Abstract
Body contouring procedures are highly impactful because of their potential to improve a patient's quality of life. These procedures, particularly when performed on patients following massive weight loss, may require secondary intervention to treat residual contour abnormalities. Presently, there is a paucity of information in the literature detailing the avoidance and correction of body contouring deformities. Herein, we will discuss the management of patients seeking revisional body contouring procedures.
Keywords: plastic surgery, body contouring, surgical revision, abdominoplasty, aesthetics
Patients who have lost large amounts of weight secondary to healthy lifestyle changes or bariatric surgery may suffer from a wide variety of contour irregularities that can be a source of significant functional and psychosocial impairment. 1 2 3 4 5 As a result, body contouring is no longer just an artform but rather a therapeutic science geared toward improving a patient's quality of life. Despite their efficacy, body contouring procedures are imperfect in nature, requiring secondary intervention in some patients to treat residual contour irregularities. Secondary body contouring procedures come with their own set of unique challenges necessitating modification by the surgeon when caring for this subset of patients. Herein, we will discuss the management of patients seeking revisional body contouring procedures.
Preoperative Evaluation
Preoperative evaluation of patients seeking revisional surgery is equally as important as the secondary procedure itself. The plastic surgeon must facilitate an open discussion regarding the patient's concerns and expectations in an empathetic and nonjudgmental manner. 6 This is highly important when managing patients seeking revisional surgery as their outlook toward body contouring may have been sullied by their previous procedure. Furthermore, discordance between the expectations held by the surgeon and patient regarding outcomes is a frequent source of patient dissatisfaction, which may result in further revisional surgery or litigation. 7 8
Surgeons should collect a thorough patient history during the preoperative evaluation to assess the patient's candidacy for revision body contouring. Common comorbidities that increase the risk of adverse outcomes include cardiovascular disease, upper and lower airway disease, renal disease, and diabetes. 9 Additionally, the surgeon must be proficient in screening for pathologies of the hematological system as a hypercoagulable state increases the risk of venous thrombosis during and after surgery. 10 11 Smoking of tobacco products, particularly cigarettes, has been proven to increase the likelihood of surgical site infection and wound healing complications by two- and threefold, respectively. 12 Surgeons are recommended to prescribe smoking cessation 4 to 6 weeks prior to surgery as it can reduce the incidence of surgical site infections by 60% and wound healing complications by 52%. 13
Collecting a comprehensive history of the patient's weight and body mass index (BMI) during the preoperative evaluation is highly important when caring for massive weight loss (MWL) patients. Weight stability should be reached prior to undergoing body contouring surgery as this may result in the patient undergoing potentially unnecessary revisional surgery at a later date. 14 15 16 It is preferable to operate on patients with BMIs of under 30 as these patients have significant reductions in surgical complications; however, 45% of MWL patients stabilize at BMIs greater than 30. 17 In these cases, surgeons must be judicious in their selection of surgical candidates to ensure that the benefits of treating a functional impairment outweigh the increased risk of surgical complications. 17
Patients with prior bariatric surgery frequently develop severe protein deficiencies and microcytic anemia, both of which increase the risk of complications due to their detrimental effects on wound healing. 15 18 19 As a result, 29% to 35% of MWL patients experience wound healing–related complications that may require future revisional surgery. 17 20 A patient's nutritional status can be gauged by both their BMI and laboratory testing, with the latter providing information that can aid in nutritional supplementation should it be needed. A patient's nutritional status for protein macronutrients is best measured using prealbumin, given its short half-life and consistency across varying levels of hydration. 21
General Principles
Revision body contouring can be performed using a wide variety of treatment modalities with treatment selection being heavily dependent on the type and severity of a patient's contour irregularity. Common concerns of patients seeking out revision body contouring include residual or intrinsic skin laxity or soft-tissue excess, malpositioned anatomic landmarks or surgical scars, aesthetically displeasing postoperative scarring, and dog ear deformities. 22 23 24 25
Skin Laxity and Soft-Tissue Excess
Deficiencies in preoperative planning and inappropriate technical selection are frequently responsible for under- or overcorrection of redundant skin and subcutaneous fat. When evaluating patients, the surgeon must conceptualize both skin tone and soft-tissue excess as separate entities. Failure to do so became evident in the early years of liposuction wherein many patients demonstrated evidence of increased skin laxity following their procedure. 26 Additionally, failure to understand the limitations of a procedure can also result in undesirable outcomes. For example, MWL patients with profound skin laxity and soft-tissue excess of the lateral abdomen would have limited correction of their contour irregularity should they be treated with traditional abdominoplasty rather than a vertical abdominoplasty. 27 Classification systems with algorithmic approaches for treating specific contour irregularities, such as the Pittsburg rating scale, are powerful tools for developing treatment plans that minimize the risk for further revisional surgery. 28 29
Redundant skin and subcutaneous fat following a primary body contouring procedure can be due to a multitude of factors. Natural changes to the integument and subcutaneous tissue due to aging can result in exacerbation of contour irregularities, often requiring revisional surgery. Thinning of the epidermis and dermis and a decrease in the number of fibroblasts located within the dermis result in lower collagen and elastin turnover, producing significant skin laxity. 30
Location of Anatomic Landmarks and Scars
Malposition of anatomic landmarks and scars following the primary surgery is often the manifestation of suboptimal presurgical planning for an excisional or body lift procedure. 25 When planning any procedure, the surgeon must account for the mechanical forces acting upon adjacent anatomic landmarks and scars as some level of transposition is expected postoperatively. 16 Correction of malpositioned landmarks and scars is best treated with secondary surgery, though the suitability of this intervention is highly dependent on the amount of residual laxity.
Postoperative Scarring
Aesthetically displeasing postoperative scarring frequently results in patients seeking out revisional surgery. As such, proper patient selection, meticulous wound closure, and prophylactic intervention are key to minimizing the risk of future scar revision. Patients who are nutrient-deficient, smoke cigarettes, or have diabetes are at risk for the development of widened or hypertrophic scars due to the detrimental effects these factors have on wound healing. 31 Additionally, patients with darker skin tones are susceptible to hypertrophic scarring. 31
Minimizing the amount of tension imposed on the skin through proper scar placement and layered wound closure greatly reduces the risk of producing wide or hypertrophic scars postoperatively, though this may also be an unavoidable consequence of certain body contouring procedures. 32 For example, the substantial tensile force imposed on the scar site following brachioplasty has the potential of causing undesirable scarring. In cases such as these, surgeons should inform the patient of these outcomes prior to surgery and place the scar where it can be minimally visualized should unappealing scarring occur.
