Abstract
Objective:
Homelessness is the greatest risk factor for HIV viremia in San Francisco. Innovative care models for people with HIV (PWH) with homelessness or unstable housing (HUH) are needed to address this inequity. We developed a novel low-barrier clinic-based program for PWH-HUH in an urban safety-net clinic (“POP-UP”) and report outcomes on care engagement and viral suppression.
Design:
Prospective cohort study
Setting:
San Francisco General Hospital HIV Clinic (Ward 86)
Participants:
We enrolled PWH who are HUH, viremic, and for whom usual care is not working (≥1 missed primary care appointment and ≥2 drop-in visits at Ward 86 in the last year).
Intervention:
POP-UP provides drop-in comprehensive primary care, housing assistance and case management, financial incentives, and patient navigation with frequent contact.
Main outcome measures:
We describe uptake of eligible patients into POP-UP, and cumulative incidence of ART initiation, return to care, and virologic suppression 6 months post-enrollment, estimated via Kaplan-Meier.
Results:
Of 192 referred patients, 152 were eligible, and 75 enrolled. All 75 were off ART and viremic; 100% had a substance use disorder; and 77% had a mental health diagnosis. Over three-quarters re-started ART within 7 days of enrollment, and 91% returned for follow-up within 90 days. The cumulative incidence of viral suppression at 6 months was 55% (95% CI 43–68%).
Conclusions:
A novel care model for PWH-HUH demonstrates early success in engaging viremic patients in care and improving viral suppression. Low-barrier, high-contact primary care programs offering comprehensive services and incentives may improve outcomes for this vulnerable population.
Keywords: HIV, Homelessness and Unstable Housing, Retention in Care
Introduction
Homelessness and unstable housing (HUH) represent a major barrier to realizing the full benefits of antiretroviral therapy (ART) for people with HIV (PWH),1 threatening targets for Ending the HIV Epidemic initiatives.2 PWH-HUH are significantly less likely to achieve viral suppression than people with stable housing, even among those accessing HIV care.1,3–5 In San Francisco, only 33% of people experiencing homelessness were virally suppressed in 2018,6 compared to 75% of those who were housed, and viral suppression rates decrease with increasing housing instability.4 Furthermore, people homeless at HIV diagnosis have a 27-fold higher odds of death compared to those with housing in San Francisco.7
Affordable housing is ultimately needed to achieve the goals of the Ending the HIV Epidemic Initiative.3 While ongoing efforts are needed to address this key structural barrier, there is an immediate need to address health needs of PWH-HUH at the clinic-level.
PWH-HUH face a number of individual-level and structural barriers to engagement in care.8,9 Multiple interventions have demonstrated some success in mitigating barriers to care for this vulnerable population, including enhanced contact,10 peer navigation,11 case management,12 and specialized provider training to reduce stigma and address substance use and psychiatric co-morbidities.13,14 Still others cite unstable housing as one potential reason for the lack of a significant intervention effect.15 These interventions have had limited impact on viral suppression when enacted in isolation. Multi-component low-barrier care models may be more effective in addressing disparate barriers, although studies to understand implementation and efficacy of such programs are needed.16–18
In January 2019, we launched POP-UP (Positive-health On-site Program for Unstably-housed Populations), a no-appointment low-threshold, multi-component model of care to address barriers to care and improve viral suppression for PWH-HUH with viremia. We describe the POP-UP clinic model and report initial care outcomes.
Methods
Study Setting, Design, and Participants
POP-UP is based at the Ward 86 HIV clinic at San Francisco General Hospital. Ward 86 is funded by the San Francisco Department of Public Health (SFDPH) and the Ryan White Care program and serves 2500 publicly insured or uninsured patients, a third of whom experience homelessness or unstable housing.4 Ward 86 patients are eligible to receive care in POP UP if they meet all of the following criteria: 1) HIV viral load >200 copies/mL or are off ART, 2) HUH, 3) ≥1 missed primary care appointment and ≥2 drop-in visits to Ward 86 over prior 12 months. For this analysis, we included Ward 86 patients who met enrollment criteria and enrolled in POP-UP from January 2019 – February 2020.
