Abstract
Male infertility induced by heat stress has been attracting more and more attention. Heat stress not only causes apoptosis of spermatocytes but also has adverse effects on Sertoli cells, further damaging spermatogenesis. Lycium barbarum polysaccharide (LBP) is the main bioactive component of Lycium barbarum, which has a protective effect on male reproduction, but its mechanism is still unclear. In this study, our results proved that LBP blocked the inhibitory effect on the proliferation activity of Sertoli cells after heat stress, reversed the dedifferentiation of Sertoli cells induced by heat stress, and ameliorated the structural integrity of the blood-testis barrier. In addition, it increased the expression of the androgen receptor and activated Akt signaling pathway to resist heat-stress-induced injury of Sertoli cells.
1. Introduction
More than half of the childbearing couples could not have children due to male infertility [1, 2], which is induced by varieties of causes including the spermatogenic quantitative or qualitative defect, catheter obstruction or dysfunction, and hypothalamic-pituitary axis disorders [3, 4]. Among these situations, abnormal spermatogenesis is the primary culprit of impaired male fertility. Spermatogenesis is a temperature-dependent process [5, 6]. For most mammals, normal spermatogenesis entails the temperature in the scrotum to be lower than body temperature. After heat treatment to local testis, male animals display testicular damages, including local testis tissue hypoxia [7, 8], germ cells apoptosis [9], blood-testis barrier (BTB) dysfunction, and reduced sperm count and quality [10–12]. Thus, scrotal temperature increases and spermatogenesis is impaired, leading to male infertility.
Spermatogenesis depends on mature Sertoli cells (SCs). In the seminiferous tubule, SCs provide structural support and supply nutrients, functional proteins, and cytokines for spermatogenesis [13, 14]. The number of SCs is proportional to the number of germ cells [15]. Occludin and zonula occludens-1 exist between adjacent SCs [16] and compose BTB which provides a suitable microenvironment for spermatogenesis [17, 18]. The decrease of occludin and (or) zonula occludens-1 causes the damage of BTB integrity, negatively effecting spermatogenesis [15, 19].
Androgen receptor (AR) is a type I steroid receptor. Androgens have to bind to AR before they can regulate the development of germ cells and SCs. Expressed in SCs, an androgen receptor (AR) plays a crucial role in spermatogenesis [20, 21]. Studies demonstrated that the loss of AR directly influences the maturation and the final quantity of SCs [22, 23], as well as spermatogenesis [24]. Besides, the absence of AR causes increased permeability of BTB in vitro or in vivo [25, 26].
Lycium barbarum polysaccharide (LBP, PubChem SID: 134223164), the main component of Chinese wolfberry, is characterized by high bioactivity and significant content [27]. The glucoside apart, which is composed of arabinose, rhamnose, xylose, mannose, galactose, and glucose (Figure 1), accounts for more than 90% of the LBP mass [28]. Evidence shows LBP could ameliorate testicular damage by upregulating the testosterone level and reducing germ cell apoptosis [29–32]. However, limited research has been conducted on how LBP influences SCs and BTB. In the present study, we explore the effects and mechanisms of LBP on heat-stress-induced damage of SCs and BTB, centered around the changes in AR.
Figure 1.
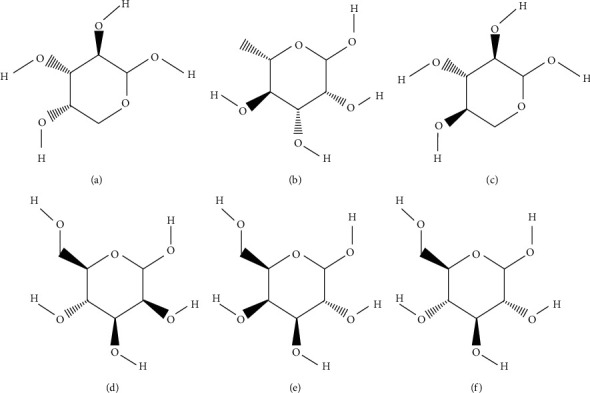
Six main monosaccharides in LBP. (a) Arabinose (PubChem CID: 439195); (b) rhamnose (PubChem CID: 25310); (c) xylose (PubChem CID: 135191); (d) mannose (PubChem CID: 18950); (e) galactose (PubChem CID: 6036); and (f) D-glucose (PubChem CID: 5793).
2. Materials and Methods
2.1. Drug and Reagents
Lycium barbarum polysaccharide powder was purchased from Nanjing Manhay Medical Technology (Nanjing, China, No. zhe B2-20090288-37).
DMEM/F12, 0.25% trypsin-ethylenediaminetetraacetic acid, collagenase IV, fetal bovine serum (FBS), and penicillin-streptomycin liquid were purchased from Gibco (BRL, Gaithersburg, MD, USA). 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), dimethyl sulfoxide (DMSO), phosphate buffered saline (PBS), and the bicinchoninic acid (BCA) protein assay kit were purchased from Solarbio Life Sciences (Beijing, China). SP link detection kits (biotin-streptavidin HRP detection systems) and the diaminobenzidine kit were purchased from ZSGB-BIO (Beijing, China). The anti-Ki67 (ab16667) and anti-AR (ab133273) were purchased from Abcam (Cambridge, UK). The anti-occludin (PA5-20755) and anti-zonula occludens-1 (61-7300) were obtained from Thermo Fisher Scientific (Waltham, MA, USA). The anti-Phospho-Akt (Ser473) (#4060) and anti-Akt (#4691) were obtained from Cell Signaling Technology (Boston, MA, USA). The anti-CK-18 antibody (10830-1-AP) and anti-beta-actin antibody (60008-1-lg) were obtained from Proteintech (Chicago, IL, USA).
2.2. Animals
Mature male Sprague Dawley rats (8 weeks of age) were purchased from Huafukang (Beijing, China, No. SYXK Jing 2011-0024). These rats were treated and sacrificed according to the National Institutes of Health Guidelines for the Care and Use of Laboratory Animals (NIH Publication No. 85-23, revised 1985). All animal procedures were approved by the Laboratory Animal Welfare and Ethics Committee of the Beijing University of Chinese Medicine (BUCM-4-2017010805-010).