Treatment of scar tissue can range from noninvasive mechanical therapy to outright excision of the scar. A more in-depth discussion regarding revisions of scar tissue is presented in this issue of Seminars in Plastic Surgery [Scar Revisions by Skochdopole et al]; however, we will highlight several noninvasive treatment modalities employed for scar management. Mechanical therapies such as scar massage, compression garments, and silicone gel sheets are noninvasive and may be used for prevention and treatment of postoperative scarring. 33 While there is limited evidence validating the anecdotal efficacy of scar massage and compression garments, silicone gel sheets have demonstrated significant efficacy as a prophylactic and therapeutic agent. 31 33 34 35 Laser therapy, both ablative and nonablative, may also be used to treat postoperative scarring. 31 35 36 Nonablative laser therapies, such as pulsed dye lasers, function by disrupting the vascular blood supply to the scar tissue to decrease its size, while ablative therapies, such as CO 2 lasers, induce rearrangement of collagen in the scar by inducing dermal injury through the direct transfer of energy. 37 While optimal laser selection for different types of scars is still being investigated, both pulsed dye and CO 2 lasers have been shown to be effective for treatment of hypertrophic scars. 31
Dog Ear Deformities
Dog ear deformities that do not resolve spontaneously following the patient's primary body contouring procedure require revisional surgery. Small dog ear deformities may be treatable with liposuction alone or by anchoring its margins to the deep fascial plane with suture. 38 39 Larger conical deformities require excision of the dog ear and lengthening of the scar with or without the use of liposuction. 38
Liposuction and Fat Grafting
In addition to treating small areas of residual adiposity, liposuction may be used in secondary excisional and body lift surgical procedures for releasing postoperative adhesions and fascial zones of adherence, respectively. 40 41 42 Liposuction as a standalone therapy is unable to effectively address moderate-to-severe redundancies of skin and soft tissue nor is it able to reposition incorrectly placed anatomic landmarks or scars. 28 29
Power-assisted liposuction (PAL) and ultrasound-assisted liposuction (UAL) have arisen as popular technical modifications of conventional suction-assisted liposuction (SAL). Both PAL and UAL have high utility in patients undergoing revisional liposuction, as disruption of postoperative adhesions using conventional SAL is a source of surgeon fatigue. 42 While highly effective at liposculpting, complications such as subcutaneous burns and relatively high rates of seroma formation make the prospect of using UAL undesirable to some surgeons. 43 44 VASER-assisted liposuction entails the use of third-generation ultrasound technologies that employ pulsatile bursts of ultrasonic energy, thereby minimizing the risk of thermal injury to the skin and subcutaneous tissue. 45 In addition to its improved safety profile, VASER-assisted liposuction demonstrated a 53% improvement in skin retraction and a 26% reduction in blood loss when compared with conventional SAL, potentially reducing the need for further revisional procedures. 45
SAFE liposuction, described by Wall Jr., is a highly regarded approach to circumferential SAL for mild-to-moderate soft-tissue excess. 46 47 The first two phases of SAFE liposuction, fat separation and aspiration, minimize the risk of suction-induced avulsion injury to the vasculature, while the final phase, fat equalization, provides a thin fatty layer to facilitate postoperative wound healing and to minimize the formation of postoperative adhesions. 46 47 Using this methodology, Wall Jr. was able to achieve a complication rate of 3% (all seromas) without any patients requiring further truncal body contouring. 46
When compared with more invasive body contouring procedures, liposuction produces minimal scarring and results in rapid postoperative recovery; however, the technique is not without its shortcomings. 48 Postoperative contour irregularities frequently observed in patients undergoing liposuction include residual skin laxity, under- or overresection, cannula line deformities, and puckered scars at the incision site. Skin laxity following lipoaspiration is a result of either poor skin retraction following surgery or inappropriate use of liposuction monotherapy in a patient who was better suited for excisional or body lift surgical procedures. 26 28 29 Cannula line deformities are the manifestation of superficial liposuction and are best avoided by targeting deeper fatty tissue. 49 Depressions and puckered scar tissue at the incision site are the result of excessive lipoaspiration and failing to turn the suction off prior to inserting or retracting the cannula, respectively. 49 Cannula line deformities or depressions at the incision site are best treated with autologous fat grafting (AFG) should they not spontaneously resolve. 42 49
Seroma formation is one postoperative complication of liposuction, especially when combined with excisional surgery, occurring in 3% to 19% of patients. 46 50 51 Proper technique, use of progressive tension sutures and/or drains, and employment of compression garments are all ways surgeons can reduce the risk of seroma formation in patients undergoing liposuction. 44 49
AFG is frequently employed to treat soft-tissue deformities and to improve contour. 40 41 52 Resorption of fatty tissue is the most common complication associated with AFG and occurs in around 45% to 48% of patients. 52 53 54 55 While resorption is unpredictable, the literature suggests that maintaining the viability of adipocyte-derived stem cells by using proper technique will help lower the risk of graft loss. 56 Surgeons may overcorrect areas with fat graft in anticipation of resorption; however, surgeons should not overindulge in this practice as this may result in central necrosis of the graft. 56
Upper Extremity
Body contouring procedures of the upper extremity are frequently employed to treat ptosis and soft-tissue excess of the arm. These contour irregularities are corrected using liposuction or brachioplasty with or without liposuction. Prior to the development of treatment algorithms for upper extremity body contouring, liposuction monotherapy was associated with poor aesthetic outcomes, with 22% of patients reporting dissatisfaction with their procedure citing postoperative skin laxity as the primary cause for dissatisfaction. 26 Since then, several treatment algorithms have been developed to prevent such problems. 28 29 In 2005, El Khatib designed a treatment algorithm which recommended that SAL monotherapy be exclusively used in patients with mild-to-moderate soft-tissue excess with minimal ptosis. 29 Using this methodology, only 5% of the author's patients had notable skin laxity following their procedure. 29
Patients with severe soft-tissue excess and moderate-to-severe ptosis are best treated with brachioplasty techniques. 29 In short, brachioplasty is a technique that improves the contour of the arm by resecting superfluous skin and subcutaneous tissue down to the muscular aponeurosis with subsequent closure of the wound margins. 57 Despite the procedure's efficacy, up to 29% of patients undergoing brachioplasty have complications, with 21% of patients seeking revisional surgery. 58 The majority of patients seeking revisional surgery following brachioplasty seek treatment for undercorrection of their primary contour irregularity or aesthetically displeasing scarring. 58
Poor excisional design is a frequent cause for undercorrection of redundant skin and subcutaneous fat during primary brachioplasty occurring in about 12% of patients. 59 This may be seen in patients who are treated using a small, transverse scar in an attempt to minimize the size of the final scar. Wide and thick scarring is frequently seen postoperatively in patients who undergo brachioplasty, with 11% to 41% of patients developing hypertrophic scar tissue. 58 59 In contrast to other contour irregularities, aesthetically displeasing scars following brachioplasty are largely unavoidable due to the magnitude of the tensile forces imposed on the incision site. 60 61 62 Plastic surgeons largely compensate for this complication by placing the scar where it is least visible. Plastic surgeons typically place brachioplasty scars in the medial, posterior, or posteromedial position, with the latter becoming increasingly popular due to its perceived superiority in hiding the brachioplasty scar. 63 64 Recently, evidence has arisen that the posteromedial scar position allows for improved scar healing. 64 In a study conducted by Simone et al, posteromedial scars exhibited shorter displacement and were found to be under decreased tensile stress when compared with scars placed along the bicipital groove. 64 In instances where the scar has displaced significantly, an elliptical resection of the scar tissue can be used to reposition the scar line should sufficient laxity exist.
