Abstract
Revision rhinoplasty presents several complex surgical challenges. Proper patient selection for revision rhinoplasty, along with thorough preoperative examination and surgical planning, is key to achieving ideal outcomes. Along with achieving a high level of understanding of primary rhinoplasty techniques, surgeons performing revision rhinoplasty must understand and diagnose deformities created by the primary surgery. A systematic approach to diagnosing rhinoplasty deformities assists in forming a suitable surgical plan. A classification system based on nasal analysis, described here, may be used to differentiate the degree of difficulty of the surgery as well as assist in surgical planning. Surgeons have a multitude of options available in their armamentarium for addressing common nasal deformities encountered during revisional surgery, and a stepwise surgical approach may facilitate the creation of an optimal aesthetic and functional result.
Keywords: revision rhinoplasty, rhinoplasty, secondary rhinoplasty, nasal analysis
Revision rhinoplasty is often described as one of the most difficult surgeries to perform in plastic surgery. The rates of revision rhinoplasty are variable but occur in up to 15% of rhinoplasty patients. 1 2 Most of these patients seek revision for cosmetic reasons and have been left with undesirable emotional and physical outcomes from a suboptimal surgical result. 2 Thus, working with revision rhinoplasty patients requires the utmost attention to detail from the first visit. Intraoperatively, revision rhinoplasty often reveals unexpected challenges, leaving surgeons assessing and reassessing their operative techniques, emphasizing the importance of preparedness for any scenario encountered intraoperatively. This article aims to provide a stepwise approach to revision rhinoplasty through a thorough preoperative assessment utilizing a novel classification system for case complexity stratification and also aims to describe operative techniques for fixing deformities encountered during revision rhinoplasty surgery.
Preoperative Assessment/Patient Evaluation
A thorough preoperative evaluation is crucial for the revision rhinoplasty patient. This begins with the history and patient interview, with the utmost importance placed on evaluating specific concerns that led the patient to seek a revision rhinoplasty. The patient's goals of revision should be discussed and clearly demarcated as well. If available, pre- and postoperative photos as well as operative notes from any previous rhinoplasties should be obtained. These operative notes can be informative but the surgeon should not depend on these for surgical planning as they can harbor inaccuracies. In evaluating current concerns, it is important to discern between functional and cosmetic concerns and have the patient and surgeon outline and stratify the importance of each, as many revision rhinoplasty patients have concerns in both areas. 3 A full medical history should be obtained, including trauma history, substance use, medications, and allergies. The next step is to determine if the patient's concerns are congruent with the physical exam findings and if these concerns are correctable with revision.
Physical Exam
The physical exam should be performed methodically with both an external and internal exam to diagnose any existing anatomic deformities. The senior author (Bressler, FJ) utilizes a preoperative evaluation form to systematically evaluate and make note of all aesthetic and functional issues (see Fig. 1 ).
Fig. 1.
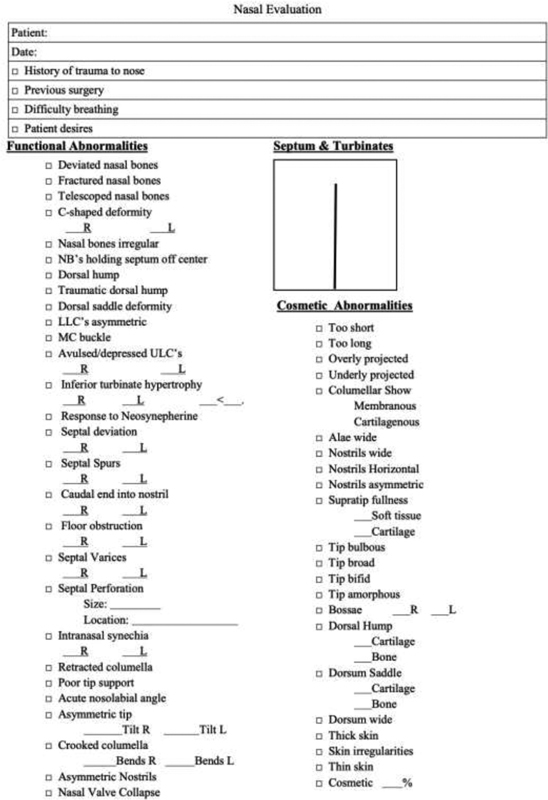
Preoperative Nasal Evaluation Form.
The skin envelope is assessed for skin thickness and skin type as well as damage from previous rhinoplasties. Careful palpation can help discern if the patient has thinning of skin from extrusion of previous graft materials or extensive scarring. The external exam can be divided into thirds for separate analysis (see Fig. 2 ). The upper third contains the bony pyramid, which is examined and palpated for asymmetries, irregularities, width, persistent dorsal hump, and open roof deformities. The middle third includes the dorsal septum and upper lateral cartilages (ULCs), which is examined for any asymmetries, deviations, and saddling. Dorsal humps should be palpated and collapse of ULCs should be noted. The lower third includes the nasal tip, caudal septum, alar cartilages, and alar base. Here, one must note domal asymmetries, fullness, depressions, and shape of the nasal tip. Tip rotation and projection are evaluated. The most common deformities encountered in revision surgery are those of the lower third, followed by those in the middle third. 4 5
Fig. 2.
