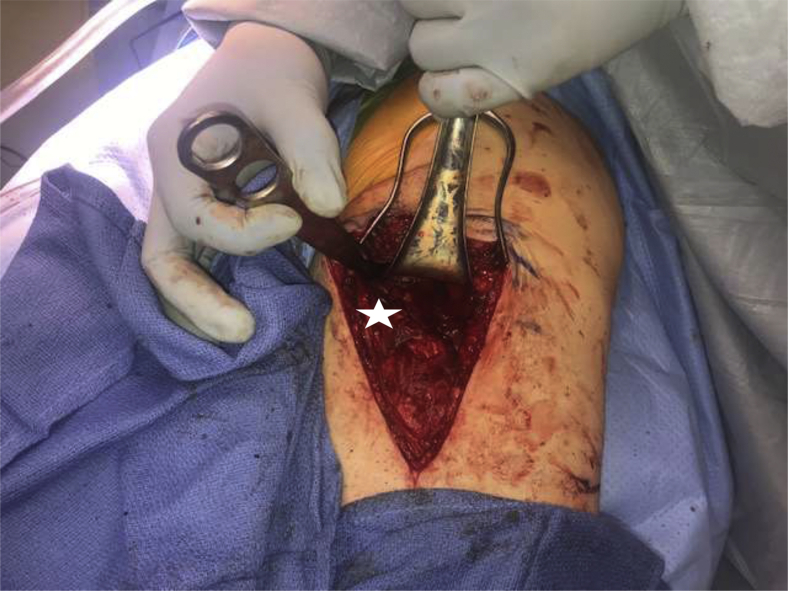
Fig 3.
Intraoperative image of right proximal hamstring tendon stump (arrow) augmented with an Achilles tendon (star) to bridge the gap. Here the first Achilles allograft has been passed in a Pulvertaft weave fashion and sewn back to itself with interrupted #5 FiberWire figure of 8 sutures. Proximally at the free end of the graft, three #5 FiberWire sutures have been passed in a running locking fashion.
Fig 4.
Intraoperative image of right proximal hamstring tendon stump with incorporation of the second Achilles allograft. The second graft (star) has been overwrapped around the allograft and native hamstring bundle and secured with interrupted 0 VICRYL sutures.
The next step is proximal fixation, which is illustrated in Appendix Video 1. The ischial tuberosity is exposed and all soft tissue cleared from the hamstring insertion site. Three 2.8-mm Q-FIX (Smith & Nephew, Andover, MA) anchors are secured to the inferior aspect of the tuberosity. Each suture limb is then passed through the allograft/native tendon bundle in a mattress fashion using a free needle from posterior to anterior. This is demonstrated in Fig 5. Each suture pair is clipped to prevent knotting and to allow the tendon to be zip lined as it is reduced to the ischium. Two 4.75-mm SwiveLock anchors (Arthrex) are then preloaded with the #5 FiberWire sutures that have been passed through the allograft. A bone punch is used to prepare for anchor placement on the proximal aspect of the ischium as shown in Appendix Video 1. At this point, the knee is held in 90° of flexion for appropriate tensioning. The anchors are then initially inserted. Each FiberWire suture is then sequentially tensioned reducing the allograft to the ischium. The anchors are then completely seated. Now having re-established the appropriate length tension on the native hamstrings and the allografts, the Q-FIX suture limbs are sequentially tied down so as to reinforce the repair between the allograft and the ischium. The final fixation is illustrated in Fig 6 and schematic representation as in Fig 7 along with Appendix Video 1. The knee is then gently taken through a 60° arc of motion while assessing for appropriate excursion of the hamstrings with no overdue tension or gapping at the repair site. A layered closure is performed with #1 VICRYL, 2-0 VICRYL, and running subcutaneous 4-0 MONOCRYL sutures followed by steri-strips.
Fig 5.
Intraoperative image of right proximal hamstring after placement of three 2.8-mm Q-FIX suture anchors into the ischial tuberosity. This image demonstrates passage of these sutures in a horizontal mattress fashion through the allograft and native hamstring bundle.
Fig 6.
Intraoperative image of right ischium with the patient in the prone position illustrating final fixation of the graft (star). The sutures from the 3 Q-FIX anchors have been sequentially tied down and the #5 FiberWire sutures at the free end of the graft have been loaded into 2 SwiveLock anchors and additionally fixed to the ischial tuberosity.
