Abstract
There is currently no drug or therapy that can cure the coronavirus disease 2019 (COVID-19), which is highly contagious and can be life-threatening in severe cases. Therefore, seeking potential effective therapies is an urgent task. An older female at the Leishenshan Hospital in Wuhan, China, with a severe case of COVID-19 with significant shortness of breath and decrease in peripheral oxygen saturation (SpO2), was treated using manual acupuncture and Chinese herbal medicine granule formula Fuzheng Rescue Lung with Xuebijing Injection in addition to standard care. The patient’s breath rate, SpO2, heart rate, ratio of neutrophil/lymphocyte (NLR), ratio of monocyte/lymphocyte (MLR), C-reactive protein (CRP), and chest computed tomography were monitored. Acupuncture significantly improved the patient’s breathing function, increased SpO2, and decreased her heart rate. Chinese herbal medicine might make the effect of acupuncture more stable; the use of herbal medicine also seemed to accelerate the absorption of lung infection lesions when its dosage was increased. The combination of acupuncture and herbs decreased NLR from 14.14 to 5.83, MLR from 1.15 to 0.33 and CRP from 15.25 to 6.01 mg/L. These results indicate that acupuncture and Chinese herbal medicine, as adjuvants to standard care, might achieve better results in treating severe cases of COVID-19.
Keywords: COVID-19, Severe case, Case report, Acupuncture, Chinese herbal medicine, Integrative therapy
1. Introduction
The outbreak of coronavirus disease 2019 (COVID-19) was announced as a pandemic by the World Health Organization (WHO) on March 12, 2020 [1]. Currently, the COVID-19 pandemic has infected a large part of the global population, causing mass sickness, hospitalization and death. To date, there has been no drug to cure this highly contagious and life-threatening disease; therefore, seeking potential therapies is an urgent task. In its report, the WHO-China Joint Mission highly praised the non-pharmacological measures of the “China model” in fighting COVID-19 [2]. While traditional Chinese herbal medicine has been recommended for COVID-19 treatment, acupuncture and moxibustion have been suggested for use in its rehabilitation stage [3]. The effect of acupuncture, along with the use of herbal medicine to treat COVID-19 patients in the acute stage, has yet to be widely reported. This case report follows the CARE Guidelines [4]; it follows the case of an older patient with severe COVID-19, who was successfully treated with acupuncture and Chinese herbal medicine in addition to standard care in Leishenshan (literally, Thunder God Mountain) Hospital, Wuhan, China.
2. Disease history
An 81-year-old female began to have a fever on January 24, 2020 after having gone out the day before. Her maximum body temperature was 39.3 °C, accompanied with moderate chills, paroxysmal dry cough, shortness of breath, dry mouth, decreased taste, poor appetite, fatigue with muscle aches and general malaise. She was admitted to Wuchang Hospital in Wuhan on day 1 of her illness (January 24, 2020). Three days later, the computed tomography (CT) examination of her chest revealed bilateral lung abnormalities, including multiple blurred patches and ground glass shadows; it was reported as “viral pneumonia.” She received the clinical diagnosis of “new coronavirus pneumonia” (now the formal term is “COVID-19”). An integrative treatment, consisting of norfloxacin (Jiangsu Yuexing Pharmaceutical Co., Ltd., Taizhou, China; 400 mg, po, bid, on January 25), a 10-day course of moxifloxacin (Schering Ltd., Guangzhou, China; 400 mg, po, qd.), a 15-day course of Lianhua Qingwen Capsules (Yiling Pharmaceutical Ltd., Shijiazhuang, China; 4 capsules, po, tid) [3] and a 5-day course of oseltamivir (Shanghai Roche Pharmaceuticals Ltd., Shanghai, China; 75 mg, po, bid). A polymerase chain reaction (PCR) test of a nasopharyngeal swab sample showed a positive result for the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on January 30, 2020. Arbidol (Hainan Simcere Pharmaceuticals Ltd., Haikou, China; 100 mg, po, tid) was used for 15 days to aid her treatments, beginning on February 6, until February 20. Her fever, diarrhea, decreased taste, and muscle aches were relieved, although she still had a cough with white phlegm, shortness of breath, fatigue, dry mouth, and low appetite. On February 10, her PCR test for SARS-COV-2 was negative.
Her CT scan showed the pneumonia “worse and with lung edema” on February 14, with edema appearing at her lower extremities. Due to her worsening condition, she was transferred from Wuchang Hospital into Wuhan Leishanshan Hospital on February 20.
3. Symptoms, examination and diagnosis
At the time of admission, the patient presented with significant shortness of breath, chest tightness, cough with light phlegm, substantial cyanosis of the lips and nails, fatigue, loss of appetite, poor sleep, dry mouth with bitter taste, but with no fever, she also had normal urination and bowel movements. Vital signs showed heart rate 108 beats/min, breath rate 23 breaths/min, and pulse oximeter test for peripheral oxygen saturation (SpO2) oxygen 90% (hypoxemic). The patient was diagnosed with a severe stage of COVID-19 [3], [5] with respiratory failure. Table 1, Table 2 showed inflammatory marker data over the course of the treatment period.
