Abstract
The medial meniscal root tear, a particular meniscal injury at the level of its posterior bone insertion, leads to a loss of impact absorption and load distribution capacity, similar to total meniscectomy. Therefore, its repair is fundamental for knee joint longevity. This type of injury often occurs in middle-aged patients with lower limbs varus malalignment, which results in mechanical overloading of the medial compartment and induces premature cartilage wear out. The success of meniscal root repair, with meniscal bone reinsertion, depends on the correction and realignment of varus deformities greater than 5° for physiological levels. In this situation, corrective tibial osteotomy combined with meniscal repair is indicated. Our goal is to describe the step-by-step technique of the valgus opening wedge tibial osteotomy combined with the arthroscopic reinsertion of the posterior meniscal root in tibia during the treatment of a patient with varus deformity and medial meniscus root tear.
Technique Video
The treated patient had undergone anterior cruciate ligament reconstruction approximately 8 years ago. In the panoramic radiographs of the lower limbs, we can see an asymmetric varus of the knee. Magnetic resonance imaging shows a posterior root tear of the medial meniscus. In the sagittal view, we observe the ghost sign. We start the surgical procedure with tibial osteotomy, initially performing the detachment of the superficial MCL, and we perform the osteotomy after the passage of the guidewires about 4 cm distal to the joint interline. In this case, we planned a 10° opening wedge. During the placement of the osteotomy plate, to avoid confluence with the tibial root tunnel, we place the most posterior proximal screw and distal screws in the traditional way and the most anterior proximal screw is placed in a shorter length. We start the arthroscopic time by visualizing a good medial joint space, since the superficial MCL has already been detached. In this way, we identified the posterior tibial root tear of the medial meniscus. We position the MU guide in the anatomical position of the meniscal root foot print, create the tibial tunnel with a 6-mm FlipCutter drill, bend the drill tip inside the joint, and return with it about 10 mm, creating a bone bed for the meniscus to be reinserted. With the aid of a needle guidewire, we introduce a looped ETHIBOND into this tunnel for future transport of the other threads. With the Knee Scorpion device, we pass a FiberWire over the end of the meniscus, and make Mickey's ear stitch into the wire, repeating this step with 2 more FiberWire threads, performing the second stitch on the second FiberWire, completing then 3 stitches. We transport the 3 FiberWires to the tibial tunnel through the ETHIBOND wire. We use the probe as a pulley to make it easier for the 3 FiberWires to “run” correctly when pulled. We then fix the 3 wires to an ABS button, tensioning the root. We visualize the reinserted root and the meniscus returning to its normal tension. This is the postoperative radiography and this is the patient with 3 months of postoperative, undergoing rehabilitation. (MCL, medial collateral ligament.)
Both medial and lateral menisci have anterior and posterior tibial bone insertions. Lesions in these regions or up to 10 mm from their bone insertion are called meniscal root tears.1, 2, 3 These injuries cause the meniscus to suddenly lose its impact absorption and load-distribution capacity, similar to what occurs in a total meniscectomy, increasing the pressure at the affected compartment.3 Meniscal root tears lead to a meniscal extrusion, a decrease at the contact area, an increase in cartilage stress, and ultimately articular degeneration.2
The gold standard treatment for meniscal root tears is the reinsertion of the affected root, which is associated with high success rates due to pain, function, and activity levels improvements.4,5 Although it is successful in most cases, failures can be related to varus malalignment greater than 5°, and it is recommended to correct the lower limb axis in these situations.2
Patients who have mechanical axis deviation in varus and mild osteoarthritis associated with medial meniscus posterior root tears can benefit from tibial valgus osteotomy. This, even isolated, can provide significant improvement of symptoms and allow healing of the root tear without the need for repair.6 Therefore, there is a clear indication of performing both procedures simultaneously or separately, in an attempt to mitigate early joint degeneration and also to protect the reinsertion of the tibial root, by reducing the overload in the compromised compartment.4
Lower limb physiological alignment varies between 5° and 8° valgus. Varus deformities lead to mechanical overload of the medial compartment of the knee and, as a consequence, to chondral and meniscal degeneration. The magnitude of the degeneration and secondary osteoarthritis development are directly proportional to the degree of varus deformity in the affected limb.7
The valgus opening tibial osteotomy is indicated to realign the limb and decompress the affected compartment in this patient profile.8 Just as physiological alignment prevents chondral degeneration, so do functional menisci, absorbing and distributing stress throughout the joint. They increase the surface contact area between the femur and tibia, allowing a more homogeneous mechanical load distribution avoiding focal overloads.9 We describe herein the step-by-step surgical technique of medial opening proximal tibial osteotomy associated with the reinsertion of the posterior root of the medial meniscus.
Technical Note
The patient is anesthetized with spinal anesthesia and placed in supine position, with a pneumatic cuff positioned at the thigh root. A 1-sheet cushion is positioned over the ipsilateral gluteus running internally the injured lower limb approximately 15°, leaving the patella at the Zenith. A leg support, lateral to the tourniquet, is fixed to the operating table, to facilitate the medial compartment opening during valgus stress. After checking the positioning, asepsis and antisepsis of the affected limb and the ipsilateral anterosuperior iliac crest are performed and sterile surgical drapes are installed.
Valgus Tibial Opening Osteotomy
An 8-cm longitudinal incision on the anteromedial surface of proximal tibia is performed. The hamstring tendons are identified and retracted. After sartorius fascia excision, the superficial medial collateral ligament is identified and released from bone, keeping its distal insertion intact (Fig 1 A and B). Through digital dissection, the head of the fibula is palpated, passing the finger anteriorly to the gastrocnemius. The medial head of the gastrocnemius is, subsequently, retracted and a retractor is placed along within the posterior tibial cortex, to protect the neurovascular bundle.
