Abstract
The authors examined trends in systolic blood pressure (SBP) and diastolic blood pressure (DBP) and the prevalence, awareness, treatment, and control of hypertension in 1988–1994 (n=1164), 1999–2004 (n=1,026), and 2005–2010 (n=1048) among US adults 80 years and older in serial National Health and Nutrition Examination Surveys. Hypertension was defined as SBP ≥140 mm Hg, DBP ≥90 mm Hg, or use of antihypertensive medication. Awareness and treatment were defined by self‐report and control as SBP/DBP<140/90 mm Hg. Mean SBP decreased from 147.3 mm Hg to 140.1 mm Hg and mean DBP from 70.2 mm Hg to 59.4 mm Hg between 1988–1994 and 2005–2010. The prevalence, awareness, and treatment of hypertension each increased over time. Controlled hypertension increased from 30.4% in 1988–1994 to 53.1% in 2005–2010. The proportion of patients taking 3 classes of antihypertensive medication increased from 7.0% to 30.9% between 1988–1994 and 2005–2010. Increases in awareness, treatment, and control of hypertension and antihypertensive polypharmacy have been observed among very old US adults.
The US population is aging and it is projected that the number of US adults 80 years and older will triple by 2050.1 Hypertension is one of the most important risk factors for coronary heart disease, stroke, and heart failure, each of which has a high incidence in the very old patients.2, 3, 4 A meta‐analysis of randomized trials that included participants 80 years and older found antihypertensive treatment to be associated with a reduced risk for stroke, cardiovascular events, and heart failure.5
Multi‐morbidity and functional impairment are common among the very old and the applicability of antihypertensive treatment trial results to this population has been questioned.6, 7, 8, 9 A major concern in using antihypertensive medications in the very old is the potential increased risk for adverse events including falls and myocardial infarction associated with low blood pressure (BP).10, 11, 12 Providers must often weigh potential cardiovascular benefits against the perceived risks of pharmacologic BP‐lowering among the very old. For these reasons, treatment patterns may be different for the very old vs the general US population.
Given the anticipated growth of the very old population in the United States, there is a need to document the prevalence of hypertension and BP treatment patterns in this population. Such information could be used to guide the development and implementation of approaches for improving BP management in this group. Therefore, we examined secular changes in SBP and DBP and hypertension prevalence, awareness, treatment, and control from 1988–1994 through 2005–2010 among representative samples of US adults aged 80 and older. In addition, we examined trends in the use of different classes of antihypertensive medications and the prevalence of antihypertensive polypharmacy among very old US adults.
Methods
Study Population
Serial National Health and Nutrition Examination Survey (NHANES) cycles from 1988–1994,1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, and 2009–2010 were analyzed for the current study. NHANES is conducted by the National Center for Health Statistics (NCHS) and utilizes a multistage stratified probability sampling approach to identify potential participants. Additional information on the design and conduct of NHANES is available online.13 The current analysis was limited to participants who were 80 years and older and completed a medical evaluation at the NHANES mobile examination center (n=3558). We excluded individuals who did not have 3 SBP and DBP measurements taken during their NHANES medical evaluation (n=228), did not answer questions about awareness and treatment of high BP (n=30), or were missing information on prescription medications (n=62). After these exclusion criteria were applied, data from 3238 participants were included in the analyses. As described online, multiple NHANES cycles can be pooled to provide stable prevalence estimates.14 To achieve stable estimates, we grouped participants into 3 time periods: 1988–1994 (n=1164), 1999–2004 (n=1026), and 2005–2010 (n=1048) for the current analyses. The protocol for NHANES was approved by the NCHS institutional review board and all participants provided written informed consent.