2.3. Primary SC Isolation, Culture, and Heat Treatment
Sertoli cell isolation was according to the previous method [33]. Briefly, the testicular tissue was obtained from the testis and washed twice in PBS precooled at 4°C. After fully centrifuged at 1000 rmp about 5 min, the sediment was treated with collagenase IV (0.5 mg/mL) for 5 min. After washing twice and certification for 5 min, the sedimentation was secondly digested with trypsin (0.05%) for 5 min. FBS in the same velum was added to stop digestion. Then, the sedimentation was filtrated through a 100-mesh filter and centrifugated at 1000 rmp for 5 min. The cells were washed twice with DMEM/F12, collected in the culture medium (DMEM plus F12 with 10% FBS and 1% penicillin-streptomycin), and cultured at 35°C in a CO2 incubator (5% CO2/95% air). After 40 h culturing, the medium was replaced to remove unattached germ cells, and 12–24 h later, when cells were confluent, they were ready for the following experiments. LBP was dissolved and diluted with PBS into different concentrations and then was added in SCs at the dose of 25 mg/L, 50 mg/L, and 100 mg/L. Cells in the control group and heat-stress group were added with the same volume of PBS. After 24 h, the control group was cultured at 35°C for another 20 minutes, and the other groups were treated in a 43°C water bath for 20 minutes.
2.4. Evaluation of Cell Viability
MTT assay has been widely used for measuring cell viability. The obtained absorbance value (OD value) under the specific wavelength is directly proportional to the number of living cells. SCs were seeded at 5 × 104 per well in 96-well plates in DMEM/F12 supplemented with 10% FBS. Cells were treated with LBP in different concentrations or PBS for 24 h. After removing some supernatant, an MTT regent (5 mg/ml) was added to each well for four hours. Then SCs were treated with DMSO by shaking for 15 min at room temperature, and the OD value was measured at 570 nm by using a microplate reader FLUO Star Omega (BMG Labtech, Offenburg, Germany). The blank group had no cells in wells and was used as the zero point of absorbance. Also, the absorbance value of each group divided by the control group was cell viability (%).
2.5. Immunohistochemistry
The immunohistochemistry protocol in our experiment followed that described previously [34]. SCs were first fixed in a 4% polyoxymethylene solution and then treated with 0.5% triton X-100 and 0.3% hydrogen peroxide, respectively. After three washes in PBS, cells were blocked with 10% goat serum to suppress the nonspecific antigen and then incubated in the primary antibody of Ki67 (1 : 200) or AR (1 : 200) overnight at 4°C. The next day, after three washes in PBS, the biotinylated secondary antibodies were added for 15 min at 37°C. After three washes in PBS, the horseradish enzyme labeling streptavidin working solution was added for 15 min at 37°C. Immunostaining was developed with the diaminobenzidine kit and counterstained with hematoxylin. Six nonoverlapping fields were selected for each group to take pictures. Image-Pro Plus (Version 6.0, Media Cybernetics, Bethesda, MD, USA) software was used to process the images and count the positive cells for statistical analysis.
2.6. Western Blot
Western blot was performed as described previously [35, 36]. The total protein was extracted from SCs and transferred to polyvinyl difluoride (PVDF) membranes. PVDF membranes were blocked in 5% nonfat milk for 1 h at room temperature and then exposed to the primary antibodies diluted in 1% blocking buffer: AR (1 : 1000), CK-18 (1 : 1000), occludin (1 : 1000), zonula occludens-1 (1 : 1000), p-Akt (Ser473) (1 : 1000), and Akt (1 : 1000) at 4°C overnight. After washing in tris-buffered saline containing 0.1% Tween-20 (TBST) three times, the membranes were incubated in horseradish-peroxidase- (HRP-) conjugated second antibodies (1 : 4000) for 1 h. After washing with TBST, the membranes were visualized by a hypersensitive electrogenerated chemiluminescence solution (Proteintech). β-Actin (1 : 5000) was used as an internal control for AR, CK-18, occluding, and zonula occludens-1. Akt was used as an internal control for phosphorylated-Akt in Ser473. Band intensities were determined by the software Quantity One, Version 4.6.2 (Bio-Rad Laboratories, Hercules, CA, USA).
2.7. Statistical Analysis
Each experiment was repeated at least three times. Statistical analysis was performed with the software SPSS version 20.0 (IBM, Albuquerque, NY, USA). Data that conformed to normal distribution or approximate normal distribution are expressed as means ± standard error of the mean (SEM). One-way analysis of variance was used for analyzing the data in different groups, and the pairwise comparisons were tested by the Tukey multiple comparison test. P < 0.05 was considered as significant, and P < 0.01 was considered as highly significant.
3. Results
3.1. The Changes in Cell Viability of SCs after Different Concentrations of LBP Treatment
To observe the effect of LPB on cell viability and select appropriate drug concentrations, we detected the OD value by MTT. As shown in Figure 2, compared with the control group, the cell viability of SCs at 25 mg/L, 50 mg/L, and 100 mg/L LBP treatment groups significantly increased (P < 0.05 or P < 0.01), while the differences in other LBP groups were not statistically significant (P > 0.05). Therefore, these three concentrations were selected as the concentration of LBP drug groups.
Figure 2.
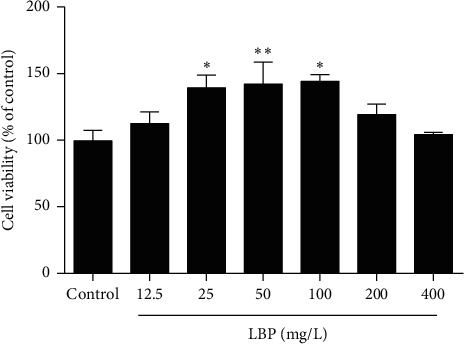
The changes of cell viability of SCs after different concentrations of LBP treatment. After treatment of LBP at 25 mg/L, 50 mg/L, and 100 mg/L, the cell viability of SCs was obviously increased. Data are presented as means ± SEM (n = 3) from three independent experiments. ∗p < 0.05 and ∗∗p < 0.01, compared to the control group.
