Abstract
Aim
This study aimed to investigate the transition from hospital to home after elective colorectal surgery performed in an Enhanced Recovery After Surgery (ERAS) programme.
Design
An integrative review.
Methods
A search of ten electronic databases was conducted. Data extraction and quality assessment were performed independently by two authors. Data analysis and synthesis were based on Meleis’ Transitions Theory (2010).
Results
Forty‐two articles were included, and most (N = 27) were of good or very good quality. The researchers identified five categories to document the nature of transition postsurgery, three conditions affecting such transition, eleven indicators informing about the quality of the transition and several nursing interventions. Overall, this review revealed that the transition from hospital to home after ERAS colorectal surgery is complex. A holistic understanding of this phenomenon may help nurses to recognize what they need to do to optimize the in‐home recovery of this clientele.
Keywords: enhanced recovery after surgery, integrative review, nurses, nursing, nursing theory, postoperative care, transitional care
1. INTRODUCTION
Since their introduction in the late 1990s, Enhanced Recovery After Surgery (ERAS) protocols have become the gold standard in the management of elective colorectal surgeries (Abeles et al., 2017). Briefly, these programmes offer a set of practices grouped into seven main principles including: pre‐admission counselling, reduction of physiological stress, perioperative maintenance of normothermia and normovolemia, use of minimally invasive techniques, early postoperative feeding, early postoperative mobilization and promotion of comfort. If applied correctly, ERAS programme can improve postoperative recovery and reduce hospital length of stay after colorectal surgery (Greco et al., 2014; Spanjersberg et al., 2011; Zhuang et al., 2013).
While evidence support the utility of ERAS to accelerate surgical patients discharge from hospital to home, the benefit of such programmes to avoid hospital readmission remains to be demonstrated (Greco et al., 2014; Lv et al., 2012; Varadhan et al., 2010; Zhuang et al., 2013). In fact, several studies have reported high readmission rates (from 9%–25%) in the 30 days following elective colorectal surgery (Adamina et al., 2011; Al‐Mazrou et al., 2018; Damle & Alavi, 2016; Lawson et al., 2014). These statistics suggest some difficulties in colorectal patients’ transition from hospital to home. Indeed, surgery implies several transitions for patients not only in terms of hospitalization, but also in the regaining of autonomy (Gonzalez et al., 2017). However, surgical recovery is not limited to the length of stay. It also relies on the patients perception of regaining their full capacity and independence once at home (Neville et al., 2014). Despite the importance of these aspects, no comprehensive study has described the global process of transition after colorectal surgery in an ERAS programme from hospital discharge until the patient's complete recovery at home.
2. BACKGROUND
According to the World Health Organization (World Health Organization, 2016), transitions in health refer to all the times when the patient moves or returns to a particular physical place, or comes into contact with a professional to receive health care. The occurrence of surgery implies several transitions for the patient both in terms of the context of care (ranging from the pre‐admission clinic to the postoperative care unit) and in the recovery of autonomy after surgery (Gonzalez et al., 2017). Of all transitions, returning home after hospitalization is recognized as a pivotal step in surgical recovery, which places the patient in a particularly vulnerable position since he/she is left to fend for himself (Kelly et al., 2016; Neville et al., 2014).
Several studies allow us to identify key factors that may affect the transition from hospital to home after colorectal surgery. Thus, advanced age, pre‐operative treatments, the presence of postoperative complications or comorbidities, and the creation of a stoma can all pre‐dispose patients to a greater risk of readmission after colorectal surgery (Al‐Mazrou et al., 2018; Damle & Alavi, 2016; Greenblatt et al., 2010; Lawson et al., 2014). In return, younger age, preparation for discharge and the presence of a support network are factors that facilitate the transition to home after hospitalization (Bragstad et al., 2012; Martin et al., 2017). The feeling of being ready to leave at the time of hospital discharge is another important factor concerning the transition from hospital to home, both in medicine and in surgery (Fiore et al., 2012; Howard‐Anderson et al., 2016). In the context of ERAS programme specifically, a recent study reviewed 11 qualitative studies and showed that: a) the information received before and during hospitalization; b) the burden of symptoms; and c) the feeling of security on discharge are factors that shape the experience of the patient enrolled in an ERAS programme (Sibbern et al., 2017). Although interesting, these results only provide a segmented portrait of all the elements affecting the patient experience during transition to home after colorectal surgery.
In nursing, Meleis’ Transitions Theory (2010) provides a framework for application in practice, research and theory building. The rationale for considering this as an important area for nursing is that people undergoing transitions tend to be more vulnerable to risks that may affect their health and well‐being. Accordingly, transition in health care includes four domains—the nature of transitions, the transition conditions (both facilitating and restrictive), the patterns of response or quality indicators and nursing interventions which are effective in helping patients regaining stability and a sense of well‐being (Meleis, 2010). The challenge for nurses in supporting patients undergoing transition is to understand transition processes and to help them complete a healthy transition. An integrative literature review informed by Meleis’ Transitions Theory could provide a better understanding of this phenomenon and allow researchers to make recommendations on the elements to be considered by nurses to optimize such transition in this clientele.
3. AIM
This study aimed to summarize the literature relating to the phenomenon of transition from hospital to home after ERAS colorectal surgery performed. Inspired by Meleis’ Transitions Theory (2010), the specific objectives were to (i) describe the nature of the transition experienced by these patients; (ii) describe any facilitating and restrictive conditions known to affect such transition; (iii) identify the different patterns of response or quality indicators that can be measured; and (iv) identify nursing interventions that have been studied to promote hospital to home transition after elective colorectal surgery.
4. METHODS
4.1. Design
An integrative review of literature based on Whittemore and Knafl (2005) approach and PRISMA guidelines (see supplementary material for checklist) was undertaken allowing the combination of diverse sources and multiple perspectives to gain an in‐depth understanding of this complex phenomenon to change clinical practice. The reason for applying this approach was that very little comprehensive research exists about this topic, limiting the development of holistic nursing care in that area.
4.2. Search strategy
The search strategy was developed and tested in collaboration with a qualified Health Sciences Librarian to ensure all relevant terms were used. Term selection referred to colorectal surgery and ERAS recovery programmes. The search was performed between November 2018 and March 2019 in ten databases: CINAHL, MEDLINE/PubMed, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews/EMB Reviews Database of Abstracts of Reviews Effects (DARE)/Cochrane Clinical Answers, Web of Science, Scopus and PsycINFO. For each database, searches were performed using keywords and the Medical Subject Headings. See Table 1 for a description of the search strategy used in CINAHL. The search was limited to English or French articles. This strategy was adapted for the other databases. The search results were imported into the EndNote X8 reference management software for screening and removal of duplicate records. This initial search was completed by examining the reference list of included studies.
Table 1.
Search strategy used in CINAHL database
| Cinahl | |||
|---|---|---|---|
| Search terms for CINAHL |
(MH "Patient Discharge") (MH "Discharge Planning") (MH "Early Patient Discharge") (MH "Patient Discharge Education") (MH "Readmission") (MH "Continuity of Patient Care+") (MH "Patient Discharge Summaries") (MH "After Care") (MH "Home Health Care") |
(MH "Enterostomy+") (MH "Colectomy") (MH "Colorectal Neoplasms+/SU") |
Recovery (MH "Postoperative Care") (MH "Postoperative Period") (MH "Postoperative Complications") |
| Keywords combination | (Discharge N3 (transit* OR plan* OR patient*)) OR (transit* N3 (home OR care OR recover*)) OR (home N3 (convalesc* OR recover*) OR (after N2 care)) | ||
| Colectomy OR Enterostomy OR Colostomy OR Ileostomy OR Enterostomy OR ((Colonic OR Colorectal Stoma OR rectal) N4 surger*) | |||
| Recovery* OR "ERAS" postoperative OR "fast‐track" postoperative | |||
Abbreviations: CINAHL, Cumulative Index to Nursing and Allied Health Literature; ERAS, Enhanced Recovery After Surgery; MH, Medical Subject Heading; SU, surgery.
4.3. Study selection
Titles and abstracts of citations retrieved from the initial search were screened independently and in duplicate by two reviewers (MCR and CA) using the specific inclusion criteria. The inclusion criteria were as follows: (a) any primary study published in a journal; (b) that explores the transition from hospital to home; (c) after colorectal surgery; and (d) in the context of an ERAS programme. Although short‐term hospitalization in a nursing home may sometime be necessary after colorectal surgery, only empirical evidence addressing the direct transition occurring between the patient's departure from the hospital and the time when he reaches full recovery at home was considered in this review. If the eligibility of a study was uncertain from the title and abstract, then the full text was obtained and examined. For studies that have been published more than once, the most complete study was chosen for inclusion. When it was not explicitly stated in the body of the article that the study had been carried out as part of an ERAS programme, the authors were contacted to confirm the information. The references list of each article included at this step was consulted. Articles that had not been identified during the initial search strategy but met the inclusion criteria were also retained. Disagreements at any stage of the selection process were resolved through discussion with a third reviewer (MPRG).
4.4. Data extraction and synthesis
An extraction data table was developed to transcribe the following information from each article: the study ID, the purpose, the design, the sample size, the characteristics of participants, the characteristics of intervention (if any), the study results and the authors' conclusion. The reviewers (MCR, MPGR, CA) piloted the data extraction table on a sample of three papers to ensure data were extracted consistently. Then, data extraction was carried out independently and in duplicate by two reviewers (MCR and CA or MCR and MPRG). Disagreements were resolved through discussion.