Inability to close the wound margins during brachioplasty and postoperative wound dehiscence are two severe complications associated with the procedure. Segmental closure of the wound margins early into the resection is vital to ensuring that the wound can be closed because the nonresected skin becomes rapidly edematous following resection. 50 62 Wound dehiscence occurs in approximately 3% to 23% of patients who undergo brachioplasty for reasons similar to that of aesthetically displeasing scars. 58 59 Many patients have wound dehiscence at the axillary component of the incision line due to the wide range of motion exhibited by the glenohumeral joint. Layered closure of wound edges and strict movement restrictions minimize the risk of dehiscence.
The median antebrachial cutaneous nerve is highly susceptible to injury during brachioplasty, with injury resulting in loss of sensation to the medial aspect of the arm. 50 62 63 Injury to the nerve is largely avoided by identifying it prior to resection. The nerve is best visualized at the distal aspect of the medial arm where it travels superficial to the brachial fascia after piercing through it 10 cm proximal to the medial epicondyle. 65 Avulsion brachioplasty, described by Knotts et al, is a technical alternative to conventional brachioplasty that greatly reduces the risk of injuring such neurovascular structures. 63 Like liposuction-assisted brachioplasty, avulsion brachioplasty uses liposuction to treat soft-tissue excess in the arm; however, the resultant skin laxity is avulsed off of the arm as opposed to excised, thereby eliminating the risk of transecting the underlying neurovascular structures during the procedure. 63
Extension of the conventional brachioplasty to the lateral trunk allows the surgeon to treat patterns of skin laxity and soft-tissue excess of the axilla and lateral chest wall seen in MWL patients. Laxity of the lateral chest wall, in particular, can result in an inferior displacement of the lateral aspect of the inframammary fold. L-brachioplasty, described by Hurwitz and Holland, extends the excision of the conventional brachioplasty to include both the axilla and lateral chest wall by making an inverse-L excision ( Fig. 1 ). This technique, when used in conjunction with excision of upper back rolls, is able to elevate the inframammary fold to aid in breast reconstruction. 60 66 67
Fig. 1.
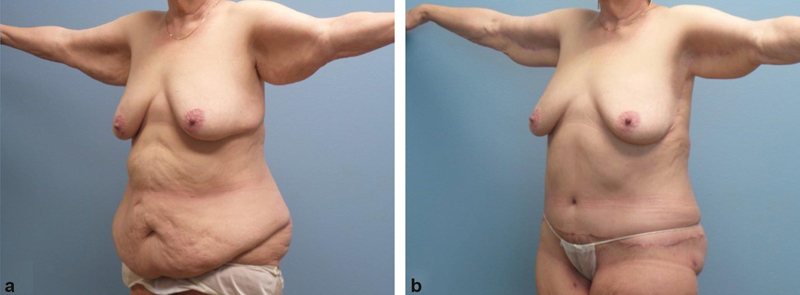
A 71-year-old patient before ( a ) and after ( b ) undergoing primary abdominoplasty and brachioplasty. Note how extending the brachioplasty excision into the axilla and lateral chest wall is able to correct the inferiorly displaced lateral aspect of the inframammary fold in addition to modest correction of the patient's upper extremity ptosis.
Lower Trunk
Body contouring procedures of the lower trunk are among the most frequently performed aesthetic surgeries in the United States, with abdominal liposuction and abdominoplasty being most frequently performed. 68 Despite the many advances in abdominal body contouring surgery, secondary surgical procedures are performed in 13% to 28% of patients. 69 70 Technical selection for revisional surgery of the abdomen is largely determined by the patient's presentation; however, plastic surgeons must account for changes in the vasculature of the abdominal wall following the primary body contouring procedure. 71
Patients with a history of abdominal surgery with extensive undermining, such as abdominoplasty, have varying levels of disruption to the vasculature of the abdominal wall and overlying tissue. This is particularly important as the majority of patients undergoing secondary abdominoplasty were initially treated with abdominoplasty for their primary intervention. 23 69 Huger zone II, the vascular system that supplies the inferior abdomen, is largely sacrificed by all abdominoplasty techniques; however, Huger zone I, the vascular supply of the midline abdomen, is variably affected depending on the level of undermining performed. 72 Similarly, the blood supply to the umbilicus may be altered due to transection of the umbilical stalk or compression of the stalk by a large umbilical hernia. 73 In these cases, the surgeon must take extra measures to minimize the risk of umbilical necrosis during the secondary abdominoplasty. Parsa et al found success in delaying the umbilicus 2 weeks prior to secondary abdominoplasty. This measure augments the umbilical blood supply of the underlying subcutaneous fat and fascia, providing the best chance of umbilical survival. 73 Should patients present with umbilical necrosis following primary abdominoplasty or flap delay, a neoumbilicus can be reconstructed during secondary abdominoplasty. 74
Secondary liposuction may be used as a standalone or adjuvant therapy for treating soft-tissue excess. Standalone liposuction has utility in treating mild soft-tissue excess, particularly at the lateral aspect of the abdominal wall and flanks. 71 Patients undergoing liposuction of the upper abdomen in conjunction with secondary abdominoplasty can do so in a safer manner than primary abdominoplasty because of the delay phenomenon.
