Abstract
Artificial intelligence (AI) holds promise for cardiovascular medicine but is limited by a lack of large, heterogeneous and granular data sets. Blockchain provides secure interoperability between siloed stakeholders and centralized data sources. We discuss integration of blockchain with AI for data-centric analysis and information flow, its current limitations and potential cardiovascular applications.
AI in cardiovascular medicine
Artificial intelligence (AI) is a rapidly advancing computational discipline that can classify complex data to make accurate predictions. AI has had notable successes in voice, facial and image recognition, in game-playing, in various industrial and scientific fields, and is now being applied to health care1. In cardiovascular medicine, AI can assess cardiac function from imaging2, infer cardiac rhythm and function from the electrocardiogram (ECG)3 and make some clinical decisions as well as experts2. However, a currently unrealized promise of AI is to power personalized cardiovascular solutions by defining novel phenotypes beyond traditional disease syndromes, improving outcome predictions and individualizing therapy. Although AI seems poised to realize this vision of precision medicine, particularly with the rise of wearable sensors and omic technologies, progress has been mixed2. A major bottleneck is the paucity of large, secure, heterogeneous and granular data sets, with accurate follow-up in broad, at-risk populations. This limitation is an increasingly recognized obstacle for AI in cardiovascular medicine4.
Blockchain in cardiovascular medicine
Blockchain is a rapidly evolving technology that provides secure, traceable and scalable data exchange, which might address the needs of ‘data-hungry’ AI and enable several innovations in medical data transactions. Blockchain was introduced in 2008 by an unknown individual or entity called Satoshi Nakamoto, as an open, shared digital ledger, which has laid the foundations for cryptocurrencies such as Bitcoin and distributed computing platforms such as Ethereum. Blockchain forces peer-to-peer transactions to be transparent and immutable, enabling a decentralized system that eliminates intermediaries such as a central bank in the case of Bitcoin or a central server in the case of Ethereum, reduces transaction fees and minimizes vulnerability to security breaches.
FIGURE 1 shows a hypothetical health-care blockchain, which mobilizes data that are currently collected and stored in separate health-care and industry silos, are utilized by separate stakeholders and are often difficult to access by the original data owner (the patient). Blockchain is a data-centric model that tracks ownership as data are transacted between stakeholders. Nodes of the blockchain network verify data transfer between stakeholders by consensus, to create a cryptographic fingerprint (‘hash’) of data transactions. Each transaction is public within the blockchain, but the identities of each stakeholder and piece of transacted data are hidden. Because access to each data element is authorized by its owner, patients in a blockchain-based electronic medical record are empowered to select the providers, technology companies or researchers who can access their data5. Of note, stakeholders do not have to be on the same information technology platform. This blockchain model can be considered a smart contract — that is, a software protocol for verifying success and enforcing irrevocable legal agreements between two or more parties.
Fig. 1 |. Integration of AI with blockchain moves patients towards the centre of the health-care process,
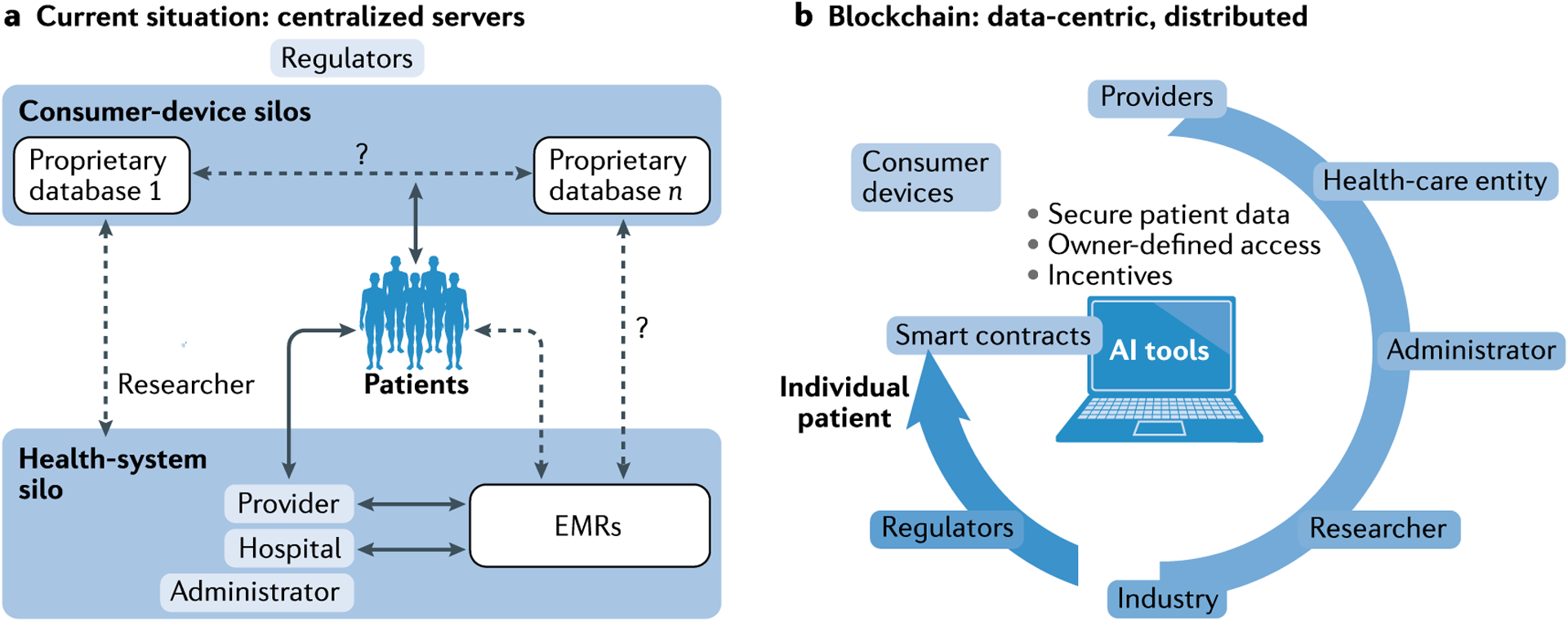