Data Collection
Data for each NHANES cycle were collected through participant interviews and a medical evaluation. Of relevance to the current analysis, variables collected during the interview included age, race/ethnicity, sex, smoking status, history of hypertension, use of antihypertensive medication, history of myocardial infarction or stroke, and impairment in activities of daily living (ADLs). Although there was no upper age limit to participate in NHANES, the publicly available NHANES datasets provided exact age for participants 90 years and younger in NHANES 1988–1994, 85 years and younger for NHANES 1999–2006, and 80 years and younger for NHANES 2007–2010. Above these cutpoints, exact age was not available. Therefore, we do not report age in the current analyses. ADLs include basic self‐care tasks that are necessary for independent living such as walking, eating, and dressing. ADL impairment was defined as answering “some difficulty,” “much difficulty,” or “unable to do” to ≥1 of the following questions “how much difficulty do you have walking from room to room,” “getting in or out of bed,” “eating,” or “dressing.”
The NHANES medical evaluation included anthropometrics and BP measurements, collection of blood and random spot urine samples, and a pill bottle review. Height, weight, and waist circumference were measured during the medical evaluation and were used to calculate body mass index (BMI). Serum glucose and serum creatinine were measured from the blood sample. Diabetes mellitus was defined by a prior diagnosis, excluding during pregnancy, with concurrent use of insulin or oral hypoglycemic medication, or fasting glucose ≥126 mg/dL or non‐fasting glucose ≥200 mg/dL. Estimated glomerular filtration rate (eGFR) was calculated using serum creatinine, recalibrated per NHANES recommendations, and the Chronic Kidney Disease Epidemiology Collaboration (CKD‐EPI) equation.15, 16 Using random spot urine samples, albumin and creatinine were measured. Albuminuria was defined as a urinary albumin‐to‐creatinine ratio ≥30 mg/g.
BP Measurement
BP was measured by a trained physician using a mercury sphygmomanometer and an appropriately sized cuff. Quality control for the BP measurement included quarterly re‐certification with retraining if necessary, annual retraining of all physicians, and monitoring of equipment and equipment repair. BP certification consisted of video test recognition of Korotkoff sounds and measurement performance on live volunteers. Additional details of the BP measurements are available online.17 Cuff sizes were selected after measurement of participants' mid‐arm circumference. Readings were obtained after 5 minutes of seated rest. Three BP measurements were obtained, at 1‐minute intervals, during the medical evaluation. As mentioned above, our analysis was restricted to participants with 3 SBP and DBP measurements and we used the mean of these measurements to define SBP and DBP.
Hypertension Prevalence, Awareness, Treatment, and Control
Hypertension was defined as SBP ≥140 mmHg and/or DBP ≥90 mm Hg, and/or self‐reported use of antihypertensive medication. Awareness of hypertension was defined as self‐report of a prior diagnosis of hypertension by a health care professional. Treatment of hypertension was defined as self‐reported use of prescription antihypertensive medication among persons reporting a prior diagnosis of hypertension. Controlled hypertension was defined as SBP/DBP <140/90 mm Hg. Isolated systolic hypertension (ISH) was defined as SBP ≥140 mm Hg and DBP <90 mm Hg. Systolic diastolic hypertension (SDH) was defined as SBP ≥140 mm Hg and DBP ≥90 mm Hg. There were too few participants 80 years and older with isolated diastolic hypertension (IDH, SBP <140 mm Hg and DBP ≥90 mm Hg) to evaluate secular changes in its prevalence.
Pill Bottle Review
Participants were asked to bring all prescription medications taken in the prior 2 weeks to the NHANES medical evaluation. Pill bottles were reviewed and medication names were recorded and coded into drug classes based on their generic equivalents. Antihypertensive medication classes included angiotensin‐converting enzyme (ACE) inhibitors, α‐blockers, aldosterone receptor blockers, angiotensin receptor blockers (ARBs), β‐blockers, calcium channel blockers (CCB), central‐acting agents, diuretics, renin inhibitors, and direct vasodilators. Single‐pill combinations were classified into their component classes. Medication dosage information was not recorded.