Table 1.
Indicators for COVID-19 severity and prognosis.
| Item | Time point |
|||||
|---|---|---|---|---|---|---|
| 2/20 | 2/24 | 2/29 | 3/4 | 3/8 | 4/29 | |
| Lactate dehydrogenase (IU/L) | 455 | 330 | 286 | 301 | 264 | – |
| C-reactive protein (mg/L) | – | 15.25 | 9.58 | 7.01 | 6.01 | – |
| Procalcitonin (ng/mL) | 0.22 | 0.12 | – | – | – | – |
| Ratio of neutrophil/lymphocyte | 14.14 | 7.55 | 11.08 | 6.86 | 6.46 | 5.83 |
| Ratio of monocyte/lymphocyte | 1.15 | 1.1 | 1.05 | 0.97 | 0.78 | 0.33 |
–: missing value.
Table 2.
Indexes of blood routine, and liver and kidney function.
| Item | Time point |
|||||
|---|---|---|---|---|---|---|
| 2/20 | 2/24 | 2/29 | 3/4 | 3/8 | 4/29 | |
| White blood cell (109/L) | 21.38 | 11.53 | 14.43 | 10.76 | 12.76 | 8.52 |
| Neutrophil (%) | 84.1 | 75.4 | 83.6 | 74 | 75.1 | 80.9 |
| Lymphocyte (%) | 5.9 | 10.0 | 7.6 | 10.8 | 11.6 | 13.8 |
| Monocyte (%) | 6.8 | 10.9 | 7.9 | 10.4 | 9 | 4.6 |
| Neutrophil (109/L) | 17.96 | 8.69 | 12.08 | 7.96 | 9.57 | 6.89 |
| Lymphocyte (109/L) | 1.27 | 1.15 | 1.09 | 1.16 | 1.48 | 1.18 |
| Monocyte (109/L) | 1.46 | 1.26 | 1.14 | 1.12 | 1.15 | 0.39 |
| Red blood cells (1012/L) | 3.29 | 3.00 | 3.45 | 3.39 | 3.78 | 4.29 |
| Hemoglobin (g/L) | 103 | 94 | 111 | 107 | 119 | 134 |
| Hematocrit (%) | 30.2 | 28.7 | 33.5 | 33.1 | 36.6 | 41.1 |
| Platelets (109/L) | 242 | 274 | 271 | 221 | 339 | 240 |
| Alanine aminotransferase (IU/L) | 38 | 32 | 48 | 50 | 35 | 10 |
| Aspartate aminotransferase (IU/L) | 25 | 25 | 46 | 41 | 25 | 20 |
| Alkaline phosphatase (IU/L) | 119 | 97 | 122 | 131 | 135 | – |
| γ Glutamyl transpeptidase (IU/L) | 56 | 39 | 41 | 41 | 38 | – |
| Total protein (g/L) | 59.7 | 60.6 | 74.3 | 74.4 | 75.5 | 72.7 |
| Albumin (g/L) | 29.9 | 35.8 | 45.2 | 42.9 | 43.6 | 46.7 |
| Globulin (g/L) | 29.8 | 24.8 | 29.1 | 31.5 | 31.9 | 26.0 |
| Total bilirubin (μmol/L) | 12.3 | 11.1 | 11.1 | 14.9 | 8.3 | 7.2 |
| Direct bilirubin (μmol/L) | 4.7 | 4.3 | 4.2 | 4.4 | 2.5 | – |
| Total bile acid (μmol/L) | 8.5 | 5.2 | 23.1 | 13.3 | 9.7 | – |
| Urea nitrogen (mmol/L) | 7.1 | 5.8 | 10 | 10 | 10 | 6.06 |
| Creatinine (μmol/L) | 57.6 | 71.4 | 115 | 95.9 | 83.6 | 78 |
| Uric acid (μmol/L) | 121 | 196 | 240 | 254 | 339 | – |
| Creatine kinase (IU/L) | 78 | 57 | 67 | 70 | 71 | – |
| Fasting blood glucose (mmol/L) | 9.6 | 8.7 | 7.6 | 6.6 | 8.0 | – |
–: missing value.
4. Treatments and timeline
After admission, based on the patient’s poor condition, high-volume oxygen was given with a mask (5 L/min) as well as an antibiotic treatment with moxifloxacin (Schering Ltd., Guangzhou, China; 0.4 g, iv, qd, for 7 d). Metoprolol (AstraZeneca AB, Sweden; 47.5 mg, po, qd) was also administered to help control the heart rate. Due to high blood glucose levels on admission day 2, insulin was given to control the blood glucose. On February 23, treatment with montelukast sodium (Merck Pharmaceuticals Ltd., Darmstadt, Germany; 10 mg, po, for 21 d) was initiated to manage the wheezing and shortness of breath caused by potential asthma and to decrease the number of asthma attacks while in the hospital.
Her postprandial blood glucose was not well controlled (on March 2, it was 26 mmol/L post-breakfast, 9.7 mmol/L post-lunch, and 16.8 mmol/L post-dinner), therefore, the hypoglycemic drugs were changed to Novolin R (Novo Nordisk China Pharmaceuticals Ltd., Beijing, China), a biosynthetic human insulin injection (16 IU, before breakfast; 12 IU, before dinner), in combination with acarbose (Shanghai Maokang Biotechnology Co., Ltd., Shanghai, China; 50 mg, po, at lunch).
