Abstract
Purpose:
To report a novel, telemedicine-friendly, smartphone-based, wireless anterior segment device with instant photo-documentation ability in the COVID-19 era.
Methods:
Anterior Imaging Module (AIM) was constructed based on a 50/50 beam splitter design, to match the magnification drum optics of slit-lamps with a three-step or higher level of magnification. The design fills the smartphone sensor fully at the lowest magnification and matches the fixed focus of the slit-lamp. It comes with a smartphone for instant photo-documentation, an in-built software application for data-management and secure HIPAA compliant cloud storage, and a Bluetooth trigger for a one-tap image capture. The construction of the device is explained, and the optical resolution measured using U.S. air-force resolution test. AIM’s performance was characterized with traceability to internationally relevant performance standards for digital slit-lamps after image quality assessment through a pilot study.
Results:
Clinically useful anterior segment images were obtained with both diffuse and slit illumination at different magnification settings with the highest magnification (40X) resolution of 359 lines per cm and the lowest magnification (16X) resolution of 113 lines per cm.
Conclusion:
AIM is a novel, wireless, telemedicine-enabled design that digitizes existing, analog slit lamps with at least three-step magnification. The settings ensure the focus is determined purely by the position of the slit-lamp. Hence, the image viewed and captured on the smartphone is exactly what the clinician sees through the eyepiece. This helps in maintaining distance from the patient in the ongoing COVID-19 pandemic, as well.
Keywords: Anterior segment imaging, conjunctiva, cornea, COVID-19, iris, lens, sclera, slit-lamp, smartphone, telemedicine, uniform illumination
Slit-lamp biomicroscopy (SLB) has been a crucial part of ophthalmic evaluation since the early twentieth century as it can provide vital information on the anterior segment structures and related pathologies. With advancements in technology and teleophthalmology platforms booming, objective image documentation is becoming a necessity. This will circumvent issues of manual recording which can be tedious, time-consuming and prone to errors. An instant, automated, photo-documentation process saves time and makes it hassle-free. A much-needed value addition for anterior segment devices is achieved by mounting commercial slit-lamp cameras, digital cameras or DSLRs on slit-lamps or using an adaptor to do so.[1,2,3,4,5] This results in quick capture of high-resolution images. Furthermore, these images can be easily transmitted for immediate consultation through teleophthalmology platforms from remote areas. Additionally, they can be used for patient education, resident training and photo-documentation for publications and conferences.[2,6] Instantaneous, objective digital imaging of anterior segment pathologies using commercial digital compact cameras have previously been validated to be at par with the clinical gold standards as well as slit-lamp cameras.[1,7] A digitized version of imaging brings about the advantage of improved data collection speed, processing power, and ease of storage of electronic data.[8] However, such methods are not devoid of their own set of shortcomings, like additional costs of installing high-end cameras on slit-lamps, training personnel to capture images seamlessly, needing separate screens to review images and the complexities of adapting to newer systems.[5]
Smartphones have been the forerunners of advanced, portable, and user-friendly technology. They are equipped with high-tech modalities, provide easy access to the internet that allow sharing of images across specified groups of people for dissemination of crucial information. These attributes make smartphones one of the most sought-after tools for telemedicine-based photo-documentation and expert consultation.[9] Photo-documentation is the sole determinant of an efficient teleophthalmology-based diagnosis and consultation system. The ease of image capture and quality of images are priorities while deciding on a device for anterior segment imaging. Smartphones with their advanced imaging capabilities, have been the choice of many ophthalmologists for use as a clinical tool and several studies have described the same.[10,11]
With countries easing lockdowns and re-opening clinics, the need of the hour are devices that allow non-emergency patients requiring semi-urgent care like post-operative follow-up or those with chronic ophthalmic conditions with vision disturbances be examined safely. This could be either via devices that support a teleophthalmology platform or in-clinic visits where safer distances can be maintained between the physician and patient.[12,13] In this paper, we describe one such novel, smartphone-based, teleophthalmology-enabled wireless, anterior segment imaging device called the Anterior Imaging Module (AIM).
