Abstract
Background:
Urological education is as important as surgical training for undergraduates. However, students in undergraduate medical schools have less exposure to urology as their curriculum focuses more on clinical skills, particularly community-based healthcare for a super-aging society. This study aimed to evaluate whether urology-related hands-on training could increase the interest of undergraduate medical students in urology.
Methods:
A 1-day elective program in urological surgery at the University of Tsukuba, particularly in robotic, laparoscopic, and endoscopic surgeries, was offered to 85 fourth-year medical students from 2018 to 2020, prior to their clinical clerkship. The average age of the participants was 22 (range: 21-25) years. We used a scoring system that comprised 1-5 Likert-type items to assess training activity, interest in surgery, and interest in urology before and after the course.
Results:
Before attending the program, the average scores of interest in urology were 3.53 in 2018, 3.15 in 2019, and 3.00 in 2020. The scores in surgery increased after the program; however, this was not significantly different from scores prior to the program. However, the average interest scores in urology were significantly increased to 3.91 ± 0.63 (P < .05), 3.88 ± 0.58 (P < .01), and 4.00 ± 0.61 (P < 0.01) in 2018, 2019, and 2020, respectively. Total likely scores of this program in 2018, 2019, and 2020 were 4.59, 4.76, and 4.88, respectively, indicating a motivation to study surgery and urology during clinical clerkship.
Conclusions:
Urological hands-on training facilitated interest in urology in medical students prior to their clinical clerkship.
Keywords: Early exposure, urology, surgical skills, simulation-based learning
Background
Medical school provides an opportunity to not only acquire knowledge and skills but also experience in various specialties. Medical students in earlier years of schooling, study and learn with the help of classroom lectures and other recently adopted clinically-oriented teaching methods. 1 After gaining basic medical knowledge, they learn skills through a rotating clinical clerkship program lasting over a period of 6 years after graduating from high school in Japan. 2 In addition to subject-specific knowledge, medical students must learn the required attitude and skills that will make them qualified to meet the needs of citizens. 3 In Japan, upcoming medical doctors are required to have clinical skills, especially in community-based health care for the super-aging society. 4 Thus, medical schools are modifying their curriculum to consider these societal needs. Resultantly, medical students obtain less experience in surgical subjects compared to other essential medical specialties, such as internal medicine, psychology, and primary healthcare. 5 To bridge this increasing gap in knowledge, several surgical departments have been trying to teach surgery more efficiently in an educational program at medical school.
Simulation-based learning is broadly used in medical schools globally. Simulation is very useful for beginners to learn invasive procedures, including physical examination, puncture procedures, and emergency treatment. 6 In surgical fields, simulation-based learning is not only known as an important tool for surgical resident education but has also been shown to increase the efficiency of trainees. Undergraduate medical students have the opportunity to experience surgery during clinical clerkship. However, medical students are often are not well-prepared to participate in surgery because they have less opportunity to learn surgical procedure even with simulation training before clinical clerkship. In order to accelerate their surgical learning, it is also important to provide some motivation for medical students before the commencement of clinical clerkship.
The school of medicine at the University of Tsukuba has given an “advanced course” to fourth-year medical students prior to starting their clinical clerkship. This short course consists of intensive lectures or workshops based on the concept of exposing pre-clinical clerkship students to recent, focused, and advanced medical issues. Several professors offer lectures or workshops on various disciplines totally 25 programs, such as basic science, medical statistics, internal medicine, psychology, surgery, anesthesia, social medicine, and space medicine. Each student can select several courses from those programs in their fields of interest over one week. To provide a chance to learn surgery, we have given hands-on seminars on endoscopic, laparoscopic, and robotic surgeries for students just before clinical clerkship since 2012. Students who attend this course as a form of early exposure of urological surgery seem to be motivated to learn and are more interested in surgery and urology following clinical clerkship.
We hypothesized that early exposure of urological and surgical experience acts as a trigger to increase their interest, and a positive experience would motivate students to learn not only surgery but also urology. This study evaluated whether this urology course, designed to provide the required exposure to medical students, could cultivate an interest in urology among medical students before they commence clinical clerkship.