POP-UP Recruitment and Enrollment
At POP-UP inception, Ward 86 patients eligible for POP-UP were identified through a combination of SFDPH surveillance data and electronic medical record review. Additionally, Ward 86 providers and a linkage-to-care program at the SFDPH referred patients who met eligibility criteria. Prior research shows that services like those included in POP-UP improve HIV outcomes. We therefore considered withholding POP-UP services from eligible patients as unethical, and randomization was not conducted. After assessing referral eligibility, POP-UP staff contacted the primary care team and the SFDPH HIV linkage-to-care navigator to determine the best way to navigate patients to Ward 86 for POP-UP enrollment once referred.
POP-UP Intervention
POP-UP includes low-threshold primary care services without the need for scheduled appointments; financial incentives; and enhanced outreach with patient navigation and case management.18 The POP-UP clinical team includes three Ward 86 MDs and a nurse practitioner who are HIV specialists; a nurse; a social worker; the clinic pharmacist and pharmacy technician; and a linkage-to-care navigator, all of whom meet for a weekly case conference to conduct panel management.
Low-threshold comprehensive primary care
POP-UP is open for drop-in visits on weekday afternoons to access medical, social, and pharmacy services without an appointment. Medical services include same-day re-start of ART, substance use treatment including buprenorphine, comprehensive primary health services, and onsite laboratory services. A psychiatrist is available for phone consultation by the medical provider. Social services include care coordination, referral to case management, referrals for emergency and permanent housing, and assistance with access to public insurance coverage. Medications can be delivered to the clinic, allowing patients to pick up medications directly from clinic.
Incentivized care
We provide financial incentives in the form of grocery store gift cards: $10 once a week for a visit with a provider or social worker; $10 for lab draws when needed; and $25 every 3 months for achieving or maintaining an HIV viral load <200 copies/mL
Enhanced Outreach
Patient navigators assist with finding and linking patients to care or other services including benefit services, Medicaid enrollment, and medical appointments. Our nurse coordinates with care providers in the community to perform wellness checks and assist with medication adherence. There is a dedicated POP-UP phone that accepts text messages.
Study Measurements
We conducted chart review to obtain demographic information, documentation of a substance use disorder or mental health disorder based on ICD-10 codes and diagnoses listed in clinic notes, housing status, CD4 count, and HIV viral load at the time of POP-UP enrollment. We abstracted subsequent clinic visit data and HIV viral load data from the electronic health record.
Analysis
Our primary outcome was cumulative incidence of viral suppression (HIV RNA < 200 copies/mL) assessed 6 months post-enrollment. Secondary outcomes included the proportion of patients restarting ART within 7 days of POP-UP enrollment, early engagement (proportion returning for a second visit within 1 month and 3 months), and sustained engagement (proportion with a visit during both the first three months and the second three months over the first six months of follow-up). Viral suppression, ART initiation, and early engagement outcomes were assessed using Kaplan-Meier, censoring at date of program unenrollment due to death, moving out of San Francisco, suspension from the program or transfer to another clinic/provider, or the last date of the analysis (February 29, 2020).
Results
From January 2019 to February 2020, 192 patients were referred to POP-UP, of whom 152 met eligibility criteria and 75 were enrolled (Figure 1). Nearly half of those who were eligible were referred from electronic medical record surveillance data (49%). Additional referral sources of enrolled patients included primary care providers (29%); urgent care providers (25%); and Positive Health Access to Services and Treatment (PHAST), a rapid response team at Ward 86 that champions HIV testing and linkage-to-care (5%). Of the 77 who were not enrolled, 67 have not been reached, 8 preferred to stay with their primary care physician, and 2 were later enrolled after the follow-up period described in this analysis.
Figure 1.