Methods
Optical design and hardware
The AIM uses high-quality Anti-Reflection (AR) coated binocular optics, combined with a 50/50 beam splitter design, [Fig. 1] that matches the magnification drum optics of slit-lamps with a three-step or higher level of magnification. It can thus convert almost any modern-day slit lamps to a digital one. The design fills the smartphone sensor fully and does not require separate adjustments to focus on the eye due to variation in distance between the camera and the eyepiece on the slit-lamp [Fig. 2a and b]. The optical design is simple and is constructed in a way such that the fixed focus of the slit-lamp drives the focus of the smartphone [Fig. 2c]. An Apple iPhone 6S, (Apple Inc., California, USA), is used in this regard. It can also be used with higher models of the iPhone like 7, 8, and XR. A Bluetooth trigger helps in instant capture of the images with just one tap on the trigger. This saves efforts on the doctor’s part from having to reach out for the capture button on the iPhone and shifting focus from the eyepiece. The overall design of AIM makes it a portable, hassle-free, wireless, anterior-segment imaging device.
Figure 1.

Optical Design of Anterior imaging Module (AIM)
Figure 2.

(a) Hardware Design of Anterior imaging Module (AIM). (b) AIM mounted on a conventional slit-lamp. (c) Anterior segment imaging on AIM
The settings in AIM application ensure that the focus is determined purely by the position of the slit-lamp. The plane of focus on the phone can be adjusted according to the structure being imaged. When one moves the slice of focus further towards the desired structure, it creates a shallow focus effect in front and behind the focal point, giving it a layered effect. As shown in Fig. 3a and b, the plane of focus has been adjusted to view the iris and the cornea respectively, at a magnification of 25X. On the other hand, imaging using gonio lenses for angles often requires extremely narrow depth of focus setting. This is often difficult to capture as the joystick wheelbase of the slit-lamp may not support such small depth of focus imaging. In such cases, the clinician can use the AIM software application to control the multi-element voice coil motor on the smartphone to capture a sharp image [a gonio image is later illustrated in Fig. 4e]. This application ensures that the image viewed and captured on the smartphone is exactly what the clinician sees through the eyepiece. This is an important feature given the current COVID-19 pandemic, wherein the physician can maintain a safer distance from the patient by viewing the phone directly without having to view through the eyepiece [Fig. 5]. A universal design requires that the image seen on the smartphone matches that seen on the eyepiece of the slit-lamp, irrespective of the light source used – halogen, warm white or cool white LED. This is achieved using the saturation temperature settings in the application that allows the image color to match the color temperature of the light source used.
Figure 3.
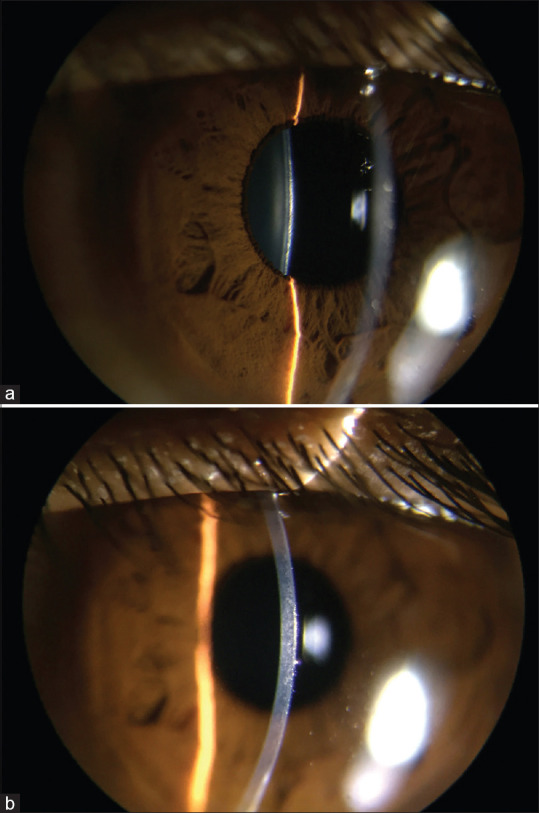
(a) Anterior Segment image showing the plane of iris and lens in focus. (b) Anterior Segment image showing the plane of cornea in focus
Figure 4.
