Abstract
PASTA (partial articular supraspinatus tendon avulsion) lesions are a subset of partial rotator cuff tears that are commonly treated by surgeons. Multiple surgical techniques exist for managing these lesions, including debridement, transtendinous repair, and completion of the tear and repair. Each of these techniques provides its own set of advantages and disadvantages, and currently there is no consensus on which method provides the best clinical outcomes or ease of procedure. Here, we present our repair technique for PASTA lesions, which involves a bursal split that takes the advantages of previous techniques by allowing improved visualization of the footprint and suture passing while avoiding the takedown any of Sharpey’s fibers.
Technique Video
The patient is positioned in the lateral position using 10 pounds of balanced suspension to distract the joint. A standard posterior portal is created, and routine diagnostic arthroscopy is performed. The location of the PASTA lesion is marked using a 18g needle and a 0 Prolene suture is inserted to tag the tear and help identify it in the subacromial space (Figure 1). Next the subacromial space is entered and a debridement of the bursa is performed through a lateral portal to allow for visualization of the rotator cuff tendon. The location of the tear is identified by the suture that was previously inserted (Figure 2). An underwater hooked electrocautery (Smith & Nephew electrode 45°blade) is used to make a longitudinal split in the tendon about the tear site in line with the tendon fibers. The size of our split is approximately 10mm (Figure 3). A shaver is then inserted to debride the tendon edges and prepare the anchor insertion site. A double-loaded Smith &d Nephew Healicoil suture anchor is placed under direct visualization at the edge of the articular surface. This is the main advantage of our technique, compared to other described methods (Figures 4 and 5). Next sutures are then passed in mattress fashion using the surgeons preferred passing technique. (Figure 6) We used an 18-gauge needle and Prolene suture to precisely place matress sutures through the tendon. The sutures are then tied down. (Figure 7) A probe is then used to identify the remaining longitudinal split in the tendon. A second double loaded Smith & Nephew Healicoil suture anchor is placed through the split. The arthroscope is placed in the lateral portal and sutures are passed to converge the split. A Synthes Mitek 45° IDEAL suture grasper is used to pass a mattress stitch through the anterior and posterior leaflets. The sutures are then tied to complete the repair (Figure 8).Next, one limb from each knot stack is grasped in preparation for a double row repair. The lateral row insertion site is prepared, and a knotless Smith and Nephew Footprint anchor is placed in standard fashion. Sutures are tensioned, then cut, and the repair is visualized from both the subacromial space and glenohumeral joint (Figure 9).
Partial-thickness rotator cuff tears (PTRCTs) are a common cause of shoulder pain, with an incidence of nearly 30% in the general population.1 Very little was known about the recognition and treatment of PTRCTs until arthroscopy and magnetic resonance imaging gained recognition in the 1990s. Partial rotator cuff tears are now further classified as articular-sided, bursal-sided, or intra-tendinous. PASTA (partial articular supraspinatus tendon avulsion) lesions are by far the most common, comprising 91% of all PTRCTs.2 It is postulated that intrinsic, extrinsic, and traumatic mechanisms are all possible causes of PASTA lesions. Changes in rotator cuff vascularity and metabolic changes associated with aging are the most common intrinsic factors studied. Extrinsic factors include shear stresses that affect the supraspinatus tendon due to narrowing of the coracoacromial arch, repetitive microtrauma especially associated with overhead activities, and internal impingement as it occurs due to repetitive contact of the articular surface of the supraspinatus and infraspinatus tendon with the posterosuperior part of the glenoid during overhead activities.
