Abstract
Aims: Understanding of the perceived stress and coping strategies adopted by people is important for contemplating the consequences of a pandemic on mental health of people globally. In this study, we intended to assess the perceived stress status under quarantine/isolation globally during the COVID-19 pandemic.
Methods: This is a multicentre, multinational cross-sectional study that recruited isolated/quarantined individuals suspected or confirmed to have COVID-19 to assess the psychological impact of the quarantine/isolation experience by answering a survey distributed online.
Results: The study was conducted across 63 participating countries, gaining 1,871 valid responses. There was a higher proportion of female participants in the Moderate to High Perceived Stress Scores (MH-PSS) group compared to the Low Perceived Stress Score group (66.0 vs. 52.0%) and a higher proportion of individuals whose marital status was single had MH-PSS (57.1%). Also, individual's religion (Christian, Hindu, and Muslim), no formal education level, being exposed to a confirmed or suspected COVID-19 patient, being forced to be quarantined/isolated, uncomfortable feeling during quarantine period may significantly increase the risk of MH-PSS (p < 0.05).
Conclusions: Many factors can predict stress in COVID-19 pandemic including female sex, being single, religion, no formal education, involuntary quarantine, location and reason of quarantine/isolation, and place of exposure.
Keywords: perceived stress status, COVID-19, mental health, quarantine, survey
Introduction
The COVID-19 pandemic, which emerged in Wuhan, China, has rampantly spread to various countries, territories, and areas globally and has been one of the most serious pandemic over more than 100 years following the influenza pandemic in 1918 (1). Apart from the burden on the healthcare industry, the COVID-19 pandemic has significantly affected the economy worldwide (2). In response to the socio-economic burden caused by this pandemic, governments in many countries launched policies and guidelines quickly in order to ascertain control over this pandemic (2). In the absence of any definitive treatment and vaccination available against SARS-CoV-2, the causative organism; health officials and organizations worldwide have asserted the necessity of non-pharmacological interventions with imposition, if indispensable to ascertain control over the ongoing pandemic (3). Some of these non-pharmacological interventions included social/physical distancing and lockdowns with isolation of COVID-19 positive and suspected COVID-19 patients, quarantine of exposed individuals, travel limitations, closure of educational institutions and workplaces, prohibition of mass gatherings, rapid testing, proper allocation and use of personal protective equipment and maintenance of personal hygiene (3, 4).
In China, particularly in Hubei province, early measures taken by the government consisted of rigorous lockdown with travel restrictions, and social distancing measures. Other measures included rapid case detection with immediate isolation and quarantine measures for the infected and suspected cases with medical observation for all the contacts. These measures have had a positive impact on controlling the COVID-19 outbreak (4–8).
The combined non-pharmacological interventions had a substantial effect on the reduced transmission of COVID-19 across China (4). Similarly, Vietnam, which was the first nation to delineate human-to-human transmission outside China, successfully controlled the outbreak using extensive control measures without enforcing a strict lockdown (9). Vietnam instituted rapid isolation and detection of primary and secondary cases and immediate quarantine of their contacts to curb transmission. Suspected cases in Vietnam were recognized and quarantined based on their epidemiological risk of infection. In Vietnam, more than 200,000 people have been quarantined for 14 days (10). Thus, non-pharmaceutical interventions have been very effective in controlling the COVID-19 pandemic. Such non-pharmaceutical interventions have also affected the mental health of people worldwide. A recent study done on 1,784 school students in China, showed that closure of schools as a part of lockdown and social distancing guidelines affected the mental health of the students with a slightly increased prevalence of depressive and anxiety symptoms (11). Another study done on healthcare workers in Italy showed that they experienced increased symptoms of depression, post-traumatic stress symptoms, insomnia, and perceived stress (12). These findings are in congruence with the past pandemics such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) (13–15). Amongst the non-pharmaceutical interventions, quarantine and isolation have been found to be the most associated with significant psychological impact (16). Quarantine and isolation both involve separation from loved ones, lack of freedom, and boredom which can affect mental health as seen in the past pandemics (16). A study done on 170 people who were self-isolated at home during the COVID-19 outbreak in China showed that anxiety and stress of isolated individuals were at higher levels and quality of sleep was low (17). However, there is a paucity of evidence quantifying perceived stress and peoples' coping strategies adopted during confinement periods in isolation/quarantine facilities globally. Understanding of the perceived stress and coping strategies adopted by people is important for contemplating the consequences of a pandemic on mental health of people globally. The findings can help health officials in drafting policies and implementing targeted measures to reduce psychological trauma faced by quarantined/isolated people during a pandemic. In this study, we intended to assess the perceived stress status of quarantine/isolation globally during the COVID-19 pandemic and examine the various correlates involved in dealing with the perceived stress.
Methods
Study Design and Participants
This is a multicenter, multinational cross-sectional study that recruited isolated/quarantined individuals suspected or confirmed to have COVID-19 (from May to June 2020) to assess the psychological impact of the quarantine/isolation experience on people in quarantine/isolation areas all over the world and evaluate the ways they confronted stress during that period. Both healthcare workers and non-healthcare workers were included. The survey was distributed online in two ways; the first was distributed directly by collaborators to a convenience sample of patients in quarantine/isolation centers worldwide. The second was distributed by collaborators using a snowball sampling technique, and the collaborators acting as gatekeepers on various social media platforms promoting the survey.