Methods
Course design
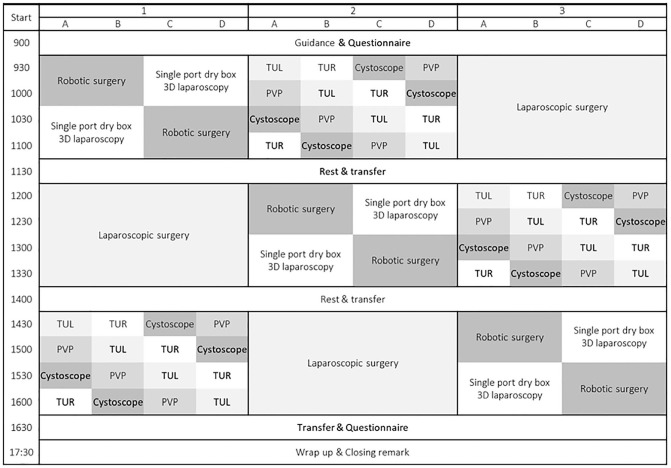
A one-day elective course focused on hands-on training in urologic surgery, particularly robotic, laparoscopic, and endoscopic surgeries, was offered to fourth-year medical students of the University of Tsukuba. Participants were separated into 3 groups. Subsequently, each group rotated through endoscopic procedures, laparoscopic suturing, and robotic surgery over 2 hours (Figure 1). The grouped students were further separated into 4 subgroups that rotated through endoscopic workshops lasting for 30 minutes each, including cystoscopy, transurethral resection, laser prostatectomy, and transurethral lithotripsy (Figure 2).
Figure 1.
Rotation schedule of medical students. Students are divided into small groups of 2 or 3 students each, and they rotated through each procedure.
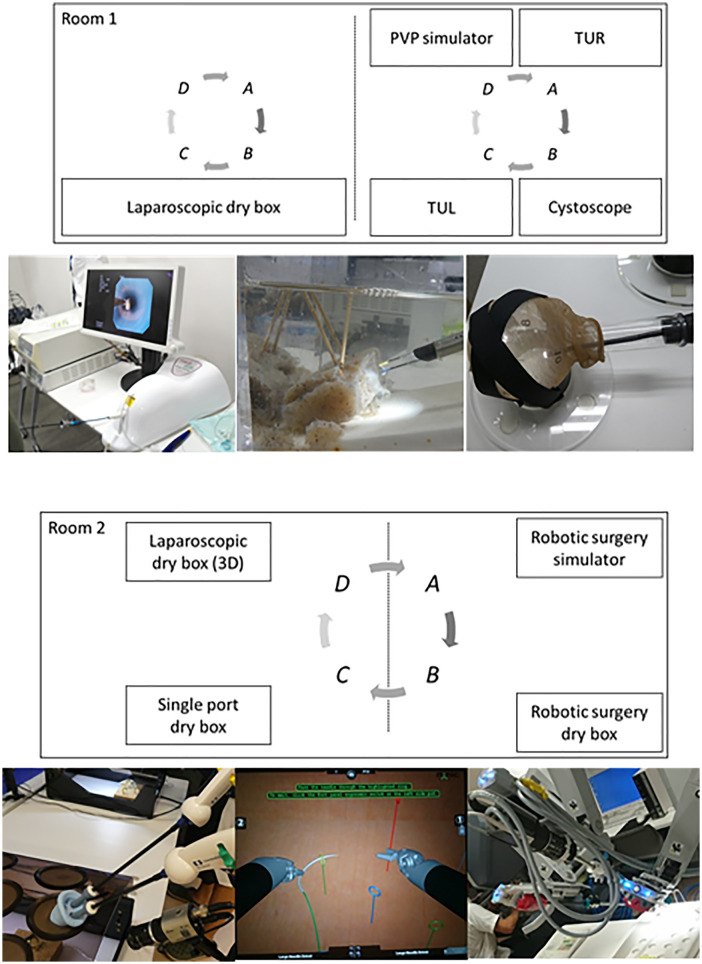
Figure 2.