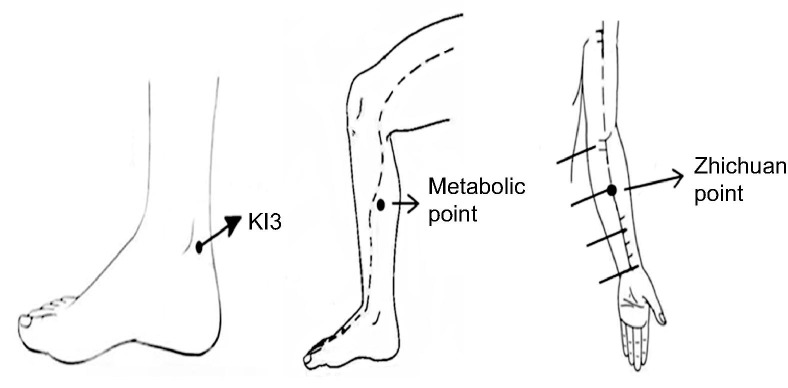
Acupuncture treatment was performed on-site on admission day 1 (February 20; in Leishenshan Hospital). Bilateral acupoints (Fig. 1 ) of Taixi, Metabolic (Metabolic-point), and Zhichuan (Breathless-relief point) were used at depths varying from 1.5 to 2.5 cm, depending on the point. Hwato 0.25 mm × 40 mm disposal needles (Suzhou Huatuo Acupuncture Equipment General Factory, Suzhou, China) were used for all points, and needling was performed for about 15–30 s with twisting and lifting until the Deqi reaction was achieved, before the needles were removed. Acupuncture was performed daily, as a major therapy for improving the patient’s condition—because it showed immediate effectiveness on the breath rate, SpO2, and the heart rate (see below).
Fig. 1.
Location of acupoints. (A) KI3 (Taixi), located at the posterior edge of medial malleolus, at the middle point between the tip of medial malleolus and the Achilles tendon posterior edge. Commonly used for the patient with symptoms of shortness of breath, fast breath rate, and slow absorption of lung lesions in respiratory diseases. (B) Metabolic point, located at 8 cun above the tip of the medial malleolus, the posterior margin of the tibia, used for loss of appetite, poor appetite, weak and fatigue. (C) Zhichuan point, located at middle-line of palm side of forearm, the upper 1/3 of the line connecting the wrist stripe and elbow stripe, used for lack of consciousness, heart palpitations, chest tightness, shortness of breath, etc.
Traditional Chinese herbal medicines were also a part of this supporting treatment plan. Fuzheng Rescue Lung (Fuzheng Jiufei) granules [6] (Table 3 ) were taken orally from February 21, at the dose of 1 pack per dose, and 2 doses per day. Three days later (February 24) Xuebijing Injection (XBJ), a Chinese herbal medicine-derived therapeutic [3], [5] was administered at a dose of 100 mL per day, for 4 d.
Table 3.
The composition of Fuzheng Rescue Lung Granules.
| Herbs (dose) | Action(s) |
|---|---|
| Aconiti Lateralis Radix Praeparaia (Shufuzi) 10 g | Warm & strengthen kidney yang |
| Zingiberis Rhizoma (Ganjiang) 15 g | Warm & strengthen kidney yang |
| Glycyrrhizae Radix et Rhizoma (Zhigancao) 20 g | Warm and strengthen kidney yang; strengthen spleen |
| Lonicerae Japonicae Flos (Jinyinhua) 10 g | Clear heat & detoxify; expel the external pathogens |
| Gleditsiae Spina (Zaojiaoci) 10 g | Clear & detoxify; drain pus |
| Wuzhaolong 20 g | Invigorate spleen-qi |
| Pogostemonis Herba (Guanghuoxiang) 10 g | Remove dampness |
| Citri Reticulatae Pericarpium (Chenpi) 5 g | Remove dampness |
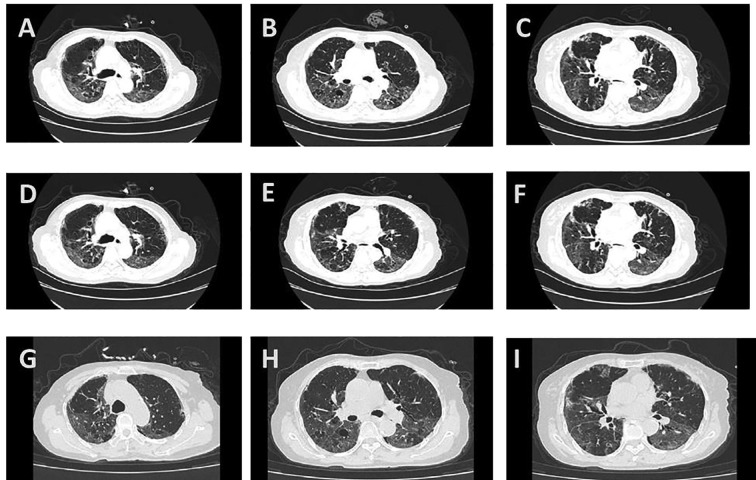
Since the CT scan indicated that the absorption of the lung infection was slow, on March 4, the dosage of Fuzheng Rescue Lung granules was doubled (2 packets per dose, two doses per day) for accelerating the absorption of pneumonia. Because the patient’s poor sleep quality affected her recovery, the herbal decoction Guizhi Gancao Longgu Muli Tang (a classic herbal formula, including Cinnamomi Ramulus, Glycyrrhizae Radix et Rhizoma, dragon bone and Ostreae Concha) [7] was also added to her treatment plan (1 dose/d of a decoction made by the Leishenshan Hospital Pharmacy, Wuhan, China) for a course of 5 d.