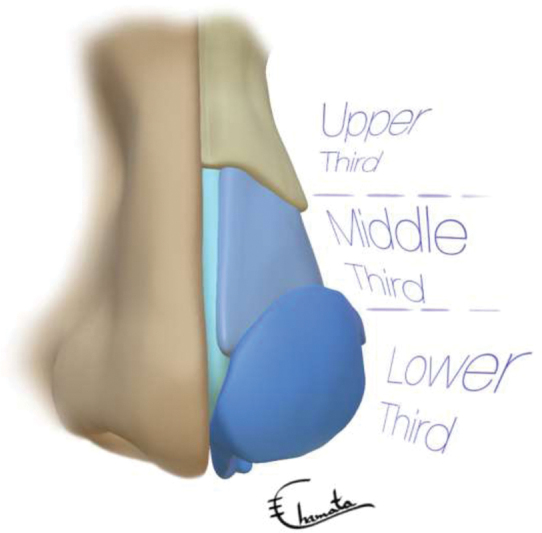
The three major zones of the nose.
The internal exam is done with a nasal speculum and includes examination of the external nasal valves, septum, internal nasal valves, and inferior turbinates. The septum is evaluated via anterior rhinoscopy or endoscopy for deviations and perforation and can be palpated and/or transilluminated to determine whether cartilage is present. Presence of any bone spurs should be noted. Turbinates are evaluated for hypertrophy. This aspect of the internal exam is often aided by sprayed decongestants as well. The nasal mucosa and vestibule are evaluated for synechiae.
Functional issues are first examined by watching the patient breathe. Patients are evaluated for dynamic collapse, first with normal breathing and then with forceful inhalation. The patient is asked to grade his or her airflow through each side of his nose on a scale from 0 to 10. The patient is asked to grade the resultant airflow again from 0 to 10 while gently occluding the contralateral nostril. The procedure is then repeated on the other side. The entire evaluation is repeated again, but with decongestant applied, to weigh the effects of mucosal edema on obstruction. These maneuvers, when combined with a thorough examination, can accurately predict the area of maximal obstruction and can help guide the surgeon as to the best surgical treatment. Internal nasal valve obstruction can also be diagnosed with the Cottle maneuver. 6 Finally, the patient may be evaluated for availability of ear and rib cartilage.
Risk Stratification
Patient selection can have as much effect on revision rhinoplasty results as the surgery itself. 7 As with primary rhinoplasty, patient selection encompasses a variety of factors. Through the history and physical exam, the surgeon will have a complete understanding of the problems that led to the patient desiring a revision and whether these problems are correctable. Open communication should be fostered during the consultation. There should be acceptable surgical risk-to-reward ratio with regard to the patient's specific concerns and potential surgical corrections.
Much has been made of the psychology of rhinoplasty patients. 8 9 10 Some believe that the most difficult aspect of revision rhinoplasty is the psychology of the revision rhinoplasty patient. 11 These patients have faced disappointing aesthetic surgery and now returned desiring improvement. Thus, evaluation of the psychology of revision rhinoplasty patients should be a part of the initial consultation. If there are any concerns, referral to a mental health specialist is prudent and further surgical evaluation would be held until this is completed. 12
Revision surgery should not be attempted in most cases until at least 1 year after the initial surgery. 13 14 15 This allows the results of the primary rhinoplasty to present themselves, as it can take up to a year for scar tissue to mature. In the case that a patient needs minimal revision, such as revision osteotomies or persistent dorsal hump surgery, revision surgery can be performed earlier than 1 year. 7 13 However, most surgeries, especially those requiring a moderate amount of soft-tissue dissection, are best approached after waiting 1 full year.
Nasal Analysis
The authors have devised a novel classification system to be utilized during the preoperative assessment, based on a systematic approach to nasal analysis (see Table 1 ). This allows the surgeon to classify the level of complexity of the surgery and also allows for proper surgical planning for the specific case at hand. The preoperative Nasal Evaluation Form alerts the surgeon to important observations such as nasal valve collapse, poor tip support, nasal bone irregularity, ULC issues, and tip bossae. These notations assist with anticipating the number of cartilage grafts or soft-tissue grafts required to successfully perform the revision.
Table 1. Revision rhinoplasty preoperative assessment classification.
| Class 1: refinement | Class 2: completion | Class 3: structural | Class 4: major | |
|---|---|---|---|---|
| Complexity | Minor | Low | Moderate | Highest |
| Primary result Outcome | Good | Incomplete | Poor | Worst |
| Previous revisions | No | No | Sometimes | Yes |
| Needs advanced tip reconstruction | Minor | No | Often | Yes |
| Needs valve repair | No | Variable | Yes, internal or external | Yes, both internal and external |
| Expected number of cartilage grafts | 0–1 | 1–3 | 1–3 | ≥3 |
| Septal cartilage present | N/A | Yes | Sometimes | No |
| Nasal septal perforation | No | No | Seldom | Variable |
| Needs revision septoplasty | No | Septum intact, cartilage present | Sometimes | Often |
| Needs costal cartilage | No | No | Sometimes | Yes |
| Needs fascia grafts or ADM | Variable | No | Sometimes | Often |
| SSTE concerns | Variable | No | Sometimes | Yes |
| Open vs. endonasal | Variable | Open preferred | Open | Open |
Abbreviations: ADM, acellular dermal matrix; SSTE, skin and soft-tissue envelope.
Class 1: Refinement Revision Surgery
These are surgeries of minor complexity. Patients have generally had a good primary outcome from their rhinoplasty; however, a limited amount of refinement is required such as finesse changes to the columella, tip, or dorsum due to persistent minor issues such as persistent dorsal fullness, wide nasal bones, mild columellar profile concerns, scar tissue, or minor intranasal synechia. These procedures may be performed endonasal or open and do not require any new cartilage or tissue grafts (see Fig. 3 ).
