Abstract
Iatrogenic hip instability is increasingly recognized as a cause of persistent pain and disability after hip arthroscopy. Many authors currently advocate capsular repair to reduce postoperative instability. However, anatomic deficiencies in the anterosuperior capsule can prevent a functional capsular repair, particularly in the revision setting. Capsular reconstruction has been shown to restore biomechanical stabilization in cadaveric models and improve short-term patient outcomes in patients with primary hip arthroscopy failure. Arthroscopic hip capsular reconstruction is technically challenging, largely owing to complex suture management and difficulties with graft placement and sizing. This article describes the capsular reconstruction technique, detailing the technical aspects of anterosuperior capsular defect identification; capsular preparation; suture management; and dermal allograft sizing, preparation, and positioning.
Technique Video
Narrated key steps of arthroscopic reconstruction of the anterosuperior hip capsule in a right hip, as viewed from the anterolateral portal (superior view using a 70° scope). The anterolateral and modified anterior portals are established through the defect of the previous interportal capsulotomy. After defect identification and measurement, the dermal allograft is oversized by 5 mm in length and width. Sutures are placed circumferentially along the periphery of the capsular defect. In the absence of viable acetabular-sided capsule, suture anchors are placed to secure the graft. Sutures are brought out one by one through a 10-mm cannula and passed through the dermal allograft using a suture-passing device. A knot pusher is placed over one of the sutures in the graft and used to parachute the graft down through the cannula. The graft is secured in place by sequentially tying the sutures, beginning with those closest to the camera and working toward the medial side to facilitate visualization and suture management. Meticulous suture management is a key technical aspect of this procedure.
Iatrogenic hip instability is increasingly recognized as a cause of persistent pain and disability after hip arthroscopy for femoroacetabular impingement.1,2 Hip arthroscopy typically requires a capsulotomy for visualization and instrumentation of the central and peripheral joint compartments. Interportal and T-type capsulotomies disrupt the anterosuperior capsule and reduce static stabilization provided by the iliofemoral ligament.3,4 Several studies have shown that different capsular management strategies result in varying levels of biomechanical stability and affect patient outcomes.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12
Most capsular management research focuses on primary capsular repair. However, patients undergoing revision surgical procedures can have frank defects not amenable to primary capsular repair.13,14 In individuals with collagen disorders, generalized ligamentous laxity, or acute trauma, symptomatic instability may develop owing to incompetent capsular tissues.1 In these settings, capsular reconstruction should be considered. Re-establishment of anterior capsular structural integrity is increasingly recognized as an important factor in restoring the biomechanical stability provided by the iliofemoral ligament and ultimately improving patient outcomes.2,13 This article describes the capsular reconstruction technique, detailing the technical aspects of anterosuperior capsular defect identification; capsular preparation; suture management; and dermal allograft sizing, preparation, and positioning.
Preoperative Patient Evaluation
Preoperative evaluation of patients with suspected iatrogenic hip instability includes a history, physical examination, and magnetic resonance arthrography.2 Patients describe a lack of improvement and persistent pain after primary hip arthroscopy and most commonly complain of the hip giving way, pain with hyperextension or external rotation, and pain with activities of daily living and exercise. Physical examination usually shows a positive axial distraction test result.2 Magnetic resonance arthrography provides detailed visualization of capsular defects.2 If possible, previous operative notes and arthroscopic images should be obtained to evaluate the prior capsular approach and management.
Surgical Technique
Patient Positioning
We use a post-free distraction system (Guardian; Stryker Medical, Kalamazoo, MI) given its lower risk of skin pressure injury and perineal neurapraxia. The patient is placed supine with Trendelenburg positioning at up to 15°, depending on body mass, which may generate sufficient frictional forces on the table to support hip traction and hip laxity.
Access to Hip Joint and Capsular Rent
The anterolateral portal is established 1 cm anterosuperior to the greater trochanter tip. Previous portal sites are used if possible. Under fluoroscopic guidance, a 17-gauge spinal needle is used to enter the hip joint.15 To minimize further capsular damage, the needle is adjusted to enter through the prior capsulotomy defect, which typically has less resistance than that felt when penetrating the hip capsule during a primary hip arthroscopy. The modified anterior portal is placed under direct arthroscopic visualization, again entering the joint through the site of capsular attenuation. Capsular irregularity or deficiency can then be evaluated.