5. Results, discharge and follow-up
5.1. Change in symptoms and signs
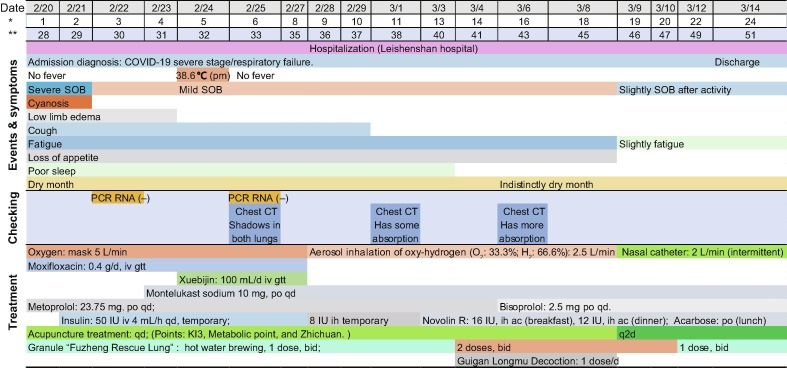
On admission day 1 (February 20), 10 min after the initial acupuncture treatment, the patient felt that her chest and lower abdomen were no longer tense, she could breathe easier and more deeply, and her state of mind was much more relaxed. Her bedside monitor showed that her heart rate decreased by 12 beats/min (to 96 beats/min) and the SpO2 increased by 8% (98%); also, her cyanosis of the lips and nails was less noticeable when checked 2 hours later. The relief of symptoms through acupuncture alone was very significant, and these treatment effects could last for a few hours (Fig. 2 ).
Fig. 2.
Events, exam, and treatment timeline accordance with date and the day of illness and hospitalization (February 20 to March 14, 2020). ac: ante cibum; SOB: shortness of breath; PCR: polymerase chain reaction; CT: computed tomography; po: per os (taken orally); ih: hypodermic injection; iv gtt: intravenous gutta (drop); bid: bis in die (twice a day); pm: post meridiem; q2d: every other day; qd: quaque die (once a day). *: day of admission; **: day of disease.
After 9-day treatment (February 29), the patient’s shortness of breath showed significant improvement; she was without cough and phlegm, with no edema in either leg, and her sleep was better; the only symptom that did not improve with this treatment was her dry mouth with bitter taste.
5.2. Change in blood tests
On February 22 and 25, her PCR tests for SARS-COV-2 were negative. Improvement in her blood tests also were observed after treatment. On February 24, the ratio of neutrophil/lymphocyte (NLR) decreasing from 14.14 to 7.55 indicated a reduction in her severe condition (Table 1). On March 8, her blood test showed more improvement (Table 1, Table 2) and the NLR of 6.46 supported this trend.
5.3. Changes in the CT scan
On admission day 6 (February 25), her CT scan showed “viral pneumonia” (Fig. 3 ).
Fig. 3.
The changes of pneumonia on patient’s CT scans. (A–C) CT scan on Feb 25; (D–F) CT scan on March 1; (G–I) CT scan on March 6. (A, D and G) represent the images of upper lungs; (B, E and H) represent middle lungs; (C, F and I) represent lower lungs.
She continued to receive daily treatment with acupuncture and traditional Chinese herbal medicines, and on admission day 11 (March 1), her chest CT showed that “pneumonia has some absorption” (Fig. 3). The patient was still experiencing some shortness of breath and poor sleep, but her dry mouth with bitter taste had significantly improved. On March 6, the CT scan showed “obvious absorption” (Fig. 3).
5.4. Discharge
On admission day 19 (March 9), the patient was in good spirits, with no fever, cough or phlegm, but with mild shortness of breath after activity and mildly dry mouth with bitter taste. Fatigue was improved, sleep was normal, and urination and bowel movement were also normal. The vital signs were: heart rate 78 beats/min, breath rate 18 beats/min and SpO2 99%. Oxygen therapy was reduced to nasal catheter oxygen inhalation at a flow of 2 L/min. Cyanosis of her lips and nails was much reduced, and she could use daily intermittent oxygen inhalation for 3–4 h per day, without obvious shortness of breath and maintaining an SpO2 95%. Based on the relief of symptoms, acupuncture treatment was reduced to once every other day. On admission day 24 (illness day 51, March 14), the patient was discharged.
