Abstract
Purpose:
Patients with glaucoma undergoing trabeculectomy develop bleb cicatrix causing poor postoperative intraocular pressure (IOP) control and low success rates. Several approaches have been explored over the years for better outcomes. This study assesses the safety, efficacy, and outcome of trabeculectomy with HealaFlow® (Anteis S. A, Geneva, Switzerland), a high-molecular-weight cross-linked hyaluronic acid viscoelastic gel, and comparing it with the antimetabolite Mitomycin-C (MMC).
Methods:
A prospective, interventional, case-controlled study conducted at a tertiary care hospital in Southern India on 60 eyes of patients requiring trabeculectomy divided in two groups – HealaFlow scleral implant and adjuvant low-dose MMC (0.1 mg/mL). Postoperative IOP reduction along with bleb morphology was assessed over follow-up at 1 week, 1 month, 3 months, 6 months, and 12 months.
Results:
Preoperatively IOP in the two groups was statistically similar. Postoperative IOP on day 1 had statistically significant reduction in both groups with greater reduction in MMC group. However, by 12 months, the IOP reduction was statistically similar in both groups, i.e., 46.24% (to 11.04 ± 2.55 mmHg) and 54.47% (to 11.99 ± 3.37 mmHg) in HealaFlow® group and MMC group, respectively (P > 0.05). The bleb morphologies were similar and complications were seen equally, which resolved by 4 weeks. A complete success rate of 89.29% and a qualified success rate of 10.71% were observed equally in both groups.
Conclusion:
Absorbable biosynthetic cross-linked hyaluronic acid and low-dose MMC are equally safe and efficacious in trabeculectomy with significant IOP reduction and good bleb morphology. Therefore, it is a novel substitute for MMC.
Keywords: Glaucoma, hyaluronic acid, mitomycin-C, trabeculectomy
Glaucoma is the leading cause of global irreversible blindness and the second most leading cause of blindness.[1] The global prevalence of glaucoma for population aged 40–80 years is 3.54%.[2] Glaucoma treatment has to be a holistic approach with detection and management of all potential causes and prevention of blindness from glaucoma.
Trabeculectomy, initially described by Cairns in 1968[3] and later modified by Watson in 1970,[4] has traditionally been considered the “gold standard” for filtration surgery, i.e., to increase aqueous outflow through a surgical fistula into the subconjunctival space.
Over the past few decades, trabeculectomy has undergone an evolution of modifications and supplementations to improve postoperative outcomes with fewer complications. The success rates of trabeculectomy can be improved by delaying wound healing process and by inhibiting inflammation and fibroblastic activity by antimetabolites, such as Mitomycin-C (MMC) and 5-fluorouracil.[5] However, antimetabolites have been associated with several postoperative complications but are still being widely used.[6]
Recent studies have shown promising effects of subconjunctival antivascular endothelial growth factor agents with possible antiangiotic and antifibrotic actions; however, it is still under research.[7,8] Other substances such as monoclonal antibodies against transforming growth factor-b2 have unfortunately not proven to be effective.[8]
Over the years, as surgeons explored novel substitutes for optimal modulation of wound healing, sodium hyaluronate turned out to be a promising alternative. HealaFlow® (Anteis S. A, Geneva, Switzerland), a cross-linked sodium hyaluronate, is a highly viscous, nonanimal origin, biodegradable product with antiinflammatory and antifibrotic properties. Due to the physical factors such as steric hindrance by the continuous polymeric network along with hydrophilic polysaccharide nature, it provides an unsuitable surface; therefore, high-molecular-weight sodium hyaluronate (4.6 × 105–2.8 × 106) inhibits phagocytosis and has space occupying characteristics.[9] Sodium hyaluronate also has shown to inhibit the interferong induced release of inflammatory factors, such as tumor necrosis factoralpha, interleukin (IL1b) and improves ocular surface irregularity and staining along with reduction in the percentages of CD4 (+), CXCR3 (+), CD 40 (+), and CD44 (+) cells in the conjunctiva.[10]
Therefore, this study was carried out to assess the safety, efficacy, and outcome of a slowly reabsorbable cross-linked form of hyaluronic acid (HealaFlow®) scleral implant during trabeculectomy in a tertiary care hospital in Southern India and observe the complications. This substance has been proposed to prevent postoperative scarring and fibrosis of the filtration site to maintain a functional filtration.
Methods
The study was a prospective, interventional, case-controlled study conducted from November 2017 to December 2019 at a tertiary care hospital in Southern India and patients were followed up for 12 months. Approval was obtained from the local Committee on Research Ethics, and informed consent according to the tenets of the Declaration of Helsinki was obtained from all subjects.
