Abstract
Aim
To explore the effects of an educational‐ counselling programme based on the precede–proceed model during pregnancy on preventing post‐partum depression.
Design
A randomized clinical trial (RCT) study.
Method
130 pregnant women were selected and randomly assigned to intervention and control groups. Data collection was carried out using questionnaires of predisposing, reinforcing and enabling factors, GHQ and Edinburgh Postnatal Depression Scale (EPDS). The Education programme was designed and performed in each group in a given weekday through four 60‐minute sessions. The whole intervention lasted for one month in all groups. The participants in the control group were given routine pregnancy care. Data were gathered before and after the intervention in both groups.
Results
Independent t test showed a significant difference between the two groups in terms of the mean score of predisposing, reinforcing, enabling factors and post‐partum depression (p < .05). Regression tests indicated predisposing, reinforcing, enabling factors and general health as the most important factors associated with post‐partum depression (p < .05). The results supported the effectiveness of the educational intervention on reducing post‐partum depression and showed that implementing these training during pregnancy leads to a reduced level of post‐partum depression.
Keywords: post‐partum depression, pregnant women, randomized controlled trial
1. INTRODUCTION
Post‐partum depression is a major public health issue and a prevalent clinical disorder post‐partum (Darcy et al., 2011; de Tychey et al., 2008; Lau et al., 2018). It is a common and debilitating psychosocial disorder which may begin during first four weeks following childbirth. Some studies have reported the onset until 12 months after birth (Gavin et al., 2014; Kazemeyni et al., 2018). A meta‐analysis of 43 articles reported a 10.4% prevalence of post‐partum depression (Paulson & Bazemore, 2010). Another study Sri Lanka estimated the prevalence of post‐partum depression was 7.8% at 4 weeks and 15.5% at 10 days post‐partum (Fan et al., 2020). Also in a study carried out in the eastern Tigray zone, Ethiopia, the prevalence of major depression at six weeks post‐partum was 19% (Arikan et al., 2017). Evidence indicates that the prevalence of post‐partum depression in Iran is 28.7% (Veisani et al., 2013). Post‐natal depression is characterized by depressed mood, irritability, lack of pleasure in daily activities, frustration, anxiety, excess fatigue, psychomotor disturbances and sleep and appetite disorders, feeling guilty, or inadequate especially in taking care of the baby. Post‐partum depression needs special attention since it may lead to a considerable amount of distress during a crucial life period of the mother with negative consequences on the child's mental growth (Gharacheh et al., 2018). Diagnosis of post‐partum depression is often neglected (Lanes et al., 2011) and left without any treatments which could impose serious effects on mother, child and the family (Ikeda & Kamibeppu, 2013).
2. BACKGROUND
Education during pregnancy is focused on the physical, emotional and mental preparation of mother and family for birth, health promotion and improved lifestyle behaviours during childbearing years. These courses are widely important in helping couples to learn about pregnancy, labour and becoming a parent (El‐Ibiary et al., 2013). A previous study showed that education could improve knowledge, attitude and function, and group education is more effective than individual methods probably due to increased motivation (Baniaghil & Khoddam, 2005). Another study indicated that participation in prenatal education programmes lowers the likelihood of post‐partum depression (Hassan, 2016). However, a study in the US concluded that education did not cause any decrease in post‐partum depression (McCarter‐Spaulding & Shea, 2016).
To gain effective and helpful results, education should be based on defined and organized theories and models. The PRECEDE model was introduced by Green and Kreuter in 1970 (Glanz et al., 2015). This model underwent some modifications. In 2005, Green and Kreuter introduced the latest modified version of the PRECEDE–PROCEED model (PPM) containing four phases of programming, one phase of implementation, and three phases of assessment as follows: social assessment, epidemiological assessment, behavioural and environmental assessments, educational and ecological assessments, management and political assessments, programme implementation, assessment of the process, assessment of the effect and assessment of the outcome (Green & Kreuter, 2005). This model pays attention to several factors that comprise the health status of individuals and clearly defines and interprets them (Moshki et al., 2017) and is founded in social/behavioural science, epidemiology, administration and education. The systematic use of this framework in a series of clinical trials confirmed the utility and predictive validity of the model as a planning tool and as a participatory model for creating successful community health promotion and other public health interventions (Green et al., 1975), such as educational intervention on life quality in hypertensive patients (Azar et al., 2020). Or community pharmacy for health needs assessment (Handyside et al., 2020). Most of the studies consider the Precede–Proceed model as a valid tool in the planning of effective prevention programmes. So the PPM is a multidimensional model that takes into account multiple factors that “shape health status and help the planner arrive at a highly focused subset of those factors as targets for intervention (Sinopoli et al., 2018). Of particular importance to the PRECEDE–PROCEED planning model is the role of theory in creating a conceptual framework that guides the construction of an intervention and its evaluation (Crosby et al., 2011).