Statistical Analysis
Participant characteristics and mean SBP and DBP were calculated for each time period (1988–1994, 1999–2004, and 2005–2010). The prevalence of hypertension, ISH, and SDH was calculated by time period. Next, the prevalence of hypertension awareness, treatment, and control was calculated. Hypertension awareness was calculated for patients with hypertension, treatment was calculated among all participants with hypertension and separately among those aware of their diagnosis, and control was calculated among all participants with hypertension and separately among those receiving treatment for their hypertension. The number of antihypertensive medication classes being taken and the distribution of classes of antihypertensive medications being taken were calculated by time period. Because prior data show that potential differences in the BP‐mortality association by frailty status may exist among the very old, we repeated this analysis separately for participants with and without ADL impairment.18 There are few data on the benefits of achieving SBP/DBP <140/90 mm Hg in patients 80 years and older. Therefore, we calculated the percentage of the population with SBP <140 mm Hg, SBP <150 mm Hg, and SBP <160 mm Hg and, separately, DBP <90 mm Hg and DBP <100 mm Hg for each time period. Additionally, to assess the potential overtreatment of individuals, we assessed the percentage with SBP <120 mm Hg and <130 mm Hg and the percentage with DBP <60 mm Hg, <70 mm Hg, and <80 mm Hg. Linear trends over time were calculated using least squares or maximum likelihood as appropriate.
All analyses were performed using SUDAAN 10.1 (Research Triangle Institute, Research Triangle Park, NC) accounting for the complex sampling design of NHANES. Sampling weights, recalibrated based on the proportion of participants missing data by sex and race‐ethnicity, were applied to all calculations to obtain US nationally representative prevalence estimates. Recalibration of the sampling weights corrects for differences in missing data across sex and race‐ethnicity strata and assumes that data within strata are missing randomly.19
Results
The proportion of participants 80 years and older who were women and non‐Hispanic white or black was similar over time (Table 1). The proportion who were Hispanic or had diabetes mellitus or an eGFR <60 mL/min/1.73 m2 increased, while current smoking decreased over time. Mean BMI and waist circumference increased from 1988–1994 through 2005–2010.
Table 1.
Characteristics of US Adults 80 Years and Older in 1988–1994, 1999–2004, and 2005–2010
| Time Period | P Value | |||
|---|---|---|---|---|
| 1988–1994 (n=1164) | 1999–2004 (n=1026) | 2005–2010 (n=1048) | ||
| Women | 65.3 | 64.3 | 63.1 | .57 |
| Race/ethnicity | ||||
| Non‐Hispanic white | 88.2 | 86.0 | 86.5 | .53 |
| Non‐Hispanic black | 7.1 | 6.5 | 6.1 | .80 |
| Hispanic | 1.5 | 5.5 | 4.2 | <.001 |
| Other | 3.2 | 2.0 | 3.2 | .34 |
| Current smoker | 5.7 | 3.8 | 2.8 | .02 |
| Body mass index, kg/m2 | 25.3 (0.15) | 26.2 (0.21) | 26.8 (0.15) | <.001 |
| Waist circumference, cm | 93.8 (0.37) | 95.7 (0.41) | 97.0 (0.46) | <.001 |
| Diabetes mellitus | 11.9 | 14.2 | 16.0 | .03 |
| C‐reactive protein >3 mg/L | 2.2 | 2.1 | 1.8 | .78 |
| eGFR <60 mL/min/1.73 m2 | 40.4 | 51.9 | 51.0 | <.001 |
| Albuminuria | 30.4 | 30.8 | 30.1 | .96 |
| History of MI | 14.2 | 13.8 | 14.1 | .98 |
| History of stroke | 11.4 | 11.5 | 14.2 | .33 |
| ADL impairment | 31.1 | 33.1 | 31.3 | .64 |
Abbreviations: ADL, activities of daily living; eGFR, estimated glomerular filtration rate; MI, myocardial infarction. Age is not reported as exact age for participants older than 80 years is not available in the public‐use National Health and Nutrition Examination Survey data set. Numbers are expressed as percentage or mean (standard error).