Mobilization of Capsule
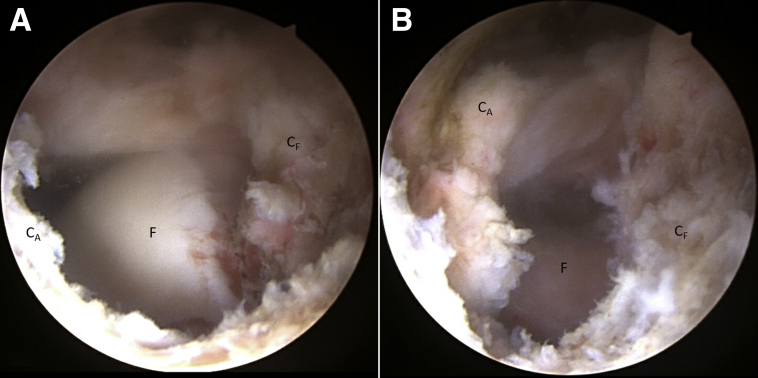
The region of deficient capsular scarring is taken down to identify the defect. A non-toothed shaver and electrocautery (coagulation setting) are preferred because these instruments tend to minimize damage to the intact capsule. The capsular tissue is thoroughly debrided to remove scarring on both the intra-articular and extra-articular margins of the remaining capsular tissue (Fig 1).
Fig 1.
The patient is positioned supine on the post-free distraction table with Trendelenburg positioning at up to 15°. After establishment of the anterolateral and modified anterior portals, the edges of competent capsule on the acetabular and femoral sides should be identified. After capsular adhesion takedown, this right hip shows a 2 × 2.5–cm capsular defect from the anterolateral portal (superior view using a 70° scope). (A) With traction. (B) Without traction. (CA, acetabular capsule; CF, femoral capsule; F, femur.)
It is important to identify the edges of competent capsule on the acetabular and femoral sides. On the acetabular side, competent capsule should be dissected free from the labrum and the rectus tendon. In the absence of competent acetabular-sided capsule, suture anchors may be used to secure the graft. The femoral-sided capsule should be freed on the extracapsular surface until healthy fat or muscle belly is encountered.
Central-Compartment Evaluation and Treatment
The central compartment of the hip is accessed and evaluated while the hip is in traction. Intra-articular pathology such as labral tears, cartilage lesions, and synovitis can be treated using appropriate techniques.
Capsule Suture and Anchor Placement
The lower extremity should be placed in 0° of flexion with the toes pointing forward to minimize graft over-tensioning. If possible, the peripheral edges of the capsular defect should be closed primarily, minimizing the size of the remaining capsular rent. If a defect remains or if the capsule closes with excessive tension, we prefer to use an acellular dermal matrix graft (Allomend; Allosource, Centennial, CO) to patch or augment the repair.
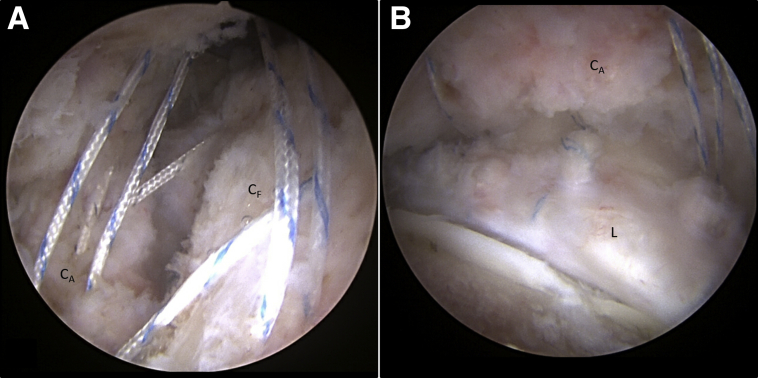
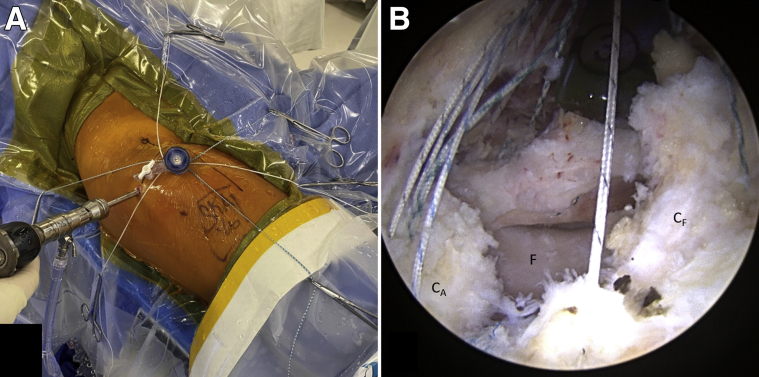
Suture limbs are placed circumferentially around the capsular rent. The first stitch is placed at the medial apex. Two to three horizontal mattress sutures are placed through the competent acetabular-sided capsule. If the acetabular-sided capsule is absent, suture anchors are placed approximately 5 mm apart to fix the graft to the acetabulum (Fig 2). Horizontal mattress sutures are placed through the femoral-sided capsular leaflet, followed by a final suture at the lateral apex. Sutures are placed one at a time, brought out of the cannula, and clamped to the surgical drapes (Fig 3). Meticulous suture management is a key technical aspect of this surgical procedure.