In recent years, various studies have been carried out in Iran regarding post‐partum depression especially in terms of prevalence and risk factors of post‐partum depression (Falah‐Hassani et al., 2016; Fantahun et al., 2018). However, limited work has been published about preventive interventions based on these models. Therefore, considering the consequences of post‐partum depression and the necessity to reduce this disorder and also lack of experimental evidence in Iran in this regard, the present study was carried out to explore the effect of an educational‐ counselling programme based on precede–proceed during pregnancy on preventing post‐partum depression in southern Razavi Khorasan Province during 2016.
3. METHODS
3.1. Design
This was a randomized clinical trial (RCT).
3.2. Setting and samples
In this study, pregnant women in southern Razavi Khorasan Province in Iran were selected. A random stratified sampling method was used. Researchers presented to health centres of Gonabad to recruit women and randomly (using the Flip the coin method) divided them into two groups of intervention and control. A total of 140 pregnant women were selected via systematic, community‐based sampling (Figure 1).
FIGURE 1.
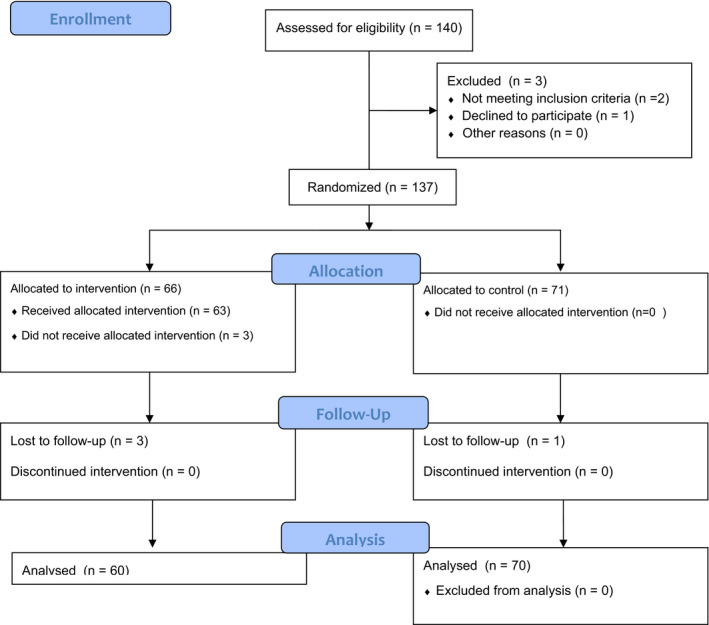
Flow chart of recruiting participants
3.3. Inclusion and exclusion criteria
Participants were selected based on the following criteria: women in 30–35 weeks of pregnancy, no history of depression, reading and writing literacy, a healthy foetus in ultrasonography, living in the city and consent for participating in the study. Exclusion criteria were as follows: the presence of severe stressful factors including the death of first degree relatives during the past three months, unwillingness to continue the study at any point, two missing sessions for the intervention group, premature labour and undesirable events during the study period.
3.4. Measures
Edinburgh Postnatal Depression Scale (EPDS): this tool is used to identify women with post‐partum depression which was first developed by Cox and colleagues in 1987. Various studies have confirmed the efficiency of this scale for identifying depressed women from healthy individuals (Cox, 2017). It includes 10 questions, and each question is scored from 0–3. The total score ranges from 0–30 and a score of 10–13 indicates mild post‐partum depression while a score of 14–15 indicates moderate post‐partum depression. A score of 16 or higher is considered as severe depression which necessitates introduction to a psychologist. In Iran, the reliability of the questionnaire was reported as 0.77 and 0.8 with Cronbach's alpha and retest methods, respectively (Montazeri et al., 2007). In the present study, an alpha of 0.78 was reported for this questionnaire.
After the literature review, a questionnaire was designed according to the educational‐ ecological assessment in the PRECEDE–PROCEED model. The first part includes 7 questions about age, education, employment, pregnancy order, marriage age, gestational age and history of stillbirth. The second part Predisposing factors were measured using 10 and 18 questions regarding knowledge and attitude, respectively. Knowledge questions were asked in three domains including knowledge of post‐partum depression, knowledge of its symptoms and ways for controlling post‐partum depression and its symptoms. Each correct answer was given one, and otherwise, no point was assigned. Attitude questions were designed as a 5‐point Likert scale (completely agree, agree, no comment, disagree and completely disagree). A score of 5 indicated the highest degree of positive attitude while the lowest was shown by a score of 1. The third section of the questionnaire related to the enabling factors which were measured through 6 questions. Yes or no questions were designed and scored as follows: no = 1, somewhat = 2, yes = 3. The fourth section of the questionnaire measures reinforcing factors through 2 questions with yes, no and somewhat answers being scored as 2, 0 and 1, respectively. In Iran, to determine content and face validity, questionnaires were reviewed by 10 faculty members. Reliability was explored in 10 respondents using the test–retest method with a two‐week interval, and Cronbach's alpha was calculated. The Correlation coefficient from the retest method for knowledge questions was r = 0.80, and Cronbach's alpha of 0.76, 0.74 and 0.79 was obtained for attitude questions and predisposing, reinforcing and enabling factors inventory, respectively.