4.5. Quality assessment
The Mixed Method Appraisal Tool (MMAT) (Pluye et al., 2011) was used to assess quality of the articles. This tool is specifically designed for the appraisal stage of mixed studies reviews. Quality assessment was carried out independently and in duplicate by two reviewers (MCR and CA or MCR and MPRG). Disagreements were resolved through discussion between reviewers. The scores obtained for each individual question and the final scores were added to the data extraction table. A colour code (red for very low quality, orange for low quality, yellow for average quality, light green for good quality and dark green for very good quality) relating to the general quality of the article according to the MMAT tool was used to help the research team visualize the quality of the articles in the subsequent analysis steps (see Table 2).
Table 2.
Main results relevant to the transition from hospital to home and until patient's complete recovery
| Study ID/country | Design/sample | Main results relevant to the transition from hospital to home and until patient's complete recovery | Relevance to Meleis’ Transition Theory | Quality 1 | |||
|---|---|---|---|---|---|---|---|
| N | C | I | NI | ||||
| Qualitative studies | |||||||
|
1 Blazeby et al. (2010)/UK |
Qualitative/Exploratory N = 22 |
Early discharge is appreciated by the patients. Home seems like a better to recover according to patients because they can accomplish their daily activities with less disruptions than in the hospital. Some patients feel rushed to leave the hospital, increasing burden on the carers. Complications lead to dissatisfaction especially when patients must be readmitted. |
x | x | x | *** | |
|
2 Norlyk and Harder (2011)/Denmark |
Qualitative/Descriptive phenomenological N = 16 |
Patients places their focus now in the whole recovery process. Discomfort causes dilemma between the regimen objectives and the need for rest. The disease and the existential threat cause vulnerability. Interaction with relatives enhance patients’ sense of security./Being able to accomplish their daily activities is considered a favourable recovery indicator./Waiting for the surgery results and lack of information promote insecurity./Patients are generally engaged in and feel responsible for their recovery process. |
x | x | x | ** | |
|
3 Taylor and Burch (2011)/UK |
Qualitative/Descriptive N = 50 |
Patients are impressed by the speed with which they can resume their daily activities following discharge./They consider more appropriate to call the hospital for help instead of their general practitioner./They express vulnerability once at home even if the discharge preparation is considered adequate./They want to know how to get help if needed. | x | * | |||
|
4 Aasa et al. (2013)/Sweden |
Qualitative/Interpretive phenomenology N = 12 |
Once at home, patients need to have the opportunity to ask questions and be listened to./A follow‐up phone call one week after discharge is as important as the pre‐operative session for patients./Family presence at the information session helps patients feel safe and improves their involvement in the recovery process./Trust and confidence in healthcare professionals enhance patients’ sense of security and control. | x | x | x | ** | |
|
5 Bernard and Foss (2014a,b)/UK |
Qualitative/Grounded theory N = 4 |
Patients have mixed perception about the amount of information needed to optimize discharge and home recovery./They prefer early discharge because it reduces life disruption./Unwellness, fatigue and delays in regaining their normal functions affect resumption of daily activities./Patients often rely on social support to optimize home recovery./There is ambiguity in the availability of postdischarge services. | x | x | x | * | |
|
6 Krogsgaard et al. (2014)/Denmark |
Qualitative/Interpretive phenomenology N = 7 |
Patients are concern about symptoms, particularly when they are unfamiliar./They have the motivation to resume their normal activities but are often limited due to weakness and fatigue./They are satisfied with the preparatory information./Hope versus fear when awaiting to obtain the surgery results can cause loss of sleep and chaotic thinking./Patients are more open to discuss their situation with other cancer survivors than with their families./To manage symptoms, patients search for information or rely on their own experience. They avoid reporting unfamiliar symptoms because they fear of the consequences and don't want to disturb. |
x | x | x | *** | |
|
7 Fecher‐Jones and Taylor (2015)/UK |
Qualitative/Interpretive phenomenology N = 11 |
Because of the Enhanced recovery programme (ERP), patients expect quicker recovery even in the presence of symptoms. At home the expectation of being better at home is replaced by worry. The emotional needs were often overlooked because they were not expected or recognized. Perception of control improves ERP compliance. Many patients struggle to achieve their ERP goals due to pain, nausea and fatigue. For stoma patients, bowel function and stoma bag management are sources of anxiety. Patients must rely on family support even though they worry about being a burden. |
x | x | x | **** | |
|
8 Lithner et al. (2015)/Sweden |
Qualitative/Exploratory N = 16 |
Perioperative Information increases patients’ participation and sense of control and helps them managing their daily activities. In contrast, bodily changes and the emotional impact of cancer interfere with resumption of daily activities. The last day in the hospital is confusing and stressful. Lack of information leads to anxiety, insecurity and reduces the ability to participate in the recovery process. |
x | x | x | **** | |
|
9 Gillis et al. (2017)/Canada |
Qualitative/Descriptive N = 27 |
Patients perceive that the ERP should cover all the surgical journey, from diagnosis to recovery. Patients want to take on an active and collaborative part in the programme. Finances, family, work and lack of information are sources of stress during home recovery. Patients generally have adequate general discharge information, but some also have unaddressed specific concerns (wound, gastrointestinal or medical problems) leading to anxiety. Mixed messages and advice caused confusion. Patients would like to have access to a well‐informed resource to answer questions once at home. |
x | x | x | *** | |
|
10 Thomsen and Hølge‐Hazelton (2017)/Denmark |
Qualitative/Participatory action research – interpretative N = 12 |
Even if patients feel ready to leave the hospital, they often feel vulnerable once at home. Family plays a significant and supportive role but the changing interactions between the family and the patient can lead to conflicts of role. Patients reported a feeling of relief when they succeeded in managing the specific situation and a feeling of insecurity when the situation remained unresolved. They felt confident in knowing they were part of a planned follow‐up programme. All patients felt well informed about the surgery; several patients expressed a lack of information and knowledge about problems that could appear after returning home. |
x | **** | |||
| Mixed‐method studies | |||||||
|
11 Wennstrom et al. (2010)/Denmark |
Mixed method N = 31 |
Fatigue, nausea and bowel disturbances are main problems after discharge, but most of them disappear after 4 weeks postsurgery. About one third of patients suffer from nausea during the first week but such condition is no longer present after 3 weeks. During the first 2 weeks postsurgery, about one third of patients have fatigue and difficulty to concentrate and two third have dyspnoea. Patients also have difficulties in walking, carrying heavy objects and during that time period. Social relationships are also reduced for 40% of patients. Patients report difficulties in contacting hospital in case of surgery‐related problems. Readmission rate within 30 days was 10%. |
X | ** | |||
|
12 Lithner et al. (2012)/Sweden |
Mixed method N = 100 (45 in an ERP programme) |
No significant difference was observed in the information needs expressed by ERP patients compared to non‐ERP patients. Half of the patients in both groups needed more information about handling symptoms and problems at home. In both groups, waiting for information about prognosis created uncertainty. In both groups, women and patients with a poorer pre‐operative had lower score on perceived information and would require more time and support for discharge preparation. |
X | X | X | ‐ | |
|
13 Jones et al. (2017)/Canada |
Mixed method ‐ survey N = 222 |
Most patients express satisfaction with the discharge information received and feel ready for discharge. Some patients feel they received inadequate information on handing complications at home. Patients with ostomies generally want more information about what to expect postdischarge and 30% of them report not feeling confident in stoma selfcare. Professional support is essential, including at home. Half of patients wants to be provided with contact information to discuss problems. |
X | * | |||
|
14 Smith et al. (2018)/Sweden |
Mixed method N−105 |
Recovery at home is mostly positive. Nausea and vomiting cause a higher level of distress and lower the sense of control. Bowel and surgery problems is linked to 20% of the stressful events experienced at home. Most frequent coping strategies are acceptance, direct action and social support. Distraction can be used for all stressful events. The least used strategy was religion but was considered most helpful. |
X | X | X | ** | |
| Quantitative/Descriptive and correlational studies | |||||||
|
15 Burch (2012) |
Quantitative/Descriptive N = 200 |
The main areas of concern were bowels (11%), wounds (8%), stoma (5%), lack of energy (3%) and pain (3%). All patients considered the follow‐up call to be useful and reassuring. |
X | ‐ | |||
|
16 Lawrence et al. (2013)/USA |
Quantitative/Descriptive N = 860 |
Home health care was used particularly by new ostomy patient. Laparoscopy patients had significantly lower overall readmission rates within 30 days than the open group: 7.2% versus 14.2%. The main indications for readmission were dehydration and small bowel obstruction. |
X | X | X | *** | |
|
17 Partoune et al. (2017)/France |
Quantitative/Descriptive N = 41 |
Hospital discharge was a stressful experience for about a quarter of the patients. A third of patients were surprised to be allowed to leave the hospital and did not feel fit to go home. Half of patients returned to full autonomy once at home and 80% of them attributed their quick recovery to ERP. Half of patients would have liked more information prior discharge. Once at home, the stress related to discharge tended to decrease in the elderly but persisted in younger patients (6% vs. 24%). A third of patients had some problems in feeding. |
X | X | * | ||
|
18 Baek et al. (2013)/Korea |