The study participants were from the following countries: Afghanistan, Albania, Angola, Bangladesh, Belgium, Bolivia, Bosnia, Brazil, Canada, Chile, China, Czech Republic, Denmark, Ecuador, Egypt, El Salvador, France, Germany, Greece, Honduras, Hungary, India, Indonesia, Italy, Japan, Jordan, Kenya, Korea, Kosovo, Lebanon, Libya, Luxembourg, Malaysia, Mexico, Nepal, Netherlands, Nigeria, Oman, Pakistan, Palestine, Peru, Philippines, Poland, Portugal, Puerto Rico, Qatar, Romania, Russia, Saudi Arabia, Scotland, Seychelles, Singapore, Somalia, South Africa, Spain, Sudan, Thailand, Timor-Leste, Turkey, United Arab Emirates, United Kingdom, United States, and Vietnam (Supplementary Table 1).
Study Questionnaire
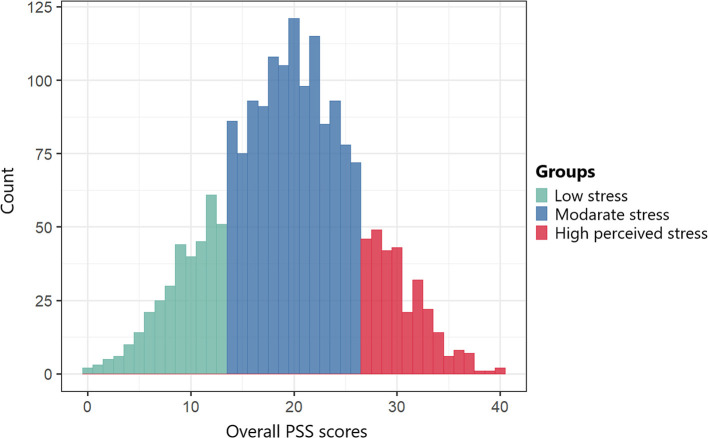
The survey questionnaire included three sections. The first section was comprised of 15 questions that obtained the sociodemographic characteristics of the participants. The second section was comprised of 10 questions that obtained the quarantine/isolation information of the participants. The third section assessed the psychological impact of quarantine/isolation and coping strategies of the participants using the Perceived Stress Scale-10 (PSS-10) (18). PSS-10 is a stress assessment tool, including ten questions rated from 0 to 4. The overall PSS score can range from 0 to 40. In this study, a score from 0 to 13 was classified as low perceived stress scores (L-PSS), while a score from 14 to 40 was classified as the moderated to high perceived stress scores (MH-PSS) [Figure 1; (18)].
Figure 1.
Distribution of study participants by the overall PSS scores.
A panel of healthcare professionals, including two epidemiologists, one psychologist, five physicians, and five medical students, revised the questionnaire. The questionnaire was validated by a pilot survey of 30 medical students and five people who had quarantine experience during the COVID-19 outbreak. This validation ensured that all the questions were phrased clearly and appropriately for comprehension and evaluated the time needed to complete the questionnaire, and served to avoid bias that might otherwise arise.
Forward and reverse translation of the questionnaire to local languages was performed. The survey was distributed in various languages, translated by native speakers. These languages included Albanian, Arabic, Bengali, Chinese, English, Filipino, French, German, Hindi, Indonesian, Japanese, Korean, Malay, Malayalam, Nepali, Pashto, Portuguese, Russian, Spanish, Tamil, Thai, Ukrainian, Urdu, and Vietnamese. The questionnaire in each language was pretested on 3–5 native speakers and subsequently modified and validated.
Participation was voluntary, anonymous and participants had to provide informed consent on the first page of the questionnaire before accessing the rest of the questionnaire. The data from the web-based survey was extracted, kept confidential, and encrypted for analysis.
Statistical Analysis
Descriptive statistics were performed to assess the differences in factors that influence the two categories of stress on the Perceived Stress Scores (PSS). The T-test was used to compare the difference in age and number of days quarantined/isolated between subjects with L-PSS and MH-PSS status, and the chi-square test was used to evaluate the remaining variables' differences. We used the logistic regression model to determine the factors related to the subject's stress. In which, the Stepwise AIC method was used to select variables related to stress status based on the optimal model. The analysis was performed using the MASS and CompareGroups packages on the R language version 3.6.0 software.
Results
Characteristics of Survey Participants
The study was conducted across 63 participating countries. We got a total of 6,005 responses, of which the number of valid responses was 1,871 (31.2%). The highest proportion of responses was recorded from Albania (20.6%), Vietnam (17%), and India (9%). Table 1 summarized the distribution of the survey participants' basic characteristics categorized as having either L-PSS or MH-PSS status. More than half of the participants belonged to the Asian continent (55%). Overall, the mean PSS scores of participants in the L-PSS and MH-PSS categories were 9.43 ± 2.96 and 29.6 ± 22.7, respectively. Nearly two-thirds of the participants were female (n = 1,174, 64%), with the mean age of 31.5 ± 10.6. Around 53.5% (n = 984) of participants were of Asian ethnic origin. Among the included participants, 34.4% (n = 637) belonged to the Muslim religion while 24.7% (n = 459), 19.7% (n = 366), 10.9% (n = 202), 6.9% (n = 128), and 3.7% (n = 68) belonged to Christianity, no religion, Hinduism, Buddhism, and other religions, respectively. Approximately three of every four respondents (72.5%) had their educational attainment completed up to the university level. At the time of the survey, 60% (n = 1,113) of the participants had employment, with only 10% (n = 194) having no job status at all. Among these participants, nearly one-third (n = 563, 30%) belonged to the healthcare profession.