Fig. 3.
Class 1 level complexity of revision. This patient presented with a hanging columella and slight residual dorsal hump. A caudal septal reduction with bilateral vestibular mucosal resection, rasping of the dorsum, and revision osteotomies were performed. (The images are provided courtesy of Fred J. Bressler, MD.)
Class 2: Completion Revision Surgery
These are low-complexity cases. These patients' primary rhinoplasty results appear incomplete. Overall, the result appears “unfinished” to the surgeon. In these scenarios, most structural cartilage structures are still intact and have not been destroyed or overly resected. The primary surgery may have been done endonasal or open and typically there is enough remaining septal cartilage for use if needed. Common deformities seen are persistently wide dorsal aesthetic lines or a persistently amorphous tip lacking proper refinement, among others (see Fig. 4 ).
Fig. 4.

Class 2 level complexity of revision. This patient presented with a pollybeak deformity caused by residual dorsal hump and tip ptosis. She underwent a completion rhinoplasty with dorsal hump reduction, columellar strut graft placement, and cephalic trim of the lower lateral cartilages with suture modification utilizing a lateral crural steal technique. Revision osteotomies were also performed. (The images are provided courtesy of Fred J. Bressler, MD.)
Class 3: Structural Revision Surgery
These are cases of moderate complexity. The primary rhinoplasty was more extensive with unsatisfactory results and will require cartilage grafts or soft-tissue grafts. These patients typically have persistent and/or acquired nasal deformity involving one or more zones of the nose (i.e., upper third, middle third, and/or lower third). A prior septoplasty may have been performed also with limited available autologous septal cartilage left for use; therefore, it will require autologous or cadaveric costal cartilage for the revision. Generally, not more than three major cartilage grafts are utilized in these scenarios (e.g., two spreader grafts and a columellar strut graft). The patient may complain of functional issues as well due to persistent septal deviation or nasal valve collapse, thus requiring simultaneous functional repair alongside repair of the aesthetic deformities. Due to the complexity of these cases, an open approach is preferred to facilitate the execution of advanced techniques (see Fig. 5 ).
Fig. 5.

Class 3 level complexity of revision. This patient presented with tip bossae along with functional deficits caused by residual septal deviation and external nasal valve collapse. Her revision included a septoplasty, placement of bilateral alar batten grafts, placement of a columellar strut graft, and advanced tip reconstruction via vertical lobular division. (The images are provided courtesy of Fred J. Bressler, MD.)
Class 4: Major Revision Surgery
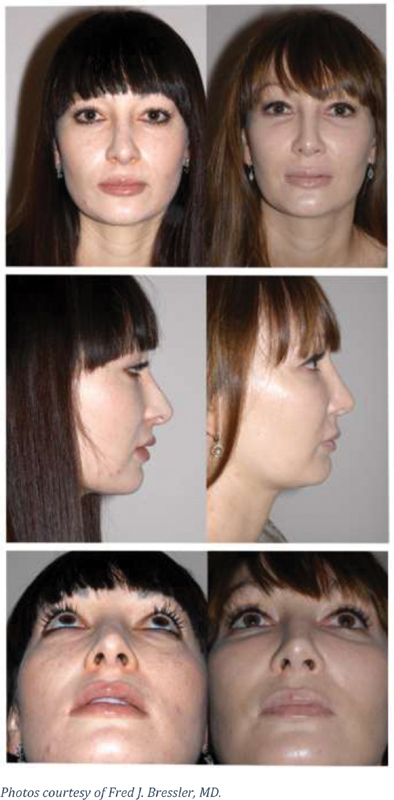
These are high-complexity cases and are the most challenging of revision rhinoplasty concerns. This category shares many of the same features and characteristics of Class 3 revisions; however, these cases often have worst outcomes from their previous surgery. Patients may also have had a prior revision or multiple previous revisions, and typically present with persistent and/or acquired nasal deformity involving all zones of the nose (i.e., upper third, middle third, and lower third). Overresection of nasal structures and poor support may be encountered in all zones, causing functional deficits and aesthetic deformities such as severe nasal tip deformities and alar notching/retraction. As with Class 3 revisions, autologous septal cartilage has likely been previously harvested; therefore, autologous or cadaveric cartilage grafts will be needed to restore the structural framework. The preoperative plan should account for the use of at least three to five grafts. The use of temporalis fascia or acellular dermal matrix (ADM) is also frequently needed. Due to the high complexity of these cases, an open approach is required for the revisions (see Fig. 6 ).
Fig. 6.

Class 4 level complexity of revision. This patient presented with a saddle nose deformity, inverted-V deformity, open roof deformity, tip overprojection, and bilateral internal and external nasal valve collapse. Her revision included the use of five cartilage grafts using cadaveric costal cartilage (bilateral spreader grafts, bilateral alar batten grafts, columellar strut graft, and dorsal augmentation graft), one soft-tissue graft using ADM, and advanced tip reconstruction via vertical lobular division. (The images are provided courtesy of Fred J. Bressler, MD.)
Class 5: Reconstructive Revision Surgery
This classification describes cases that may require reconstruction of the skin and soft-tissue envelope after primary rhinoplasty, cancer, trauma, or burns. They involve the use of local, regional, or free flaps for coverage, as well as reconstruction of the underlying osseocartilaginous framework when needed. Patients who fall into this category may not have had a prior rhinoplasty, as these cases are frequently performed after cancer excision. This class will not be further discussed in this article as it falls beyond the scope of this revision rhinoplasty topic.