Quantitative/Correlational descriptive N = 303 |
Emergency department visits or readmission within a month after discharge were more frequent in the older group (> 70 years old) (11.7%) than the younger group (≤ 70 years old) (4%). Main cause of readmission was ileus. |
X | X | **** | ||
|
19 Gustafsson et al. (2011)/Sweden |
Quantitative/Correlational descriptive N = 953 |
Rise in ERP protocol adherence (about 27%) is associated with a reduction in relative risk of 30‐day morbidity (decrease of 27%) and the occurrence of symptoms causing delayed discharge (decrease of 47%). | X | X | X | **** | |
|
20 Feroci et al. (2013)/Italy |
Quantitative/Correlational descriptive N = 606 |
Readmission rate was within 30 days was of 2.3%. Reasons for readmission were anastomotic leakage, ileus, metabolic disorders caused by ileostomy, intra‐abdominal abscess and pneumonia. Age (> 75 years old) was an independent predictor of mortality and morbidity. American Society of Anesthesiologists (ASA) grade was an independent predictor of morbidity. |
X | X | **** | ||
|
21 Krpata et al. (2013)/USA |
Quantitative/Correlational descriptive N = 193 |
Readmission rate within 30 days was 10.4%. The white blood cell count two days after surgery and the difference from baseline were associated with readmission. An elevated white blood count cell on postoperative day 2 was a significant predictor of readmission. |
X | X | ** | ||
|
22 Keller, Swendsteid, Khan et al. (2014)/USA |
Quantitative/Descriptive N = 332 (Ileostomy surgery patients) |
Small bowel obstruction and dehydration were the most frequent readmission diagnoses. 17% of readmitted patients received neoadjuvant therapy before their index operation and ileostomy reversal. Readmission rate within 30 days was of 12.4%. |
X | X | **** | ||
|
23 Keller, Swendsteid, Khorgami et al. (2014)/USA |
Quantitative/Correlational descriptive N = 3,504 |
Higher ASA score, anterior abdominal surgery, intensive care unit stay and dysmotility/constipation surgery were all independent predictors for readmission. A procedure performed by an anorectal approach was a protective factor for readmission. |
X | X | **** | ||
|
24 Chand et al. (2015)/UK |
Quantitative/Correlational descriptive N = 244 |
Patients suffering from obesity had a statistically significant higher ASA grade. | X | *** | |||
|
25 Francis et al. (2015)/UK |
Quantitative/Correlational descriptive N = 268 |
Readmission rate within 30 days was of 12.7%. Bowel obstruction and infection were the most frequent reasons for readmission. ERP programme adherence lower than 93% and pre‐operative neoadjuvant therapy were independent predictors of 30‐day readmission for patients with rectal cancer. |
X | X | *** | ||
|
26 Pisarka et al. (2016)/Poland |
Quantitative/Correlational descriptive N = 251 |
There was a significant decrease in complication rate and severity of complications with increasing compliance to the ERAS protocol. | X | X | **** | ||
|
27 Curtis et al. (2017)/UK |
Quantitative/Correlational descriptive N = 1,023 |
Readmission rate within 30 days was of 16%. Bowel dysfunction and wound complications were the most frequent reasons for readmission. Younger age, rectal cancer and longer initial length of stay were significant predictors of readmission. |
X | X | *** | ||
|
28 Pecorelli et al. (2017)/Canada |
Quantitative/Correlational descriptive N = 347 |
ERP adherence was associated with successful recovery, lower length of stay and lower 30‐day morbidity. Most common reasons for readmission were intraperitoneal or pelvic abscess, bowel obstruction, anastomotic leak and other gastrointestinal complications. Laparoscopy, early mobilization and early termination of IV infusion were predictors of recovery, morbidity and complication severity. |
X | X | *** | ||
|
29 Bennedsen et al. (2018)/Denmark |
Quantitative/Correlational descriptive N = 587 |
Readmission rate within 30 days was of 14%. Surgical complications were the main cause of readmissions. ASA score ≥ 3, total mesorectal excision and operation time ≥ 300 min were significantly associated with readmission. | X | X | **** | ||
|
30 Braga et al. (2018)/Italy |
Quantitative/Correlational descriptive N = 315 |
Median time for readiness for discharge and length of hospital stay were longer with increasing age. | X | *** | |||
|
31 Wood et al. (2018)/Canada |
Quantitative/Correlational descriptive N = 2,876 |
Most common emergency room reasons for consultation were surgical site infections (34.5%), wound complications (10%) and urinary tract infections (8.6%). Ileus and nausea/vomiting (26.1%), intra‐abdominal abscess (23.9%) and surgical site infection (11.5%) were the most common causes of readmission. Extreme body mass index, rectal surgery and open surgery were independent factors of emergency room consultation. Rectal surgery, stoma formation surgery and reoperation were independent factors for readmission. |
X | X | **** | ||
|
32 Jakobsson et al. (2016)/Sweden |
Quantitative/Correlational descriptive N = 105 |
Poor recovery on the day of discharge was a predictor of recovery at 1 month. Better pre‐operative health was associated with several dimensions of good recovery at 1 month. Abdominoperineal resection, length of stay and presence of stoma were associated with several dimensions of bad recovery 1 month after surgery. Higher ASA, longer length of stay and presence of stoma were associated with several dimensions of bad recovery at 6 months. |
X | X | *** | ||
|
33 Yuen et al. (2016) Canada |
Quantitative/Correlational descriptive N = 2,582 |
There were not more complications or readmission between patients discharged 2 days after surgery than patients discharged later. Male sex, smoking and open surgery were found to be independent predictors of 30‐day adverse events. Longer operative time, hypertension and open surgery were independent predictors of 30‐day readmission. |
X | X | ** | ||
| Quantitative/Pre‐experimental and experimental studies | |||||||
|
34 Ihedioha et al. (2012)/UK |
Quantitative/Pre‐experimental N = 32 |
Oral information was considered the most useful information for 56% of patients compared to video information for 26% of patients and written material information for 16% of patients. | X | * | |||
|
35 Stewart et al. (2012)/UK |
Quantitative/Pre‐experimental N = 72 |
Patients were contacted by telephone on two occasions following discharge by a clinical nurse practitioner. The readmission rate after this intervention was 2.7% versus 5,8% prior the intervention. Some patients (8.3%) contacted the clinical nurse practitioner for advice. |
X | X | ** | ||
|
36 Carrier et al. (2016)/France |
Quantitative/Pre‐experimental (Pilot study) N = 111 |
An intervention of home surveillance by text messaging was found feasible and acceptable for patients. The text alerts were mostly caused by poor observance of pain management medication, banal symptoms not being linked to a surgical complication, or text‐messaging errors. Median satisfaction was 5 (scale from 1 to 5). |
X | *** | |||
|
37 Pajaron‐Guerrero et al. (2017)/Spain |
Quantitative/Pre‐experimental/N = 50 | For patients that attained discharge criteria, hospital‐at‐home intervention, including nursing or medical daily monitoring was found safe and led to a theoretical saving of EUR 3,171 by episode. | X | X | ** | ||
|
38 Bragg et al. (2017)/UK |
Quantitative/Pre‐experimental (Pilot study) N = 18 | Use of telehealth in the early follow‐up of patients after discharge was found feasible and acceptable for patients. | X | X | **** | ||
|
39 Fabrizion et al. (2017)/USA |
Quantitative/Pre‐experimental N = 607 |
Implementation of ERP did impact on length of stay but did not on 30‐day readmission rate. ERPs did not impact perceptions of care transitions. |
X | *** | |||
|
40 Shah et al. (2017)/USA |
Quantitative/Pre‐experimental N = 707 |
ERAS protocol decreased risk of readmission and ileostomy increased the risk of readmission. | X | X | *** | ||
|
41 Ihedioha et al. (2013)/UK |
Quantitative/Randomized control trial N = 60 |
The use of video education (15‐min clip that explained patients’ pre‐operative assessment and recovery after surgery including postoperative advice on discharge) as a supplement to verbal and written information did not improve length of stay, pain, nausea or health status measured with SF‐36. | X | X | *** | ||
|
42 Forsmo et al. (2018)/Norway |
Quantitative/Randomized control trial N = 164 |
Extended pre‐operative counselling performed by a dedicated ERAS nurse reduced length of stay but not morbidity; reoperation rate; readmission rate and 30‐day mortality. | X | X | *** | ||
Quality score on MMAT score (Pluye, 2011) 100%, 75%, 50%, 25%, 0%.
4.6. Data analysis
An in‐depth content analysis was performed for each of the components of Meleis’ Transitions Theory. Briefly, all the empirical evidence relating to the nature of the transition were grouped by theme, according to the trajectory of the transition. A similar exercise was carried out for the other components (conditions, indicators, nursing intervention). Analysis was first performed by one reviewer (MCR) and validated by the two others (MPRG and CA). Results of analysis are summarized in the Data extraction and data analysis table (see Table 2).
4.7. Ethics
As this review was performed on published data, patients were not directly involved in any stages of the review process. Thus, research ethics board approval and acquisition of patient informed consent were not required.
5. RESULTS
5.1. 5.1 Summary of search results
Figure 1 presents the PRISMA flow diagram of the systematic search. The initial search strategy yielded 1,590 citations. After removing duplicates, 1,180 citations remained and were screened for eligibility based on title and abstract examination. Of them, 1,079 did not meet the inclusion criteria (see Figure 1 for specific reasons), leaving 101 articles for full‐text retrieval. Following detailed examination, 34 articles met the inclusion criteria. After reading the reference list of 34 included articles, 8 other relevant articles were retained. A total of 42 original articles were included in the final review. Of these studies, 28 were quantitative, 10 were qualitative, and 4 used a mixed‐methods design.
Fig. 1.

PRISMA flow diagram of search strategy
5.2. Articles quality appraisal
According to the quality score on the MMAT, 12 articles can be considered of very good quality, 15 of good quality, eight of medium quality, five of low quality and two of very poor quality. The main limitations of qualitative studies include the lack of data saturation and the response bias linked to the researcher's involvement in the care team. The main limitations of few quantitative studies are the small sample sizes, the use of an unvalidated measurement tool or the absence of a control group for experimental studies.