Despite many advances in our understanding of PASTA lesions, the natural history of these tears remains unclear. Conservative treatment of PASTA lesions includes nonsteroidal anti-inflammatory drugs, rest, physical therapy, and corticosteroid injections. However, spontaneous healing of PTRCTs is unlikely, and therefore surgery is often required. There are 3 primary surgical techniques for managing these types of lesions, and they include debridement, transtendinous repair, or takedown and repair (Table 1). Debridement has been recommended as the surgical treatment of choice in tears involving less than 50% of the tendon thickness whereas repair is recommended with greater than 50% involvement of the tendon. Classically, acute tears in younger patients are treated with in situ repair whereas degenerative tears in older patients are treated with tear completion, debridement, and repair. Currently, there is no consensus on which technique offers the best clinical and functional outcomes, and there continues to be variation and innovation in surgical techniques used for these rotator cuff tears. The purpose of this article is to describe a minimally invasive technique for transtendinous repair of PASTA lesions that avoids disruption of Sharpey’s fibers but still allows good visibility for footprint preparation and suture passage.
Table 1.
Pros and Cons of Various Repair Techniques
| Technique | Pros | Cons |
|---|---|---|
| Bursal split | Improved visualization | Potentially larger bursal incision |
| Easier to prepare footprint and insert anchor | ||
| No disruption of Sharpey's fibers | ||
| Free access for suture passing | ||
| Transtendinous repair | Smaller bursal incision | Decreased visualization |
| Difficult to pass sutures | ||
| Takedown and repair | Similar to standard rotator cuff repair | Disruption of Sharpey's fibers |
| Improved visualization | Conversion to full-thickness tear takes down a large area of healthy tissue |
Surgical Technique (With Video Illustration)
The patient is positioned in the lateral position using 10 pounds of balanced suspension to distract the joint. A standard posterior portal is created, and a routine diagnostic arthroscopy is performed. The location of the PASTA lesion is marked using an 18-g needle, and a 0 PROLENE suture is inserted to tag the tear and help identify it in the subacromial space (Video 1, Fig 1).
Fig 1.
The circle demonstrates passage of a 0 PROLENE suture through an 18-g needle, which is inserted to tag the tear and help identify it in the subacromial space.
Next, the subacromial space is entered and a debridement of the bursa is performed through a lateral portal to allow for visualization of the rotator cuff tendon. The location of the tear is identified by the marking suture that was previously inserted (Fig 2).
Fig 2.
The subacromial space is entered and the bursa is debrided to allow visualization of the rotator cuff tendon.
An underwater electrocautery hook (electrode 45° blade; Smith & Nephew, Andover, MA) is used to make a longitudinal split in the tendon about the tear site in line with the tendon fibers. The size of our split is approximately 10 mm (Fig 3).
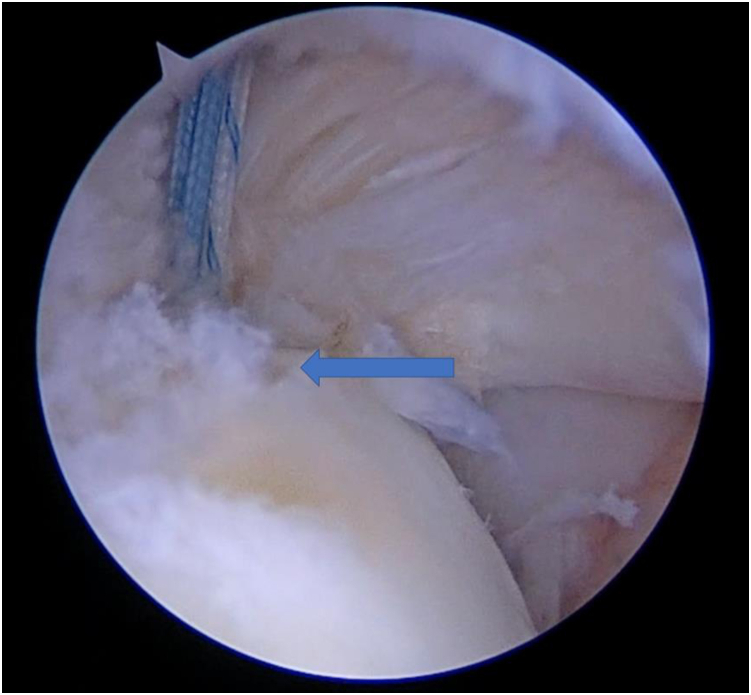
Fig 3.