Fig 2.
Capsular reconstruction begins with the placement of sutures circumferentially around the capsular rent in a horizontal mattress fashion. If the acetabular-sided capsule is absent, suture anchors are placed approximately 5 mm apart to fix the graft to the acetabulum. As shown from the anterolateral portal (superior view using a 70° scope), acetabular-sided leaflet sutures are placed in the healthy acetabular-sided capsule, prior to anterosuperior capsular reconstruction, in a right hip (A), and acetabular-sided suture anchors are placed in the acetabular rim in the setting of acetabular-sided capsular deficiency in a left hip (B). (CA, acetabular capsule; CF, femoral capsule; L, labrum.)
Fig 3.
Sutures are placed one at a time, brought out of the cannula, and clamped to the surgical drapes for suture management. (A) Right hip showing outside suture management prior to passing the graft downward through the cannula. (B) Left hip showing suture placement circumferentially around the capsular rent from the anterolateral portal (superior view using a 70° scope). (CA, acetabular capsule; CF, femoral capsule; F, femur.)
Measurement of Graft Size
Graft sizing is key to an appropriately tensioned reconstruction (Video 1). A knot pusher is slid down the most medial suture limb and used to guide this suture limb to the opposite side of the defect. The suture limb is then gently tensioned, and a hemostat is applied to mark the length of the limb. The knot pusher is brought to the opposite side of the defect at the origin of this limb, and a hemostat is again applied to gently tensioned suture. The distance between these 2 hemostats is measured to estimate graft width. This process is repeated in the superior-to-inferior direction to estimate graft length.
Graft Preparation
On the back table, the dermal allograft is measured, oversizing by 5 mm in length and width. Once the graft has been cut, a marker is used to denote the suture holes as determined by the previous capsular suture placement.
Graft Placement
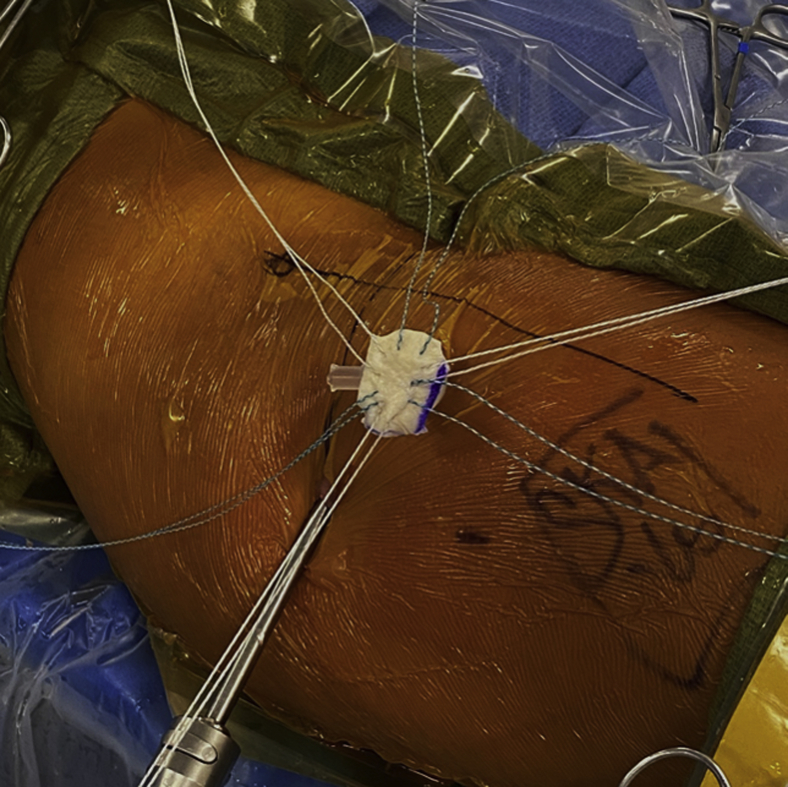
A 10-mm cannula (Smith & Nephew, Watford, England) is used for suture management and graft passage. A suture-passing device (Injector; Stryker Medical) is used to place each of the respective suture limbs through the graft in a horizontal mattress fashion to match up with the location of each stitch placed in the capsule. One by one, sutures are grasped through the cannula, untwisted, and passed through the graft. It is extremely important to make sure that the sutures do not cross one another within the cannula because this will disrupt suture management (Fig 4). Once all sutures are passed, the graft is placed over the cannula and a knot pusher is used to press the graft downward through the cannula in a parachute-like fashion. Individual tensioning of each of the suture limbs can