Patients were considered eligible, provided they met the inclusion criteria (age >18 years, glaucoma requiring trabeculectomy for IOP control, no previous intraocular surgery). Data from only the selected eye of each eligible patient were used for the study.
Patients were excluded from the analysis if there was history of neovascular, uveitic, and posttraumatic glaucoma or uncooperative attitude, i.e., unable to understand and follow verbal commands (children, mentally challenged, involuntary movements), patients with retinal pathology or previous laser procedures for glaucoma.
Sample size was calculated by using G*Power software. There were two groups in the study. By assuming medium effect size as 0.1, 5% level of significance, power 80%, nonsphericity correction ɛ taken as 1 (by assuming data follows sphericity assumption) and by assuming 0.7 correlation present between repeated measures, sample size was obtained as 30 subjects in each group.
With random computerized distribution, the patients were divided equally into two groups based on adjuvant used: Group A – Cross-linked hyaluronic acid (HealaFlow®) scleral implant, and Group B – Low dose MMC (0.1 mg/mL).
Preoperative Characteristics: Preoperative characteristics were age, gender, type of glaucoma, IOP, visual acuity and compliance, adherence, and effect of antiglaucoma medications.
Intraoperative Characteristics: Intraoperative characteristics were surgical technique and occurrence of any intraoperative complications. The number of cases undergoing combined trabeculectomy was equally distributed in both groups.
Postoperative Characteristics: Postoperative characteristics were IOP, complications, and postoperative glaucoma medications used.
Outcome: The following were followed for defining primary outcome:
Complete success: Postoperative IOP ≤21 mmHg and ≥5 mmHg or a reduction in preoperative IOP of ≥ 20% without antiglaucoma medication.
Qualified success: Postoperative IOP ≤21 mmHg and ≥5 mmHg or a reduction in preoperative IOP of ≥20% with antiglaucoma medication.
Failed surgery: Postoperative IOP >21 mmHg and <5 mmHg or a reduction in preoperative IOP <20% even with antiglaucoma medication or the need for additional surgery including needling or bleb revision on two consecutive study visits.
Secondary study outcomes included the postoperative complications. Bleb was graded as per the Moorfields Bleb Grading.
Surgical Technique: All surgeries were performed by single surgeon. After peribulbar anesthesia with lignocaine 1%, the eye was prepared and draped. A 4-0 silk superior rectus suture was taken, and a fornix-based conjunctival flap was raised. A partial thickness rectangular scleral flap of approximately 4 × 4 mm was raised. For the patients in MMC category, MMC soaked gel-sponges (0.1 mg/mL) were placed for 2 min followed by thorough wash. Lens extraction was carried out by phaco-emulsification (in combined trabeculectomy cases). Thorough wash of viscoelastic substance was performed. After maintaining anterior chamber with air, sclerostomy of 1 × 3 mm was performed with Vanna’s scissors/Kelly’s punch followed by a peripheral iridectomy. The scleral flap was sutured with two 10-0 nylon sutures, one in each corner.
For patients in HealaFlow® group, just before conjunctival closure, 0.05 mL of HealaFlow® was injected under the scleral flap ensuring no spillage in the anterior chamber (to prevent postoperative IOP spikes), and a larger amount 0.1–0.4 mL was injected between the sclera and conjunctiva and air tight conjunctival sealing was done with 8-0 vicryl. Subconjunctivally dexamethasone and gentamicin were injected. Postoperatively, a topical fixed combination of chloramphenicol, polymyxin B, and dexamethasone 1 mg/mL was administered six to eight times daily for 4 weeks and then gradually tapered. Homatropine 1% eye drops were used two times daily for 2 weeks.
Statistical Analysis: Data were analyzed using statistical software R 3.6.3 and Excel. Demographic, preoperative data, and postoperative complications were analyzed using x2 test. IOP comparisons within the groups were done by Friedman’s test. Surgical success has been demonstrated by Kaplan Meier survival curve [Fig. 1b]. To compare mean/distributions, t-test/Mann–Whitney test was used. QQ plot/Shapiro-Wilk’s test were used to check the normality of variables. Statistically significant level was set at P ≤ 0.05.
Figure 1.