3.2. LBP Alleviates the Decrease of SC Proliferation Activity after Heat Stress
To investigate the effect of LBP on the proliferation activity of SCs after heat stress, we tested the Ki67 in SCs (Figure 3). Ki67 expresses in the SCs nucleus. Compared with the control group, the positive signal of Ki67 significantly decreased in the heat-stress group and 25 mg/L LBP group (P < 0.05 or P < 0.01), and the 50 mg/L LBP and 100 mg/L LBP group have no significant change. Compared with the heat-stress group, the positive signal of Ki67 in LBP treatment groups showed a noticeable increase (P < 0.01). These data indicated that LBP treatment could resist the reduction of Ki67 expression induced by heat stress; however, the 25 mg/L LBP group still had a noticeable difference compared to the control group, and 50 mg/L LBP and 100 mg/L LBP could improve the proliferation activity of SCs after heat stress to the level of normal statement.
Figure 3.
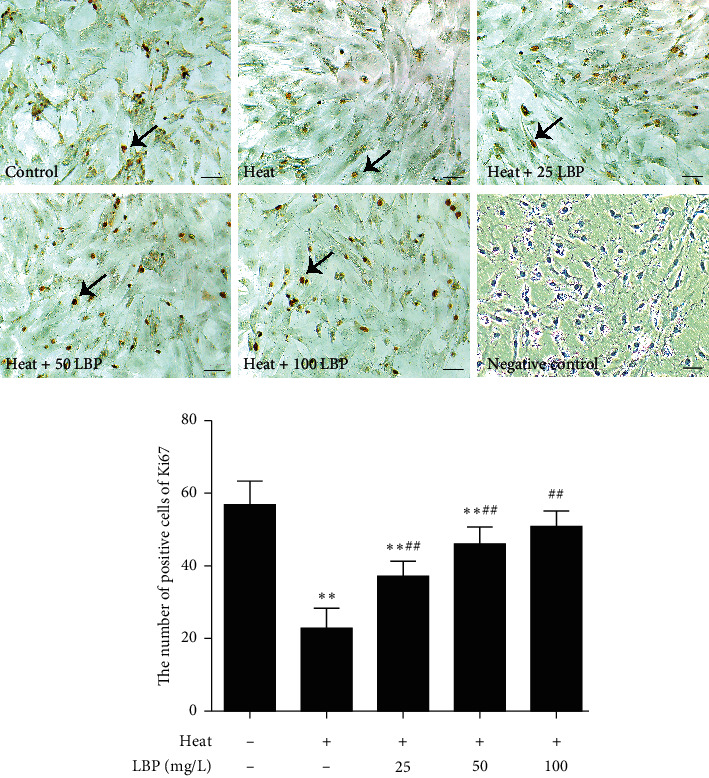
LBP improves the proliferation activity of SCs after heat stress. The expression of Ki67 was observed with the immunohistochemical assay. Scale bar: 50 μm. The brown areas are Ki67 positive Sertoli cells (black arrows). Data are presented as means ± SEM (n = 3) from three independent experiments. ∗∗p < 0.01, compared to the control group. ##p < 0.01, compared to the heat-stress group.
3.3. LBP Inhibits the Dedifferentiation of SCs after Heat Stress
To observe the effect of LBP on the differentiation of SCs, we tested the expression of CK-18 (Figure 4). The expression of CK-18 in the heat-stress group significantly increased (P < 0.05 or P < 0.01) when compared with the control group. Moreover, compared with the heat-stress group, the expression of CK-18 in LBP treatment groups (25, 50, and 100 mg/L) decreased significantly (P < 0.01).
Figure 4.
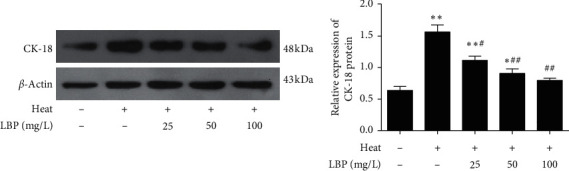
LBP inhibits the dedifferentiation of SCs after heat stress. CK-18 was checked by western blot. Data are presented as means ± SEM (n = 3) from three independent experiments. ∗p < 0.05 and ∗∗p < 0.01, compared to control group. #p < 0.05 and ##p < 0.01, compared to the heat-stress group.
3.4. LBP Maintains the Integrity of BTB after Heat Stress
To clarify the effect of LBP on BTB, we detected the TJ-associated protein, occludin (Figure 5(a)) and zonula occludens-1 (Figure 5(b)). As shown in Figure 5, compared with the control group, the expression of occludin and zonula occludens-1 in the heat-stress group significantly decreased (P < 0.05 or P < 0.01). Compared with the heat-stress group, the expression of occludin and zonula occludens-1 in LBP treatment groups increased significantly (P < 0.01) in a dose-dependent manner (P < 0.05 or P < 0.01).
Figure 5.
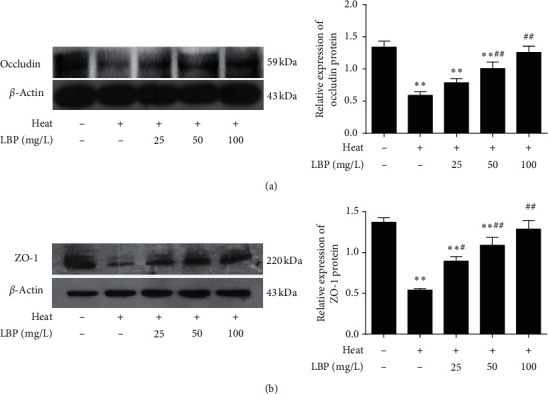
LBP maintains the integrity of BTB after heat stress. Occludin and ZO-1 in SCs were detected with western blot (a, b). Data are presented as means ± SEM (n = 3) from three independent experiments. ∗∗p < 0.01, compared to the control group. #p < 0.05, ##p < 0.01, compared to the heat-stress group.
