Abstract
Purpose:
Maternal adverse childhood experiences (ACEs) and intimate partner violence (IPV) are temporally distinct risk factors that negatively impact mothers and their offspring. Risk associated with ACEs and IPV begin during pregnancy, a period of increased physical and psychological demands. The current study examined a person-centered method to empirically identify profiles of pregnant women based on type and severity of ACEs and past-year IPV. Profiles were then differentiated on psychosocial functioning indicators.
Methods:
A primarily Latinx, low socioeconomic sample of women (n = 225) completed measures assessing ACEs and past-year IPV, perceived and experienced stress, emotion regulation, and trauma-related symptoms during their third trimester. Latent profile analysis (LPA) was used to identify unique profiles of women based on seven dimensional indicators reflecting threat- and deprivation-based ACEs and IPV.
Results:
A 4-class solution best fit the data: (1) low probability of ACEs or IPV (64.9%), (2) childhood neglect-only (20.4%), (3) childhood abuse/neglect (10.2%), and (4) polytrauma characterized by a combination of childhood abuse, neglect, and IPV (4.4%). Women with the “childhood abuse/neglect” or “polytrauma” profiles reported more stress and symptoms than women with the “low exposure” profile. Women in the “childhood neglect-only” profile were generally similar to women in the “low exposure” profile, but did report greater difficulties in emotion regulation.
Conclusions:
These results suggest that childhood abuse and IPV, exposure types involving threat, are potent correlates of stress, emotion regulation, and mental health difficulties during pregnancy. However, exposure characterized by deprivation alone generally did not increase difficulties.
Keywords: Adverse childhood experiences, intimate partner violence, pregnancy, emotion regulation, posttraumatic stress, depression, anxiety
Introduction
Pregnancy is often accompanied by increasing demands that include changes in relationships, health-related concerns, preparation for parenthood, and financial stress (Yali & Lobel, 2002). Not surprisingly, pregnancy can be a period that exacerbates or marks the onset of mental health impairment. This is compounded by suboptimal access to mental health care for pregnant women, especially in disadvantaged populations (Farr, Bitsko, Hayes, & Dietz, 2010; Glover, 2014). Failure to navigate greater psychosocial and mental health challenges can lead to adverse pregnancy, birth, and developmental outcomes (Dunkel Schetter & Tanner, 2012; Mulder et al., 2002). Therefore, adapting to this heightened period of stress and increased demands necessitates greater access to and utilization of personal resources (e.g., ability to cope with and regulate stress reactions) and social capital (e.g., instrumental and emotional support; Collins, Dunkel-Schetter, Lobel, & Scrimshaw, 1993; Elsenbruch et al., 2007; O’Hara, 1986)
Pregnant women with a history of adverse childhood experiences (ACEs) and/or intimate partner violence (IPV) may be especially vulernable. Among pregnant women, nearly a third have a history of childhood abuse or neglect, about 25% have a lifetime history of IPV, and 4–8% are victimized by a partner during pregnancy (Campbell, 2002; Hussey, Chang, & Kotch, 2006; Silverman, Decker, Reed, & Raj, 2006). Although temporally distinct, ACEs and IPV are inextricably linked as women with a history of ACEs are more likely to become victims of IPV (Bensley, Van Eenwyk, & Wynkoop Simmons, 2003; Coid et al., 2001; Gartland, Giallo, Woolhouse, Mensah, & Brown, 2019; Smith Slep & O’Leary, 2001; Whitfield, Anda, Dube, & Felitti, 2003).
ACEs and IPV predict poorer outcomes in pregnancy, birth, and continue to impact into their offspring’s childhood (Atzl, Narayan, Rivera, & Lieberman, 2019; Campbell, 2002; Jasinski, 2004; Olsen, 2018; Wadsworth, Degesie, Kothari, & Moe, 2018). A history of childhood abuse is associated with increased stressful life events (Benedict, Paine, Paine, Brandt, & Stallings, 1999), depression (Benedict et al., 1999; Chung, Mathew, Elo, Coyne, & Culhane, 2008; Leeners, Rath, Block, Görres, & Tschudin, 2014), post-traumatic stress symptoms (Lev-Wiesel, Daphna-Tekoah, & Hallak, 2009), and suicidal ideation during pregnancy (Leeners et al., 2014). Similarly, pregnant women exposed to IPV are more likely to experence anxiety (Sarkar, 2008; Wadsworth et al., 2018), depression (Kendall-Tackett, 2007; Sarkar, 2008), problems with tobacco, alcohol, or drug use (Jasinski, 2004; Sarkar, 2008), and suicidal ideation (Wadsworth et al., 2018). Women with IPV often experience financial hardships, housing, and employment instabilit; they may not have control over family finances or subsist on a single income (Adams, Tolman, Bybee, Sullivan, & Kennedy, 2012; Gilroy, McFarlane, Maddoux, & Sullivan, 2016). Consequently, financial costs associated with pregnancy may place even greater strain on women experiencing IPV. Moreover, these women may be reluctant or unable to obtain social support due to concerns about partner retaliation or stigma associated with being a victim of IPV (Coker et al., 2002).
While both ACEs and IPV are well-established risk factors, less work has focused on unpacking their independent and combined effects on outcomes during pregnancy (Rich-Edwards et al., 2011; Seng, Sperlich, & Low, 2008). Some evidence suggests synergistic/cumulative effects of ACEs and IPV on outcomes (Fogarty, Fredman, Heeren, & Liebschutz, 2008; Nelson, Uscher-Pines, Staples, & Ann Grisso, 2010). However, ACES and IPV are heterogenous risk factors. For instance, ACEs can be distinguished by whether they are characterized by deprivation or threat; emerging studies demonstrate that these distinct, yet often co-occurring dimensions are differentially associated with outcomes (McLaughlin, Sheridan, & Lambert, 2014; Sheridan & McLaughlin, 2014). Threat-based experiences and events are characterized by potential or actual danger to one’s physical integrity and are similar to events that are often described as being traumatic in nature, whereas deprivation-based experiences are better characterized as an absence of needed cognitive and social environmental inputs. Growing evidence indicates that exposure to threats in childhood predicts increased risk of psychopathology and impairments in emotion regulation, whereas deprivation-related experiences are more generally associated with cognitive, academic or socioeconomic outcomes (McLaughlin, 2016).