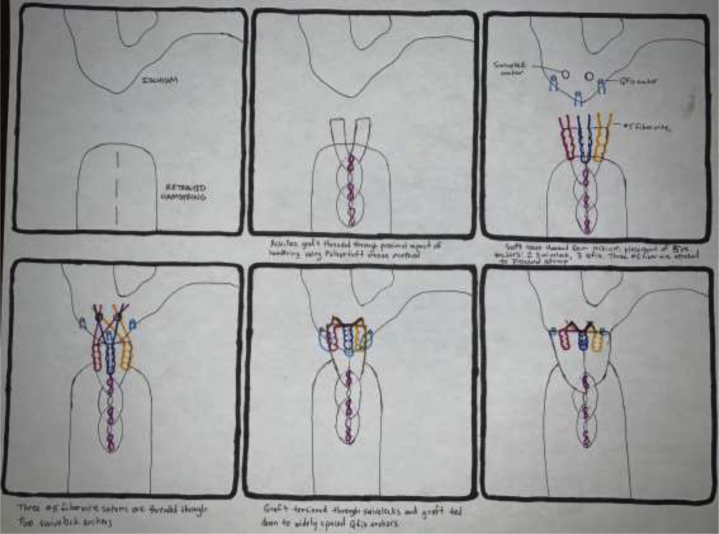
Fig 7.
Schematic diagram of a left ischium depicting the technique of tensioning the allograft from the tendon stump to the Q-FIX anchors.
Postoperative Rehabilitation
Postoperatively, the patient is placed in a total range of motion brace locked in 90° of flexion at the knee. The patient is advised not to perform any active hip extension so as to avoid excessive stress on the repair. Activity is restricted to toe-touch weight-bearing in the brace for 3 weeks followed by slow progression to full weight bearing. The full postoperative protocol can be accessed as part of the Appendix.
Discussion
Surgical management is generally recommended for proximal hamstring avulsions involving all 3 tendons, 2 tendon avulsions with >2-cm retraction, displaced bony avulsions, and patients with resulting chronic pain and functional impairment.2,9 This is most easily accomplished acutely after injury as a direct or primary repair. However, many patients still have a delayed presentation either secondary to missed diagnosis or an initial trial of nonoperative management.10,11 These chronic ruptures present a more challenging operation, as the tendon is often significantly retracted.9 Outcomes for return to sport and activities of daily living tend to be better with acute repair within 6 weeks of injury; however, overall patient satisfaction is still comparable with delayed repair and reconstruction. In addition, patients who undergo surgical reconstruction after chronic injuries have a greater incidence of return to sport and preinjury functional status compared with nonoperatively managed patients.5,6
While more technically challenging, surgical management of chronic tears is possible and can lead to acceptable outcomes. Cross et al.10 presented a series of 8 patients treated an average of 36 months after injury. Following primary repair in these chronic complete tears, hamstring muscles strength was 60% of the uninjured side and endurance averaged 57% compared with the uninjured side. In a systematic review of the literature on acute versus delayed repairs by Van der Made et al.,12 no statically significant differences were noted in return to sport, patient satisfaction, pain, or functional outcome scores. However, when the authors adjusted the Marx scale to tailor it specifically to hamstring function, there was a statistically significant greater function seen in acute repairs compared to delayed. Harris et al.11 performed a systematic review comparing operative and nonoperative management as well as clinical outcomes for acute versus chronic tears. They reported improved outcomes in those who presented acutely and underwent immediate repair, most significantly increased return to preinjury level of function. In addition, they noted acute repair allowed for a technically easier surgery with smaller incisions, less mobilization of tendon required, and decreased need for sciatic nerve neurolysis. These studies show that while acute repair leads to improved outcomes compared to chronic repair or reconstruction, operative treatment of chronic tears still leads to good results with improved function compared to ongoing non operative management.
Previously, multiple surgical approaches and techniques have been reported. Atzmon et al.9 described a combined endoscopic and open approach to allograft reconstruction involving endoscopic preparation of the ischial tuberosity proximally with open preparation of the retracted stump and Achilles tendon allograft bridging. They advised that while an endoscopic approach requires a smaller incision with reduced soft tissue undermining, it is technically difficult. Others have reported on open approaches involving either a transverse incision at the level of the ischial tuberosity or a longitudinal posterior midline incision. In chronic tears with a high degree of tendon retraction necessitating need for stump mobilization and sciatic nerve neurolysis, an extensile longitudinal incision is often used.3,13
Some studies have reported on direct repair in cases of chronic rupture. Wood et al.3 reported that all but one of their chronic cases were repaired directly by dissecting out the tendon stump and positioning the knee in flexion to facilitate apposition. Klingele and Sallay13 described use of distal fractional lengthening of the hamstring muscles to facilitate direct repair in chronic injuries. They made a series of chevron incisions distally in the biceps and semitendinosus tendons and were able to gain 2-3 cm of increased tendon excursion.
When tendon retraction reaches >5 cm, reconstruction using a graft is often necessary.5 While most techniques involve use of Achilles tendon allograft, other grafts have been described. Ebert et al.14 reported a case series of 6 patients who underwent reconstruction of chronic proximal hamstring avulsion injuries using ipsilateral distal hamstring autograft. They noted good outcomes with improved strength and endurance as well as return to recreational and sporting activities. Lempainen et al.15 reported on a series of 5 patients who underwent proximal hamstring reconstruction using an ipsilateral fascia lata autograft. The graft was secured with 3-4 suture anchors to the ischial tuberosity.
