Abstract
BACKGROUND AND PURPOSE: Recurrent pain after vertebroplasty is relatively common, usually representing a new fracture at a different vertebral level. In a small cohort described herein, clinical and imaging findings indicated that recurrent pain arose from abnormality of the previously treated level. Our purpose was to demonstrate that repeat percutaneous vertebroplasty performed within the same fractured vertebra can offer therapeutic benefit for patients with recurrent pain after initial treatment.
METHODS: We conducted a retrospective review of consecutive vertebroplasty procedures performed at our institution to define a patient population that underwent repeat vertebroplasty for recurrent pain at previously treated vertebral levels. We identified six such patients over an 8-year period, and clinical outcomes were assessed through quantitative measurements of pre- and postoperative levels of pain and mobility.
RESULTS: Initial vertebroplasty resulted in substantial improvement in pain in all six patients. Patients developed recurrent pain between 8 days and 167 days after initial vertebroplasty. After repeat vertebroplasty, five of the six patients reported a reduction of at least 3 points in their rating of pain, with a mean reduction of 6.5 points and a mean postoperative pain level of 3.5 points (11-point scale). Four of six patients reported impaired mobility before repeat vertebroplasty, and all four demonstrated a postoperative improvement in mobility. Mean increase in mobility was 1.50 points, and the mean postoperative mobility impairment was 0.25 points (5-point scale).
CONCLUSION: The clinical outcomes of the patients within this case series suggest that repeat percutaneous vertebroplasty performed at previously treated vertebral levels for recurrent pain offer therapeutic benefit.
In recent years, percutaneous vertebroplasty has surfaced as an effective, minimally invasive treatment for painful osteoporotic vertebral compression fractures (1–7). Recurrent pain after vertebroplasty is relatively common and usually represents a new fracture at a different vertebral level (8). In a small cohort described herein, clinical and imaging findings suggested that recurrent pain arose from continued abnormality of the previously treated level. In this study, we report the therapeutic courses of six patients treated at our institution with recurrent pain after initial percutaneous vertebroplasty who underwent repeat procedures at the previously treated levels. Our purpose was to demonstrate that repeat percutaneous vertebroplasty performed within the same fractured vertebra can offer therapeutic benefit for such patients with recurrent pain after initial treatment.
Methods
We conducted a retrospective review of the records of consecutive percutaneous vertebroplasty procedures performed at our institution to define a population of patients that underwent repeat vertebroplasty procedures for recurrent pain at previously treated vertebral levels (Table 1). Among 250 patients treated between 1983 and 2001, we identified six such patients, and clinical outcomes were assessed through quantitative measurements of pre- and postoperative levels of pain (11-point scale) and mobility (5-point scale). Within our chart review, we looked at both parameters as reported on the day before the procedure, with follow-up on postoperative day 1 and again between 1 week and 1 month postoperatively.
TABLE 1:
Patient characteristics
| Patient (No.) | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Sex | F | M | F | F | F | M |
| Age (y) | 66 | 78 | 49 | 56 | 67 | 76 |
| Re-treated level | L1 | L2 | T6 | L1 | T10 | L1 |
| Interoperative interval (days) | 167 | 18 | 8 | 22 | 9 | 21 |
| Approach | ||||||
| Initial treatment | L* | B† | L | L | L | L |
| Repeat treatment | R‡ | R | R | L | R | R |
| Amount PMMA (cc) | ||||||
| Initial treatment | 3.5 | 15 | 5 | 1.1 | 1.2 | 3 |
| Repeat treatment | 1.5 | 5 | 1.5 | 2.5 | 3.5 | 1.2 |
| Initial Treatment | ||||||
| Preoperative pain | 10 | 10 | 10 | 10 | 7 | 10 |
| Postoperative pain | 0 | 5 | 0 | 0 | 3 | 3 |
| Preoperative mobility | 0 | 2 | 0 | 3 | 0 | 1 |
| Postoperative mobility | 0 | 1 | 0 | 0 | 0 | 0 |
| Repeat treatment | ||||||
| Preoperative pain | 10 | 10 | 10 | 10 | 10 | 10 |
| Postoperative pain | 8 | 1 | 2 | 0 | 4 | 6 |
| Preoperative mobility | 1 | 2 | 1 | 0 | 0 | 3 |
| Postoperative mobility | 0 | 1 | 0 | 0 | 0 | 0 |
Note.—Pain was assessed using an 11-point scale (0–10), with 0 representing no pain and 10 representing “most pain ever experienced.” Mobility was assessed using a 5-point scale as follows: 0, walking without assistance; 1, walking with assistance; 2, wheelchair bound; 3, restricted to sitting in bed; 4, restricted to lying flat in bed. Follow-up was obtained between 1 week and 1 month postoperatively.