be useful in working the graft down the limbs and onto the capsule. Once the graft is in place, a suture grasper can be used to firmly seat the graft onto the capsule and act as a second check to ensure the sutures are not tangled. Once well seated, the graft is secured into place by sequentially tying each suture. Once the capsular reconstruction is complete, a shaver is introduced to lightly abrade surrounding tissue to stimulate gentle bleeding and increase biological activity in the area (Fig 5).
Fig 4.
A suture-passing device is used to place each of the respective suture limbs through the graft in a horizontal mattress fashion to match up with the location of each stitch placed in the capsule. One by one, sutures are grasped through the cannula, untwisted, and passed through the graft. The dermal allograft with suture arrangement is shown in a right hip prior to passing through the cannula in a parachute-like fashion.
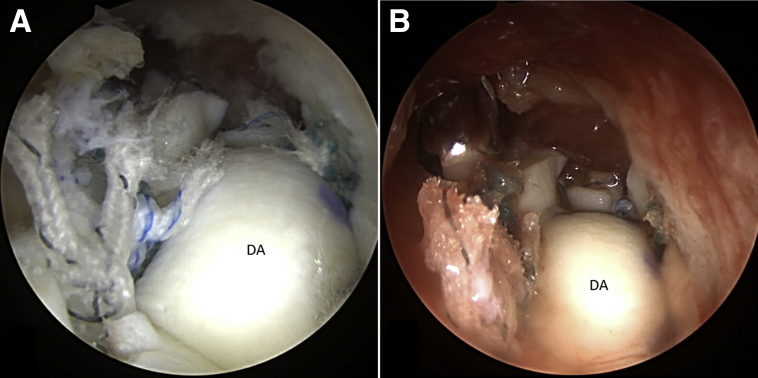
Fig 5.
Once well seated onto the capsule, the graft is secured into place by sequentially tying each suture. A shaver is then introduced to lightly abrade surrounding tissue to stimulate gentle bleeding and increase biological activity in the area. Arthroscopic images of the same left hip from the anterolateral portal (superior view using a 70° scope) show the graft in its final placement after tying each suture limb (A) and the final construct after light abrading of the surrounding soft tissue (B). (DA, dermal allograft.)
Discussion
As the number of hip arthroscopy procedures performed in the young adult hip-preservation population increases, the incidence of iatrogenic hip instability will also increase. Accurate and efficient reconstruction of the iliofemoral ligament and anterosuperior capsule is anticipated to be of increasing importance for hip arthroscopists. Revision arthroscopic capsular reconstruction presents a unique set of challenges, including organized suture management, efficient graft transfer and placement, and correct graft positioning. We present a capsular reconstruction technique outlined stepwise in Table 1 and Video 1.
Table 1.
Steps of Arthroscopic Capsular Reconstruction With Acellular Dermal Allograft
|
|
|
|
|
|
|
Table 2 lists pearls and pitfalls of this technique. Capsular defect measurement is essential to determine appropriate graft size. Meticulous suture management must be maintained to prevent suture tangling and allow for guiding the graft into the appropriate position. Complications may include inappropriate graft tensioning and further hip destabilization. Patients whose symptoms fail to resolve may have been improperly indicated for surgery. Standard hip arthroscopy complications, including nerve injury and complications associated with concurrent osteoplasty, as well as cartilage or labral work, may occur.16, 17, 18
Table 2.