Patients with residual mild, infraumbilical vertical skin laxity and soft-tissue excess may be treated with direct excision with or without adjuvant liposuction. 75 Vertical abdominoplasty techniques, such as the fleur-de-lis and corset abdominoplasty, are indicated for patients with severe vertical and horizontal skin laxity and soft-tissue excess ( Fig. 2 ). 2 Most patients undergoing this technique as a revisional procedure exhibit extensive horizontal laxity due to improper technical selection during the primary procedure. Vertical abdominoplasty produces midline vertical scar; however, removal of extensive soft-tissue excess is prioritized over scar aesthetics in these cases. Bilateral vertical flank incisions can also be utilized to avoid the midline abdominal scar. Liposuction can be safely performed with traditional abdominoplasty; however, the surgeon must preserve a single deep superior epigastric artery perforator bilaterally to avoid flap necrosis. 51 72
Fig. 2.

A 35-year-old patient with soft-tissue excess of the abdomen ( a, b ) who was treated with fleur-de-lis abdominoplasty and rectus diastasis repair. The patient's procedure was complicated by seroma formation postoperatively ( c, d ) and was subsequently treated with surgical excision of the seroma ( e, f ).
Patients with a high-riding transverse scar or a mispositioned umbilicus frequently seek out revisional surgery. Both contour irregularities are best treated with secondary abdominoplasty, though this may not be possible due to insufficient skin laxity. 25 For optimal cosmesis, the nadir of the transverse abdominoplasty scar should be placed 6 to 9 cm superior to the anterior vulvar commissure (or penile base in men) and should extend in superolateral fashion to a point just inferior to the anterior superior iliac spine. 25 76 Patients with insufficient abdominal laxity for repeat abdominoplasty are best served By undergoing noninvasive treatment modalities for scar revision. 25
For optimal aesthetic results, the umbilicus should be located in the area between the midpoint and the intersection between the upper two-thirds and lower one-third of an imaginary line extending from the xyphoid to pubic symphysis ( Fig. 3 ). 75 It should be noted, however, that the umbilicus is rarely midline, with more than 55% of patients exhibiting lateral deviation of umbilicus by 2% or more of the transverse length of the abdominal wall. 77 Selecting the new positioning of the umbilicus is heavily dependent on the native location of the umbilicus, the amount of surrounding abdominal laxity, and the status of its vascular supply. 73 75 In patients with a viable umbilical stalk and sufficient skin laxity, the umbilicus can be transposed via secondary abdominoplasty, though a vertical scar will be necessary should there be significant cranial transposition of the umbilicus during the procedure. 25 Additionally, patients with a high-riding umbilicus may have their umbilicus “floated” inferiorly, though this allows for shorter transposition than traditional abdominoplasty. 73 75 A neoumbilicus may also be created in cases of disfigurement or absence of the umbilicus due to previous compromise from surgery. This new umbilicus is formed in the ideal location from neighboring abdominal skin and soft tissue. 78
Fig. 3.
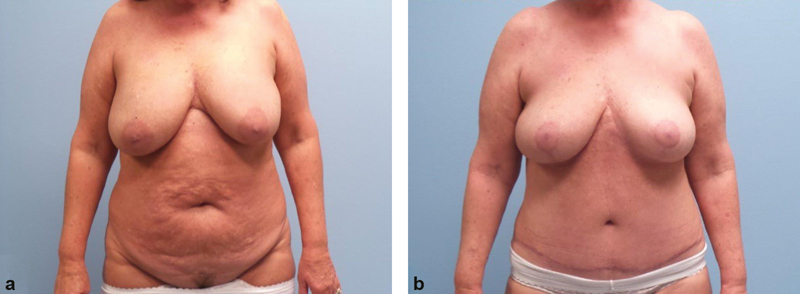
A 59-year-old patient before ( a ) and after ( b ) undergoing abdominoplasty and reduction mammaplasty. Note that the umbilicus is located in the area between the midpoint and the intersection between the upper two-thirds and lower one-third of an imaginary line extending from the xyphoid process to the pubic symphysis.
Patients may also undergo secondary abdominoplasty for the treatment of residual or previously untreated rectus diastasis. Rectus diastasis is characterized by aponeurotic laxity of the linea alba as a result of chronic distention or congenital weakness of the abdominal wall. 79 Most frequently, rectus diastasis presents as a centrally located epigastric bulge in a patient with a history of truncal obesity or pregnancy; however, patients can present with abdominal pain or discomfort, back pain, or urogynecological symptoms in rare cases. 79 80 Plication of the rectus sheath is the gold standard treatment for rectus diastasis. There are several techniques that may be employed for rectus diastasis repair, though plastic surgeons typically use an open approach (via abdominoplasty) and plicate the anterior rectus sheath. Recurrence of rectus diastasis is uncommon following plication, with studies reporting recurrence in only 0% to 4% of patients. 80 81 82
Lower Body
Lower body lift procedures are powerful tools for correcting the significant skin laxity and soft-tissue excess observed in the lower extremity and trunk of MWL patients. Ted Lockwood, the visionary behind the lower body lift, emulated the principles of the modern facelift by incorporating fascial suspension to the lower extremity and trunk. 27 83 Since first described, the circumferential lower body lift has evolved substantially, with many centers developing their own approaches to these challenging cases. 84 Despite the procedure's innate ability to correct superfluous tissue of the trunk and lower body, 42% to 78% of patients experience complications, with wound dehiscence and seroma formation being most common ( Fig. 4 ). 85 86 87 These complications, along with the unpredictable nature of skin and soft tissue in MWL patients, are responsible for the procedure's associated 8% to 28% revision rate. 88 89 90
Fig. 4.

A 59-year-old patient before ( a, b ) and after ( c, d ) undergoing fleur-de-lis abdominoplasty, circumferential lower body lift, and medial thigh lift. The medial aspect of the patient's left and right lower extremities exhibited fullness postoperatively secondary to seroma formation and residual soft-tissue excess, respectively. A natural contour was achieved by excising the seroma of the left lower extremity and performing liposuction of the right lower extremity ( e, f ).