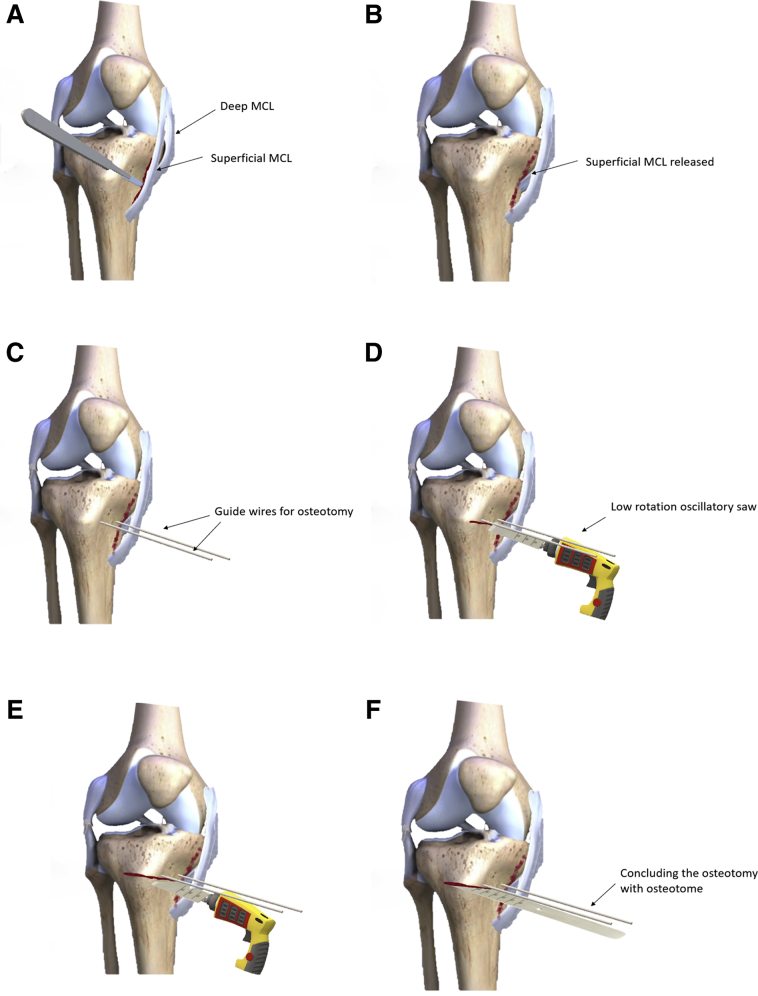
Fig 1.
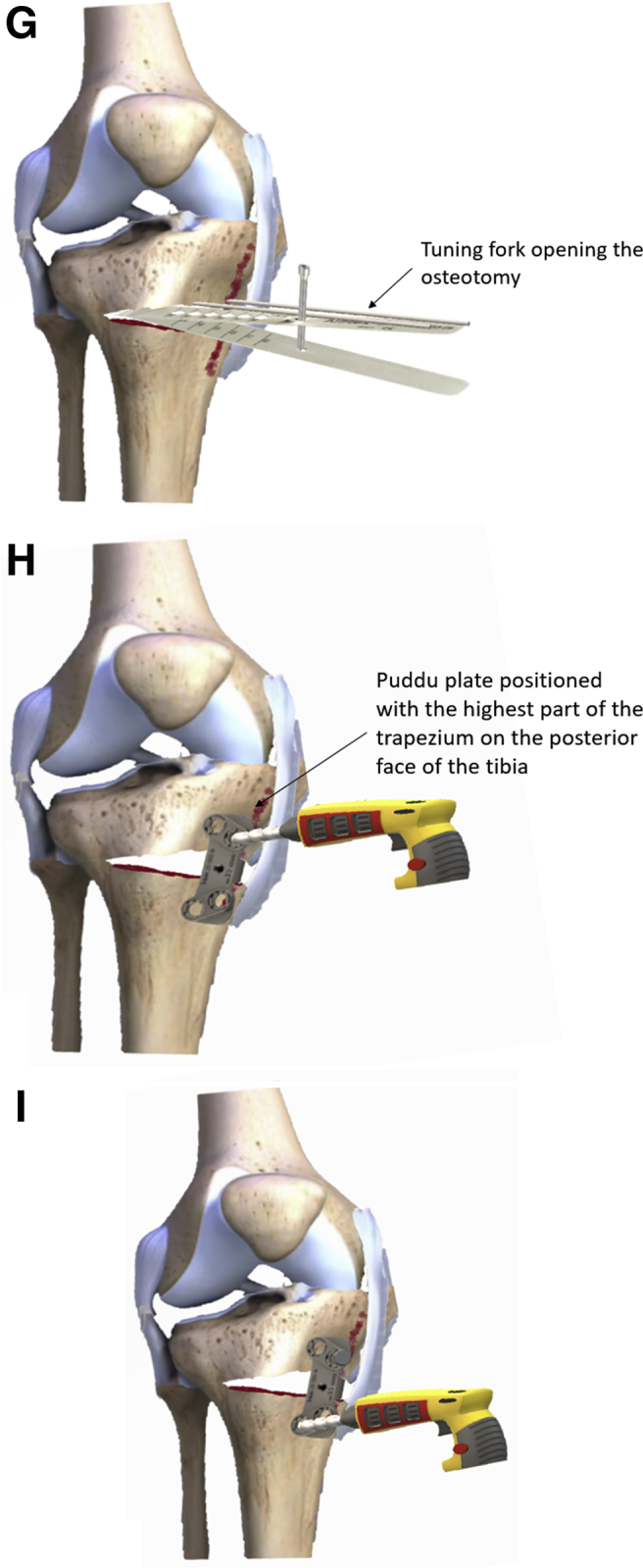
The superficial medial collateral ligament is released from the bone, keeping intact its distal insertion (A and B). Two guidewires are inserted 4 cm distal to the joint line, obliquely, with their end pointing toward the fibula head (C). With a low rotation oscillatory saw, we start the tibial osteotomy (D and E). The osteotomy is finished with osteotomes, taking care to preserve the tibial lateral cortex (F). With the aid of a tuning fork and spreader-type retractors, a medial wedge is opened until the mechanical axis reaches the Fujisawa point (G). A trapezoidal wedge plate, with the longest face aligned with the posterior tibial cortex, is used to keep the wedge open (H). The plate is then fixed with 4 blocked screws, 2 proximal and 2 distal to the osteotomy (I).