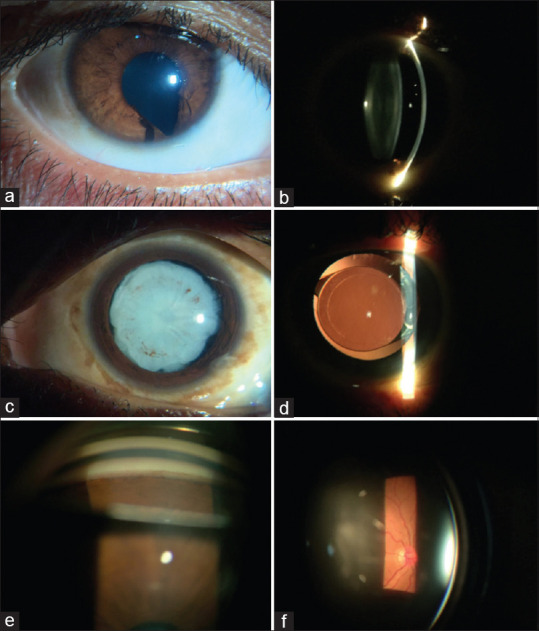
(a) Diffuse illumination showing a congenital infero-nasal Coloboma (25X). (b) Optical section showing a clear lens (25X). (c) Diffuse illumination depicting a hyper mature sclerotic cataract with iris pigments on anterior lens surface (25X). (d) Retro illumination showing a well-centered capsulorhexis with single piece posterior chamber IOL in the capsular bag (16X). (e) Gonioscopy showing an open inferior angle up to ciliary body band with a possible neovascularization of the angle (25X). (f) Slit-lamp biomicroscopy with a 90D volk lens showing a healthy optic disc (25X)
Figure 5.

AIM can effectively increase the physical distance between patient and examiner in the current COVID-19 pandemic
Software
The built-in patient-management software offers the convenience of instantaneous capture and unlimited storage of patient data securely on a HIPAA compliant cloud server powered by Amazon Web Services (Amazon.com, Inc., Seattle, USA). A customized desktop-based interface can be provided additionally to support a DICOM-based transfer for institutes with a centralized EMR/PACS system. The AIM software is teleophthalmology enabled and allows seamless data transfer and generation of immediate reports. The application can also be integrated with third-party video conferencing software for live consultation through the screen-sharing facility.
AIM is manufactured under ISO 13485 Quality Management Systems and is compliant with all standards pertaining to quality, risk management and safe use of ophthalmic devices, including ISO 15004-1, ISO 15223-1, ISO 14971, IEC 62304:2006 + A1:2015, IEC 62366:2007 + A1:2014, & 1041:2008 + A1:2013.
To report the usefulness of this anterior segment imaging device in photo-documentation of clinical findings, we mounted the AIM on the binocular eyepiece of an affordable Labomed eVO 300 slit-lamp (Labo America Inc., California, USA). This model of AIM used the iPhone 6S (Apple Inc., California, USA) which uses Sony RGBW IMX315 12MP BSI sensor (Sony Corporation or Sonī Kabushiki Kaisha, Tokyo, Japan) of 1/3″ (4.80 x 3.60 mm) allowing capture of images with a maximum resolution of 4032 × 3024 pixels (~12 megapixels). It has a higher pixel density with a pixel dimension of 1.22 mm in comparison to previous iPhone models. We chose a low-cost iPhone like the 6S rather than the XR in order to keep the price of the entire system low. The optical design of AIM adds an additional 4.0901X magnification to the in-built magnification of the slit-lamp. A 1.33X digital zoom feature is also enabled on the AIM software to be used as per the physician’s choice. With an aperture of ƒ/2.2, AIM has a depth of field of 0.05743 mm (57.4 mm). This ensures that physicians can view layers that are at least 57 mm apart, clearly on the phone and capture high quality images, helping in differentiating between planes of the anterior segment. A resolution test card (U. S. Air Force 1951, Edmund Optics, Inc, Barrington, NJ) was used to test the spatial resolution at different magnification levels on the slit-lamp with the AIM digital attachment. Fig. 6a-c shows the clarity of all the elements of the test card when observed on the iPhone 6S screen, with a resolution of 750 x 1334 pixels, at a 16:9 ratio and a pixel density of ~ 326 ppi [Table 1].