An electrocautery hook is used to make a longitudinal split in the tendon in line with the tendon fibers measuring approximately 10 mm. The split is centered at the suture, as indicated by the arrow.
A shaver is then inserted to debride the PASTA lesion and prepare the anchor insertion site. A double-loaded Smith & Nephew HEALICOIL suture anchor is placed under direct visualization at the edge of the articular surface. This is the main advantage of our technique, compared to other described methods (Figs 4 and 5).
Fig 4.
A shaver is inserted to debride the PASTA lesion and prepare the anchor insertion site at the articular margin (arrow).
Fig 5.
A double-loaded suture anchor is placed at the edge of the articular margin (arrow).
Next. sutures are then passed in mattress fashion using the surgeons preferred passing technique (Fig 6). We used an 18-gauge needle and PROLENE suture to precisely place mattress sutures in the tendon.
Fig 6.
Sutures are then passed in mattress fashion using the surgeon’s preferred technique.
The sutures are then tied using arthroscopic knot-tying techniques (Fig 7). A probe is then used to identify the remaining longitudinal split in the tendon. A second double-loaded Smith & Nephew HEALICOIL suture anchor is placed through the bursal split. The arthroscope is placed in the lateral portal and sutures are passed to converge the split. A 45° IDEAL suture grasper (DePuy Synthes Mitek, Raynham, MA) is used to pass a mattress suture with one limb in each leaflet. The sutures are then tied to complete the repair (Fig 8).
Fig 7.
Sutures are then tied down and a probe is used to identify the remaining longitudinal split.
Fig 8.
Viewing from the lateral portal. A second-double loaded suture anchor is placed through the bursal split. A simple suture is used to converge the tear.
Next, one limb from each knot stack is grasped in preparation for a double-row repair. The lateral row insertion site is prepared, and a knotless Smith & Nephew FOOTPRINT anchor is placed in standard fashion. Sutures are tensioned, then cut, and the repair is visualized from both the subacromial space and glenohumeral joint (Fig 9). The pearls and pitfalls of this technique are discussed in Table 2.
Fig 9.
Finally, one limb from each suture is grasped in preparation for a double-row repair. The lateral row insertion site is prepared and a knotless suture anchor is placed in standard fashion. The image on the right demonstrates the intra-articular view after repair.
Table 2.
Pearls and Pitfalls
| Pitfalls | Pearls |
|---|---|
| Don’t make split too medial | Mark appropriate location of split using PROLENE marking suture |
| Avoid injury to articular surface | Make split over footprint for improved visualization for anchor insertion |
| Bursal split not in line with bursal fibers | Incisions in-line with the fibers allow for side-to-side tendon healing after repair |
| Partial-thickness repair | Articular side of tear is typically retracted medially. Before placing a passing suture, use a grasper from the lateral portal to pull the articular portion of tear laterally to aid in passing sutures |
| Adequacy of repair | Pull on sutures before tying knots to confirm adequacy of repair from glenohumeral joint |
Discussion
Multiple techniques have been proposed for dealing with PASTA lesions. Our technique has several distinct advantages compared with traditional percutaneous repair methods. First, the longitudinal split in the tendon allows for better visualization of the rotator cuff footprint for preparation and anchor placement. This same incision and split also creates improved access for the passage and shuttling of instruments and sutures. Lastly, this technique does not require the take down of Sharpey’s fibers to repair the lesion. We believe that the preservation of these fibers may preserve the healing response, maintain the integrity of those fibers that are still intact, and provide similar healing rates to percutaneous methods, although this has yet to be investigated through clinical trials. Despite these benefits, this procedure may be associated with some theoretical risks. This procedure requires disruption of intact bursal fibers, which may create more tendon disruption to heal. In our view, we believe the bursal split is less traumatic than percutaneous anchor placement and easier to repair. The technique is also limited by appropriate location and length of the bursal split. Increased technical skill is required to pass instruments through the subacromial space and through the split while viewing through the glenohumeral joint. It is the authors’ belief that the benefits of the proposed technique outweigh these disadvantages; however, no data are currently available.