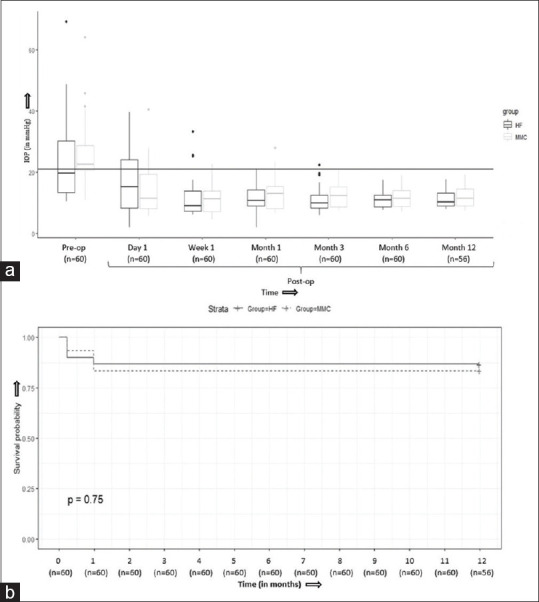
(a) Distribution of mean IOP on follow-up visits (b) Kaplan–Meier survival curve at 12 months for complete success(IOP ≤21 mmHg and ≥5 mmHg) (HF-HealaFlow®, MMC-Mitomycin-C)
Results
Sixty eyes of consecutive eligible patients who were matched for age, gender, visual acuity, laterality, glaucoma type, and preoperative IOP were enrolled in the study and were divided equally as per random computerized distribution into two groups based on adjuvant used: Group A- HealaFlow®, Group B – Low dose MMC with 30 patients in each group. A 12 months follow up was performed as per the inclusion criteria. A loss to follow up of four eyes at 12 months was observed [Flow Chart 1].
Flow Chart 1.
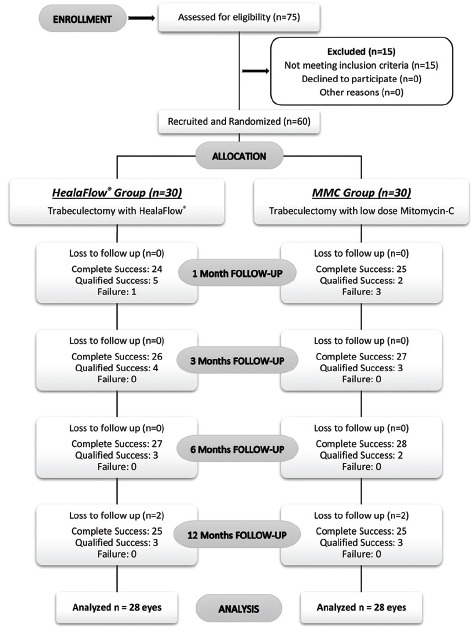
The enrollment, randomization and the success rate at different follow-ups in the two groups
Preoperative Characteristics: Demographic and preoperative data have been summarized in Table 1 of both groups. The HealaFlow® group had a mean age range of 67.63 ± 8.86 years, whereas the MMC group had a mean age range of 69.96 ± 11.01 years. There was a higher male predisposition with an M: F ratio of 1.72:1. Majority of the patients were diagnosed with POAG, i.e., 46 (76.67%) patients; however, the distribution in the two groups was statistically similar. Preoperatively, the IOP in the HealaFlow® group was 23.59 ± 13.81 mmHg, and in the MMC group, it was 25.81 ± 11.01 mmHg.
Table 1.
Demographic and preoperative characteristics of HealaFlow® and MMC group
| HealaFlow® Group | MMC Group | P | |
|---|---|---|---|
| Number of eyes | 30 | 30 | |
| Age (years) | |||
| Mean (±SD) | 67.63 (±8.86) | 69.96 (±11.00) | 0.786 |
| Range | 31-79 | 31-80 | |
| Gender | |||
| Female | 12 (40%) | 10 (33.33%) | |
| Male | 18 (60%) | 20 (66.67%) | 0.788 |
| Diagnosis | |||
| ACG | 4 (13.33%) | 5 (16.67%) | |
| NTG | 4 (13.33%) | 2 (3.33%) | 0.4508MC |
| POAG | 22 (73.33%) | 23 (38.33%) | |
| Preoperative IOP (mmHg) | |||
| Mean (±SD) | 23.60 (±13.81) | 25.81 (±11.01) | 0.133 |
| Range | 10-69 | 10-64 |
MC: Monte-Carlo’s simulation used to obtain P
Intraoperative Characteristics: No intraoperative complications were observed in either of the groups.
Postoperative Characteristics: The mean IOP in both the groups during the follow-up visits has been listed in Table 2 and graphically described in Fig. 1a. No statistical difference was observed in the reduction rate between the two groups. On day 1 postoperatively, there was IOP reduction of 30.09% (to 16.50 ± 9.92 mmHg) and 44.59% (to 14.29 ± 8.01 mmHg) in the HealaFlow® group and the MMC group, respectively. By 12 months, the trend of IOP fall remained statistically similar in both the groups, i.e., 46.24 (to 11.04 ± 2.55 mmHg) and 54.47% (to 11.99 ± 3.37 mmHg) in the HealaFlow® group and MMC group, respectively.
Table 2.
