Despite advances in cancer care, anticancer therapeutics still cause significant acute and long-term morbidities, including cancer-related fatigue, neuropathies, cardiopulmonary limitations, lymphedema, and neurocognitive sequelae. Cancer survivors in Southeast Asia are often not prepared for these complications of cancer and its treatment which often results in physical disability, causing high levels of psychological distress and poorer quality of life.[1] However, the treatment rates for readily remediable physical impairments are reported to be <2%, even in developed countries.[2]
Cancer Rehabilitation Paradigms and Challenges in Adoption
The field of cancer rehabilitation addresses the needs of cancer survivors through optimizing physical, social, psychological, and vocational functions within the limits imposed by the disease and its treatment. It embodies a patient-centered, comprehensive, and integrated approach through a dedicated and interdisciplinary rehabilitation team with domain expertise in oncology nursing, rehabilitation medicine, physiotherapy, occupational therapy, exercise physiology, psychology, speech language pathology, nutrition, and counseling among others.[2] Cancer rehabilitation can be divided into various paradigms, comprising preventative rehabilitation (reducing the effect of expected disabilities), restorative rehabilitation (returning patients to previous levels of function), supportive rehabilitation (helping patients adapt to their disabilities), and palliative rehabilitation (minimizing complications and providing comfort and support).
While much is known about the benefits of cancer rehabilitation, several practical barriers constrain the scope of survivor-centered supportive care in Singapore. The majority of cancer survivors still consult their oncologists for their survivorship care needs, who may not have the sufficient time or knowledge to identify and manage lesser known supportive care issues. The involvement of other healthcare disciplines such as nursing and allied health is also often ad hoc in nature and not integrated into routine cancer care pathways, leading to care fragmentation. Patients also often opt to receive such rehabilitative services in tertiary-level centers and are not aware of community-level rehabilitation services. The level of healthcare literacy on the subacute and long-term sequelae of cancer complications in local cancer survivors is also unknown and possibly lower than in western countries, resulting in lower awareness of cancer rehabilitation services.[3]
Thankfully, the role of cancer rehabilitation in cancer survivorship is gaining recognition among healthcare providers and patients in Singapore. However, rehabilitation still remains largely limited to the immediate inpatient posttreatment or postoperative period, where an acute deterioration in function usually occurs. In addition, while the increasing adoption of cancer rehabilitation services is encouraging, there appears to be an under-emphasis on the preventative aspects of rehabilitation (i.e., prehabilitation) and the role of exercise-based interventions situated in the community after acute cancer treatment.
Prehabilitation in Patients with Cancer
The primary goal of prehabilitation is to build up the physiological reserves of at-risk patients even before treatment has commenced, allowing patients to reduce the severity of treatment-related impairments and have a faster recovery to pretreatment physiological levels [Figure 1].[4] This involves a functional assessment to establish baseline fitness and identify impairments, followed by targeted physical, nutritional, and psychosocial interventions in the pretreatment phase, so as to prevent or reduce posttreatment functional decline.
Figure 1.
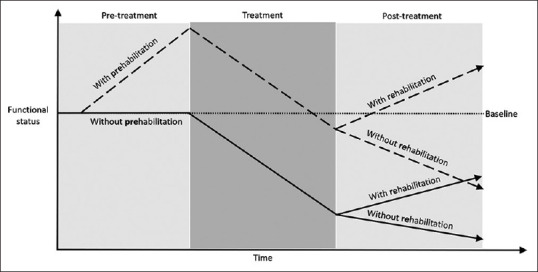
Relationship between prehabilitation and rehabilitation and the proposed differences in outcome[4]
Cancer prehabilitation has also shown encouraging long-term outcomes, including improved gait, cardiopulmonary function, urinary continence, mood, and quality of life measures.[5] These may also translate into reduced surgical complications, hospital length of stay, hospital readmissions, and overall healthcare costs.[5]
One of the earliest prehabilitation programs in Singapore was piloted at the Division of General Surgery, Khoo Teck Puat Hospital, since 2007 for elderly frail patients requiring colorectal surgery. This was a transdisciplinary, collaborative model of care involving nurse clinicians, physiotherapists, dieticians, surgeons, and physicians. A dedicated nurse clinician was designated as the coordinator, who then performed patient assessment, directed nursing care, and obtained inputs from members of the prehabilitation service, culminating in individualized prehabilitation targets for patients. These targets included the patient's level of education of the disease and surgery, ideal weight, dietary intake, and functional measures (chair-stand, 10-m walk test, and Modified Barthel Index). The nurse clinician then discussed these targets and the prehabilitation program with the patients, who were then stratified to either commence prehabilitation at home or in a day rehabilitation center 2 weeks before surgery. This program led to significantly shorter hospital stays and full functional recovery in all patients receiving prehabilitation.[6] Although the benefits of prehabilitation are obvious, such programs have yet to gain widespread adoption among patients with other types of cancer in Singapore. Clearly, there is an important role for oncology nurses in developing such prehabilitation services, which should then be integrated into existing cancer care pathways.[6]
Exercise in Patients with Cancer
Even in the absence of any cancer-specific morbidity, virtually, all cancer survivors experience impaired cardiorespiratory and skeletal muscle oxidative capacity as a result of cancer therapy. Therefore, addressing fitness impairment through patient education and targeted exercise prescription is integral to any cancer survivorship program.