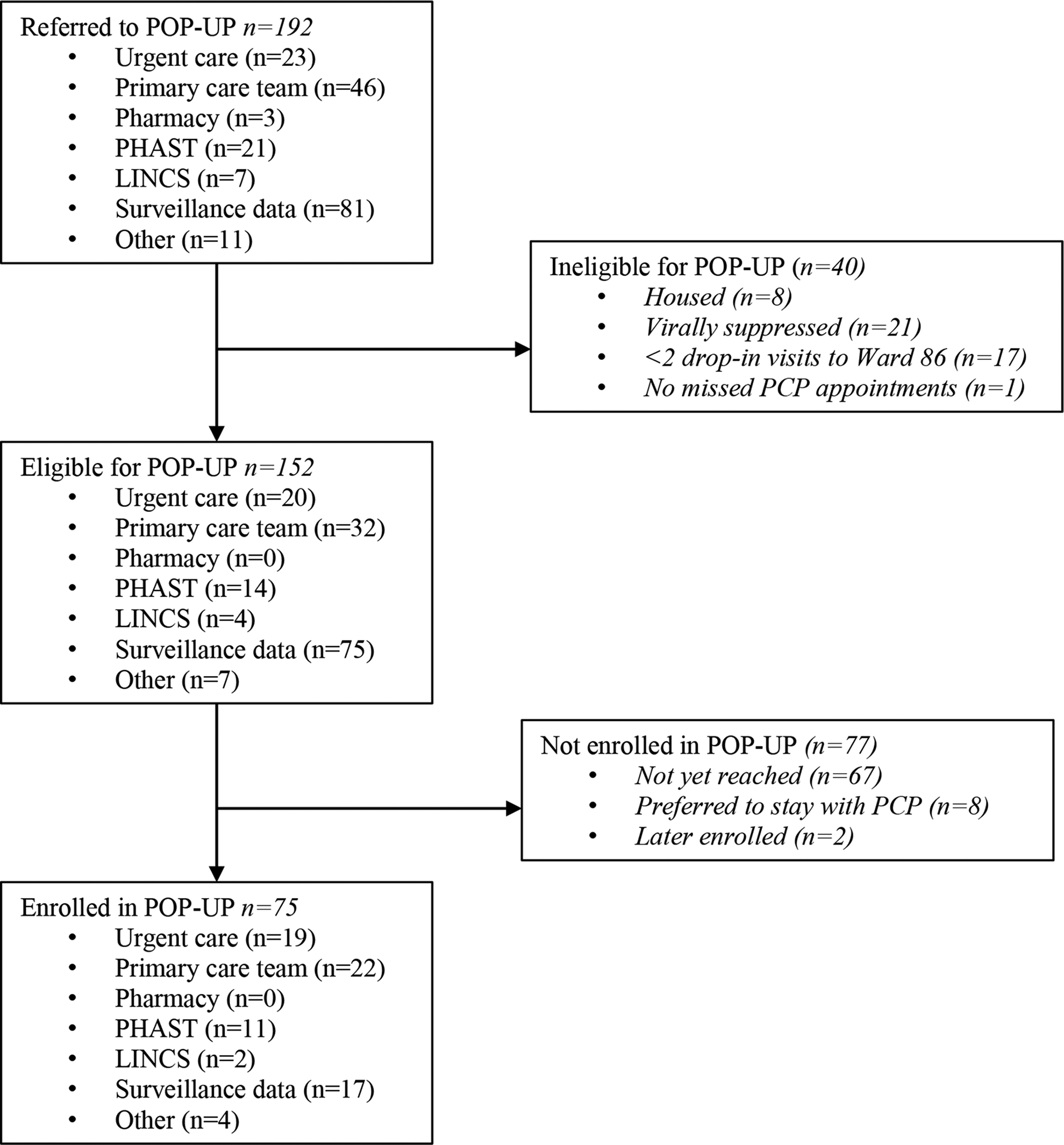
Flowchart of POP-UP clinic referrals, January 2019 to February 2020
Demographics and clinical characteristics
Table 1 summarizes the baseline characteristics of the first 75 patients enrolled in POP-UP. Overall, two-thirds were aged 50 or younger, and 55% were non-white. The majority were cisgender men; 9% cisgender women; and 5% trans-women or gender non-binary. In terms of housing status, 51% were street homeless at enrollment. All enrolled patients had a documented substance use disorder, 91% with methamphetamines and 15% with opiates. Three quarters (77%) had a mental health diagnosis and 51% had a depressive disorder. At baseline, 40% of those enrolled had a CD4 count <200 copies/mL. All patients were either virally unsuppressed at baseline or reported being off ART with no viral load measured; 17 (23%) of patients had at least one HIV viral load <200 copies/mL in the 12 months prior to enrollment, however, none were suppressed at the baseline visit.