Surgical Planning
Standardized preoperative rhinoplasty photos are taken in the frontal, lateral, oblique, and base views, both static and smiling. These photos are critically analyzed for all deformities and correlated with physical exam findings. Photo analysis should also be communicated with the patient for a better understanding of their deformity. 16
After completing this nasal analysis, specific corrections can then be planned. Rhinoplasty worksheets, nasal evaluation forms, and review of preoperative photographs allow the surgeon to map out the deformities and to note their corrections in one comprehensive visual aid. 17
Computer imaging is becoming an increasingly popular tool for preoperative evaluation and surgical planning in rhinoplasty, serving a similar function to the rhinoplasty worksheet. 18 With the advent of 3D imaging, this technology has advanced to be able to provide precise facial measurements preoperatively and simulate postoperative results. 19 These images can facilitate communication and set expectations for patients, possibly increasing their postoperative satisfaction. 20 For the surgeon, these tools can lead to better appreciation of the individualized anatomical structures, allowing for more informed preoperative planning. 21
Revision rhinoplasty patients often require structural support or reshaping with cartilage grafting. The available graft options must be assessed preoperatively and their harvest incorporated into the surgical plan. Septal cartilage is the ideal graft material given that it is easily harvested, avoids an additional harvest site, and has the appropriate composition. 22 However, its use is limited in revision rhinoplasty as it is often harvested during the primary surgery. Conchal and costal cartilages are other autologous options, with disadvantages of creating additional harvest sites and added operative times. 3 23 Conchal cartilage also lacks the rigidity of other cartilage grafts. Costal cartilage, on the other hand, provides strong support but is prone to warping. 5 24 25 Options described in the literature to limit warping include carving the graft with the concave side down, cross-sectional carving, or K-wire placement. 25 26 27 Nonautologous options for cartilage grafting include cadaveric cartilage allograft or irradiated rib cartilage, with the authors' preference being fresh frozen cadaveric costal cartilage. 28
The specific surgical approach is based on the needs of each individual case and surgeon preference. In revision rhinoplasty, the external approach is favored due to increased visualization of nasal structures to facilitate proper diagnosis and correction. 29 The internal approach should be reserved for more minor revisions with deformities in single anatomic region. 13 It is best used for dorsal hump reduction, osteotomies, or single graft strut placement for tip support.
In revision rhinoplasty, the surgeon must always be prepared for the unexpected. There can be any number of intraoperative findings not described on the original operative note. A second and third option for graft material should be available, and the patient should be made aware of possible needs to harvest temporalis fascia or use different graft material such as ADM.
Stepwise Approach to Revision Rhinoplasty
Anesthesia Choice
The choice of whether to perform the revision procedure under general anesthesia or local anesthesia is made with the same considerations as with primary procedures. Patient preference, surgeon preference, and expected length of surgery are factors that determine which anesthetic choice to utilize.
Injection of a local anesthetic with epinephrine is used to block the field, assist in hemostasis, and decrease postoperative pain. Hydrodissection with these injections assists in creating a plane, and thus should be injected in the anticipated plane of surgical dissection. 30 This is, of course, more challenging in scarred planes from previous surgery.
The Septum
The nasal septum may be addressed either prior to opening the nose with a hemitransfixion incision or after opening the nose by dissection through the anterior septal angle (ASA). 31 In either scenario, septal problems should be assessed after complete dissection and exposure of the septum from the mucoperichondrium.
Depending on the specific problem at hand, deformities or deviations in the caudal septum can be fixed with resection, relocation, or reinforcement/replacement. Several millimeters of the caudal septum can be resected to correct caudal septal excess. In cases of caudal septal deviation, relocation can be performed by freeing it from its distal attachments, bringing it across the midline, and then suturing it to the anterior nasal spine (ANS). The septum must be rigidly fixed onto the nondeviated side of the ANS. Reinforcement and/or replacement with graft material is used when the structural integrity of the caudal septum is compromised. 32
Bony deviations of the septum can be resected and straight deflections can be fractured back to midline. Any bony spurs should be excised and removed as well. Care should be taken to not twist or forcefully pull bony fragments. This prevents propagation of fractures and thus protects the cribriform plate from cerebrospinal fluid (CSF) leak. 33 The senior author has found that the best way to prevent CSF leak when removing bone fragments is to detach the perpendicular plate below the skull base horizontally and posterior to the septal cartilage L-strut with double-action scissors, which frees the surgeon to gently remove all posterior bony obstructions without twisting and without excessive force.
If the septum is addressed prior to opening the nose, closure of the hemitransfixion incision and dead-space closure between mucoperichondrial flaps are then performed after the septum is addressed. This causes less swelling and creates an area of precise dorsal pockets for spreader graft placement if needed.