Table 1.
Basic characteristics among the survey participants across three groups of perceived stress categories.
| Total N = 1,871 | Low perceived stress score (L-PSS) | Moderate to high perceived stress score (MH-PSS) | p-value | |
|---|---|---|---|---|
| N = 354 | N = 1,507 | |||
| Age (year) (n=) [Mean, SD] | 32.3 (9.62) | 30.7 (10.5) | 0.008 | |
| Number of quarantine days (n=) [Mean, SD] | 23.9 (19.6) | 29.6 (22.7) | < 0.001 | |
| PSS (Total points) (n=) [Mean, SD] | 9.43 (2.96) | 22.0 (5.33) | < 0.001 | |
| Gender (n = 1,856) | < 0.001 | |||
| Female | 184 (52.0%) | 990 (66.0%) | ||
| Male | 170 (48.0%) | 510 (34.0%) | ||
| Race (n = 1,839) | < 0.001 | |||
| White/Caucasian | 73 (21.0%) | 532 (35.7%) | ||
| Asia | 243 (70.0%) | 741 (49.7%) | ||
| Hispanic/Latino | 12 (3.46%) | 105 (7.04%) | ||
| Others | 19 (5.48%) | 114 (7.64%) | ||
| Religion (n = 1,850) | < 0.001 | |||
| No religion | 112 (31.7%) | 244 (16.3%) | ||
| Buddhist | 39 (11.0%) | 89 (5.95%) | ||
| Christian | 58 (16.4%) | 401 (26.8%) | ||
| Hindu | 32 (9.07%) | 170 (11.4%) | ||
| Muslim | 101 (28.6%) | 536 (35.8%) | ||
| Others | 11 (3.12%) | 57 (3.81%) | ||
| Marital status (n = 1,856) | 0.004 | |||
| Single | 166 (47.3%) | 859 (57.1%) | ||
| Divorced/ Widowed/Separated | 17 (4.84%) | 57 (3.79%) | ||
| Married/Domestic partnership | 168 (47.9%) | 589 (39.1%) | ||
| Level of education (n = 1,845) | 0.001 | |||
| Master/PhD/Doctoral | 92 (26.1%) | 433 (29.0%) | ||
| University | 137 (38.8%) | 676 (45.3%) | ||
| Vocational training | 34 (9.63%) | 117 (7.84%) | ||
| Primary school/Secondary school/High school | 88 (24.9%) | 242 (16.2%) | ||
| No formal education | 2 (0.57%) | 24 (1.61%) | ||
| Employment status (n = 1,860) | < 0.001 | |||
| Full time employment | 211 (59.8%) | 677 (44.9%) | ||
| Casual employment | 9 (2.55%) | 76 (5.04%) | ||
| Part time employment | 29 (8.22%) | 111 (7.37%) | ||
| Retired | 5 (1.42%) | 34 (2.26%) | ||
| Student | 69 (19.5%) | 403 (26.7%) | ||
| Unemployed | 20 (5.67%) | 174 (11.5%) | ||
| Others | 10 (2.83%) | 32 (2.12%) | ||
| Average income (USD) (n = 1,791) | 0.052 | |||
| < 250 | 87 (25.3%) | 484 (33.4%) | ||
| 250–500 | 89 (25.9%) | 356 (24.6%) | ||
| 500–750 | 56 (16.3%) | 204 (14.1%) | ||
| 750–1,000 | 37 (10.8%) | 145 (10.0%) | ||
| Over 1,000 | 75 (21.8%) | 258 (17.8%) | ||
| Main laborer in the family (n = 1,860) | < 0.001 | |||
| No | 179 (50.6%) | 949 (63.0%) | ||
| Yes | 175 (49.4%) | 557 (37.0%) | ||
| Healthcare worker (n = 1,851) | 0.091 | |||
| No | 232 (65.7%) | 1,056 (70.5%) | ||
| Yes | 121 (34.3%) | 442 (29.5%) | ||
| Reason for quarantine/isolation (n = 1,773) | < 0.001 | |||
| F0 | 61 (17.3%) | 151 (10.6%) | ||
| F1 | 75 (21.3%) | 205 (14.4%) | ||
| F2/F3/F4 | 89 (25.3%) | 423 (29.8%) | ||
| I live, stay or work at a place nearby a confirmed COVID-19 patient | 81 (23.0%) | 408 (28.7%) | ||
| I returned from affected geographic areas | 46 (13.1%) | 234 (16.5%) | ||
| Place of exposure (n = 1,546) | < 0.001 | |||
| In hospital | 96 (31.3%) | 265 (21.4%) | ||
| At home | 18 (5.86%) | 98 (7.91%) | ||
| At hotel/ At a hall, concert, cinema | 2 (0.65%) | 39 (3.15%) | ||
| At workplace | 34 (11.1%) | 185 (14.9%) | ||
| During travel by airplane/by bus/by taxi/by train | 28 (9.12%) | 159 (12.8%) | ||
| I do not know the source of my exposure | 73 (23.8%) | 303 (24.5%) | ||
| Others | 56 (18.2%) | 190 (15.3%) | ||
| Place of isolation (n = 1,762) | < 0.001 | |||
| At home | 196 (57.8%) | 1,098 (77.2%) | ||
| At the designated place by the Government | 52 (15.3%) | 178 (12.5%) | ||
| In hospital | 91 (26.8%) | 147 (10.3%) | ||
| Which of the following was true about your quarantine/isolation? (n = 1,756) | < 0.001 | |||
| I was forced to quarantine/isolated | 38 (11.3%) | 330 (23.2%) | ||
| I was voluntarily quarantined/isolated | 297 (88.7%) | 1,091 (76.8%) | ||
| Who are you quarantined with (n = 1,737) | 0.007 | |||
| No, only me | 212 (63.3%) | 779 (55.6%) | ||
| Family | 97 (29.0%) | 535 (38.2%) | ||
| Others | 26 (7.76%) | 88 (6.28%) | ||
| Comfortable in isolation time (n = 1,824) | < 0.001 | |||
| Not at all | 13 (3.71%) | 103 (6.99%) | ||
| A little bit | 35 (10.0%) | 195 (13.2%) | ||
| Moderately | 116 (33.1%) | 592 (40.2%) | ||
| Quite a bit | 104 (29.7%) | 402 (27.3%) | ||
| Extremely | 82 (23.4%) | 182 (12.3%) | ||
| Continent (n = 1,854) | < 0.001 | |||
| Africa | 12 (3.39%) | 81 (5.40%) | ||
| America | 21 (5.93%) | 138 (9.20%) | ||
| Asia | 256 (72.3%) | 785 (52.3%) | ||
| Europe | 65 (18.4%) | 496 (33.1%) |