Additionally, IPV and ACEs may manifest as psychological (e.g., harsh verbal/coercive control IPV or verbal/emotional childhood abuse) or physical in nature. Isolating profiles of risk associated with these distinct experiences and characteristics may help to identify targets for prevention and intervention. For instance, adult IPV is generally threatening in nature. Therefore, IPV and threat-related ACEs may have similar psychosocial and mental health correlates. Gaining insight into how different patterns and characteristics of exposure to ACEs and IPV impact maternal functioning during pregnancy may have implications for how best to support these women.
One approach for exploring the various permutations of ACEs and IPV is by way of person-centered analytic methods. Unlike variable-centered methods (e.g., factor analysis) that isolate the variance of indicators on specific outcomes, person-centered methods, such as latent profile analysis, establish probabilistically determined subgroups of individuals based on a set of indicators, which may be differentially associated with outcomes. Thus, unlike variable-centered approaches in which variables are the units of analysis and the inter-relationships among variables within a sample are assumed to hold steady, person-centered methods use the individual as the unit of analysis and thus are capable of detecting interindividual differences (Bergman, Magnusson, & El Khouri, 2003; McCutcheon, 1987). This may be especially useful for clarifying the independent or cumulative effects of ACEs and IPV, either of which may be characterized by deprivation or threat and psychological or physical features. Indeed, person-centered models have shown utility for determing whether outcomes differ across patterns of exposure (Cavanaugh et al., 2012); however, this approach has not been used to examine patterns of ACEs, IPV, and characteristics of these experiences in a sample of pregnant women. Person-centered approaches can be especially useful for synthesizing information across multiple risk factors that may lead to improved clinical decision making about targeted interventions.
Therefore, the current study: (1) uses a person-centered approach to empirically classify pregnant women into risk profiles based on indicators of different types and severities of ACEs and past-year IPV; and (2) examines differential associations between risk profiles and a) demographic characteristics, b) stress-related mental health symptoms during pregnancy, c) perceived general and pregnancy-specific stress, d) perceived social support, and e) financial hardship. Financial hardship was examined given that pregnancy increases financial demands and women exposed to IPV may face greater finacial difficulties (Adams et al., 2012; Gilroy et al., 2016). Our sample was drawn from an urban, lower income, and mainly Hispanic/Latinx sample – characteristics that may also increase risk for IPV during pregnancy (Charles & Perreira, 2007; Silverman et al., 2006).
Materials and Methods
Participants and Procedures
The data used in this secondary analysis are from a larger study examining prenatal stress and epigenetic effects on the stress response system in newborns (Grasso, Ford, & Greene, 2019). The study was approved by the institutional review boards of the University of Connecticut School of Medicine, Connecticut Children’s Medical Center, and Hartford Hospital. Pregnant women in their third trimester were invited to participate in the study when attending prenatal care visits at an urban clinic. Women were considered eligible if they were English speaking, having a singleton pregnancy, and planned to deliver at Hartford Hospital. Participants provided informed consent. Among the full sample of 239 women, 14 did not provide information on childhood abuse and neglect and/or IPV, giving a final sample of 225. Participants missing data did not differ from the final sample on age, race/ethnicity, or any other major study variable.
Of those with complete data on adversity measures, the majority of the sample identified as Latinx and did not identify a racial group (n = 115; 51.1%) followed by those who identified as Latinx and Caucasian (n = 51; 22.7%), Black (n = 31; 13.8%), Caucasian and not Latinx (n = 13; 5.8%), Black and Latinx (n = 11; 4.9%), and other (n = 4; 1.8%). The sample ranged in age from 18 to 43 years (M = 26.98, SD = 5.38). The majority of the sample (90.4%) reported less than $20,000 annual income or were Medicaid recipients (this variable was not used to compare classes given its low variability). Most of the sample had at least a high school degree (n = 167; 74.2%). More specifically, 57 (25.4%) of the sample had less than a high school degree, 80 (35.6%) had a high school degree or GED, 11 (4.9%) had trade/vocational degrees, 50 (22.2%) had attended some college, 13 (5.8%) had a 2 year degree, 9 (4.0%) had a 4 year degree, 4 (1.8%) had a graduate degree, and 1 (0.4%) did not report educational information. Approximately half of the sample was single and not in a committed relationship at the time of the assessment (56.9%).
Measures
The Revised Conflict Tactics Scales (CTS2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996) is a self-report measure that assesses 39 behaviors pertaining to psychological and physical conflict between couples from partner to respondent and respondent to partner. Participants were asked to rate the frequency of behaviors within the past year using a 7-point scale. An additional option was included if the event or behavior occurred prior to the past year. For this study we calculated CTS chronicity scores by converting responses as indicated by the measure developers: i.e., Never = 0, Once = 1, Twice = 2, 3–5 times = 4, 6–10 times = 8, 11–20 times = 15, More than 20 times = 25. Extreme scores on the physical scale were capped at 20 (e.g., scores above 20 were recoded to 20) and the psychological scale was capped at 70. The CTS also includes a sexual coercion scale, but it was not used in the current analysis because of low endorsement rates.
The Childhood Trauma Questionnaire Short Form (CTQ-SF; Bernstein et al., 2003) is a 28-item retrospective self-report measure of childhood abuse and neglect. Items are rated on a 5-point scale with options ranging from 1 (“Never True”) to 5 (“Very Often True”). For this study, we used all 5 subscales including, emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect (Internal consistencies: .89, .82, .94, .87, .74, respectively). Previous reports found similar reliability ranging from 0.79 to 0.94 (Bernstein et al., 2003).
The Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) is a 10-item self-report measure of how much stress a person has experienced, their responsiveness, and their appraisal of stress occurring within the past month. Items are rated on a 5-point scale with options ranging from 0 (“Never”) to 4 (“Very often”). Internal consistency was .79 in our sample, similar to reliabilities in the mid .80s observed in other studies (Cohen et al., 1983).
The Prenatal Distress Questionnaire (PDQ; Yali & Lobel, 1999) is a 12-item self-report measure of various medical, psychological, social, and pregnancy related concerns with convergent validity with other measures of stress, anxiety, and depression (Alderdice, Lynn, & Lobel, 2012). Items are rated on a 5-point scale indicating the degree of concern with response option from 0 (“Not at all”) to 4 (“Extremely”). Internal consistency was .80. Previous reports have also found internal reliability of .80 (Alderdice et al., 2012).
The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, 1988) is a 12-item self-report measure of ones perception of support from friends, family, and partner with 4 items about each source of support. Items are rated on 7-point scale with options ranging from 1 (“Very Strongly Disagree) to 7 (“Very strongly agree”). Internal consistency was .95. Previous studies have found reliabilities of approximately .88 (Zimet et al., 1988).