Variable techniques for graft fixation are also described. Rust et al.5 used a bone–tendon Achilles allograft and fixation with a titanium interference screw. Marx et al.16 describes the use of a nonabsorbable Krakow suture for Achilles allograft attachment to the native hamstring tendon stump. The knee was positioned in 90° flexion for fixation to the ischial tuberosity, which was accomplished using 2 suture anchors. Others have similarly used only 2 to 3 suture anchors for attachment to the tuberosity such as in the previously cited series by Klingele and Sallay, Ebert, as well as Atzmon et al.9,13,14 However, as described in a study by Moatshe et al.,17 the use of 5 anchors is biomechanically stronger and more similar to native hamstring tendon strength. While this technique was used in repair of acute injuries, the use of 5 suture anchors may improve strength of chronic reconstructions as well. Hamming et al.18 performed a biomechanical study on cadavers comparing intact tendon load to failure with that of tendons repaired by either 2 small suture anchors, 2 large suture anchors, or 5 small suture anchors. Repairs with 5 small suture anchors were significantly stronger and better approximated the strength of native intact hamstring tendon. While Moatshe et al.17 used this technique in acute repair of a proximal hamstring avulsion, we have expanded its use to reconstruction using allograft for chronic injuries. A review of advantages and disadvantages of this technique can be found in Table 1. Pearls and pitfalls of the operation are summarized in Table 2.
Table 1.
Advantages and Disadvantages of Allograft Augmentation Repair/Reconstruction of Chronic Proximal Hamstring Avulsion Injury
| Advantages | Disadvantages |
|---|---|
| Repair even in chronic injuries leads to improved outcomes with increased strength and return to preinjury sports and recreational activities. Use of 5 suture anchors better reproduces native hamstring tendon strength. Use of a second Achilles allograft as an overwrap prevents excessive adhesions post operatively which may decrease incidence of sciatic nerve symptoms. |
An extensile longitudinal approach is often needed for exposure and adequate mobilization of the retracted tendon stump. In chronic cases, adhesions and fibrous tissue make sciatic nerve neurolysis and mobilization of the retracted tendon stump more challenging. Significant tendon retraction >5 cm often precludes a direct repair and necessitates the use of allograft for reconstruction. |
Table 2.
Pearls and Pitfalls of Allograft Augmentation Repair/Reconstruction of Chronic Proximal Hamstring Avulsion Injury
| Pearls | Pitfalls |
|---|---|
| Correct knowledge of anatomy is key as adhesions in chronic injuries distort the anatomy making mobilization of the retracted tendon stump and sciatic nerve neurolysis more technically challenging. A longitudinal incision is recommended due to often significant tendon retraction in chronic injuries. Fixation with 5 suture anchors better reproduces native hamstring tendon attachment and strength. Small anchors may be used if the use of 5 suture anchors is not permitted by space. Graft fixation with the knee in 90° flexion decreases the length of gap needed to bridge. Additionally, bracing in 90° flexion postoperatively protects the reconstruction. |
In chronic injuries, tendon retraction often precludes a direct repair. In these cases, allograft augmentation is often necessary. Significant adhesions and tendon retraction distort the anatomy in chronic injuries. Care must be taken to identify all neurovascular structures to avoid iatrogenic injury. |
Unique to our reconstruction was the use of 2 Achilles tendon allografts. The first was secured with a combination of running locked sutures and a Pulvertaft weave construction. We then overlay a second allograft in a wrapped configuration. This provides an additional layer of fixation as well as a biologic overwrap to help limit adhesions between the allograft and the surrounding soft tissues and to prevent suture knot pain for the patient. In previously reported cases of chronic injuries, there can be significant retraction and scarring that can lead to entrapment of the sciatic nerve and development of nagging neurological symptoms.13 In our reported technique not only was the sciatic nerve identified and released, the second Achilles tendon graft also was used to limit possible adhesions with the sciatic nerve and subsequent neurologic pain.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Simulation of proximal hamstring reconstruction using the aforementioned technique via a sawbones model. The sawbones pelvis is positioned prone. A model graft is shown representing the Achilles allograft with demonstration of the suture technique used. The video then demonstrates placement of the suture anchors into the ischium with tensioning of the graft.