General Health Questionnaire (GHQ): it consists of 4 subscales including physical symptoms, anxiety symptoms, social functioning and depressive symptoms. Each scale is made of seven questions which are assessed based on a Likert scale scoring as never (0), few (1), high (2) and very high (3). The total score for each person ranges from 0–84. The cut‐off point for the questionnaire is reported to be 23. In this method, individuals with a score of 23 or less are considered healthy and those with a score of 24 or higher are suspected to be mentally disordered. In Iran, the validity and reliability of this questionnaire were confirmed with Cronbach's alpha of 0.72–0.91 (Ataie et al., 2018; Malakouti et al., 2007). In the present study, Cronbach's alpha was used to explore the reliability of the questionnaire which was reported as 0.77.
3.5. Intervention
3.5.1. Stage 1: Social assessment
In this phase, factors affecting general health and post‐partum depression in women were evaluated by the use of different data collection tools such as reviewing the literature, holding private sessions and establishing focus groups. The pre‐test results showed that lack of awareness of post‐partum depression and ways to prevent it were among the main social problems of participants.
3.5.2. Stage 2: Epidemiologic behavioural and environmental assessment
In this phase, researchers collected information about post‐partum depression and ways to prevent it. This information included post‐partum depression prevalence, significance and related factors in Iran and other countries based on online databases and other sources. Classification of behaviours (behavioural and non‐behavioural factors) was also done based on their significance.
3.5.3. Stage 3: Educational and ecological assessment
In this phase, based on literature review and focus groups with pregnant women was determined predisposing, enabling and reinforcing factors’ that affect health‐related behaviours. In a primary review of the literature by the researcher, knowledge, attitude and acknowledgment and attitude were chosen as predisposing factors. Enabling factors included access to databases and attending educational courses. Reinforcing factors included family support by the husband and friends and verbal encouragement. Also in this stage, the general and objective goals of the educational programme were compiled.
3.5.4. Stage 4: Assessment of management and policies and designing Interventions
In this phase, location, time, resources and available and required facilities for the programme were determined. The organizational policies of the research centre, which was the health centre, were evaluated and the necessary coordination was made with the authorities.
3.5.5. Stage 5: Implementation
The educational intervention programme according to the PRECEDE–PROCEED model was conducted for five groups (n = 12), with each session held once a week and the programme was held during four consecutive sessions (60–90 min). Discussed topics included anatomical and physiologic changes, prenatal and post‐natal care, mental health during pregnancy and after, events during pregnancy and after childbirth, maternal feelings and thoughts and post‐partum issues, and their solutions. Sessions were conducted and controlled by the researcher.
3.5.6. Stage 6: Assessment of process
During the implementation of the educational course, the progression of the participants was assessed based on predetermined goals by regular assessments.
3.5.7. Stage 7: Assessment of the impact
The change in knowledge and attitude of participants, predisposing factors, enabling factors and reinforcing factors, and GHQ were assessed immediately after the intervention by analysing the questionnaires.
3.5.8. Stage 8: Assessment of outcome
Change in post‐partum depression was assessed 4–6 weeks after childbirth in group discussion and question‐and‐answer sessions (by analysing the EPDS).
It should be noted that training was performed routinely at the same time in the control group. The participants in the control group were given routine pregnancy care including healthcare and childbirth preparation classes. These sessions from the 20th week of pregnancy are held in 8 sessions and the form of lectures.
3.6. Data analysis
Data were stratified and analysed with SPSS, 20 (SPSS Inc. Chicago, Illinois). Normality was confirmed using the Kolmogorov–Smirnov test (p > .05). Then, the chi‐square test, t test, linear regression and Pearson correlation were used for data analysis.
3.7. Ethics
This study is registered on www.ClinicalTrials.gov (NCT04129476). The study protocol was approved by the ethics committee of Gonabad University of Medical Sciences. Study objectives, the confidentiality of the information and the right to drop out of the study at any time point during the study period were discussed with the participants, and written consent was obtained.