3.5. LBP Maintains the Expression of AR in SCs after Heat Stress
Testosterone only works when combining to the androgen receptor. To determine the AR in SCs and to better understand the mechanism of AR, we analyzed AR with immunohistochemistry staining (Figure 6(a)) and western blot (Figure 6(b)). Figure 6(a) shows that AR mainly expresses in the nucleus and few are expressed in the cytoplasm of mature SCs. As shown in Figure 6, the expression of AR did significantly decrease (P < 0.01) after heat treatment. Compared with the heat-stress group, the expression of AR in LBP treatment groups increased significantly (P < 0.01).
Figure 6.
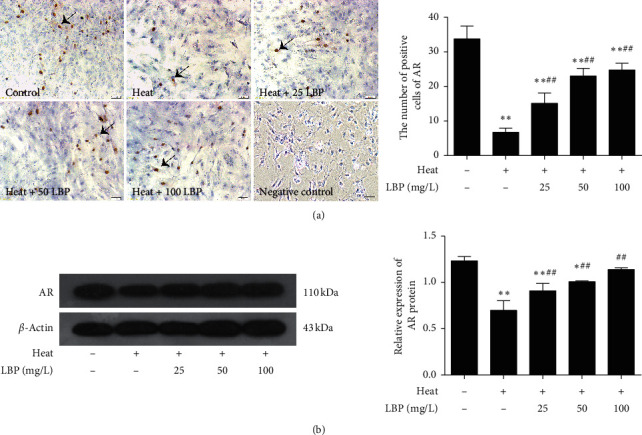
LBP upregulates the expression of AR in SCs after heat stress. The expression of AR was observed by immunohistochemical assay (scale bar: 50 μm) and western blot (b). The brown areas are AR-positive Sertoli cells (black arrows). Data are presented as means ± SEM (n = 3) from three independent experiments. ∗p < 0.05 and ∗∗p < 0.01, compared to the control group. ##p < 0.01, compared to the heatstress group.
3.6. LBP Maintains the Akt Phosphorylation in SCs after Heat Stress
We all know the critical role of the Akt signaling pathway in cell activity. It has been found that there is an interaction between AR and Akt phosphorylation at Ser473 [37]. Consequently, we tested the expression of p-Akt (Ser473) to explore the effective way of LBP on SCs (Figure 7). Compared with the control group, the expression of p-Akt (Ser473) in the heat-stress group significantly decreased (P < 0.01). Compared with the heat-stress group, the expression of p-Akt (Ser473) in LBP treatment groups increased significantly (P < 0.01). These data indicated that Akt phosphorylation at Ser473 was involved in the protective effect of LBP on SCs and BTB.
Figure 7.
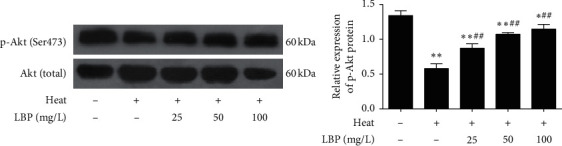
LBP promotes the Akt phosphorylation in SCs after heat stress. The phosphorylated Akt was detected with western blot. Data are presented as means ± SEM (n = 3) from three independent experiments. ∗p < 0.05 and ∗∗p < 0.01, compared to the control group. ##p < 0.01, compared to the heat-stress group.
4. Discussion
Sertoli cells are the most crucial somatic cells for spermatogenesis. The number and maturations of SCs determine the spermatogenesis. In this study, our data indicate that LBP could resist the decrease of proliferation activity, inhibit the dedifferentiation of SCs after heat stress, and more importantly, preserve BTB integrity and permeability by maintaining AR and phosphorylated-Akt (Ser473).
Lycium barbarum fruits, as a traditional Chinese medicine and health food for people, have been used to nourish the kidney and improve fertility for thousands of years [38, 39]. The polysaccharide is the primary active component responsible for those biological activities in L. barbarum fruits [28]. Also, LBP has been reported to possess a wide range of pharmacological activities, including antioxidant, anticancer, and neuroprotective effects, immune regulation, and others [40]. Recently, there are some reports about the effects of LBP on male fertility, for example, increasing the serum testosterone level and decreasing apoptosis of germ cells. However, the effects of LBP on SCs and BTB are rarely reported. Thus, this study intends to investigate the effects and underlying mechanisms of LBP on SCs and BTB.
Temperature is an essential controller for reproductive activity and testicular homeostasis [41]. Only can physiological scrotal hypothermia guarantee the normal spermatogenesis in most mammals [42]. Despite that SCs are more tolerant to heat than germ cells, heat stress still can cause damaged structure and dysfunction of SCs [43], resulting in spermatogenic arrest and weak fertilizing capacity in vivo and in vitro [10, 44]. Some evidence and our previous study proved that local testis heat treatment (43°C for 20 min) successfully leads to dyszoospermia of monkey and rodents [33, 45, 46]. Furthermore, compared with other modeling methods of spermatogenesis disorder, heat-stress-induced impairment on testis is reversible, which is very suitable to study the sequence and interaction between SCs and germ cells.
We first selected three suitable concentrations of LBP by MTT (Figure 2) to treat Sertoli cell. As we previously said, the number of SCs directly determines the number of sperm. Ki67, a nuclear antigen closely related to cell mitosis, is often considered as a marker of cell proliferative activity [47, 48]. For rat SCs, the number of SCs keeps increasing after birth, as well as the number of Ki67 positive cells, while it began to decline at the age of 90 days [49], which suggest SCs of 60-day-old rats are not fully mature and some of them still can proliferate. Intervention on SCs of 60-day-old rats can affect the final number of SCs in seminiferous tubules. Therefore, we detected the expression of Ki67 to observe the proliferation activity of SCs. The result confirmed that LBP could preserve the cell proliferative activity of SCs after heat stress (Figure 3). Furthermore, only mature SCs can support spermatogenesis. CK-18 is a cytoskeleton molecule, which expresses in the prepubertal SCs and gradually disappears after puberty on mammals [50, 51]. High expression of CK-18 indicates that SCs are immature and dysfunctional [52]. Our results imply that LBP treatment could inhibit the re-expression of CK-18 after heat stress (Figure 4) to prevent the dedifferentiation of SCs.
