Abstract
Objectives
To explore the correlations among social isolation and symptoms of anxiety and depression among patients with breast cancer in China and to further verify the mediating role of social support in social isolation and symptoms of depression or anxiety.
Design
A cross‐sectional survey.
Settings
The cluster sampling method was conducted for 456 female inpatients diagnosed with breast cancer at the Tumor Hospital Affiliated of Harbin Medical University from April 2019–September 2019.
Methods
Pearson correlation analysis was used for identifying correlations among all the variables. Mediation effect analysis was used to examine the role of social support in social isolation and symptoms of depression or anxiety.
Results
The results showed a prevalence of 73.26% and 70.44% for anxiety and depression symptoms in patients with breast cancer, respectively. Anxiety was significantly negatively correlated with social support (r = −.334, p < .01) and significantly positively correlated with social isolation (r = .369, p < .01). Similarly, depression was significantly negatively correlated with social support (r = −.289, p < .01) and significantly positively correlated with social isolation (r = .466, p < .01). Social support played a mediating role in social isolation and f symptoms of anxiety or depression among these patients.
Conclusions
Social isolation was positively correlated with symptoms of anxiety and depression in patients with breast cancer, respectively. Social support for patients with breast cancer has a mediating effect on the patients’ social isolation and symptoms of anxiety and depression. Therefore, the support of family, friends, hospitals, and organizations plays a positive role in reducing social isolation as well as symptoms of depression and anxiety in these patients.
Keywords: anxiety, breast cancer, depression, social isolation, social support
1. INTRODUCTION
According to the 2020 statistics, the incidence rate of breast cancer, among various cancers, was 11.7%, accounting for 6.9% of the mortality rate worldwide (Observatory TGC GLOBOCAN, 2020). Moreover, breast cancer is the most common cancer type among females globally, and it is also one of the malignant tumours that seriously affect women's health (Tsaras et al., 2018). Different treatments and long‐term exposure to breast cancer become a huge burden for both the patients and their caregivers (Kusi et al., 2020). It also affects the mental health of patients, inducing problems such as symptoms of depression and anxiety (Ecclestone et al., 2016; Kale & Carroll, 2016; Kugbey et al., 2020).
Symptoms of anxiety and depression are the most common psychological problems among patients with breast cancer (Beatty and Kissane, 2017; Kugbey et al., 2020). Previous studies have shown that patients with breast cancer experienced different levels of anxiety and depression symptoms (Balouchi et al., 2019; Ho et al., 2013; Ju et al., 2018; Lan et al., 2020; Liu et al., 2011; So et al., 2013; Tsaras et al., 2018). Results from a previous study showed that 50.5% of patients with breast cancer had at least mild depression and 42.4% had at least mild anxiety (Ju et al., 2018). Ho et al.’s (2013) study on female patients with breast cancer also showed that more than half of the respondents had symptoms of anxiety or depression, and 15.6% had symptoms of two psychopathological conditions at the same time. Moreover, a systematic review and meta‐analysis showed that the prevalence of depression among patients with breast cancer worldwide was 32.2% (Balouchi et al., 2019). Further, the highest prevalence of depression symptoms was noted in the Eastern Mediterranean region, with middle‐income countries displaying a prevalence twice as high as that in developed countries (Balouchi et al., 2019).
Various factors can account for the prevalence of anxiety and depression symptoms in patients with breast cancer, including demographic characteristics (age, marital status, education level and cancer stage), social support and social isolation (Puigpinós‐Riera et al., 2018; Tsaras et al., 2018). Social support refers to the functions or regulations provided by a person's social network (Duan et al., 2019). As shown by previous research, social support from family and friends significantly reduced women’ s anxiety and depression levels, whereas social support from their partner reduced anxiety levels (Akdag Topal and Terzioglu, 2019; Hu et al., 2018; Jeong et al., 2016). Another study showed that social support for patients with breast cancer is negatively correlated with symptoms of anxiety and depression (Liu et al., 2011). Further, it has been indicated that intimate conversations can reduce the incidence rate of depression and anxiety symptoms among patients with breast cancer (Balouchi et al., 2019).
Social support is also considered to play a key role in the relationship between social networks and physical and mental health (Harasemiw et al., 2018; Thoits, 2011). Restricted social networking is considered social isolation, consistent with the viewpoint that social isolation is a state of having limited social contact or communication, limited participation in social activities or meeting with friends (Harasemiw et al., 2018; Holt‐Lunstad et al., 2015). Social isolation is also an identified risk factor for higher occurrence of symptoms of anxiety and depression among patients with breast cancer (Puigpinós‐Riera et al., 2018). Compared to objective social isolation, perceived social isolation is more harmful to mental health (Cacioppo et al., 2011). Many mechanisms have been proposed to explain the relationship between social networks and physical and mental health (Harasemiw et al., 2018; Thoits, 2011; Tittman et al., 2016). A longitudinal mediation analysis determined that social disconnectedness predicted higher perceived isolation, which in turn predicted higher symptoms of depression and anxiety (Santini et al., 2020). A study also showed that lack of contact with close friends is significantly related to depression, anxiety and adverse mood disorders (Chou et al., 2011).