4. RESULTS
In this study, 130 women in 30–35 weeks during the 30th–35th week of pregnancy were examined (7 people were lost in the allocation and follow up stages). The mean age of the participants was 27.9 ± 5.81. Other demographic characteristics are seen in Table 1. The results showed that the prevalence of post‐partum depression after the intervention was 6.7% and 34% in the case and control groups, respectively, and a significant difference was observed between the two groups in terms of depression prevalence (p = .001) (Table 2).
TABLE 1.
Demographic factors in participants
| Variables | Test group | Intervention Number (per cent) | Control Number (per cent) | Statistical Test |
|---|---|---|---|---|
| Job | Housewife | 52 (86.7) | 52 (78.8) |
Kendall' tau –c p = .291 |
| Employee | 4 (6.7) | 9 (13.6) | ||
| Student | 4 (6.7) | 5 (7.6) | ||
| Education | Elementary | 16 (26.66) | 14 (19.7) |
Chi‐square : χ 2 = 8.586 df = 4 p = .072 |
|
middle school |
8 (13.33) | 9 (12.7) | ||
| High school, high school diploma | 16 (26.66) | 26 (36.6) | ||
| College/University education | 20 (33.33) | 22 (13) | ||
| Pregnancy grade | First | 36 (60) | 32 (43.8) |
Chi‐square : χ 2 = 0.4.044 df = 3 p = .257 |
| Second | 12 (20) | 24 (32.9) | ||
| Third | 8 (13.3) | 10 (13.7) | ||
| Four and above | 4 (6.7) | 7 (9.6) | ||
| Abortion history | Have | 12 (20) | 14 (19.2) |
Chi‐square: χ 2 = 0.081 df = 1 p = .776 |
| Have not | 48 (80) | 59 (80.8) | ||
| Average age to year (SD) | 28 (6.39) | 27.80 (5.29) |
T test: t = 0.187 df = 114.9 p = .852 |
|
| Average marriage to month (SD) | 70.80 (74.06) | 79.52 (62.34) |
T test: t = −0.735 df = 130 p = .464 |
TABLE 2.
Comparison of the prevalence of post‐partum depression after the intervention in the two groups
| Groups/post‐partum depression | Intervention (N = 60) | Control (N = 70) | p‐value |
|---|---|---|---|
| Not depressed | 56(93.3%) | 46(65.5%) | (Fisher's exact test) p = .001 |
| Depressed | 4(6.7%) | 24(34.3%) |
Table 3 shows markers of the precede–proceed model, general health and post‐partum depression in both groups after the intervention. As can be seen, all markers are significant except for general health.
TABLE 3.
Comparison of Precede–Proceed model indexes, general health and post‐partum depression, before and after the intervention in the two groups
| Variables | Mean ± standard deviation before the intervention | Mean ± standard deviation after the intervention | p‐value Before and after the intervention (Independent t test) | ||
|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||
| Knowledge | 17.88 + 6.87 | 17.44 ± 8.15 | 19.41 ± 3.41 | 17.55 ± 7.94 | p = .016 |
| Attitude | 27.2 ± 3.39 | 42.3 ± 483.26 | 67.3 ± 33.28 | 98.5 ± 206.26 |
t = −3.043* df = 88.551 p = .003 |
| Enabling factors | 18 ± 13.85 | 29.57 ± 10.01 | 57.3 ± 538.21 | 30.15 ± 529.53 |
t = −2.366* df = 16.558 p = .030 |
| Reinforcing factors | 7.96 ± 1.53 | 8.25 ± 0.73 | 35.1 ± 066.8 | 49.2 ± 945.5 |
t = 6.229* df = 114.626 p = .001 |
| General Health | 17.78 ± 6.02 | 19.16 ± 10.83 | 17.80 ± 8.27 | 16.50 ± 6.62 | p = .281 |
| post‐partum depression | 11.45 ± 5.02 | 10.79 ± 5.24 | 7.68 ± 4.02 | 10.69 ± 4.88 | p = .001 |
Regression analysis showed that among studied variables, predisposing (attitude and age of marriage), reinforcing and enabling factors and general health were the most important factors associated with post‐partum depression (Table 4).
TABLE 4.