Comparison of IOP reduction from preoperative IOP on follow-up visits in the HealaFlow® and MMC group
| HealaFlow® Group (mmHg) (n=30) | MMC Group (mmHg) (n=30) | Percentage Reduction from Pre-op IOP | ||
|---|---|---|---|---|
| HealaFlow® Group (%) | MMC Group (%) | |||
| Post-operative IOP | 16.50±9.92 | 14.29±8.01 | 30.09% | 44.59% |
| Day 1 IOP Week 1 IOP |
11.63±6.52 | 11.40±4.72 | 50.69% | 55.83% |
| Month 1 IOP | 11.55±4.16 | 12.95±5.27 | 51.10% | 49.82% |
| Month 3 IOP | 11.22±4.03 | 12.35±3.79 | 52.5% | 52.15% |
| Month 6 IOP | 10.87±2.43 | 11.74±3.36 | 53.94% | 54.51% |
| Month 12 IOP* | 11.04±2.55 | 11.99±3.37 | 46.24% | 54.47% |
*n=28 in each group
Primary Outcome: Table 3 depicts the outcome of surgery, and it was observed that both groups had similar outcomes, i.e., complete success 89.29% and qualified success 10.71% & was distributed uniformly in both the groups with four cases (two cases each for group) as loss to follow up at 12 months.
Table 3.
Assessment of bleb morphologies, outcomes, and complications in the HealaFlow® and MMC group at 12 months
| Variables | Group | P | ||
|---|---|---|---|---|
| HealaFlow® (n=28) (%) | MMC (n=28) (%) | |||
| Outcome | Complete success | 25 (89.29%) | 25 (89.29%) | 1MC |
| Qualified success | 3 (10.71%) | 3 (10.71%) | ||
| Complications | Nil | 25 (89.29%) | 25 (89.29%) | 1MC |
| Hyphaema | 2 (7.14%) | 2 (7.14%) | ||
| Subconjunctival hemorrhage under bleb | 1 (3.57%) | 1 (3.57%) | ||
| Central bleb area | 25% | 22 (78.57%) | 18 (64.29%) | 0.2367 |
| 50% | 6 (21.43%) | 10 (35.71%) | ||
| Peripheral bleb area | 0% | 8 (28.57%) | 11 (39.29%) | 0.3972 |
| 25% | 20 (71.43%) | 17 (60.71%) | ||
| Bleb height | Low | 11 (39.29%) | 4 (14.29%) | 0.1068 |
| Flat | 4 (14.29%) | 6 (21.43%) | ||
| Moderately elevated | 13 (46.43%) | 18 (64.29%) | ||
| Bleb Vascularity | Normal | 13 (46.43%) | 13 (46.43%) | 0.7575 |
| Mild | 5 (17.86%) | 7 (25%) | ||
| Avascular | 10 (35.71%) | 8 (28.57%) | ||
MC: Monte-Carlo’s simulation used to obtain P
The Kaplan–Meier curve in Fig. 1b shows that there is no significant difference between the survival probabilities over the two groups by log rank test (x2 = 0.1, P value: 0.75). Complete success was taken as the event of interest.
Secondary Outcome: Table 3 gives a comparison of post-operative complications in the HealaFlow® and MMC group and it was seen that there were two cases (7.14%) of hyphaema and one case (3.57%) of sub-conjunctival hemorrhage under bleb in both the groups equally which resolved by the end of 4 weeks. Fisher exact test stated that P value was not significant.
Table 3 also shows a comparison of bleb morphologies and IOP at 12 months in the HealaFlow® and MMC group. Majority of the patients had 25% central bleb area, 25% peripheral bleb area, moderately elevated with normal vascularity at 12 months. No needling revision of blebs or laser suture lysis was needed in either of the groups.
Fig. 2–c depicts the postoperative bleb morphology at day 1, week 1, and week 12 months, respectively, of patients from HealaFlow® group.
Figure 2.