Residual laxity and soft-tissue excess are frequently observed in patients following a circumferential lower body lift procedure ( Fig. 5 ). Residual or relapsed tissue excess of the lateral thigh at the level of the inferior gluteal fold, also known as a saddlebag deformity, occurs in around 8% of patients postoperatively. This deformity is most effectively treated with a secondary lateral thigh lift. 89 Abducting the leg during the primary procedure maximizes the amount of tissue excised and may decrease the likelihood of the patient developing a postoperative saddlebag deformity. 91 92
Fig. 5.

A 71-year-old patient before ( a–c ) and after ( d–f ) undergoing a staged circumferential lower body lift and medial thigh lift for correction of excess skin at the medial and lateral aspects of her lower extremities. Note how the patient's body lift procedures were successful in removing excess skin; however, they were unable to correct intrinsic skin laxity as evidenced by cellulite pre- and postoperatively.
Gluteal autoaugmentation is often incorporated into the circumferential lower body lift to restore the volume and projection of the buttocks that is lost in MWL patients. 89 Flap transposition can be used to rejuvenate the buttocks; however, these techniques do not restore volume to its lateral aspect and have variable efficacy overall. 89 AFG is frequently employed for gluteal autoaugmentation as a secondary surgery. In contrast to flap transposition techniques, AFG can effectively treat the superior and lateral aspects of the buttocks, thereby giving the patient an hourglass shape. 93 When performing gluteal autoaugmentation with AFG, the surgeon should stay clear of the imaginary triangle formed by the intragluteal cleft apex and medial third of the buttocks bilaterally. 93 This region, aptly named the “danger zone,” should be avoided due to the high density of neurovascular structures within it. 93 Lastly, surgeons should remain in the subcutaneous plane when performing this procedure to avoid the risk of fat embolism. 89 93 94
Conclusion
Body contouring procedures are high-impact therapies with the potential to significantly improve a patient's quality of life. While these procedures have been demonstrated to be highly efficacious, complication rates are high, with many patients requiring revisional surgery. Technical selection, if surgery is indicated, is highly dependent on the patient's contour irregularity. Plastic surgeons must also consider postsurgical changes to the patient's anatomy following the primary procedure. While highly prevalent in the field of plastic surgery, revision body contouring is severely underrepresented in the literature. We encourage plastic surgeons to publish their experiences with these procedures so that we may achieve the best outcomes for our patients going forward.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Toma T, Harling L, Athanasiou T, Darzi A, Ashrafian H. Does body contouring after bariatric weight loss enhance quality of life? A systematic review of QOL studies. Obes Surg. 2018;28(10):3333–3341. doi: 10.1007/s11695-018-3323-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Almutairi K, Gusenoff J A, Rubin J P. Body contouring. Plast Reconstr Surg. 2016;137(03):586e–602e. doi: 10.1097/PRS.0000000000002140. [DOI] [PubMed] [Google Scholar]
- 3.Hammond D C, Chandler A R, Baca M E, Li Y K, Lynn J V. Abdominoplasty in the overweight and obese population: Outcomes and patient satisfaction. Plast Reconstr Surg. 2019;144(04):847–853. doi: 10.1097/PRS.0000000000006018. [DOI] [PubMed] [Google Scholar]
- 4.Hunecke P, Toll M, Mann O, Izbicki J R, Blessmann M, Grupp K. Clinical outcome of patients undergoing abdominoplasty after massive weight loss. Surg Obes Relat Dis. 2019;15(08):1362–1366. doi: 10.1016/j.soard.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs J M, Schechner S, Jacobs J S. Abdominoplasty following massive weight loss. Semin Plast Surg. 2006;20(01):15–23. [Google Scholar]
- 6.Sachdev M, Britto G R. Essential requirements to setting up an aesthetic practice. J Cutan Aesthet Surg. 2014;7(03):167–169. doi: 10.4103/0974-2077.146675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paik A M, Mady L J, Sood A, Lee E S. Beyond the operating room: a look at legal liability in body contouring procedures. Aesthet Surg J. 2014;34(01):106–113. doi: 10.1177/1090820X13513459. [DOI] [PubMed] [Google Scholar]
- 8.Therattil P J, Chung S, Sood A, Granick M S, Lee E S. An analysis of malpractice litigation and expert witnesses in plastic surgery. Eplasty. 2017;17:e30. [PMC free article] [PubMed] [Google Scholar]
- 9.Ning C, Hu X, Liu F. Post-surgical outcomes of patients with chronic kidney disease and end stage renal disease undergoing radical prostatectomy: 10-year results from the US National Inpatient Sample. BMC Nephrol. 2019;20(01):278. doi: 10.1186/s12882-019-1455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedman T, O'Brien Coon D, Michaels V J. Hereditary coagulopathies: practical diagnosis and management for the plastic surgeon. Plast Reconstr Surg. 2010;125(05):1544–1552. doi: 10.1097/PRS.0b013e3181d51344. [DOI] [PubMed] [Google Scholar]
- 11.Nakashima M O, Rogers H J. Hypercoagulable states: an algorithmic approach to laboratory testing and update on monitoring of direct oral anticoagulants. Blood Res. 2014;49(02):85–94. doi: 10.5045/br.2014.49.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rinker B. The evils of nicotine: an evidence-based guide to smoking and plastic surgery. Ann Plast Surg. 2013;70(05):599–605. doi: 10.1097/SAP.0b013e3182764fcd. [DOI] [PubMed] [Google Scholar]