The schema of the arrangement of the training room and pictures of each procedure. Small groups move around the room in a circle, spending 30 minutes at each station.
In the robotic surgery course, students used the DaVinci skills simulator of preinstalled tasks including “Endo Wrist Manipulation”, “Energy and Dissection”, and “Needle Control and Driving”. In the laparoscopic course, the students were trained in suturing skills using strings with a needle in a dry box. Meanwhile, the students in the endoscopic course were divided into 4 groups: transurethral resection (TUR), photo-selective vaporization of the prostate (PVP), cystoscopy, and transurethral lithotripsy (TUL). During the TUR session, the students cut a konjac plate (a jelly-like food made from the starch of the konjac potato) under a saline pool using the TUR system. During the PVP session, the laser vaporization procedure was demonstrated to students using a PVP simulator. During the cystoscopy session, students performed the cystoscopy procedure using a flexible cystoscope on a flask, which resembled the urinary bladder. During the TUL session, students used a flexible ureteroscope and basket forceps to remove simulated renal stones out of a urinary tract model. Eleven urology faculty members including 2 female urologists and several staff of the medical equipment company helped to teach in the workshops.
Evaluation
Before the commencement of training, the participating students were asked to provide their demographic information in a pre-course survey. To check their filed of interest, the multiple selections were allowed in a list box which include internal medicine, surgery, urology, and so on. Furthermore, they provided a self-assessment (1-5 Likert-type items) on their interests. They checked the “5” score when they were very interested, while a “1” was scored when they were not interested at all. After the training, the participating students and faculty members were made to answer a post-course survey in which they were able to provide free descriptions in response to the questions. To evaluate the long-term effect of the course, we administered a web questionnaire to participating students. Evaluation of the participating students was performed at 3 months, 1 year, and 2 years after they took the course from 2018 to 2020. The questionnaire was the same as the provided self-assessment (1-5 Likert-type items) and free description surveys.
Assessment
Data for these evaluations were collected from all students enrolled in the course who completed the pre- and post-course surveys. We analyzed the mean difference in the interest score in surgery and urology before and after the program using paired t-tests with Bonferroni correction. All data analyses were performed using JMP14 (SAS Institute Inc., SAS Campus Drive, Cary, North Carolina 27513), and Microsoft Excel® ver. 2019. Descriptive statistics, chi-square test, or Fisher’s exact test were used, as appropriate. We also analyzed the answers obtained from the free description section of the questionnaire.
Results
Overall, 259 medical students were selected and enrolled in our course since 2012. Of these, 32, 26, and 27 students took this course among approximately 140 medical school fourth-year students each year in 2018, 2019, and 2020 respectively (Table 1). We could receive pre- and post-course survey from all participants each year. The average age of the participants was 22.2 (range: 21-25) years. Overall, 38.8% of participants were females as same as the ratio of female medical students had been between 30% and 40% each year at our school. Before attending the course, the average interest scores in surgery and urology were 4.01 and 3.25, respectively. The proportion of students who had considered a career in urology was 31.8%. Attending students were already interested in surgery but not so much in urology.
Table 1.
Background characteristics of participants.
| Fiscal year | Total | 2018 | 2019 | 2020 | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. of students | 85 | 32 | 26 | 27 | |||||
| Age | |||||||||
| Median | 22 | 22 | 22 | 22 | n.s. | ||||
| Range | 21-25 | 21-24 | 21-25 | 21-24 | |||||
| Sex | |||||||||
| Male | 52 | 61.2% | 21 | 65.6% | 16 | 61.5% | 15 | 55.5% | n.s. |
| Female | 33 | 38.8% | 11 | 34.4% | 10 | 38.5% | 12 | 44.5% | |
| Curiosity | |||||||||
| Internal medicine | 53 | 62.4% | 20 | 62.5% | 15 | 57.7% | 18 | 66.7% | n.s. |
| Surgery | 48 | 56.5% | 22 | 68.8% | 15 | 57.7% | 11 | 40.7% | n.s. |
| Urology | 27 | 31.8% | 14 | 43.8% | 5 | 19.2% | 8 | 29.7% | n.s. |
| Pre-course likely score | |||||||||
| Surgery | |||||||||
| Average | 4.01 | 4.12 | 4.00 | 3.89 | n.s. | ||||
| SD | 0.790 | 0.148 | 0.111 | 0.916 | |||||
| Urology | |||||||||
| Average | 3.25 | 3.53 | 3.15 | 3.00 | n.s. | ||||
| SD | 0.766 | 0.149 | 0.613 | 0.72 | |||||
Abbreviations: n.s, not significant; SD, standard deviation.