References
- 1.Ahmad C.S., Redler L.H., Ciccotti M.G., Maffulli N., Longo U.G., Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41:2933–2947. doi: 10.1177/0363546513487063. [DOI] [PubMed] [Google Scholar]
- 2.Cohen S., Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–355. doi: 10.5435/00124635-200706000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Wood D.G., Packham I., Trikha S.P., Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90:2365–2374. doi: 10.2106/JBJS.G.00685. [DOI] [PubMed] [Google Scholar]
- 4.Sallay P.I., Friedman R.L., Coogan P.G., Garrett W.E. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130–136. doi: 10.1177/036354659602400202. [DOI] [PubMed] [Google Scholar]
- 5.Rust D.A., Giveans M.R., Stone R.M., Samuelson K.M., Larson C.M. Functional Outcomes and Return to Sports After Acute Repair, Chronic Repair, and Allograft Reconstruction for Proximal Hamstring Ruptures. Am J Sports Med. 2014;42:1377–1383. doi: 10.1177/0363546514528788. [DOI] [PubMed] [Google Scholar]
- 6.Murray P.J., Lowe W.R. Achilles allograft reconstruction of a chronic complete proximal hamstring rupture. Knee Surg Sports Traumatol Arthrosc. 2009;17:1360–1363. doi: 10.1007/s00167-008-0670-3. [DOI] [PubMed] [Google Scholar]
- 7.Degen R.M. Proximal hamstring injuries: Management of tendinopathy and avulsion injuries. Curr Rev Musculoskelet Med. 2019;12:138–146. doi: 10.1007/s12178-019-09541-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mariani C., Caldera F.E., Kim W. Ultrasound versus magnetic resonance imaging in the diagnosis of an acute hamstring tear. PM R. 2012;4:154–155. doi: 10.1016/j.pmrj.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Atzmon R., Amar E., Maor D., Rath E. A combined endoscopic and open surgical approach for chronic retracted proximal hamstring avulsion. J Hip Preserv Surg. 2019;6:284–288. doi: 10.1093/jhps/hnz037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross M.J., Vandersluis R., Wood D., Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26:785–788. doi: 10.1177/03635465980260060801. [DOI] [PubMed] [Google Scholar]
- 11.Harris J.D., Griesser M.J., Best T.M., Ellis T.J. Treatment of proximal hamstring ruptures—a systematic review. Int J Sports Med. 2011;32:490–495. doi: 10.1055/s-0031-1273753. [DOI] [PubMed] [Google Scholar]
- 12.van der Made A.D., Reurink G., Gouttebarge V., Tol J.L., Kerkhoffs G.M. Outcome after surgical repair of proximal hamstring avulsions: A systematic review. Am J Sports Med. 2015;43:2841–2851. doi: 10.1177/0363546514555327. [DOI] [PubMed] [Google Scholar]
- 13.Klingele K.E., Sallay P.I. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742–747. doi: 10.1177/03635465020300051901. [DOI] [PubMed] [Google Scholar]
- 14.Ebert J.R., Gormack N., Annear P.T. Reconstruction of chronic proximal hamstring avulsion injuries using ipsilateral distal hamstring tendons results in good clinical outcomes and patient satisfaction. Knee Surg Sports Traumatol Arthrosc. 2019;27:2958–2966. doi: 10.1007/s00167-018-5310-y. [DOI] [PubMed] [Google Scholar]
- 15.Lempainen L., Sarimo J., Orava S. Recurrent and chronic complete ruptures of the proximal origin of the hamstring muscles repaired with fascia lata autograft augmentation. Arthroscopy. 2007;23:441.e1-5. doi: 10.1016/j.arthro.2006.07.044. [DOI] [PubMed] [Google Scholar]
- 16.Marx R.G., Fives G., Chu S.K., Daluiski A., Wolfe S.W. Allograft reconstruction for symptomatic chronic complete proximal hamstring tendon avulsion. Knee Surg Sports Traumatol Arthrosc. 2009;17:19–23. doi: 10.1007/s00167-008-0588-9. [DOI] [PubMed] [Google Scholar]
- 17.Moatshe G., Chahla J., Vap A.R., et al. Repair of proximal hamstring tears: A surgical technique. Arthrosc Tech. 2017;6:e311–e317. doi: 10.1016/j.eats.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamming M.G., Philippon M.J., Rasmussen M.T., et al. Structural properties of the intact proximal hamstring origin and evaluation of varying avulsion repair techniques: An in vitro biomechanical analysis. Am J Sports Med. 2015;43:721–728. doi: 10.1177/0363546514560878. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Simulation of proximal hamstring reconstruction using the aforementioned technique via a sawbones model. The sawbones pelvis is positioned prone. A model graft is shown representing the Achilles allograft with demonstration of the suture technique used. The video then demonstrates placement of the suture anchors into the ischium with tensioning of the graft.
Simulation of proximal hamstring reconstruction using the aforementioned technique via a sawbones model. The sawbones pelvis is positioned prone. A model graft is shown representing the Achilles allograft with demonstration of the suture technique used. The video then demonstrates placement of the suture anchors into the ischium with tensioning of the graft.