The patellar tendon is identified, by blunt dissection, and protected with a hooked retractor, to avoid iatrogenic injury. Under fluoroscopic view, 2 guidewires are inserted 4 cm distal to the joint line, obliquely, with their end pointing toward the fibular head (Fig 1C). The exact osteotomy entry point is located just below the guidewires. A bone-cutting guide is then attached to the wires. The tibial osteotomy began with the aid of a low rotation oscillatory saw (Fig 1 D and E), and finishing with the use of osteotomes (Fig 1F). Attention is taken to preserve the lateral cortex.
With the aid of a tuning fork and spreader-type retractors, a medial wedge is opened until the mechanical axis reached the Fujisawa point (Fig 1G). Then a trapezoidal wedge plate, with the longest face aligned with the posterior tibial cortex is used to keep the wedge open (Fig 1H).
A radioscopic image control in the sagittal plane is important at this point to ensure that the tibial slope is being preserved. Another important precaution is to place the plate as far back as possible, which helps avoiding the tibial slope to be inadvertently affected, and also allows the plate-fixing screws not to interfere with the bone tunnel of the meniscal root repair. The plate is then fixed with 4 blocked screws (2 placed proximal and 2 distal to the osteotomy) (Fig 1I).
Simultaneously with the osteotomy, another team member removes the bone graft from the ipsilateral iliac crest in a conventional manner.
Meniscal Root Repair (With Video Illustration)
We started this surgical step after the tibial osteotomy because, by releasing the superficial medial collateral ligament, the arthroscopic step is considerably easier to be performed due to the increase in the tibiofemoral space (Video 1). After limb exsanguination, the tourniquet is inflated at 300 mm Hg. The anterolateral, anteromedial, and transpatellar arthroscopic portals are created. Then, the posterior root tear of the medial meniscus and its tibial footprint are identified. An “MU” guide (Arthrex, Naples, FL), calibrated with a 50° inclination, is introduced through the anteromedial portal and positioned posterior to the medial tibial spine, on the footprint of the posterior root (Fig 2A). The entry point of the guidewire must be positioned so as to avoid confluence with the anterior and proximal screw that fix the osteotomy plate, if it has already been placed.
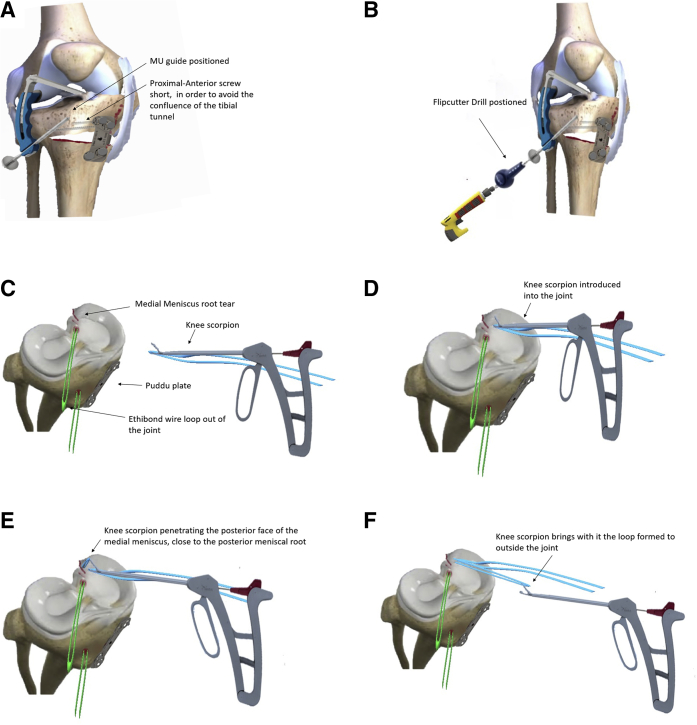
Fig 2.