The formation of BTB occurs at the beginning of puberty, and BTB is partly composed of tight junction (TJ), which directly affects the permeability [53]. Occludin is a highly phosphorylated transmembrane TJ-associated protein [54], believed as the initiator of BTB formation [55], and it is related to the initiation of spermatogenesis as well [56, 57]. Zonula occludens-1, a peripheral transmembrane protein, forms a link between the transmembrane proteins and the cytoskeletal compartment [58, 59] to maintain the integrity of BTB and support the migration and release of germ cells [60]. Reports have shown that increased permeability and dysfunction of BTB are blamed for the loss of occludin and (or) zonula occludens-1, resulting in harmful influence to spermatogenesis [61, 62]. Therefore, we selected occludin and zonula occludens-1 as the molecule marker of BTB integrity. Our data indicated that LBP could maintain the expression of them in SCs to ameliorate the heat-stress-induced increasing permeability and dysfunction of BTB (Figure 5).
It is well known that testosterone and AR are the decisive factors for maintaining male fertility and secondary sexual characteristics. AR is believed as a crucial upstream factor in controlling the development of SCs and the forming of BTB [63]. AR deficiency caused failure of SCs maturation [64] and decrease of TJ-associated protein expression [10, 11, 65]. In the present study, our data demonstrated that LBP could against the decrease of AR induced by heat stress, which was consistent with the change of tight junction protein, but opposite to CK-18 (Figure 6). Furthermore, through in vivo experiments, it was found that LBP increased the serum testosterone level in rats. We concluded the increase of testosterone and AR can improve their binding efficiency, which may be an important reason for LBP to ameliorate heat-stress-induced damage of SCs dedifferentiation and increase of BTB integrity and permeability.
Akt/protein kinase B (PKB), a serine/threonine kinase, is a mediator in the growth and proliferation of Sertoli cells [66, 67]. Akt is activated by phosphorylation on threonine 308 (Thr308) and serine 473 (Ser473), with phosphorylation at Ser473 resulting in maximal Akt activity [68]. Upregulated Akt phosphorylation could promote the expression of Ki67 [69]. Besides, studies showed that the Akt signaling pathway is related to the expressions of occludin and zonula occludens-1 [70, 71], and activation of Akt by enhancing phosphorylation of p-Akt (Thr308) and p-Akt (Ser473) can effectively prevent the destruction of the TJ barrier [72]. Also, after blocking the Akt signaling pathway, AR transduction was blocked into the testosterone signaling pathway in SCs, and Akt phosphorylation at Ser473 is the key molecule in the pathway of AR trafficking [37, 73]. In our results, the expression p-Akt (Ser473) of heat-stress SCs decreased while it increased after LBP treatment (Figure 7), as well as AR. Therefore, we concluded that the Akt signaling pathway involves in the effect of LBP on ameliorating heat-stress-induced damages in SCs and BTB.
In summary, our study indicates that LBP can preserve the expression of Ki67 and occludin and zonula occludens-1 and inhibit the expression of CK-18 to prevent heat-stress-induced impairment of Sertoli cells and BTB through maintaining AR and Akt phosphorylation at Ser473 (Figure 8). Also, it provides the experimental evidence for clinical prevention of male reproductive heat-stress injury.
Figure 8.
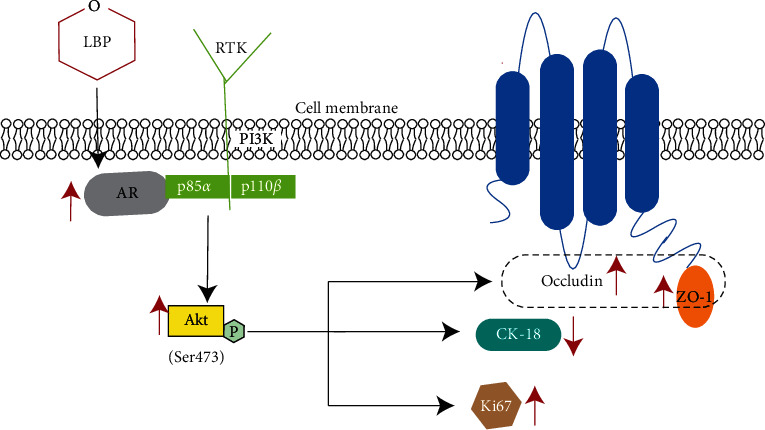
Effects and mechanism of LBP on Sertoli cells and BTB after heat stress. AR could directly interact with PI3K regulatory subunit p85α to activate kinase Akt [37, 73]. LBP maintained the expression of Ki67 and TJ protein and suppressed the re-expression of CK-18 by resisting the decrease of AR and maintaining phosphorylation of Akt in Sertoli cells after heat stress.
Acknowledgments
This research was supported by grants from the National Natural Science Foundation of China (81273610) and Research and Development Fund of Beijing University of Chinese Medicine (2019-ZFXZJJ-021).
Data Availability
The data supporting the conclusions of this article are included within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Jian Guo conceived of the study and directed the work; Suqin Hu performed the experiments; Dianlong Liu, Sijia Liu, and Chunrui Li also contributed to the experiments; Suqin Hu drafted the manuscript; Jian Guo made the critical revisions and improvements for the manuscript; and Suqin Hu and Jian Guo finalized the paper.