In brief, substantial research has been conducted to explore the relationships among social isolation, social support and anxiety or depression among patients with breast cancer, but few studies have investigated the role of social support in social isolation and anxiety or depression symptoms among patients with breast cancer in China. Moreover, the traditional concept of family in Chinese society has led patients with breast cancer to rely mainly on their family's support and care during treatment (Jeong et al., 2016; Ying et al., 2011). Therefore, this study explored the correlations among social isolation and symptoms of anxiety and depression in patients with breast cancer, while also examining the mediating role of social support in social isolation and anxiety or depression. This can help hospitals as well as patients’ families to pay more attention to signs of social isolation, provide more social support and identify and treat any symptoms of mental illness. Based on this, we proposed the following hypotheses: (a) there is a significant correlation between social isolation and symptoms of anxiety and depression among patients with breast cancer; and (b) social support plays a mediating role in social isolation and symptoms of anxiety or depression among patients with breast cancer.
2. METHODS
2.1. Sample
A cross‐sectional survey was conducted on 456 female patients diagnosed with breast cancer at the Tumor Hospital Affiliated of Harbin Medical University, from April–September 2019. This hospital was selected because it is the only tertiary hospital specializing in tumours in the Heilongjiang province, and therefore, most patients with breast cancer visit this hospital for treatment. Thus, it is an appropriate site to use the cluster sampling method to investigate patients with breast cancer. The inclusion criteria for the respondents were: (a) voluntary participation; (b) confirmed diagnosis of breast cancer; (c) no other chronic diseases and (d) no other traumatic events experienced during the past year.
2.2. Data collection
The survey was conducted face‐to‐face using an anonymous, self‐report questionnaire. Before the formal investigation, a pre‐investigation was conducted, and 50 questionnaires were issued and collected; the data from these were not included in the main study. In the formal survey, an average of 38 patients were investigated in each breast surgery wards (the management, layout and environment of the wards are basically the same) and a total of 456 questionnaires were distributed and recovered. The questionnaires with missing data or invalid responses were eliminated and finally analysed 389 valid questionnaires were retained, with an effective recovery rate of 85.3%.
2.3. Measurement instruments
Patients’ demographic data included age, weight, marital status, monthly financial support for children, monthly financial support for the elderly, the number of people who took care of the patient during hospitalization, and whether they were currently taking medications, among others.
The Hospital Anxiety and Depression Scale was developed by Zigmond and Snaith in 1983, and it is mainly used for screening anxiety and depression symptoms in hospitalized patients during the past month (Zigmond & Snaith, 1983). The scale includes two subscales of anxiety and depression, each consisting of 7 items which are rated on a four‐point Likert scale ranging from 0 (never)–3 (almost all the time). The total possible scores of the anxiety and depression subscales are between 0–21. Higher scores indicate the occurrence of more severe symptoms. The scores of the two subscales were classified as follows: 0–7 for no anxiety or depression; 8–10 for mild anxiety or depression; 11–21 for obvious anxiety or depression. Previous studies have shown that the scale has high reliability and validity for the Chinese population (Lin et al., 2017; Xi et al., 2019). This study found that the Cronbach's α coefficients for the anxiety or depression subscale were .762 and .787, respectively.
Social support was evaluated using the Chinese version of the Social Support Rating Scale (Feng et al., 2007; Li et al., 2011), which is a brief measure of the respondents’ social support after a diagnosis of breast cancer. The scale includes 10 items and three dimensions (objective support, subjective support and utilization of support). Previous studies have shown that Social Support Rating Scale is widely used in China (Li et al., 2011; Shi et al., 2017). The present study revealed that Cronbach's α for Social Support Rating Scale was .876, and for the three subscales was .848 (subjective support), .895 (objective support) and .883 (availability of support).
Social isolation implies that an individual is isolated from interpersonal interaction and relationships (Harasemiw et al., 2018; Holt‐Lunstad et al., 2015). Social isolation was assessed using a self‐made scale with reference from the simplified version of Lubben's Social Network (Lubben & Gironda, 2003). The social isolation scale consisted of 6 items, including 3 reverse‐scored items. Each item was rated on a five‐point Likert scale ranging from 1 (almost always)–5 (never). The higher the score, the greater the social isolation. Cronbach's alpha for this scale was .875, and its Kaiser‐Meyer‐Olkin coefficient was .913.
2.4. Ethical consideration
This study was approved by the Research Ethics Committee of the Tumor Hospital Affiliated of Harbin Medical University. Eligible respondents were asked to sign an informed consent after they were informed of the purpose, significance and risks of the study. Moreover, they were informed that they could withdraw from the study at any point in time without penalty. All respondents participated voluntarily and anonymously and provided written informed consent.
2.5. Data analysis
Data analysis was performed using the IBM SPSS 23.0 statistical software. A descriptive analysis was conducted for demographic characteristics, and the scores of each scale were described using means and standard deviations. The normality test was performed for the scores of each scale. The t test and one‐way analysis of variance were used to test whether the demographic characteristics were statistically significant in the analysis of anxiety, depression, social isolation and social support. Pearson correlation analysis was used to determine the links among anxiety and depression, social isolation and social support. The mediation analyses were based on the proposed model number 4 of Hayes 2013) and bootstrapping (1,000 bootstrap samples) using 95% confidence intervals (CI) and 5% margins of error. Statistically significant variables in the univariate analysis were included as covariates: social isolation as the independent variables (X), social support as the mediator variables (M), and anxiety and depression as the dependent variables (Y). The SPSS PROCESS can obtain direct effects, indirect effects and total effects. The effect is significant when the 95% CI does not include 0. Based on the bootstrap mediation effect test, there were two steps. First, we tested whether a*b was significant. If a*b was significant, we needed to test the positivity or negativity of a*b*c. If a*b*c was positive, it indicated a complementary mediation. All variables were tested for multicollinearity. A p‐value <.05 was considered statistically significant.