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report measure of one’s capacity and behaviors related to emotion regulation across six dimensions: Non-acceptance, Goals, Impulse, Strategy, Clarity, and Awareness. Items are rated on a 5-point scale gauging the frequency of emotion regulation related behaviors or experiences with response options ranging from 0 (“Almost never”) to 4 (Almost always”). The DERS total score, calculated by summing the subscale scores, was used in the current study. Internal consistency in our study was .87, previous studies have found .93 (Gratz & Roemer, 2004).
The Depression Anxiety and Stress Scale (DASS-42; Lovibond & Lovibond, 1995) is a 42-item self-report measure assessing negative emotional symptoms experienced within the past week with separate scales for depressive, anxiety, and stress-reactivity, each consisting of 14 items. Items are rated on a 4-point scale ranging from 1 (“Did not apply to me at all”) to 4 (“Applied to me very much, or most of the time”). For these analyses we used the depression and anxiety scales only. Internal consistencies in the current sample were .96 and .91 for depression and anxiety, respectively. Previous reports found reliability of .91 and .81 for depression and anxiety, respectively (Lovibond & Lovibond, 1995).
The Structured Trauma-Related Experiences and Symptoms Screener for Adults (STRESS-A; Grasso et al., 2019) is a self-report measure of childhood and adult trauma-related impairment and PTSD symptoms with a structure that corresponds to the DSM-5 4-factor model of PTSD. Participants first complete an inventory of DSM-5 Criterion A events, such as car accidents, natural disasters, or physical violence that occurred in childhood or adulthood. This is then followed by a section on PSTD symptoms and functional impairment. In this study, we calculated total symptom scores as the aggregate of the four symptom subscale scores. Internal consistency of total symptom scores was .96.
The Home Hardship Scale (Sullivan, Turner, & Danziger, 2008) is a 16-item self-report measure of experiences related to a person (and their families) difficult living and financial circumstances occurring over the past year. Items are rated using dichotomous Yes/No options to indicate whether a given hardship occurred (e.g., inability to afford medical or household expenses). Internal consistency was .80.
Data Analytic Plan
Latent profile analysis (LPA) was conducted in Mplus Version 8 (Muthén & Muthén, 2017) using maximum likelihood estimation with robust standard errors to identify classes from 5 CTQ and 2 CTS continuous scale scores. Specifically, the LPA included the CTQ physical abuse, emotional abuse, sexual abuse, physical neglect, and emotional neglect scales and the CTS physical chronicity and psychological chronicity scales. We examined classes incrementally starting with a single class solution and continuing to add classes until a solution no longer converged. To determine the optimal solution we compared fit indices and the Lo-Mendell-Rubin test (Lo, Mendell, & Rubin, 2001). The Lo-Mendell-Rubin test is useful for comparing models as a non-significant value suggests that adding one additional class doesn’t statistically improve model fit. We also considered entropy values with scores closer to 1 representing better separation between classes. While Mplus can handle missing data, we restricted analyses to include participants with complete data on the CTS and CTQ.
We used Mplus BCH and DCAT options, the recommended methods for examining continuous and categorical distal outcome variables, respectively (Asparouhov & Muthén, 2018). When comparing between classes, Mplus provides an omnibus test using the chi-square and then individual pairwise chi-squares. This approach is conceptually similar to using an ANOVA in which each participant is assigned to a single “group” based on the profile that best characterizes their ACE and IPV exposure. Missing data on distal outcomes was rare (comparison with the smallest n included 96% of participants).
Results
Latent Profile Model Description and Fit
Descriptive statistics and correlations among the CTQ and CTS scales used to create the latent profiles are provided in Supplemental Table 1. Detailed fit statistics comparing 2-, 3- and 4-class solutions are provided in Supplemental Table 2. Fit statistics supported a 4-class solution as indicated by a significant Lo-Mendell-Rubin test (p <.01; favoring 4- vs. 3-classes), the smallest BIC, and a negligible change in entropy (0.99 vs 0.97 for 3- and 4-classes, respectively).
To examine the characteristics of each of the four classes, their mean scores on each of the 5 CTQ and 2 CTS scales are provided in Figure 1. The 4-class solution suggests a polytrauma class composed of childhood abuse/neglect and IPV (n = 10; 4.4%), a childhood abuse/neglect class (n = 23; 10.2%), a childhood neglect-only class (n = 46; 20.4%), and lastly, a class with low exposure to IPV and childhood abuse (n = 146; 64.9%). The polytrauma class was characterized by more severe scores on the CTS physical and psychological abuse chronicity scales and modestly elevated scores on the CTQ childhood abuse and neglect scales. Women classified in the childhood abuse/neglect class tended to have high scores on all CTQ childhood abuse and neglect scales, but relatively low chronicity scores on past-year IPV on the CTS. Women classified in the childhood neglect-only class had elevated scores on the CTQ emotional and physical neglect scales, but relatively low scores on the CTQ abuse scales and the CTS IPV scales. Finally, the fourth class had generally low scores on CTQ and CTS compared to the rest of the sample.
Figure 1.