Among US adults 80 years and older, mean SBP was 147.3 mm Hg (95% confidence interval [CI], 145.4–149.2 mm Hg) in 1988–1994, 148.2 mm Hg (95% CI, 146.5–149.9 mm Hg) in 1999–2004, and 140.1 mmHg (95% CI, 138.6–141.6 mm Hg) in 2005–2010 (P<.001). Mean DBP decreased from 70.2 mm Hg (95% CI, 69.1–71.3 mm Hg) in 1988–1994 to 61.1 mm Hg (95% CI, 59.4–62.8 mm Hg) in 1999 to 2004 and was 59.4 mm Hg (95% CI, 58.4–60.4 mm Hg) in 2005 to 2010 (P<.001). Mean pulse pressure increased from 77.2 mm Hg (95% CI, 75.3–79.1 mm Hg) in 1988–1994 to 87.1 mm Hg (95% CI, 84.4–89.8 mm Hg) in 1999–2004 and decreased to 80.7 mm Hg (95% CI, 79.1–82.4 mm Hg) in 2005–2010. The prevalence of hypertension increased from 69.2% in 1988–1994 to 76.5% in 1999–2004 and remained 76.5% in 2005–2010 (Figure 1). The prevalence of ISH was 52.8% and 55.3% in 1988–1994 and 1999–2004, respectively, and declined to 43.9% in 2005–2010. The prevalence of SDH decreased progressively over the 3 time periods. Among those with hypertension, awareness and treatment increased over time (Figure 2). Treatment among those aware of their hypertension increased from 1988–1994 through 2005–2010. Among all participants with hypertension and those receiving treatment for their hypertension, BP control increased over the 3 time periods.
Figure 1.
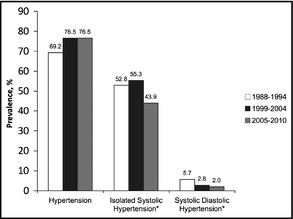
Prevalence of hypertension, isolated systolic hypertension, and systolic‐diastolic hypertension among US adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010. Hypertension: Systolic blood pressure >140 mm Hg and/or diastolic blood pressure >90 mm Hg, and/or self‐reported use of antihypertensive medication. Isolated Systolic Hypertension: Systolic blood pressure >140 mm Hg and diastolic blood pressure <90 mm Hg. Systolic Diastolic Hypertension: Systolic blood pressure >140 mm Hg and diastolic blood pressure >90 mm Hg. Note: Too few participants had isolated diastolic hypertension (systolic blood pressure <140 mm Hg and diastolic blood pressure >90 mm Hg) to produce stable prevalence estimates. *Among those with hypertension.
Figure 2.
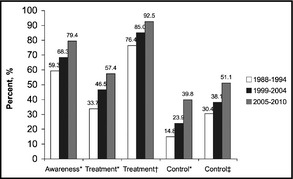
Prevalence of awareness, treatment, and control among adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010. Awareness: self‐report of a prior diagnosis of hypertension by a health care professional. Treatment: self‐reported use of prescription antihypertensive medication. Control: Systolic blood pressure/Diastolic blood pressure <140/90 mm Hg. *Among those with hypertension; †Among those aware of their diagnosis of hypertension; ‡Among those treated for their hypertension.
The mean number of antihypertensive medication classes being taken and the percentage of those with hypertension taking ≥3 classes of antihypertensive medication increased from 1988–2004 to 2005–2010, while the percentage of the hypertensive population taking 0 or 1 classes of antihypertensive medication decreased over time (Table 2). The use of ACE inhibitors, aldosterone receptor blockers, α‐blockers, ARBs, β‐blockers, and CCBs increased significantly over time. Use of central‐acting agents and direct vasodilators decreased over time. The percentage of those taking diuretics did not change over time (P=.29). Trends in mean SBP and DBP and use of antihypertensive medication over time were similar for individuals with and without impairments in ADLs (Supplemental Table 1).
Table 2.