Pearls and Pitfalls
| Pearls |
| The entry portals should be established through the area of the capsular defect to minimize further damage to the native capsule. |
| A non-toothed shaver and electrocautery (coagulation setting) should be used to gently remove scarring to identify the remaining competent capsule on both the acetabular and femoral sides. Suture anchors should be used on the acetabular side if the capsule is absent. |
| The lower extremity should be placed in a neutral position (0° of flexion, toes pointed to ceiling) to minimize capsular over-tensioning. |
| For suture passage around the capsular defect, sutures of alternating colors should be used. |
| The defect size should be measured in the medial-to-lateral and proximal-to-distal directions using suture limbs and a knot-pusher technique. |
| Meticulous suture management is the key to this procedure. It is important to avoid crossing stitches throughout the surgical procedure, especially when retrieving sutures through the cannula during graft passage (although there are multiple sutures at a time within the cannula). |
| The surrounding soft tissue should be lightly abraded with the shaver to stimulate bleeding to increase biological activity in the area. |
| Pitfalls |
| Suture tangling prevents appropriate graft positioning. Meticulous suture management is extremely important. |
| The working cannula needs to be large enough to adequately pass the graft. |
Our technique uses a dermal allograft that has been shown in a cadaveric biomechanical study to restore distractive strength after hip capsule reconstruction.19 Other grafts have been used in capsular reconstruction, including Achilles tendon allograft and iliotibial band allograft.14,20, 21, 22 The presented technique provides an efficient and reliable surgical method for capsular reconstruction that can be utilized for measurement, placement, and fixation regardless of graft material.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.C.O. receives education support from Active Medical and food and beverage support from Acumed, outside the submitted work. S.K.A. receives travel and lodging support from Stryker; receives food and beverage support from Stryker and Smith & Nephew; receives consulting fees from Stryker; and receives education support from Active Medical, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Narrated key steps of arthroscopic reconstruction of the anterosuperior hip capsule in a right hip, as viewed from the anterolateral portal (superior view using a 70° scope). The anterolateral and modified anterior portals are established through the defect of the previous interportal capsulotomy. After defect identification and measurement, the dermal allograft is oversized by 5 mm in length and width. Sutures are placed circumferentially along the periphery of the capsular defect. In the absence of viable acetabular-sided capsule, suture anchors are placed to secure the graft. Sutures are brought out one by one through a 10-mm cannula and passed through the dermal allograft using a suture-passing device. A knot pusher is placed over one of the sutures in the graft and used to parachute the graft down through the cannula. The graft is secured in place by sequentially tying the sutures, beginning with those closest to the camera and working toward the medial side to facilitate visualization and suture management. Meticulous suture management is a key technical aspect of this procedure.
References
- 1.Safran M.R. Microinstability of the hip—Gaining acceptance. J Am Acad Orthop Surg. 2019;27:12–22. doi: 10.5435/JAAOS-D-17-00664. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill D.C., Mortensen A.J., Cannamela P.C., Aoki S.K. Clinical and radiographic presentation of capsular iatrogenic hip instability after previous hip arthroscopy. Am J Sports Med. 2020;48:2927–2932. doi: 10.1177/0363546520949821. [DOI] [PubMed] [Google Scholar]
- 3.Abrams G.D., Hart M.A., Takami K., et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 4.Philippon M.J., Trindade C.A.C., Goldsmith M.T., et al. Biomechanical assessment of hip capsular repair and reconstruction procedures using a 6 degrees of freedom robotic system. Am J Sports Med. 2017;45:1745–1754. doi: 10.1177/0363546517697956. [DOI] [PubMed] [Google Scholar]
- 5.Ortiz-Declet V., Mu B., Chen A.W., et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34:303–318. doi: 10.1016/j.arthro.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 6.Khair M.M., Grzybowski J.S., Kuhns B.D., Wuerz T.H., Shewman E., Nho S.J. The effect of capsulotomy and capsular repair on hip distraction: A cadaveric investigation. Arthroscopy. 2017;33:559–565. doi: 10.1016/j.arthro.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Wuerz T.H., Song S.H., Grzybowski J.S., et al. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016;32:1571–1580. doi: 10.1016/j.arthro.2016.01.049. [DOI] [PubMed] [Google Scholar]