The results of multiple regression analysis of the Precede–Proceed model indexes in predicting post‐partum depression in intervention group
| Predictive variables | β | t | F | df | p‐value | R 2 | 95% CI |
|---|---|---|---|---|---|---|---|
| knowledge | −0.22 | −0.81 | 0.66 | 2 | .43 | 0.04 | [−1.233, 0.557] |
| age | 0.43 | 0.15 | 0.02 | 1 | .81 | 0.002 | [−0.324, 0.374] |
| Spouse's age | −0.04 | −0.37 | 0.03 | 1 | .71 | 0.002 | [−0.380, 0.322] |
| attitude | −0.41 | −2.40 | 5.77 | 1 | .02 | 0.17 | [−0.631, −0.050] |
| marriage age | 0.23 | 2.45 | 5.00 | 1 | .01 | 0.27 | [0.001, 0.052] |
| Enabling factors | 0.37 | 3.26 | 687/1 | 1 | .002 | 202/0 | [1.53, 7.22] |
| Reinforcing factors | 0.52 | 2.23 | 5 | 1 | p < .001 | 0.27 | [0.08, 4.97] |
| General health | 0.49 | 6.36 | 478/4 | 1 | p < .001 | 242/0 | [0.193, 0.371] |
5. DISCUSSION
The results showed that developing and implementing an educational‐ counselling programme according to the precede–proceed model could significantly influence the knowledge and attitude in terms of post‐partum depression prevention. A research in this regard also indicated reduced depression in patients undergoing open‐heart surgery after an education programme based on the precede model (Sabzmakan et al., 2012). Moreover, another study stated that an educational intervention was effective in reducing post‐partum distress which led to improved quality of life (Akbarzadeh et al., 2012). These results are consistent with our research.
In this study, knowledge and attitude in the intervention group were enhanced after the implementation of the educational‐ counselling programme based on the precede–proceed model. It can be postulated that an educational‐ counselling programme method according to precede–proceed model caused mothers in the intervention group to reach logical thinking regarding pregnancy and events during pregnancy and to develop necessary preparation. It seems that the education programme could increase the knowledge level of the participants in terms of post‐partum conditions and associated mood swings. In other words, it is likely that with an educational‐ counselling programme based on the precede–proceed model, mothers are empowered to manage their behaviours and to avoid thoughts and behaviours that lead to post‐partum depression.
A study regarding educational programmes in post‐partum depression showed that these programmes could result in higher knowledge among women especially in terms of post‐partum depression (Feth, 2017). Health education programmes are a prerequisite for behaviour change which increases knowledge and positive attitudes. It is obvious that attempts to promote women's knowledge to reinforce self‐care improve their quality of life during pregnancy (M. Moshki et al., 2015).
In this study, reinforcing factors included support from family especially from the husband and verbal persuasion and encouragement of women and the results showed that the mean score of these factors was significantly higher after the intervention. It can be said that strategies based on support, reinforcement and access to services are required as a normal part of the pre‐pregnancy period. These could help fathers to better understand their partner's circumstances and their attitudes towards their condition (Feth, 2017). A meta‐analysis about biological and psychosocial predictors of post‐partum depression concluded that social support is a predictor of post‐partum depression. In particular, if the support is from the partner, it could reduce the risk of post‐partum depression (Yim et al., 2015).
Enabling factors were access to information sources and to hold educational classes, and the results indicated that the mean score of these factors significantly increased after the intervention. A study titled as the effectiveness of discharge education on post‐partum depression demonstrated that education did not reduce depressive symptoms (McCarter‐Spaulding & Shea, 2016). Also, a study in 2017 in Istanbul found that training programmes may not be effective in decreasing post‐partum depression (Gurkan & Eksi, 2017) which is inconsistent with the results of the present study. The reason for this inconsistency could be that in that study, depression questionnaires were completed 6 weeks, 3 and 6 month after the intervention while in the present study, questionnaires were filled out 6 weeks and 6 months after. Also, in this study, questionnaires were completed at 4–6 weeks of childbirth and this time interval between intervention and data collection could have reduced the effectiveness of the intervention.
We found that educational intervention based on the precede–proceed model did not significantly affect women's general health score. A review article in 2006 concluded that No evidence was found to confirm the provision of post‐partum support to improve parenting, maternal mental or physical health (Shaw et al., 2006) which is in line with our findings. However, another research paper confirmed the effectiveness of an educational programme based on the PRECEDE model on improving general health in heart surgery patients (Sabzmakan et al., 2012) which is in contrast with the present study. these differences in results are attributable to characteristics of study participants, type of interventions, and individual or group education method. A systematic review reported the influence of variations in intervention duration, onset and modes of the provision on reduced post‐partum depression (Trivedi, 2014). The results of the present study showed that predisposing (attitude and age of marriage), reinforcing and enabling factors and general health are predictive of post‐partum depression. Research also demonstrates that paternal excessive protection and care, lack of maternal care, lack of social support and poor perception of mental health are among important predictors of post‐partum depression (Ganann et al., 2016; Norouzi, 2015). Another study states that prenatally low paternal support is predictive of post‐partum depression (Leung et al., 2017).
Finally, post‐partum depression was measured using EPDS, and prevalence of depression was estimated as 34,3% and 6.7% in the control and case groups, respectively. In a study of supportive activities during pregnancy on post‐partum depression, prevalence depression in the study group was 6.5% versus 18.6% in the control group (Ajh et al., 2006). In another study, the prevalence of depressive symptoms 6 weeks and 6 months after birth was 11.8% and 10.1%, respectively (Fiala et al., 2017). This has been reported to be 21% in Japan (Ikeda & Kamibeppu, 2013) and 8.69% in Canada (Lanes et al., 2011). Differences in culture, beliefs and customs may explain these discrepancies in results.