Left unilateral transpediculate approach.
Bilateral transpediculate approach.
Right unilateral transpediculate approach.
The six patients included in the study had undergone initial percutaneous vertebroplasty procedures for radiologically confirmed vertebral compression fractures with pain that had remained refractory to appropriate medical management and bed rest. Patient selection for vertebroplasty included a thorough medical history, physical examination, and imaging studies varying from radiography, CT, MR imaging, or bone scanning, depending on clinical indications. The initial procedures all proceeded without complication. Of the five unilateral transpediculate approaches, operators noted bilateral filling of the vertebral body in four subjects, with one procedure demonstrating only unilateral filling. In this case, technical considerations dissuaded the attempt to canalize the contalateral hemiverteba. All six subjects reported severe preoperative pain, and three of six reported preoperative impaired mobility. Follow-up on postoperative day 1 after initial treatment demonstrated a significant improvement in pain for all six subjects and improved mobility in all three previously impaired subjects. After periods of reduced pain of varying lengths, each of the subjects returned with renewed complaints of back pain similar to that experienced before initial vertebroplasty. Subjects were selected for repeat vertebroplasty on the basis of the same diagnostic procedures as previously performed for the initial treatments, including medical history, physical examination, and appropriate imaging studies. Radiologic workup of these patients demonstrated abnormal findings only at the previously treated vertebral levels, as depicted in Table 2.
TABLE 2:
Findings in patients before repeat treatment, including those at physical examination and imaging
| Patient (No.) | Findings at Physical Examination | Imaging Findings |
|---|---|---|
| 1 | Point tenderness over L1 spinous process | Increased uptake at L1 on bone scan |
| 2 | Point tenderness over L2 spinous process | Increased uptake at L2 on bone scan |
| 3 | Point tenderness over T6, T7 spinous processes | Increased compression of T6 on radiograph |
| 4 | Tenderness 4 inches lateral to L1 spinous process | Stable fracture with diffuse edema at L1 on MR image |
| 5 | Point tenderness over T10 spinous process | Increased radiotracer uptake at T10 on bone scan |
| 6 | Point tenderness over L1 spinous process | No evidence of new fracture on CT scan |
The operators performing vertebroplasty believed these new episodes of back pain to represent new fractures within the same vertebral levels, possibly occurring around previously deposited cement or propagating as a result of insufficient initial cement deposition. As such, we interpreted these findings to demonstrate secondary failures, rather than primary failures of the initial treatments. Procedural reports documented no complications or difficulties in the either the initial or repeat treatments.
The interprocedural period for the six patients ranged from 8 days to 167 days, with a mean duration of 41 days; during that interval, none of the subjects underwent other invasive procedures to alleviate their back pain. Conservative management of varying degree and duration were attempted, consisting of analgesics and bed rest. One patient received facet injections at the time of repeat treatment at separate vertebral levels from that of the vertebroplasty procedure. Radicular signs on physical examination and bone scan findings of increased uptake of radiotracer guided this ancillary procedure.
Results
The study group included four women and two men, with a mean age of 65 years (range, 49–78 years). Initial treatments entailed five unilateral transpediculate approaches and one bilateral transpediculate approach, with a mean cement volume of 4.8 mL Repeat vertebroplasty was performed on the basis of the following findings: one patient demonstrated continued point tenderness over the previously treated fracture; one patient demonstrated continued point tenderness over the previously treated fracture and increased compression was seen on radiographs; one patient demonstrated edema on MR images; and three patients demonstrated continued point tenderness over the previously treated fracture and increased radiotracer uptake on a bone scan. The interoperative period between treatment and repeat treatment ranged from 8 days to 167 days, with a mean of 40.8 days. Repeat treatment consisted of six unilateral transpediculate approaches contralateral to the initial treatment in all but one case, with a mean cement volume of 2.5 mL After repeat treatment, five (83%) of the six patients demonstrated reduction of at least 3 points in their rating of pain, with a mean reduction of 6.5 points and a mean postoperative pain level of 3.5 points. Four of six patients reported impaired mobility before repeat treatment, and all four (100%) demonstrated an improvement in mobility. Mean increase in mobility was 1.5 points, and the mean postoperative mobility level was 0.25 points. A representative case is given below.