Patient-reported outcomes, such as those reported by Deutsch3 and Porat et al.,4 have been very promising, with significant improvements reported in American Shoulder and Elbow scores, pain relief, and overall satisfaction. There is still controversy in the literature regarding differences in the technique used for in situ repair, as no technique thus far has demonstrated a clear advantage.5 A recent study investigating long term follow-up with a minimum of 8 years after in situ repair of partial-thickness rotator cuff tear has demonstrated excellent functional outcomes in more than 80% of patients. No revision surgeries were performed, and 3 patients developed adhesive capsulitis.6 We expect our patients to do similarly well, as our repair should produce reliable tendinous healing. We believe there is considerable upside to this procedure compared with the transtendinous and complete takedown techniques, although outcome studies are needed to fully evaluate its clinical efficacy.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned in the lateral position using 10 pounds of balanced suspension to distract the joint. A standard posterior portal is created, and routine diagnostic arthroscopy is performed. The location of the PASTA lesion is marked using a 18g needle and a 0 Prolene suture is inserted to tag the tear and help identify it in the subacromial space (Figure 1). Next the subacromial space is entered and a debridement of the bursa is performed through a lateral portal to allow for visualization of the rotator cuff tendon. The location of the tear is identified by the suture that was previously inserted (Figure 2). An underwater hooked electrocautery (Smith & Nephew electrode 45°blade) is used to make a longitudinal split in the tendon about the tear site in line with the tendon fibers. The size of our split is approximately 10mm (Figure 3). A shaver is then inserted to debride the tendon edges and prepare the anchor insertion site. A double-loaded Smith &d Nephew Healicoil suture anchor is placed under direct visualization at the edge of the articular surface. This is the main advantage of our technique, compared to other described methods (Figures 4 and 5). Next sutures are then passed in mattress fashion using the surgeons preferred passing technique. (Figure 6) We used an 18-gauge needle and Prolene suture to precisely place matress sutures through the tendon. The sutures are then tied down. (Figure 7) A probe is then used to identify the remaining longitudinal split in the tendon. A second double loaded Smith & Nephew Healicoil suture anchor is placed through the split. The arthroscope is placed in the lateral portal and sutures are passed to converge the split. A Synthes Mitek 45° IDEAL suture grasper is used to pass a mattress stitch through the anterior and posterior leaflets. The sutures are then tied to complete the repair (Figure 8).Next, one limb from each knot stack is grasped in preparation for a double row repair. The lateral row insertion site is prepared, and a knotless Smith and Nephew Footprint anchor is placed in standard fashion. Sutures are tensioned, then cut, and the repair is visualized from both the subacromial space and glenohumeral joint (Figure 9).