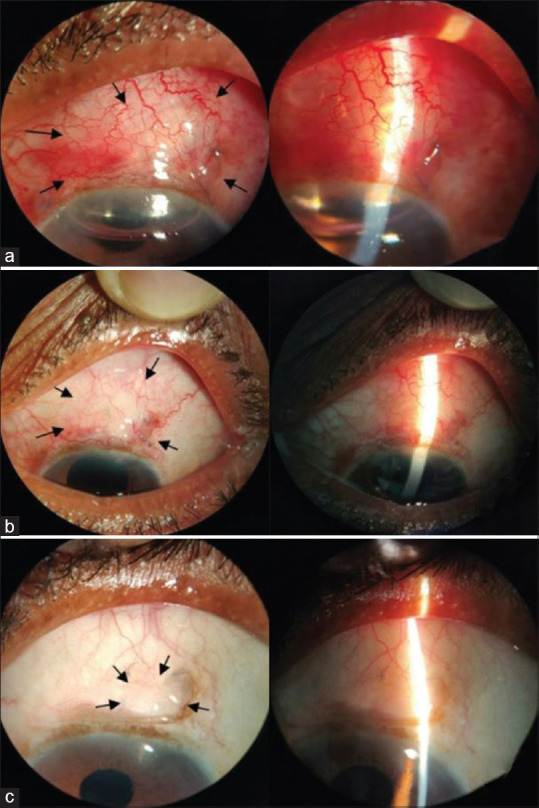
(a) Postoperative Day 1, Bleb morphology indicated with black arrows (b) Postoperative Week 1, Bleb morphology indicated with black arrows. (c) Postoperative 12 months, Bleb morphology indicated with black arrows
Discussion
As trabeculectomy remains the mainstay of surgical treatment for glaucoma patients not responding to maximal medical treatment, it is mandatory to prevent bleb cicatrix and serious complications that occur due to adjuvants being used currently. MMC has proven to significantly improve the success rate of trabeculectomy and has been accepted as a standard adjuvant. However, several possibilities have been explored over the years and recently a novel substitute – crosslinked hyaluronic acid gel scleral implant has been introduced. Previously, it has been used to reduce ocular surface damage in patients with dry eye and even in patients with rheumatoid arthritis and osteoarthritis.[11–13] Its placement as a scleral implant inhibits fibrosis locally and prevents vascularization. This reduces bleb failure and enables a good success rate and long-term effect.
To the best of our knowledge, this is the first study conducted on Indian population to assess the safety and efficacy of trabeculectomy with crosslinked hyaluronic acid gel (HealaFlow®) scleral implant and compare it with low-dose MMC in trabeculectomy with a follow-up of 12 months.
Forrester et al. studied the effect of sodium hyaluronate on phagocytosis using a sensitive polystyrene latex sphere assay in mouse peritoneal macrophage monolayers. Viscous solutions of high-molecular-weight hyaluronate (4.6 × 105–2.8 × 106) caused a dose-dependent inhibition of phagocytosis, but low-molecular-weight hyaluronate (9.0 × 104) was not inhibitory at equivalent viscosity.[9]
Along with having an inhibitory effect on inflammatory factors,[10] sodium hyaluronate with different molecular weight showed variability in biological functions. In an in vitro study on human nasal epithelial cells, Albano et al. observed that only high-molecular-weight form of sodium hyaluronate efficiently inhibited the rhIL17Amediated activation of ERK1/2, IkBa phosphorylation and NF-kB signal pathway activation, ROS production, IL-8 and NOX-4 proteins, and mRNA levels, therefore exhibiting an anti-inflammatory/anti-oxidative effect.[14] Crosslinked sodium hyaluronate had a more stable structure and a longer biodegradation time than the non-crosslinked product. Moreover, crosslinked and non-crosslinked sodium hyaluronate also showed different effects on proliferation of fibroblasts.[15]
Previously, various investigators have worked with different dosages and durations of MMC application and have concluded that 0.2–0.4 mg/mL MMC applied over 2–5 min gave an IOP reduction of 41.4–59.9%, which is similar to the reduction in our study, i.e., 53.23% (with 0.1 mg/mL).[16–23] Studies have been performed with lower dosage of 0.1 mg/mL MMC for 2 min and have shown a successful reduction to 11.1 ± 3.1 mmHg in the MMC group and an IOP reduction of 50.6 ± 1.23%.[24,25] Therefore, to prevent complications related to MMC, an accepted low-dose MMC regimen, i.e., 0.1 mg/mL for 2 min was taken up for this study.
IOP reduction analysis in our study stated that preoperatively the IOP in the HealaFlow® group was 23.59 ± 13.81 mmHg and in the MMC group it was 25.81 ± 11.01 mmHg, which is similar without any significant difference. On day 1 postoperatively, there was IOP reduction of 30.09% (to 16.50 ± 9.92 mmHg) and 44.59% (to 14.29 ± 8.01 mmHg) in the HealaFlow® group and the MMC group, respectively. The difference between the reduction could be due to presence of HealaFlow® in anterior chamber postoperatively, which resolved by the end of 1 week and so after 1 week. No postoperative spikes were observed. However, after 1 week, the IOP reduction was 50.69 (to 11.63 ± 6.52 mmHg) and 55.83% (to 11.40 ± 4.72 mmHg) in the HealaFlow® group and MMC group, respectively, which shows significant and equal fall in both the groups. By 12 months, the trend of IOP fall remained statistically similar in both the groups, i.e., 46.24 (to 11.04 ± 2.55 mmHg) and 54.47% (to 11.99 ± 3.37 mmHg) in the HealaFlow® group and MMC group, respectively.