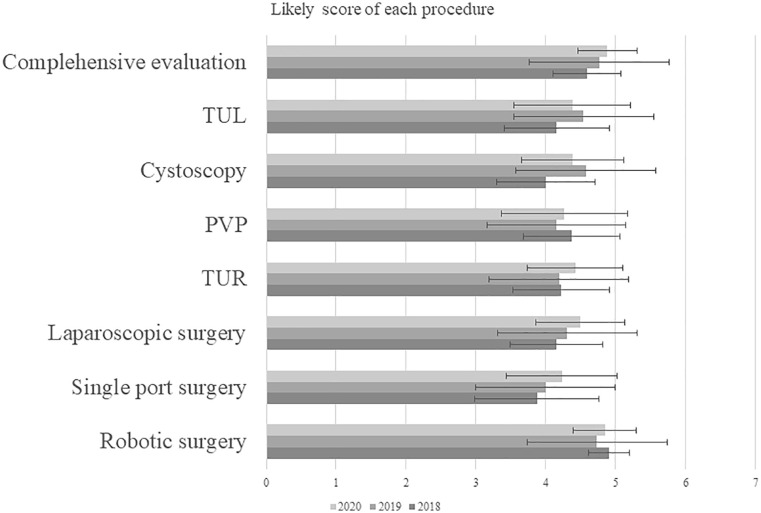
After training, robotic surgery was the most interesting to participants in both periods. Regarding laparoscopic suturing, single port surgery tended to have more of a “less likely” score than classical laparoscopic procedures. Endoscopic procedures, such as TUR, PVP simulation, cystoscopy, and TUL were also attractive to medical students. The comprehensive evaluation scores of this course in 2018, 2019, and 2020 were 4.59, 4.76, and 4.88, respectively (Figure 3)
Figure 3.
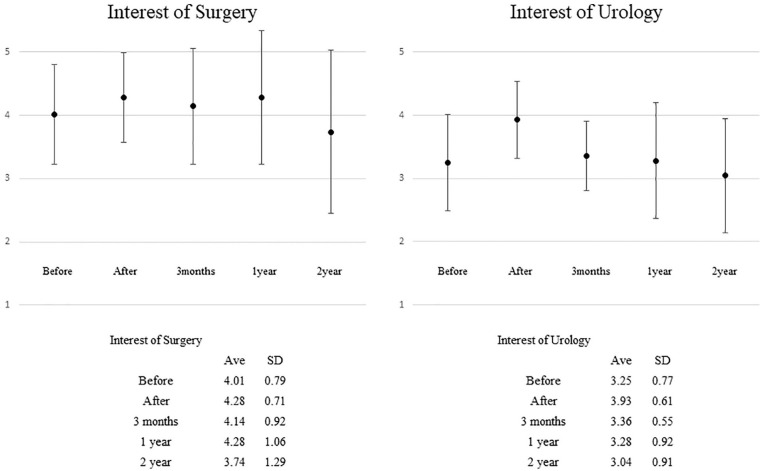
Likely scores of interest for surgery and urology before and after the course.