Table 1.
Participant Characteristics
| Enrolled (n=75) | ||
|---|---|---|
| n | % | |
| Referral source | ||
| Urgent care | 19 | 25% |
| Primary care team | 22 | 29% |
| PHAST team | 12 | 16% |
| LINCS | 2 | 3% |
| Surveillance data | 19 | 25% |
| Other | 4 | 5% |
| Age | ||
| 18–35 | 21 | 28% |
| 35–50 | 29 | 39% |
| >50 | 25 | 33% |
| Gender | ||
| Cisgender man | 64 | 85% |
| Cisgender woman | 7 | 9% |
| Transgender woman | 1 | 1% |
| Nonbinary/Gender nonconforming | 3 | 4% |
| Race/Ethnicity | ||
| Black/African American | 26 | 35% |
| White | 34 | 45% |
| Hispanic/Latinx | 7 | 9% |
| Asian/Pacific Islander | 0 | 0% |
| American Indian/Native American | 5 | 7% |
| Other | 3 | 4% |
| Housing status at enrollment | ||
| Single room occupancy | 5 | 7% |
| Transitional housing | 9 | 12% |
| Treatment program | 2 | 3% |
| Couch surfing | 11 | 15% |
| Shelter | 10 | 13% |
| Street | 38 | 51% |
| Baseline CD4 count (cells/mm3) | ||
| <200 | 30 | 40% |
| 200–349 | 20 | 27% |
| 350–499 | 16 | 21% |
| ≥500 | 12 | 16% |
| Substance use disorder (any) | 75 | 100% |
| Methamphetamine | 68 | 91% |
| Cocaine | 8 | 11% |
| Opioids | 11 | 15% |
| Alcohol | 7 | 9% |
| Mental health disorder (any) | 58 | 77% |
| Psychotic disorder | 12 | 16% |
| Bipolar disorder | 11 | 15% |
| Depressive disorder | 38 | 51% |
| Anxiety disorder | 14 | 19% |
Outcomes
The cumulative incidence of restarting ART within 7 days of enrollment was 79% (95% confidence interval (CI) 69–87%). The cumulative incidence of returning for a visit (with either a POP-UP provider or a social worker) within 1 month was 68% (95% CI 57–78%) and, within 3 months, was 91% (95% CI 83–96%). Overall, 86% of the 49 patients with at least 6 months of follow up had visits in both the first and second quarters. During the first 6 months following enrollment, the mean financial incentive per month per patient was $15.98 (SD =18.22). Cumulative incidence of viral suppression by 6 months among the entire cohort (n=75) was 55% (95% CI 43–68%). Among the 41 who attained viral suppression, eight subsequently had viral rebound ≥200 copies/mL by six months. Among the eight, five re-suppressed to <200 copies/ml a second time and three remained ≥200 copies/mL at six months. Sixteen patients (21%) were disenrolled from the program (5 died, 3 transferred back to their primary care provider, 3 moved, 3 suspended for violent behavior, 1 went to prison, 1 institutionalized in a long-term care facility).
Discussion
Within an exceptionally vulnerable population of HUH, viremic safety-net clinic patients living with HIV, we demonstrate that over half can achieve viral suppression within the first six months following enrollment in a low-barrier, high-intensity HIV care program. Though interventions have demonstrated some success with similar populations, our intervention is the first clinic-based multi-component care model to specifically focus on PWH-HUH. The Project HOPE study evaluated the effect of incentives and care navigation on viral suppression among PWH on hospital discharge, though only 38% of participants reported any housing instability in the six months prior to enrollment. Among participants in Project HOPE not virally suppressed at baseline, 42% in the incentives-plus-navigation arm achieved viral suppression at 6 months compared to 32% in the usual-treatment arm (RD, 10.2%; 95% CI, 1.4% to 19.1%), a rate of viral suppression lower than that seen in POP-UP. In Project HOPE, participants in the navigation-plus-incentive arm received a median incentive payment of $716 (IQR $495–890) over the 6 month intervention, substantially higher than the mean incentive payment of $16 per month received by patients in POP-UP.11 The Max Clinic in Seattle is a similar low-barrier, high-intensity HIV primary care clinic that provides multi-component interventions such as financial incentives, intensive case management, and enhanced outreach to patients not engaged in traditional primary care, 65% of whom were homeless or unstably housed. Six months after enrollment, 51% of patients in the Max clinic attained viral suppression, similar to the results seen in POP-UP.17
Nearly half of patients eligible for POP-UP could not be reached to offer enrollment, highlighting the challenges of linking this patient population even to low-threshold models of care. Furthermore, participants identified through surveillance data were the least likely to enroll in POP-UP, reflecting the challenges of data-to-care interventions.19 Provider and staff training on eligibility criteria generated a greater proportion of successful referrals to POP-UP, particularly from primary care and urgent care providers at the clinic.