Mohamed et al. showed the mean reduction rate of the IOP at the ninth month was 9.4 ± 7.7 (37.3%) and 11.4 ± 4.8 mmHg (45.8%) in the sodium hyaluronate group and MMC group, respectively.[8] In the study by Papaconstantinou D et al., the IOP at 6-month follow-up was lower than 18 mmHg in both the groups, which is similar to the observations in this study.[26] Wang X et al. stated that by 5 years 78% patients had postoperative IOP below 21 mmHg with sodium hyaluronate and 54% reached the goal in the group with only trabeculectomy.[27]
Raitta C et al. stated that even though there was an early postoperative IOP peak of 21 mmHg or more in 27% of the sodium hyaluronate eyes, the postoperative mean IOP reduction was significant with reduced need for glaucoma medications 1 month after surgery.[28] Roy et al. assessed 55 eyes and observed that the mean preoperative IOP was 21.6 ± 7.2 mmHg, which reduced to 11.5 ± 3.0 mmHg (46.6%) by 1 year, which is similar to our observations of reduction of 46.24% by 1 year.[29] In a study by Lopes JF et al., the mean IOP decreased from 26.0 ± 10.0 to 12.2 ± 3.7 mmHg by the end of 6 months.[30]
With the above-mentioned observations, it was concluded that the cross-linked sodium hyaluronate prevents postoperative scarring and fibrosis at the site of filtration and helps in maintaining its function, therefore lowers the IOP significantly and maintains it on subsequent visits.
In the current study, most of the patients presented with blebs with central area of 25%, maximal peripheral area of 25%, moderately elevated and normal vascularity equally distributed in HealaFlow® and MMC group. Similarly, Papaconstantinou D et al., demonstrated similar bleb vascularity in both groups and even though the sodium hyaluronate bleb was morphologically more prominent initially; it got gradually absorbed over the next few weeks.[26] Previous studies conducted on trabeculectomy with sodium hyaluronate demonstrated that well-visualized, diffuse blebs, loculated with thinner walls with good bleb height and extent, were mostly formed with sodium hyaluronate.[27,29–31] These findings are similar to this study.
We observed that in this study two cases developed postoperative hyphaema and one developed subconjunctival hemorrhage under bleb in the HealaFlow® group and similar observations were made in the MMC group. However, Mohamed et al. found severe complications like corneal abrasions, early bleb leak, dense subconjunctival hemorrhage with early impaired filtration, choroidal detachment, obliterated ostium with peripheral anterior synechiae, excessive corkscrew conjunctival vessels and Tenon’s cyst formation[8] and Papaconstantinou D et al. also observed complications like hypotony, flat anterior chamber, hyphaemas, and positive siedel test and encapsulated bleb.[26] In studies where patients underwent trabeculectomy with sodium hyaluronate by Raitta C et al. and Roy S et al. occurrence of hypotony, choroidal detachment, hyphaema, and iris incarcerations were noted.[28,29]
Studies carried out on MMC showed that bleb leak was the most common complication,[32–35] followed by aqueous misdirection, corneal abrasion, and Tenon’s cyst formation. In the current study, we did not observe major complications and the hyphaema and subconjunctival hemorrhage also resolved by the 4 week follow-up.
The outcome in the form of success rates was similar in both the groups in our study. In the HealaFlow® group as well as in the MMC group, complete success of 89.29% and qualified success of 10.71% was observed equally, which was statistically similar. However, Mohamed et al. observed a complete success of 63.6 and 90.9%, respectively, in the sodium hyaluronate and MMC group by 6 months. As per Papaconstantinou D et al., no statistically significant difference was observed between sodium hyaluronate and MMC and complete success at 6 months was observed in 60% sodium hyaluronate eyes and in 65% MMC eyes.[26] This shows that the efficacy of sodium hyaluronate and MMC is similar. A variation in outcomes has been observed, which could be due to patient compliance and postoperative care.
Keeping in mind the complications of MMC reported in the previous studies and considering the high cost of cross-linked hyaluronic acid viscoelastic scleral implant, it is recommended to use HealaFlow® in affording patients after considering its advantages on individual basis.
Prospective studies with larger number of patients and longer follow-up are recommended for confirmation of the conclusions of this study.