5.5. Follow-up
After discharge, she was sent to a designated quarantine center in the Hongshan Community of Wuhan for recovery. She stayed there for additional two weeks before returning to her home. During her time in quarantine, her PCR tests (taken two times) were negative. A follow-up check was done on April 25, 2020; the patient reported she still had occasional mild cough with little phlegm, slight dry mouth, and a little shortness of breath after activity. Beside these symptoms, her appetite and sleep were fine, and she was without other discomfort. Her PCR test for SARS-COV-2 remained negative. Other follow-up tests were conducted on April 29, 2020 (Table 1, Table 2).
6. Discussion
This case study was about the treatment program used for an elderly patient with recalcitrant severe COVID-19, with undiscovered diabetes, repeated symptoms and prolonged illness (two admissions, for total 51 d in hospitals). This disease profile typically has a high fatality rate. In Wuhan, the fatality rate could be as high as 45.4% in patients with severe or critical COVID-19 [8]. The diagnosis of this patient with severe COVID-19 was based on her clear COVID-19 illness history, typical clinical symptoms, signs and laboratory testing [3]; even her PCR test, done via nasopharyngeal swab sample, became negative while her condition worsened. Evidence from pathology showed that residual SARS-CoV-2 viruses were present in the pulmonary tissues of a patient whose PCR test from nasopharyngeal swab had been negative for three consecutive days and who was ready-for-discharge [9]. This indicates that a PCR-test turning negative does not mean that the COVID-19 is gone from the body, and the pathology caused by the SARS-CoV-2 virus may continue to cause multiple organ damage, dysfunction and even patient death. Studies have shown that patients with COVID-19 have the highest viral load in nasopharyngeal swabs on days 4–5, and seroconversion of most patients occurs in the second week of symptoms. However, the seroconversion does not completely eliminate the virus immediately, and the viral load will decrease slowly [10]. The main organ affected in COVID-19 is the lung, where the large airways and alveoli are damaged, transforming the disease into a critical illness and acute respiratory distress syndrome. The lung tissue develops pulmonary edema formed by hyaline membrane, pulmonary vasodilatation, congestion, lymphocyte infiltration and thrombosis [9], [11].
Acupuncture and traditional Chinese herbal medicine were integrated into the treatment plan for this patient. Based on pattern differentiation, acupuncture and Chinese herbal medicines used in this case focused on improving the patient’s critical clinical symptoms, such as shortness of breath, rapid heart rate, and anorexia, while her COVID-19 disease was still at a severe stage. The integration of these therapies with standard care, which included oxygen therapy, adjusting the glucose levels, and antibiotic medications. The effect of the antiviral medicines used for this COVID-19 patient, oseltamivir and arbidol, have not been associated with statistically significant clinical benefits [12] while antibacterial medicine moxifloxacin may have been helpful in preventing bacterial infection.
NLR is a useful indicator for evaluating the severity of a COVID-19 patient’s condition. An NLR of 4.06 may be indicative of severe COVID-19, while an NLR of 9.38, with increased neutrophil numbers, could be an indication of a COVID-19 patient in critical condition [13], [14]. Studies show that severe COVID-19 cases had higher leucocyte levels, higher neutrophil levels, a higher ratio of monocyte/lymphocyte (MLR) and a higher NLR; in critical cases, NLR numbers as high as 14.44 were reported [13], [14]. This patient’s NLR and MLR were 14.14 and 1.15, respectively, on the day of admission to Leishenshan Hospital. After treatment and before discharge, they were reduced to 6.46 and 0.78 respectively, and had continued to fall to 5.83 and 0.33 at the follow-up (on April 29; 46 days post-discharge). At the same time, the inflammatory markers lactate dehydrogenase and C-reactive protein (CRP) also significantly decreased (Table 1, Table 2). All of these were indications of significant improvement, while her clinical symptoms almost disappeared.
Acupuncture for the treatment of COVID-19, especially in the severe stage, was under-used, under-evaluated, and under-reported both in China and the West. One of the possible reasons for this phenomenon is that acupuncture has not been adopted as a first-line therapy, due to the concern that patients may transmit this disease to healthcare providers through prolonged, close contact. In China, Chinese medicine doctors are one type of physician [15], [16] and they are eligible to treat patients with COVID-19 in hospitals, using integrative therapies, including acupuncture [17]. In the West, especially in the United States (U.S.), limited by law, the majority of Chinese medicine providers are licensed acupuncturists (LACs) [15], [16] and are not eligible to directly treat COVID-19 patients, especially in COVID wards in hospitals, due to legal barriers [18]. It is the current authors’ experience that it is difficult to publish this academic paper in the U.S., mainly because the editors and reviewers of some medical journals are afraid of LACs learning this research and directly treating COVID-19 patients by themselves, which may cause disputes in legal fields.