Figure 6.
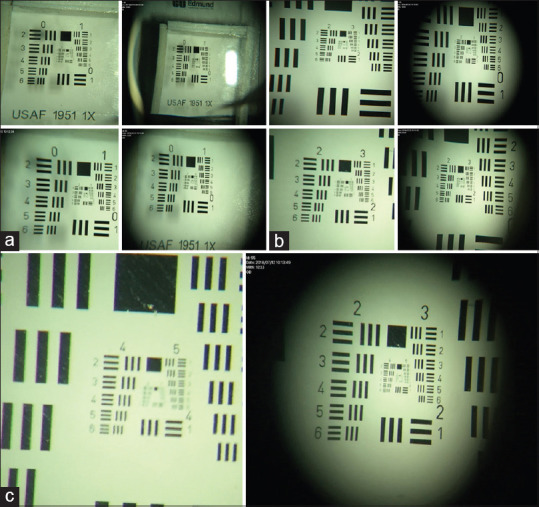
(a) Airforce Resolution Test for 6.5X (Row 1) and 10X magnification (Row 2). (b) Airforce Resolution Tests for 16X (Row 1) and 25X magnification (Row 2). (c) Airforce Resolution Tests for 40X magnification
Table 1.
Airforce Test Results for Different Levels of Magnification
| Magnification | Group | Element | Lines per cm |
|---|---|---|---|
| 6.5x | 2 | 6 | 71.27 |
| 10x | 3 | 1 | 80.00 |
| 16x | 3 | 4 | 113.14 |
| 25x | 4 | 6 | 285.09 |
| 40x | 5 | 2 | 359.17 |
AIM is an FDA 510(k) exempted, class I device with a CE mark, which does not have an internal light source and hence did not need additional safety clearances. Hence, an informed, written consent from patients for capture of pathology images was deemed suitable by the authorities at Aravind Eye Hospital, Pondicherry, for demonstrating AIM’s capacity to document high-quality photos. The study was carried out after an approval from the Ethics Committee of the hospital and was performed in accordance with the tenets of the Declaration of Helsinki. A pilot study enrolled 20 consecutive patients attending the hospital. Patients who were unable to co-operate for imaging due to acute pain and hypersensitivity to light were excluded. An ophthalmologist captured one image per patient with an imaging protocol (diffuse or slit illumination with standard settings). Post our image acquisition, we assessed the images on the basis of clinical utility and compared the image quality with those captured on a high-end slit lamp, Topcon SL-D701 (Topcon Corporation, Tokyo, Japan). Images captured on the same 20 patients with same imaging protocol on the Topcon SL – D701 were chosen from the hospital’s database and used for comparison and assessment. All the images were deidentified and sent for grading by a certified ophthalmologist who was blinded to the devices. A scale of 1-5 was used to assess the image quality. Images were graded as below:
Poor- Significant defocus/blur or under/over exposure or artifacts/others involving more than half of the image. Image quality insufficient for any interpretation
Fair- Significant defocus/blur or under/over exposure or artifacts/others involving half of the image. Image interpretation difficult
Good- Defocus/blur or under/over exposure or artifacts/others involving 1/3rd to less than half of image. Image interpretation possible
Very good- peripheral 1/3rd of image showing defocus/blur or under/over exposure or artifact/others. No issue with image interpretation
Excellent – No issue with any image quality factor or image interpretation
An image with a quality score of 3 and above was deemed ‘clinically useful’. An image with a quality score below 3 was considered as ‘clinically not gradable’. An agreement (Kappa statistic) was calculated for image quality of ‘clinically useful’ images between two devices on the basis of the ophthalmologist’s grading.