Conclusion
Therefore, it can be concluded from the present study that absorbable biosynthetic cross-linked hyaluronic acid (HealaFlow®) and low-dose MMC both are equally safe and efficacious in trabeculectomy at 12 months follow-up. By the last follow-up, the preoperative IOP had a similar reduction in both the groups with good bleb morphology. Therefore, absorbable biosynthetic cross-linked hyaluronic acid is a novel substitute for MMC and can be used successfully as an adjunct in trabeculectomy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82:887–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040:A systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968;66:673–9. [PubMed] [Google Scholar]
- 4.Watson PG, Barnett F. Effectiveness of trabeculectomy in glaucoma. Am J Ophthalmol. 1975;79:831–45. doi: 10.1016/0002-9394(75)90745-x. [DOI] [PubMed] [Google Scholar]
- 5.Xiong Q, Li Z, Li Z, Zhu Y, Abdulhalim S, Wang P, et al. Anti-VEGF agents with or without antimetabolites in trabeculectomy for glaucoma:A meta-analysis. PLoS One. 2014;9:e88403. doi: 10.1371/journal.pone.0088403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beckers HJM, Kinders KC, Webers CA. Five-year results of trabeculectomy with mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2003;241:106–10. doi: 10.1007/s00417-002-0621-5. [DOI] [PubMed] [Google Scholar]
- 7.Bao P, Kodra A, Tomic-Canic M, Golinko MS, Ehrlich HP, Brem H. The role of vascular endothelial growth factor in wound healing. J Surg Res. 2009;153:347–58. doi: 10.1016/j.jss.2008.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohamed MH, Abdelshafik MA, El Ibiary HM, Mohammed TH. Evaluation of the efficacy and safety of injectable cross-linked hyaluronic acid compared with mitomycin C in trabeculectomy surgery. J Egypt Ophthalmol Soc. 2015;108:173–9. [Google Scholar]
- 9.Forrester JV, Balazs EA. Inhibition of phagocytosis by high molecular weight hyaluronate. Immunology. 1980;40:435–46. [PMC free article] [PubMed] [Google Scholar]
- 10.Oh HJ, Li Z, Park SH, Yoon KC. Effect of hypotonic 0.18% sodium hyaluronate eyedrops on inflammation of the ocular surface in experimental dry eye. J Ocul Pharmacol Ther. 2014;30:533–42. doi: 10.1089/jop.2013.0050. [DOI] [PubMed] [Google Scholar]
- 11.Rolando M, Vagge A. Safety and efficacy of cortisol phosphate in hyaluronic acid vehicle in the treatment of dry eye in sjogren syndrome. J Ocul Pharmacol Ther. 2017;33:383–90. doi: 10.1089/jop.2016.0147. [DOI] [PubMed] [Google Scholar]
- 12.Chou CL, Li HW, Lee SH, Tsai KL, Ling HY. Effect of intra-articular injection of hyaluronic acid in rheumatoid arthritis patients with knee osteoarthritis. J Chin Med Assoc. 2008;71:411–5. doi: 10.1016/S1726-4901(08)70092-3. [DOI] [PubMed] [Google Scholar]
- 13.Egelius N, Jonsson E, Sunblad L. Studies of hyaluronic acid in rheumatoid arthritis. Ann Rheum Dis. 1956;15:357–63. doi: 10.1136/ard.15.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albano GD, Bonanno A, Cavalieri L, Ingrassia E, Di Sano C, Siena L, et al. Effect of high, medium, and low molecular weight hyaluronan on inflammation and oxidative stress in an in vitro model of human nasal epithelial cells. Mediators Inflamm. 2016;2016:289. doi: 10.1155/2016/8727289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wohlrab J, Wohlrab D, Neubert RHH. Comparison of noncross-linked and cross-linked hyaluronic acid with regard to efficacy of the proliferative activity of cutaneous fibroblasts and keratinocytes in vitro. J Cosmet Dermatol. 2013;12:36–40. doi: 10.1111/jocd.12024. [DOI] [PubMed] [Google Scholar]
- 16.Beatty S, Potamitis T, Kheterpal S, O'Neill EC. Trabeculectomy augmented with mitomycin C application under the scleral flap. Br J Ophthalmol. 1998;82:397–403. doi: 10.1136/bjo.82.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh J, O'Brien C, Chawla HB. Success rate and complications of intraoperative 0.2 mg/ml mitomycin C in trabeculectomy surgery. Eye (Lond) 1995;9:460–6. doi: 10.1038/eye.1995.107. [DOI] [PubMed] [Google Scholar]
- 18.Mietz H, Krieglstein GK. Mitomycin C for trabeculectomy in complicated glaucoma:Preliminary results after 6 months. Ger J Ophthalmol. 1994;3:164–7. [PubMed] [Google Scholar]