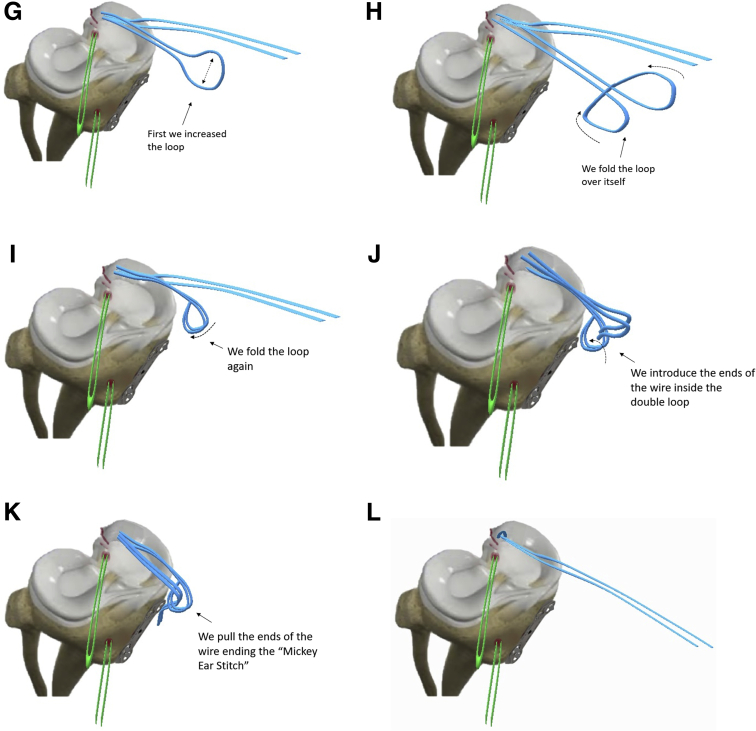
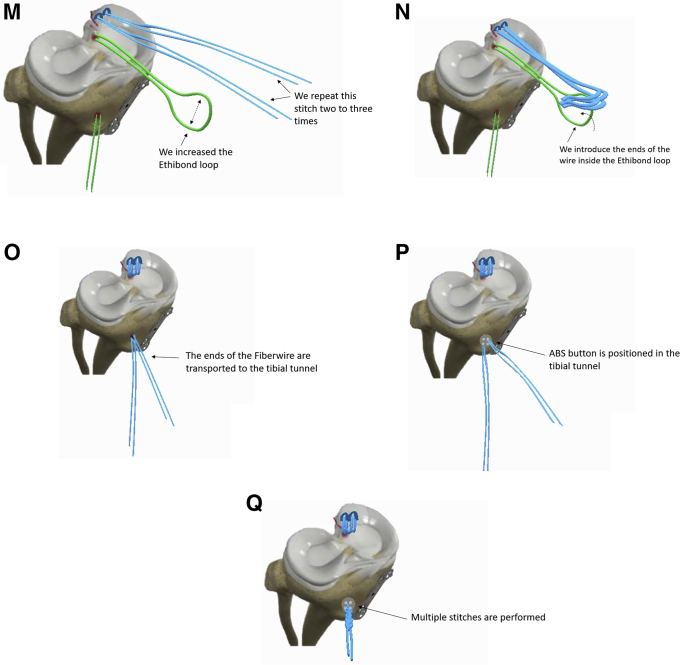
The proximal and anterior screw must be shorter to avoid the confluence with the tibial tunnel of the meniscal root repair. An MU guide (Arthrex), calibrated with at 50° inclination, is introduced through the anteromedial portal and positioned posterior to the medial tibial spine, on the footprint of the posterior root (A). A 6-0 FlipCutter drill is used to drill the tibial tunnel for fixing the meniscal root. We position the MU guide anterior and proximal to the osteotomy plate screws (B). The ETHIBOND wire loop is pulled out the joint through the transpatellar portal, using 2 fingers or probe tweezers, and the Knee Scorpion (Arthrex) device is prepared (C). The Knee Scorpion device is introduced into the joint, penetrating the posterior horn of the medial meniscus; thus, a loop of the FiberWire is passed through this meniscal site. When we remove the device from the inside of the joint, it brings with it the loop formed (D-F). With the loop out of the joint, we perform the “Mickey Ear Stich,” which is performed by folding the loop over itself twice, forming a double loop, and we pass inside the double loop the 2 ends of the fiber wire (G-K). Then, we pull the ends of the wire so that the stitch “runs,” ending the “Mickey Ear Stitch” (L). We repeat this step 2 or 3 more times (M). We pass the ends of the FiberWires inside the ETHIBOND and pull the ETHIBOND loop, transporting the FiberWires into the tibial tunnel (O). We pass the ends of the FiberWires through the inside of the orifices of the ABS button and make multiple points tensioning them, reducing and also tensioning the medial meniscus (P and Q).
The bone tunnel for fixation of the meniscal root is drilled with a 6-0 FlipCutter drill (Arthrex), proximal and anterior to the osteotomy plate screws (Fig 2B). When it gained the joint, we activated the drill bit and drilled backwards through a 10-mm long tunnel. The cannula of the FlipCutter bit must be kept in the tunnel because it serves as a guide for the entry of a needle steel wire loaded with a 2-0 ETHIBOND traction wire in loop (Ethicon, Somerville, NJ). Upon reaching the joint, the wire loop is pulled out through the transpatellar portal, using a 2 fingers tweezer (Fig 2C). At this point, we place 3 FiberWire threads stitches at the meniscus, along the free edge of the injured root, with the aid of a specific suture device, called Knee Scorpion (Arthrex), which enters the joint through the anteromedial portal (Fig 2 D-F). In each pair of suture threads, a Mickey ear-type knot is given (Fig 2 G-L).10
The traction wire that is in the transpatellar portal is then pulled through the anteromedial portal so that all the wires came out through the same portal. The suture thread is introduced into the traction thread loop and then pulled through the tibial tunnel (Fig 2 M-O) and tied to an ABS button (Arthrex) (Fig 2 P and Q) right after the correct tension of the threads ensures the reduction of the meniscal root inside the bone tunnel, under arthroscopic control. The incisions are thoroughly washed out and the autologous iliac crest graft is inserted into the osteotomy. A review of hemostasis is performed and the wounds is sutured in layers and occlusive dressing.
Rehabilitation
The key point for rehabilitation of this surgical procedure is not to load the operated limb in the first 6 weeks.10, 11, 12, 13 In this combined surgical procedure, we have 2 main reasons to avoid load on the operated limb. One is to wait for the tibial osteotomy consolidation, which occurs around the 6th postoperative week,7 and the second reason is to wait for the healing of the meniscal root reinserted in the bone tunnel, which also occurs in the same period of time.10,13 If the patient does not follow this main recommendation, there is a great risk of fracture and misalignment of the proximal tibia, and also a risk of root repair failure, leading to a serious complication. With this main recommendation in mind, we will describe below the other recommendations for postoperative rehabilitation.