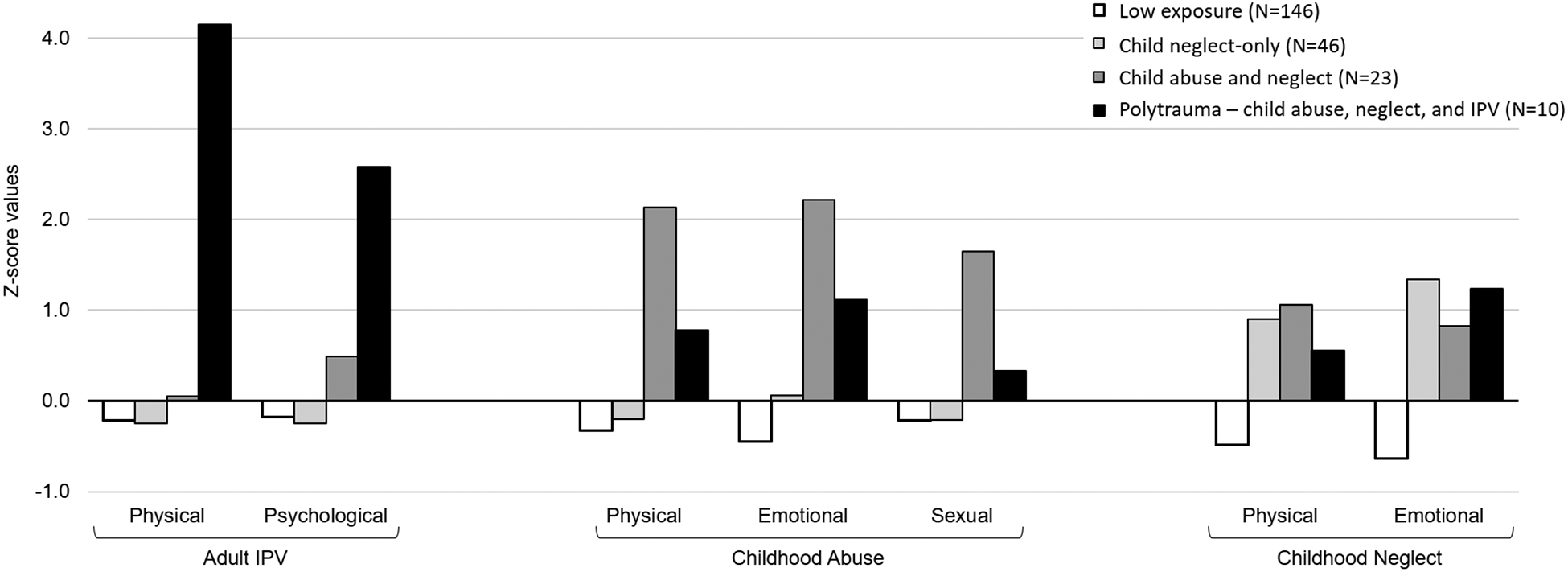
Childhood Trauma and Intimate Partner Violence Classes in Pregnant Women.
The ACEs and IPV indicators are given as the average standardized Z-scores for each of the LPA profiles.
Comparison of Classes
Results comparing the profiles on outcome variables are reported in Tables 1 and 2. The means and standard errors for the outcomes along with the omnibus chi-square are provided in Table 1. Table 2 contains the effect size differences of pairwise comparisons between profiles.
Table 1.
Class differences on demographics, psychological functioning, and pregnancy outcomes
| Outcome variable | Class 1 Low exposure (n=146) |
Class 2 Child neglect-only (n =46) |
Class 3 Child abuse/neglect (n =23) |
Class 4 Polytrauma abuse, neglect and IPV (n =10) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | M or % | SE | M or % | SE | M or % | SE | M or % | SE | χ2 | |
| Demographics | ||||||||||
| Age | 225 | 26.89 | 0.47 | 26.77 | 0.72 | 27.66 | 1.01 | 27.80 | 1.90 | 0.77 |
| Latinx | 225 | 75.4% | 0.04 | 84.6% | 0.05 | 91.3% | 0.06 | 70.0% | 0.15 | 6.48 |
| Couple status | 223 | 44.0% | 0.04 | 38.7% | 0.08 | 52.1% | 0.11 | 20.0% | 0.13 | 4.31 |
| Education | 224 | 79.8% | 0.03 | 50.0% | 0.16 | 67.9% | 0.07 | 65.3% | 0.10 | 6.32 |
| Household Hardship | 225 | 3.10 | 0.22 | 3.80 | 0.51 | 6.67 | 0.68 | 6.60 | 1.20 | 32.02*** |
| Stress and Social Support | ||||||||||
| MSPSS | 224 | 69.82 | 1.36 | 50.70 | 2.90 | 55.75 | 2.86 | 43.80 | 3.65 | 75.91*** |
| PSS | 225 | 18.35 | 0.54 | 13.75 | 1.39 | 22.64 | 1.15 | 21.60 | 1.15 | 31.16*** |
| Stressful Life Events | 225 | 2.67 | 0.20 | 3.05 | 0.41 | 5.10 | 0.89 | 6.50 | 1.51 | 13.26** |
| PDQ | 225 | 8.51 | 0.50 | 9.76 | 1.18 | 11.32 | 1.36 | 11.40 | 1.44 | 6.86† |
| Symptoms and Emotion Dysregulation | ||||||||||
| DERS | 225 | 63.89 | 1.33 | 77.51 | 2.32 | 83.06 | 5.43 | 98.20 | 9.63 | 43.12*** |
| DASS Depression | 225 | 3.09 | 0.52 | 3.95 | 0.66 | 10.83 | 2.45 | 19.60 | 3.87 | 26.81*** |
| DASS Anxiety | 225 | 3.44 | 0.43 | 3.46 | 0.51 | 10.44 | 2.21 | 15.60 | 3.05 | 25.12*** |
| STRESS PTSD | 225 | 17.69 | 1.49 | 16.24 | 2.34 | 26.38 | 3.39 | 33.50 | 5.27 | 14.51** |
| Alcohol in pregnancy | 217 | 0.25 | 0.04 | 0.17 | 0.06 | 0.48 | 0.10 | 0.10 | 0.10 | 8.96* |
Note. Latinx was coded such that 1 indicates Latinx status and 0 indicates non-Latinx. Couple status was coded such that a 1 indicates being married or in a committed relationship and a 0 indicates being single, divorced, or widowed. Education was coded such that a 1 meant high school graduate or more education and 0 indicates less than a high school education.
p < .10,
p < .05,
p < .01,
p < .001
Table 2.