a | In the current model, patient data are maintained on centralized servers, which might be both difficult to access and incompatible between health-system silos and other stakeholders. Consumer devices have separate proprietary servers, b | In the blockchain model, smart contracts start as patient-owned data elements, which are the centrepiece for secure and transparent information flow. The data owner (typically a patient) can selectively turn access to individual data elements on or off for various stakeholders. Artificial intelligence (AI) tools can interact with smart contracts, and AI tools can also be blockchain-enabled. These analytical tools, databases or clinical trials do not reside in any particular silo but are distributed. Incentives can flow on the basis of data ownership, the importance of the data to each process, or by value added by a provider, health-care entity or consumer firm. Regulatory oversight will have to adapt between models. EMR, electronic medical record.
Blockchain opens up a major conceptual advance via ‘incentives’ that flow to the owner of each data element on the basis of its value6. This arrangement could form the basis for a health cryptocurrency, with far-reaching implications. Incentives could reward the owner of original data (for example, genetic, blood or ECG) but also providers whose efforts lead to a diagnosis or improve outcomes. Similarly, incentives could be routed to administrators who improve patient outcomes or resource utilization. For research, incentives could be routed to owners of data that help in research or who curate a useful database, or to developers of successful analysis algorithms.
Integration of blockchain with AI
Blockchain can accelerate the development of data-hungry AI applications. For instance, convolutional neural networks were recently trained using ECGs from one specific wearable monitor in 53,549 patients and provided cardiologist-level diagnostic accuracy for arrhythmias3. Nevertheless, some arrhythmias were under-represented in that data source, and results might differ if other data sets were used. A blockchain-enabled data marketplace could facilitate secure integration of data from other vendors or health-care platforms to increase instances of those arrhythmias in the data set, to improve training. Accordingly, several potential strategies are being used to integrate blockchain with AI.
Blockchain forms a natural foundation to standardize health-data structures for AI training, clinical trials and regulatory purposes. An emerging challenge is to merge data from diverse cardiovascular sources, such as portable ECG monitors, other wearable devices, existing hospital-based electronic medical records, biobanks, and non-medical data such as activity logs, social media or e-mail threads. Blockchain provides a scalable solution to this problem.
Blockchain provides the capacity to trace independent block (record) types and dissect granular data. Therefore, the geographical variations in the results from the TOPCAT trial7 could have been readily tracked if the data had been collected using blockchain. Partitioning data in this way is of critical and growing importance for AI applications and precision health, particularly given known variations in drug metabolism or disease propensity between geographical regions, genetic groups or other population differences.
The health cryptocurrency model suggested above might incentivize contributions of rare data, which are often poorly represented in single-centre studies or even large registries. Examples include under-represented racial subgroups, geographical regions or uncommon conditions. Blockchain-based AI could thereby accelerate the definition of phenotype-specific outcomes of orphan diseases, improve the representation of racial minorities and reduce sex-specific inequality.