5.3. Nature of the transition
The nature of the transition can be summarized into five categories that overlap throughout colorectal surgery patients’ trajectory from hospital to home: (a) expectations and preparation; (b) experience of early discharge; (c) awareness of the transition experience; (d) self‐management; and (e) follow‐up and support.
5.3.1. Expectations and preparation
Elective colorectal surgery patients generally feel confident in their ability to experience a healthy recovery at home because they are enrolled in a planned follow‐up programme and consider home to be a better place to recover (Fecher‐Jones & Taylor, 2015; Thomsen & Hølge‐Hazelton, 2017). However, patient satisfaction towards transition preparation is mixed. Although most patients are satisfied with the preparation for discharge, (Gillis et al., 2017; Jones et al., 2017; Krogsgaard et al., 2014; Taylor & Burch, 2011; Thomsen & Hølge‐Hazelton, 2017), other results suggest that preparation for discharge is deficient and sometimes marked by contradictory advice (Aasa et al., 2013; Gillis et al., 2017; Lithner et al., 2012; Partoune et al., 2017; Thomsen & Hølge‐Hazelton, 2017). Patients would also like the information to be more personalized to their individual needs (Bernard & Foss, 2014a, 2014b; Jones et al., 2017).
5.3.2. Experience of early discharge
The day of hospital discharge is often a stressful moment for elective colorectal surgery patients (Lithner et al., 2015; Partoune et al., 2017). They sometimes feel pressured to leave (Blazeby et al., 2010; Partoune et al., 2017). On the other hand, they appreciate that most of the recovery will take place in their own home (Smith et al., 2018), because it will allow them to reinstate their routine even if that implies additional responsibilities in taking care of themselves (Bernard & Foss, 2014a,b; Blazeby et al., 2010).
5.3.3. Awareness of the transition experience
Once at home, most elective colorectal surgery patients feel very vulnerable (Fecher‐Jones & Taylor, 2015; Taylor & Burch, 2011; Thomsen & Hølge‐Hazelton, 2017). The fact that they now have to take full responsibility for their condition (Thomsen & Hølge‐Hazelton, 2017), the impression that recovery should be quicker (Fecher‐Jones & Taylor, 2015) and disease severity (Norlyk & Harder, 2011; Wennstrom et al., 2010) all contribute to this feeling of vulnerability. New onset of symptoms can also make the patients feel more vulnerable. During the first two weeks of hospital discharge, difficulty concentrating, moving objects, walking, breathing (Wennstrom et al., 2010) and eating are commonly reported (Partoune et al., 2017). Fatigue, gastrointestinal discomfort and nausea are also common in the first month postdischarge (Wennstrom et al., 2010).
5.3.4. Recovery self‐management
Elective colorectal surgery patients generally engage actively in their recovery process (Aasa et al., 2013; Norlyk & Harder, 2011). As a result, most of them regain their autonomy quickly (Krogsgaard et al., 2014; Partoune et al., 2017). Still, patients' ability to perform self‐care can lead to conflicting feelings. On one side, they feel relieved when they can manage a problem well. On the other, they feel insecure when they are unable to do so (Thomsen & Hølge‐Hazelton, 2017). In terms of coping strategies, patients mostly use preparation information to manage problems at home (Lithner et al., 2015). They also rely on acceptance of their condition, or direct action in case of problems in particular when the problem is related to ostomy (Smith et al., 2018). Indeed, management of self‐care is an important source of anxiety for ostomy patients (Fecher‐Jones & Taylor, 2015). A third of ostomy patients have little confidence in self‐care and show greater information needs in terms of symptoms management (Jones et al., 2017).
5.3.5. Follow‐up and social support
Most elective colorectal surgery patients express the need to have easy access to a trusted contact person for clinical follow‐up and informational support (Aasa et al., 2013; Gillis et al., 2017; Jones et al., 2017; Taylor & Burch, 2011). The need for acquiring information relating to the management of gastrointestinal disorders (Smith et al., 2018; Wennstrom et al., 2010), ostomy or wound care, pain and lack of energy is often reported (Burch, 2012). Paradoxically, patients often avoid contacting the nurse in charge of their follow‐up because they feel they should not have to or do not want to disturb (Fecher‐Jones & Taylor, 2015; Krogsgaard et al., 2014). They indicate that access to nursing follow‐up in person or by telephone at home is essential, especially for advice on managing ostomy or wound care (Burch, 2012; Lawrence et al., 2013). However, during all the surgical trajectory, patients report that their emotional needs should be more noticed and taken into account by health professionals (Aasa et al., 2013; Fecher‐Jones & Taylor, 2015).
Once at home, colorectal surgery patients rely strongly on relatives for support (Bernard & Foss, 2014a,b; Fecher‐Jones & Taylor, 2015; Thomsen & Hølge‐Hazelton, 2017). However, they may experience conflicting relationships with loved ones during their convalescence as a result of changing roles in the family unit (Thomsen & Hølge‐Hazelton, 2017). During the first two weeks after returning home, difficulties in performing daily activities reduce family and social relationships (Wennstrom et al., 2010). As a consequence, some patients will try to be very independent at home so as to not be a burden for loved ones (Blazeby et al., 2010; Fecher‐Jones & Taylor, 2015). In terms of social support, patients stated to be more comfortable to discuss their situation with other cancer survivors who have had similar health experiences (Krogsgaard et al., 2014).
5.4. Facilitating and restrictive conditions
Conditions affecting the transition from hospital to home after elective colorectal surgeries are related to (a) the surgery; (b) patient and his/her family; and (c) healthcare services.
5.4.1. Conditions related to the surgery
Surgery type, hospitalization characteristics and surgical complications are all surgery‐related conditions that may potentially have an impact on the quality of transition after elective colorectal surgery. Minimally invasive laparoscopic surgery (Pecorelli et al., 2017) and anorectal approach contribute to a better recovery and a lower risk of readmission and complications severity (Keller et al., 2014; Lawrence et al., 2013; Wood et al., 2018; Yuen et al., 2016). Inversely, stoma creation surgery, rectal surgery, total mesorectal excision and longer surgical procedures are related to a higher risk of emergency room consultation (Wood et al., 2018) and the readmission (Bennedsen et al., 2018; Shah et al., 2017; Wood et al., 2018; Yuen et al., 2016). Abdominoperineal resection of the rectum is associated with several dimension of poor recovery at one month (Jakobsson et al., 2016). Patients requiring hospitalization to the intensive care unit (Keller et al., 2014) and those with prolonged length of stay (Curtis et al., 2017; Jakobsson et al., 2016) or requiring reoperation (Wood et al., 2018) have more chances to be readmitted. Surgical complications, such as anastomotic leak, intra‐abdominal abscess and gastrointestinal disorders, including nausea and vomiting or ileus and obstruction, are the main reasons for emergency room consultation and readmission (Baek et al., 2013; Bennedsen et al., 2018; Curtis et al., 2017; Feroci et al., 2013; Lawrence et al., 2013; Pecorelli et al., 2017; Wood et al., 2018). Infectious diseases, such as surgical site infection, urinary tract infection and pneumonia are also frequent causes for emergency room consultation and readmission (Curtis et al., 2017; Feroci et al., 2013; Keller et al., 2014; Wood et al., 2018).
5.4.2. Conditions related to the patient and his/her family
Patient's characteristics can influence the quality of the transition from hospital to home after elective colorectal surgery. Indeed, advancing in age extends the time required to be ready to discharge and increases the risk of readmission (Braga et al., 2018; Feroci et al., 2013). However, younger patients may be more stressed at home (Partoune et al., 2017). A high American Society of Anesthesiologists (ASA) score (an indicator of poor physical status) is another characteristic that increases the risk of readmission (Bennedsen et al., 2018; Keller et al., 2014) and postoperative morbidity (Feroci et al., 2013). Even if obesity is associated to a higher ASA score (Chand et al., 2015), only extreme body mass index patients have a higher risk of readmission (Wood et al., 2018). An history of past abdominal surgery is another characteristic that increases the risk of readmission (Keller et al., 2014). Finally, smoking and male sex are generally associated with a higher risk of 30‐day adverse events, while hypertension is associated with higher risk of 30‐day readmission (Yuen et al., 2016). For cancer patients, a diagnostic of rectal neoplasm (Curtis et al., 2017) and pre‐operative neoadjuvant treatment increases (Francis et al., 2015) the risk of readmission. Female cancer patients and those with lower pre‐operative health status in particular may have more difficulty to perceive information and, therefore, would thereby need more support (Lithner et al., 2012).
Presence of symptoms may also affect the quality of the transition. In fact, bodily and emotional changes affect the patient ability to manage daily life activities (Lithner et al., 2015). More specifically, pain, nausea and fatigue reduce patients’ capacity to perform the ERAS daily goals (Fecher‐Jones & Taylor, 2015). Fatigue and weakness also impede patients to do more demanding activities (Bernard & Foss, 2014a,b; Krogsgaard et al., 2014). Nausea and the incapacity to identify unfamiliar symptoms increase the patient's feeling of distress (Krogsgaard et al., 2014; Smith et al., 2018).
Patient engagement towards his/her care and family relations are known to influence the quality of the transition. More specifically, patient's motivation enhances his/her ability to achieve the programme daily goals (Krogsgaard et al., 2014). Likewise, patient's sense of control over the situation (Fecher‐Jones & Taylor, 2015) is increased when the patient manage his/her own care (Aasa et al., 2013). On the other hand, family interactions raise the patient's sense of security (Norlyk & Harder, 2011). It seems that the presence of a family member at the pre‐operative counselling and education session favours patients and family level of engagement in the home recovery process (Aasa et al., 2013).