Pairwise comparisons and effect size differences between classes
| Outcome variable | Low vs. Neglect 1 vs. 2 |
Low vs. ChAb/Neg 1 vs. 3 |
Low vs. Polytrauma 1 vs. 4 |
Neg vs. ChAb/Neg 2 vs. 3 |
Neg vs. Polytrauma 2 vs. 4 |
ChAb/Neg vs. Polytrauma 3 vs. 4 |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age | 0.02 | 0.14 | 0.16 | 0.18 | 0.20 | 0.03 |
| Latinx | 0.22 | 0.35* | 0.10 | 0.19 | 0.41 | 0.60 |
| Couple status | 0.11 | 0.17 | 0.50 | 0.25 | 0.36 | 0.65 |
| Education | 0.48† | 0.33 | 0.40 | 0.20 | 0.15 | 0.08 |
| Household Hardship | 0.24 | 1.30** | 1.28** | 0.85** | 0.80* | 0.02 |
| Stress and Social Support | ||||||
| MSPSS | 1.11*** | 0.87*** | 1.61*** | 0.28 | 0.37 | 0.93** |
| PSS | 0.63** | 0.67*** | 0.51** | 1.06*** | 0.90*** | 0.21 |
| Stressful Life Events | 0.15 | 0.89** | 1.47* | 0.61 | 1.08 | 0.32 |
| PDQ | 0.19 | 0.46† | 0.48† | 0.21 | 0.22 | 0.01 |
| Symptoms and Emotion Dysregulation | ||||||
| DERS | 0.85*** | 1.08*** | 1.99*** | 0.28 | 1.09* | 0.55 |
| DASS Depression | 0.15 | 1.07** | 2.44*** | 0.90** | 2.42*** | 0.74† |
| DASS Anxiety | 0.00 | 1.13** | 2.19*** | 1.04** | 2.41*** | 0.50 |
| STRESS PTSD | 0.08 | 0.49* | 0.88** | 0.63* | 1.08* | 0.43 |
| Alcohol in pregnancy | 0.18 | 0.49* | 0.32 | 0.72* | 0.18 | 0.87* |
Note. Class 1 = Low exposure to child abuse, neglect and IPV; Class 2 = Child Neglect-Only; Class 3 = Child Abuse/Neglect; Class 4 = polytrauma. Pairwise comparisons are given as Cohen’s D. Latinx was coded such that 1 indicates Latinx status and 0 indicates non-Latinx. Couple status was coded such that a 1 indicates being married or in a committed relationship and a 0 indicates being single, divorced, or widowed. Education was coded such that a 1 meant high school graduate or more education and 0 indicates less than a high school education.
p < .10,
p < .05,
p < .01,
p < .001
Classes compared on demographics.
We first examined how the classes compared on demographic variables (see Table 1). We examined race/ethnicity across classes according to whether individuals identified as Latinx or not (n = 177; 78.7%); the omnibus test was not statistically significant. However, when examining all pairwise comparisons, the childhood abuse/neglect class had a significantly greater proportion of Latinx individuals than the low exposure group. There were no significant educational differences; however, there was a trend effect such that those in the neglect-only class had lower rates of high school graduation. There were no age or couple status differences.
The Home Hardship scale revealed significant and large effect size differences across classes such that the childhood abuse/neglect and polytrauma classes reported experiencing greater economic difficulties (e.g., trouble with bills or food insecurity) compared to the low exposure class and compared to the neglect-only class.
Classes compared on stressors and social support.
Second, we examined and found significant class differences on perceived social support (MSPSS), perceived stress (PSS), and experiences of stressful life events. On the MSPSS, the polytrauma, childhood abuse/neglect, and childhood neglect-only classes all reported significantly lower social support compared to the low exposure class, with large effect sizes (Table 2). The polytrauma class reported significantly lower social support than the childhood abuse/neglect class. However, the childhood neglect-only class did not significantly differ from either the childhood abuse/neglect or polytrauma classes.
On the PSS, the polytrauma and childhood abuse/neglect classes had significantly greater perceived stress than the low exposure class. The childhood neglect-only class had lower perceived stress than the childhood abuse/neglect and polytrauma classes, and paradoxically, the low exposure class.
The stressful life events total score revealed significantly greater numbers of stressful events in the polytrauma and childhood abuse/neglect classes compared to the low exposure class (effect size differences were large); however, there were no observed class differences across the polytrauma, childhood abuse/neglect, and childhood neglect-only classes. Scores on the PDQ did not significantly differ across classes. Overall, these results suggest differences in perceived social support and total number of stressful events between those with exposure to childhood abuse and neglect or IPV compared to those with low exposure. While the three exposure classes had relatively low social support, the childhood neglect-only class was unique in reporting the least amount of perceived stress.
Classes compared on mental health functioning.
We next examined how the groups compared on symptoms and emotion regulation. The polytrauma and childhood abuse/neglect classes consistently differed from both the childhood neglect-only and low exposure classes on DASS Depression and Anxiety and STRESS PTSD symptom severity scores (effect sizes ranged from large to very large). With regard to emotion dysregulation, all three exposure classes differed from the low exposure class. The polytrauma and childhood abuse/neglect classes did not differ from one another on any symptom measures or on emotion dysregulation; however, the polytrauma class had significantly greater mean scores on emotion dysregulation relative to the childhood neglect-only class. We also observed a significant difference across classes on rates of alcohol use during pregnancy. The mothers in the childhood abuse/neglect class were more likely to consume alcohol during pregnancy compared to all other groups. Overall, these results indicate significant and large effect size differences in mental health functioning of pregnant mothers with a history of childhood abuse/neglect or past-year IPV compared to those with low levels of exposure to childhood abuse and IPV. Interestingly, the childhood neglect-only class had relatively low levels of symptomatology.
Nearly identical results were obtained when we utilized a more traditional approach for examining outcome variables and relationships with latent classes/profiles in which individual “group” membership was extracted and ANOVA based analysis were conducted. We opted to report the BCH and DCAT results as these are considered current best practices.
Discussion
Stress and psychopathology during pregnancy are important given their influence on women’s increasing risk for adverse pregnancy, birth, and developmental outcomes (Dunkel Schetter & Tanner, 2012). Childhood abuse and IPV are public health problems with immediate and long term effects that are widespread and costly (Campbell, 2002; Zeanah & Humphreys, 2018). In particular, pregnant women’s own childhood abuse history and current IPV directly and indirectly affect physical and psychosocial outcomes that they themselves experience as well as their offspring (Campbell, 2002). Given that many survivors of childhood abuse go on to experience IPV, simultaneously accounting for both risk factors improves studies of stress, emotion regulation, and mental health in pregnancy. In the current study, latent profile analysis was used as a person-centered, empirically-based approach to explore how childhood abuse and neglect history along with current IPV relate to psychosocial functioning during pregnancy.
The latent profile analysis suggested an optimal solution consisting of 4-classes. Specifically, we found profiles characterized by (1) low probability of ACEs or IPV, (2) childhood neglect-only, (3) childhood abuse/neglect, and (4) combined childhood abuse/neglect and IPV. To note, more than a third of the sample was classified in one of the three ‘exposure’ classes. There are several reasons why these profiles may have emerged. While we identified a childhood abuse/neglect and neglect-only class, we did not identify an IPV only class, which likely reflects how common childhood maltreatment is in individuals impacted by IPV. Indeed, some estimates suggest that childhood abuse leads to more than a 3-fold increase in experiencing IPV as an adult (Coid et al., 2001; Whitfield et al., 2003). The emergence of two separate profiles, one consisting of neglect-only and a second characterized by both childhood abuse/neglect might also have been anticipated given past findings. In general, it is common to experience multiple forms of abuse and neglect; however, childhood neglect is the most common type of childhood maltreatment and neglect is more likely to occur as the only type of maltreatment one experiences compared to other forms of abuse (Zeanah & Humphreys, 2018).