In this case report, we find that acupuncture played a significant role in decreasing the patient’s difficulty of breathing, increasing the SpO2 and decreasing the elevated heart rate. At the same time, acupuncture made the patient calmer and presented an anti-inflammatory effect. Its effectiveness was observed immediately after the first treatment, and daily acupuncture treatments made the effects more stable. The acupuncture was easy to perform and did not have obvious adverse effects; further acupuncture could be practiced while maintaining the safety of the practitioner. We hope acupuncture can be used for more COVID-19 patients. LACs should work with medical doctors and law-makers and overcome the legal barriers, to allow integration of acupuncture and Western medical care in COVID wards.
From the perspective of biomedicine, studies have found that acupuncture can regulate the activity of immune cells such as macrophages and lymphocytes [19] and can also significantly reduce inflammation [20]. He et al. [21] pointed out that for COVID-19, acupuncture may be used, and it can play an anti-inflammatory effect by activating the vagus nerve through the cholinergic anti-inflammatory pathway [22]. In severe inflammation such as in the sepsis stage, evidence in both preclinical studies and clinical trials shows that activating the autonomic nervous system by acupuncture can significantly modulate the immunity, protect the function of internal organs and decrease the fatality rate [23]. From the perspective of Chinese medicine, current acupuncture treatments were focused on strengthening the kidney and spleen, and adjusting the lung, heart and liver. Taixi points (Fig. 1) are the Yuan (source) points of kidney meridians, which are classic points frequently used in clinical practice to improve shortness of breath, rapid shallow breathing or dyspnea, and slow absorption of inflammatory lesions. Studies show that acupuncture at Taixi with Sanyinjiao (SP6), Zusanli (ST36), Neiguan (PC6) and other acupoints, compared to the no-acupuncture group, significantly improved the lung function of patients with asthma [24]. Needling Taixi with points SP6, Shenshu (BL23) and Pishu (BL20) improved the fatigue, insomnia and other symptoms of patients with chronic fatigue syndrome. Its mechanism may be related to the reduction of serum interleukin-6 and interferon-γ level [25]. Metabolic and Zhichuan points (Fig. 1) are extra-meridian acupoints adopted from Professor Xu Zou’s experience. The former is at the intersection of spleen and liver meridians and is good for improving appetite, fatigue and weakness; the latter is on the palmar side of the forearm and is good for treating dizziness, heart palpitations, chest tightness and shortness of breath. The location of Zhichuan point is consistent with the position of “Lung Disease Point” (LDP) in Professor Wang Wenyuan’s balance acupuncture. Xu et al. [26] reported that needling LDP has a positive and rapid effect on the relief of asthma symptoms, without significant adverse effects. Chai et al. [27] revealed that the total effective rate of needling at LDP, combined with “Chest Pain Point,” is 83.3% in the treatment of patients with chest pain, following bronchial lung cancer. It is noted that acupuncture’s effects are felt quickly, and it is safe and convenient to use. The combination of Taixi, Metablic and Zhichuan points are called “Leishen Three Acupoints,” which were used by Zou’s team on COVID-19 patients in several stages; they were able to improve patients’ lung and heart function, reduce respiration rate and heart rate, and to prevent the worsening of cardiopulmonary conditions.
Herbal therapies have been recommended by the China National Health Commission for the treatment of COVID-19 [3] and 91.5% (or 74,187) COVID-19 patients in China use Chinese herbal medicine combined with standard care [17]. Zhang et al. [28] proposed that Chinese herbal medicines play a role by regulating immune balance. Song et al. [5] and Ren et al. [29] pointed out that such herbal medicine can decrease the cytokine storm in COVID-19 patients. Chinese medicine XBJ, a Chinese patented medicine, is recommended to be used in the severe and critical cases for preventing the cytokine storm and systemic inflammatory response syndrome [30]. Following the guideline [3] XBJ was adapted to this patient’s treatment. It may decrease the level of sepsis, improve organs’ function and successfully truncate the bad prognosis of the patient’s condition. Wen et al. [31] reported that in severe COVID-19 patients, compared with the control group, XBJ improved the white blood cell and lymphocyte counts, reduced the level of CRP and the red blood cell sedimentation rate and reduced the Acute Physiology and Chronic Health Evaluation II score (APACHE II score), resulting in improved patient prognosis. The study by Ma et al. [32] showed that XBJ significantly reduced the severity of pneumonia index in critically ill patients with COVID-19, the average time to improve symptoms and signs, the time for nucleic acid (PCR-test) to become negative, lung imaging (chest X-ray/chest CT) improvement time and mechanical ventilation time. Chinese herbal medicines also played an auxiliary role in the balance of the patient’s immune function. Integrating acupuncture and herbal medicine with the standard care may have increased the rate of patient and reduced adverse effects [17]. In this case, Fuzheng Rescue Lung granules, an empirical formula (a Chinese patent medicine granule, developed by Professor Zhongde Zhang and Professor Xu Zou), was administered as a basic herbal remedy, especially when patient’s lung infection was worse and not absorbed very well even after multiple treatments had been applied. The course of illness lasted over one and half months. With the help of acupuncture and herbs, especially the addition of the herbal formula dosage on March 4 (illness day 41), the absorption of the patient’s lung infection was much better, and most symptoms disappeared after the herb doses were doubled. At the same time, obvious adverse effects on complete blood counts, and liver and kidney functions were not found.