The cumulative incidence of re-starting ART within 7 days was high at 79%, suggesting acceptability and feasibility of rapid re-starts among this population. While same day ART initiation has been associated with very high rates of subsequent viral suppression,20 patients in our study were all ART-experienced, so POP-UP focuses on re-starting ART and addressing known adherence barriers. The high proportion of methamphetamine use (91%) and mental health diagnoses (77%) among those enrolled in POP-UP demonstrate additional challenges to care engagement faced by this patient population, in addition to the structural challenges posed by lack of housing. Despite these individual and structural barriers, we observed early and sustained engagement in the POP-UP program. A primary limitation of our analysis is that it was not controlled, thus limiting our ability to determine whether increases in viral suppression were due to the POP-UP program. We also implemented this intervention at a single site, and the generalizability of our results is uncertain.
POP-UP has features that are similar to other low-barrier primary care models,16,17 though it differs in focusing exclusively on patients who are homeless or unstably housed. Low-barrier, high-intensity primary care programs offering comprehensive services and incentives similar to POP-UP may improve patient outcomes for PWH-HUH in other urban settings. Further research is needed to understand the costs associated with this model of care and how programs such as POP-UP can expand their reach to include patients not currently accessing care. An expansion of similar programs, tailored specifically for high-risk populations, may improve HIV outcomes across geographic locations, which could provide a new cornerstone for strategies to end the HIV epidemic.
Acknowledgments
The “Ward 86” HIV program in the Division of HIV, ID and Global Medicine received an unrestricted investigator-initiated grant from the Gilead Foundation to support implementation and evaluation of the ‘POP-UP’ program, a clinical program for PLWH experiencing HUH (Grant # IN-US-985-5691). Gilead had no role in the interpretation or presentation of these results.
Direct CFAR Funding Support: This research was supported by an Ending the HIV Epidemic Supplemental grant from the National Institutes of Health to the UCSF-Gladstone Center for AIDS Research (P30 AI027763).
Indirect/Partial Funding Support: This publication/presentation/grant proposal was made possible with help from an Ending the HIV Epidemic supplement to the UCSF-Gladstone Center for AIDS Research (CFAR), an NIH-funded program (P30 AI027763).
Footnotes
No Conflicts of Interest to report
REFERENCES
- 1.Doshi RK, Milberg J, Jumento T, Matthews T, Dempsey A, Cheever LW. For Many Served By The Ryan White HIV/AIDS Program, Disparities In Viral Suppression Decreased, 2010–14. Health Aff (Millwood). 2017;36(1):116–123. doi: 10.1377/hlthaff.2016.0655 [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV Epidemic: A Plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- 3.Griffin A, Dempsey A, Cousino W, et al. Addressing disparities in the health of persons with HIV attributable to unstable housing in the United States: The role of the Ryan White HIV/AIDS Program. PLOS Med. 2020;17(3):e1003057. doi: 10.1371/journal.pmed.1003057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clemenzi-Allen A, Geng E, Christopoulos K, et al. Degree of Housing Instability Shows Independent “Dose-Response” With Virologic Suppression Rates Among People Living With Human Immunodeficiency Virus. Open Forum Infect Dis. 2018;5(3):ofy035. doi: 10.1093/ofid/ofy035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riley ED, Vittinghoff E, Koss CA, et al. Housing First: Unsuppressed Viral Load Among Women Living with HIV in San Francisco. AIDS Behav. 2019;23(9):2326–2336. doi: 10.1007/s10461-019-02601-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colfax G, Aragon T, Enanoria W, Scheer S. HIV Epidemiology: Annual Report, 2018.; 2019.