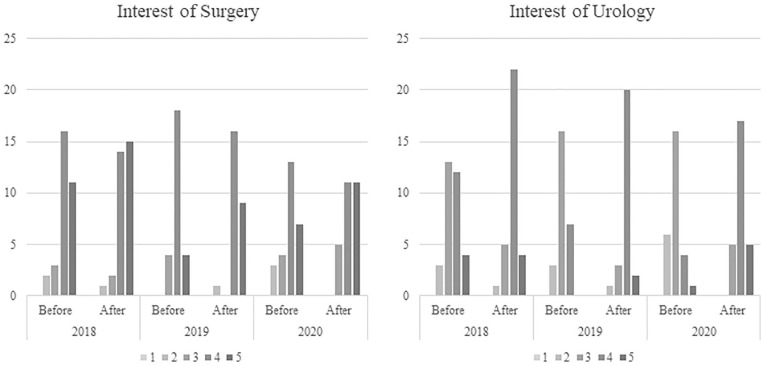
Table 2 shows the difference in likely scores before and after the course. After attending the course, the likely scores in surgery were higher, but this difference was not significantly different to what was obtained prior to the course each years (Effect size 0.27, small, P = 0.01). Interestingly, the scores for urology after the course were significantly increased compared to the pre-course scores (Effect size 0.60, large, P < 0.001). Particularly, the number of students who selected a score of 4 or 5 increased, and the number of students who selected a score of 2 or 3 decreased (Figure 4). Free description questionnaire results showed that medical students became more interested in urology and felt motivated for their clinical clerkship. Faculty members perceived teaching workload and cost as a burden. However, they felt that the course was very important for medical students in addition to clinical practice.
Table 2.
Likely scores of interest for surgery and urology before and after the course.
| Surgery |
Urology |
|||||||
|---|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | Total | 2018 | 2019 | 2020 | Total | |
| Average | ||||||||
| Before | 4.13 | 4.00 | 3.89 | 4.01 | 3.53 | 3.15 | 3.00 | 3.24 |
| After | 4.34 | 4.27 | 4.22 | 4.28 | 3.91 | 3.88 | 4.00 | 3.93 |
| Effect size | 0.18 | 0.35 | 0.33 | 0.27 | 0.35 | 0.72 | 0.77 | 0.60 |
| Mean difference | 0.22 | 0.27 | 0.33 | 0.27 | 0.38 | 0.73 | 1.00 | 0.68 |
| Standard deviation | 0.21 | 0.14 | 0.18 | 0.11 | 0.18 | 0.14 | 0.160 | 0.10 |
| Upper 95% | 0.65 | 0.56 | 0.71 | 0.48 | 0.74 | 1.02 | 1.330 | 0.88 |
| Lower 95% | −0.21 | −0.02 | −0.05 | 0.06 | 0.01 | 0.44 | 0.670 | 0.49 |
| P value | .30 | .07 | .08 | .01 | .04 | <.001 | <.001 | <.0001 |
Figure 4.
Likely scores in each course after the training.
To evaluate the long-term effect of this course, we performed a post-course web questionnaire, with 28(32.9%) after 3-months, 25(29.4%) after 1-year, and 23(27.1%) after 2-year students completing the questionnaire (Table 3). Regarding memory, “Remember the course” maintained very high scores of 4.46 ± 0.50, 4.36 ± 0.89, and 4.48 ± 0.58 at 3 months, 1 year, and 2 years after the course, respectively. Regarding the effect on motivation at clinical clerkship, this course played a significant role on the effect of learning both surgery and urology at just after the course. However, the scores obtained for interest and intention to choose a career in surgery and urology gradually decreased over time (Figure 5.). The average likely scores also decreased both in surgery and urology.
Table 3.
Long-term effect of this course.