3. RESULTS
3.1. Participants’ characteristics
Among the 389 patients with breast cancer included in this study, 43.7% were 35–50 years old; 40.6% of them weighed between 50–60 kg, and 34.4% weighed between 60–70 kg. A large majority of the participants were married (86.9%). Further, 65.0% of the patients were cared for by one person; 70.2% of them were not currently taking drugs; 9.5% had lesions with metastatic disease, and breast cancer recurred in 3.3% of the patients. The demographic characteristics of the respondents are shown in Table 1.
TABLE 1.
Demographic characteristics of patients (n = 389)
| Variables | n | Percentage (%) |
|---|---|---|
| Age | ||
| ≤35 | 44 | 11.3 |
| 35–50 | 170 | 43.7 |
| 50–65 | 153 | 39.3 |
| >65 | 22 | 5.7 |
| Weight (kg) | ||
| ≤50 | 36 | 9.3 |
| 50–60 | 158 | 40.6 |
| 60–70 | 134 | 34.4 |
| >70 | 61 | 15.7 |
| Marital status | ||
| Unmarried | 11 | 2.8 |
| Married | 338 | 86.9 |
| Divorce/Separation/Widowed | 40 | 10.3 |
| Monthly financial support for children (CNY) | ||
| ≤2,000 | 333 | 85.6 |
| 2,000–4,000 | 44 | 11.3 |
| >4,000 | 12 | 3.1 |
| Monthly financial support for the elderly (CNY) | ||
| ≤2,000 | 367 | 94.4 |
| 2,000–4,000 | 20 | 5.1 |
| >4,000 | 2 | .5 |
| Taken care of by a few people | ||
| 1 | 253 | 65.0 |
| ≥2 | 136 | 35.0 |
| Are you taking medications | ||
| No | 273 | 70.2 |
| Yes | 116 | 29.8 |
| Metastasis of breast cancer | ||
| Yes | 37 | 9.5 |
| No | 352 | 90.5 |
| Recurrence of breast cancer | ||
| Yes | 13 | 3.3 |
| No | 376 | 96.7 |
3.2. Prevalence of anxiety and depression symptoms
The prevalence of the symptoms of depression and anxiety in patients with breast cancer was 70.44% and 73.26%, respectively. The number of patients with suspected depression and anxiety was 75 and 73, respectively, as shown in Table 2.
TABLE 2.
Prevalence of anxiety and depression symptoms among patients with breast cancer
| Category | Anxiety symptom | Depression symptoms | ||
|---|---|---|---|---|
| n | % | n | % | |
| No symptom (score:0–7) | 31 | 7.97 | 40 | 10.28 |
| Mild symptoms (score:8–10) | 73 | 18.77 | 75 | 19.28 |
| Obvious symptoms (score:11–21) | 285 | 73.26 | 274 | 70.44 |
3.3. Correlations between measurement variables
Table 3 shows the mean, standard deviation and correlation coefficient of each scale score. Anxiety was significantly negatively correlated with social support (r = −.334, p < .01) and significantly positively correlated with social isolation (r = .369, p < .01); depression was significantly negatively correlated with social support (r = −.289, p <.01) and significantly positively correlated with social isolation (r = .466, p <.01); and social support was significantly negatively correlated with social isolation (r = −.223, p <.01).
TABLE 3.
Pearson correlation analysis among anxiety, depression, social support and social isolation
| Variables | M ± SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Anxiety | 7.66 ± 3.60 | 1 | |||
| Depression | 7.01 ± 4.00 | 0.711** | 1 | ||
| Social support | 39.77 ± 7.54 | −0.334** | −0.289** | 1 | |
| Social isolation | 12.45 ± 3.91 | 0.369** | 0.466** | −0.223** | 1 |
p <0.01
3.4. Difference between respondents’ characteristics and scores of multiple variables
The correlations between the characteristics of patients with breast cancer and their scores on anxiety, depression, social support and social isolation scores are shown in Table 4. According to patient demographics, there were significant differences in depression scores for patients with different number of caregivers (t = −2.816, p =.005). Further, the scores were different based on whether or not patients were currently taking medications (t = 3.998, p <.001).
TABLE 4.