- 13.Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert J O. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med. 2011;124(02):144–1.54E10. doi: 10.1016/j.amjmed.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Naghshineh N, Rubin J P. Preoperative evaluation of the body contouring patient: the cornerstone of patient safety. Clin Plast Surg. 2014;41(04):637–643. doi: 10.1016/j.cps.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Brower J P, Rubin J P. Abdominoplasty after massive weight loss. Clin Plast Surg. 2020;47(03):389–396. doi: 10.1016/j.cps.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Shrivastava P, Aggarwal A, Khazanchi R K.Body contouring surgery in a massive weight loss patient: an overview Indian J Plast Surg 200841(Suppl):S114–S129. [PMC free article] [PubMed] [Google Scholar]
- 17.Coon D, Gusenoff J A, Kannan N, El Khoudary S R, Naghshineh N, Rubin J P. Body mass and surgical complications in the postbariatric reconstructive patient: analysis of 511 cases. Ann Surg. 2009;249(03):397–401. doi: 10.1097/SLA.0b013e318196d0c6. [DOI] [PubMed] [Google Scholar]
- 18.Bal B S, Finelli F C, Shope T R, Koch T R. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8(09):544–556. doi: 10.1038/nrendo.2012.48. [DOI] [PubMed] [Google Scholar]
- 19.Agha-Mohammadi S, Hurwitz D J. Nutritional deficiency of post-bariatric surgery body contouring patients: what every plastic surgeon should know. Plast Reconstr Surg. 2008;122(02):604–613. doi: 10.1097/PRS.0b013e31817d6023. [DOI] [PubMed] [Google Scholar]
- 20.Staalesen T, Olsén M F, Elander A. Complications of abdominoplasty after weight loss as a result of bariatric surgery or dieting/postpregnancy. J Plast Surg Hand Surg. 2012;46(06):416–420. doi: 10.3109/2000656X.2012.717898. [DOI] [PubMed] [Google Scholar]
- 21.Beck F K, Rosenthal T C.Prealbumin: a marker for nutritional evaluation[Published correction appears in Am Fam Physician 2002 Dec 15;66(12):2208]Am Fam Physician 200265081575–1578. [PubMed] [Google Scholar]
- 22.Sinno S, Chang J B, Brownstone N D, Saadeh P B, Wall S., Jr Determining the safety and efficacy of gluteal augmentation: a systematic review of outcomes and complications. Plast Reconstr Surg. 2016;137(04):1151–1156. doi: 10.1097/PRS.0000000000002005. [DOI] [PubMed] [Google Scholar]
- 23.Matarasso A, Wallach S G, Rankin M, Galiano R D. Secondary abdominal contour surgery: a review of early and late reoperative surgery. Plast Reconstr Surg. 2005;115(02):627–632. doi: 10.1097/01.prs.0000150154.36846.7b. [DOI] [PubMed] [Google Scholar]
- 24.Gusenoff J A. Prevention and management of complications in body contouring surgery. Clin Plast Surg. 2014;41(04):805–818. doi: 10.1016/j.cps.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Cormenzana P. Revision abdominoplasty and proper umbilical positioning. Clin Plast Surg. 2010;37(03):541–546. doi: 10.1016/j.cps.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Pitman G H, Teimourian B. Suction lipectomy: complications and results by survey. Plast Reconstr Surg. 1985;76(01):65–72. [PubMed] [Google Scholar]
- 27.Lockwood T E. Lower-body lift. Aesthet Surg J. 2001;21(04):355–370. doi: 10.1067/maj.2001.118028. [DOI] [PubMed] [Google Scholar]
- 28.Song A Y, Jean R D, Hurwitz D J, Fernstrom M H, Scott J A, Rubin J P.A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale Plast Reconstr Surg 2005116051535–1544., discussion 1545–1546 [DOI] [PubMed] [Google Scholar]
- 29.El Khatib H A. Classification of brachial ptosis: strategy for treatment. Plast Reconstr Surg. 2007;119(04):1337–1342. doi: 10.1097/01.prs.0000254796.40226.92. [DOI] [PubMed] [Google Scholar]
- 30.Farage M A, Miller K W, Elsner P, Maibach H I. Characteristics of the aging skin. Adv Wound Care (New Rochelle) 2013;2(01):5–10. doi: 10.1089/wound.2011.0356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khansa I, Harrison B, Janis J E.Evidence-based scar management: how to improve results with technique and technology Plast Reconstr Surg 2016138(3, Suppl):165S–178S. [DOI] [PubMed] [Google Scholar]
- 32.Son D, Harijan A. Overview of surgical scar prevention and management. J Korean Med Sci. 2014;29(06):751–757. doi: 10.3346/jkms.2014.29.6.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atiyeh B S, El Khatib A M, Dibo S A. Pressure garment therapy (PGT) of burn scars: evidence-based efficacy. Ann Burns Fire Disasters. 2013;26(04):205–212. [PMC free article] [PubMed] [Google Scholar]
- 34.Shin T M, Bordeaux J S. The role of massage in scar management: a literature review. Dermatol Surg. 2012;38(03):414–423. doi: 10.1111/j.1524-4725.2011.02201.x. [DOI] [PubMed] [Google Scholar]
- 35.Ward R E, Sklar L R, Eisen D B. Surgical and noninvasive modalities for scar revision. Dermatol Clin. 2019;37(03):375–386. doi: 10.1016/j.det.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 36.Block L, Gosain A, King T W. Emerging therapies for scar prevention. Adv Wound Care (New Rochelle) 2015;4(10):607–614. doi: 10.1089/wound.2015.0646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel S P, Nguyen H V, Mannschreck D, Redett R J, Puttgen K B, Stewart F D. Fractional CO 2 laser treatment outcomes for pediatric hypertrophic burn scars . J Burn Care Res. 2019;40(04):386–391. doi: 10.1093/jbcr/irz046. [DOI] [PubMed] [Google Scholar]
- 38.Kang A S, Kang K S. A systematic review of cutaneous dog ear deformity: a management algorithm. Plast Reconstr Surg Glob Open. 2020;8(09):e3102. doi: 10.1097/GOX.0000000000003102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jaber O, Vischio M, Faga A, Nicoletti G. The three-bite technique: a novel method of dog ear correction. Arch Plast Surg. 2015;42(02):223–225. doi: 10.5999/aps.2015.42.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fredman R, Katz A J, Hultman C S. Fat grafting for burn, traumatic, and surgical scars. Clin Plast Surg. 2017;44(04):781–791. doi: 10.1016/j.cps.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 41.Strong A L, Cederna P S, Rubin J P, Coleman S R, Levi B. The current state of fat grafting: a review of harvesting, processing, and injection techniques. Plast Reconstr Surg. 2015;136(04):897–912. doi: 10.1097/PRS.0000000000001590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tabbal G N, Ahmad J, Lista F, Rohrich R J. Advances in liposuction: five key principles with emphasis on patient safety and outcomes. Plast Reconstr Surg Glob Open. 2013;1(08):e75. doi: 10.1097/GOX.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ablaza V J, Gingrass M K, Perry L C, Fisher J, Maxwell G P. Tissue temperatures during ultrasound-assisted lipoplasty. Plast Reconstr Surg. 1998;102(02):534–542. doi: 10.1097/00006534-199808000-00039. [DOI] [PubMed] [Google Scholar]