- 8.Wylie J.D., Beckmann J.T., Maak T.G., Aoki S.K. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44:39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 9.Bolia I.K., Fagotti L., Briggs K.K., Philippon M.J. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35:1828–1834. doi: 10.1016/j.arthro.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 10.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 11.Larson C.M., Ross J.R., Stone R.M., et al. Arthroscopic management of dysplastic hip deformities: Predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2015;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 12.Riff A.J., Kunze K.N., Movassaghi K., et al. Systematic review of hip arthroscopy for femoroacetabular impingement: The importance of labral repair and capsular closure. Arthroscopy. 2019;35:646–656.e3. doi: 10.1016/j.arthro.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 13.Fagotti L., Soares E., Bolia I.K., Briggs K.K., Philippon M.J. Early outcomes after arthroscopic hip capsular reconstruction using iliotibial band allograft versus dermal allograft. Arthroscopy. 2019;35:778–786. doi: 10.1016/j.arthro.2018.10.110. [DOI] [PubMed] [Google Scholar]
- 14.Trindade C.A.C., Sawyer G.A., Fukui K., Briggs K.K., Philippon M.J. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4:e71–e74. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aoki S.K., Beckmann J.T., Wylie J.D. Hip arthroscopy and the anterolateral portal: Avoiding labral penetration and femoral articular injuries. Arthrosc Tech. 2012;1:e155–e160. doi: 10.1016/j.eats.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larson C., Clohisy J., Beaule P., Kelly B., Giveans M.R., Samuelson K. Complications after hip arthroscopy: A prospective, multicenter study using a validated grading classification. Arthroscopy. 2013;29:e204. [Google Scholar]
- 17.Frandsen L., Lund B., Grønbech Nielsen T., Lind M. Traction-related problems after hip arthroscopy. J Hip Preserv Surg. 2017;4:54–59. doi: 10.1093/jhps/hnw044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris J.D., McCormick F.M., Abrams G.D., et al. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Casp A., Gwathmey F.W. Hip arthroscopy: Common problems and solutions. Clin Sports Med. 2018;37:245–263. doi: 10.1016/j.csm.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Jacobsen S., Guth J.J., Schimoler P.J., et al. Biomechanical response to distraction of hip capsular reconstruction with human acellular dermal patch graft. Arthroscopy. 2020;36:1337–1342. doi: 10.1016/j.arthro.2019.12.026. [DOI] [PubMed] [Google Scholar]
- 21.Kurz A.Z., Memon M., Williams D., Ayeni O.R. Anterior capsule reconstruction of the native hip: A technique guide. Arthrosc Tech. 2019;8:e1247–e1253. doi: 10.1016/j.eats.2019.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mei-Dan O., Garabekyan T., McConkey M., Pascual-Garrido C. Arthroscopic anterior capsular reconstruction of the hip for recurrent instability. Arthrosc Tech. 2015;4:e711–e715. doi: 10.1016/j.eats.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Narrated key steps of arthroscopic reconstruction of the anterosuperior hip capsule in a right hip, as viewed from the anterolateral portal (superior view using a 70° scope). The anterolateral and modified anterior portals are established through the defect of the previous interportal capsulotomy. After defect identification and measurement, the dermal allograft is oversized by 5 mm in length and width. Sutures are placed circumferentially along the periphery of the capsular defect. In the absence of viable acetabular-sided capsule, suture anchors are placed to secure the graft. Sutures are brought out one by one through a 10-mm cannula and passed through the dermal allograft using a suture-passing device. A knot pusher is placed over one of the sutures in the graft and used to parachute the graft down through the cannula. The graft is secured in place by sequentially tying the sutures, beginning with those closest to the camera and working toward the medial side to facilitate visualization and suture management. Meticulous suture management is a key technical aspect of this procedure.
Narrated key steps of arthroscopic reconstruction of the anterosuperior hip capsule in a right hip, as viewed from the anterolateral portal (superior view using a 70° scope). The anterolateral and modified anterior portals are established through the defect of the previous interportal capsulotomy. After defect identification and measurement, the dermal allograft is oversized by 5 mm in length and width. Sutures are placed circumferentially along the periphery of the capsular defect. In the absence of viable acetabular-sided capsule, suture anchors are placed to secure the graft. Sutures are brought out one by one through a 10-mm cannula and passed through the dermal allograft using a suture-passing device. A knot pusher is placed over one of the sutures in the graft and used to parachute the graft down through the cannula. The graft is secured in place by sequentially tying the sutures, beginning with those closest to the camera and working toward the medial side to facilitate visualization and suture management. Meticulous suture management is a key technical aspect of this procedure.