- 7.Spinelli MA, Hessol NA, Schwarcz S, et al. Homelessness at diagnosis is associated with death among people with HIV in a population-based study of a US city. AIDS Lond Engl. 2019;33(11):1789–1794. doi: 10.1097/QAD.0000000000002287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Toole Thomas P, Pirraglia PA, Dosa D, et al. Building Care Systems to Improve Access for High-Risk and Vulnerable Veteran Populations. J Gen Intern Med. 2011;26(2):683. doi: 10.1007/s11606-011-1818-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGuire J, Rosenheck R. The quality of preventive medical care for homeless veterans with mental illness. J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2005;27(6):26–32. [DOI] [PubMed] [Google Scholar]
- 10.Gardner LI, Giordano TP, Marks G, et al. Enhanced personal contact with HIV patients improves retention in primary care: a randomized trial in 6 US HIV clinics. Clin Infect Dis Off Publ Infect Dis Soc Am. 2014;59(5):725–734. doi: 10.1093/cid/ciu357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Metsch LR, Feaster DJ, Gooden L, et al. Effect of Patient Navigation With or Without Financial Incentives on Viral Suppression Among Hospitalized Patients With HIV Infection and Substance Use: A Randomized Clinical Trial. JAMA. 2016;316(2):156–170. doi: 10.1001/jama.2016.8914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kushel MB, Colfax G, Ragland K, Heineman A, Palacio H, Bangsberg DR. Case management is associated with improved antiretroviral adherence and CD4+ cell counts in homeless and marginally housed individuals with HIV infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2006;43(2):234–242. doi: 10.1086/505212 [DOI] [PubMed] [Google Scholar]
- 13.Bhatta DN, Liabsuetrakul T, McNeil EB. Social and behavioral interventions for improving quality of life of HIV infected people receiving antiretroviral therapy: a systematic review and meta-analysis. Health Qual Life Outcomes. 2017;15(1):80. doi: 10.1186/s12955-017-0662-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Risher KA, Kapoor S, Daramola AM, et al. Challenges in the Evaluation of Interventions to Improve Engagement Along the HIV Care Continuum in the United States: A Systematic Review. AIDS Behav. 2017;21(7):2101–2123. doi: 10.1007/s10461-017-1687-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christopoulos KA, Riley ED, Carrico AW, et al. A Randomized Controlled Trial of a Text Messaging Intervention to Promote Virologic Suppression and Retention in Care in an Urban Safety-Net Human Immunodeficiency Virus Clinic: The Connect4Care Trial. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;67(5):751–759. doi: 10.1093/cid/ciy156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dombrowski JC, Ramchandani M, Dhanireddy S, Harrington RD, Moore A, Golden MR. The Max Clinic: Medical Care Designed to Engage the Hardest-to-Reach Persons Living with HIV in Seattle and King County, Washington. AIDS Patient Care STDs. 2018;32(4):149–156. doi: 10.1089/apc.2017.0313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dombrowski JC, Galagan SR, Ramchandani M, et al. HIV Care for Patients With Complex Needs: A Controlled Evaluation of a Walk-In, Incentivized Care Model. Open Forum Infect Dis. 2019;6(7). doi: 10.1093/ofid/ofz294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clemenzi-Allen A, Hickey M, Conte M, et al. Improving Care Outcomes for PLWH Experiencing Homelessness and Unstable Housing: A Synthetic Review of Clinic-Based Strategies. Curr HIVAIDS Rep. 2020;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dombrowski JC, Hughes JP, Buskin SE, et al. A Cluster Randomized Evaluation of a Health Department Data to Care Intervention Designed to Increase Engagement in HIV Care and Antiretroviral Use. Sex Transm Dis. 2018;45(6):361–367. doi: 10.1097/OLQ.0000000000000760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coffey Susa, Bacchetti Peter, Sachdev Darpun, et al. RAPID antiretroviral therapy. AIDS. 2019;33(5): 825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]