- 44.Mendez B M, Coleman J E, Kenkel J M. Optimizing patient outcomes and safety with liposuction. Aesthet Surg J. 2019;39(01):66–82. doi: 10.1093/asj/sjy151. [DOI] [PubMed] [Google Scholar]
- 45.Nagy M W, Vanek P F., Jr A multicenter, prospective, randomized, single-blind, controlled clinical trial comparing VASER-assisted lipoplasty and suction-assisted lipoplasty. Plast Reconstr Surg. 2012;129(04):681e–689e. doi: 10.1097/PRS.0b013e3182442274. [DOI] [PubMed] [Google Scholar]
- 46.Wall S H, Jr, Lee M R. Separation, aspiration, and fat equalization: SAFE liposuction concepts for comprehensive body contouring. Plast Reconstr Surg. 2016;138(06):1192–1201. doi: 10.1097/PRS.0000000000002808. [DOI] [PubMed] [Google Scholar]
- 47.Wall S., Jr SAFE circumferential liposuction with abdominoplasty. Clin Plast Surg. 2010;37(03):485–501. doi: 10.1016/j.cps.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 48.Bellini E, Grieco M P, Raposio E. A journey through liposuction and liposculture: review. Ann Med Surg (Lond) 2017;24:53–60. doi: 10.1016/j.amsu.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dixit V V, Wagh M S. Unfavourable outcomes of liposuction and their management. Indian J Plast Surg. 2013;46(02):377–392. doi: 10.4103/0970-0358.118617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bossert R P, Dreifuss S, Coon D. Liposuction of the arm concurrent with brachioplasty in the massive weight loss patient: is it safe? Plast Reconstr Surg. 2013;131(02):357–365. doi: 10.1097/PRS.0b013e3182789de9. [DOI] [PubMed] [Google Scholar]
- 51.Saldanha O R, Pinto E B, Matos W N, Jr, Lucon R L, Magalhães F, Bello E M. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;21(06):518–526. doi: 10.1067/maj.2001.121243. [DOI] [PubMed] [Google Scholar]
- 52.Krastev T K, Alshaikh G AH, Hommes J, Piatkowski A, van der Hulst R RWJ. Efficacy of autologous fat transfer for the correction of contour deformities in the breast: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2018;71(10):1392–1409. doi: 10.1016/j.bjps.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 53.Coleman S R.Structural fat grafting: more than a permanent filler Plast Reconstr Surg 2006118(3, Suppl):108S–120S. [DOI] [PubMed] [Google Scholar]
- 54.Negenborn V L, Groen J W, Smit J M, Niessen F B, Mullender M G. The use of autologous fat grafting for treatment of scar tissue and scar-related conditions: a systematic review. Plast Reconstr Surg. 2016;137(01):31e–43e. doi: 10.1097/PRS.0000000000001850. [DOI] [PubMed] [Google Scholar]
- 55.Coleman S R. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24(02):347–367. [PubMed] [Google Scholar]
- 56.Suga H, Eto H, Aoi N. Adipose tissue remodeling under ischemia: death of adipocytes and activation of stem/progenitor cells. Plast Reconstr Surg. 2010;126(06):1911–1923. doi: 10.1097/PRS.0b013e3181f4468b. [DOI] [PubMed] [Google Scholar]
- 57.Guerrerosantos J. Brachioplasty. Aesthet Surg J. 2004;24(02):161–169. doi: 10.1016/j.asj.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 58.Sisti A, Cuomo R, Milonia L. Complications associated with brachioplasty: a literature review. Acta Biomed. 2018;88(04):393–402. doi: 10.23750/abm.v88i4.5609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nguyen L, Gupta V, Afshari A, Shack R B, Grotting J C, Higdon K K. Incidence and risk factors of major complications in brachioplasty: analysis of 2,294 patients. Aesthet Surg J. 2016;36(07):792–803. doi: 10.1093/asj/sjv267. [DOI] [PubMed] [Google Scholar]
- 60.Hurwitz D J, Jerrod K. L-brachioplasty: an adaptable technique for moderate to severe excess skin and fat of the arms. Aesthet Surg J. 2010;30(04):620–629. doi: 10.1177/1090820X10380857. [DOI] [PubMed] [Google Scholar]
- 61.Nguyen A T, Rohrich R J. Liposuction-assisted posterior brachioplasty: technical refinements in upper arm contouring. Plast Reconstr Surg. 2010;126(04):1365–1369. doi: 10.1097/PRS.0b013e3181ebe23c. [DOI] [PubMed] [Google Scholar]
- 62.Gusenoff J A, Coon D, Rubin J P. Brachioplasty and concomitant procedures after massive weight loss: a statistical analysis from a prospective registry. Plast Reconstr Surg. 2008;122(02):595–603. doi: 10.1097/PRS.0b013e31817d54a9. [DOI] [PubMed] [Google Scholar]
- 63.Knotts C D, Kortesis B G, Hunstad J P. Avulsion brachioplasty: technique overview and 5-year experience. Plast Reconstr Surg. 2014;133(02):283–288. doi: 10.1097/01.prs.0000437261.31693.3c. [DOI] [PubMed] [Google Scholar]
- 64.Simone P, Carusi C, Segreto F. Postbariatric brachioplasty with posteromedial scar: physical model, technical refinements, and clinical outcomes. Plast Reconstr Surg. 2018;141(02):344–353. doi: 10.1097/PRS.0000000000004060. [DOI] [PubMed] [Google Scholar]
- 65.Stylianos K, Konstantinos G, Pavlos P, Aliki F.Brachial branches of the medial antebrachial cutaneous nerve: a case report with its clinical significance and a short review of the literature[Published correction appears in J Neurosci Rural Pract. 2017 Apr-Jun;8(2):323]J Neurosci Rural Pract 2016703443–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hurwitz D J, Holland S W.The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla, and lateral chest Plast Reconstr Surg 200611702403–411., discussion 412–413 [DOI] [PubMed] [Google Scholar]
- 67.Langer V, Singh A, Aly A S, Cram A E. Body contouring following massive weight loss. Indian J Plast Surg. 2011;44(01):14–20. doi: 10.4103/0970-0358.81439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.American Society of Plastic Surgeons Plastic Surgery Statistics Report. 2019Available at:https://www.plasticsurgery.org/documents/News/Statistics/2019/plastic-surgery-statistics-full-report-2019.pdf