Overall, the stress and mental health functioning outcomes largely reflect that greater exposure to ACEs and/or IPV leads to the worst outcomes. Moreover, our results can be understood as largely consistent with the expected effects for deprivation- and threat-related experiences. Greater mental health difficulties are proposed to be a more common outcome of threat-related experiences, whereas deprivation-related experiences may be associated with cognitive deficits (McLaughlin et al., 2014). The childhood abuse/neglect class, as well as the polytrauma class, both included aspects of threat experiences and individuals in these groups tended to report more stressful life events, lower social support, greater perceived stress, elevated financial and household difficulties, greater difficulties in emotion regulation, and higher levels of anxiety, depression, and PTSD symptoms. These results align with a large body of evidence linking ACEs and IPV to poor psychosocial functioning in pregnancy (Campbell, 2002; Dunkel Schetter & Tanner, 2012; Rich-Edwards et al., 2011; Sarkar, 2008). Overall, the childhood abuse/neglect and the IPV classes were generally similar across outcomes with one notable exception, the childhood abuse/neglect class was more likely to drink alcohol during pregnancy. It is possible that women experiencing IPV in our sample may have been restricted from drinking as a result of controlling partners or limited financial resources to purchase alcohol; although, most studies have found elevated alcohol consumption among those with IPV (Foran & O’Leary, 2008).
Interestingly, the childhood neglect-only class was rather similar to the low exposure class with regard to symptom measures. In contrast, past research has established a strong link between childhood neglect and negative outcomes. Our sample was drawn from a largely socioeconomically disadvantaged population, including our low exposure comparisons group, which may have contributed to why the childhood neglect class did not appear to differentiate as strongly from the low exposure class. In other words, it is possible that some aspects of socioeconomic disadvantage are comparable to neglect-only. This is in line with the literature on deprivation-based ACEs having a greater impact on cognitive/educational outcomes as opposed to mental health difficulties. However, the childhood neglect-only class did exhibit elevated emotion dysregulation compared to the low exposure class, which suggests they may be at risk for developing symptoms and/or responding poorly to stressors. Paradoxically, the childhood neglect-only class had the lowest levels of perceived stress. It is possible that this class did not assess their current experiences as being particularly negative, which may also function to buffer against other negative outcomes.
Overall, our results are in line with recent theories positing a distinction between ACES characterized by deprivation- and threat-based ACEs (McLaughlin et al., 2014; Sheridan & McLaughlin, 2014). Specifically, we found that the childhood-neglect class, a class characterized by deprivation only, was generally similar to the low exposure class. In contrast, the classes characterized by greater exposure to threats in childhood or through recent IPV carried a significant burden of psychosocial and financial stress, as well as mental health symptoms.
These findings make an important contribution to the literature on stress and mental health in pregnancy by employing a person-centered approach in which patterns of exposure to ACEs and IPV differentially increased risk. The current paper has several strengths including its use of a higher risk sample, the assessment of multiple forms of abuse, neglect, and IPV, inclusion of multiple symptom measures, and the use of latent profile analysis. However, the paper also has some limitations. First, we did not assess country of origin or immigration status in our sample. Increased stress associated with migration has been found to be an important risk factor for IPV (Caetano, Vaeth, & Harris, 2007; Jackson et al., 2015; Kaufman Kantor, Jasinski, & Aldarondo, 1994). While there are notable gaps in the literature examining the influence of culture and ethnicity, Latinx individuals may experience higher rates of recurrent IPV and compared to other racial/ethnic groups, Latinx individuals are at increased likelihood of negative mental health outcomes following IPV(Cummings, Gonzalez-Guarda, & Sandoval, 2013). However, it is worth noting that we did include ethnicity in our model and found that it did not differentiate between the groups identified in the LPA. Although, past research has found considerable variability within ethnic groups (Kaufman Kantor et al., 1994), which may have limited our ability to detect effects related to ethnicity. Second, the sample size in our study is modest and this is especially relevant given that the smallest class size represented about 5% of the overall sample. However, the entropy we observed in the model was high, suggesting good separation between classes and even more importantly, the small-sized polytrauma class also emerged in the 3-class model. Future research is needed to confirm whether this class can be reliability observed. Third, our measures were all completed using self-report and we did not assess mental health diagnoses using clinical interviews. However, there is an advantage to these measures as they were used to create dimensional scores, which more accurately reflect the underlying nature of psychopathology and dimensional scores generally lead to greater statistical power. Lastly, we used seven indicators in our latent profile analysis and the inclusion of more indicators might have improved our model; however, the indicators we did include are well validated assessments and these measures produced a model with excellent entropy. Regardless, future studies, especially those using latent profile analysis, would benefit from larger samples and may also be improved by including additional indicators.
Conclusions
Mental health care for pregnant women may be improved by understanding the independent and cumulative effects of violence exposure. LPA is a person-centered approach ideally suited to identifying sub-samples at various levels of risk, aiding opportunities for targeted prevention or intervention. Our results indicated notable differences depending on exposures to threat vs. deprivation, which may have implications for developing targeted screening and interventions. It is likely that a thorough assessment of both IPV, childhood abuse, and neglect may be helpful when considering the needs of pregnant women. These risk factors may not be examined sufficiently in routine practice and further studies are needed to develop clearer guidelines for practitioners (Bailey, 2010). Future studies can be improved by including additional forms of violence (e.g., community violence) and utilization of sophisticated statistical models that can account for complex patterns of violence exposure.
Supplementary Material
Acknowledgements
We thank Ms. Victoria Scranton for study coordination and data collection and management, Ms. Meghan Clough for recruitment and data collection, Drs. Joseph Newell, Margaret McLaren, Sandra Motta, Sonia Chaudhry, and the medical staff at Hartford Hospital Labor and Delivery and Postpartum units for their assistance in sample collection. We especially thank Dr. Amy Johnson for her role in overseeing the study at Hartford Hospital and the Women’s Ambulatory Health Services Clinic. Finally, we thank the Hartford Hospital Women’s Ambulatory Health Services clinic for their vital role in supporting recruitment.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Author Disclosures Statement
No competing financial interest exist for these authors.