Univariate analysis and description of each scale a
| Variables | Anxiety | Depression | Social support | Social isolation |
|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | |
| Age | ||||
| ≤35 | 7.75 ± 3.34 | 7.25 ± 3.95 | 40.25 ± 7.27 | 12.48 ± 3.89 |
| 35–50 | 7.80 ± 3.58 | 6.92 ± 4.04 | 40.71 ± 6.82 | 12.41 ± 3.84 |
| 50–65 | 7.46 ± 3.79 | 6.95 ± 4.05 | 38.93 ± 8.08 | 12.64 ± 4.03 |
| >65 | 7.73 ± 3.01 | 7.68 ± 3.64 | 37.32 ± 8.73 | 11.32 ± 3.75 |
| F/t | 0.253 | 0.297 | 2.372 | 0.737 |
| p | .859 | .828 | .070 | .530 |
| Weight (kg) | ||||
| ≤50 | 7.83 ± 2.97 | 7.19 ± 3.77 | 39.92 ± 7.67 | 12.33 ± 4.07 |
| 50–60 | 7.61 ± 3.40 | 6.69 ± 3.98 | 39.18 ± 7.70 | 12.59 ± 3.82 |
| 60–70 | 7.72 ± 4.01 | 7.11 ± 4.14 | 40.88 ± 7.66 | 12.28 ± 4.18 |
| >70 | 6.20 ± 4.21 | 6.55 ± 4.27 | 38.78 ± 6.54 | 11.47 ± 3.28 |
| F/t | 2.755 | 0.459 | 1.657 | 1.215 |
| p | .042 | .711 | .176 | .304 |
| Marital status | ||||
| Unmarried | 7.36 ± 4.01 | 6.36 ± 4.34 | 39.55 ± 9.68 | 12.45 ± 4.50 |
| Married | 7.71 ± 3.63 | 7.09 ± 3.99 | 40.11 ± 7.42 | 12.45 ± 3.78 |
| Divorce/Separation/Widowed | 6.89 ± 3.03 | 6.11 ± 3.82 | 37.03 ± 7.30 | 12.33 ± 5.03 |
| F/t | 0.965 | 1.215 | 3.041 | 0.017 |
| p | .382 | .298 | .049 | .983 |
| Monthly financial support for children (CNY) | ||||
| ≤2,000 | 7.52 ± 3.58 | 7.09 ± 3.96 | 39.85 ± 7.62 | 12.48 ± 3.81 |
| 2,000–4,000 | 7.95 ± 3.01 | 7.07 ± 3.95 | 40.41 ± 6.51 | 12.45 ± 3.80 |
| >4,000 | 8.33 ± 5.87 | 6.58 ± 5.28 | 39.42 ± 6.72 | 13.83 ± 5.91 |
| F/t | 0.534 | 0.094 | 0.134 | 0.707 |
| p | .587 | .910 | .875 | .494 |
| Monthly financial support for the elderly (CNY) | ||||
| ≤2,000 | 7.75 ± 3.57 | 7.02 ± 3.98 | 39.64 ± 7.47 | 12.40 ± 3.79 |
| 2,000–4,000 | 8.15 ± 4.52 | 7.20 ± 4.63 | 39.05 ± 7.41 | 13.30 ± 4.86 |
| >4,000 | 12.00 ± 2.83 | 7.00 ± 5.66 | 41.50 ± 7.78 | 14.50 ± 3.54 |
| F/t | 1.473 | 0.019 | 0.123 | 0.802 |
| p | .231 | .981 | .884 | .449 |
| Taken care of by a few people | ||||
| 1 | 7.51 ± 3.73 | 6.62 ± 4.10 | 38.75 ± 8.07 | 12.21 ± 4.02 |
| ≥2 | 8.06 ± 3.53 | 7.82 ± 3.83 | 42.44 ± 5.15 | 12.75 ± 3.67 |
| F/t | −1.413 | −2.816 | −5.486 | −1.302 |
| p | .158 | .005 | <.001 | .194 |
| Are you taking medications | ||||
| No | 7.86 ± 3.47 | 7.53 ± 3.86 | 39.93 ± 7.62 | 12.85 ± 3.67 |
| Yes | 7.17 ± 3.85 | 5.79 ± 4.08 | 39.39 ± 7.38 | 11.49 ± 4.30 |
| F/t | 1.736 | 3.998 | 0.645 | 3.172 |
| p | .083 | <.001 | .519 | .002 |
| Metastasis of breast cancer | ||||
| Yes | 8.03 ± 2.87 | 7.11 ± 3.54 | 38.95 ± 7.92 | 13.24 ± 3.24 |
| No | 7.62 ± 3.67 | 7.00 ± 4.05 | 39.85 ± 7.50 | 12.36 ± 3.97 |
| F/t | 0.803 | 0.159 | −0.691 | 1.303 |
| p | .426 | .874 | .490 | .193 |
| Recurrence of breast cancer | ||||
| Yes | 7.00 ± 3.14 | 7.08 ± 4.92 | 40.23 ± 6.42 | 12.00 ± 3.19 |
| No | 7.68 ± 3.61 | 7.01 ± 3.97 | 39.75 ± 7.58 | 12.46 ± 3.94 |
| F/t | −0.670 | 0.062 | 0.225 | −0.416 |
| p | .503 | .951 | .822 | .678 |
The Hospital Anxiety and Depression Scale was assessed the symptoms of depression and anxiety among patients with breast cancer; social support and social isolation of patients with breast cancer were evaluated using the Chinese version of the Social Support Rating Scale and Social Isolation Scale, respectively.
3.5. Mediation regression models of the study variables
The results of the mediation effect analysis are shown in Table 5. The direct effect of social isolation on social support was −0.7297, the direct effect of social support on anxiety was −0.0698, the direct effect of social isolation on anxiety was 0.3366, the indirect effect of social isolation on anxiety was 0.0509, and the total effect of social isolation on anxiety was 0.3875. The bootstrap 95% CI of the indirect effect was (0.0199, 0.0915), and the confidence interval did not include 1, indicating that social support mediates the social isolation and anxiety of patients with breast cancer. Meanwhile, a*b*c’ was positive, showing the mediating role of social support in explaining the relationship between the social isolation and anxiety in patients with breast cancer (Figure 1). Similarly, Table 5 also indicates that the direct effect of social isolation on depression was 0.4075, the indirect effect of social isolation on depression was 0.0353, and the total effect of social isolation on depression was 0.4428. The bootstrap 95% CI of the indirect effect was (0.0090, 0.0677), and the confidence interval did not include 1, indicating that social support mediates social isolation and depression in patients with breast cancer. Meanwhile, a*b*c was positive, showing the mediating role of social support in the relationship between social isolation and depression in patients with breast cancer.
TABLE 5.