| 3 months |
1 year |
2 years |
||||
|---|---|---|---|---|---|---|
| n = 28 (32.9%) |
n = 25 (29.4%) |
n = 23 (27.1%) |
||||
| Ave | SD | Ave | SD | Ave | SD | |
| Remembering | ||||||
| Whole course | 4.46 | 0.50 | 4.36 | 0.89 | 4.48 | 0.58 |
| Robotic surgery | 4.36 | 0.67 | 4.12 | 0.91 | 4.04 | 0.69 |
| Single port surgery | 3.79 | 0.98 | 3.32 | 1.05 | 3.26 | 0.85 |
| 3-D laparoscopy | 4.07 | 0.59 | 3.80 | 0.80 | 3.52 | 1.02 |
| Laparoscopic surgery | 4.11 | 0.86 | 4.28 | 0.60 | 3.74 | 0.74 |
| TUR | 2.96 | 0.82 | 3.40 | 1.02 | 3.13 | 1.03 |
| PVP | 3.36 | 0.97 | 3.44 | 0.98 | 3.04 | 0.95 |
| Cystoscopy | 3.11 | 0.98 | 3.32 | 0.93 | 3.22 | 0.93 |
| TUL | 3.07 | 0.96 | 3.32 | 0.97 | 3.04 | 0.91 |
| Interested in | ||||||
| Surgery | 4.14 | 1.06 | 4.28 | 0.92 | 3.74 | 1.29 |
| Urology | 3.36 | 0.55 | 3.28 | 0.92 | 3.04 | 0.91 |
| Affect the learning at clerkship | ||||||
| Surgery | 4.14 | 0.83 | 3.92 | 1.23 | 3.96 | 0.91 |
| Urology | 3.79 | 0.77 | 4.16 | 0.78 | 4.26 | 0.74 |
| Intention to choose a career | ||||||
| Surgery | 3.61 | 0.90 | 3.72 | 0.96 | 3.26 | 1.39 |
| Urology | 2.68 | 0.60 | 2.68 | 0.88 | 2.35 | 0.96 |
Abbreviations: ave, average; PVP, photo-selective vaporization of the prostate; SD, standard deviation; TUL, transurethral lithotripsy; TUR, transurethral resection.
Figure 5.
Time course of likely scores of interests for surgery and urology.
Discussion
According to this study, early exposure to urological hands-on training in pre-clinical clerkship students resulted in an increasing interest, especially in urology. Surgical training courses are generally conducted during clinical clerkship or postgraduate periods. 7 The most novel aspect of this study was conducting a hands-on course that focused on urological training in medical students prior to clinical clerkship.
Early exposure is an effective method of educating medical students in not only basic science but also clinical clerkship.8,9 This study showed that hands-on training in urological procedures impacted pre-clinical clerkship medical students as it increased their interest in urology. However, this course did not increase the interest in surgery of students who already had an interest in surgery prior to the course. Thus, it was of limited value to those who showed an interest prior to the course. In contrast, with regards to urology, this course made a good impression on students. Generally, there were more students interested in surgery than in urology. Moreover, what urologists do is relatively unknown to the public, even medical students, compared to what is done in surgery, internal medicine, pediatrics, and other specialties. Lesser-known specialties may be able to promote their specialty and showcase the roles they play to medical students in their earlier years of training. As medical students are rarely provided with experience in performing not only surgical procedures but also independent simulated surgeries prior to undergoing their clinical clerkship. However, for non-surgically minded medical students, this simulation course might have been more complex urological procedures. We would care about learners’ preliminary conditions to conduct the program a small portion of more core surgical procedure. This course could have a great impact on medical students prior to their clinical clerkship. To increase the numbers of urologically minded medical students, we should try to integrate the course into the wider curriculum.
As a systematic review and meta-analysis showed that technology-enhanced simulation was more effective than instructional methods, actual experience could be beneficial for learners. 10 In this course, students could perform surgical procedures and use simulators for a certain amount of time under the supervision of several faculty members. Regarding endourologic skills, early feedback can be beneficial when learning through novel simulation training. 11 Concerning acquisition of surgical skills, it is not enough to teach procedures using a one-day hands-on training. However, this experience may encourage students to learn surgery and urology further after their clinical clerkship. Motivation was found to be one of the most important factors for continuing learning in the field of medical education. 12 Of course, a 1-day course is not enough to stay motivated in surgery and urology. We revealed that their interest of urology decreased with time. It was thought to be causally related to some possibilities. For example, their urological interest was just only temporary, they forgot urology as clinical clerkship progressed, they got other interest rather than urology, and so on. To maintain and improve the effect of the course, we should continue offering students the opportunity to obtain surgical experience and should hold other courses that are related to their specialty, using technical and educational approaches, such as the motivational dynamic model. 12
In Japan, medical students finally decide their specialty during a 2-year primary residency course followed by a 4-year specialized medical course. 13 For medical undergraduates, exposure to specialties and the timing of this exposure are crucial to career choice; this is true for any specialty. 14 As there are several reports that show that early exposure to surgical subspecialties could influence students to pursue a career.15-18 In contrast, early surgical exposure increased their understanding and interests; although, it did not affect their surgical career choices.18,19 This study showed that participants got interested in urology while it did not seem to lead to choosing surgery or urology as a career. Increasing the number of surgeons might require continuous efforts using other strategies.