Results
We captured 20 images of the same patients in each device at Aravind Eye Hospital and have illustrated a selection of different pathologies obtained on AIM. Keeping the ISO set at 100 and using magnifications of 16X, 25X and 40X, anterior segment images were obtained. The maximum field of view achieved in this process was 16 mm.
The images captured [Fig. 4a-f and 7a-h] show different pathologies right from the ocular surface up to the lens. A conjunctival cyst in the lower fornix as well papillary changes in the upper tarsal conjunctiva are depicted in Fig. 7a and b, respectively. Pathologies in different layers of the cornea are well documented [Fig. 7c-g]. Anterior chamber showing emulsified silicone oil as an inverted hypopyon is shown in Fig. 7h. Iris & lens details are also well captured as seen in Fig. 4a-c, respectively. The retro-illumination image depicts the details of the capsular bag and posterior chamber intra-ocular lens in Fig. 4d. The ease of use AIM is highlighted by the fact that it can be combined alongside other examination techniques like gonioscopy [Fig. 4e] to visualize the angle structures as well as slit-lamp biomicroscopy with an appropriate lens [Fig. 4f] to examine the optic disc and macula.
Figure 7.
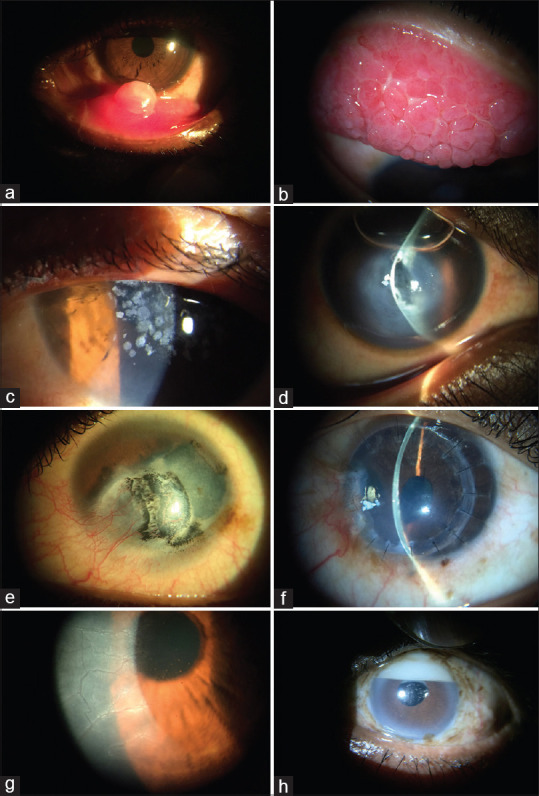
(a) Conjunctival cyst in lower fornix (16X). (b) Upper tarsal conjunctiva showing a cobblestone appearance seen in giant papillary conjunctivitis (25X). (c) Granular corneal dystrophy showing discrete bread crumb-like opacities in the central anterior stroma of the cornea (40X). (d) Slit-image depicting a case of corneal hydrops following a break in Descemet’s membrane leading to corneal edema, managed with intracameral injection of air (25X). (e) Diffuse illumination showing a corneal scar with residual tattoo pigments (25X). (f) Slit illumination showing Post penetrating keratoplasty graft rejection (25X). (g) Indirect illumination under high magnification showing pigmented keratic precipitates on the corneal endothelium and ghost vessels (40X). (h) Emulsified silicone oil in the superior portion of the anterior chamber manifests as an “inverted hypopyon” or “hyperoleon” (25X)
All images from both devices got an image quality score ≥3 showing that all images qualified as being ‘clinically useful’. Hence, the agreement (Kappa statistic) between both devices for image quality of clinically useful images was 1.