Implications for practice and or policy: This model helps healthcare professionals with design, implementation and evaluation of an education programme and could provide necessary solutions for empowering individuals to apply effective interventions in health problems. Also, the results of the present study could help health planners especially in terms of mental health to confront problems during pregnancy and after with the help of mothers and their family through an orderly and arranged framework.
Limitations: Small sample size was recruited. Also, considering different traditions in Iran as compared to other parts of the world, the results may not be generalizable to other maternal populations. Also, the questionnaire was completed 4–6 weeks of childbirth which was difficult due to maternal circumstances during this period.
Conclusion: Overall, the results indicated that an educational‐ counselling programme based on the precede–proceed model in pregnancy could significantly prevent post‐partum depression and could be considered an effective intervention to reduce maternal depression after childbirth.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
ACKNOWLEDGMENTS
This study was approved by Health Education & Promotion of the School of Health at Gonabad University of Medical Sciences. The authors wish to thank the Health Centers of the southern Razavi Khorasan Province and all the pregnant women who participated in this project for their sincere cooperation during the study.
Beydokhti TB, Dehnoalian A, Moshki M, Akbary A. Effect of educational‐ counseling program based on precede‐proceed model during Pregnancy on postpartum depression. Nurs Open. 2021;8:1578–1586. 10.1002/nop2.770
DATA AVAILABILITY STATEMENT
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data are not available.
REFERENCES
- Ajh, N. , Unesian, M. , Fili, A. , & Abasi Motejaded, A. (2006). The study of supportive activities during pregnancy on postpartum depression. Hayat, 12(3), 73–80. [Google Scholar]
- Akbarzadeh, M. , Toosi, M. , Zare, N. , & Sharif, F. (2012). Effect of relaxation training to pregnant mothers on quality of life and postpartum blues. Knowledge & Health, 7(2), 83–88. [Google Scholar]
- Arikan, I. , Korkut, Y. , Demir, B. K. , Sahin, S. , & Dibeklioglu, S. E. (2017). The prevalence of postpartum depression and associated factors: A hospital‐based descriptive study. Journal of Clinical and Analytical Medicine, 8, (Suplement 4), 10.4328/jcam.5030. [DOI] [Google Scholar]
- Ataie, Z. , Allahverdi, A. , Dehnoalian, A. , & Orooji, A. (2018). The Relationship between Lifestyle and General Health among Elderly People in Neyshabur. Iran Journal of Nursing, 31(111), 10–19. 10.29252/ijn.31.111.10 [DOI] [Google Scholar]
- Azar, F. E. F. , Solhi, M. , Azadi, N. A. , Ziapour, A. , Lebni, J. Y. , & Chaboksavar, F. (2020). The effect of educational intervention based on precede proceed model on life quality in hypertensive patients. In: Research Square. 10.21203/rs.2.19628/v1 [DOI] [Google Scholar]
- Baniaghil, A. , & Khoddam, H. (2005). Impact of group and individual education of family Practice of women. Journal of Gorgan University of Medical Sciences, 7(1), 43–46. [Google Scholar]
- Cox, J. (2017). Use and misuse of the Edinburgh Postnatal Depression Scale (EPDS): A ten point 'survival analysis'. Arch Womens Ment Health, 20(6), 789–790. 10.1007/s00737-017-0789-7 [DOI] [PubMed] [Google Scholar]
- Crosby, R. , & Noar, S. M. (2011). What is a planning model? An introduction to PRECEDE‐PROCEED. Journal of Public Health Dentistry, 71, S7–S15. 10.1111/j.1752-7325.2011.00235.x [DOI] [PubMed] [Google Scholar]
- Darcy, J. M. , Grzywacz, J. G. , Stephens, R. L. , Leng, I. , Clinch, C. R. , & Arcury, T. A. (2011). Maternal depressive symptomatology: 16‐month follow‐up of infant and maternal health‐related quality of life. J Am Board Fam Med, 24(3), 249–257. 10.3122/jabfm.2011.03.100201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Tychey, C. , Briançon, S. , Lighezzolo, J. , Spitz, E. , Kabuth, B. , de Luigi, V. , Messembourg, C. , Girvan, F. , Rosati, A. , Thockler, A. , & Vincent, S. (2008). Quality of life, postnatal depression and baby gender. Journal of Clinical Nursing, 17(3), 312–322. 10.1111/j.1365-2702.2006.01911.x [DOI] [PubMed] [Google Scholar]