Regarding urology, only a limited number of medical schools require a formal educational rotation in urological surgery; thus, medical students perceive their knowledge of urology as poor even when they are aware of urology as a specialty. 20 A survey targeting program directors in the US showed that 32% of medical schools had no urology faculty lectures in the preclinical years. 21 In Canada, only 24.3% of students had a selective urology clerkship rotation. 22 Unfortunately, medical students had less chance to have urological clerkship because very few medical colleges have mandatory urological clerkship worldwide.22,23 Actually, about 60% of medical students felt they had received good clinical exposure to urology in UK. 24 Generally, medical students have less opportunity to expose urology. In contrast, clinical performance during a rotation in medical school is the most important factor taken into account when choosing future urology residents. 25 A report showed that third-year medical students were more likely to consider urology than final-year students due to multifactorial reasons. 26 Accordingly, this early exposure course, provided during the fourth-year could be an initiation to a urological interest for medical students prior to clinical clerkship.
This study has some limitations. First, the number of students was small because this course was conducted by a single urology department at a medical school. Second, we only evaluated the change in likely scores before and after the course, and we did not compare this to a control group. Third, as students had not yet graduated and selected their specialty, their real career paths could not be evaluated, Further, long-term observations are required to confirm whether the course triggers students to learn and achieve higher level of skills in urology. However, such an early exposure course could be used by other departments to encourage students to learn or take up their specialties.
Conclusions
Urological hands-on training encouraged interest in urology among medical students prior to their clinical clerkship. Early experience in actual surgical techniques could motivate students to learn about surgical specialties during their clinical clerkship.
Acknowledgments
We would like to thank Editage (www.editage.com) for editing and reviewing this manuscript for English language.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author contributions: T.Ki. processed the experimental data, performed the analysis, drafted the manuscript and designed the figures. K.K, M.S., I.C., A.I., S.K.,T.Ko,and H.N. helped carry out the simulation program. J.H. were involved in planning and supervised the work, T.Ko. and H.N. aided in interpreting the results and worked on the manuscript. All authors discussed the results and commented on the manuscript.
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate: This study was approved by the Ethics Committee at University of Tsukuba (approval number 19-1394). The study participants provided written informed consent.
ORCID iDs: Tomokazu Kimura  https://orcid.org/0000-0003-1201-1260
https://orcid.org/0000-0003-1201-1260
Shuya Kandori  https://orcid.org/0000-0003-4621-8470
https://orcid.org/0000-0003-4621-8470
References
- 1. Zinski A, Blackwell KTCPW, Belue FM, Brooks WS. Is lecture dead? A preliminary study of medical students’ evaluation of teaching methods in the preclinical curriculum. Int J Med Educ. 2017;8:326-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Onishi H. History of Japanese medical education. Korean J Med Educ. 2018;30:283-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Densen P. Challenges and opportunities facing medical education. Trans Am Climatol Assoc. 2011;122:48-58. [PMC free article] [PubMed] [Google Scholar]
- 4. Arai H, Ouchi Y, Toba K, et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr Gerontol Int. 2015;15:673-687. [DOI] [PubMed] [Google Scholar]
- 5. Model Core Curriculum for Medical Education in Japan AY 2016. Revision Medical Education Model Core Curriculum Coordination Committee Medical Education Model Core Curriculum Expert Research Committee.