Number of Antihypertensive Medication Classes Being Taken and Percentage of the Population Taking Each Antihypertensive Medication Class for US Adults 80 Years and Older With Hypertension in 1988–1994, 1999–2004, and 2005–2010
| Time Period | P Value | |||
|---|---|---|---|---|
| 1988–1994 (n=798) | 1999–2004 (n=769) | 2005–2010 (n=781) | ||
| Antihypertensive medication classes, mean (standard error) | 1.0 (0.05) | 1.5 (0.06) | 1.9 (0.04) | <.001 |
| Agents taking, % | ||||
| 0 classes | 36.4 | 26.2 | 15.0 | <.001 |
| 1 classes | 33.3 | 26.0 | 26.2 | .01 |
| 2 classes | 23.4 | 28.5 | 27.9 | .11 |
| 3 classes | 7.0 | 19.2 | 30.9 | <.001 |
| Specific classes, % | ||||
| Angiotensin‐converting enzyme inhibitors | 11.3 | 23.4 | 31.3 | <.001 |
| Angiotensin receptor blockers | 0.0 | 11.4 | 21.3 | <.001 |
| Aldosterone receptor blockers | 0.8 | 1.2 | 3.8 | .01 |
| α‐Blockers | 3.5 | 6.0 | 9.7 | <.001 |
| β‐Blockers | 12.7 | 25.6 | 43.1 | <.001 |
| Calcium channel blockers | 22.0 | 29.2 | 28.7 | .03 |
| Central‐acting agents | 5.1 | 2.0 | 2.4 | .01 |
| Diuretics | 39.0 | 43.1 | 42.7 | .29 |
| Renin inhibitors | 0.0 | 0.0 | 0.2 | .20 |
| Direct vasodilators | 7.9 | 3.6 | 3.5 | .01 |
There were 4.21, 5.74, and 7.27 million US adults 80 years and older with hypertension in 1988–1994, 1999–2004, and 2005–2010, respectively (Supplemental Table 2). The number of US adults aged 80 years and older with controlled BP increased progressively over the 3 time periods with 0.62, 1.37, and 2.89 million US adults aged 80 years and older having controlled BP in 1988–1994, 1999–2004, and 2005–2010, respectively.
Achievement of Alternate SBP and DBP Goals
The percentage of US adults aged 80 years and older with SBP <140 mm Hg increased from 41.5% in 1988–1994 to 41.9% and 54.1% in 1999–2004 and 2005–2010, respectively (Supplemental Table 3). Also, the percentage of patients with SBP <120 mm Hg was12.5% in 1988–1994, 11.9% in 1999–2004, and 19.0% in 2005–2010. The percentage of US adults 80 years and older with DBP <90 mm Hg increased over time (93.9%, 97.2%, and 97.9% in 1988–1994, 1999–2004, and 2005–2010, respectively) and ≥99% of the population had DBP <100 mm Hg in each time period. Additionally, the percentage of patients with DBP <60 mm Hg increased from 15.5% to 48.9% between 1988–1994 and 2005–2010.
Discussion
Using serial national cross‐sectional samples of US adults 80 years and older, the current analysis indicates that the prevalence of hypertension has increased modestly among the very old over the past 20 years and that 76.5% of US adults 80 years and older had hypertension in 2005–2010. The increase in the prevalence of hypertension observed in the current study appears to be the result of increased use of antihypertensive medication; awareness, treatment, and control of hypertension increased over time among US adults 80 years and older at the same time that mean SBP and DBP declined in this age group. Among patients with hypertension, the mean number of antihypertensive medication classes being taken doubled between 1988–1994 and 2005–2010. Additionally, the proportion of US adults 80 years and older taking ≥3 classes of antihypertensive medications increased from 7.0% to 30.9%. The prevalence of ISH and SDH decreased between 1988–1994 and 2005–2010. Since it is one of the more prevalent forms of uncontrolled hypertension, the decline in the prevalence of ISH also highlights the increase in controlled hypertension.
Previous analyses have reported a high prevalence of hypertension among US adults 60 years and older and that the prevalence has increased over time.20, 21, 22, 23, 24, 25 Prior NHANES analyses also indicate that awareness, treatment, and control of hypertension have increased over the past 20 years among US adults 20–39, 40–59, and 60 years and older.20, 21, 22, 23, 24 However, data for participants 80 years and older were not reported. An analysis of the Framingham Heart Study's original and offspring cohort data from the 1990s examined the prevalence, treatment, and control of hypertension by age.26 In this study, 74% of participants 80 years and older had hypertension. Of those with hypertension, 74.2% were treated and <50% of those treated had an SBP/DBP <140/90 mm Hg. Our study extends these findings to a nationally representative sample of US adults 80 years and older in a more contemporary era and documents increasing awareness and treatment of hypertension and substantial reductions in SBP and DBP among US adults over the past 20 years.