Contributor Information
Brandon L. Goldstein, Department of Psychiatry, University of Connecticut School of Medicine;
Margaret Briggs-Gowan, Department of Psychiatry, University of Connecticut School of Medicine;.
Damion J. Grasso, Department of Psychiatry, University of Connecticut School of Medicine.
References
- Adams AE, Tolman RM, Bybee D, Sullivan CM, & Kennedy AC (2012). The Impact of Intimate Partner Violence on Low-Income Women’s Economic Well-Being. Violence Against Women, 18(12), 1345–1367. 10.1177/1077801212474294 [DOI] [PubMed] [Google Scholar]
- Alderdice F, Lynn F, & Lobel M (2012). A review and psychometric evaluation of pregnancy-specific stress measures. Journal of Psychosomatic Obstetrics and Gynecology, Vol. 33, pp. 62–77. 10.3109/0167482X.2012.673040 [DOI] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2018). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes, 21(2), 1–22. [Google Scholar]
- Atzl VM, Narayan AJ, Rivera LM, & Lieberman AF (2019). Adverse Childhood Experiences and Prenatal Mental Health: Type of ACEs and Age of Maltreatment Onset. Journal of Family Psychology. [DOI] [PubMed] [Google Scholar]
- Bailey BA (2010). Partner violence during pregnancy: Prevalence, effects, screening, and management. International Journal of Women’s Health, 2(1), 183–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedict MI, Paine LL, Paine LA, Brandt D, & Stallings R (1999). The association of childhood sexual abuse with depressive symptoms during pregnancy, and selected pregnancy outcomes. Child Abuse and Neglect, 23(7), 659–670. 10.1016/S0145-2134(99)00040-X [DOI] [PubMed] [Google Scholar]
- Bensley L, Van Eenwyk J, & Wynkoop Simmons K (2003). Childhood family violence history and women’s risk for intimate partner violence and poor health. American Journal of Preventive Medicine, 25(1), 38–44. 10.1016/S0749-3797(03)00094-1 [DOI] [PubMed] [Google Scholar]
- Bergman LR, Magnusson D, & El Khouri BM (2003). Studying individual development in an interindividual context: A person-oriented approach. Psychology Press. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Zule W (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Caetano R, Vaeth PAC, & Harris TR (2007). Drinking , and Intimate Hispanic Couples in the U . S 1431–1447. 10.1177/0886260507305568 [DOI] [PubMed]
- Campbell JC (2002). Health consequences of intimate partner violence. Lancet, 359, 1331–1336. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE, Messing JT, Petras H, Fowler B, La Flair L, Kub J, … Campbell JC (2012). Patterns of violence against women: A latent class analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 4(2), 169–176. 10.1037/a0023314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles P, & Perreira KM (2007). Intimate partner violence during pregnancy and 1-year post-partum. Journal of Family Violence, 22(7), 609–619. 10.1007/s10896-007-9112-0 [DOI] [Google Scholar]
- Chung EK, Mathew L, Elo IT, Coyne JC, & Culhane JF (2008). Depressive Symptoms in Disadvantaged Women Receiving Prenatal Care: The Influence of Adverse and Positive Childhood Experiences. Ambulatory Pediatrics, 8(2), 109–116. 10.1016/j.ambp.2007.12.003 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Coid J, Petruckevitch A, Feder G, Chung WS, Richardson J, & Moorey S (2001). Relation between childhood sexual and physical abuse and risk of revictimisation in women: A cross-sectional survey. Lancet, 358(9280), 450–454. 10.1016/S0140-6736(01)05622-7 [DOI] [PubMed] [Google Scholar]
- Coker AL, Smith PH, Thompson MP, McKeown RE, Bethea L, & Davis KE (2002). Social Support Protects against the Negative Effects of Partner Violence on Mental Health. Journal of Women’s Health & Gender-Based Medicine, 11(5), 465–476. 10.1089/15246090260137644 [DOI] [PubMed] [Google Scholar]
- Collins NL, Dunkel-Schetter C, Lobel M, & Scrimshaw SCM (1993). Social Support in Pregnancy: Psychosocial Correlates of Birth Outcomes and Postpartum Depression. Journal of Personality and Social Psychology, 65(6), 1243–1258. 10.1037/0022-3514.65.6.1243 [DOI] [PubMed] [Google Scholar]
- Cummings AM, Gonzalez-Guarda RM, & Sandoval MF (2013). Intimate Partner Violence Among Hispanics: A Review of the Literature. Journal of Family Violence, 28(2), 153–171. 10.1007/s10896-012-9478-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, & Tanner L (2012). Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry, 25(2), 141–148. 10.1097/YCO.0b013e3283503680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, … Arck PC (2007). Social support during pregnancy: Effects on maternal depressive symptoms, smoking and pregnancy outcome. Human Reproduction, 22(3), 869–877. 10.1093/humrep/del432 [DOI] [PubMed] [Google Scholar]
- Farr SL, Bitsko RH, Hayes DK, & Dietz PM (2010). Mental health and access to services among US women of reproductive age. American Journal of Obstetrics and Gynecology. 10.1016/j.ajog.2010.07.007 [DOI] [PubMed] [Google Scholar]
- Fogarty CT, Fredman L, Heeren TC, & Liebschutz J (2008). Synergistic effects of child abuse and intimate partner violence on depressive symptoms in women. Preventive Medicine, 46(5), 463–469. 10.1016/j.ypmed.2007.12.009 [DOI] [PubMed] [Google Scholar]
- Foran HM, & O’Leary KD (2008). Alcohol and intimate partner violence: A meta-analytic review. Clinical Psychology Review, 28(7), 1222–1234. 10.1016/j.cpr.2008.05.001 [DOI] [PubMed] [Google Scholar]
- Gartland D, Giallo R, Woolhouse H, Mensah F, & Brown SJ (2019). Intergenerational Impacts of Family Violence - Mothers and Children in a Large Prospective Pregnancy Cohort Study. EClinicalMedicine. 10.1016/j.eclinm.2019.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilroy H, McFarlane J, Maddoux J, & Sullivan C (2016). Homelessness, housing instability, intimate partner violence, mental health, and functioning: A multi-year cohort study of IPV survivors and their children. Journal of Social Distress and the Homeless, 25(2), 86–94. 10.1080/10530789.2016.1245258 [DOI] [Google Scholar]
- Glover V (2014). Maternal depression, anxiety and stress during pregnancy and child outcome; What needs to be done. Best Practice and Research: Clinical Obstetrics and Gynaecology, 28(1), 25–35. 10.1016/j.bpobgyn.2013.08.017 [DOI] [PubMed] [Google Scholar]