- 69.Matarasso A, Schneider L F, Barr J. The incidence and management of secondary abdominoplasty and secondary abdominal contour surgery. Plast Reconstr Surg. 2014;133(01):40–50. doi: 10.1097/01.prs.0000436525.56422.4d. [DOI] [PubMed] [Google Scholar]
- 70.van Uchelen J H, Werker P M, Kon M. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. 2001;107(07):1869–1873. doi: 10.1097/00006534-200106000-00037. [DOI] [PubMed] [Google Scholar]
- 71.Sterodimas A, Boriani F, Nicaretta B, Pereira L H. Revision abdominoplasty with truncal liposculpting: a 10-year experience. Aesthetic Plast Surg. 2019;43(01):155–162. doi: 10.1007/s00266-018-1176-0. [DOI] [PubMed] [Google Scholar]
- 72.Smith L F, Smith L F., Jr Safely combining abdominoplasty with aggressive abdominal liposuction based on perforator vessels: technique and a review of 300 consecutive cases. Plast Reconstr Surg. 2015;135(05):1357–1366. doi: 10.1097/PRS.0000000000001200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parsa F D, Cheng J, Hu M S, Kim L, Castel N, Parsa A A. The importance of umbilical blood supply and umbilical delay in secondary abdominoplasty: a case report. Aesthet Surg J. 2018;38(05):NP81–NP87. doi: 10.1093/asj/sjy003. [DOI] [PubMed] [Google Scholar]
- 74.Barbosa M V, Nahas F X, Sabia Neto MÂ, Ferreira L M. Strategies in umbilical reconstruction. J Plast Reconstr Aesthet Surg. 2009;62(06):e147–e150. doi: 10.1016/j.bjps.2008.08.074. [DOI] [PubMed] [Google Scholar]
- 75.Hoyos A E, Perez M E, Castillo L. Dynamic definition mini-lipoabdominoplasty combining multilayer liposculpture, fat grafting, and muscular plication. Aesthet Surg J. 2013;33(04):545–560. doi: 10.1177/1090820X13484493. [DOI] [PubMed] [Google Scholar]
- 76.Patronella C K. Redefining abdominal anatomy: 10 key elements for restoring form in abdominoplasty. Aesthet Surg J. 2015;35(08):972–986. doi: 10.1093/asj/sjv112. [DOI] [PubMed] [Google Scholar]
- 77.Rohrich R J, Sorokin E S, Brown S A, Gibby D L.Is the umbilicus truly midline? Clinical and medicolegal implications Plast Reconstr Surg 200311201259–263., discussion 264–265 [DOI] [PubMed] [Google Scholar]
- 78.Lee Y T, Kwon C, Rhee S C, Cho S H, Eo S R. Four flaps technique for neoumbilicoplasty. Arch Plast Surg. 2015;42(03):351–355. doi: 10.5999/aps.2015.42.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Corvino A, Rosa D, Sbordone C. Diastasis of rectus abdominis muscles: patterns of anatomical variation as demonstrated by ultrasound. Pol J Radiol. 2019;84:e542–e548. doi: 10.5114/pjr.2019.91303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jessen M L, Öberg S, Rosenberg J. Treatment options for abdominal rectus diastasis. Front Surg. 2019;6:65. doi: 10.3389/fsurg.2019.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mommers E HH, Ponten J EH, Al Omar A K, de Vries Reilingh T S, Bouvy N D, Nienhuijs S W. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017;31(12):4934–4949. doi: 10.1007/s00464-017-5607-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nahas F X, Ferreira L M, Mendes JdeA. An efficient way to correct recurrent rectus diastasis. Aesthetic Plast Surg. 2004;28(04):189–196. doi: 10.1007/s00266-003-0097-7. [DOI] [PubMed] [Google Scholar]
- 83.Richter D F, Stoff A, Velasco-Laguardia F J, Reichenberger M A.Circumferential lower truncal dermatolipectomy Clin Plast Surg 2008350153–71., discussion 93 [DOI] [PubMed] [Google Scholar]
- 84.Small K H, Constantine R, Eaves F F, III, Kenkel J M. Lessons learned after 15 years of circumferential bodylift surgery. Aesthet Surg J. 2016;36(06):681–692. doi: 10.1093/asj/sjv265. [DOI] [PubMed] [Google Scholar]
- 85.Poodt I G, van Dijk M M, Klein S, Hoogbergen M M. Complications of lower body lift surgery in postbariatric patients. Plast Reconstr Surg Glob Open. 2016;4(09):e1030. doi: 10.1097/GOX.0000000000001030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Losco L, Roxo A C, Roxo C W. Lower body lift after bariatric surgery: 323 consecutive cases over 10-year experience. Aesthetic Plast Surg. 2020;44(02):421–432. doi: 10.1007/s00266-019-01543-x. [DOI] [PubMed] [Google Scholar]
- 87.Kitzinger H B, Cakl T, Wenger R, Hacker S, Aszmann O C, Karle B. Prospective study on complications following a lower body lift after massive weight loss. J Plast Reconstr Aesthet Surg. 2013;66(02):231–238. doi: 10.1016/j.bjps.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 88.Makipour J J, Nuveen E, Abbott D. Safety of outpatient circumferential body lift: evidence from 42 consecutive cases. Plast Reconstr Surg. 2017;139(06):1355–1362. doi: 10.1097/PRS.0000000000003392. [DOI] [PubMed] [Google Scholar]
- 89.Swanson E. Near-circumferential lower body lift: a review of 40 outpatient procedures. Plast Reconstr Surg Glob Open. 2019;7(12):e2548. doi: 10.1097/GOX.0000000000002548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bullocks J, Basu C B, Hsu P, Singer R. Prevention of hematomas and seromas. Semin Plast Surg. 2006;20(04):233–240. [Google Scholar]
- 91.Dreifuss S E, Beidas O E, Rubin J P, Gusenoff J A. Characterizing the saddlebag deformity after lower body lift. Aesthet Surg J. 2018;38(10):1115–1123. doi: 10.1093/asj/sjy105. [DOI] [PubMed] [Google Scholar]
- 92.Hurwitz D J, Rubin J P, Risin M, Sajjadian A, Sereika S. Correcting the saddlebag deformity in the massive weight loss patient. Plast Reconstr Surg. 2004;114(05):1313–1325. doi: 10.1097/01.prs.0000135862.83833.5f. [DOI] [PubMed] [Google Scholar]
- 93.O'Neill R C, Abu-Ghname A, Davis M J, Chamata E, Rammos C K, Winocour S J. The role of fat grafting in buttock augmentation. Semin Plast Surg. 2020;34(01):38–46. doi: 10.1055/s-0039-3401038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mofid M M, Teitelbaum S, Suissa D. Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J. 2017;37(07):796–806. doi: 10.1093/asj/sjx004. [DOI] [PMC free article] [PubMed] [Google Scholar]