References
- 1.de Kretser D. Male infertility. The Lancet. 1997;349(9054):787–790. doi: 10.1016/s0140-6736(96)08341-9. [DOI] [PubMed] [Google Scholar]
- 2.Thonneau P., Marchand S., Tallec A., et al. Incidence and main causes of infertility in a resident population (1, 850, 000) of three French regions (1988-1989)∗. Human Reproduction. 1991;6(6):811–816. doi: 10.1093/oxfordjournals.humrep.a137433. [DOI] [PubMed] [Google Scholar]
- 3.Tournaye H., Krausz C., Oates R. D. Novel concepts in the aetiology of male reproductive impairment. The Lancet Diabetes & Endocrinology. 2017;5(7):544–553. doi: 10.1016/s2213-8587(16)30040-7. [DOI] [PubMed] [Google Scholar]
- 4.Babakhanzadeh E., Nazari M., Ghasemifar S., Khodadadian A. Some of the factors involved in male infertility: a prospective review. International Journal of General Medicine. 2020;13:29–41. doi: 10.2147/ijgm.s241099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y.-X. Control of spermatogenesis in primate and prospect of male contraception. Archives of Andrology. 2005;51(2):77–92. doi: 10.1080/01485010490485768. [DOI] [PubMed] [Google Scholar]
- 6.Garolla A., Torino M., Sartini B., et al. Seminal and molecular evidence that sauna exposure affects human spermatogenesis. Human Reproduction. 2013;28(4):877–885. doi: 10.1093/humrep/det020. [DOI] [PubMed] [Google Scholar]
- 7.Aitken R. J., Roman S. D. Antioxidant systems and oxidative stress in the testes. Advances in Experimental Medicine and Biology. 2008;636:154–71. doi: 10.1007/978-0-387-09597-4_9. [DOI] [PubMed] [Google Scholar]
- 8.Reyes J. G., Farias J. G., Henriquez-Olavarrieta S., et al. The hypoxic testicle: physiology and pathophysiology. Oxidative Medicine and Cellular Longevity. 2012;2012:15. doi: 10.1155/2012/929285.929285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaur S., Bansal M. P. Protective role of dietary-supplemented selenium and vitamin E in heat-induced apoptosis and oxidative stress in mice testes. Andrologia. 2015;47(10):1109–1119. doi: 10.1111/and.12390. [DOI] [PubMed] [Google Scholar]
- 10.Chen M., Cai H., Yang J.-L., et al. Effect of heat stress on expression of junction-associated molecules and upstream factors androgen receptor and Wilms’ tumor 1 in monkey sertoli cells. Endocrinology. 2008;149(10):4871–4882. doi: 10.1210/en.2007-1093. [DOI] [PubMed] [Google Scholar]
- 11.Li X. X., Chen S. R., Shen B., et al. The heat-induced reversible change in the blood-testis barrier (BTB) is regulated by the androgen receptor (AR) via the partitioning-defective protein (par) polarity complex in the mouse. Biology of Reproduction. 2013;89(1):p. 12. doi: 10.1095/biolreprod.113.109405. [DOI] [PubMed] [Google Scholar]
- 12.Bedford J. M. Human spermatozoa and temperature: the elephant in the room. Biology of Reproduction. 2015;93:p. 97. doi: 10.1095/biolreprod.115.130658. [DOI] [PubMed] [Google Scholar]
- 13.Rato L., Socorro S., Cavaco J. E. B., Oliveira P. F. Tubular fluid secretion in the seminiferous epithelium: ion transporters and aquaporins in sertoli cells. The Journal of Membrane Biology. 2010;236(2):215–224. doi: 10.1007/s00232-010-9294-x. [DOI] [PubMed] [Google Scholar]
- 14.Griswold M. D. Interactions between germ cells and sertoli cells in the testis. Biology of Reproduction. 1995;52(2):211–216. doi: 10.1095/biolreprod52.2.211. [DOI] [PubMed] [Google Scholar]
- 15.Lui W.-Y., Lee W. M., Cheng C. Y. Transforming growth factor-β3 perturbs the inter-sertoli tight junction permeability barrier in vitro possibly mediated via its effects on occludin, zonula occludens-1, and claudin-111. Endocrinology. 2001;142(5):1865–1877. doi: 10.1210/endo.142.5.8116. [DOI] [PubMed] [Google Scholar]
- 16.Tarulli G. A., Meachem S. J., Schlatt S., Stanton P. G. Regulation of testicular tight junctions by gonadotrophins in the adult Djungarian hamster in vivo. Reproduction. 2008;135(6):867–877. doi: 10.1530/rep-07-0572. [DOI] [PubMed] [Google Scholar]
- 17.Lee N., Wong E., Mruk D., Cheng C. Testicular cell junction: a novel target for male contraception. Current Medicinal Chemistry. 2009;16(7):906–915. doi: 10.2174/092986709787549262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stanton P. G. Regulation of the blood-testis barrier. Seminars in Cell & Developmental Biology. 2016;59:166–173. doi: 10.1016/j.semcdb.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Fink C., Weigel R., Hembes T., et al. Altered expression of ZO-1 and ZO-2 in sertoli cells and loss of blood-testis barrier integrity in testicular carcinoma in situ. Neoplasia. 2006;8(12):1019–1027. doi: 10.1593/neo.06559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker M. E. Steroid receptor phylogeny and vertebrate origins. Molecular and Cellular Endocrinology. 1997;135(2):101–107. doi: 10.1016/s0303-7207(97)00207-4. [DOI] [PubMed] [Google Scholar]
- 21.Wang R.-S., Yeh S., Chen L.-M., et al. Androgen receptor in sertoli cell is essential for germ cell nursery and junctional complex formation in mouse testes. Endocrinology. 2006;147(12):5624–5633. doi: 10.1210/en.2006-0138. [DOI] [PubMed] [Google Scholar]
- 22.Enmark E., Gustafsson J. A. Orphan nuclear receptors—the first eight years. Molecular Endocrinology. 1996;10(11):1293–1307. doi: 10.1210/mend.10.11.8923456. [DOI] [PubMed] [Google Scholar]
- 23.Hazra R., Corcoran L., Robson M., et al. Temporal role of sertoli cell androgen receptor expression in spermatogenic development. Molecular Endocrinology. 2013;27(1):12–24. doi: 10.1210/me.2012-1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh S., Tsai M.-Y., Xu Q., et al. Generation and characterization of androgen receptor knockout (ARKO) mice: an in vivo model for the study of androgen functions in selective tissues. Proceedings of the National Academy of Sciences. 2002;99(21):13498–13503. doi: 10.1073/pnas.212474399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Florin A., Maire M., Bozec A., et al. Androgens and postmeiotic germ cells regulate claudin-11 expression in rat sertoli cells. Endocrinology. 2005;146(3):1532–1540. doi: 10.1210/en.2004-0834. [DOI] [PubMed] [Google Scholar]