- El‐Ibiary, S. Y. , Hamilton, S. P. , Abel, R. , Erdman, C. A. , Robertson, P. A. , & Finley, P. R. (2013). A pilot study evaluating genetic and environmental factors for postpartum depression. Innovations in Clinical Neuroscience, 10(9–10), 15. [PMC free article] [PubMed] [Google Scholar]
- Falah‐Hassani, K. , Shiri, R. , & Dennis, C.‐L. (2016). Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. Journal of Affective Disorders, 198, 142–147. 10.1016/j.jad.2016.03.010 [DOI] [PubMed] [Google Scholar]
- Fan, Q. , Long, Q. , De Silva, V. , Gunarathna, N. , Jayathilaka, U. , Dabrera, T. , & Østbye, T. J. A. (2020). Prevalence and risk factors for postpartum depression in Sri Lanka: A population‐based study. Asian Journal of Psychiatry, 47, 101855– 10.1016/j.ajp.2019.101855 [DOI] [PubMed] [Google Scholar]
- Fantahun, A. , Cherie, A. , & Deribe, L. (2018). Prevalence and factors associated with postpartum depression among mothers attending public health centers of Addis Ababa, Ethiopia, 2016. Clinical Practice & Epidemiology in Mental Health, 14(1), 196–206. 10.2174/1745017901814010196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feth (Kalyn), L. (2017). PostPartum Depression Educational Intervention.UNLV Theses, Dissertations, Professional Papers, and Capstones. 2970.
- Fiala, A. , Švancara, J. , Klánová, J. , & Kašpárek, T. (2017). Sociodemographic and delivery risk factors for developing postpartum depression in a sample of 3233 mothers from the Czech ELSPAC study. BMC Psychiatry, 17(1), 104. 10.1186/s12888-017-1261-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganann, R. , Sword, W. , Thabane, L. , Newbold, B. , & Black, M. (2016). Predictors of postpartum depression among immigrant women in the year after childbirth. Journal of Women's Health, 25(2), 155–165. 10.1089/jwh.2015.5292 [DOI] [PubMed] [Google Scholar]
- Gavin, N. I. , Meltzer‐Brody, S. , Glover, V. , & Gaynes, B. N. (2014). Is population‐based identification of perinatal depression and anxiety desirable? A public health perspective on the perinatal depression care continuum. Jeannette Milgrom Alan W. Gemmill Identifying Perinatal Depression and Anxiety: Evidence‐Based Practice in Screening (pp. 11–31). Psychosocial Assessment, and Management. [Google Scholar]
- Gharacheh, M. , Ranjbar, F. , & Azadi, S. (2018). Women’s quality of life and postpartum depression. Iran Journal of Nursing, 30(110), 68–77. 10.29252/ijn.30.110.68 [DOI] [Google Scholar]
- Glanz, K. , Rimer, B. K. , & Viswanath, K. (2015). Health behavior: Theory, research, and practice, (95–97). John Wiley & Sons. [Google Scholar]
- Green, L. , & Kreuter, M. (2005). Health Program Planning: An educational and ecological approach, 4 thedn, New York: McGraw Hill. [Google Scholar]
- Green, L. W. , Levine, D. M. , & Deeds, S. (1975). Clinical trials of health education for hypertensive outpatients: Design and baseline data. Preventive Medicine, 4(4), 417–425. 10.1016/0091-7435(75)90030-4 [DOI] [PubMed] [Google Scholar]
- Gurkan, O. C. , & Eksi, Z. (2017). Effects of antenatal education program on postpartum functional status and depression/Antenatal egitimin dogum sonrasi fonksiyonel statu ve depresyona etkisi. Clinical and Experimental Health Sciences, 7(4), 133–139. 10.5152/clinexphealthsci.2017.284 [DOI] [Google Scholar]
- Handyside L., Warren R., Devine S., Drovandi A. (2021). Utilisation of the PRECEDE‐PROCEED model in community pharmacy for health needs assessment: A narrative review. Research in Social and Administrative Pharmacy, 17, (2), 292–299. 10.1016/j.sapharm.2020.03.021. [DOI] [PubMed] [Google Scholar]
- Hassan, J. (2016). Prenatal education and postpartum well‐being. J Preg Child Health, 3(2), 2–6. 10.4172/2376-127X.1000248 [DOI] [Google Scholar]
- Ikeda, M. , & Kamibeppu, K. (2013). Measuring the risk factors for postpartum depression: Development of the Japanese version of the Postpartum Depression Predictors Inventory‐Revised (PDPI‐RJ). BMC Pregnancy and Childbirth, 13(1), 112. 10.1186/1471-2393-13-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemeyni, M. , Bakhtiari, M. , & Nouri, M. (2018). Effectiveness of acceptance and commitment group therapy on postpartum depression and psychological flexibility. Journal of Clinical Nursing and Midwifer, 4(3).20–31. [Google Scholar]