5.4.3. Conditions related to healthcare services
Colorectal surgery patients perceive that the healthcare services embedded into the ERAS programme are responsible for their rapid autonomy regain (Partoune et al., 2017). Supporting this perception, a higher adherence to the ERAS protocols reduces the 30‐day mortality rate (Gustafsson et al., 2011; Pecorelli et al., 2017), the risk of readmission (Francis et al., 2015) and the risk of complications (Pisarska et al., 2016). Trust in healthcare professionals also enhances patients’ sense of security and control (Aasa et al., 2013), while encouragements and information transmitted by them may promote patients’ sense of responsibility (Aasa et al., 2013; Bernard & Foss, 2014a,b; Lithner et al., 2015). Information about the ERAS programme specifically increases patients’ participation in self‐care at home (Gillis et al., 2017; Lithner et al., 2015). Inversely, lack of information can cause distress and insecurity (Lithner et al., 2015), especially when lack of information concern surgery outcomes and prognosis (Gillis et al., 2017; Lithner et al., 2012; Norlyk & Harder, 2011).
5.5. Quality indicators of transition
The quality of transition from hospital to home following elective colorectal surgery can be assessed through 11 indicators (summarized in Table 3 from most to less frequently mentioned in the selected studies). These indicators include hospital consultation and readmission, level of distress, incidence of morbidity, patient's ability to accomplish daily life activities, as well as patient's sense of security, sense of control, perception of recovery, use of healthcare services, satisfaction, mortality and adverse events.
Table 3.
Name and description of quality indicators of transition
| Indicator name/Description | Authors |
|---|---|
|
Hospital consultation and readmission Refers to the rate or the relative risk for a patient to visit the emergency room service or be readmitted to the hospital |
Baek et al. (2013), Bennedsen et al. (2018), Curtis et al. (2017), Fabrizio et al. (2017), Feroci et al. (2013), Francis et al. (2015), Keller, Swendseid, Khan et al. (2014), Keller, Swendseid, Khorgami et al. (2014), Krpata et al. (2013), Lawrence et al. (2013), Pecorelli et al. (2017), Pisarska et al. (2016), Shah et al. (2017), Stewart et al. (2012), Wood et al. (2018), Yuen et al. (2016) |
|
Level of distress Refers to the occurrence or the intensity of patient's distress including anxiety (doubt (uncertainty (fear (anguish and stress |
Fecher‐Jones and Taylor (2015), Gillis et al. (2017), Jakobsson et al. (2016), Krogsgaard et al. (2014), Lithner et al. (2012), Lither et al. (2015), Partoune et al. (2017), Smith et al. (2018) |
|
Morbidity Refers to the relative risk of factors contributing to patient's morbidity or general health status |
Feroci et al. (2013), Gustafsson et al. (2011), Ihedioha et al. (2013), Jakonssob et al. (2016), Pecorelli et al. (2017) |
|
Daily life activities Refers to the patient's ability to accomplish his/her daily life activities almost to the same level as before the surgery |
Bernard and Foss (2014a,b), Krogsgaard et al. (2014), Lithner et al. (2015), Norlyk and Harder (2011) |
|
Sense of security Refers to the patient's perception of being in security |
Aasa et al. (2013), Lithner et al. (2015), Norlyk and Harder (2011) |
|
Sense of control Refers to the patient's perception of being in control of his/her life situation |
Aasa et al. (2013), Fecher‐Jones and Taylor (2015), Lithner et al. (2015) |
|
Perception of recovery Refers to the patient's perception of having fully recovered from the surgery both physically and psychologically |
Fecher‐Jones and Taylor (2015), Pecorelli et al. (2017) |
|
Utilization of healthcare services Refers to the level or rate of patient's demand for healthcare services |
Bragg et al. (2017), Stewart et al. (2012) |
|
Satisfaction Refers to the level of satisfaction expressed by the patients about a specific aspect of the surgery trajectory or its globality |
Blazeby et al. (2010), Feroci et al. (2013) |
|
Mortality Refers to the relative risk of factors contributing to patient's mortality |
Feroci et al. (2013) |
|
Adverse events Refers to the relative risk of factors contributing to adverse events or complications |
Yuen et al. (2016) |
5.6. Nursing interventions
Pre‐operative counselling and education and postoperative monitoring and follow‐ups are two types of nursing interventions that have been tested to help with the transition from hospital to home after elective colorectal surgery. There were only few studies about nursing interventions. Therefore, the results are not as rich than those about the other components.
5.6.1. Pre‐operative counselling and education
An educational 15‐min pre‐operative video explaining patients’ pre‐operative assessment and recovery has been tested. Even if more than 90% of participants considered the video was relevant and useful for their recovery, no effect was found on length of stay, pain, nausea or 3‐month postoperative health status (Ihedioha et al., 2013) in a randomized controlled trial (RCT) study (N = 61).
One or two additional 30–45 pre‐operative counselling sessions by a dedicated ERAS nurse including information about the operation, hospital stay and pain management have been assessed in an RCT involving cancer patients (N = 164). According to the study results, this intervention may reduce hospital length of stay and increase adherence to postoperative ERAS recommendations but the impact on readmissions, morbidity and mortality could not be established (Forsmo et al., 2018).
5.6.2. Postoperative monitoring and follow‐up
Two pilot studies (Bragg et al., 2017; Carrier et al., 2016) have been conducted to evaluate the feasibility of text messaging for recovery monitoring following elective colorectal surgery. The intervention involved the automatic sending of text messages to patients to assess symptoms. Patients’ responses were analysed by a healthcare professional who contacted those reporting concerns or abnormal symptoms for further assessment. Combined, these studies showed that text‐messaging monitoring is not only safe and satisfactory for patients, but it could reduce the number of telephone consultations during postoperative recovery (Bragg et al., 2017).
Like text‐messaging monitoring, telephone follow‐up could contribute to decrease hospital readmission after elective colorectal surgery (5.8%–2.7%) according to a small pre‐experimental study (Stewart et al., 2012). In this study, patients were contacted by telephone two times after discharge by a clinical nurse practitioner.
More recently, the safety of a hospital‐at‐home (HAH) model of care has been studied. This intervention involved a home care nursing and medical systematic follow‐up monitoring lasting seven days after the surgery, for patients who had met the discharge criteria and had been sent home at day 3 after surgery. Such intervention was found safe and allowed a theoretical economy of more than 3,000 Euros per healthcare episode, based on the hospitalization cost savings (Pajaron‐Guerrero et al., 2017).
6. DISCUSSION
The aim of this integrative review of the literature was to summarize the existing literature addressing the transition from hospital to home after elective colorectal surgery performed in an ERAS programme. Overall, 42 articles were reviewed and analysed. Relevant data were categorized according to the four components of Meleis’ Transitions Theory (2010). Through this categorization, this review identified five categories relating to the nature of the transition, three main themes of conditions affecting the transition, eleven indicators that can inform about the quality of the transition and two types of nursing interventions that have been tested to help with the transition from hospital to home in these patients. Using Meleis’ Transitions Theory framework, a tentative model of the phenomenon of transition from hospital to home after an ERAS colorectal surgery programme was produced (Figure 2). The model depicts how ERAS nurses, researchers and policymakers may set standards of care and measure quality of hospital to home transition following elective colorectal surgery.
Fig. 2.
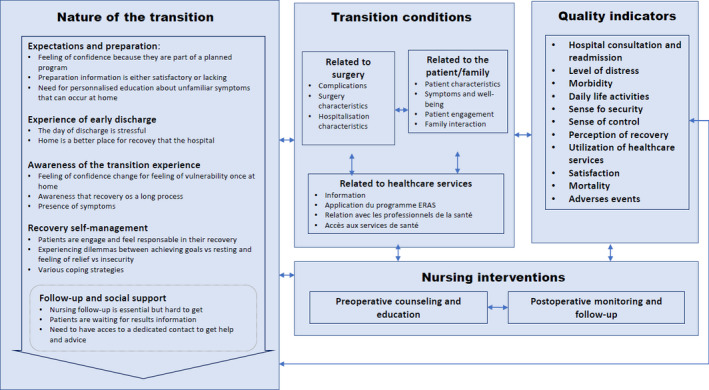
Phenomenon of transition from hospital to home after ERAS programme colorectal surgery
Taking each component of Meleis’ Transitions Theory (2010) individually, our review show that the recovery process following elective colorectal surgery is longer and more complex than the hospital stay. These results are consistent with those of Sibbern et al. (2017) showing that colorectal surgery patients become particularly vulnerable in the first few days following home reintegration, mainly because symptom burden and self‐care needs are still high during that period. These patients require personalized information and support from both their loved ones and from healthcare professionals to maintain a sense of security after discharge (Aasa et al., 2013; Lithner et al., 2015; Norlyk & Harder, 2011). Unfortunately, the ERAS Guidelines for Perioperative Care in Elective Colorectal Surgery (Gustafsson et al., 2019) have no specific recommendation for clinicians on how to optimize the transition from hospital to home in this clientele. However, they do recommend the implication of the family in the pre‐operative preparation. Our review shows the importance of family implication not only during the pre‐operative period, but rather throughout the hospital recovery process and during the transition from hospital to home and until the patient's complete recovery. Patients also expressed the need for nursing support once at home to be able to ask questions, to help them manage their physical and psychological symptoms (Aasa et al., 2013; Gillis et al., 2017; Jones et al., 2017; Taylor & Burch, 2011; Thomsen & Hølge‐Hazelton, 2017).
This review also highlights the wide panoply of conditions (eleven in total) that may interfere with patient's transition from hospital to home after elective colorectal surgery. This suggests that the addition of a thorough assessment of risk of difficulty in transition could be beneficial to personalized hospital discharge planning and optimize the transition from hospital to home and until the patient's complete recovery.