Current applications
Several applications are emerging that integrate blockchain with AI. The AHA has partnered with the Open Health Network to develop AI and blockchain products such as PatientSphere, a blockchain-based, Health Insurance Portability and Accountability Act (HIPAA)-compliant, data-sharing platform that uses AI to deliver treatment plans and exercise tips8. Overall, start-up enterprises are working in three main areas. First, to use blockchain to store data for the development of an AI model that predicts events such as acute myocardial infarction by analysing demographics, cardiac imaging and other inputs9. Second, to decentralize AI algorithms and data. For instance, a partnership between the MedStar Health Research Institute and ObEN monitors patients with heart failure and provides incentives to patients who engage in health-giving behaviours. Third, to use blockchain as the backbone for an AI-linked network of sensors to predict cardiovascular disease, such as initiatives by Farasha Labs or the Health2Sync diabetes data trust.
Challenges to widespread use
Challenges exist to integrating blockchain and AI. Primarily, blockchain applications in health care must be secure. Given that no system is completely secure, enthusiasm to place sensitive data into an immutable blockchain might be limited5. Ethical issues might also be a concern for AI-blockchain integration. Although the identity of stakeholders is private, public accessibility of medical data in a blockchain ledger might not always be desirable. In general, medical data should not be publicly available but perhaps only the list of encrypted transactions or blocks containing access permissions to the data; medical data would thereby remain on distributed servers. Blockchain might also be vulnerable to a so-called 51% attack, a scenario in which a malicious user obtains majority control. This situation has been seen in the Bitcoin network, in which four mining pools contribute most computational power. Although health-care organizations would not be seen as malicious, they might inevitably contribute >51% of hashes. Finally, consensus and professional society guidelines and regulators will have to consider a very wide range of issues on data security, scalability, data integrity, ethics and computational resources10.
Conclusions
The integration of blockchain with AI is a natural marriage that could advance the aim of personalized cardiovascular medicine by greatly increasing the availability of data for AI development and training, sharing proprietary AI algorithms for generalization, decentralizing databases of different vendors or health systems, and incentivizing solutions that improve outcomes over others that do not. However, such applications are still in their infancy, and some concerns about their implementation exist. Further research is needed in areas related to trust at the technical level, whether competing organizations would in practice desire this flow of data, reimbursement and ethical considerations.
Acknowledgements
The NIH has awarded grant funding to A.J.R. (F32HL144101) and S.M.N. (HL83359 and HL103800).
Footnotes
Competing interests
S.M.N. has consulted for Abbott Laboratories and beyond.ai and declares Intellectual Property Rights from University of California Regents and Stanford University. The other authors declare no competing interests.
RELATED LINKS
Bitcoin: https://bitcoin.org/en/
Ethereum: https://www.ethereum.org/
Farasha Labs: https://www.f6s.com/farashalabs
Health2Sync: https://www.health2sync.com/
MedStar Health Research Institute: https://www.medstarhealth.org/mhri/
ObEN: https://oben.me/
Open Health Network: https://www.openhealth.cc/
References
- 1.Topol EJ High-performance medicine: the convergence of human and artificial intelligence. Nat. Med 25, 44–56 (2019). [DOI] [PubMed] [Google Scholar]
- 2.Krittanawong C et al. Deep learning for cardiovascular medicine: a practical primer. Eur. Heart J 40, 2058–2073 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Minchole A & Rodriguez B Artificial intelligence for the electrocardiogram. Nat. Med 25, 22–23 (2019). [DOI] [PubMed] [Google Scholar]
- 4.Loring Z, Mehrotra S & Piccini JP Machine learning in ‘big data’: handle with care. Europace 21,1284–1285 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giordanengoa A Possible usages of smart contracts (blockchain) in healthcare and why no one is using them. Stud. Health Technol. Inform 264, 596–600 (2019). [DOI] [PubMed] [Google Scholar]
- 6.Mamoshina P et al. Converging blockchain and next-generation artificial intelligence technologies to decentralize and accelerate biomedical research and healthcare. Oncotarget 9, 5665–5690 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Denus S et al. Spironolactone metabolites in TOPCAT — new insights into regional variation. N. Engl. J. Med 376, 1690–1692 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiggers K PatientSphere uses AI and blockchain to personalize treatment plans. VentureBeat https://venturebeat.com/2018/10/25/patientsphere-uses-ai-and-blockchain-to-personalize-treatment-plans/ (2018). [Google Scholar]
- 9.Popov G The future of artifical intelligence in healthcare! SkyChain https://skychain.global/upload/iblock/89a/wp_english_Newest.pdf (2019). [Google Scholar]
- 10.O’Donoghue O et al. Design choices and trade-offs in health care blockchain implementations: systematic review. J. Med. Internet Res 21, el 2426 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]