The Skin Envelope
When choosing an incision for revision rhinoplasty, one must be aware of where previous incisions were made. However, in regard to scar quality, previous incisions can be ignored and the incision that gives the best possible exposure should be chosen. 34 If possible, the skin envelope should be opened the same way as if it was a primary rhinoplasty. Opening requires careful elevation to avoid buttonholing. Less cautery should be used to prevent devascularization. The dissection should be kept midline and deep, and one should stay subperiosteal above the keystone area. Thick and thin skin should be addressed differently. 35
A thick skin envelope can limit tip definition and obscure contours created by the underlying cartilages. 36 To address this, scarred soft tissue overlying alar cartilages may be resected. Debulking of fibrofatty tissue on the undersurface of the skin envelope can be performed, starting with the lobular skin and supratip area. Debulking is performed judiciously to prevent compromise and devascularization of the skin flap. 32
In contrast, a thin skin envelope uncovers underlying imperfections of the bony and cartilaginous architecture. Thus, it is critical to maintain a deep dissection in direct contact with the underlying cartilage in these cases, proceeding slowly and meticulously to avoid skin perforation. Additional soft-tissue padding with deep temporal fascia or ADM can be placed over the bone or cartilages if needed. 32
Osseocartilaginous Framework
Once the skin envelope is completely elevated and exposure is complete, the underlying osseocartilaginous framework and its deformities are then assessed. This should be performed in a systematic fashion by evaluating the anatomic components of the nose. At this point, the operative plan is reevaluated, going through once again what repairs need to be performed and what grafts will be needed, making adjustments as necessary. The nose is typically then deconstructed to its anatomic units to further define the underlying deformities. For example, ULCs may be released from the septum and lower lateral cartilages may be released from one another for further evaluation, exposure, and treatment. Problematic grafts such as displaced or misplaced grafts are also removed at this point.
Structural modifications can then be made in a systematic fashion, working from the top down. With each area to be addressed, the simplest and least destructive maneuvers should be performed first, and more complex maneuvers are undertaken as needed. Resection of tissues should be done gradually, as one can always excise more tissue if needed. Do not burn bridges.
Upper Third
Upper-third deformities in the radix and dorsum are to be addressed first. They are often due to under- or overresection of the bony hump, or osteotomy irregularities. 14 The radix contains the nasion point, which is the deepest portion of the nasofrontal angle. Establishing the correct nasion point is crucial as it defines the nasal start point, which contributes to nasal length. Rasping can correct bony underresection. Revision osteotomies need to be performed for a variety of deformities. Incomplete or greenstick deformities may have occurred with previous rhinoplasty. Osteotomies may have been asymmetrically placed, leading to deviations. Adequate lateral osteotomies can correct open roof deformities and can also narrow a wide nasal pyramid, and spreader grafts may also be used for persistent open roof deformities to fill this space. 37 38 The timing of osteotomies is variable and highly surgeon dependent. The senior author prefers to perform them at the end of surgery and before splint placement to minimize swelling, bleeding, and bruising.
Middle Third
Middle third deformities include pollybeak deformity, saddle nose, and inverted-V deformity. A pollybeak deformity occurs when the supratip area projects further than the tip, leading to a rounded tip with supratip fullness. Soft-tissue fullness due to scar formation after overresection of the dorsal septum can lead to these deformities. In these cases, scar tissue will need to be excised at revision surgery and the patient will undergo interval steroid injections after revision. Pollybeak deformity may also be caused by cartilaginous septum excess from underresection and thus can be corrected with excision of the undertreated area. 39 Nasal tip support with a columellar strut graft or septal extension grafts is also necessary to prevent future tip ptosis and is a crucial aspect of preventing recurrence.
Saddle nose occurs due to loss of septal cartilage in the middle vault of the nose, often caused by overresection of septal cartilage or septal necrosis from infection or hematoma. This is corrected with layered onlay grafting. 13 To avoid visible edges of the graft, edges are smoothed and can be covered with other soft tissue such as temporalis fascia or ADM. 13 Spreader grafts can help support onlay grafting and reconstruct dorsal aesthetic lines.
Inverted-V deformity occurs when there is a narrow middle third of the nose and the caudal border of the nasal bones forms an inverted-V at the junction of the middle vault and upper nasal vault. This is often caused by reduction of the cartilaginous hump without supporting the junction between the ULCs and dorsal septum, leading to collapse of the ULCs and internal nasal valve. Spreader grafts are used to support and lateralize the ULCs and can open the internal nasal valve. 40 These are placed in a submucoperichondrial tunnel with sufficient spaces up to the caudal border of the nasal bones. Middle vault reconstruction with spreader grafts is one of the most important tools for addressing many of the deformities seen in the middle third.
After reconstruction and closure of the middle vault, augmentation of an overresected dorsum is performed to restore dorsal height and/or width. For dorsal augmentation, graft material is carved in a canoelike shape and placed in a tight subperiosteal pocket. 7 The graft is also sutured to the middle vault and to the spreader grafts via circumferential sutures to further prevent any graft displacement. The graft should be carved so that its lateral side walls align properly with the nasal sidewalls to allow for smooth dorsal aesthetic lines. ADM can be used as a cover to create smoother contours.
Lower Third
Due to complex anatomy and previous manipulation, revising the nasal tip requires a multifaceted approach. Like many of the other deformities discussed, tip deformities can be due to inadequate correction of existing anatomical features or flawed correction of previous abnormalities, creating new deformities. The tripod theory of the nasal tip is useful for conceptualizing nasal tip modifications. 41 42 Lengthening or shortening of any of the three legs can have effects on tip positioning.