The immediate postoperative period to the first week includes the following recommendations11,12:
-
•
Cryotherapy;
-
•
Care for the surgical wound (keeping it always clean, dry, and with an occlusive dressing);
-
•
Pain and edema control with analgesia;
-
•
Use of prophylactic anticoagulation (we recommend enoxaparin at a dose of 40 mg once a day);
-
•
Mobilization of the patella, patellar tendon; and quadriceps;
-
•
Tibial tarsal pump;
-
•
Use of knee immobilizer;
-
•
Nonloading of the operated limb;
-
•
Force passive and active extension gain;
-
•
Passive flexion up to 90° is allowed and should be stimulated to avoid joint stiffness; and
-
•
Quadriceps activation (with isometric exercise).
The first to third week includes the following recommendations11,12:
-
•
Cryotherapy;
-
•
Immobilizer is no longer needed;
-
•
Care for the surgical wound (keeping it always clean, dry and with an occlusive dressing, removing the stitches around the third week);
-
•
Pain and edema control with analgesia;
-
•
Use of prophylactic anticoagulation (we recommend enoxaparin at a dose of 40mg once a day, until the 14th postoperative day);
-
•
Tibial tarsal pump;
-
•
Do not load with the operated limb;
-
•
Force passive and active extension gain;
-
•
Passive flexing up to 90° allowed;
-
•
Quadriceps isometric exercises; and
-
•
Abductor and adductor isometric exercises.
Third to sixth week includes the following recommendations11,12:
-
•
Nonloading of the operated limb;
-
•
Force passive and active extension gain;
-
•
Passive flexion beyond 90° allowed as tolerated by the patient;
-
•
Quadriceps isometric exercises;
-
•
Abductor and adductor isometric exercises; and
-
•
Frontal and lateral radiographs of the knee are recommended to observe bone healing of osteotomy.
The sixth week to eighth week includes the following recommendations11,12:
-
•
The knee radiograph is repeated, and if it shows bone consolidation, start partial load with 2 crutches;
-
•
Start active flexion gain; • Full passive joint gain; and
-
•
The use of a stationary bike with an elevated seat and without resistance is incorporated.
The eighth to 12th week includes the following recommendations11,12:
-
•
Use 1 crutch for 2 more weeks;
-
•
Focus on full active joint amplitude gain;
-
•
Start proprioception training;
-
•
Start resistance on the stationary bike; and
-
•
Start closed kinetic chain exercises with knee flexion restriction angle between 0° and 30 °, always with double legs (leg press, squat).
The 12th to 16th week includes the following recommendations11,12:
-
•
Closed kinetic chain exercises are maintained by increasing the knee joint range to 0 ° × 70 °
-
•
Progression of exercises from double-leg to single-leg can be started if the patient shows an evolutionary improvement in exercises performed with double leg.
-
•
Freestyle swimming, elliptical, and walking on the treadmill are allowed to increase cardiovascular conditioning.
The 16th week to sixth month11,12 includes the following recommendations:
-
•
Closed and open kinetic chain exercises are maintained by increasing the knee joint range to 0 ° × 90 °;
-
•
Single leg exercises allowed;
-
•
Focus on muscle strengthening of the quadriceps, abductors and external hip rotators;
-
•
Freestyle swimming, elliptical, and walking on the treadmill are allowed to increase cardiovascular conditioning; and
-
•
Quadriceps index must be assessed with a manual dynamometer and at this stage the strength of the quadriceps on the operated limb must be above 80% of the unaffected limb.
Finally, after the sixth month11,12 the following recommendations are instituted:
-
•
Maintain muscle strengthening;
-
•
Quadriceps index must be assessed with a manual dynamometer and at this stage the strength of the quadriceps on the operated limb must be above 90% of the unaffected limb; and
-
•
Evaluate return for sports activity.
Discussion
Posterior root tear of the medial meniscus is usually degenerative and observed mainly in middle-aged women, corresponding to approximately 20% of lesions of the posterior horn of the medial meniscus.4 They usually occur spontaneously without a well-defined trauma. It is common for the patient report hearing a sudden snap when crouching, followed by severe pain at the level of the medial joint line. Magnetic resonance imaging (MRI) has a high diagnostic sensitivity (77%), preferably in T2. A high signal perpendicular to the meniscus in the axial view, a truncation sign, and meniscal extrusion in the coronal view and the ghost sign in the sagittal view are characteristic.3,4
This type of injury can lead to a rapid progression to osteoarthritis in the affected compartment and, in addition, studies show a strong association between meniscal root injuries and osteonecrosis.14,15 Up to 80% of patients with “spontaneous” osteonecrosis have a posterior root tear of the medial meniscus associated.3
Arthroscopic repair is the treatment of choice for posterior root tears of the meniscus because it restores joint kinematics, improves load distribution and symptoms, and delays evolution to osteoarthritis.4 The repair is not indicated in patients with diffuse osteoarthritis (Outerbridge grades III and IV) of the affected compartment, asymptomatic chronic lesions, and uncorrected misalignments. Varus deformity greater than 3o, chondral lesion grade 3 or greater, and meniscal extrusion greater than 3 mm are poor prognosis factors.1, 2, 3, 4 As treatment alternatives to repair, conservative and partial meniscectomy are described, both with similar poor results, and a conversion rate to total knee arthroplasty of 50% in 5 years.3
One of the possible causes of injury to the posterior medial root is the increased load in this compartment due to varus deformity. This deformity can overload the medial compartment, leading to the root injury, but it can also occur after the root injury, due to chondral wear and collapse of the joint that occurs due to meniscus incompetence. The fact is that the deformity, whether primary or secondary to root damage, must be corrected before or together with root repair when it is greater than 5° of varus.1,2,4,6,16
Nha et al.6 evaluated the degree of meniscal healing of the posterior root, through an arthroscopic second-look evaluation, in patients undergoing isolated tibial osteotomy, without meniscal repair, and found 10 (50%) cases with complete healing, 6 (30%) with incomplete healing, and 4 (20%) with no healing.6 Tibial osteotomy in selected patients presents satisfactory results, with a return-to-sports rate of approximately 75% (55%-100%) and a return-to-work activity rate around 80% (41%-100%).17