In the current analysis, mean DBP decreased from 70.2 mm Hg in 1988–1994 to 59.5 mm Hg in 2005–2010. In addition, the prevalence of US adults 80 years and older with DBP <60 mm Hg increased from 15.5% to 48.9% between 1988–1994 and 2005–2010. Low DBP has been associated with an increased risk of stroke and cardiovascular disease among patients with ISH and has been shown to have a J‐shaped association with mortality among the elderly.11, 27 Among those with coronary heart disease, there is an increased risk of all‐cause mortality and myocardial infarction with low DBP.10 Despite the improvements in BP control documented in the current study, aggressive treatment of hypertension comes with its share of potential risks including those associated with excessively low DBP.
The Hypertension in the Very Elderly Trial (HYVET) randomized individuals 80 years and older with sustained SBP ≥160 mm Hg to active treatment (with indapamide and if needed perindopril) with a target SBP/DBP <150/80 mm Hg or placebo in order to evaluate the benefits and risks of antihypertensive treatment in patients 80 years and older.28 In HYVET, active treatment was associated with a 30% reduction in the risk of stroke, 21% reduction in death from any‐cause, 39% reduction in fatal stroke, and a 64% reduction in heart failure.28 Following publication of HYVET, a meta‐analysis of 8 randomized controlled trials comparing antihypertensive treatment to placebo or usual care (ie, no treatment), including HYVET, was conducted to assess outcomes associated with treatment of hypertension among adults 80 years and older.5 This analysis found that antihypertensive medication reduces the risk for stroke, cardiovascular events, and heart failure.5 In contrast to HYVET, data from the analysis did not support a mortality risk reduction with antihypertensive medication in the very old. Additionally, the meta‐analysis suggested that the reduction in mortality was achieved in trials with the lowest intensity of therapy; therefore, the authors concluded that maximal antihypertensive therapy should be limited to 2 drugs in low doses.5 Contrary to this recommendation, the current analysis found a 4‐fold increase in the proportion of the very old taking ≥3 classes of antihypertensive medication.
Despite the benefits of antihypertensive therapy demonstrated in these trials, BP treatment goals for the very old remain controversial. A 2011 American College of Cardiology Foundation/American Heart Association Consensus Document on Hypertension in the Elderly recommended an SBP/DBP treatment goal of <140/90 mm Hg; however, for patients 80 years and older with SBP >150 mm Hg, a goal SBP of 140 to 145 mm Hg was considered acceptable.29 The task force acknowledged this goal to be based on expert opinion rather than clinical trial evidence. Recently, the 2013 European Society of Hypertension/European Society of Cardiology on the management of arterial hypertension recommended that elderly hypertensive patients with an SBP ≥160 mm Hg be treated to an SBP of 140 to 150 mm Hg.30 No BP goal was specified for frail elderly individuals, with treatment decisions left to the discretion of the treating physician based on the patient's response to treatment.30
Given the increasing use of antihypertensive medication and antihypertensive polypharmacy and high prevalence of impaired ADLs in the very old, data are needed to evaluate the benefit and potential harm of aggressive antihypertensive treatment among the very old with hypertension.31, 32 Aggressively lowering DBP has been shown to be associated with an increased risk for all‐cause mortality and myocardial infarction in hypertensive patients with coronary heart disease.10, 27 In addition, falls are common among the very old and the use of antihypertensive medication has been shown to be associated with an increased risk of falling.33, 34 To further evaluate the benefits and harms of antihypertensive treatment among the very old, in 2010 the US National Institutes of Health launched the Systolic Blood Pressure Intervention Trial (SPRINT), which is designed to determine whether maintaining SBP/DBP <120/80 mm Hg vs <140/90 mm Hg will further reduce the risk of cardiovascular and kidney disease, as well as age‐related cognitive decline in adults 55 years and older.35 Age 75 years and older is an a priori–defined subgroup in SPRINT. SPRINT may help identify the optimal SBP/DBP goal for the very old with hypertension.