The tip can be under- or overrotated after previous rhinoplasty. To fix underrotation, one can shorten the lateral crura or support the medial crura. Domal suturing of the lateral crura can recruit them medially for a lateral crural steal technique to increase rotation. 14 This can also be accomplished with lateral crural overlay or cephalic resection of lower lateral cartilages. 43 Overrotation can occur when the cephalic lateral crura are narrowed or with overresection of the ASA. It is difficult to fix this directly; therefore, corrections are focused on creating an illusion of derotation by increasing nasal length. This can be done with suturing a shield infratip lobule graft or with a septal extension graft. 13 The medial crura can be transected and overlapped to pull the tip down, which decreases rotation but also deprojects the nose. In extreme cases, a composite graft can be placed between the upper and lower lateral cartilages to derotate the nose. A key aspect of tip reshaping is providing long-term structural support to the tip, which may be achieved with septal extension grafts or columellar strut grafts. 44
Other tip deformities also require correction such as the presence of nasal bossae. These are knoblike protuberances that can form after primary rhinoplasty due to manipulation of the skin and/or alar cartilages, or from postoperative scar contracture. Effective correction of this deformity preferred by the authors involves dome division and suture reconstitution, although camouflage grafting may also be used. 45
Alar retraction also affects definition and shape of the lower third of the nose. This deformity may be caused by overresecting the cephalic margin of the lower lateral cartilages and leaving less than 7 mm of lateral crura behind. Alar retraction can be corrected with alar contour grafts. These grafts are inserted into a subcutaneous pocket created posterior and parallel to the alar rim. 46 Correction of alar retraction may also be performed using advanced lower lateral cartilage division and repositioning techniques. Composite conchal cartilage grafting or chondrocutaneous flaps are options for more complex defects of the alar rim. 14
A hanging columella after primary rhinoplasty is usually a result of failed diagnosis and undertreatment but can also occur from oversized columellar strut grafts. If it is due to excess membranous septum, resection of the caudal septum may be performed. Another option to treat a hanging columella is with a tongue-in-groove technique. 47 Columellar retraction, on the other hand, may be caused by overresection of the caudal septum or due to poor support to weak medial crura. A columellar strut placed between the medial crura provides shape and support for the columella in these scenarios. Other options include caudal septal extension grafts. 14
More severe deformities in which entire domal segments or large portions of the alar cartilages have been excised require more extensive graft reconstruction to provide support and to restore proper nasal function and aesthetics. 48
Postoperative Care
Postoperative care for revision rhinoplasty patients is similar to primary patients. Nasal packing is placed at the conclusion of surgery and is removed the next day. Some surgeons use lubricated Doyle splints instead that are sutured together to compress the mucosal leaflets if the patient has received turbinate or septal work to minimize risk of septal hematoma and prevent synechiae formation. Doyle splints are removed 7 days after surgery if used. In lieu of Doyle splints, the senior author prefers septal quilting mattress sutures. Steri-Strips are placed on the nose from the radix to the supratip to compress the skin envelope, reduce edema, and model the tip. The authors prefer custom-fit aluminum splints for external nasal splint placement, although plastic molded splints may be used alternatively. Pain medications and oral antibiotics are prescribed. The patient is instructed to clean all sutures two to three times daily with hydrogen peroxide and to remove any crusts. The patient is informed to avoid aerobic exercise and weightlifting for 3 weeks and contact sports for 6 weeks. On postoperative day 6 or 7, the external nasal splint and Steri-Strips are removed and the nose is cleaned. Columellar and alar sutures are taken out and the nose is gently cleaned with hydrogen peroxide. Our postoperative protocol does not typically involve retaping once the splints have been removed; however, if retaping is performed by the surgeon, the patient is asked to return 2 to 3 days later for tape removal. Although some surgeons instruct their patients to retape the nose nightly for several weeks after surgery, we believe this causes unnecessary trauma to the nasal skin and soft-tissue envelope and leads to more postoperative edema; therefore, we ask our patients to avoid retaping. The patient is seen again for routine exam and cleaning on a weekly basis for 3 weeks after surgery, then twice in the second month, and once in the third month. Postoperative photographs are taken at 3, 6, and 12 months after surgery to monitor progress and healing. Reassuring and informing the patient that complete healing can take up to 1 year is helpful. Patients are seen annually thereafter to track progress.
Conclusion
The complexity of revision rhinoplasty cannot be understated. Treating revision rhinoplasty patients begins with an honest conversation about the patient's assessment of their own previous rhinoplasty during the first preoperative visit. Through meticulous surgical planning, the surgeon limits the number of surprises inevitably encountered during the surgery. Becoming a competent revision rhinoplasty surgeon requires an extensive understanding of nasal anatomy and how to restore this anatomy in both a functional and aesthetic manner.
Footnotes
Conflict of Interest None declared.