Discussion
The primary thought behind designing AIM is high-quality, instantaneous, easy to use, objective photo-documentation of anterior segment pathologies. We found that it was possible to use a smartphone to capture and document images without compromising on the quality. Owing to its unique design, AIM fits into the binocular eyepiece of any slit-lamp with a magnification of 3X and higher, converting the same to a digital slit-lamp. In doing so, it effectively minimizes the wiring hassles faced while using a digital camera, adapter, computer, monitor, multiple cables, keyboard, and mouse, separately. In comparison to other available monocular adapters,[14] the AIM has a universal design made to fit exactly into the smartphone sensor, requiring no additional adjustments between the eye piece and the slit-lamp. The plane of focus can be adjusted to visualize the lens, cornea, iris, or eyelids/lashes, or even the angles, as desired. It helps in capturing a sharper image of the particular structure or differentiate between different planes of the anterior segment. The ease of photo-documentation is amplified due to a Bluetooth trigger that allows instant capture of the image without shifting focus from the eyepiece. These features make anterior-segment imaging on AIM, a unique, compact, wireless, and portable, user-friendly experience. Since the phone captures exactly what is seen on the eyepiece, the doctor can see the phone and confirm findings on the spot. Objective photo-documentation for progressive eye diseases like corneal ulcers or swellings can also help in avoiding errors encountered during manual documentation processes.[6] The use of screen mirroring with Apple TV (Apple Inc, CA, USA), allows for the images to also be seen with minimal lag, wirelessly on Smart TVs for the education of the patient along with training of residents. With an integrated, holistic, image management software and a HIPPA compliant cloud server, ease of use and data security have been made a priority. One can adjust the light-settings to suit the ambient light conditions while capturing the photograph using the AIM application. In cases where patients face constraints in traveling for a specialist consultation, the application can be integrated with any third-party video-conferencing applications (such as Zoom, Google Meet etc.). The technician attending the patient can share screen while using the video-conferencing application on the phone, sharing the images live with the specialist and get an opinion on the spot. This makes the setup teleophthalmology-friendly.
Smartphones have made for efficient clinical tools and have shown to produce high-quality images in anterior imaging.[10] Data show a considerable rise in smartphone use among population in developing nations from a median of 21% in 2013 to 37% in 2015. This supports the trend of smartphone-cent red ocular examination with increased accessibility in terms of both cost and convenience to underserved populations.[15] Studies have also revealed that operating smartphone-based diagnostic devices require significantly lesser levels of training and skillsets, which reduces the labor-related costs, otherwise borne by vision centers. The quality of the images captured does remain subjective of the technician but is largely acceptable for analysis by professionals.[15]