- 26.Meng J., Holdcraft R. W., Shima J. E., Griswold M. D., Braun R. E. Androgens regulate the permeability of the blood-testis barrier. Proceedings of the National Academy of Sciences. 2005;102(46):16696–16700. doi: 10.1073/pnas.0506084102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu W., Liu Y., Zhu R., et al. Structure characterization, chemical and enzymatic degradation, and chain conformation of an acidic polysaccharide from Lycium barbarum L. Carbohydrate Polymers. 2016;147:114–124. doi: 10.1016/j.carbpol.2016.03.087. [DOI] [PubMed] [Google Scholar]
- 28.Cheng J., Zhou Z. W., Sheng H. P., et al. An evidence-based update on the pharmacological activities and possible molecular targets of Lycium barbarum polysaccharides. Drug Design, Development and Therapy. 2015;9:33–78. doi: 10.2147/DDDT.S72892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo Q., Li Z., Huang X., Yan J., Zhang S., Cai Y.-Z. Lycium barbarum polysaccharides: protective effects against heat-induced damage of rat testes and H2O2-induced DNA damage in mouse testicular cells and beneficial effect on sexual behavior and reproductive function of hemicastrated rats. Life Sciences. 2006;79(7):613–621. doi: 10.1016/j.lfs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Luo Q., Li J., Cui X., Yan J., Zhao Q., Xiang C. The effect of Lycium barbarum polysaccharides on the male rats׳ reproductive system and spermatogenic cell apoptosis exposed to low-dose ionizing irradiation. Journal of Ethnopharmacology. 2014;154(1):249–258. doi: 10.1016/j.jep.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 31.Varoni M. V., Gadau S. D., Pasciu V., et al. Investigation of the effects of Lycium barbarum polysaccharides against cadmium induced damage in testis. Experimental and Molecular Pathology. 2017;103(1):26–32. doi: 10.1016/j.yexmp.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 32.Shi G.-J., Zheng J., Wu J., et al. Protective effects of Lycium barbarum polysaccharide on male sexual dysfunction and fertility impairments by activating hypothalamic pituitary gonadal axis in streptozotocin-induced type-1 diabetic male mice. Endocrine Journal. 2017;64(9):907–922. doi: 10.1507/endocrj.ej16-0430. [DOI] [PubMed] [Google Scholar]
- 33.Guo J., Tao S.-X., Chen M., et al. Heat treatment induces liver receptor homolog-1 expression in monkey and rat sertoli cells. Endocrinology. 2007;148(3):1255–1265. doi: 10.1210/en.2006-1004. [DOI] [PubMed] [Google Scholar]
- 34.Zhang Y., Sun H.-M., He X., et al. Da-Bu-Yin-Wan and Qian-Zheng-San, two traditional Chinese herbal formulas, up-regulate the expression of mitochondrial subunit NADH dehydrogenase 1 synergistically in the mice model of Parkinson’s disease. Journal of Ethnopharmacology. 2013;146(1):363–371. doi: 10.1016/j.jep.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Y., Gong X.-G., Wang Z.-Z., et al. Overexpression of DJ-1/PARK7, the Parkinson’s disease-related protein, improves mitochondrial function via Akt phosphorylation on threonine 308 in dopaminergic neuron-like cells. European Journal of Neuroscience. 2016;43(10):1379–1388. doi: 10.1111/ejn.13216. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y., Gong X. G., Sun H. M., et al. Da-Bu-Yin-Wan improves the ameliorative effect of DJ-1 on mitochondrial dysfunction through augmenting the Akt phosphorylation in a cellular model of Parkinson’s disease. Frontiers in Pharmacology. 2018;9:p. 1206. doi: 10.3389/fphar.2018.01206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun M., Yang L., Feldman R. I., et al. Activation of phosphatidylinositol 3-kinase/Akt pathway by androgen through interaction of p85α, androgen receptor, and Src. Journal of Biological Chemistry. 2003;278(44):42992–43000. doi: 10.1074/jbc.m306295200. [DOI] [PubMed] [Google Scholar]
- 38.Amagase H., Farnsworth N. R. A review of botanical characteristics, phytochemistry, clinical relevance in efficacy and safety of Lycium barbarum fruit (Goji) Food Research International. 2011;44(7):1702–1717. doi: 10.1016/j.foodres.2011.03.027. [DOI] [Google Scholar]
- 39.Jin M., Huang Q., Zhao K., Shang P. Biological activities and potential health benefit effects of polysaccharides isolated from Lycium barbarum L. International Journal of Biological Macromolecules. 2013;54:16–23. doi: 10.1016/j.ijbiomac.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 40.Kwok S. S., Bu Y. S., Lo A. C. Y., et al. A systematic review of potential therapeutic use of Lycium barbarum polysaccharides in disease. Biomed Research International. 2019;2019:18. doi: 10.1155/2019/4615745.4615745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Costa G. M. J., Lacerda S. M. S. N., Figueiredo A. F. A., Leal M. C., Rezende-Neto J. V., França L. R. Higher environmental temperatures promote acceleration of spermatogenesis in vivo in mice (Mus musculus) Journal of Thermal Biology. 2018;77:14–23. doi: 10.1016/j.jtherbio.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Danno S., Itoh K., Matsuda T., Fujita J. Decreased expression of mouse Rbm3, a cold-shock protein, in sertoli cells of cryptorchid testis. The American Journal of Pathology. 2000;156(5):1685–1692. doi: 10.1016/s0002-9440(10)65039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hikim A. P. S., Lue Y., Yamamoto C. M., et al. Key apoptotic pathways for heat-induced programmed germ cell death in the testis. Endocrinology. 2003;144(7):3167–3175. doi: 10.1210/en.2003-0175. [DOI] [PubMed] [Google Scholar]