References
- 1.Kamer F M, McQuown S A. Revision rhinoplasty. Analysis and treatment. Arch Otolaryngol Head Neck Surg. 1988;114(03):257–266. doi: 10.1001/archotol.1988.01860150039014. [DOI] [PubMed] [Google Scholar]
- 2.Sharif-Askary B, Carlson A, Van Noord M, Marcus J. Incidence of postoperative adverse events after rhinoplasty: a systematic review. Plast Reconstr Surg. 2020;145(03):669–684. doi: 10.1097/PRS.0000000000006561. [DOI] [PubMed] [Google Scholar]
- 3.Bouaoud J, Loustau M, Belloc J B. Functional and aesthetic factors associated with revision of rhinoplasty. Plast Reconstr Surg Glob Open. 2018;6(09):e1884. doi: 10.1097/GOX.0000000000001884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vuyk H D, Watts S J, Vindayak B. Revision rhinoplasty: review of deformities, aetiology and treatment strategies. Clin Otolaryngol Allied Sci. 2000;25(06):476–481. doi: 10.1046/j.1365-2273.2000.00353.x. [DOI] [PubMed] [Google Scholar]
- 5.Parkes M L, Kanodia R, Machida B K. Revision rhinoplasty. An analysis of aesthetic deformities. Arch Otolaryngol Head Neck Surg. 1992;118(07):695–701. doi: 10.1001/archotol.1992.01880070025005. [DOI] [PubMed] [Google Scholar]
- 6.Fung E, Hong P, Moore C, Taylor S M. The effectiveness of modified Cottle maneuver in predicting outcomes in functional rhinoplasty. Plastic Surg Int. 2014;2014:618313. doi: 10.1155/2014/618313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Becker D G, Park S S. New York, NY: Thieme; 2008. Revision Rhinoplasty; p. 73. [Google Scholar]
- 8.Marcus P. Psychological aspects of cosmetic rhinoplasty. Br J Plast Surg. 1984;37(03):313–318. doi: 10.1016/0007-1226(84)90073-0. [DOI] [PubMed] [Google Scholar]
- 9.Veale D, De Haro L, Lambrou C. Cosmetic rhinoplasty in body dysmorphic disorder. Br J Plast Surg. 2003;56(06):546–551. doi: 10.1016/s0007-1226(03)00209-1. [DOI] [PubMed] [Google Scholar]
- 10.Brucoli M, Baena R RY, Boffano P, Benech A. Psychological profiles in patients undergoing orthognathic surgery or rhinoplasty: a preoperative and preliminary comparison. Oral Maxillofac Surg. 2019;23(02):179–186. doi: 10.1007/s10006-019-00758-1. [DOI] [PubMed] [Google Scholar]
- 11.Adamson P A, Warner J, Becker D, Romo T J, III, Toriumi D M. Revision rhinoplasty: panel discussion, controversies, and techniques. Facial Plast Surg Clin North Am. 2014;22(01):57–96. doi: 10.1016/j.fsc.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Javanbakht M, Nazari A, Javanbakht A, Moghaddam L. Body dysmorphic factors and mental health problems in people seeking rhinoplastic surgery. Acta Otorhinolaryngol Ital. 2012;32(01):37–40. [PMC free article] [PubMed] [Google Scholar]
- 13.Paun S H, Nolst Trenité G J. Revision rhinoplasty: an overview of deformities and techniques. Facial Plast Surg. 2008;24(03):271–287. doi: 10.1055/s-0028-1083082. [DOI] [PubMed] [Google Scholar]
- 14.Bagal A A, Adamson P A. Revision rhinoplasty. Facial Plast Surg. 2002;18(04):233–244. doi: 10.1055/s-2002-36491. [DOI] [PubMed] [Google Scholar]
- 15.Sachs M E. New York, NY: Springer; 2006. Mastering Revision Rhinoplasty. [Google Scholar]
- 16.Zijlker T D, Vuyk H, Adamson P A. Rhinoplasty: preoperative photographic analysis. Clin Otolaryngol Allied Sci. 1992;17(04):361–369. doi: 10.1111/j.1365-2273.1992.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 17.Rohrich R J, Adams W P, Jr, Ahmad J, Adams W P. New York, NY: Thieme Medical Publishers, Incorporated; 2014. Dallas Rhinoplasty. [Google Scholar]
- 18.Singh P, Pearlman S. Use of computer imaging in rhinoplasty: a survey of the practices of facial plastic surgeons. Aesthetic Plast Surg. 2017;41(04):898–904. doi: 10.1007/s00266-017-0858-3. [DOI] [PubMed] [Google Scholar]
- 19.Persing S, Timberlake A, Madari S, Steinbacher D. Three-dimensional imaging in rhinoplasty: a comparison of the simulated versus actual result. Aesthetic Plast Surg. 2018;42(05):1331–1335. doi: 10.1007/s00266-018-1151-9. [DOI] [PubMed] [Google Scholar]
- 20.Moscatiello F, Herrero Jover J, González Ballester M A, Carreño Hernández E, Piombino P, Califano L. Preoperative digital three-dimensional planning for rhinoplasty. Aesthetic Plast Surg. 2010;34(02):232–238. doi: 10.1007/s00266-009-9455-4. [DOI] [PubMed] [Google Scholar]
- 21.Lekakis G, Claes P, Hamilton G S, III, Hellings P W. Evolution of preoperative rhinoplasty consult by computer imaging. Facial Plast Surg. 2016;32(01):80–87. doi: 10.1055/s-0035-1570125. [DOI] [PubMed] [Google Scholar]
- 22.Gunther S, Guyuron B. Economizing the septal cartilage for grafts during rhinoplasty, 40 years' experience. Aesthetic Plast Surg. 2021;45(01):224–228. doi: 10.1007/s00266-020-01894-w. [DOI] [PubMed] [Google Scholar]
- 23.Cárdenas-Camarena L, Guerrero M T. Use of cartilaginous autografts in nasal surgery: 8 years of experience. Plast Reconstr Surg. 1999;103(03):1003–1014. doi: 10.1097/00006534-199903000-00039. [DOI] [PubMed] [Google Scholar]
- 24.Harris S, Pan Y, Peterson R, Stal S, Spira M. Cartilage warping: An experimental model. Plast Reconstr Surg. 1993;92(05):912–915. [PubMed] [Google Scholar]