In response to the question of the place of exposure among the participants, 37.5% (n = 580) reported hospital or workplace as their source of exposure, and 24.3% (n = 376) could not identify the source, while 12.1% (n = 187) individuals got exposure while traveling. Nearly three-fourths of the individuals (73%, n = 1,294) kept themselves isolated at home either alone (56.4%, n = 991) or with family (36.0%, n = 632). The majority of the participants (79%, n = 1,388) remained in quarantine/isolation voluntarily, and 81% (n = 1,478) of participants reported their comfort to be ranging from extreme to quite a6 bit while being in isolation.
Factors Associated Across Different Level of Perceived Stress Score Status
All the explored characteristics in Table 1, across the L-PSS and MH-PSS categories, were statistically significantly different except average income and healthcare worker characteristics. Table 1 showed that the increase in the number of quarantine days was associated with an increased level of perceived stress across L-PSS and MH-PSS categories, reporting a mean of 23.9 ± 19.6 days and 29.6 ± 22.7 days, respectively (p < 0.001). There was a higher proportion of female participants in the MH-PSS compared to L-PSS category (66.0 vs. 52.0%). Among the Asian ethnic respondents, a higher proportion of respondents was reported in the L-PSS group (70.0%), while the White/Caucasian respondents reported a higher proportion of respondents in the MH-PSS group (35.7%). The study estimated that a higher proportion of individuals whose marital status was single experienced high stress (57.1%). People with no formal education were more likely to have higher stress (p < 0.001).
Interestingly, there was a higher proportion of respondents in the MH-PSS category than the L-PSS category group among non-healthcare participants (70.5 vs. 65.7%) in contrast to the findings among healthcare participants (29.5 vs. 34.3%). The study found a higher proportion of respondents in the MH-PSS group than the L-PSS group among participants who underwent quarantine/isolation due to their residence or workplace being near a confirmed COVID-19 patient, returnees from affected geographic areas, and close contacts of confirmed or suspected COVID-19 cases. A higher proportion of respondents was found among the MH-PSS group compared to the L-PSS group among respondents who were unaware of their source of exposure. Also, a higher prevalence of participants having higher PSS was found among those whose place of isolation was home compared with those residing in a hospital or at a government-designated place.
Predictors of MH-PSS Among the Survey Participants
Table 2 illustrated the explanatory variables in the multivariate ordinal regression model that contributed to predicting MH-PSS among the included survey participants. In the regression result, male respondents were more likely to have MH-PSS (OR: 1.43, 95% CI: 1.02–2.02, p = 0.038) compared to their female counterparts. The study found that an individual's religion may increase the odds of MH-PSS compared to the participants who identified themselves as having no religion. Compared to those with no religious affiliation, the odds of having MH-PSS were significantly higher among those who identified as Hindus (OR: 4.40, 95% CI: 2.41–78.32), followed by Christians (OR: 4.11, 95% CI: 2.46–7.03), and Muslims (OR: 2.47, 95% CI: 1.62–3.80) (p < 0.001). Individuals who possessed no formal education were more likely to have MH-PSS (OR: 9.60, 95% CI: 1.74–180.51, p = 0.035) compared to individuals who had attained higher educational status. Students (OR: 1.63, 95% CI: 1.07–2.51, p = 0.023) and those on casual employment (OR: 2.56, 95% CI: 1.08–7.20, p = 0.047) had a significantly higher odds of having MH-PSS when compared to full-time employed respondents. The index case (F1) had about 1.96 times higher odds to be in the MH-PSS category (OR: 1.96, 95% CI: 1.17–3.28, p = 0.011) than the corresponding F0 case. The study also found that participants had 1.99 times increased odds of MH-PSS when the workplace (OR: 1.99, 95% CI: 1.13–3.61, p = 0.02) was designated as the place of exposure to COVID-19 compared to been exposed in the hospital setting. Participants who were voluntarily isolated/quarantine (OR: 0.51, 95% CI: 0.31–0.80, p = 0.005) were less likely to have MH-PSS category than participants who were forced to quarantine/isolation. There were decreased odds of MH-PSS category when an individual reported that they remained comfortable during the period of isolation/quarantine. Participants reporting that they were not at all comfortable during isolation/quarantine time had the highest likelihood of higher stress (OR: 3.56, 95% CI: 1.44–10.20, p = 0.010) compared to those that were extremely comfortable during isolation.