Study Limitations
The findings from this study should be interpreted in the context of several limitations. Enrollment in NHANES is restricted to noninstitutionalized US adults, and individuals residing in nursing homes were not included. Due to the cross‐sectional nature of NHANES data, information on outcomes is not available. Exact age is not available for participants 80 years and older in all of the NHANES cycles included in our analyses. Therefore, we were unable to report changes in the age distribution for our study population over time. BP was obtained during a single visit and may not capture participants' long‐term mean levels. Data on the indications for taking the different antihypertensive medication classes were not available. Therefore, some antihypertensive classes being taken by participants may have been prescribed for a primary reason other than BP reduction. Finally, NHANES data are available only through 2010. HYVET, which was published in 2008, may have had substantial influence on antihypertensive medication use and SBP/DBP goal attainment among the very old. However, we did not have sufficient data following the publication of HYVET to assess its impact.
Conclusions
Based on national surveys of US adults aged 80 years and older from 1988 through 2010, there have been marked increases in the awareness, treatment, and control of hypertension. In addition, the prevalence of ISH and SDH decreased over time, which reflects better BP control. Hypertension polypharmacy has increased among the very old, with most hypertensive adults 80 years and older taking ≥2 classes of antihypertensive medication. Given the substantial increase in antihypertensive medication use over the past 2 decades and lack of data on the benefits and risks of aggressive BP‐lowering among the very old, studies are needed to determine the optimal treatment approach and SBP and DBP goals for this age group.
Supporting information
Table S1. Mean blood pressure and prevalence of hypertension among US adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010 for people without (top panel) and with (bottom panel) impairments in activities of daily living.
Table S2. Number of US adults 80 years and older with hypertension in 1988–1994, 1999–2004, and 2005–2010.
Table S3. Prevalence of systolic blood pressure <120 mm Hg, <130 mm Hg, <140 mm Hg, <150 mm Hg, and <160 mm Hg and diastolic blood pressure <60 mm Hg, <70 mm Hg, <80 mm Hg, <90 mm Hg, and <100 mm Hg among US adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010.
J Clin Hypertens(Greenwich). 2014; 270–276. DOI: 10.1111/jch.12281. © 2014 Wiley Periodicals, Inc.
References
- 1. Vincent GK, Velkoff VA. The Next Four Decades – The Older Population in the United States: 2010 to 2050. 2010. http://www.census.gov/prod/2010pubs/p25-1138.pdf. Accessed May 15, 2013.
- 2. MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. [DOI] [PubMed] [Google Scholar]
- 3. He J, Whelton PK. Elevated systolic blood pressure as a risk factor for cardiovascular and renal disease. J Hypertens Suppl. 1999;17:S7–S13. [PubMed] [Google Scholar]
- 4. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 5. Bejan‐Angoulvant T, Saadatian‐Elahi M, Wright JM, et al. Treatment of hypertension in patients 80 years and older: the lower the better? A meta‐analysis of randomized controlled trials J Hypertens. 2010;28:1366–1372. [DOI] [PubMed] [Google Scholar]
- 6. Abramov D, Cheng H. Controversy in treating the oldest old with hypertension: is the hypertension in the very elderly trial the final answer? J Am Geriatr Soc. 2009;57:570–571. [DOI] [PubMed] [Google Scholar]
- 7. Yoshikawa TT. Future direction of geriatrics: “gerogeriatrics.” J Am Geriatr Soc. 2012;60:632–634. [DOI] [PubMed] [Google Scholar]
- 8. Larson EB. Evidence, guidelines, performance incentives, complexity, and old people: a clinician's dilemma. J Am Geriatr Soc. 2009;57:353–354. [DOI] [PubMed] [Google Scholar]
- 9. Molander L, Lövheim H, Norman T, et al. Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc. 2008;56:1853–1859. [DOI] [PubMed] [Google Scholar]
- 10. Messerli FH, Mancia G, Conti CR, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006;144:884–893. [DOI] [PubMed] [Google Scholar]
- 11. Somes GW, Pahor M, Shorr RI, et al. The role of diastolic blood pressure when treating isolated systolic hypertension. Arch Intern Med. 1999;159:2004–2009. [DOI] [PubMed] [Google Scholar]
- 12. Kario K, Tobin JN, Wolfson LI, et al. Lower standing systolic blood pressure as a predictor of falls in the elderly: a community‐based prospective study. J Am Coll Cardiol. 2001;38:246–252. [DOI] [PubMed] [Google Scholar]
- 13. Statistics NCHS . National Health and Nutrition Examination Survey: Center for Disease Control and Prevention. http://www.cdc.gov/nchs/nhanes.htm. Accessed May 15, 2013.