- 25.Gunter J P, Clark C P, Friedman R M. Internal stabilization of autogenous rib cartilage grafts in rhinoplasty: a barrier to cartilage warping. Plast Reconstr Surg. 1997;100(01):161–169. doi: 10.1097/00006534-199707000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Lopez M A, Shah A R, Westine J G, O'Grady K, Toriumi D M. Analysis of the physical properties of costal cartilage in a porcine model. Arch Facial Plast Surg. 2007;9(01):35–39. doi: 10.1001/archfaci.9.1.35. [DOI] [PubMed] [Google Scholar]
- 27.Gibson T, Davis W B. The distortion of autogenous cartilage grafts: its cause and prevention. Br J Plast Surg. 1957;10:257–274. [Google Scholar]
- 28.Mohan R, Shanmuga Krishnan R R, Rohrich R J. Role of fresh frozen cartilage in revision rhinoplasty. Plast Reconstr Surg. 2019;144(03):614–622. doi: 10.1097/PRS.0000000000005996. [DOI] [PubMed] [Google Scholar]
- 29.Lee M, Unger J G, Gryskiewicz J, Rohrich R J. Current clinical practices of the Rhinoplasty Society members. Ann Plast Surg. 2013;71(05):453–455. doi: 10.1097/SAP.0b013e3182503ca1. [DOI] [PubMed] [Google Scholar]
- 30.Toriumi D M, Bared A. Revision of the surgically overshortened nose. Facial Plast Surg. 2012;28(04):407–416. doi: 10.1055/s-0032-1319835. [DOI] [PubMed] [Google Scholar]
- 31.Kamer F M, Churukian M M. High septal hemitransfixion for the correction of caudal septal deformities. Laryngoscope. 1984;94(03):391–394. doi: 10.1288/00005537-198403000-00017. [DOI] [PubMed] [Google Scholar]
- 32.Daniel R K. Berlin Heidelberg: Springer; 2010. Mastering Rhinoplasty. [Google Scholar]
- 33.Youssef A, Ahmed S, Ibrahim A A, Daniel M, Abdelfattah H M, Morsi H. Traumatic cerebrospinal fluid leakage following septorhinoplasty. Arch Plast Surg. 2018;45(04):379–383. doi: 10.5999/aps.2017.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Unger J, Roostaeian J, Cheng D. The open approach in secondary rhinoplasty: choosing an incision regardless of prior placement. Plast Reconstr Surg. 2013;132(04):780–786. doi: 10.1097/PRS.0b013e31829ad339. [DOI] [PubMed] [Google Scholar]
- 35.Barone M, Cogliandro A, Salzillo R. The role of skin thickness in the choice of a rhinoplasty technique for thin-skinned patients: analysis of long-term results and patient satisfaction. Aesthetic Plast Surg. 2020;44(05):1742–1750. doi: 10.1007/s00266-020-01763-6. [DOI] [PubMed] [Google Scholar]
- 36.Cobo R, Camacho J G, Orrego J. Integrated management of the thick-skinned rhinoplasty patient. Facial Plast Surg. 2018;34(01):3–8. doi: 10.1055/s-0037-1617445. [DOI] [PubMed] [Google Scholar]
- 37.Cochran C S, Ducic Y, Defatta R J. Rethinking nasal osteotomies: an anatomic approach. Laryngoscope. 2007;117(04):662–667. doi: 10.1097/MLG.0b013e318030e3ff. [DOI] [PubMed] [Google Scholar]
- 38.Sheen J H. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984;73(02):230–237. [PubMed] [Google Scholar]
- 39.Foda H MT. Rhinoplasty for the multiply revised nose. Am J Otolaryngol. 2005;26(01):28–34. doi: 10.1016/j.amjoto.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 40.Teymoortash A, Fasunla J A, Sazgar A A, Fasunla J, Sazgar A. The value of spreader grafts in rhinoplasty: a critical review. Eur Arch Otorhinolaryngol. 2012;269(05):1411–1416. doi: 10.1007/s00405-011-1837-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gunter J P, Yu Y L. The tripod concept for correcting nasal-tip cartilages. Aesthet Surg J. 2004;24(03):257–260. doi: 10.1016/j.asj.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 42.Larrabee W F., Jr The tripod concept. Arch Otolaryngol Head Neck Surg. 1989;115(10):1168–1169. doi: 10.1001/archotol.1989.01860340022011. [DOI] [PubMed] [Google Scholar]
- 43.Kridel R WH, Konior R J. Controlled nasal tip rotation via the lateral crural overlay technique. Arch Otolaryngol Head Neck Surg. 1991;117(04):411–415. doi: 10.1001/archotol.1991.01870160065011. [DOI] [PubMed] [Google Scholar]
- 44.Ghavami A, Janis J E, Acikel C, Rohrich R J. Tip shaping in primary rhinoplasty: an algorithmic approach. Plast Reconstr Surg. 2008;122(04):1229–1241. doi: 10.1097/PRS.0b013e31817d5f7d. [DOI] [PubMed] [Google Scholar]
- 45.Kridel R WH, Yoon P J, Koch R J. Prevention and correction of nasal tip bossae in rhinoplasty. Arch Facial Plast Surg. 2003;5(05):416–422. doi: 10.1001/archfaci.5.5.416. [DOI] [PubMed] [Google Scholar]
- 46.Rohrich R, Raniere J, Ha R. The alar contour graft: correction and prevention of alar rim deformities in rhinoplasty. Plast Reconstr Surg. 2002;109(07):2495–2505. doi: 10.1097/00006534-200206000-00050. [DOI] [PubMed] [Google Scholar]
- 47.Kridel R WH, Scott B A, Foda H MT.The tongue-in-groove technique in septorhinoplasty. A 10-year experience Arch Facial Plast Surg 1999104246–256., discussion 257–258 [DOI] [PubMed] [Google Scholar]
- 48.Daniel R K. Rhinoplasty: dorsal grafts and the designer dorsum. Clin Plast Surg. 2010;37(02):293–300. doi: 10.1016/j.cps.2009.12.009. [DOI] [PubMed] [Google Scholar]