Table 2.
Multivariable logistic regression analysis for factors associated with perceived stress among the quarantined/isolated participants.
| Variables | Univariate analysis | Multivariable analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age (10 years) | 1.17 (1.06–1.31) | 0.003 | 1.20 (1.06–1.38) | 0.007 |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.68 (1.27–2.24) | < 0.001 | 1.43 (1.02–2.02) | 0.038 |
| Religion | ||||
| No religion | Reference | Reference | ||
| Buddhist | 1.63 (0.98–2.77) | 0.067 | 1.38 (0.77–2.52) | 0.280 |
| Christian | 4.84 (3.06–7.84) | < 0.001 | 4.11 (2.46–7.03) | < 0.001 |
| Hindu | 2.87 (1.69–5.04) | < 0.001 | 4.40 (2.41–8.32) | < 0.001 |
| Muslim | 2.53 (1.76–3.65) | < 0.001 | 2.47 (1.62–3.80) | < 0.001 |
| Others | 2.93 (1.32–7.33) | 0.013 | 2.44 (1.04–6.48) | 0.053 |
| Level of education | ||||
| Master/ PhD/Doctoral | Reference | Reference | ||
| University | 1.03 (0.72–1.47) | 0.851 | 1.28 (0.86–1.90) | 0.224 |
| Vocational training | 0.73 (0.42–1.28) | 0.261 | 1.16 (0.62–2.20) | 0.654 |
| Primary school/Secondary school/High school | 0.57 (0.38–0.87) | 0.009 | 0.65 (0.39–1.09) | 0.101 |
| No formal education | 4.55 (0.92–82.32) | 0.143 | 9.60 (1.74–180.51) | 0.035 |
| Employment status | ||||
| Full time employment | Reference | Reference | ||
| Casual employment | 2.59 (1.18–6.83) | 0.031 | 2.57 (1.08–7.20) | 0.047 |
| Part time employment | 0.95 (0.59–1.59) | 0.843 | 0.68 (0.39–1.21) | 0.176 |
| Retired | 1.95 (0.66–8.37) | 0.286 | 3.51 (1.02–16.73) | 0.070 |
| Student | 1.57 (1.10–2.27) | 0.015 | 1.63 (1.07–2.51) | 0.023 |
| Unemployed | 2.89 (1.50–6.31) | 0.003 | 2.13 (1.01–5.00) | 0.061 |
| Others | 0.88 (0.33–2.74) | 0.804 | 0.80 (0.26–2.83) | 0.717 |
| Reason for quarantine/isolation | ||||
| I was F0 | Reference | Reference | ||
| I was F1 | 1.66 (1.06–2.58) | 0.026 | 1.96 (1.17–3.28) | 0.011 |
| I was F2/F3/F4 | 2.15 (1.43–3.23) | < 0.001 | 2.05 (1.27–3.29) | 0.003 |
| I live, stay or work at a place nearby a confirmed COVID-19 patient | 2.78 (1.72–4.58) | < 0.001 | 1.33 (0.73–2.45) | 0.351 |
| I returned from affected geographic areas | 2.72 (1.65–4.58) | < 0.001 | 2.07 (1.15–3.80) | 0.017 |
| Place of exposure | ||||
| In hospital | Reference | Reference | ||
| At home | 1.07 (0.60–1.99) | 0.826 | 1.58 (0.81–3.20) | 0.194 |
| At hotel/At a hall, concert, cinema | 8.71 (1.83–156.35) | 0.035 | 12.36 (2.39–227.72) | 0.017 |
| At workplace | 1.63 (1.00–2.75) | 0.057 | 1.99 (1.13–3.61) | 0.020 |
| During travel by airplane/by bus/by taxi/by train | 1.40 (0.85–2.38) | 0.200 | 1.95 (1.10–3.53) | 0.024 |
| I do not know the source of my exposure | 0.74 (0.51–1.08) | 0.120 | 1.23 (0.77–1.96) | 0.383 |
| Others | 0.89 (0.55–1.46) | 0.643 | 0.94 (0.54–1.67) | 0.842 |
| Which of the following was true about your quarantine/isolation? | ||||
| I was forced to quarantine/isolated | Reference | Reference | ||
| I was voluntarily quarantined/isolated | 0.44 (0.28–0.66) | < 0.001 | 0.51 (0.31–0.80) | 0.005 |
| Comfortable in isolation time | ||||
| Extremely | Reference | Reference | ||
| Quite a bit | 1.51 (1.00–2.27) | 0.050 | 1.40 (0.88–2.24) | 0.158 |
| Moderately | 1.88 (1.26–2.81) | 0.002 | 2.09 (1.32–3.30) | 0.001 |
| A little bit | 1.91 (1.12–3.35) | 0.020 | 2.31 (1.24–4.41) | 0.010 |
| Not at all | 4.15 (1.82–11.26) | 0.002 | 3.56 (1.44–10.20) | 0.010 |
| Continent | ||||
| Asia | Reference | Reference | ||
| Africa | 2.90 (1.33–7.62) | 0.015 | 2.50 (1.05–7.01) | 0.055 |
| America | 1.90 (1.16–3.26) | 0.015 | 1.60 (0.88–3.03) | 0.133 |
| Europe | 2.96 (1.97–4.61) | < 0.001 | 2.58 (1.51–4.52) | 0.001 |
Discussion
We examined the various factors attributed to stress among individuals who were quarantined or isolated during the COVID-19 pandemic through our survey. There appeared to be a strong correlation between the number of days spent in quarantine and the PSS score, with a calculated risk of 0.7% increase in the PSS score with each additional day of quarantine. The impact of the duration of quarantine on mental health has been studied previously, particularly during the SARS outbreak, which demonstrated that prolonged quarantine periods were associated with symptoms of post-traumatic stress, anger, avoidance behavior, and overall poor mental health (19–21). In their study during the early days of the COVID-19 pandemic, Lu et al. (22) observed a similar relationship between quarantine duration and anxiety/depression by monitoring the activity of quarantined individuals on their Twitter accounts. The authors collectively analyzed 214,874 tweets from 1,278 quarantined individuals and 250,198 tweets from 1,278 individuals who served as controls. Besides, they also discovered fluctuations in the psychological state of the individuals, which was characterized by an increase in anxiety/depression at the start of the quarantine, followed by a gradual decrease, and a resurgence in anxiety/depression beyond 14 days of quarantine (22). Hawryluck et al. (19) demonstrated a significant rise in post-traumatic stress symptoms in individuals quarantined for more than 10 days during the SARS outbreak as opposed to individuals quarantined <10 days (19). In perspective, the number of days spent in quarantine was much higher among our study participants in comparison to previous studies, with the average duration of quarantine being 28.5 days, most likely attributed to the long incubation period associated with the illness (23). Regardless, the correlation between quarantine duration and impact on mental stress was demonstrated despite this aspect.