There have been studies showing the reproducibility of images taken using an iPhone[5] with those captured by standard anterior segment cameras (a slit-lamp BP 900® (Haag-Streit, USA) with custom-mounted 6.3-megapixel Canon® EOS 10D digital single-lens reflex camera (Canon, Japan)) using the validated Lens Opacification Classification System III (LOCS III).[10] The image quality of iPhone camera was superior to the professional slit-lamp camera in some aspects whereas it was comparable to the others.[10] This study also highlighted that securing a smartphone on a slit-lamp through a telescopic mount, significantly reduced shake and improved photo usability adding to the ease of anterior segment imaging.[9] It should be kept in mind that the cost of professional slit-lamp cameras ranges from upwards of USD 15,000.[5,16] Mounting CCD or other professional DSLR cameras can cost upwards of USD 1000 in addition to the cost of adapters,[5] and there is the additional cost of needing a computer and screen as well. In these cases, smartphones have been shown to be a more dependable and affordable alternative for anterior imaging, even in terms of picture quality at only a fraction of the cost of professional slit-lamp cameras. Studies have shown that iPhone 4S produces nearly as good images as the Sony HD camera and the Nikon and Sony VGA cameras as well. Hence, combining their picture quality to the ease of internet connectivity and synchronization, smartphones vouch for the most dependable, telemedicine-friendly options for anterior segment imaging for the masses. The current COVID-19 pandemic also warrants simple, user-friendly devices that can be used for the masses, ensuring optimum safety.[5]
Commercially available slit-lamp adapters that attach to any of the eyepieces, like EyePhotoDoc, Zarf iPhone Adaptor, Magnifi iPhone adaptor, Steady iPix Telescope Photo adaptor for iPhone, iExaminer, Tiger Lens and Skylight are available from USD 75.00 to USD 520.00.[17] Using DIY adapters for smartphones, as demonstrated by Akkara et al.[18,19] can be useful alternatives. However, they come at the cost of not filling the sensor fully, and not being able to match the focus exactly of the slit-lamp and the smartphone. Additionally, it requires the smartphone and adaptor to be taken out each time the ophthalmologist or technician wishes to use the binocular eyepiece for viewing, making it cumbersome to use. This approach often needs a variation in the position of the smartphone from the eyepiece, customization for the aperture and diameter of the eyepiece, depending on the magnification of the eyepiece, leading to smaller fill of the smartphone sensor, lower resolution images and non-uniformly illuminated images. In case of universal phone holders, the doctor must use his own phone with no built-in patient management software or cloud storage; moreover, the doctor might be interrupted during his examination due to incoming calls or messages. The AIM overcomes all these issues, being a certified, professional anterior segment imaging device. AIM balances the resource constraints, quality, and accessibility parameters in the best possible way in the present situation. One limitation is that it can only be used to differentiate between structures with a minimum distance of 57 mm between them. Hence, micro-details like the corneal endothelial cells with an average size of 10–20 mm,[20] cannot be viewed through AIM. However, with newer models of phones beyond the iPhone 6 – such as iPhone 7,8, XR and SE de-noising algorithms may help improve the digital resolution of the system.
Conclusion
In conclusion, with the experience that the current COVID-19 pandemic has brought on, the world is moving towards a teleophthalmology integrated practice where devices like AIM make anterior segment imaging and photo-documentation more accessible and affordable without compromising on quality. Thus, devices like AIM are paving the way for harnessing the true potential of smartphone-based devices in ophthalmology.
Financial support and sponsorship
Nil.
Conflicts of interest
Sreetama Dutt, Shanmuganathan Nagarajan, Siva S Vadivel, Amrutha Galagali, Divya Parthasarathy Rao, and Anand Sivaraman are all employees of Remidio Innovative Solutions Pvt. Ltd.
Acknowledgements
We would like to acknowledge the contributions of Mr. Adeeb Ulla Baig, Mr. Timi Thomas, Mr. Mathew Dominic, Mr. Venkatesh S. and Mr. Vighnesh MJ from Remidio Innovative Solutions Pvt. Ltd. for helping us out with acquisition of images.