- 14. NHANES . Analytic Note Regarding 2007–2010 Survey Design Changes and Combining Data Across other Survey Cycles. 2010. http://www.cdc.gov/nchs/data/nhanes/analyticnote_2007-2010.pdf. Accessed November 8, 2013.
- 15. Selvin E, Manzi J, Stevens LA, et al. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis. 2007;50:918–926. [DOI] [PubMed] [Google Scholar]
- 16. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. NHANES . Blood Pressure Questionnaire. 2007. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/bpq07_08_eng.pdf. Accessed June 17, 2013.
- 18. Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172:1162–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: third national health and nutrition examination survey. Am J Kidney Dis. 2003;41:1–12. [DOI] [PubMed] [Google Scholar]
- 20. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606. [DOI] [PubMed] [Google Scholar]
- 21. Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–2114. [DOI] [PubMed] [Google Scholar]
- 22. Ostchega Y, Dillon CF, Hughes JP, et al. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056–1065. [DOI] [PubMed] [Google Scholar]
- 23. Ong KL, Cheung BMY, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 24. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 25. Lloyd‐Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. [DOI] [PubMed] [Google Scholar]
- 26. Lloyd‐Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. [DOI] [PubMed] [Google Scholar]
- 27. Pastor‐Barriuso R, Banegas JR, Damián J, Appel LJGE. Systolic blood pressure, diastolic blood pressure, and pulse pressure: an evaluation of their joint effect on mortality. Ann Intern Med. 2003;139:731–739. [DOI] [PubMed] [Google Scholar]
- 28. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. [DOI] [PubMed] [Google Scholar]
- 29. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123:2434–2506. [DOI] [PubMed] [Google Scholar]
- 30. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:192–193. [DOI] [PubMed] [Google Scholar]
- 31. Collard RM, Boter H, Schoevers RA, Oude VR. Prevalence of frailty in community‐dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60:1487–1492. [DOI] [PubMed] [Google Scholar]
- 32. Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community‐living older persons. J Gerontol A Biol Sci Med. Sci. 2003;58:70–75. [DOI] [PubMed] [Google Scholar]
- 33. Gribbin J, Hubbard R, Gladman JRF, et al. Risk of falls associated with antihypertensive medication: population‐based case‐control study. Age Ageing. 2010;39:592–597. [DOI] [PubMed] [Google Scholar]
- 34. Woolcott JC, Richardson KJ, Wiens MO, et al. Meta‐analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. [DOI] [PubMed] [Google Scholar]
- 35. NIH . Systolic Blood Pressure Intervention Trial (SPRINT). 2013.. Available at: http://clinicaltrials.gov/ct2/show/NCT01206062. Accessed May 28, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Mean blood pressure and prevalence of hypertension among US adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010 for people without (top panel) and with (bottom panel) impairments in activities of daily living.
Table S2. Number of US adults 80 years and older with hypertension in 1988–1994, 1999–2004, and 2005–2010.
Table S3. Prevalence of systolic blood pressure <120 mm Hg, <130 mm Hg, <140 mm Hg, <150 mm Hg, and <160 mm Hg and diastolic blood pressure <60 mm Hg, <70 mm Hg, <80 mm Hg, <90 mm Hg, and <100 mm Hg among US adults 80 years and older in 1988–1994, 1999–2004, and 2005–2010.