Differences in gender distribution were also observed across the groups of varying PSS scores. In general, females were more likely to report being stressed during the quarantine than males. This is in line with previous studies, which have also demonstrated a gender gap in the mental health impact caused by quarantine during outbreaks. Song et al. discovered a similar trend in their study among Chinese individuals in quarantine during the COVID-19 pandemic. In addition, the authors identified that the risk factors for stress were different for males and females. Among males, occupations with unstable income, higher education status, and quarantine duration were the most common risk factors.
In contrast, the need for information about the pandemic, worsening of the outbreak locally, and health problems during the quarantine were the key risk factors among females. Interestingly, the authors noted that males were less adaptive and had a lower tendency to recognize the need for psychological support when compared with females; however, they were more likely to seek medical care in response to infective symptoms (24). The observed gender differences are postulated to be due to the variation in psychological, physiological, and cognitive processes between the two sexes and their consequent response to stressful situations (25–27).
We also observed a relationship between relationship status and PSS scores, with single individuals being at the most significant risk of higher stress. This is in line with the findings from a recent study by Pieh et al. (28) during the COVID19 pandemic, where the authors demonstrated that participants with a good quality relationship scored significantly better on all mental health scales than individuals who were not in a relationship of any kind or those who were in a poor-quality relationship, in that order. The authors concluded that while being in a relationship in itself did not determine mental health status during quarantine, the quality of the relationship certainly played a role (28).
Contrary to expectations, MH-PSS was observed more frequently among individuals with religious beliefs compared to those with no religious beliefs. However, it is essential to note that nearly 80% of our study population identified with a religion, which may have contributed to this unexpected result. Yildirim et al. (29) found that positive religious coping mediated a greater meaning in life, which reduced loneliness during the coronavirus crises in Turkey. In line with this, the Thomas and Barbato (30) published similar findings demonstrating that positive religious coping was inversely related to depressive symptoms and a history of psychological disorders during the COVID-19 pandemic. Interestingly, the authors also found that Muslims had higher levels of positive religious coping than the Christians in their sample population. In our study, we did not assess the extent of religious involvement or the various religious coping tools/ strategies used by participants, which is believed to have played a role in our findings. In our study, we found that a higher educational status was associated with increased stress. The data on the link between educational status and psychological stress during quarantine is obscure. In a study among horse owners during an equine influenza outbreak, Taylor et al. observed that individuals with lower formal educational qualifications were at an increased risk of negative psychological impacts (31). On the other hand, Hawryluck et al. reported that the level of education did not affect both the understanding of quarantine requirements or the psychological impact of quarantining (19). In contrast, Song et al. noted that a higher educational status correlated positively with stress levels during the COVID-19 pandemic (24). Regardless, the need for information about the illness from public health officials and its clarity have been reported to influence the mental health of individuals in quarantine/isolation (32). The educational status of the individual may perhaps play a role in the understanding of this information and, therefore, affect the psychosocial impact of quarantine.