References
- 1.Yamamoto A., Takagishi K., Osawa T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Gartsman G.M., Milne J.C. Articular surface partial-thickness rotator cuff tears. J Shoulder Elbow Surg. 1995;4:409–415. doi: 10.1016/s1058-2746(05)80031-x. [DOI] [PubMed] [Google Scholar]
- 3.Deutsch A. Arthroscopic repair of partial-thickness tears of the rotator cuff. J Shoulder Elbow Surg. 2007;16:193–201. doi: 10.1016/j.jse.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Porat S., Nottage W.M., Fouse M.N. Repair of partial thickness rotator cuff tears: A retrospective review with minimum two-year follow-up. J Shoulder Elbow Surg. 2008;17:729–731. doi: 10.1016/j.jse.2008.02.019. [DOI] [PubMed] [Google Scholar]
- 5.Castricini R., La Camera F., De Gori M. Functional outcomes and repair integrity after arthroscopic repair of partial articular supraspinatus tendon avulsion. Arch Orthop Trauma Surg. 2019;139:369–375. doi: 10.1007/s00402-018-3044-4. [DOI] [PubMed] [Google Scholar]
- 6.Rossi L.A., Atala N.A., Bertona A. Long-term outcomes after in situ arthroscopic repair of partial rotator cuff tears. Arthroscopy. 2019;35:698–702. doi: 10.1016/j.arthro.2018.09.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned in the lateral position using 10 pounds of balanced suspension to distract the joint. A standard posterior portal is created, and routine diagnostic arthroscopy is performed. The location of the PASTA lesion is marked using a 18g needle and a 0 Prolene suture is inserted to tag the tear and help identify it in the subacromial space (Figure 1). Next the subacromial space is entered and a debridement of the bursa is performed through a lateral portal to allow for visualization of the rotator cuff tendon. The location of the tear is identified by the suture that was previously inserted (Figure 2). An underwater hooked electrocautery (Smith & Nephew electrode 45°blade) is used to make a longitudinal split in the tendon about the tear site in line with the tendon fibers. The size of our split is approximately 10mm (Figure 3). A shaver is then inserted to debride the tendon edges and prepare the anchor insertion site. A double-loaded Smith &d Nephew Healicoil suture anchor is placed under direct visualization at the edge of the articular surface. This is the main advantage of our technique, compared to other described methods (Figures 4 and 5). Next sutures are then passed in mattress fashion using the surgeons preferred passing technique. (Figure 6) We used an 18-gauge needle and Prolene suture to precisely place matress sutures through the tendon. The sutures are then tied down. (Figure 7) A probe is then used to identify the remaining longitudinal split in the tendon. A second double loaded Smith & Nephew Healicoil suture anchor is placed through the split. The arthroscope is placed in the lateral portal and sutures are passed to converge the split. A Synthes Mitek 45° IDEAL suture grasper is used to pass a mattress stitch through the anterior and posterior leaflets. The sutures are then tied to complete the repair (Figure 8).Next, one limb from each knot stack is grasped in preparation for a double row repair. The lateral row insertion site is prepared, and a knotless Smith and Nephew Footprint anchor is placed in standard fashion. Sutures are tensioned, then cut, and the repair is visualized from both the subacromial space and glenohumeral joint (Figure 9).
The patient is positioned in the lateral position using 10 pounds of balanced suspension to distract the joint. A standard posterior portal is created, and routine diagnostic arthroscopy is performed. The location of the PASTA lesion is marked using a 18g needle and a 0 Prolene suture is inserted to tag the tear and help identify it in the subacromial space (Figure 1). Next the subacromial space is entered and a debridement of the bursa is performed through a lateral portal to allow for visualization of the rotator cuff tendon. The location of the tear is identified by the suture that was previously inserted (Figure 2). An underwater hooked electrocautery (Smith & Nephew electrode 45°blade) is used to make a longitudinal split in the tendon about the tear site in line with the tendon fibers. The size of our split is approximately 10mm (Figure 3). A shaver is then inserted to debride the tendon edges and prepare the anchor insertion site. A double-loaded Smith &d Nephew Healicoil suture anchor is placed under direct visualization at the edge of the articular surface. This is the main advantage of our technique, compared to other described methods (Figures 4 and 5). Next sutures are then passed in mattress fashion using the surgeons preferred passing technique. (Figure 6) We used an 18-gauge needle and Prolene suture to precisely place matress sutures through the tendon. The sutures are then tied down. (Figure 7) A probe is then used to identify the remaining longitudinal split in the tendon. A second double loaded Smith & Nephew Healicoil suture anchor is placed through the split. The arthroscope is placed in the lateral portal and sutures are passed to converge the split. A Synthes Mitek 45° IDEAL suture grasper is used to pass a mattress stitch through the anterior and posterior leaflets. The sutures are then tied to complete the repair (Figure 8).Next, one limb from each knot stack is grasped in preparation for a double row repair. The lateral row insertion site is prepared, and a knotless Smith and Nephew Footprint anchor is placed in standard fashion. Sutures are tensioned, then cut, and the repair is visualized from both the subacromial space and glenohumeral joint (Figure 9).