Moon et al.18 developed a retrospective study analyzing 63 patients who underwent reinsertion of the posterior root of the medial meniscus. To participate in the study, patients needed to be younger than 65 years old, with a Kellgren–Lawrence score equal or less than 2, nonsevere varus of the lower limb with lower limb alignment less than 10°, and less than 5° difference between the contracted limb side. The average age of these patients was 54.9 years, mean body mass index of 26.2, with an average onset of symptoms until surgical treatment of 18.1 weeks. The authors submitted all participants to the technique of meniscal reinsertion through a tibial transosseous tunnel with button fixation. Patients were evaluated for clinical visual analog scale and International Knee Documentation Committee (IKDC) scores, also were evaluated with a panoramic radiograph of the lower limbs with preoperative load, with 1 year postoperatively and 2 years postoperatively, and joint degeneration and lower limb alignment were analyzed. MRI also was analyzed preoperatively and 1 year after surgery. Patients were divided into 2 groups according to the degree of meniscal extrusion assessed at preoperative and postoperative MRI. The authors observed that the clinical results improved with statistical significance in both groups in the 2 years of evaluations. However, the joint degeneration was analyzed radiologically advanced in both groups, and in the group with greater meniscal extrusion (group 2), this progression was significantly greater. An increase in the varus misalignment of the progressive affected limb also was observed in panoramic radiographs performed 1 and 2 years after surgery in both groups. The only difference between the 2 groups was the time between injury and surgery, which was significantly shorter in the group with less meniscal extrusion (group 1). Thus, the authors concluded that an early approach to surgical treatment for patients with meniscal root injury has a greater chance of decrease meniscal extrusion by decreasing the speed of joint degeneration. One factor that was not considered in the author’s conclusions was if an osteotomy associated with root repair in these cases could further decrease the progression of joint degeneration and prevent a progressive misalignment in this patient profile.18
In 2019, Kodama et al.19 performed a retrospective study analyzing 22 patients undergoing surgical treatment for posterior root tears of the medial meniscus. The authors evaluated the degree of meniscal extrusion on preoperative MRI in extension and 90° flexion in the postoperative period, and repeated this examination 3 and 12 months after the operation. They also researched the following clinical scores, Lysholm, IKDC, Tegner, and visual analog scale, during the same pre- and postoperative periods. One year after the operation, the authors performed a second-look arthroscopy to assess chondral status. The authors found a clinical improvement of all scores, with statistical significance without clinical correlation with the degree of meniscal extrusion found in the period of 1 year after surgery. On MRIs performed in flexion, the authors observed a decrease in meniscal extrusion compared with the preoperative examination, whereas on MRIs performed in extension, the degree of extrusion was greater than the preoperative. In the assessment of chondral status, there was a chondral degeneration of the loading area of the medial femoral condyle. Kodama et al. concluded that despite observing a slight increase in the chondral degeneration of the load area of the medial femoral condyle and the meniscal extrusion of the medial meniscus in extension, the clinical scores were not affected by these changes, being observed an improvement with statistical significance for all patients. The authors also concluded that the surgical treatment of the meniscal root tear, treated with transosseous fixation, allows a delay in the meniscal extrusion at 90° of knee flexion and prevents a chondral degeneration at the area of the femoral condyle that articulates with the tibial plateau and meniscus in 90° of flexion.19
A recently published study retrospectively compared 71 patients with posterior root tears of the medial meniscus and submitted to a medial opening valgus tibial osteotomy. The authors divided these patients into 3 groups. In the first group, only the osteotomy was performed and no treatment was performed on the meniscal root tear. In the second group, the tibial osteotomy was associated with a transosseous root repair and in the third group, the patients underwent osteotomy associated with the repair “side by side” of the meniscal root. The authors evaluated patients with clinical questionnaires (Lysholm, IKDC, Kellgren–Lawrence and Tegner), progression of joint degeneration assessed radiologically by the classification, and a second-look arthroscopy was performed 24 months after surgery (performed at the time of removal osteotomy plate and screws) to assessed the chondral status and the meniscal root healing. The authors found a clinical improvement of all scores in the 3 groups with no significant differences between them. They observed a better chondral quality in the group that osteotomy was associated with the transosseous meniscal reinsertion technique, but without statistical difference between the other 2 groups. This same group had the greatest rate of meniscal healing of 24%. In the radiologic analysis, only 1 patient in the group in which the osteotomy was performed isolated presented osteoarthritis progression, in the other groups none of the patients worsened. The authors concluded that the association of posterior meniscal root repair of the medial meniscus with osteotomy seems to improve the quality of the chondral status during the second arthroscopic look; however, in the short term, the repair of the meniscal root did not present significant differences with the group in which meniscal root has not been addressed.20 We believe that the number of patients involved in this study and short follow-up prevented the observation of a substantial improvement in the group that underwent medial opening valgus tibial osteotomy associated the medial posterior root repair. Another important fact of the study is that the tibial osteotomy, even performed in isolation, improved the clinical scores evaluated with statistical significance, being similar to the other groups, showing the relevance and importance of correcting the mechanical axis in patients with varus deformity and meniscal tear.
Although tibial osteotomy can be performed before root repair, we believe that performing both in the same surgical time allows recovery and return to daily activities much faster, in addition to not exposing the patient to 2 surgical interventions. The advantages, disadvantages, risks, and pitfalls of this technique are shown in Table 1.
Table 1.