More importantly, this shows the limits of the systematic practices promoted by ERAS philosophy. Surgical and hospitalization conditions and some patient's characteristic must be recognized by the nurse to personalized transitional care and decrease the risk of readmission (Baek et al., 2013; Bennedsen et al., 2018; Curtis et al., 2017; Feroci et al., 2013; Keller et al., 2014; Lawrence et al., 2013; Wood et al., 2018; Yuen et al., 2016). Also, the nurse must favours facilitating conditions such as patient and family implication and provide clear information about symptoms management (Aasa et al., 2013; Gillis et al., 2017; Krogsgaard et al., 2014; Lithner et al., 2012, 2015; Norlyk & Harder, 2011; Taylor & Burch, 2011).
As previously mentioned, the application of an ERAS programme for elective colorectal surgery has been shown to shorten length of stay (Greco et al., 2014; Spanjersberg et al., 2011; Zhuang et al., 2013). Still, the true impact of such programmes to optimize or accelerate in‐home recovery remain to be properly investigated. Accordingly, our review has identified eleven quality indicators that could be used by clinicians and researcher to estimate the quality of recovery following the transition from hospital to home after elective colorectal surgery. Considering the frequency of citations in the reviewed articles, patient hospital consultation and readmission, level of distress, morbidity and reuptake of daily life activities are most popular. The use of these indicators could play a major role to demonstrate the effectiveness of nursing care in the optimization of home recovery after colorectal surgery. Indeed, it is well known that transitional nursing care is effective to reduce readmission after hospitalization in other populations (Coleman et al., 2006; Naylor et al., 1999). Our results support the importance of these care throughout recovery process until the total recovery at home. The level of distress happens to be a major indicator to assess the quality of the transition. This result supports the importance of paying more attention to the patient's experience indicator to evaluate ERAS programme.
In terms of concrete nursing interventions that could be implemented to optimize the transition from hospital to home after elective colorectal surgery, pre‐operative counselling was found particularly useful to increase adherence to postoperative ERAS recommendations and decrease hospital length of stay (Forsmo et al., 2018). However, more research is needed to refine the counselling content and processes to have a significant impact on patients’ readmission and the experience of hospital to home transition. Although less validated, postoperative monitoring by text messaging and follow‐up by telephone could be promising to optimize the transition from hospital to home after elective colorectal surgery (Bragg et al., 2017; Carrier et al., 2016). Even if this intervention needs more research to clearly demonstrate its effectiveness to optimize transition to home after ERAS surgery, this type of intervention is recommended in the ERAS guidelines (Gustaffson et al., 2019) and seems to be appreciated by patients (Burch, 2012; Lawrence et al., 2013).
6.1. Limitations
This review was not without limitations. Clearly distinguishing a study results relating to the nature of the transition rather than to a condition (as conceptualized by Meleis’ Transitions Theory) was not always easy. Taking social support, for instance, it was considered to be part of nature in some studies because it was reported by patients as an integral part of the transition. In other studies, however, interaction with loved ones (a concept similar to social support) was considered a facilitating condition, since it has a positive effect on one indicator, the feeling of security. Another weakness stems from the methodological shortcomings of the studies selected (mainly those with a qualitative design) for carrying out this integrative review, as well as the lack of inclusion of theoretical studies on transition. Considering the high number of primary studies identified (n = 42), the research team decided to limit the search to these writings. The use of Meleis’ Transitions Theory (2010) as a theoretical grounding compensate for this limitation.
7. CONCLUSION
ERAS programmes are one of the most important advancements in surgical practice in the last decades, but its efficacy on the patient's full recovery remained to be demonstrated. This integrative review imbedded in Meleis’ Transitions Theory (2010) highlights healthcare gaps that lead patients to a state of vulnerability once at home and support the necessity to enhanced transitional care. Nurses could play a pivotal role to optimize the transitional experience that can then lead to better outcomes on readmission and complications of the patients enrolled in an ERAS programme for elective colorectal surgery.
8. RELEVANCE TO CLINICAL PRACTICE
ERAS nurses should assess the needs of patients and family to personalized hospital discharge planning and optimize the transition from hospital to home and until the patient's complete recovery.
ERAS nurses should be involved in the postdischarge assessment of home transition quality indicators, mainly patients’ level of distress in the ability to accomplish their daily activities.
Aside from hospital length of stay, the efficacy of ERAS programme on elective colorectal surgery should be evaluated based on outcomes known to be sensitive to patients’ experience of transition from hospital to home until full recovery.
The nursing community needs to pursue research on the validation of nursing interventions to optimize transition from hospital to home after an ERAS colorectal surgery.
CONFLICT OF INTEREST
None to declare.
Funding information
None to declare.
ACKNOWLEDGEMENTS
The authors would like to thank Assia Mourid for supporting search strategy and Professor Anne Bourbonnais for her advices regarding this work.
Ruel M‐C, Ramirez Garcia M‐P, Arbour C. Transition from hospital to home after elective colorectal surgery performed in an enhanced recovery program: An integrative review. Nurs Open. 2021;8:1550–1570. 10.1002/nop2.730
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- World Health Organization . (2016). Transitions of Care: Technical Series on Safer Primary Care.
- Aasa, A. , Hovback, M. , & Bertero, C. M. (2013). The importance of preoperative information for patient participation in colorectal surgery care. Journal of Clinical Nursing, 22(11–12), 1604–1612. 10.1111/jocn.12110 [DOI] [PubMed] [Google Scholar]
- Abeles, A. , Kwasnicki, R. M. , & Darzi, A. (2017). Enhanced recovery after surgery: Current research insights and future direction. World Journal of Gastrointestinal Surgery, 9(2), 37–45. 10.4240/wjgs.v9.i2.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adamina, M. , Kehlet, H. , Tomlinson, G. A. , Senagore, A. J. , & Delaney, C. P. (2011). Enhanced recovery pathways optimize health outcomes and resource utilization: A meta‐analysis of randomized controlled trials in colorectal surgery. Surgery, 149(6), 830–840. 10.1016/j.surg.2010.11.003 [DOI] [PubMed] [Google Scholar]
- Al‐Mazrou, A. M. , Chiuzan, C. , & Kiran, R. P. (2018). Factors influencing discharge disposition after colectomy. Surgical Endoscopy, 32(7), 3032–3040. 10.1007/s00464-017-6013-z [DOI] [PubMed] [Google Scholar]
- Baek, S. J. , Kim, S. H. , Kim, S. Y. , Shin, J. W. , Kwak, J. M. , & Kim, J. (2013). The safety of a "fast‐track" program after laparoscopic colorectal surgery is comparable in older patients as in younger patients. Surgical Endoscopy, 27(4), 1225–1232. 10.1007/s00464-012-2579-7 [DOI] [PubMed] [Google Scholar]
- Bennedsen, A. L. B. , Eriksen, J. R. , & Gogenur, I. (2018). Prolonged hospital stay and readmission rate in an enhanced recovery after surgery cohort undergoing colorectal cancer surgery. Colorectal Disease, 20(12), 1097–1108. 10.1111/codi.14446 [DOI] [PubMed] [Google Scholar]
- Bernard, H. , & Foss, M. (2014a). The impact of the enhanced recovery after surgery (ERAS) programme on community nursing. British Journal of Community Nursing, 19(4), 184–188. 10.12968/bjcn.2014.19.4.184 [DOI] [PubMed] [Google Scholar]
- Bernard, H. , & Foss, M. (2014b). Patient experiences of enhanced recovery after surgery (ERAS). British Journal of Nursing, 23(2), 100–106. 10.12968/bjon.2014.23.2.100 [DOI] [PubMed] [Google Scholar]
- Blazeby, J. M. , Soulsby, M. , Winstone, K. , King, P. M. , Bulley, S. , & Kennedy, R. H. (2010). A qualitative evaluation of patients' experiences of an enhanced recovery programme for colorectal cancer. Colorectal Disease, 12(10), e236–242. 10.1111/j.1463-1318.2009.02104.x [DOI] [PubMed] [Google Scholar]