Analysis results of mediation effect
| Models | a | b | c’ | a*b | 95% CI of a*b | c | SE | R 2 |
|---|---|---|---|---|---|---|---|---|
| 1.SI→SS→A | −0.7297** | −0.0698* | 0.3366** | 0.0509* | (0.0199, 0.0915) | 0.3875** | 0.0186 | .1679 |
| 2.SI→SS→D | −0.6194** | −0.0570* | 0.4075** | 0.0353* | (0.0090, 0.0677) | 0.4428** | 0.0151 | .2325 |
A, Anxiety; a*b, indirect effect; c', direct effect; c, total effect; D, Depression; R 2, variance accounted for; SE, Bootstrap regression standard error; SI, Social Isolation; SS, Social Support.
p <0.05,
p <0.01.
FIGURE 1.
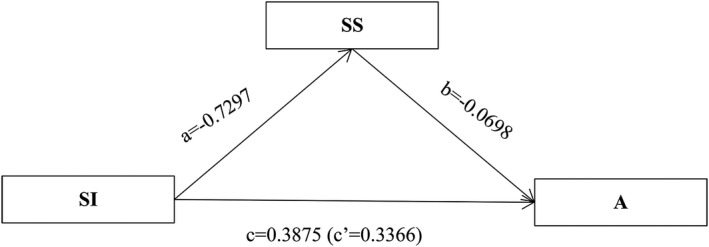
Model 1 of social isolation, social support and anxiety in patients with breast cancer. N = 389; controlled by several people and currently taking medications; A, anxiety; a, direct effect of SI on SS; b, direct effect of SS on A; c, total effect of SI on A; c’, direct effect of SI on A; SI, social isolation; SS, social support
4. DISCUSSION
The purpose of this study was to explore the correlations among social isolation, anxiety and depression symptoms in patients with breast cancer and to verify the role of social support in social isolation and symptoms of anxiety or depression.
The results showed that the prevalence of depression and anxiety symptoms in patients with breast cancer was 70.44% and 73.26%, respectively. This finding was higher than previous studies which used the same scale to measure the prevalence of symptoms of anxiety and depression in patients with breast cancer (Hassan et al., 2015; Ng et al., 2017; Park et al., 2018). Moreover, the prevalence of depression and anxiety symptoms was also higher than that found in other Asian (i.e. Malaysia, Korean and Jordan) women with breast cancer (Hassan et al., 2015; Jang et al., 2013). The results were also significantly higher than the previously reported results in patients with breast cancer, using different scales (Maass et al., 2015; Tsaras et al., 2018). Our results were similar to the study conducted by Fanakidou et al. (2018); however, the prevalence of anxiety and depression symptoms was found to be higher. The possible reasons for the different results are listed as follows: (a) different designs and methods used in various studies; (b) cultural differences in the study population and differences in self‐evaluation of anxiety and depression among different groups; and (c) different scales with different critical value ranges (Abou Kassm et al., 2018; Tsaras et al., 2018).
It is worth noting that social isolation is positively correlated with anxiety and depression in patients with breast cancer, consistent with the results of previous studies (Matthews et al., 2016; Santini et al., 2020). One possible reason for this phenomenon is that patients with breast cancer have few social ties or participate less in social activities and lack support (Puigpinós‐Riera et al., 2018); these conditions aggravate the response to the disease, reduce their coping abilities and increase the risk of anxiety and depression (Santini et al., 2020).
The strengths of this study included finding that social support played a mediating role between social isolation and symptoms of anxiety or depression in patients with breast cancer. It implies that proper social support can help reduce symptoms of anxiety and depression in patients with breast cancer, which are caused due to social isolation. Generally, patients with breast cancer receive social support from families, friends, hospitals and work units (Puigpinós‐Riera et al., 2018; Wondimagegnehu et al., 2019).
Family is the most important source of support among patients with breast cancer in China (Li et al., 2018). Family members play the role of long‐term companions for patients, and they are the most important part of social support for patients (Li et al., 2018). The alienation of family relationships has a great impact on patients’ psychology (Li et al., 2018; Puigpinós‐Riera et al., 2018; Wondimagegnehu et al., 2019). The closeness of family relationships directly affects the quality of support for patients with breast cancer. If the family relationships are loosely tied, family support to the patients is limited, and patients’ social activities are reduced; hence, the risk of depression and anxiety symptoms caused by social isolation may be greater (Li et al., 2018; Puigpinós‐Riera et al., 2018; Wondimagegnehu et al., 2019). A study also indicated that intimacy was negatively correlated with depression symptoms (Lee et al., 2013). Friends are chosen based on mutual affinity, often having similar life experiences, and provide different types of support and social interaction as compared to family members. Results of a study by Taylor et al. 2018) confirmed the importance of friendship and proved that it is harmful to be separated from friends subjectively. Therefore, the support of friends contributes to reducing the occurrence of depression and anxiety symptoms (Puigpinós‐Riera et al., 2018; Wondimagegnehu et al., 2019). During treatment, patients may be more dependent on the medical staff for social interaction. The attitude of medical staff in providing services and the frequency of communication with patients can reduce the symptoms of depression and anxiety caused by social isolation (Puigpinós‐Riera et al., 2018). In addition, patients can experience the support of the organization through the support of leaders and colleagues, which can help alleviate their social isolation, and thereby reducing the occurrence of depression and anxiety (Puigpinós‐Riera et al., 2018; Wondimagegnehu et al., 2019). In brief, patients with a high level of social isolation do not have a suitable outlet for pressure release (Puigpinós‐Riera et al., 2018). Strong social relationships can distract the patients, pull them out of social isolation and painful emotions, directly enhance their sense of self‐worth and play an important role in alleviating anxiety and depression (Forsythe et al., 2014; Puigpinós‐Riera et al., 2018).
Some limitations of this study also need attention. First, this was a cross‐sectional study, which cannot explain the causal relationship between the variables. A longitudinal study may be able to solve this problem. Second, the depression and anxiety scale was used to investigate the situation of patients in the preceding month; therefore, there may be a recall bias. Finally, the sample size of this study was small and limited to one province; thus, the results of this study need to be further tested using a national sample.
4.1. Implications for clinical practice
Anxiety and depression symptoms are common among patients with breast cancer.
Hospitals and nursing professionals should pay attention to patients’ mental health.
Family members of patients also need to pay attention to the mental health of patients and give more encouragement and support to reduce their social isolation.
5. CONCLUSIONS
In conclusion, the social isolation was positively correlated with symptoms of anxiety and depression in patients with breast cancer, respectively. The results also indicated that social support for patients with breast cancer has a mediating effect on the patients’ social isolation and symptoms of anxiety and depression. The hospitals and patients’ family and friends should pay more attention to the patients so that they experience and utilise social support to reduce the occurrence of social isolation and overcome feelings of anxiety and depression associated with the illness.
6. CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
7. AUTHOR CONTRIBUTIONS
BL, XW, LS, YY and DL conceived and designed the experiments. HL, DW, XW and YL performed the experiments. BL, LS and HM analysed the data. HL, DW, XL, YL, YY and DL contributed reagents/materials/analysis tools. BL, XW and LS wrote the paper. BL, XW, LS, HL, DW, XL, YL, YY and DL approved the final manuscript for publication.
ACKNOWLEDGMENTS
The authors would like to thank all participants in this study. This work was supported by the Humanities Program of 2018 Innovation Science Research Fund of Harbin Medical University (601847) and Haiyan Research Fund of the Tumor Hospital Affiliated to Harbin Medical University (JJMS2020‐06) to B.L; was funded by the Excellent Youth Project of Natural Science Foundation of Heilongjiang Province (YQ2020H027) to XW; and also funded by Guangdong Basic and Applied Basic Research Foundation (2020A1515110369) to LS.
Liu B, Wu X, Shi L, et al. Correlations of social isolation and anxiety and depression symptoms among patients with breast cancer of Heilongjiang province in China: The mediating role of social support. Nurs Open. 2021;8:1981–1989. 10.1002/nop2.876
Bingshuo Liu, Xinyu Wu and Lei Shi contributed equally to this work.
Contributor Information
Yue Yang, Email: yuelianghaiyang@126.com.
Danni Li, Email: danni8778@163.com.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Abou Kassm, S. , Hlais, S. , Khate, C. , Chehade, I. , Haddad, R. , Chahine, J. , Yazbeck, M. , Abi Warde, R. , & Naja, W. (2018). Depression and religiosity and their correlates in Lebanese breast cancer patients. Psychooncology, 27(1), 99–105. [DOI] [PubMed] [Google Scholar]
- Akdag Topal, C. , & Terzioglu, F. (2019). Assessment of depression, anxiety, and social support in the context of therapeutic abortion. Perspect Psychiatr Care, 55(4), 618–623. [DOI] [PubMed] [Google Scholar]
- Balouchi, A. , Hashemi, S. M. , Rafiemanesh, H. , Amirshahi, M. , & Afsargharehbagh, R. (2019). Global prevalence of depression among breast cancer patients: A systematic review and meta‐analysis. Breast Cancer Research and Treatment, 176(1), 519–533. [DOI] [PubMed] [Google Scholar]
- Beatty, L. , & Kissane, D. (2017). Anxiety and depression in women with breast cancer. Cancer Forum, 41(1), 67–72. [Google Scholar]
- Cacioppo, J. T. , Hawkley, L. C. , Norman, G. J. , & Berntson, G. G. (2011). Social isolation. Annals of the New York Academy of Sciences, 1231(1), 17–22. 10.1111/j.1749-6632.2011.06028.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou, K. , Liang, K. , & Sareen, J. (2011). The association between social isolation and DSM‐IV mood, anxiety, and substance use disorders: Wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry, 72(11), 1468. [DOI] [PubMed] [Google Scholar]
- Duan, X. , Ni, X. , Shi, L. , Zhang, L. , Ye, Y. , Mu, H. , Li, Z. , Liu, X. , Fan, L. , & Wang, Y. (2019). The impact of workplace violence on job satisfaction, job burnout, and turnover intention: The mediating role of social support. Health and Quality of Life Outcomes, 17(1):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecclestone, C. , Chow, R. , Pulenzas, N. , Zhang, L. , Leahey, A. , Hamer, J. , DeAngelis, C. , Bedard, G. , McDonald, R. , Bhatia, A. , Ellis, J. , Rakovitch, E. , Vuong, S. , Chow, E. , & Verma, S. (2016). Quality of life and symptom burden in patients with metastatic breast cancer. Supportive Care in Cancer, 24(9), 4035–4043. 10.1007/s00520-016-3217-z [DOI] [PubMed] [Google Scholar]
- Fanakidou, I. , Zyga, S. , Alikari, V. , Tsironi, M. , Stathoulis, J. , & Theofilou, P. (2018). Mental health, loneliness, and illness perception outcomes in quality of life among young breast cancer patients after mastectomy: The role of breast reconstruction. Quality of Life Research, 27(2), 539–543. 10.1007/s11136-017-1735-x [DOI] [PubMed] [Google Scholar]
- Feng, S. , Tan, H. , Benjamin, A. , Wen, S. , Liu, A. , Zhou, J. , Li, S. , Yang, T. , Zhang, Y. , Li, X. , & Li, G. (2007). Social support and posttraumatic stress disorder among flood victims in Hunan. China. Ann Epidemiol, 17(10), 827–833. 10.1016/j.annepidem.2007.04.002 [DOI] [PubMed] [Google Scholar]
- Forsythe, L. P. , Alfano, C. M. , Kent, E. E. , Weaver, K. E. , Bellizzi, K. , Arora, N. , Aziz, N. , Keel, G. , & Rowland, J. H. (2014). Social support, self‐efficacy for decision‐making, and follow‐up care use in long‐term cancer survivors. Psychooncology, 23(7), 788–796. 10.1002/pon.3480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harasemiw, O. , Newall, N. , Shooshtari, S. , Mackenzie, C. , & Menec, V. (2018). From social integration to social isolation: the relationship between social network types and perceived availability of social support in a national sample of older canadians. Res Aging, 40(8), 715–739. [DOI] [PubMed] [Google Scholar]
- Hassan, M. R. , Shah, S. A. , Ghazi, H. F. , Mohd Mujar, N. M. , Samsuri, M. F. , & Baharom, N. (2015). Anxiety and depression among breast cancer patients in an urban setting in Malaysia. Asian Pacific Journal of Cancer Prevention, 16(9), 4031–4035. [DOI] [PubMed] [Google Scholar]
- Hayes, A. (2013). Introduction to mediation, moderation, and conditional processanalysis. Journal of Educational Measurement, 51(3), 335–337. [Google Scholar]
- Ho, S. S. , So, W. K. , Leung, D. Y. , Lai, E. T. , & Chan, C. W. (2013). Anxiety, depression and quality of life in Chinese women with breast cancer during and after treatment: A comparative evaluation. European Journal of Oncology Nursing, 17(6), 877–882. 10.1016/j.ejon.2013.04.005 [DOI] [PubMed] [Google Scholar]
- Holt‐Lunstad, J. , Smith, T. B. , Baker, M. , Harris, T. , & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta‐analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hu, T. , Xiao, J. , Peng, J. , Kuang, X. , & He, B. (2018). Relationship between resilience, social support as well as anxiety/depression of lung cancer patients: A cross‐sectional observation study. Journal of Cancer Research & Therapy, 14(1), 72–77. [DOI] [PubMed] [Google Scholar]
- Jang, J. E. , Kim, S. W. , Kim, S. Y. , Kim, J. M. , Park, M. H. , Yoon, J. H. , Shin, H. Y. , Kang, H. J. , Bae, K. Y. , Shin, I. S. , & Yoon, J. S. (2013). Religiosity, depression, and quality of life in Korean patients with breast cancer: A 1‐year prospective longitudinal study. Psychooncology, 22(4), 922–929. [DOI] [PubMed] [Google Scholar]
- Jeong, A. , Shin, D. W. , Kim, S. Y. , Yang, H. K. , & Park, J. H. (2016). Avoidance of cancer communication, perceived social support, and anxiety and depression among patients with cancer. Psychooncology, 25(11), 1301–1307. [DOI] [PubMed] [Google Scholar]
- Ju, H.‐B. , Kang, E.‐C. , Jeon, D.‐W. , Kim, T.‐H. , Moon, J.‐J. , Kim, S.‐J. , Choi, J.‐M. , & Jung, D.‐U. (2018). Associations among plasma stress markers and symptoms of anxiety and depression in patients with breast cancer following surgery. Psychiatry Investigation, 15(2), 133–140. 10.30773/pi.2017.07.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kale, H. P. , & Carroll, N. V. (2016). Self‐reported financial burden of cancer care and its effect on physical and mental health‐related quality of life among US cancer survivors. Cancer, 122(8), 283–289. 10.1002/cncr.29808 [DOI] [PubMed] [Google Scholar]
- Kugbey, N. , Oppong, A. K. , & Meyer‐Weitz, A. (2020). Depression, anxiety and quality of life among women living with breast cancer in Ghana: Mediating roles of social support and religiosity. Supportive Care in Cancer, 28(6), 2581–2588. [DOI] [PubMed] [Google Scholar]
- Kusi, G. , Boamah, M. A. B. , Boamah, M. K. , Dzomeku, V. M. , Apiribu, F. , Duodu, P. A. , Adamu, B. , Agbadi, P. , & Bonsu, K. O. (2020). The experiences of family caregivers living with breast cancer patients in low‐and middle‐income countries: A systematic review. Systematic Reviews, 9(1), 165. 10.1186/s13643-020-01408-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan, B. , Jiang, S. , Li, T. , Sun, X. , & Ma, F. (2020). Depression, anxiety, and their associated factors among Chinese early breast cancer in women under 35 years of age: A cross sectional study. Current Problems in Cancer, 44(5), 100558. [DOI] [PubMed] [Google Scholar]
- Lee, S. , Rhie, S. , & Chae, K. Y. (2013). Depression and marital intimacy level in parents of infants with sleep onset association disorder: a preliminary study on the effect of sleep education. Korean journal of pediatrics, 56(5), 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, H. , Yan, C. , Zhu, S. , Cheng, L. , He, G. , & Lei, J. (2011). Correlation among coping style, social support, and negative emotion in infertile women. Journal of Central South University, 36(2), 138–142. [DOI] [PubMed] [Google Scholar]
- Li, Y. , Wang, K. , Yin, Y. , Li, Y. , & Li, S. (2018). Relationships between family resilience, breast cancer survivors' individual resilience, and caregiver burden: A cross‐sectional study. International Journal of Nursing Studies, 88, 79–84. [DOI] [PubMed] [Google Scholar]
- Lin, X. , Chen, Z. , Jin, L. , Gao, W. , Qu, B. O. , Zuo, Y. , Liu, R. , & Yu, M. (2017). Rasch analysis of the hospital anxiety and depression scale among Chinese cataract patients. PLoS One, 12(9), e0185287. 10.1371/journal.pone.0185287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, D. G. , Wang, S. S. , Peng, R. J. , Qin, T. , & Yuan, Z. Y. (2011). Interaction of social support and psychological stress on anxiety and depressive symptoms in breast cancer patients. Asian Pacific Journal of Cancer Prevention, 12(10), 2523–2529. [PubMed] [Google Scholar]
- Lubben, J. E. , & Gironda, M. W. (2003). Centrality of Social Ties to the Health and Well‐Being of Older Adults. In: Berkman, L . and Harooytan, L. , (Eds.), Social Work and Health Care in an Aging World (pp. 319–350). New York: Springer Press. [Google Scholar]
- Maass, S. W. M. C. , Roorda, C. , Berendsen, A. J. , Verhaak, P. F. M. , & de Bock, G. H. (2015). The prevalence of long‐term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas, 82(1), 100–108. 10.1016/j.maturitas.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Matthews, T. , Danese, A. , Wertz, J. , Odgers, C. L. , Ambler, A. , Moffitt, T. E. , & Arseneault, L. (2016). Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Social Psychiatry and Psychiatric Epidemiology, 51(3), 339–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng, C. G. , Mohamed, S. , Kaur, K. , Sulaiman, A. H. , Zainal, N. Z. , & Taib, N. A. , MyBCC Study Group (2017). Perceived distress and its association with depression and anxiety in breast cancer patients. PLoS One, 12(3), e0172975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Observatory TGC GLOBOCAN (2020) GLOBOCAN. Breast Cancer 2020. http://gco.iarc.fr/today/data/factsheets/cancers/20‐Breast‐fact‐sheet.pdf [Google Scholar]
- Park, E. M. , Gelber, S. , Rosenberg, S. M. , Seah, D. S. E. , Schapira, L. , Come, S. E. , & Partridge, A. H. (2018). Anxiety and depression in young women with metastatic breast cancer: A cross‐sectional study. Psychosomatics, 59(3), 251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puigpinós‐Riera, R. , Graells‐Sans, A. , Serral, G. , Continente, X. , Bargalló, X. , Domènech, M. , Espinosa‐Bravo, M. , Grau, J. , Macià, F. , Manzanera, R. , Pla, M. , Quintana, M. J. , Sala, M. , & Vidal, E. (2018). Anxiety and depression in women with breast cancer: Social and clinical determinants and influence of the social network and social support (DAMA cohort). Cancer Epidemiology, 55, 123–129. 10.1016/j.canep.2018.06.002 [DOI] [PubMed] [Google Scholar]
- Santini, Z. I. , Jose, P. E. , York Cornwell, E. , Koyanagi, A. , Nielsen, L. , Hinrichsen, C. , Meilstrup, C. , Madsen, K. R. , & Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health, 5(1), e62–e70. [DOI] [PubMed] [Google Scholar]
- Shi, L. , Wang, L. , Jia, X. , Li, Z. , Mu, H. , Liu, X. , Peng, B. , Li, A. , & Fan, L. (2017). Prevalence and correlates of symptoms of post‐traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross‐sectional study. BMJ Open, 7(7), e016810. 10.1136/bmjopen-2017-016810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- So, W. K. , Leung, D. Y. , Ho, S. S. , Lai, E. T. , Sit, J. W. , & Chan, C. W. (2013). Associations between social support, prevalent symptoms and health‐related quality of life in Chinese women undergoing treatment for breast cancer: A cross‐sectional study using structural equation modelling. European Journal of Oncology Nursing, 17(4), 442–448. 10.1016/j.ejon.2012.11.001 [DOI] [PubMed] [Google Scholar]
- Taylor, H. O. , Taylor, R. J. , Nguyen, A. W. , & Chatters, L. (2018). Social isolation, depression, and psychological distress among older adults. Journal of aging and health, 30(2), 229–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits, P. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52, 145–161. [DOI] [PubMed] [Google Scholar]
- Tittman, S. M. , Harteau, C. , & Beyer, K. M. (2016). The effects of geographic isolation and social support on the health of Wisconsin women. WMJ, 115(2), 65–69. [PubMed] [Google Scholar]
- Tsaras, K. , Papathanasiou, I. V. , Mitsi, D. , Veneti, A. , & Fradelos, E. C. (2018). Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pacific Journal of Cancer Prevention, 19(6), 1661–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wondimagegnehu, A. , Abebe, W. , Abraha, A. , & Teferra, S. (2019). Depression and social support among breast cancer patients in Addis Ababa, Ethiopia. BMC Cancer, 19(1):836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi, X. , Lu, Q. , Wo, T. , Pei, P. , Lin, G. , Hu, H. , & Ung, C. O. L. (2019). Doctor’s presenteeism and its relationship with anxiety and depression: A cross‐sectional survey study in China. British Medical Journal Open, 9(7), e028844. 10.1136/bmjopen-2018-028844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying, C. Z. , Li, D. , & Loke, A. Y. (2011). Life after cervical cancer: Quality of life among Chinese women. Nursing & Health Sciences, 13(3), 296–302. [DOI] [PubMed] [Google Scholar]
- Zigmond, A. S. , & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