Advantages, Disadvantages, Risks, and Tips Associated With Posterior Root Repair of Medial Meniscus Combined With Valgus Tibial Opening Osteotomy
| Advantages | Disadvantages | Risks | Tips |
|---|---|---|---|
| Faster recovery | Longer surgical time | Confluence of the tibial tunnel and proximal anterior screw | The tibial bone tunnel must be exactly on the native footprint of the meniscal root |
| The release of the MCL for osteotomy favors the medial joint space opening and facilitates the root repair | Articular Fracture of the proximal tibia | Protect the neurovascular popliteal bundle during tibial osteotomy | |
| Decompression of the medial compartment favors the root healing | Keep the lateral cortex of the tibia intact to allow the hinge wedge opening. | ||
| In the proximal and anterior orifice of the osteotomy plate, use a screw of shorter length, preventing it from interfering with the perforation of the tibial tunnel to reinsert the meniscal root |
MCL, medial collateral ligament.
We hope that the details of the combined surgical technique will allow the procedure to be performed in a more accurate and reproducible manner, increasing success rates.
Acknowledgments
The filming of the surgical procedure was performed by the filmmaker Paulo Cézar Vieira de Freitas.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The treated patient had undergone anterior cruciate ligament reconstruction approximately 8 years ago. In the panoramic radiographs of the lower limbs, we can see an asymmetric varus of the knee. Magnetic resonance imaging shows a posterior root tear of the medial meniscus. In the sagittal view, we observe the ghost sign. We start the surgical procedure with tibial osteotomy, initially performing the detachment of the superficial MCL, and we perform the osteotomy after the passage of the guidewires about 4 cm distal to the joint interline. In this case, we planned a 10° opening wedge. During the placement of the osteotomy plate, to avoid confluence with the tibial root tunnel, we place the most posterior proximal screw and distal screws in the traditional way and the most anterior proximal screw is placed in a shorter length. We start the arthroscopic time by visualizing a good medial joint space, since the superficial MCL has already been detached. In this way, we identified the posterior tibial root tear of the medial meniscus. We position the MU guide in the anatomical position of the meniscal root foot print, create the tibial tunnel with a 6-mm FlipCutter drill, bend the drill tip inside the joint, and return with it about 10 mm, creating a bone bed for the meniscus to be reinserted. With the aid of a needle guidewire, we introduce a looped ETHIBOND into this tunnel for future transport of the other threads. With the Knee Scorpion device, we pass a FiberWire over the end of the meniscus, and make Mickey's ear stitch into the wire, repeating this step with 2 more FiberWire threads, performing the second stitch on the second FiberWire, completing then 3 stitches. We transport the 3 FiberWires to the tibial tunnel through the ETHIBOND wire. We use the probe as a pulley to make it easier for the 3 FiberWires to “run” correctly when pulled. We then fix the 3 wires to an ABS button, tensioning the root. We visualize the reinserted root and the meniscus returning to its normal tension. This is the postoperative radiography and this is the patient with 3 months of postoperative, undergoing rehabilitation. (MCL, medial collateral ligament.)
References
- 1.Bonasia D.E., Pellegrino P., D'Amelio A., Cottino U., Rossi R. Meniscal root tear repair: Why, when and how? Orthop Rev (Pavia) 2015;7:5792. doi: 10.4081/or.2015.5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung K.S., Ha J.K., Ra H.J., Kim J.G. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy. 2016;32:1319–1327. doi: 10.1016/j.arthro.2015.12.046. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 4.Pache S., Aman Z.S., Kennedy M., et al. Meniscal root tears: Current concepts review. Arch Bone Joint Surg. 2018;6:250–259. [PMC free article] [PubMed] [Google Scholar]
- 5.Chahla J., LaPrade R.F. Meniscal root tears. Arthroscopy. 2019;35:1304–1305. doi: 10.1016/j.arthro.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Nha K.W., Lee Y.S., Hwang D.H., et al. Second-look arthroscopic findings after open-wedge high tibia osteotomy focusing on the posterior root tears of the medial meniscus. Arthroscopy. 2013;29:226–231. doi: 10.1016/j.arthro.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 7.Brouwer R.W., Huizinga M.R., Duivenvoorden T., et al. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014;12:CD004019. doi: 10.1002/14651858.CD004019.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonasia D.E., Governale G., Spolaore S., Rossi R., Amendola A. High tibial osteotomy. Curr Rev Musculoskelet Med. 2014;7:292–301. doi: 10.1007/s12178-014-9234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau B.C., Conway D., Mulvihill J., Zhang A.Z., Feeley B.T. Biomechanical consequences of meniscal tear, partial meniscectomy, and meniscal repair in the knee. JBJS Rev. 2018;6:e3. doi: 10.2106/JBJS.RVW.17.00125. [DOI] [PubMed] [Google Scholar]
- 10.Rocha de Faria J.L., Pavão D.M., Pedrinha I.S.M., et al. Posterior meniscal root repair using a meniscal suture device. Arthrosc Tech. 2020;9:e905–e912. doi: 10.1016/j.eats.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller B.T., Moulton S.G., O'Brien L., LaPrade R.F. Rehabilitation following meniscal root repair: A clinical commentary. J Orthop Sports Phys Ther. 2016;46:104–113. doi: 10.2519/jospt.2016.6219. [DOI] [PubMed] [Google Scholar]
- 12.Dean R.S., DePhillipo N.N., Monson J.K., LaPrade R.F. Peripheral stabilization suture to address meniscal extrusion in a revision meniscal root repair: Surgical technique and rehabilitation protocol. Arthrosc Tech. 2020;9:e1211–e1218. doi: 10.1016/j.eats.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steineman B.D., LaPrade R.F., Haut Donahue T.L. Loosening of transtibial pullout meniscal root repairs due to simulated rehabilitation is unrecoverable: A biomechanical study. Arthroscopy. 2019;35:1232–1239. doi: 10.1016/j.arthro.2018.11.041. [DOI] [PubMed] [Google Scholar]