- Lanes, A. , Kuk, J. L. , & Tamim, H. (2011). Prevalence and characteristics of postpartum depression symptomatology among Canadian women: A cross‐sectional study. BMC Public Health, 11(1), 302. 10.1186/1471-2458-11-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, Y. , Htun, T. P. , & Kwong, H. K. D. (2018). Sociodemographic, obstetric characteristics, antenatal morbidities, and perinatal depressive symptoms: A three‐wave prospective study. PLoS One, 13(2), e0188365. 10.1371/journal.pone.0188365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, B. M. Y. , Letourneau, N. L. , Giesbrecht, G. F. , Ntanda, H. , & Hart, M. (2017). Predictors of Postpartum Depression in Partnered Mothers and Fathers from a Longitudinal Cohort. Community Mental Health Journal, 53(4), 420–431. 10.1007/s10597-016-0060-0 [DOI] [PubMed] [Google Scholar]
- Malakouti, S. K. , Fatollahi, P. , Mirabzadeh, A. , & Zandi, T. (2007). Reliability, validity and factor structure of the GHQ‐28 used among elderly Iranians. International Psychogeriatrics, 19(4), 623–634. 10.1017/s1041610206004522 [DOI] [PubMed] [Google Scholar]
- McCarter‐Spaulding, D. , & Shea, S. (2016). Effectiveness of discharge education on postpartum depression. The American Journal of Maternal Child Nursing, 41(3), 168. https://dx.doi.org/10.1097%2FNMC.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montazeri, A. , Torkan, B. , & Omidvari, S. (2007). The Edinburgh Postnatal Depression Scale (EPDS): Translation and validation study of the Iranian version. BMC Psychiatry, 7(1), 11. 10.1186/1471-244X-7-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshki, M. , Dehnoalian, A. , & Alami, A. (2017). Effect of precede–proceed model on preventive behaviors for type 2 diabetes mellitus in high‐risk individuals. Clinical Nursing Research, 26(2), 241–253. 10.1177/1054773815621026 [DOI] [PubMed] [Google Scholar]
- Moshki, M. , Kharazmi, A. , Cheravi, K. , & Beydokhti, T. B. (2015). The prediction of postpartum depression: The role of the PRECEDE model and health locus of control. Journal of Family Medicine and Primary Care, 4(3), 454–460. 10.4103/2249-4863.161354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norouzi, Z. (2015). Prediction of postpartum depression based on parental bonding, history of anxiety, and depression among women attended health care centers in shiraz. Razi Journal of Medical Sciences, 21(127), 24–30. [Google Scholar]
- Paulson, J. F. , & Bazemore, S. D. (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: A meta‐analysis. JAMA, 303(19), 1961–1969. 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- Sabzmakan, L. , Hazavei, S. M. M. , Rabiei, K. , Jahani Hashemi, H. , Sadeghi, M. M. , & Roohafza, H. (2012). Effect of PRECEDE educational model on depression and quality of life of patients with coronary artery bypass graft surgery. ARYA Atheroscler, 7, S55–S62. [PMC free article] [PubMed] [Google Scholar]
- Shaw, E. , Levitt, C. , Wong, S. , & Kaczorowski, J. (2006). Systematic review of the literature on postpartum care: Effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth, 33(3), 210–220. 10.1111/j.1523-536X.2006.00106.x [DOI] [PubMed] [Google Scholar]
- Sinopoli, A , Saulle, R , Marino, M , De Belvis, AG , Federici, A , & La Torre, G (2018). The PRECEDE–PROCEED model as a tool in Public Health screening. European Journal of Public Health, 28, (suppl_4), 372. 10.1093/eurpub/cky214.182. [DOI] [PubMed] [Google Scholar]
- Trivedi, D. (2014). Cochrane Review Summary: Psychosocial and psychological interventions for preventing postpartum depression. Primary Health Care Research & Development, 15(3), 231–233. 10.1017/S1463423614000206 [DOI] [PubMed] [Google Scholar]
- Veisani, Y. , Delpisheh, A. , Sayehmiri, K. , & Rezaeian, S. (2013). Trends of postpartum depression in Iran: A systematic review and meta‐analysis. Depression Research and Treatment, 2013, 8. 10.1155/2013/291029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim, I. S. , Stapleton, L. R. T. , Guardino, C. M. , Hahn‐Holbrook, J. , & Schetter, C. D. (2015). Biological and psychosocial predictors of postpartum depression: Systematic review and call for integration. Annual Review of Clinical Psychology, 11(1), 99–137. 10.1146/annurev-clinpsy-101414-020426 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data are not available.