- Grasso DJ, Ford JD, & Greene CA (2019). Preliminary psychometrics of the Structured Trauma-Related Experiences and Symptoms Screener for Adults (STRESS-A) in an urban prenatal healthcare clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 11(8), 927–935. 10.1037/tra0000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118(3), 933–942. 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Jackson CL, Ciciolla L, Crnic KA, Luecken LJA, Gonzales NAA, & Coonrod DVA (2015). Intimate partner violence before and during pregnancy: Related demographic and psychosocial factors and postpartum depressive symptoms among mexican american women. Journal of Interpersonal Violence, 30(4), 659–679. 10.1177/0886260514535262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasinski JL (2004). Pregnancy and Domestic Violence: A Review of the Literature. Trauma, Violence, & Abuse, 5(1), 47–64. 10.1177/1524838003259322 [DOI] [PubMed] [Google Scholar]
- Kaufman Kantor G, Jasinski JL, & Aldarondo E (1994). Sociocultural status and incidence of marital violence in Hispanic families. Violence and Victims, 9(3), 207–222. 10.1891/0886-6708.9.3.207 [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA (2007). Violence against women and the perinatal period: The impact of lifetime violence and abuse on pregnancy, postpartum, and breastfeeding. Trauma, Violence, and Abuse, 8(3), 344–353. 10.1177/1524838007304406 [DOI] [PubMed] [Google Scholar]
- Leeners B, Rath W, Block E, Görres G, & Tschudin S (2014). Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. Journal of Perinatal Medicine, 42(2), 171–178. 10.1515/jpm-2013-0003 [DOI] [PubMed] [Google Scholar]
- Lev-Wiesel R, Daphna-Tekoah S, & Hallak M (2009). Childhood sexual abuse as a predictor of birth-related posttraumatic stress and postpartum posttraumatic stress. Child Abuse and Neglect, 33(12), 877–887. 10.1016/j.chiabu.2009.05.004 [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- McCutcheon AL (1987). Latent class analysis. Sage. [Google Scholar]
- McLaughlin KA (2016). Future Directions in Childhood Adversity and Youth Psychopathology. Journal of Clinical Child and Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, & Lambert HK (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience and Biobehavioral Reviews, 47, 578–591. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulder EJH, Robles De Medina PG, Huizink AC, Van Den Bergh BRH, Buitelaar JK, & Visser GHA (2002). Prenatal maternal stress: Effects on pregnancy and the (unborn) child. Early Human Development. 10.1016/S0378-3782(02)00075-0 [DOI] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (2017). Mplus user’s guide (version 8.0). In Mplus user’s guide (Eighth Ed). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nelson DB, Uscher-Pines L, Staples SR, & Ann Grisso J (2010). Childhood Violence and Behavioral Effects Among Urban Pregnant Women. Journal of Women’s Health, 19(6), 1177–1183. 10.1089/jwh.2009.1539 [DOI] [PubMed] [Google Scholar]
- O’Hara MW (1986). Social support, life events, and depression during pregnancy and the puerperium. Archives of General Psychiatry, 43(6), 569–573. [DOI] [PubMed] [Google Scholar]
- Olsen JM (2018). Integrative Review of Pregnancy Health Risks and Outcomes Associated With Adverse Childhood Experiences. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 47(6), 783–794. 10.1016/j.jogn.2018.09.005 [DOI] [PubMed] [Google Scholar]
- Rich-Edwards JW, James-Todd T, Mohllajee A, Kleinman K, Burke A, Gillman MW, & Wright RJ (2011). Lifetime maternal experiences of abuse and risk of pre-natal depression in two demographically distinct populations in Boston. International Journal of Epidemiology, 40(2), 375–384. 10.1093/ije/dyq247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar NN (2008). The impact of intimate partner violence on women’s reproductive health and pregnancy outcome. Journal of Obstetrics and Gynaecology, Vol. 28, pp. 266–271. 10.1080/01443610802042415 [DOI] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, & Low LK (2008). Mental Health, Demographic, and Risk Behavior Profiles of Pregnant Survivors of Childhood and Adult Abuse. Journal of Midwifery and Women’s Health, 53(6), 511–521. 10.1016/j.jmwh.2008.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan MA, & McLaughlin KA (2014). Dimensions of early experience and neural development: Deprivation and threat. Trends in Cognitive Sciences. 10.1016/j.tics.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Reed E, & Raj A (2006). Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: Associations with maternal and neonatal health. American Journal of Obstetrics and Gynecology, 195(1), 140–148. 10.1016/j.ajog.2005.12.052 [DOI] [PubMed] [Google Scholar]
- Smith Slep AMS, & O’Leary SG (2001). Examining partner and child abuse: Are we ready for a more integrated approach to family violence? Clinical Child and Family Psychology Review, 4(2), 87–107. 10.1023/A:1011319213874 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of Family Issues, 17(3), 283–316. [Google Scholar]
- Sullivan JX, Turner L, & Danziger S (2008). The relationship between income and material hardship. Journal of Policy Analysis and Management, 27(1), 63–81. 10.1002/pam.20307 [DOI] [Google Scholar]
- Wadsworth P, Degesie K, Kothari C, & Moe A (2018). Intimate partner violence during the perinatal period. The Journal for Nurse Practitioners, 14(10), 753–759. 10.1016/j.nurpra.2018.08.009 [DOI] [Google Scholar]
- Whitfield CL, Anda RF, Dube SR, & Felitti VJ (2003). Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. Journal of Interpersonal Violence, 18(2), 166–185. 10.1177/0886260502238733 [DOI] [Google Scholar]
- Yali AM, & Lobel M (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics and Gynaecology, 20(1), 39–52. 10.3109/01674829909075575 [DOI] [PubMed] [Google Scholar]
- Yali Ann Marie, & Lobel M (2002). Stress-resistance resources and coping in pregnancy. Anxiety, Stress & Coping, 15(3), 289–309. 10.1080/1061580021000020743 [DOI] [Google Scholar]
- Zeanah CH, & Humphreys KL (2018). Child Abuse and Neglect. Journal of the American Academy of Child and Adolescent Psychiatry, 57(9), 637–644. 10.1016/j.jaac.2018.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