- Braga, M. , Beretta, L. , Pecorelli, N. , Maspero, M. , Casiraghi, U. , Borghi, F. , Pellegrino, L. , Bona, S. , Monzani, R. , Ferrari, G. , Radrizzani, D. , Iuliani, R. , Bima, C. , Scatizzi, M. , Missana, G. , Guicciardi, M. A. , Muratore, A. , Crespi, M. , Bouzari, H. , … Ficari, F. (2018). Enhanced recovery pathway in elderly patients undergoing colorectal surgery: Is there an effect of increasing ages? Results from the perioperative Italian Society Registry. Updates in Surgery, 70(1), 7–13. 10.1007/s13304-017-0474-4 [DOI] [PubMed] [Google Scholar]
- Bragg, D. D. , Edis, H. , Clark, S. , Parsons, S. L. , Perumpalath, B. , Lobo, D. N. , & Maxwell‐Armstrong, C. A. (2017). Development of a telehealth monitoring service after colorectal surgery: A feasibility study. World Journal of Gastrointestinal Surgery, 9(9), 193–199. 10.4240/wjgs.v9.i9.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bragstad, L. K. , Kirkevold, M. , Hofoss, D. , & Foss, C. (2012). Factors predicting a successful post‐discharge outcome for individuals aged 80 years and over. International Journal of Integrated Care, 12, e4. 10.5334/ijic.691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burch, J. (2012). Enhanced recovery and nurse‐led telephone follow‐up post surgery. British Journal of Nursing, 21(Sup16), S24–S29. 10.12968/bjon.2012.21.Sup16.S24 [DOI] [PubMed] [Google Scholar]
- Carrier, G. , Cottee, E. , Beyer‐Berjot, L. , Faucheron, J. L. , Joris, J. , Slim, K. (2016). Post‐discharge follow‐up using text messaging within an enhanced recovery program after colorectal surgery. Journal of Visceral Surgery, 153(4), 249–252. 10.1016/j.jviscsurg.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Chand, M. , De'Ath, H. D. , Siddiqui, M. , Mehta, C. , Rasheed, S. , Bromilow, J. , & Qureshi, T. (2015). Obese patients have similar short‐term outcomes to non‐obese in laparoscopic colorectal surgery. World Journal of Gastrointestinal Surgery, 7(10), 261–266. 10.4240/wjgs.v7.i10.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman, E. A. , Parry, C. , Chalmers, S. , & Min, S. (2006). The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine, 166(17), 1822–1828. 10.1001/archinte.166.17.1822 [DOI] [PubMed] [Google Scholar]
- Curtis, N. J. , Noble, E. , Salib, E. , Hipkiss, R. , Meachim, E. , Dalton, R. , Allison, A. , Ockrim, J. , & Francis, N. K. (2017). Does hospital readmission following colorectal cancer resection and enhanced recovery after surgery affect long term survival? Colorectal Disease, 19(8), 723–730. 10.1111/codi.13603 [DOI] [PubMed] [Google Scholar]
- Damle, R. N. , & Alavi, K. (2016). Risk factors for 30‐day readmission after colorectal surgery: A systematic review. Journal of Surgical Research, 200(1), 200–207. 10.1016/j.jss.2015.06.052 [DOI] [PubMed] [Google Scholar]
- Fabrizio, A. C. , Grant, M. C. , Siddiqui, Z. , Alimi, Y. , Gearhart, S. L. , Wu, C. , Efron, J. E. , & Wick, E. C. (2017). Is enhanced recovery enough for reducing 30‐d readmissions after surgery? Journal of Surgical Research, 217, 45–53. 10.1016/j.jss.2017.04.007 [DOI] [PubMed] [Google Scholar]
- Fecher‐Jones, I. , & Taylor, C. (2015). Lived experience, enhanced recovery and laparoscopic colonic resection. British Journal of Nursing, 24(4), 223–228. 10.12968/bjon.2015.24.4.223 [DOI] [PubMed] [Google Scholar]
- Feroci, F. , Lenzi, E. , Baraghini, M. , Garzi, A. , Vannucchi, A. , Cantafio, S. , & Scatizzi, M. (2013). Fast‐track surgery in real life: How patient factors influence outcomes and compliance with an enhanced recovery clinical pathway after colorectal surgery. Surgical Laparoscopy Endoscopy & Percutaneous Techniques, 23(3), 259–265. 10.1097/SLE.0b013e31828ba16f [DOI] [PubMed] [Google Scholar]
- Fiore, J. F. Jr , Bialocerkowski, A. , Browning, L. , Faragher, I. G. , & Denehy, L. (2012). Criteria to determine readiness for hospital discharge following colorectal surgery: An international consensus using the delphi technique. Diseases of the Colon and Rectum, 55(4), 416–423. 10.1097/DCR.0b013e318244a8f2 [DOI] [PubMed] [Google Scholar]
- Forsmo, H. M. , Erichsen, C. , Rasdal, A. , Tvinnereim, J. M. , Korner, H. , & Pfeffer, F. (2018). Randomized controlled trial of extended perioperative counseling in enhanced recovery after colorectal surgery. Diseases of the Colon and Rectum, 61(6), 724–732. 10.1097/dcr.0000000000001007 [DOI] [PubMed] [Google Scholar]
- Francis, N. K. , Mason, J. , Salib, E. , Allanby, L. , Messenger, D. , Allison, A. S. , Smart, N. J. , & Ockrim, J. B. (2015). Factors predicting 30‐day readmission after laparoscopic colorectal cancer surgery within an enhanced recovery programme. Colorectal Disease, 17(7), O148–O154. 10.1111/codi.13002 [DOI] [PubMed] [Google Scholar]
- Gillis, C. , Gill, M. , Marlett, N. , MacKean, G. , GermAnn, K. , Gilmour, L. , Nelson, G. , Wasylak, T. , Nguyen, S. , Araujo, E. , Zelinsky, S. , & Gramlich, L. (2017). Patients as partners in Enhanced Recovery After Surgery: A qualitative patient‐led study. British Medical Journal Open, 7(6), 10. 10.1136/bmjopen-2017-017002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González, M. G. , Kelly, K. N. , Dozier, A. M. , Fleming, F. , Monson, J. R. T. , Becerra, A. Z. , Aquina, C. T. , Probst, C. P. , Hensley, B. J. , Sevdalis, N. , & Noyes, K. (2017). Patient perspectives on transitions of surgical care: examining the complexities and interdependencies of care. Qualitative Health Research, 27(12), 1856–1869. 10.1177/1049732317704406 [DOI] [PubMed] [Google Scholar]
- Greco, M. , Capretti, G. , Beretta, L. , Gemma, M. , Pecorelli, N. , & Braga, M. (2014). Enhanced recovery program in colorectal surgery: A meta‐analysis of randomized controlled trials. World Journal of Surgery, 38(6), 1531–1541. 10.1007/s00268-013-2416-8 [DOI] [PubMed] [Google Scholar]
- Greenblatt, D. Y. , Weber, S. M. , O'Connor, E. S. , LoConte, N. K. , Liou, J. I. , & Smith, M. A. (2010). Readmission after colectomy for cancer predicts one‐year mortality. Annals of Surgery, 251(4), 659–669. 10.1097/SLA.0b013e3181d3d27c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson, U. O. , Hausel, J. , Thorell, A. , Ljungqvist, O. , Soop, M. , & Nygren, J. (2011). Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Archives of Surgery, 146(5), 571–577. 10.1001/archsurg.2010.309 [DOI] [PubMed] [Google Scholar]
- Gustafsson, U. O. , Scott, M. J. , Hubner, M. , Nygren, J. , Demartines, N. , Francis, N. , & Ljungqvist, O. (2019). Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS((R))) society recommendations: 2018. World Journal of Surgery, 43(3), 659–695. 10.1007/s00268-018-4844-y [DOI] [PubMed] [Google Scholar]
- Howard‐Anderson, J. , Busuttil, A. , Lonowski, S. , Vangala, S. , & Afsar‐Manesh, N. (2016). From discharge to readmission: Understanding the process from the patient perspective. Journal of Hospital Medicine, 11(6), 407–412. 10.1002/jhm.2560 [DOI] [PubMed] [Google Scholar]
- Ihedioha, U. , Sangal, S. , Mastermann, J. , Singh, B. , & Chaudhri, S. (2012). Preparation for elective colorectal surgery using a video: A questionnaire‐based observational study. Journal of the Royal Society of Medicine Short Reports, 3(8), 58. 10.1258/shorts.2011.011126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ihedioha, U. , Vaughan, S. , Mastermann, J. , Singh, B. , & Chaudhri, S. (2013). Patient education videos for elective colorectal surgery: Results of a randomized controlled trial. Colorectal Disease, 15(11), 1436–1441. 10.1111/codi.12348 [DOI] [PubMed] [Google Scholar]
- Jakobsson, J. , Idvall, E. , & Wann‐Hansson, C. (2016). General health and state anxiety in patients recovering from colorectal cancer surgery. Journal of Advanced Nursing, 72(2), 328–338. 10.1111/jan.12841 [DOI] [PubMed] [Google Scholar]
- Jones, D. , Musselman, R. , Pearsall, E. , McKenzie, M. , Huang, H. , & McLeod, R. S. (2017). Ready to go home? Patients' experiences of the discharge process in an enhanced recovery after surgery (ERAS) program for colorectal surgery. Journal of Gastrointestinal Surgery, 21(11), 1865–1878. 10.1007/s11605-017-3573-0 [DOI] [PubMed] [Google Scholar]
- Keller, D. S. , Swendseid, B. , Khan, S. , & Delaney, C. P. (2014). Readmissions after ileostomy closure: Cause to revisit a standardized enhanced recovery pathway? American Journal of Surgery, 208(4), 650–655. 10.1016/j.amjsurg.2014.05.003 [DOI] [PubMed] [Google Scholar]
- Keller, D. S. , Swendseid, B. , Khorgami, Z. , Champagne, B. J. , Reynolds, H. L. Jr , Stein, S. L. , & Delaney, C. P. (2014). Predicting the unpredictable: Comparing readmitted versus non‐readmitted colorectal surgery patients. American Journal of Surgery, 207(3), 346–351. 10.1016/j.amjsurg.2013.09.008 [DOI] [PubMed] [Google Scholar]