- 14.Robertson D.D., Armfield D.R., Towers J.D., Irrgang J.J., Maloney W.J., Harner C.D. Meniscal root injury and spontaneous osteonecrosis of the knee: An observation. J Bone Joint Surg Br. 2009;91:190–195. doi: 10.1302/0301-620X.91B2.21097. [DOI] [PubMed] [Google Scholar]
- 15.Hussain Z.B., Chahla J., Mandelbaum B.R., Gomoll A.H., LaPrade R.F. The role of meniscal tears in spontaneous osteonecrosis of the knee: A systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47:501–507. doi: 10.1177/0363546517743734. [DOI] [PubMed] [Google Scholar]
- 16.Laprade R.F., Spiridonov S.I., Nystrom L.M., Jansson K.S. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28:354–364. doi: 10.1016/j.arthro.2011.08.310. [DOI] [PubMed] [Google Scholar]
- 17.Kunze K.N., Beletsky A., Hannon C.P., et al. Return to work and sport after proximal tibial osteotomy and the effects of opening versus closing wedge techniques on adverse outcomes: A systematic review and meta-analysis. Am J Sports Med. 2020;48:2295–2304. doi: 10.1177/0363546519881638. [DOI] [PubMed] [Google Scholar]
- 18.Moon H.S., Choi C.H., Jung M., Lee D.Y., Hong S.P., Kim S.H. Early surgical repair of medial meniscus posterior root tear minimizes the progression of meniscal extrusion: 2-year follow-up of clinical and radiographic parameters after arthroscopic transtibial pull-out repair. Am J Sports Med. 2020;48:2692–2702. doi: 10.1177/0363546520940715. [DOI] [PubMed] [Google Scholar]
- 19.Kodama Y., Furumatsu T., Masuda S., et al. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients. Knee Surg Sports Traumatol Arthrosc. 2020;28:3416–3425. doi: 10.1007/s00167-019-05810-x. [DOI] [PubMed] [Google Scholar]
- 20.Lee D.W., Lee S.H., Kim J.G. Outcomes of medial meniscal posterior root repair during proximal tibial osteotomy: Is root repair beneficial? Arthroscopy. 2020;36:2466–2475. doi: 10.1016/j.arthro.2020.04.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The treated patient had undergone anterior cruciate ligament reconstruction approximately 8 years ago. In the panoramic radiographs of the lower limbs, we can see an asymmetric varus of the knee. Magnetic resonance imaging shows a posterior root tear of the medial meniscus. In the sagittal view, we observe the ghost sign. We start the surgical procedure with tibial osteotomy, initially performing the detachment of the superficial MCL, and we perform the osteotomy after the passage of the guidewires about 4 cm distal to the joint interline. In this case, we planned a 10° opening wedge. During the placement of the osteotomy plate, to avoid confluence with the tibial root tunnel, we place the most posterior proximal screw and distal screws in the traditional way and the most anterior proximal screw is placed in a shorter length. We start the arthroscopic time by visualizing a good medial joint space, since the superficial MCL has already been detached. In this way, we identified the posterior tibial root tear of the medial meniscus. We position the MU guide in the anatomical position of the meniscal root foot print, create the tibial tunnel with a 6-mm FlipCutter drill, bend the drill tip inside the joint, and return with it about 10 mm, creating a bone bed for the meniscus to be reinserted. With the aid of a needle guidewire, we introduce a looped ETHIBOND into this tunnel for future transport of the other threads. With the Knee Scorpion device, we pass a FiberWire over the end of the meniscus, and make Mickey's ear stitch into the wire, repeating this step with 2 more FiberWire threads, performing the second stitch on the second FiberWire, completing then 3 stitches. We transport the 3 FiberWires to the tibial tunnel through the ETHIBOND wire. We use the probe as a pulley to make it easier for the 3 FiberWires to “run” correctly when pulled. We then fix the 3 wires to an ABS button, tensioning the root. We visualize the reinserted root and the meniscus returning to its normal tension. This is the postoperative radiography and this is the patient with 3 months of postoperative, undergoing rehabilitation. (MCL, medial collateral ligament.)
The treated patient had undergone anterior cruciate ligament reconstruction approximately 8 years ago. In the panoramic radiographs of the lower limbs, we can see an asymmetric varus of the knee. Magnetic resonance imaging shows a posterior root tear of the medial meniscus. In the sagittal view, we observe the ghost sign. We start the surgical procedure with tibial osteotomy, initially performing the detachment of the superficial MCL, and we perform the osteotomy after the passage of the guidewires about 4 cm distal to the joint interline. In this case, we planned a 10° opening wedge. During the placement of the osteotomy plate, to avoid confluence with the tibial root tunnel, we place the most posterior proximal screw and distal screws in the traditional way and the most anterior proximal screw is placed in a shorter length. We start the arthroscopic time by visualizing a good medial joint space, since the superficial MCL has already been detached. In this way, we identified the posterior tibial root tear of the medial meniscus. We position the MU guide in the anatomical position of the meniscal root foot print, create the tibial tunnel with a 6-mm FlipCutter drill, bend the drill tip inside the joint, and return with it about 10 mm, creating a bone bed for the meniscus to be reinserted. With the aid of a needle guidewire, we introduce a looped ETHIBOND into this tunnel for future transport of the other threads. With the Knee Scorpion device, we pass a FiberWire over the end of the meniscus, and make Mickey's ear stitch into the wire, repeating this step with 2 more FiberWire threads, performing the second stitch on the second FiberWire, completing then 3 stitches. We transport the 3 FiberWires to the tibial tunnel through the ETHIBOND wire. We use the probe as a pulley to make it easier for the 3 FiberWires to “run” correctly when pulled. We then fix the 3 wires to an ABS button, tensioning the root. We visualize the reinserted root and the meniscus returning to its normal tension. This is the postoperative radiography and this is the patient with 3 months of postoperative, undergoing rehabilitation. (MCL, medial collateral ligament.)