The observed relationship between being a confirmed case of infection, or the index case, in a family and the high levels of perceived stress, has been documented in previous studies. In a study by Jeong et al. during the MERS outbreak, it was reported that individuals who were isolated due to suspicion or confirmation of infection were more likely to manifest anxiety if they experienced symptoms characteristic of the infection and link it to the infection even if the suspected exposure was several months prior to the presentation of these symptoms (33). Studies also show that individuals who have been exposed to the risk of infection tend to worry about spreading the infection to their family members and others who have come into contact with them (32–34).
Recent studies in this area have identified other pre-existing individual characteristics that contribute to stress during pandemics. Osimo et al. (35) investigated the influence of personality traits on stress response during COVID-19 lockdowns and reported that individuals with a lower resilience and emotional stability and higher alexithymia had a poorer emotional response during home containment. Similarly, Moccia et al. (36), through their study on the Italian population during the COVID-19 pandemic, found that individuals with cyclothymic, depressive, and anxious temperaments and those who had a “Need for approval” style as per the Attachment Style Questionnaire (ASQ) were at higher risk of moderate-to-severe psychological distress; whereas ASQ “Confidence” and ASQ “Discomfort with closeness” was found to be protective traits. Another study conducted by Fiorillo et al. (37) during March to May 2020 in Italian population showed individuals with known mental disorders and physical disease had worse levels of depression and anxiety symptoms while individuals with cohabiting people, living with more number of family members and having higher level of satisfaction with one's own life were found to be protective against development of psychiatric symptoms.
Based on our search of the literature, the strength of our study is its multinational population, with participants from a total of 63 countries, making it one of the most diverse of recent publications on the relationship between quarantine during the COVID-19 pandemic and its psychological impact. We identified some of the key risk factors that contribute to anxiety/stress during the period of quarantine/isolation through our analysis. As with any study, there are several limitations to our research. While our survey reached participants of multiple countries, providing a heterogeneous multinational sample, the overall number of responses was relatively low, limiting the size of the study. In addition, we aimed to keep the survey at a length that was palatable to respondents. We were unable to assess several other factors such as pre-existing mental health illnesses, religious coping, individual temperament and self-control, ability to work from home, and living conditions. We believe that our study captures some of the major risk factors for mental stress during quarantine/isolation, specific to the COVID-19 pandemic, and paves the way for further research in this area. The findings of this study should be considered when dealing with psychosocial issues that arise during infectious outbreaks and help identify high-risk groups for negative psychological impact for early intervention.
Taken together our findings, many factors can predict stress in pandemics such as COVID-19, including female sex, being single, higher education status, and being of the non-healthcare profession. These and similar factors should be considered in handling stress and in managing future pandemics.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by ethical approval was obtained from the ethical committee of the IRB of Nagasaki University (Ref. No. 117; Approval number: NU_TMGH_2020_117_1). The patients/participants provided their written informed consent to participate in this study.
Consent to Publish
All authors give the full consent to publish this study.
Patient and Public Involvement
We collected data from the individuals who were quarantined/isolated after being suspected or confirmed to have contracted COVID-19. However, they have not involved directly in the setting of the research question or outcome measures. They did not have any role in designing or implementing this work or interpretation of the results.
Author Contributions
NH, ND, and LM: design of the idea and study workflow. ND, SM, TG, VT, LL, and PT: data acquisition. ND, SM, LM, AH, TG, LT, AR, FD, VT, and PT: data interpretation. LM, LT, and VT: final analysis. SM, AH, AR, and SD: drafting of the manuscript. NH, ND, LM, and SD: critical revision. All authors contributed to the final approved the final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Contributor Information
TMGH-Global COVID-19 Collaborative:
Nguyen Tien Huy, Nguyen Tran Minh Duc, Shamael Thabit Mohammed Alhady, Luu Ngoc Mai, Amr K. Hassan, Tran Van Giang, Le Van Truong, Rohanti Ravikulan, Akshay Raut, Farouq Muhammad Dayyab, Shyam Prakash Durme, Vu Thi Thu Trang, Le Quang Loc, and Pham Ngoc Thach
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.656664/full#supplementary-material
References
- 1.World Health Organization . Coronavirus Disease 2019 (COVID-19): Situation Report, 200. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200807-covid-19-sitrep-200.pdf?sfvrsn=2799bc0f_2 (accessed December 20, 2020).
- 2.Ozili P, Arun T. Spillover of COVID-19: Impact on the Global Economy. SSRN (2020). Available online at: https://ssrn.com/abstract=3562570 (accessed December 23, 2020).