References
- 1.Oliphant H, Kennedy A, Comyn O, Spalton DJ, Nanavaty MA. Commercial slit lamp anterior segment photography versus digital compact camera mounted on a standard slit lamp with an adapter. Curr Eye Res. 2018;43:1290–4. doi: 10.1080/02713683.2018.1490435. [DOI] [PubMed] [Google Scholar]
- 2.Mohan A, Kaur N, Sharma V, Sen P, Jain E, Gajraj M. Ophthalmologists on smartphones:Image-based teleconsultation. Br Ir Orthopt J. 2019;15:3–7. doi: 10.22599/bioj.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin R. Cornea and anterior eye assessment with slit lamp biomicroscopy, specular microscopy, confocal microscopy, and ultrasound biomicroscopy. Indian J Ophthalmol. 2018;66:195–201. doi: 10.4103/ijo.IJO_649_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konstantopoulos A, Hossain P, Anderson DF. Recent advances in ophthalmic anterior segment imaging:A new era for ophthalmic diagnosis? Br J Ophthalmol. 2007;91:551–7. doi: 10.1136/bjo.2006.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye Y, Jiang H, Zhang H, Karp CL, Zhong J, Tao A, et al. Resolution of slit-lamp microscopy photography using various cameras. Eye Contact Lens. 2013;39:205–13. doi: 10.1097/ICL.0b013e318286bc0f. [DOI] [PubMed] [Google Scholar]
- 6.Patel TP, Prajna NV, Farisu S, Valikodath NG, Niziol LM, Dudeja L, et al. Novel image-based analysis for reduction of clinician-dependent variability in measurement of corneal ulcer size. Cornea. 2018;37:331–9. doi: 10.1097/ICO.0000000000001488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar S, Yogesan K, Constable IJ. Telemedical diagnosis of anterior segment eye diseases:Validation of digital slit-lamp still images. Eye. 2009;23:652–60. doi: 10.1038/eye.2008.11. [DOI] [PubMed] [Google Scholar]
- 8.Bennett TJ, Barry CJ. Ophthalmic imaging today:An ophthalmic photographer's viewpoint-A review. Clin Experiment Ophthalmol. 2009;37:2–13. doi: 10.1111/j.1442-9071.2008.01812.x. [DOI] [PubMed] [Google Scholar]
- 9.Mohammadpour M, Mohammadpour L, Hassanzad M. Smartphone assisted slit lamp free anterior segment imaging:A novel technique in teleophthalmology. Contact Lens Anterior Eye. 2016;39:80–1. doi: 10.1016/j.clae.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Chen DZ, Tan CW. Smartphone imaging in ophthalmology:A Comparison with traditional methods on the reproducibility and usability for anterior segment imaging. Ann Acad Med Singap. 2016;45:6–11. [PubMed] [Google Scholar]
- 11.Wintergerst MWM, Jansen LG, Holz FG, Finger RP. Smartphone-based fundus imaging–Where are we now? Asia-Pac J Ophthalmol. 2020;9:308–14. doi: 10.1097/APO.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 12.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology:Telemedicine in a COVID-19 era. Am J Ophthalmol. 2020;216:237–42. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sommer AC, Blumenthal EZ. Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol. 2020;258:2341–52. doi: 10.1007/s00417-020-04879-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.David Myung MP, Alexandre Jais MD, Lingmin He MM, Robert T, Chang MD. Simple, low-cost smartphone adapter for rapid, high quality ocular anterior segment imaging:A photo diary. J Mob Technol Med. 2014;3:2–8. [Google Scholar]
- 15.Ludwig CA, Newsom MR, Jais A, Myung DJ, Murthy SI, Chang RT. Training time and quality of smartphone-based anterior segment screening in rural India. Clin Ophthalmol. 2017;11:1301–7. doi: 10.2147/OPTH.S134656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuan J, Jiang H, Mao X, Ke B, Yan W, Liu C, et al. Slit-lamp photography and videography with high magnifications. Eye Contact Lens. 2015;41:391–7. doi: 10.1097/ICL.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan JB, Ho HC, Ngah NF, Hussein E. DIY-Smartphone slit-lamp adaptor. J Mob Technol Med. 2014;3:16–22. [Google Scholar]
- 18.Akkara JD, Kuriakose A. How-to guide for smartphone slit-lamp imaging. Kerala J Ophthalmol. 2019;31:64–71. [Google Scholar]
- 19.Akkara JD. Commentary:Dawn of smartphones in frugal ophthalmic innovation. Indian J Ophthalmol. 2018;66:1619. doi: 10.4103/ijo.IJO_1002_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y, Fu Z, Liu J, Li M, Zhang Y, Wu X. Corneal endothelial characteristics, central corneal thickness, and intraocular pressure in a population of Chinese age-related cataract patients. J Ophthalmol. 2017;2017:1–8. doi: 10.1155/2017/9154626. [DOI] [PMC free article] [PubMed] [Google Scholar]