- 44.Cai H., Ren Y., Li X.-X., et al. Scrotal heat stress causes a transient alteration in tight junctions and induction of TGF-β expression. International Journal of Andrology. 2011;34(4):352–362. doi: 10.1111/j.1365-2605.2010.01089.x. [DOI] [PubMed] [Google Scholar]
- 45.He M., Wang L., Chen Y., Zhang T., Guo J. Effect of Wuziyanzong pill on levels of sex hormones, and expressions of nuclear- associated antigen Ki-67 and androgen receptor in testes of young rats. Journal of Traditional Chinese Medicine. 2016;36:743–748. doi: 10.1016/s0254-6272(17)30009-2. [DOI] [PubMed] [Google Scholar]
- 46.Pei Y., Wu Y., Qin Y. Effects of chronic heat stress on the expressions of heat shock proteins 60, 70, 90, A2, and HSC70 in the rabbit testis. Cell Stress and Chaperones. 2012;17(1):81–87. doi: 10.1007/s12192-011-0287-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miettinen M., Virtanen I., Talerman A. Intermediate filament proteins in human testis and testicular germ-cell tumors. The American journal of pathology. 1985;120:402–10. [PMC free article] [PubMed] [Google Scholar]
- 48.Sobecki M., Mrouj K., Colinge J., et al. Cell-cycle regulation accounts for variability in Ki-67 expression levels. Cancer Research. 2017;77(10):2722–2734. doi: 10.1158/0008-5472.can-16-0707. [DOI] [PubMed] [Google Scholar]
- 49.McCoard S., Wise T., Lunstra D., Ford J. Stereological evaluation of sertoli cell ontogeny during fetal and neonatal life in two diverse breeds of swine. Journal of Endocrinology. 2003;178(3):395–403. doi: 10.1677/joe.0.1780395. [DOI] [PubMed] [Google Scholar]
- 50.Franke F. E., Pauls K., Rey R., Marks A., Bergmann M., Steger K. Differentiation markers of sertoli cells and germ cells in fetal and early postnatal human testis. Anatomy and Embryology. 2004;209:169–77. doi: 10.1007/s00429-004-0434-x. [DOI] [PubMed] [Google Scholar]
- 51.Zhang X.-S., Zhang Z.-H., Guo S.-H., et al. Activation of extracellular signal-related kinases 1 and 2 in sertoli cells in experimentally cryptorchid rhesus monkeys. Asian Journal of Andrology. 2006;8(3):265–272. doi: 10.1111/j.1745-7262.2006.00142.x. [DOI] [PubMed] [Google Scholar]
- 52.Fedder J. Prevalence of small testicular hyperechogenic foci in subgroups of 382 non-vasectomized, azoospermic men: a retrospective cohort study. Andrology. 2017;5(2):248–255. doi: 10.1111/andr.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mruk D. D., Cheng C. Y. The mammalian blood-testis barrier: its biology and regulation. Endocrine Reviews. 2015;36(5):564–591. doi: 10.1210/er.2014-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McCabe M. J., Foo C. F., Dinger M. E., Smooker P. M., Stanton P. G. Claudin-11 and occludin are major contributors to sertoli cell tight junction function, in vitro. Asian Journal of Andrology. 2016;18:620–626. doi: 10.4103/1008-682X.163189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagano T., Suzuki F. The postnatal development of the junctional complexes of the mouse sertoli cells as revealed by freeze-fracture. The Anatomical Record. 1976;185(4):403–417. doi: 10.1002/ar.1091850403. [DOI] [PubMed] [Google Scholar]
- 56.Cyr D. G., Hermo L., Egenberger N., Mertineit C., Trasler J. M., Laird D. W. Cellular immunolocalization of occludin during embryonic and postnatal development of the mouse testis and epididymis∗. Endocrinology. 1999;140(8):3815–3825. doi: 10.1210/endo.140.8.6903. [DOI] [PubMed] [Google Scholar]
- 57.Gerber J., Weider K., Hambruch N., Brehm R. Loss of connexin43 (Cx43) in sertoli cells leads to spatio-temporal alterations in occludin expression. Histology and Histopathology. 2014;29:935–948. doi: 10.14670/HH-29.935. [DOI] [PubMed] [Google Scholar]
- 58.Chang L., Lu Z., Li D., et al. Melamine causes testicular toxicity by destroying blood-testis barrier in piglets. Toxicology Letters. 2018;296:114–124. doi: 10.1016/j.toxlet.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 59.Van Itallie C. M., Anderson J. M. Architecture of tight junctions and principles of molecular composition. Seminars in Cell & Developmental Biology. 2014;36:157–165. doi: 10.1016/j.semcdb.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smith B. E., Braun R. E. Germ cell migration across sertoli cell tight junctions. Science. 2012;338(6108):798–802. doi: 10.1126/science.1219969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Erkanli Senturk G., Ersoy Canillioglu Y., Umay C., Demiralp-Eksioglu E., Ercan F. Distribution of zonula occludens-1 and occludin and alterations of testicular morphology after in utero radiation and postnatal hyperthermia in rats. International Journal of Experimental Pathology. 2012;93:438–449. doi: 10.1111/j.1365-2613.2012.00844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Saitou M., Fujimoto K., Doi Y., et al. Occludin-deficient embryonic stem cells can differentiate into polarized epithelial cells bearing tight junctions. Journal of Cell Biology. 1998;141(2):397–408. doi: 10.1083/jcb.141.2.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sharpe R., McKinnell C., Kivlin C., Fisher J. Proliferation and functional maturation of sertoli cells, and their relevance to disorders of testis function in adulthood. Reproduction. 2003;125:769–784. doi: 10.1530/rep.0.1250769. [DOI] [PubMed] [Google Scholar]
- 64.Regadera J., Martinez-Garcia F., Gonzalez-Peramato P., Serrano A., Nistal M., Suarez-Quian C. Androgen receptor expression in sertoli cells as a function of seminiferous tubule maturation in the human cryptorchid testis. Journal of Clinical Endocrinology & Metabolism. 2001;86(1):413–421. doi: 10.1210/jc.86.1.413. [DOI] [PubMed] [Google Scholar]
- 65.Willems A., Batlouni S. R., Esnal A., et al. Selective ablation of the androgen receptor in mouse sertoli cells affects sertoli cell maturation, barrier formation and cytoskeletal development. PloS One. 2010;5:p. e14168. doi: 10.1371/journal.pone.0014168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Manning B. D., