Abstract
Objectives
To assess the economic burden of COVID-19 that would arise absent behavioral or policy responses under the herd immunity approach in the United States and compare it to the total burden that also accounts for estimates of the value of lives lost.
Methods
We use the trajectories of age-specific human and physical capital in the production process to calculate output changes based on a human capital–augmented production function. We also calculate the total burden that results when including the value of lives lost as calculated from mortality rates of COVID-19 and estimates for the value of a statistical life in the United States based on studies assessing individual’s willingness to pay to avoid risks.
Results
Our results indicate that the GDP loss associated with unmitigated COVID-19 would amount to a cumulative US$1.4 trillion by 2030 assuming that 60 percent of the population is infected over three years. This is equivalent to around 7.7 percent of GDP in 2019 (in constant 2010 US$) or an average tax on yearly output of 0.6 percent. After applying the value of a statistical life to account for the value of lives lost, our analyses show that the total burden can mount to between US$17 and 94 trillion over the next decade, which is equivalent to an annual tax burden between 8 and 43 percent.
Conclusion
Our results show that the United States would incur a sizeable burden if it adopted a non-interventionist herd immunity approach.
Funding
Research reported in this paper was supported by the Alexander von Humboldt Foundation, the Bill & Melinda Gates Foundation (Project INV-006261), and the Sino-German Center for Research Promotion (Project C-0048), which is funded by the German Research Foundation (DFG) and the National Natural Science Foundation of China (NSFC). Preparation of this article was also supported by the Value of Vaccination Research Network (VoVRN) through a grant from the Bill & Melinda Gates Foundation (Grant OPP1158136). The content is solely the responsibility of the authors.
Keywords: COVID-19, Economic burden, Health-augmented macroeconomic model, Herd immunity, Human capital, Production function, United States, Value of a statistical life
Introduction
In late 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes the coronavirus disease 2019 (COVID-19), emerged in the city of Wuhan in China (Wang et al., 2020). The virus then rapidly spread to almost all countries in the world. Millions of people have been infected since then, many of them were hospitalized, and more than 2.7 million people worldwide were confirmed dead with or from COVID-19 as of March 22, 2021. About 20 percent of those deaths occurred in the United States (Johns Hopkins University, 2020). To fight the spread of the disease, most countries enacted unprecedented lockdown measures, such as closing schools, restaurants, and shops; restricting national and international travel; and implementing social distancing measures or preventing gatherings altogether (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c, Chen et al., 2020d, Dye et al., 2020, Omar et al., 2020, Parodi and Liu, 2020). Besides the large health and social burden, the economic burden of COVID-19 and of the policy measures against its spread are also huge. Several studies show that this holds for various policy and behavioral scenarios (Acemoglu et al., 2020, Cutler and Summers, 2020, Eichenbaum et al., 2020, Glover et al., 2020, International Monetary Fund, 2020a, International Monetary Fund, 2020b, Krueger et al., 2020).
One crucial difficulty in estimating the economic burden of COVID-19 involves disentangling the economic impact of the disease due to higher mortality, morbidity, and reduced investment because of treatment costs, from the indirect impact of behavioral and policy responses. While the disruptions caused by lockdown measures and travel restrictions have yielded demonstrably large losses in consumption, output, and investment, these are indirect effects of the disease, some portion of which is transitory. For a thorough understanding of the tradeoff that policymakers face in the context of COVID-19, knowing the economic consequences of the outbreak without behavioral and policy responses is essential. Researchers have made highly valuable contributions in identifying these consequences by means of susceptible-infected-recovered (SIR) amended macroeconomic models employed in simulation studies (Acemoglu et al., 2020, Eichenbaum et al., 2020, Glover et al., 2020, Krueger et al., 2020). However, these approaches typically feature simplified production functions, where output is produced only by labor under a constant returns to scale technology, and the age structure of the workforce is usually not considered. While these simplifications make these complex models with many different behavioral channels and general equilibrium repercussions more manageable, they also prevent a deeper understanding of (i) nonlinearities when larger parts of the population fall ill, (ii) longer-term effects through changes in capital accumulation, and (iii) the age-structure-dependent effects of COVID-19 that are associated with a much higher mortality of individuals beyond the prime working ages.
Our contribution aims to complement the results of SIR-amended macroeconomic models by establishing the economic burden of COVID-19 absent behavioral and policy responses, accounting for the age- and human capital-specific effects of COVID-19 on the workforce and the effects of treatment costs on capital accumulation. In doing so, we apply the health-augmented macroeconomic model (HMM), which is based on a human-capital augmented production function that we have co-developed and applied previously to estimate the economic burden of noncommunicable diseases, of diseases due to smoking or air pollution, and of road accidents (Bloom et al., 2020a, Bloom et al., 2020b, Bloom et al., 2020c, Bloom et al., 2020d, Bloom et al., 2019, Chen et al., 2018, Chen et al., 2019a, Chen et al., 2019b, Chen et al., 2019c, Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c, Chen et al., 2020d, Chen et al., 2020e, Chen et al., 2020f, Chen et al., 2021). This approach traces the disease’s age-specific mortality and morbidity impacts on labor supply and the effects of treatment costs on physical capital accumulation. The resulting trajectories of age-specific human capital and physical capital in the production process are then used to calculate disease-induced output changes based on the human capital–augmented production function calibrated with parameters of the U.S. economy.
We are considering a counterfactual scenario in which behavioral reactions of individuals and policy responses are absent. This scenario allows us to establish a nonintervention benchmark against which to assess the “stakes” of policymaking. The benchmark can be understood as a conservative estimate of the total burden associated with the disease if the U.S. follows a strategy of achieving herd immunity through overcoming natural infection (see e.g. the Great Barrington Declaration; Alwan et al., 2020)—a conservative estimate because the assessment does not include the value of human lives lost or the value of suffering from the disease, which likely (and we show) greatly outweigh the economic burden (Cutler and Summers, 2020). Our scenario may also be considered conservative as it does not factor in behavioral responses, i.e., changes in consumption and work patterns for fear of infection even absent any policy. These have shown to be substantial (Goolsbee and Syverson, 2020). The savings response is somewhat more ambiguous, as people might save more both because consumption decreases and as a precaution for future uncertain work prospects. Furthermore, as Polyakova et al. (2020) show, there might be spillover effects of infections that our framework does not capture.
The crucial lesson of our paper is that even our estimate of the economic burden of COVID-19 is sizeable and strongly supports investing in health care infrastructure, early disease surveillance, and the delivery of treatments and vaccines to prevent or contain potential future epidemics at an early stage. When we consider the value of lives lost in addition to the loss of gross domestic product (GDP), the total burden of COVID-19 increases substantially, which only strengthens our conclusion.
Methodology
Model description and data sources
A pandemic affects the economy in the long run via the following direct channels: (i) disease-specific and age-dependent mortality reduces labor supply and therefore human capital. The extent to which it does so depends on the age structure of those who die because of the disease. (ii) Disease- and age-specific morbidity also reduces individual labor supply, but recovery usually follows such that the morbidity effects are not permanent. This hinges on the assumption that recovery is full, which might not be the case for all patients in reality (Carfì et al., 2020). To account for this possibility, we include an additional scenario with long-term morbidity in our projections; (iii) Treatment is costly and can be paid for in two ways. First, by reducing consumption—which is tantamount to reallocating expenditures toward healthcare and, as such, does not affect GDP—and, second, by reducing savings/investment, which reduces capital accumulation and therefore future output.
To capture these channels and to allow for a certain degree of substitutability among workers and between workers and physical capital, we consider an economy in which aggregate output (GDP) is produced according to the production function
| (1) |
where refers to total factor productivity; denotes the physical capital stock used in production; is the elasticity of output with respect to physical capital; and is aggregate human capital, which is the product of age-specific labor supply, , age-specific human capital, , and age-specific productivity (e.g., as determined by morbidity), , summed from the age of labor market entry up to retirement at age . This calculation is based on the labor force projections of the International Labour Organization (2017) and allows us to recognize that children do not work and that older adults might be retired. The dynamics of individual human capital are based on the educational attainment projections of Barro and Lee (2013) and workforce experience within a Mincerian specification (Mincer, 1974). The estimated parameters for the Mincerian specification come from Psacharopoulos and Patrinos (2018) for education and Heckman et al. (2006) for experience (Heckman et al., 2006). Data on age-specific COVID-19 mortality come from Stokes et al. (2020). We assume that 60 percent of the population will be infected over three years (Anderson et al., 2020) and that for those who enjoy a full recovery the process takes an average of 14 days, (World Health Organization, 2020) which is also the time span of a quarantine in many countries.
In a closed economy without a government, aggregate output equals aggregate income. Output/income can be consumed or saved such that the aggregate capital accumulation equation is given by
| (2) |
where and are aggregate treatment costs and aggregate consumption, respectively; is the saving rate, which, in the underlying Solow (1956) framework for a closed economy, is tantamount to the gross investment rate; and is the rate at which physical capital depreciates. For the parameters, we either assume standard values from the literature or values that are consistent with the data such that we have , , and (Prettner, 2019, U.S. Bureau of Labor Statistics, 2017, World Bank, 2020b). Finally, for the treatment costs we use US$3,045 per infection as calculated by Bartsch et al. (2020) for symptomatic infections and assume that the fraction of treatment costs that is paid out of savings is the same as the gross saving rate in the United States.
Using physical capital and age-specific human capital projections, we calculate the economic burden of COVID-19 as the difference between a simulated counterfactual economy without the disease and a simulated economy in which 60 percent of the population is eventually infected. For the economic projections we consider the time span 2020–2030 and assume that the pandemic occurs in the first three years after which herd immunity is achieved. This timing rests on the assumption that herd immunity without vaccination requires 230 million persons to be infected. At the peak of infections in January 2021, there were approximately 200,000 infections per day. At that pace, it would have required approximately three years to reach 230 million infections. While our scenario is therefore plausible, other dynamics of infections could also have easily emerged. However, our results only change marginally under the assumption of a different timing (e.g., a concentration of infections within two years or spreading out the infections over four years). Our projections deliberately abstract from behavioral and policy responses, in particular, the availability of vaccination (Anderson et al., 2020). The Online Appendix provides a more detailed description of the model and our simulation approach.
Projection scenarios
We construct and analyze the following projection scenarios: (i) baseline scenario: we use the fatality rates from Stokes et al. (2020); (ii) high-mortality scenario: we take the result by Weinberger et al. (2020), who report that (overall) excess mortality was 28 percent higher than reported COVID-19 mortality and use this to scale up the fatality rates from Stokes et al. (2020); (iii) low-mortality scenario: because many people who had COVID-19 may have been asymptomatic and were not tested, we use the estimated infection fatality rate (instead of the case fatality rate) of New York City (Yang et al., 2020) for this scenario; and (iv) long-term morbidity scenario: we assume 30 percent of those who contracted COVID-19 show symptoms in the long run and would therefore permanently lose on average 10 percent of their productivity. This is similar to estimates related to the SARS outbreak in 2002/2003 (Ahmed et al., 2020, Fraser, 2020). In all scenarios we assume that there is no reinfection.
Total burden after accounting for the loss of life
We estimate the total burden after accounting for the value of lives lost by relying on the value of a statistical life (VSL) approach. The VSL, defined as the willingness to pay for survival or, equivalently, the marginal rate of substitution between survival and consumption, measures the present value of the utility stream over the remaining expected life-course and is, thus, well grounded in life-cycle theory (Murphy and Topel, 2006). Notably, for plausible parametrizations of the utility function and based on consumption/income data one arrives at magnitudes of the VSL that are comparable to empirical estimates derived, e.g., from compensating wage regressions for hazardous occupations (Murphy and Topel, 2006, Viscusi and Aldy, 2003). As we illustrate in the Online Appendix, the value of lost lives is, indeed, additive to the GDP loss when assessing the total welfare loss from COVID-19. For scenarios (i) to (iii), we use the corresponding case fatality rates to calculate the number of deaths, which equals the population × total infection rate × case fatality rate. Then we multiply the death count with a recent estimate of the VSL in the U.S. that amounts to 7 million US$, the same number used in Cutler and Summers (2020), which is a conservative estimate compared to the 9.6 million US$ in Viscusi and Masterman (2017). For scenario (iv), we further added to the estimate in the baseline scenario a loss in the quality of life from long-term disease, where we assume that 30 percent of the infected individuals experience a 10 percent reduction in the VSL.
When calculated as a population mean based on the distribution of general mortality, the average VSL may be too high in the context of COVID-19. This is because COVID-19 mortality is heavily skewed towards older adults who face a lower remaining life-time and, thus, a lower age-specific VSL (Murphy and Topel, 2006). For the sake of robustness, we thus provide, for each scenario, an additional set of calculations based on an age-adjusted VSL. For this, we apply the age-specific VSL figures calculated based on Greenstone and Nigam (2020) 1 to the age-specific death counts in Stokes et al. (2020) and arrive at an age-adjusted estimate of the VSL in the U.S. that amounts to 4.5 million US$.
Results
Our baseline results show that the economic burden of COVID-19 amounts to about US$1.4 trillion cumulatively by 2030 (Table 1 ). For comparison, this is approximately 7.7 percent of U.S. GDP in 2019 (in constant 2010 US$). The economic burden of COVID-19 each year up to 2030 is tantamount to a tax on yearly income between 0.4 and 1.7 percent (and 0.6 percent on average). After accounting for the value of lives lost, the total burden of COVID-19 amounts to an aggregate loss between US$ 17 trillion and 94 trillion cumulatively by 2030, which is equivalent to a tax on yearly income between 8 and 43 percent.
Table 1.
Economic burden of COVID-19 and the overall burden of COVID-19 after accounting for the value of lives lost in the United States.
| Scenario | Economic burden, billions of constant 2010 US$ | Percentage of total gross domestic product in 2020–2030 | Per capita burden1, constant 2010 US$ | Aggregate Deaths (million) |
|---|---|---|---|---|
| Baseline | 1354 | 0.63% | 4036 | 7.405 |
| High mortality | 1609 | 0.75% | 4793 | 9.479 |
| Low mortality | 808 | 0.38% | 2409 | 3.568 |
| Long-term morbidity | 3733 | 1.73% | 11,125 | 7.405 |
| Baseline (VSL)2 | 51,841 | 24.04% | 154,527 | 7.405 |
| High mortality (VSL) | 66,356 | 30.78% | 197,795 | 9.479 |
| Low mortality (VSL) | 24,978 | 11.59% | 74,454 | 3.568 |
| Long-term morbidity (VSL) | 93,547 | 43.39% | 278,846 | 7.405 |
| Baseline (age-adjusted VSL)3 | 33,901 | 15.72% | 101,052 | 7.405 |
| High mortality (age-adjusted VSL) | 42,946 | 19.92% | 128,014 | 9.479 |
| Low mortality (age-adjusted VSL) | 17,391 | 8.07% | 51,837 | 3.568 |
| Long-term morbidity (age-adjusted VSL) | 78,652 | 36.48% | 234,447 | 7.405 |
Note: 1 Per capita burden is calculated as the GDP reduction divided by the average population over the projected period.2 VSL based on Cutler and Summers (2020); 3 Age-adjusted VSL based on age-specific VSL, as reported in Greenstone and Nigam (2020), and age-specific COVID-19 death rates, as reported in Stokes et al. (2020).
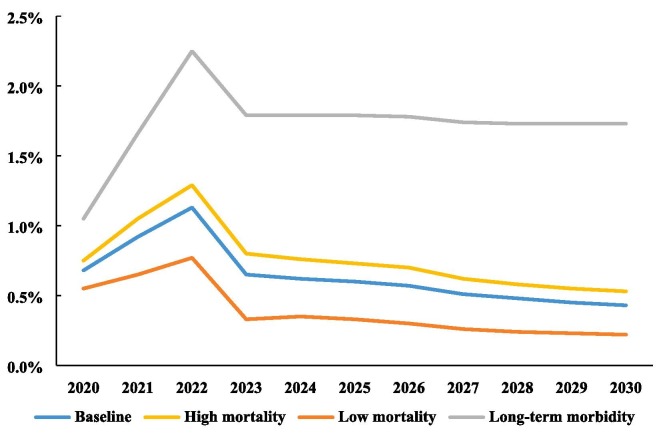
Fig. 1 illustrates the evolution of the tax rate corresponding to the economic burden (without the value of lives lost) over time. Because our assumptions are that the pandemic will end after three years and that 60 percent of the population will become infected by then, the burden is particularly high in the first three years.2 Morbidity effects (with the exception of long-term morbidity in Scenario ii) and treatment costs both only accrue in the first three years of the pandemic in the baseline scenario. However, the mortality effects are permanent because they reduce labor supply not only in the three years in which people died but over the whole time horizon of the projections. Altogether, morbidity and treatment cost effects amount to 22.5 percent and 9 percent of the total loss of GDP in 2020–2030, with mortality making up for 68.5 percent.
Fig. 1.
Economic burden of COVID-19 under a herd immunity approach in the U.S. expressed as a percentage of yearly GDP (excluding short-run effects through, e.g., travel restrictions, lockdown measures, and social distancing).
Eichenbaum et al. (2020) estimate a long-run GDP drop of 0.65 percent, which, unlike current reductions in GDP and associated short-run projections, is permanent and can be compared with our long-run yearly burden of 0.44 percent of GDP after 10 years. Our somewhat lower estimate is due to three differences between our analysis and that of Eichenbaum et al. (2020): (i) They assume that 65 percent of the population will be infected eventually, which is a bit higher than the 60 percent suggested by Anderson et al. (2020) (ii) Unlike Eichenbaum et al. (2020), we consider the age structure of the workers who die. Because they are predominantly older and might not be working anymore, the calculated economic burden is somewhat smaller as compared with the scenario of Eichenbaum et al. (2020). (iii) We allow for capital in the production function. In comparison to Eichenbaum et al. (2020), capital-for-labor substitution then mitigates the impact of the loss of labor on GDP in the short-run. However, the reduction in capital accumulation due to treatment costs leads to an additional loss in GDP in the long-run.
At this point we must stress that many (very different) assumptions about the disease dynamics are plausible. First, the pandemic could end much earlier, for example, with the development of a vaccine (Mullard, 2020). However, vaccination is a behavioral/policy response to the pandemic from which we abstract deliberately. Even if we were to consider vaccination, vaccines may be delayed in terms of development, testing, manufacture, or delivery, they may confer imperfect protection, or their acceptance may be too low among the population to stop the pandemic. Second, how long immunity lasts after recovery remains unclear. If immunity is long lasting, the pandemic will likely die out. If, by contrast, immunity is short lived, the pandemic might not end and COVID-19 could become a recurring disease similar to the flu (Chen et al., 2020a, Chowell and Mizumoto, 2020). Third, many asymptomatic cases may not have been detected (Long et al., 2020). This would lead to an overestimate of the burden in our framework because more of the population was already infected and could be immune. However, many of those who get infected may not recover fully, (Carfì et al., 2020) which would suggest that our estimates are conservative. Overall, these points underscore the uncertainties associated with the estimates of the economic burden of COVID-19 and point to the need for reliable and representative underlying epidemiological data.
To alleviate these concerns to some extent, we considered alternative scenarios with (i) a higher mortality rate based on estimates of excess mortality (Weinberger et al., 2020), (ii) a lower mortality rate in line with the infection fatality rate (instead of the case fatality rate) of New York City (Yang et al., 2020) which takes into consideration that many people who had COVID-19 may have been asymptomatic and were not tested, and (iii) a permanent morbidity effect of 10 percent for 30 percent of the population, similar to the estimates related to the SARS outbreak in 2002/2003 (Ahmed et al., 2020, Fraser, 2020). In the low-mortality scenario without a long-term morbidity effect, the economic burden reduces to US$808 billion; whereas in the high-mortality scenario it increases to US$1.6 trillion; and in case of baseline mortality but long-term morbidity effects, the economic burden rises to US$3.7 trillion. While this indicates considerable uncertainty of the calculations depending on the underlying epidemiological properties, the general conclusion of a sizeable economic burden of COVID-19 is clearly upheld.
Discussion
Our results show that the economic burden of COVID-19 under a herd immunity approach is sizeable. This is despite the fact that COVID-19 disproportionately affects people beyond their prime working ages and despite the fact that treatment costs for surviving individuals do not accrue over the full remaining lifetime, as they would for chronic diseases, but typically only over a few weeks. For the 10-year time span 2020–2030, we estimate an economic burden of COVID-19 of US$1.4 trillion, which is equivalent to around 7.7 percent of GDP in 2019 (in constant 2010 US$) (World Bank World Bank database, 2020a). The magnitude of the economic burden of COVID-19 becomes evident when we compare it to our model’s estimate of the economic burden of all chronic respiratory diseases (US$ 0.4 trillion) or all cardiovascular diseases (US$ 1.1 trillion) for the U.S. over the same time period (Chen et al., 2018). Our calculations also show that accounting for the value of lost lives would raise the burden substantially to a value of 17 to 94 trillion US$, or equivalently to an annual tax burden of 8 to 43 percent, over the next decade even using a conservative estimate of the VSL as the underlying value. Our results are prone to depict a lower bound of the total burden for further reasons. First, we have not included the treatment cost and value of quality of life lost due to mental health issues associated with an unchecked pandemic. Second, we did not consider the loss of life and health due to the lack of treatment of other diseases within an overloaded healthcare system. Third, neither have we included the value of the economic contributions of older adults, such as care for their grandchildren, as is assessed in Bloom et al. (2020c). Finally, we did not consider the loss from pain and suffering.
Our results indicate that implementing the so-called herd immunity approach, as suggested by the Great Barrington Declaration, would lead to a sizeable economic burden, which increases further when accounting for lives lost. In the latter case, we arrive at values of about 1.6 to 5.9 times the 16 trillion US$ loss estimated by Cutler and Summers (2020) under their assumptions on the disease dynamics, particularly that the pandemic will be substantially contained by the fall of 2021 (Cutler and Summers, 2020).
Overall, our results stand in sharp contrast to the remarks of then White House economic adviser Lawrence Kudlow, who claimed that “It’s like a big bad hurricane or a bad snowstorm. It’s a natural disaster. And we’ve seen in the past with natural disasters, they come and they inflict enormous pain. And this virus has inflicted horrible pain. But the disaster passes and therefore has very little damage to what I call the structural aspects of the economy.” (Axios)
Ultimately, the long-run economic burden is so high that it dwarfs plausible cost calculations for financing the development, manufacture, and delivery of a vaccine or developing and delivering an effective COVID-19 treatment. Estimates of the costs of developing new vaccines for epidemic infectious diseases range from US$2.8 billion to US3.7 billion (Gouglas et al., 2018), and the European Union committed to funding US$7.6 billion to develop a vaccine against SARS-CoV-2 in early May 2020 (Geoffard, 2020). Furthermore, investing in research and development (R&D) of treatments, vaccines, and infrastructure that contribute to containing similar future epidemics would be highly beneficial in the long run. R&D incentives may be improved in this respect by introducing innovation prizes or advance market commitments as well as by governmental coordination and support, such as the U.S. “Operation Warp Speed” and similar initiatives around the globe (Bloom et al., 2020a, Kremer et al., 2020, Kremer and Williams, 2010, Slaoui and Hepburn, 2020). Our calculations also make clear that high priority should be placed on preventing future pandemics at the outset and to design emergency mechanisms that allow for an optimal response in case of a future outbreak. In the initial phase of an epidemic with the threat of becoming a pandemic, lockdown measures are the only game in town to keep the spread in check. The sooner vaccines, treatments, sufficient protective equipment for the extensive use even by the general population, and population-wide testing and contact tracing at massive scale become feasible, the shorter is the period in which societies would need to rely on lockdowns and their negative repercussions.
The limitations of our study are that (i) it relies strongly on the underlying assumptions about the disease dynamics and therefore requires solid data as inputs from epidemiological studies; (ii) with our framework we cannot assess the effects of COVID-19 on inequality and regional disparities; (iii) a potential long-run effect of behavioral responses could emerge if changes in today’s behavior lead to changing technological progress in the future such as more automation, because machines are not susceptible to pathogens that affect humans (Prettner and Bloom, 2020); (iv) we cannot consider productivity effects of worsened mental health and worsened physical health due to the lack of treatment of non-COVID diseases in overloaded healthcare systems, (v) we cannot consider the repercussions of the pandemic on educational outcomes, and (vi) global trade patterns could change due to disruptions in supply chains and efforts toward reshoring (at least strategically important) production. Analyzing the effects of COVID-19 on automation, education, general health, inequality, and the incentives to reshore production would require a much more detailed modeling of the socioeconomic background of the household side of the economy, of international trade patterns and supply chains, and of the R&D sector to characterize innovation and technology adoption. Models that address these issues but in a setting with representative agents in which health does not play any role are currently being developed (Krenz et al., 2021, Prettner and Strulik, 2020). To focus on the macroeconomic burden of COVID-19 mortality and morbidity and its treatment costs, we abstract from these types of complications. However, adopting these frameworks to account for health and in particular for infectious diseases is a challenging but interesting avenue for further research.
Appendix
CRediT authorship contribution statement
Simiao Chen: Conceptualization, Methodology, Data curation, Formal analysis. Klaus Prettner: Conceptualization, Methodology, Data curation, Formal analysis. Michael Kuhn: Conceptualization, Methodology, Data curation, Formal analysis. David E. Bloom: Conceptualization, Methodology, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We would like to thank Maddalena Ferranna for thoughtful comments and suggestions.
Footnotes
See Table S2 in the Online Appendix.
In other words, the sharp decline after three years is due to the fact that the morbidity effect and the treatment costs accrue only during the time periods in which the pandemic rages and infections spread. Afterwards, the morbidity effect and the corresponding treatment cost effect vanish, which explains the drop after three years. The mortality effect, however, is permanent because people who died cannot recover. At the aggregate level, this effect only vanes with the general mortality of the rest of the population.
References
- Acemoglu, D., Chernozhukov, V., Werning, I., & Whinston, M. D. A multi-risk SIR model with optimally targeted lockdown (2020) (0898-2937). Retrieved from Cambridge, Massachusetts.
- Ahmed H., Patel K., Greenwood D.C., Halpin S., Lewthwaite P., Salawu A., Jones A. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J. Rehabil. Med. 2020;52(5) doi: 10.2340/16501977-2694. jrm00063. [DOI] [PubMed] [Google Scholar]
- Alwan, N. A., Burgess, R. A., Ashworth, S., Beale, R., Bhadelia, N., Bogaert, D., . . . Ziauddeen, H. Scientific consensus on the COVID-19 pandemic: we need to act now. The Lancet, Published Online October 14, 2020. doi:10.1016/S0140-6736(20)32153-X. [DOI] [PMC free article] [PubMed]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.Déirdre. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axios. (Jun 23, 2020). Why the pandemic isn't like a hurricane. Retrieved from https://www.axios.com/larry-kudlow-coronavirus-big-bad-hurricane-00025a6f-1b79-4959-bed3-6888cb37628d.html.
- Barro, R. J., & Lee, J. W. (2013). A new data set of educational attainment in the world, 1950–2010. J. Develop. Econ., 104(September 2013), 184–198. Retrieved from http://www.barrolee.com.
- Bartsch S.M., Ferguson M.C., McKinnell J.A., O'Shea K.J., Wedlock P.T., Siegmund S.S., Lee B.Y. The potential health care costs and resource use associated with COVID-19 In The United States: a simulation estimate of the direct medical costs and health care resource use associated with COVID-19 infections in the United States. Health Aff. 2020;39(6):927–935. doi: 10.1377/hlthaff.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom, D. E., Cadarette, D., Tortorice, D.L., 2020. Vaccine finance and epidemics: An ounce of prevention is worth a pound of cure. Finance and Development. Retrieved from https://www.imf.org/external/pubs/ft/fandd/2020/09/vaccine-finance-epidemics-and-prevention-bloom.htm.
- Bloom D.E., Chen S., Kuhn M., McGovern M.E., Oxley L., Prettner K. The economic burden of chronic diseases: Estimates and projections for China, Japan, and South Korea. J. Econ. Age. 2020;17(2020):10016. doi: 10.1016/j.jeoa.2018.09.002. [DOI] [Google Scholar]
- Bloom, D.E., Chen, S., Kuhn, M., Prettner, K., 2019. The flip side of “live long and prosper”: Noncommunicable diseases in the OECD and their macroeconomic impact. In: D. E. Bloom (Ed.), Live Long and Prosper? The Economics of Ageing Populations (pp. 44).
- Bloom D.E., Khoury A., Algur E., Sevilla J.P. Valuing productive non-market activities of older adults in Europe and the US. De Economist. 2020;168(2):153–181. [Google Scholar]
- Bloom, D.E., Kuhn, M., Prettner, K., 2020. Modern Infectious Diseases: Macroeconomic Impacts and Policy Responses (0898-2937). Retrieved from Cambridge, Massachusetts.
- Carfì A., Bernabei R., Landi F. Persistent symptoms in patients after acute covid-19. JAMA. 2020;324(6):603. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Bloom D.E., Sun Q. The macroeconomic burden of noncommunicable diseases associated with air pollution in China. PLoS ONE. 2019;14(4):e0215663. doi: 10.1371/journal.pone.0215663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Chen Q., Yang W., Xue L., Liu Y., Yang J., Wang C., Bärnighausen T. Buying time for an effective epidemic response: the impact of a public holiday for outbreak control on COVID-19 epidemic spread. Engineering. 2020;6(10):1108–1114. doi: 10.1016/j.eng.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Jin Z., Bloom D.E. Institute of Labor Economics; Bonn, Germany: 2020. Act Early to Prevent Infections and Save Lives: Causal Impact of Diagnostic Efficiency on the COVID-19 Pandemic. [Google Scholar]
- Chen S., Kuhn M., Prettner K. Tobacco Control policies: the authors reply. Health Affairs (Project Hope) 2020;39(2):346. doi: 10.1377/hlthaff.2019.01661. [DOI] [PubMed] [Google Scholar]
- Chen S., Kuhn M., Prettner K., Bloom D.E., Husain M.J. The macroeconomic burden of noncommunicable diseases in the United States: Estimates and projections. PLoS ONE. 2018;13(11):e0206702. doi: 10.1371/journal.pone.0206702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Kuhn M., Prettner K., Bloom D.E. The global macroeconomic burden of road injuries: estimates and projections for 166 countries. Lancet Planetary Health. 2019;3(9):e390–e398. doi: 10.1016/S2542-5196(19)30170-6. [DOI] [PubMed] [Google Scholar]
- Chen S., Kuhn M., Prettner K., Bloom D.E. Noncommunicable diseases attributable to tobacco use in China: macroeconomic burden and tobacco control policies. Health Aff. 2019;38(11):1832–1839. doi: 10.1377/hlthaff.2019.00291. [DOI] [PubMed] [Google Scholar]
- Chen S., Prettner K., Cao B., Geldsetzer P., Kuhn M., Bloom D.E., Wang C. Revisiting the association between temperature and COVID-19 transmissibility across 117 countries. ERJ Open Res. 2020;6(4) doi: 10.1183/23120541.00550-2020. 00550-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395(10226):764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Zhang Z., Yang J., Wang J., Zhai X., Bärnighausen T., Wang C. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Prettner K., Kuhn M., Geldsetzer P., Wang C., Bärnighausen T., Bloom D.E. Climate and the spread of COVID-19. Sci. Rep. 2021;11(1):1–6. doi: 10.1038/s41598-021-87692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowell G., Mizumoto K. The COVID-19 pandemic in the USA: what might we expect? The Lancet. 2020;395(10230):1093–1094. doi: 10.1016/S0140-6736(20)30743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D.M., Summers L.H. The COVID-19 pandemic and the $16 trillion virus. JAMA. 2020;324(15):1495–1496. doi: 10.1001/jama.2020.19759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye D., Sarker M., Chen S., Lenjani A., Tikka P., Bärnighausen T., Geldsetzer P. Healthcare worker attendance during the early stages of the COVID-19 pandemic: a longitudinal analysis of daily fingerprint-verified data from all public-sector secondary and tertiary care facilities in Bangladesh. J. Global Health. 2020;10(2) doi: 10.7189/jogh.10.020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichenbaum, M. S., Rebelo, S., Trabandt, M., 2020. The macroeconomics of epidemics (2020) (0898-2937). Retrieved from Cambridge, Massachusetts.
- Fraser E. Long term respiratory complications of covid-19. Br. Med. J. 2020;2020(370) doi: 10.1136/bmj.m3001. [DOI] [PubMed] [Google Scholar]
- Geoffard, P.-Y. (June 4, 2020). Covid-19: Speeding up vaccine development. Retrieved from https://voxeu.org/article/accelerating-development-covid-19-vaccine.
- Glover, A., Heathcote, J., Krueger, D., Ríos-Rull, J.-V., 2020. Health versus wealth: On the distributional effects of controlling a pandemic (2020) (0898-2937). Retrieved from Cambridge, Massachusetts.
- Goolsbee A., Syverson C. Fear, lockdown, and diversion: comparing drivers of pandemic economic decline 2020. J. Public Econ. 2020;193 doi: 10.1016/j.jpubeco.2020.104311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouglas D., Thanh Le T., Henderson K., Kaloudis A., Danielsen T., Hammersland N.C., Robinson J.M., Heaton P.M., Røttingen J.-A. Estimating the cost of vaccine development against epidemic infectious diseases: a cost minimisation study. Lancet Global Health. 2018;6(12):e1386–e1396. doi: 10.1016/S2214-109X(18)30346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenstone, M., Nigam, V., 2020. Does social distancing matter? University of Chicago, Becker Friedman Institute for Economics Working Paper(2020-26).
- Heckman, J.J., Lochner, L.J., Todd, P.E., 2006. Earnings functions, rates of return and treatment effects: The Mincer equation and beyond. Handbook of the Economics of Education, 1(2006), 307–458. doi:10.1016/S1574-0692(06)01007-5.
- International Labour Organization. (2017). Labour force by sex and age (thousands). Retrieved from http://ilo.org/global/statistics-and-databases/lang--en/index.htm.
- International Monetary Fund. (June 2020). A Crisis Like No Other, An Uncertain Recovery. Retrieved from https://www.imf.org/en/Publications/WEO/Issues/2020/06/24/WEOUpdateJune2020.
- International Monetary Fund. (April 2020). World Economic Outlook, April 2020: The Great Lockdown. Retrieved from https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020.
- Johns Hopkins University. (Oct 19, 2020). COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Retrieved from https://coronavirus.jhu.edu/map.html.
- Kremer, M., Levin, J., & Snyder, C. M. (2020). Advance Market Commitments: Insights from Theory and Experience. Paper presented at the AEA Papers and Proceedings.
- Kremer M., Williams H. Incentivizing innovation: Adding to the tool kit. Innov. Policy Econ. 2010;10(1):1–17. [Google Scholar]
- Krueger, D., Uhlig, H., Xie, T., 2020. Macroeconomic dynamics and reallocation in an epidemic (2020) (0898-2937). Retrieved from Cambridge, Massachusetts.
- Krenz A., Prettner K., Strulik H. European Economic Review; 2021. (Robots, Reshoring, and The Lot of Low-Skilled Workers). In press. [Google Scholar]
- Long Q.-X., Tang X.-J., Shi Q.-L., Li Q., Deng H.-J., Yuan J., Hu J.-L., Xu W., Zhang Y., Lv F.-J., Su K., Zhang F., Gong J., Wu B., Liu X.-M., Li J.-J., Qiu J.-F., Chen J., Huang A.-L. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 2020;26(8):1200–1204. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- Mincer J. Schooling, Experience, and Earnings. Human Behavior & Social Institutions. 1974;No. 2:261. [Google Scholar]
- Mullard A. COVID-19 vaccine development pipeline gears up. Lancet. 2020;395(10239):1751–1752. doi: 10.1016/S0140-6736(20)31252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy K.M., Topel R.H. The value of health and longevity. J. Political Econ. 2006;114(5):871–904. [Google Scholar]
- Omar, S., Bartz, C., Becker, S., Basenach, S., Pfeifer, S., Trapp, C., Zanger, P., 2020. Duration of SARS-CoV-2 RNA detection in COVID-19 patients in home isolation, Rhineland-Palatinate, Germany, 2020 – an interval-censored survival analysis. Eurosurveillance, 25(30), 2001292. doi:doi:https://doi.org/10.2807/1560-7917.ES.2020.25.30.2001292. [DOI] [PMC free article] [PubMed]
- Parodi S.M., Liu V.X. From containment to mitigation of COVID-19 in the US. JAMA. 2020;323(15):1441–1442. doi: 10.1001/jama.2020.3882. [DOI] [PubMed] [Google Scholar]
- Polyakova M., Kocks G., Udalova V., Finkelstein A. Initial economic damage from the COVID-19 pandemic in the United States is more widespread across ages and geographies than initial mortality impacts. Proc. Natl. Acad. Sci. 2020;117(45):27934–27939. doi: 10.1073/pnas.2014279117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prettner K. A note on the implications of automation for economic growth and the labor share. Macroeconomic Dynamics. 2019;23(3):1294–1301. [Google Scholar]
- Prettner K., Bloom D. Elsevier; United States and United Kingdom: 2020. Automation and Its Macroeconomic Consequences: Theory, Evidence, and Social Impacts. [Google Scholar]
- Prettner K., Strulik H. Innovation, automation, and inequality: policy challenges in the race against the machine. J. Monetary Econ. 2020;116:249–265. [Google Scholar]
- Psacharopoulos G., Patrinos H.A. Returns to investment in education: a decennial review of the global literature. Educat. Econ. 2018;26(5):445–458. doi: 10.1080/09645292.2018.1484426. [DOI] [Google Scholar]
- Slaoui M., Hepburn M. Developing safe and effective Covid vaccines—Operation Warp Speed’s strategy and approach. N. Engl. J. Med. 2020;383(18):1701–1703. doi: 10.1056/NEJMp2027405. [DOI] [PubMed] [Google Scholar]
- Solow R.M. A contribution to the theory of economic growth. Quart. J. Econ. 1956;70(1):65–94. [Google Scholar]
- Stokes E.K., Zambrano L.D., Anderson K.N., Marder E.P., Raz K.M., El Burai Felix S., Tie Y., Fullerton K.E. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. Morb. Mortal. Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. (February 2017). Estimating the U.S. labor share. Retrieved from https://www.bls.gov/opub/mlr/2017/article/estimating-the-us-labor-share.htm.
- Viscusi W.K., Aldy J.E. The value of a statistical life: a critical review of market estimates throughout the world. J. Risk Uncertainty. 2003;27(1):5–76. [Google Scholar]
- Viscusi W.K., Masterman C.J. Income elasticities and global values of a statistical life. J. Benefit-Cost Anal. 2017;8(2):226–250. [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., Pitzer V.E., Reich N.G., Russi M., Simonsen L., Watkins A., Viboud C. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Internal Med. 2020;180(10):1336. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. (2020a). World Bank database, GDP (constant 2010 US$). Retrieved from https://data.worldbank.org/indicator/NY.GDP.MKTP.KD?view=chart.
- World Bank. (2020b). World Development Indicators. Retrieved from https://databank.worldbank.org/source/world-development-indicators.
- World Health Organization. (2020). Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Retrieved from Geneva, Switzerland.
- Yang W., Kandula S., Huynh M., Greene S.K., Van Wye G., Li W., Chan H.T., McGibbon E., Yeung A., Olson D., Fine A., Shaman J. Estimating the infection-fatality risk of SARS-CoV-2 in New York City during the spring 2020 pandemic wave: a model-based analysis. Lancet. Infect. Dis. 2020;21(2):203–212. doi: 10.1016/S1473-3099(20)30769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]