- 3.Alvi M, Sivasankaran S, Singh M. Pharmacological and non-pharmacological efforts at prevention, mitigation, and treatment for COVID-19. J Drug Target. (2020) 28:742–54. 10.1080/1061186X.2020.1793990 [DOI] [PubMed] [Google Scholar]
- 4.Lai S, Ruktanonchai N, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. (2020) 585:410–3. 10.1038/s41586-020-2293-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau H, Khosrawipour V, Kocbach P, Mikolajczyk A, Schubert J, Bania J, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. (2020) 27:taaa037. 10.1093/jtm/taaa037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ainslie K, Walters C, Fu H, Bhatia S, Wang H, Xi X Baguelin M, et al. Evidence of initial success for China exiting COVID-19 social distancing policy after achieving containment. Wellcome Open Research. (2020) 5:81. 10.12688/wellcomeopenres.15843.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilder-Smith A, Freedman D. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. (2020) 27:taaa020. 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Du Z, Xu X, Wang L, Fox S, Cowling B, Galvani A, et al. Effects of proactive social distancing on COVID-19 outbreaks in 58 cities, China. Emerg Infect Dis. (2020) 26:2267–9. 10.3201/eid2609.201932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phan L, Nguyen T, Luong Q, Nguyen T, Nguyen H, Le HQ Nguyen TT, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. (2020) 382:872–4. 10.1056/NEJMc2001272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pham Q, Rabaa M, Duong H, Dang Q, Tran D, Quach HL, et al. The first 100 days of SARS-CoV-2 control in Vietnam. Clin Infect Dis. (2020) 1:ciaa1130. 10.1093/cid/ciaa1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in hubei province, China. JAMA Pediatr. (2019) 174:898–900. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. (2020) 3:e2010185. 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mak I, Chu C, Pan P, Yiu M, Chan V. Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry. (2009) 31:318–26. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee S, Kang W, Cho A, Kim T, Park J. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehens Psychiatry. (2018) 87:123–7. 10.1016/j.comppsych.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee A, Wong J, McAlonan G, Cheung V, Cheung C, Sham P, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. (2007) 52:233–40. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- 16.Brooks S, Webster R, Smith L, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19). Outbreak in January 2020 in China. Med Sci Monitor. (2020) 26:e923921. 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.State of New Hampshire Employee Assistance Program . Perceived Stress Scale. (2014). Available online at: Percieved Stress Scale.pdf (nh.gov) (accessed December 23, 2020). [Google Scholar]
- 19.Hawryluck L, Gold W, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marjanovic Z, Greenglass E, Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud. (2007) 44:991–8. 10.1016/j.ijnurstu.2006.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reynolds D, Garay J, Deamond S, Moran M, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. (2007) 136:997–1007. 10.1017/S0950268807009156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu W, Yuan L, Xu J, Xue F, Zhao B, Webster C. The Psychological Effects of Quarantine During COVID-19 Outbreak: Sentiment Analysis of Social Media Data. SSRN (2020). Available at: https://ssrn.com/abstract=3627268 (accessed December 23, 2020).
- 23.Wilder-Smith A, Chiew C, Lee V. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. (2020) 20:e102–7. 10.1016/S1473-3099(20)30129-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yan S, Xu R, Stratton TD, Kavcic V, Luo D, Hou F, et al. (2021). Sex differences and psychological stress: responses to the COVID-19 pandemic in China. BMC Public Health. 21:79. 10.1186/s12889-020-10085-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stevens J, van Rooij S, Jovanovic T. Developmental contributors to trauma response: the importance of sensitive periods, early environment, and sex differences. Curr Top Behav Neurosci. (2016) 38:1–22. 10.1007/7854_2016_38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldstein J, Jerram M, Abbs B, Whitfield-Gabrieli S, Makris N. Sex differences in stress response circuitry activation dependent on female hormonal cycle. J Neurosci. (2010) 30:431–8. 10.1523/JNEUROSCI.3021-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldstein J, Lancaster K, Longenecker J, Abbs B, Holsen L, Cherkerzian S, et al. Sex differences, hormones, and fMRI stress response circuitry deficits in psychoses. Psychiatry Res Neuroimaging. (2015) 232:226–36. 10.1016/j.pscychresns.2015.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pieh C, O'Rourke T, Budimir S, Probst T. Relationship quality and mental health during COVID-19 lockdown. PLoS ONE. (2020) 15:e0238906. 10.1371/journal.pone.0238906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yildirim M Kizilgeçit M Seçer I Karabulut F Angin Y Dagci A . et al. (2021) Meaning in life, religious coping, and loneliness during the coronavirus health crisis in Turkey. J Relig Health. (2020). 10.1007/s10943-020-01173-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomas J, Barbato M. Positive religious coping and mental health among christians and muslims in response to the COVID-19 pandemic. Religions. (2020) 11:498. 10.3390/rel11100498 [DOI] [Google Scholar]
- 31.Taylor M, Agho K, Stevens G, Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia's first outbreak of equine influenza. BMC Public Health. (2008) 8:347. 10.1186/1471-2458-8-347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cava M, Fay K, Beanlands H, McCay E, Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nursing. (2005) 22:398–06. 10.1111/j.0737-1209.2005.220504.x [DOI] [PubMed] [Google Scholar]
- 33.Jeong H, Yim H, Song Y, Ki M, Min J, Cho J, et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. (2016) 38:e2016048. 10.4178/epih.e2016048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Desclaux A, Badji D, Ndione A, Sow K. Accepted monitoring or endured quarantine? Ebola contacts' perceptions in Senegal. Soc Sci Med. (2017) 178:38–45. 10.1016/j.socscimed.2017.02.009 [DOI] [PubMed] [Google Scholar]
- 35.Osimo S, Aiello M, Gentili C, Ionta S, Cecchetto C. The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Front Psychol. (2021) 12:630751. 10.3389/fpsyg.2021.630751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moccia L, Janiri D, Pepe M, Dattoli L, Molinaro M, De Martin V, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. (2020) 87:75–9. 10.1016/j.bbi.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fiorillo A, Sampogna G, Giallonardo V, Del Vecchio V, Luciano M, Albert U, et al. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur Psychiatry J Assoc Eur Psychiatr. (2020) 63:e87. 10.1192/j.eurpsy.2020.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.