Case 1
A 76 year-old man presented to his primary care physician complaining of severe low back pain of 3 months’ duration that continued to be refractory to conservative management. He reported midline back pain at his belt line with radiation to his left hip, and he was using a walker to assist in ambulation. Physical examination elicited tenderness to palpation over his L1 vertebra, as well as over his left sacroiliac joint, without any focal neurologic findings. Findings at conventional radiography performed at this visit were unchanged from those obtained at the onset of symptoms and demonstrated a 60% compression fracture of his L1 vertebra. A subsequent bone scan demonstrated increased uptake of radiotracer at the L1 level, and MR imaging demonstrated edema at the same level. At that time, he was referred to our institution for evaluation for candidacy for percutaneous vertebroplasty.
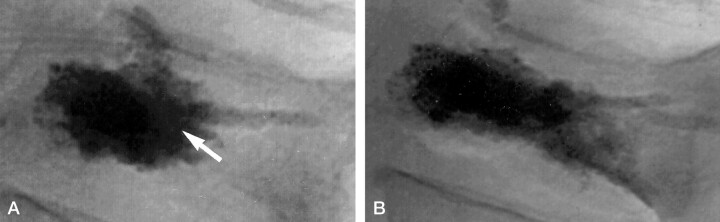
After undergoing a screening and preprocedural workup, as described by Jensen et al (9), he underwent a percutaneous vertebroplasty procedure, performed as described by Kim et al (10). Using a left unilateral transpediculate approach, the operator injected 3 mL of PMMA cement and noted an opacification pattern that filled both hemivertebrae, as seen on an anteroposterior radiograph, and filled predominantly the anterior half of the vertebral body, as seen on a lateral radiograph (Figure 1A). Preoperatively, the patient reported pain of 10/10 in severity, with mobility restricted to the use of a walker to assist with ambulating. At 1 week postoperatively, however, he reported complete pain relief (0/10 in severity), with no restriction of mobility.
Fig 1.
76-year-old man with L1 vertebral body fracture.
A, Lateral conventional radiograph after initial vertebroplasty. After administration of 3 mL of cement via a left unilateral transpediculate approach, the cement opacifies the anterior portion of the vertebral body (arrow). The patient reported complete pain relief after the procedure.
B, Lateral conventional radiograph after repeat vertebroplasty. After administration of an additional 1.2 mL of cement via a right unilateral transpediculate approach, the filling pattern has changed from A to include prominent posterior opacification. The patient reported moderate pain relief after the procedure.
Over the course of the next 2 weeks, the patient’s back pain recurred and progressively worsened. He returned to his primary care physician and reported low back pain and left hip pain identical to that experienced preoperatively. Physical examination again elicited tenderness to palpation over his L1 vertebra, as well as over his left sacroiliac joint, without any focal neurologic findings. Conventional radiography performed at that time showed no interval change from images acquired immediately postoperatively. A CT scan showed no evidence of new fracture, infection, abnormal cement placement, or herniated disk.
At that time, he was referred to our institution again for evaluation for candidacy for percutaneous vertebroplasty. Despite the absence of new radiologic findings, we opted to re-treat the L1 vertebral body on the basis of the patient’s medical history and physical findings. The procedure was again performed as described by Kim et al (10), this time by using a right transpediculate approach with the injection of 1.2 mL of PMMA cement. The cement-filling pattern visualized on a lateral radiograph changed from the initial procedure to include prominent posterior opacification (Figure 1B). The patient also received left L3–L4 and left L4–L5 facet injections to alleviate the left hip pain because of the findings on a previous bone scan demonstrating increased uptake of radiotracer at the facets at those levels. Preoperatively, the patient reported pain of 10/10 in severity, with mobility restricted to sitting in bed. At 1 week postoperatively, however, he reported moderate pain relief, with a reduction in pain to 6/10 in severity, and his only restriction in mobility was the use of a walker to assist in ambulating.
Discussion
Percutaneous vertebroplasty has rapidly evolved into an effective, minimally invasive procedure for the treatment of osteoporotic compression fractures. Numerous studies have been published demonstrating significant improvements in pain and mobility in as many as 95% of patients treated with the procedure for such lesions (1–7). No data currently exist, however, that evaluate the clinical outcomes of patients re-treated because of recurrent pain. Most patients treated at our institution for their vertebral fractures have osteoporosis. Thus, with osteoporosis being a diffuse process, many patients treated at our institution present with recurrent pain. Usually, diagnostic evaluation of this recurrent pain demonstrates a new compression fracture at a different vertebral level, and most of these patients have benefited from repeat procedures performed at the newly fractured level. Thorough evaluation of this cohort before repeat treatment, however, evinced no findings other than continued abnormality at the previously treated level.