- 19.Kitazawa Y, Suemori-Matsushita H, Yamamoto T, Kawase K. Low-dose and High-dose mitomycin trabeculectomy as an initial surgery in primary open-angle glaucoma. Ophthalmology. 1993;100:1624–8. doi: 10.1016/s0161-6420(93)31426-0. [DOI] [PubMed] [Google Scholar]
- 20.Annen DJ, Stürmer J. [Follow-up of a pilot study of trabeculectomy with low dosage mitomycin C (0.2 mg/ml for 1 minute). Independent evaluation of a retrospective nonrandomized study] Klin Monbl Augenheilkd. 1995;206:300–2. doi: 10.1055/s-2008-1035446. [DOI] [PubMed] [Google Scholar]
- 21.Lee JJ, Park KH, Youn DH. The effect of low-and high-dose adjunctive mitomycin C in trabeculectomy. Korean J Ophthalmol. 1996;10:42–7. doi: 10.3341/kjo.1996.10.1.42. [DOI] [PubMed] [Google Scholar]
- 22.Costa VP, Comegno PE, Vasconcelos JP, Malta RF, José NK. Low-dose mitomycin C trabeculectomy in patients with advanced glaucoma. J Glaucoma. 1996;5:193–9. [PubMed] [Google Scholar]
- 23.Mégevand GS, Salmon JF, Scholtz RP, Murray AD. The effect of reducing the exposure time of mitomycin C in glaucoma filtering surgery. Ophthalmology. 1995;102:84–90. doi: 10.1016/s0161-6420(95)31049-4. [DOI] [PubMed] [Google Scholar]
- 24.Martini E, Laffi GL, Sprovieri C, Scorolli L. Low-dosage mitomycin C as an adjunct to trabeculectomy, A prospective controlled study. Eur J Ophthalmol. 1997;7:40–8. doi: 10.1177/112067219700700108. [DOI] [PubMed] [Google Scholar]
- 25.Sihota R, Angmo D, Chandra A, Gupta V, Sharma A, Pandey RM. Evaluating the long-term efficacy of short-duration 0.1 mg/ml and 0.2 mg/ml MMC in primary trabeculectomy for primary adult glaucoma. Graefes Arch Clin Exp Ophthalmol. 2015;253:1153–9. doi: 10.1007/s00417-015-3028-9. [DOI] [PubMed] [Google Scholar]
- 26.Papaconstantinou D, Diagourtas A, Petrou P, Rouvas A, Vergados A, Koutsandrea C, et al. Trabeculectomy with healaflow versus trabeculectomy for the treatment of glaucoma:A case-control study. J Ophthalmol. 2015;2015:836269. doi: 10.1155/2015/836269. doi:10.1155/2015/836269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Dai WW, Dang YL, Hong Y, Zhang C. Five years'outcomes of trabeculectomy with cross-linked sodium hyaluronate gel implantation for chinese glaucoma patients. Chin Med J (Engl) 2018;131:1562–8. doi: 10.4103/0366-6999.233655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raitta C, Lehto I, Puska P, Vesti E, Harju M. A randomized, prospective study on the use of sodium hyaluronate (Healon) in trabeculectomy. Ophthalmic Surg. 1994;25:536–9. [PubMed] [Google Scholar]
- 29.Roy S, Thi HD, Feusier M, Mermoud A. Crosslinked sodium hyaluronate implant in deep sclerectomy for the surgical treatment of glaucoma. Eur J Ophthalmol. 2012;22:70–6. doi: 10.5301/ejo.5000054. [DOI] [PubMed] [Google Scholar]
- 30.Lopes JF, Moster MR, Wilson RP, Altangerel U, Alvim HS, Tong MG, et al. Subconjunctival sodium hyaluronate 2.3% in trabeculectomy:A prospective randomized clinical trial. Ophthalmology. 2006;113:756–60. doi: 10.1016/j.ophtha.2006.01.040. [DOI] [PubMed] [Google Scholar]
- 31.Charteris DG, McConnell JM, Adams AD. Effect of sodium hyaluronate on trabeculectomy filtration blebs. J R Coll Surg Edinb. 1991;36:107–8. [PubMed] [Google Scholar]
- 32.Senthil S, Rao HL, Babu JG, Mandal AK, Garudadri CS. Comparison of outcomes of trabeculectomy with mitomycin C vs. ologen implant in primary glaucoma. Indian J Ophthalmol. 2013;61:338–42. doi: 10.4103/0301-4738.109520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cillino S, Casuccio A, Di Pace F, Cagini C, Ferraro LL, Cillino G. Biodegradable collagen matrix implant versus mitomycin-C in trabeculectomy:Five-year follow-up. BMC Ophthalmol. 2016;16:24. doi: 10.1186/s12886-016-0198-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.He M, Wang W, Zhang X, Huang W. Ologen implant versus mitomycin C for trabeculectomy:A systematic review and meta-analysis. PLoS One. 2014;9e:2. doi: 10.1371/journal.pone.0085782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bindlish R, Condon GP, Schlosser JD, D'Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy:Five-year follow-up. Ophthalmology. 2002;109:1336–41. doi: 10.1016/s0161-6420(02)01069-2. discussion 1341-2. [DOI] [PubMed] [Google Scholar]