It should be noted that acupuncture providers must wear medical protective clothing and gloves to see COVID-19 patients; even it may increase the difficulty of performing acupuncture. The role of acupuncture and Chinese herbal medicine, as one part of integrative therapies discussed in this paper, did not replace the effect of standard care, although specific drugs and therapies for COVID-19 are still lacking. The standard care, especially the supporting therapies, antibiotics and symptomatic treatments, has played an important role in the recovery of patients with severe COVID-19.
7. Conclusion
Based on the potential effectiveness and the safety of the treatment, we recommend that acupuncture and Chinese herbal medicine be integrated with standard care for COVID-19 patients, even for severe cases, since there is no drug or therapy that can cure this highly contagious and life-threatening disease. The current case report is an exploratory and preliminary study; therefore, more rigorous clinical trials are warranted to further study the effectiveness and safety of acupuncture and herbal medicine in the treatment of COVID-19 or similar conditions.
Acknowledgments
Acknowledgements
We express thanks to Dr. Sarah Faggert Alemi for English editing, and Dr. David Riley, an editor of the CARE (Case Reports) Guidelines for manuscript reviewing.
Funding
Guangdong Provincial Famous TCM Veteran Experts Zou Xu Inheritance Studio.
Authors’ contribution
AYF proposed this English case report project, after XZ had briefed his team’s work in a WeChat discussion in early April 2020. XZ, AYF and SX initiated the project together. XY, SBC, LTT, LMC, ZDZ and XZ drafted the first manuscript in Chinese, and AYF, SX and XZ discussed further and extensively, drafted the English version, revised and finalized the manuscript.
Declaration of competing interest
The authors have no conflicts of interest.
References
- 1.World Health Organization. WHO Director-General’s opening remarks at the Mission briefing on COVID-19—12 March 2020. (2020-03-12) [2020-11-26]. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mission-briefing-on-covid-19---12-march-2020.
- 2.World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). (2020-02-16) [2020-11-26]. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 3.National Health Commission & State Administration of Traditional Chinese Medicine. Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7). (2020-03-03) [2020-11-26]. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.
- 4.Gagnier J.J., Kienle G., Altman D.G., Moher D., Sox H., Riley D., CARE Group The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv. Health Med. 2013;2(5):38–43. doi: 10.7453/gahmj.2013.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song Y., Yao C., Yao Y., Han H., Zhao X., Yu K., et al. Xuebijing Injection versus placebo for critically ill patients with severe community-acquired pneumonia: a randomized controlled trial. Crit Care Med. 2019;47(9):e735–e743. doi: 10.1097/CCM.0000000000003842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China. Beijing: China Medical Science and Technology Press; 2015: 14, 45, 87, 177, 191, 221.
- 7.Wang Z., Ke D., Huang X., Ding Y., Wang C. Effect of Guizhi Gancao Longgu Muli Tang on sleep disturbances in menopausal women. J Tradit Chin Med. 2017;37(1):23–29. doi: 10.1016/s0254-6272(17)30022-5. [DOI] [PubMed] [Google Scholar]
- 8.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yao X.H., He Z.C., Li T.Y., Zhang H.R., Wang Y., Mou H.M., et al. Pathological evidence for residual SARS-CoV-2 in pulmonary tissues of a ready-for-discharge patient. Cell Res. 2020;30(6):541–543. doi: 10.1038/s41422-020-0318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wölfel R., Corman V.M., Guggemos W., Seilmaier M., Zange S., Müller M.A., et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 11.Zhou B, Zhao W, Feng R, Zhang X, Li X, Zhou Y, et al. The pathological autopsy of coronavirus disease 2019 (COVID-2019) in China: a review. Pathog Dis 2020; 78(3):ftaa026. [DOI] [PMC free article] [PubMed]
- 12.Lian N., Xie H., Lin S., Huang J., Zhao J., Lin Q. Umifenovir treatment is not associated with improved outcomes in patients with coronavirus disease 2019: a retrospective study. Clin Microbiol Infect. 2020;26(7):917–921. doi: 10.1016/j.cmi.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma Y, Shi N, Fan YP, Wang JY, Zhao C, Li GX, et al. Predictive value of the neutrophil-to-lymphocyte ratio (NLR) for diagnosis and worse clinical course of the COVID-19: findings from ten provinces in China. SSRN. (2020-04-14) [2020-11-26]. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3569838.
- 14.Sun S., Cai X., Wang H., He G., Lin Y., Lu B., et al. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou. China. Clin Chim Acta. 2020;507:174–180. doi: 10.1016/j.cca.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fan A.Y., Wei H., Tian H., Huang J., Alemi S.F. Universities of Chinese medicine enter the global stage of best universities rankings in 2020. Med Acupunct. 2020;32(3):136–142. doi: 10.1089/acu.2019.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fan A.Y., He D., Gu S., Tian H., Ouyang H., Wei H., et al. Estimated number of acupuncture practitioners in mainland China in 2018: multiperspectives. Med Acupunct. 2020;32(5):310–319. doi: 10.1089/acu.2020.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fan A.Y., Gu S., Alemi S.F. Research Group for Evidence-based Chinese Medicine. Chinese herbal medicine for COVID-19: current evidence with systematic review and meta-analysis. J Integr Med. 2020;18(5):385–394. doi: 10.1016/j.joim.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Certification Commission for Acupuncture and Oriental Medicine. NCCAOM updates on coronavirus (COVID-19). (2021-01-04) [2021-03-10]. https://www.nccaom.org/nccaom-covid19-hub-coronavirus-updates/.