The clinical outcomes of the patients within this case series suggest that repeat percutaneous vertebroplasty performed at previously treated vertebral levels for recurrent pain may offer a therapeutic benefit. Indeed, our cohort showed excellent pain relief after repeat treatment, with five (83%) of six subjects demonstrating significant pain relief and all four (100%) with preoperative impaired mobility demonstrating improvement postoperatively. This cohort, which comprises the sum of patients re-treated at the same vertebral level at our institution over the past 8 years, represents a diagnostic quandary. All six patients demonstrated clinical improvement after their initial treatment, only to return with recurrent back pain. Diagnostic workup of this recurrent pain (Table 2), which included history and physical examination, as well as radiologic studies, evinced abnormalities only in the previously treated vertebral levels.
The mechanism behind their continued physical and radiographic abnormalities remains unclear. These abnormalities could represent new fractures around the PMMA cement or poor fracture healing from insufficient cement filling. With five out of the six patients presenting within 1 month of their initial procedure, either one of these theories may explain the increased uptake of radiotracer on bone scans and evidence of edema on MR images and CT scans. It remains possible that the need for repeat treatment resulted from inadequate cement deposition, especially since most patients were treated with a unilateral rather than a bilateral approach. However, short-term relief was seen in all of the patients, suggesting that sufficient cement deposition occurred. Also, we have recently reported no difference in clinical outcome between unipediculate and bipediculate approaches (10), suggesting that the presentations of recurrent pain in this series did not result from unipediculate approaches. Whatever the mechanism, repeat treatment at the previously treated vertebral level offered significant clinical benefit.
Although this case series represents a unique examination of this relatively uncommon phenomenon, it suffers limitations. Its retrospective nature lacks the randomization of a prospective clinical trial, and the small, heterogeneous sample of patients likely lacks the power necessary to demonstrate statistically significant data. Prospective studies and larger patient populations may aid in improving the power of such a hypothesis and expand the fund of knowledge that we currently possess about this promising intervention. Also, the use of ancillary procedures such as facet injections, used concurrently with vertebroplasty procedures, may be confounding factors in the therapeutic benefit derived by this cohort. This occurred in only one patient, however, and the treatment was guided by physical findings and imaging studies indicating facet disease at separate vertebral levels from that treated during repeat vertebroplasty.
The mechanism of therapeutic benefit of percutaneous vertebroplasty remains elusive. Does the injected cement provide structural support, inhibiting further compression, or does the heat emitted from the highly exothermic solidification process offer pain relief? Or, is the therapeutic benefit nothing more than a dramatic placebo effect? Deciphering this mechanism may lead us to understand why the procedure works for most patients, and more importantly, why it fails to work for those unlucky few. Can the results found in this case series be extrapolated to those patients who report primary failure of vertebroplasty and may repeat treatment at the same level offer them clinical improvements? These are some of the questions that remain uncertain and necessitate prospective, randomized trials to elucidate the truth.
Conclusion
The clinical outcomes of the patients within this case series suggest that repeat percutaneous vertebroplasty procedures performed at previously treated vertebral levels for recurrent pain offer therapeutic benefit.
References
- 1.Chiras J, Depriester C, Weill A, Sola-Martinez MT, Deramond H. Vertebroplasties purcutanees. J Neuroradiol 1997;24:45–59 [PubMed] [Google Scholar]
- 2.Gangi A, Kastler BA, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR Am J Neuroradiol 1994;15:83–86 [PMC free article] [PubMed] [Google Scholar]
- 3.Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology 2000;39:1410–1414 [DOI] [PubMed] [Google Scholar]
- 4.Martin JB, Jean B, Sugui K, et al. Vertebroplasty: clinical experience and follow-up results. Bone 1999;25[suppl]:11S–15S. [DOI] [PubMed] [Google Scholar]
- 5.Maynard AS, Jensen ME, Schweickert PA, Marx WF, Short JG, Kallmes DF. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol 2000;21:1807–1812 [PMC free article] [PubMed] [Google Scholar]
- 6.Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol 2001;22:373–381 [PMC free article] [PubMed] [Google Scholar]
- 7.Weill A, Chiras J, Simon JM, Rose M, SolaMartinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology 1996;99:241–247 [DOI] [PubMed] [Google Scholar]
- 8.Jensen ME, Kallmes DF, Schweickert PA, Marx WF, Short JG. Percutaneous vertebroplasty does not increase the risk of adjacent vertebral fractures. Presented at the annual meeting of the ASNR; San Diego, CA:1999
- 9.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in treatment of osteoporotic vertebral fractures: technical factors. AJNR Am J Neuroradiol 1997;18:1897–1904 [PMC free article] [PubMed] [Google Scholar]
- 10.Kim AK, Jensen ME, Dion JE, Schweickert PA, Kaufmann TJ, Kallmes DF. Unilateral transpedicular vertebroplasty: initial experience. Radiology 2002;222:737–741 [DOI] [PubMed] [Google Scholar]