Multiple international organizations have published exercise recommendations in patients with cancer based on consistently strong evidence.[7] Adequate levels of exercise consist of thrice-weekly aerobic exercise of at least moderate intensity over 30 min each session and twice-weekly resistance exercise (one exercise per major muscle, 8–15 repetitions per set, two sets per exercise). Physical activity is beneficial for the prevention of several types of cancers and may have mortality benefits in patients with breast, colon, and prostate cancers.[7] Moreover, it improves anxiety, depression, fatigue, physical function, and health-related quality of life in cancer survivors [Table 1].[8]
Table 1.
Physical exercises for cancer related impairments[8]
| Cancer related impairments | Aerobic exercise | Resistance exercise | Strength exercise | Weight and impact exercise | Balance exercise | Flexibility and relaxation exercise |
|---|---|---|---|---|---|---|
| Physical domains | ||||||
| Bone loss/disease | • | • | ||||
| Muscle and fat mass dysfunction | • | • | ||||
| Cachexia | • | • | ||||
| Peripheral neuropathy | • | • | ||||
| Lymphedema | • | |||||
| Psychological domains | ||||||
| Depression, anxiety | • | |||||
| Quality of life | • | • | • | • | ||
| Self esteem | • | |||||
| Psychosocial domains | ||||||
| Pain | • | |||||
| Fatigue | • | • | • | • | ||
| Sleep disorder | • | • |
Dots indicate the specific exercise interventions which are appropriate for that particular cancer related impairment
Although physical activity is suitable for most cancer survivors in stable condition, a pre-exercise assessment, which can be performed by oncology nurses, is recommended in all patients to screen for impairments and potential complications that may affect a person's ability to safely engage in exercise.[9] The evaluation may result in special exercise modifications, which take into consideration cancer-specific impairments such as lymphedema, peripheral neuropathy, musculoskeletal issues, and poor bone health. A cancer rehabilitation specialist may be required to perform risk assessment before exercise commencement in patients with certain conditions, e.g., cardiopulmonary disease, recent lung or abdominal surgery, ostomies, or severe fatigue.[9]
Despite published exercise guidelines, nearly 70% of cancer survivors do not meet current physical activity requirements. This is often due to the lack of awareness of the value of exercise in cancer, the lack of suitable exercise programs available for cancer survivors, and the uncertainty by cancer patients or healthcare providers regarding the safety or suitability of exercise.[10] One possible solution, through which we have achieved early success, is to empower oncology nurses who can be exercise advocates when engaging cancer patients in the inpatient or oncology clinic setting. They can then coordinate the transition of patients from the hospital to a community-based cancer rehabilitation program.
Conclusions
While the components for successful cancer rehabilitation programs exist within the Singapore healthcare system, there is still potential for the further development of a patient-centric cancer rehabilitation model. Oncology nursing has a clear and important role in promoting prehabilitation and exercise-based interventions among cancer survivors and in assisting patients to navigate the survivorship continuum from tertiary care to the community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.ACTION Study Group. Health-related quality of life and psychological distress among cancer survivors in Southeast Asia: Results from a longitudinal study in eight low- and middle-income countries. BMC Med. 2017;15:10. doi: 10.1186/s12916-016-0768-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silver JK, Baima J, Mayer RS. Impairment-driven cancer rehabilitation: An essential component of quality care and survivorship. CA Cancer J Clin. 2013;63:295–317. doi: 10.3322/caac.21186. [DOI] [PubMed] [Google Scholar]
- 3.Loh KW, Ng T, Choo SP, Saw HM, Mahendran R, Tan C, et al. Cancer supportive and survivorship care in Singapore: Current challenges and future outlook. J Glob Oncol. 2018;4:1–8. doi: 10.1200/JGO.17.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Macmillan Cancer Support, NIHR Cancer and Nutrition Collaboration, Royal College of Anaesthetists. Prehabilitation for people with cancer: Principles and guidance for prehabilitation within the management and support of people with cancer. Macmillan; 2019. [Last accessed on 2021 Jan 23]. Available from: www.macmillan.org.uk/assets/prehabilitation-guidance-for-people-with-cancer.pdf . [Google Scholar]
- 5.Shun SC. Cancer Prehabilitation for Patients starting from active treatment to surveillance. Asia Pac J Oncol Nurs. 2016;3:37–40. doi: 10.4103/2347-5625.178169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chia CL, Mantoo SK, Tan KY. 'Start to finish trans-institutional transdisciplinary care': A novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis. 2016;18:O43–50. doi: 10.1111/codi.13166. [DOI] [PubMed] [Google Scholar]
- 7.Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019;51:2375–90. doi: 10.1249/MSS.0000000000002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferioli M, Zauli G, Martelli AM, Vitale M, McCubrey JA, Ultimo S, et al. Impact of physical exercise in cancer survivors during and after antineoplastic treatments. Oncotarget. 2018;9:14005–34. doi: 10.18632/oncotarget.24456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Denlinger CS, Ligibel JA, Are M, Baker KS, Demark-Wahnefried W, Dizon D, et al. Survivorship: Healthy lifestyles, version 2.2014. J Natl Compr Canc Netw. 2014;12:1222–37. doi: 10.6004/jnccn.2014.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmitz KH, Campbell AM, Stuiver MM, Pinto BM, Schwartz AL, Morris GS, et al. Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA Cancer J Clin. 2019;69:468–84. doi: 10.3322/caac.21579. [DOI] [PMC free article] [PubMed] [Google Scholar]