- 19.Yamaguchi N., Takahashi T., Sakuma M., Sugita T., Uchikawa K., Sakaihara S., et al. Acupuncture regulates leukocyte subpopulations in human peripheral blood. Evid Based Complement Alternat Med. 2007;4(4):447–453. doi: 10.1093/ecam/nel107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao YX, He W, Jing XH, Liu JL, Rong PJ, Ben H, et al. Transcutaneous auricular vagus nerve stimulation protects endotoxemic rat from lipopolysaccharide-induced inflammation. Evid Based Complement Alternat Med 2012;2012:627023. [DOI] [PMC free article] [PubMed]
- 21.He W., Shi X.S., Zhang Z.Y., Su Y.S., Wan H.Y., Wang Y., et al. Discussion on the effect pathways of preventing and treating coronavirus disease 2019 by acupuncture and moxibustion from the regulation of immune inflammatory response. Zhongguo Zhen Jiu. 2020;40(8):799–802. doi: 10.13703/j.0255-2930.20200305-0001. [Chinese with abstract in English] [DOI] [PubMed] [Google Scholar]
- 22.Gao YQ. Therapeutic strategies for COVID-19 based on its pathophysiological mechanisms. Zhongguo Bing Li Sheng Li Za Zhi 2020; 36(3):568–72,576 [Chinese with abstract in English].
- 23.Pan W.X., Fan A.Y., Chen S., Alemi S.F. Acupuncture modulates immunity in sepsis: Toward a science-based protocol. Auton Neurosci. 2021;232 doi: 10.1016/j.autneu.2021.102793. [DOI] [PubMed] [Google Scholar]
- 24.Zhang WP. Effects of acupuncture on the pulmonary function and heart rate variability in different state of bronchial asthma. Zhen Ci Yan Jiu 2007;1:42–8 [Chinese with abstract in English]. [PubMed]
- 25.Xu Y.X., Luo H.S., Sun D., Wang R., Cai J. Acupuncture in the treatment of chronic fatigue syndrome based on “interaction of brain and kidney” in TCM: a randomized controlled trial. Zhongguo Zhen Jiu. 2019;39(2):123–127. doi: 10.13703/j.0255-2930.2019.02.003. [Chinese with abstract in English] [DOI] [PubMed] [Google Scholar]
- 26.Xu G.F., Yan F., Li M. Balance acupuncture for 33 cases of asthma syndrome. Zhongguo Zhen Jiu. 2012;32(6):527–528. [Chinese with abstract in English] [PubMed] [Google Scholar]
- 27.Chai X.S., Wu W.Y., Deng H., Zhou Y.S., Zhao Y.J. Treatment of 24 cases of chest pain following lung cancer by balancing acupuncture therapy. J Acupunct Tuina Sci. 2008;6:363–365. [Google Scholar]
- 28.Zhang Y.G., Tan R.R., Ren S.C., Ma X., Yan Z.X., Hua H., et al. New method for evaluating pharmacodynamics of traditional Chinese medicine compounds based on its moderate regulation and principle of balanced adjustment of immunity under pan-immunomic. Zhongguo Zhong Yao Za Zhi. 2018;43(16):3229–3234. doi: 10.19540/j.cnki.cjcmm.20180629.002. [Chinese with abstract in English] [DOI] [PubMed] [Google Scholar]
- 29.Ren Y., Yao M.C., Huo X.Q., Gu Y., Zhu W.X., Qiao Y.J., et al. Study on treatment of “cytokine storm” by anti-2019-nCoV prescriptions based on arachidonic acid metabolic pathway. Zhongguo Zhong Yao Za Zhi. 2020;45(6):1225–1231. doi: 10.19540/j.cnki.cjcmm.20200224.405. [Chinese with abstract in English] [DOI] [PubMed] [Google Scholar]
- 30.Yin Q., Li C. Treatment effects of Xuebijing Injection in severe septic patients with disseminated intravascular coagulation. Evid Based Complement Altern Med. 2014;2014 doi: 10.1155/2014/949254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wen L., Zhou Z., Jiang D., Huang K. Effect of Xuebijing Injection on inflammatory markers and disease outcome of coronavirus disease 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32(4):426–429. doi: 10.3760/cma.j.cn121430-20200406-00386. [Chinese with abstract in English] [DOI] [PubMed] [Google Scholar]
- 32.Ma Q., Qiu M., Zhou H., Chen J., Yang X., Deng Z., et al. The study on the treatment of Xuebijing Injection (XBJ) in adults with severe or critical corona virus disease 2019 and the inhibitory effect of XBJ against SARS-CoV-2. Pharmacol Res. 2020;160 doi: 10.1016/j.phrs.2020.105073. [DOI] [PMC free article] [PubMed] [Google Scholar]