- 6. McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003-2009. Med Educ. 2010;44:50-63. [DOI] [PubMed] [Google Scholar]
- 7. Glass CC, Acton RD, Blair PG, et al. American College of Surgeons/Association for Surgical Education medical student simulation-based surgical skills curriculum needs assessment. Am J Surg. 2014;207:165-169. [DOI] [PubMed] [Google Scholar]
- 8. Tang KP, Chen CY, Wu MS, Chen TT, Wu BW, Tsai PF. Correlation between early clinical exposure environment, attitudes toward basic medicine, and medical students’ basic science learning performance. BMC Med Educ. 2019;19:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dornan T, Bundy C. What can experience add to early medical education? Consensus survey. BMJ. 2004;329:834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cook DA, Brydges R, Hamstra SJ, et al. Comparative effectiveness of technology-enhanced simulation versus other instructional methods: a systematic review and meta-analysis. Simul Healthc. 2012;7:308-320. [DOI] [PubMed] [Google Scholar]
- 11. Lee JY, McDougall EM, Lineberry M, Tekian A. Optimizing the timing of expert feedback during simulation-based spaced practice of endourologic skills. Simul Healthc. 2016;11:257-263 [DOI] [PubMed] [Google Scholar]
- 12. Pelaccia T, Viau R. Motivation in medical education. Med Teach. 2017;39:136-140. [DOI] [PubMed] [Google Scholar]
- 13. Nomura K, Yano E, Aoki M, Kawaminami K, Endo H, Fukui T. Improvement of residents’ clinical competency after the introduction of new postgraduate medical education program in Japan. Med Teach. 2008;30:e161-e169. [DOI] [PubMed] [Google Scholar]
- 14. Pianosi K, Bethune C, Hurley KF. Medical student career choice: a qualitative study of fourth-year medical students at Memorial University, Newfoundland. CMAJ Open. 2016;4:E147-E152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Head LK, Greene B, Gawad N, Hamstra SJ, Brandys T. Harvesting the ‘SEAD’: long-term follow-up of the surgical exploration and discovery program. J Surg Educ. 2020;77:96-103. [DOI] [PubMed] [Google Scholar]
- 16. Ramaswamy RS, Fung D, Tiwari T, et al. Factors influencing selection of an interventional radiology training program. Clin Imaging. 2019;57:30-34. [DOI] [PubMed] [Google Scholar]
- 17. Coyan GN, D’Angelo MP, Kilic A, et al. Evaluation of a simulation-based mini-elective on medical student interest in cardiac surgery. J Card Surg. 2019;34:901-907. [DOI] [PubMed] [Google Scholar]
- 18. Hicks KE, Doubova M, Winter RM, Seabrook C, Brandys T. Surgical exploration and discovery program: early exposure to surgical subspecialties and its influence on student perceptions of a surgical career. J Surg Educ. 2019;76:1248-1257. [DOI] [PubMed] [Google Scholar]
- 19. Zuccato JA, Kulkarni A. The impact of early medical school surgical exposure on interest in neurosurgery. Can J Neurol Sci. 2016;43:410-416. [DOI] [PubMed] [Google Scholar]
- 20. Whiles BB, Thompson JA, Griebling TL, Thurmon KL. Perception, knowledge, and interest of urologic surgery: a medical student survey. BMC Med Educ. 2019;19:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Loughlin KR. The current status of medical student urological education in the United States. J Urol. 2008;179:1087-1090. [DOI] [PubMed] [Google Scholar]
- 22. Domes T, Vellani S, Couture F, Bhojani N, Andonian S, Ismail S, Rourke KF, MacLellan D. The current landscape of urological undergraduate education in Canada. Can Urol Assoc J. 2020;14:E549-E554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Slaughenhoupt B, Ogunyemi O, Giannopoulos M, Sauder C, Leverson G. An update on the current status of medical student urology education in the United States. Urology. 2014;84:743-747. [DOI] [PubMed] [Google Scholar]
- 24. Jones P, Rai BP, Qazi HA, Somani BK, Nabi G. Perception, career choice and self-efficacy of UK medical students and junior doctors in urology. Can Urol Assoc J. 2015;9:E573-E578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nguyen DD, Lee JY, Domes T, et al. Survey of Canadian urology programs: which aspects of the Canadian Residency Matching Service (CaRMS) application are the most important? Can Urol Assoc J. 2020;14:169-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jayakumar N, Ahmed K, Challacombe B. Factors affecting UK medical students’ decision to train in urology: a national survey. Minerva Urol Nefrol. 2016;68:409-416. [PubMed] [Google Scholar]