- Kelly, K. N. , Noyes, K. , Dolan, J. , Fleming, F. , Monson, J. R. T. , Gonzalez, M. , Sevdalis, N. , & Dozier, A. (2016). Patient perspective on care transitions after colorectal surgery. Journal of Surgical Research, 203(1), 103–112. 10.1016/j.jss.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Krogsgaard, M. , Dreyer, P. , Egerod, I. , & Jarden, M. (2014). Post‐discharge symptoms following fast‐track colonic cancer surgery: A phenomenological hermeneutic study. Springerplus, 3, 276. 10.1186/2193-1801-3-276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krpata, D. M. , Keller, D. S. , Samia, H. , Lawrence, J. , Obokhare, I. , Marderstein, E. , Brady, K. M. , & Delaney, C. P. (2013). Evaluation of inflammatory markers as predictors of hospital stay and unplanned readmission after colorectal surgery. Polish Journal of Surgery, 85(4), 198–203. 10.2478/pjs-2013-0030 [DOI] [PubMed] [Google Scholar]
- Lawrence, J. K. , Keller, D. S. , Samia, H. , Ermlich, B. , Brady, K. M. , Nobel, T. , Stein, S. L. , & Delaney, C. P. (2013). Discharge within 24 to 72 hours of colorectal surgery is associated with low readmission rates when using Enhanced Recovery Pathways. Journal of the American College of Surgeons, 216(3), 390–394. 10.1016/j.jamcollsurg.2012.12.014 [DOI] [PubMed] [Google Scholar]
- Lawson, E. H. , Hall, B. L. , Louie, R. , Zingmond, D. S. , & Ko, C. Y. (2014). Identification of modifiable factors for reducing readmission after colectomy: A national analysis. Surgery, 155(5), 754–766. 10.1016/j.surg.2013.12.016 [DOI] [PubMed] [Google Scholar]
- Lithner, M. , Johansson, J. , Andersson, E. , Jakobsson, U. , Palmquist, I. , & Klefsgard, R. (2012). Perceived information after surgery for colorectal cancer – an explorative study. Colorectal Disease, 14(11), 1340–1350. 10.1111/j.1463-1318.2012.02982.x [DOI] [PubMed] [Google Scholar]
- Lithner, M. , Klefsgard, R. , Johansson, J. , & Andersson, E. (2015). The significance of information after discharge for colorectal cancer surgery‐a qualitative study. Bmc Nursing, 14, 8. 10.1186/s12912-015-0086-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv, L. , Shao, Y. F. , & Zhou, Y. B. (2012). The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: An update of meta‐analysis of randomized controlled trials. International Journal of Colorectal Disease, 27(12), 1549–1554. 10.1007/s00384-012-1577-5 [DOI] [PubMed] [Google Scholar]
- Martin, L. A. , Finlayson, S. R. G. , & Brooke, B. S. (2017). Patient preparation for transitions of surgical care: is failing to prepare surgical patients preparing them to fail? World Journal of Surgery, 41(6), 1447–1453. 10.1007/s00268-017-3884-z [DOI] [PubMed] [Google Scholar]
- Meleis, A. I. (2010). Transitions theory. Middle range and situation specific theories in nursing research and practice. : S. P. Company Ed. [Google Scholar]
- Naylor, M. D. , Brooten, D. , Campbell, R. , Jacobsen, B. S. , Mezey, M. D. , Pauly, M. V. , & Schwartz, J. S. (1999). Comprehensive discharge planning and home follow‐up of hospitalized elders: A randomized clinical trial. Journal of the American Medical Association, 281(7), 613–620. 10.1001/jama.281.7.613 [DOI] [PubMed] [Google Scholar]
- Neville, A. , Lee, L. , Antonescu, I. , Mayo, N. E. , Vassiliou, M. C. , Fried, G. M. , & Feldman, L. S. (2014). Systematic review of outcomes used to evaluate enhanced recovery after surgery. British Journal of Surgery, 101(3), 159–170. 10.1002/bjs.9324 [DOI] [PubMed] [Google Scholar]
- Norlyk, A. , & Harder, I. (2011). Recovering at home: Participating in a fast‐track colon cancer surgery programme. Nursing Inquiry, 18(2), 165–173. 10.1111/j.1440-1800.2011.00519.x [DOI] [PubMed] [Google Scholar]
- Pajarón‐Guerrero, M. , Fernández‐Miera, M. F. , Dueñas‐Puebla, J. C. , Cagigas‐Fernández, C. , Allende‐Mancisidor, I. , Cristóbal‐Poch, L. , Gómez‐Fleitas, M. , Manzano‐Peral, M. A. , Gonzalez‐Fernandez, C. R. , Aguilera‐Zubizarreta, A. , & Sanroma‐Mendizábal, P. (2017). Early discharge programme on hospital‐at‐home evaluation for patients with immediate postoperative course after laparoscopic colorectal surgery. European Surgical Research, 58(5–6), 263–273. 10.1159/000479004 [DOI] [PubMed] [Google Scholar]
- Partoune, A. , Coimbra, C. , Brichant, J. F. , & Joris, J. (2017). Quality of life at home and satisfaction of patients after enhanced recovery protocol for colorectal surgery. Acta Chirurgica Belgica, 117(3), 176–180. 10.1080/00015458.2017.1279871 [DOI] [PubMed] [Google Scholar]
- Pecorelli, N. , Hershorn, O. , Baldini, G. , Fiore, J. F. , Stein, B. L. , Liberman, A. S. , Charlebois, P. , Carli, F. , & Feldman, L. S. (2017). Impact of adherence to care pathway interventions on recovery following bowel resection within an established enhanced recovery program. Surgical Endoscopy, 31(4), 1760–1771. 10.1007/s00464-016-5169-2 [DOI] [PubMed] [Google Scholar]
- Pisarska, M. , Pędziwiatr, M. , Małczak, P. , Major, P. , Ochenduszko, S. , Zub‐Pokrowiecka, A. , Kulawik, J. , & Budzyński, A. (2016). Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. International Journal of Surgery, 36, 377–382. 10.1016/j.ijsu.2016.11.088 [DOI] [PubMed] [Google Scholar]
- Pluye, P. , Robert, E. , Cargo, M. , Bartlett, G. , O’Cathain, A. , Griffiths, F. , Boardman, F. , Gagnon, M. P. , & Rousseau, M. C. (2011). Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. Retrieved fromhttp://mixedmethodsappraisaltoolpublic.pbworks.com
- Shah, P. M. , Johnston, L. , Sarosiek, B. , Harrigan, A. , Friel, C. M. , Thiele, R. H. , & Hedrick, T. L. (2017). Reducing readmissions while shortening length of stay: The positive impact of an enhanced recovery protocol in colorectal surgery. Diseases of the Colon & Rectum, 60(2), 219–227. 10.1097/dcr.0000000000000748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibbern, T. , Bull Sellevold, V. , Steindal, S. A. , Dale, C. , Watt‐Watson, J. , & Dihle, A. (2017). Patients' experiences of enhanced recovery after surgery: A systematic review of qualitative studies. Journal of Clinical Nursing, 26(9–10), 1172–1188. 10.1111/jocn.13456 [DOI] [PubMed] [Google Scholar]
- Smith, F. , Öhlén, J. , Persson, L. O. , & Carlsson, E. (2018). Daily assessment of stressful events and coping in early post‐operative recovery after colorectal cancer surgery. European Journal of Cancer Care, 27(2), 1–10. 10.1111/ecc.12829 [DOI] [PubMed] [Google Scholar]
- Spanjersberg, W. R. , Reurings, J. , Keus, F. , & van Laarhoven, C. J. (2011). Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Systematic Review, 16(2), CD007635. 10.1002/14651858.CD007635.pub2 [DOI] [PubMed] [Google Scholar]
- Stewart, J. , Lloyd, G. M. , Smith, J. K. , Acheson, A. G. , Williams, J. P. , & Maxwell‐Armstrong, C. A. (2012). Could telephone reviews reduce read mission rates after laparoscopic colorectal surgery? Bulletin of the Royal College of Surgeons of England, 94(5), 162–164. 10.1308/147363512x13311314195295 [DOI] [Google Scholar]
- Taylor, C. , & Burch, J. (2011). Feedback on an enhanced recovery programme for colorectal surgery. British Journal of Nursing, 20(5), 286–290. 10.12968/bjon.2011.20.5.286 [DOI] [PubMed] [Google Scholar]
- Thomsen, T. G. , & Hølge‐Hazelton, B. (2017). Patients’ vulnerability in follow‐up after colorectal cancer: A qualitative action research study. Cancer Nursing, 40(2), 152–159. 10.1097/NCC.0000000000000367 [DOI] [PubMed] [Google Scholar]
- Varadhan, K. K. , Neal, K. R. , Dejong, C. H. , Fearon, K. C. , Ljungqvist, O. , & Lobo, D. N. (2010). The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: A meta‐analysis of randomized controlled trials. Clinical Nutrition, 29(4), 434–440. 10.1016/j.clnu.2010.01.004 [DOI] [PubMed] [Google Scholar]
- Wennstrom, B. , Stomberg, M. W. , Modin, M. , & Skullman, S. (2010). Patient symptoms after colonic surgery in the era of enhanced recovery‐a long‐term follow‐up. Journal of Clinical Nursing, 19(5–6), 666–672. 10.1111/j.1365-2702.2009.03099.x [DOI] [PubMed] [Google Scholar]
- Whittemore, R. , & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546–553. 10.1111/j.1365-2648.2005.03621.x [DOI] [PubMed] [Google Scholar]
- Wood, T. , Aarts, M.‐A. , Okrainec, A. , Pearsall, E. , Victor, J. C. , McKenzie, M. , Rotstein, O. , & McLeod, R. S. (2018). Emergency room visits and readmissions following implementation of an enhanced recovery after surgery (iERAS) program. Journal of Gastrointestinal Surgery, 22(2), 259–266. 10.1007/s11605-017-3555-2 [DOI] [PubMed] [Google Scholar]
- Yuen, A. , Elnahas, A. , Azin, A. , Okrainec, A. , Jackson, T. D. , & Quereshy, F. A. (2016). Is expedited early discharge following elective surgery for colorectal cancer safe? An analysis of short‐term outcomes. Surgical Endoscopy, 30(9), 3904–3909. 10.1007/s00464-015-4696-6 [DOI] [PubMed] [Google Scholar]
- Zhuang, C. L. , Ye, X. Z. , Zhang, X. D. , Chen, B. C. , & Yu, Z. (2013). Enhanced recovery after surgery programs versus traditional care for colorectal surgery: A metaanalysis of randomized controlled trials. Diseases of the Colon and Rectum, 56(5), 667–678. 10.1097/DCR.0b013e3182812842 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


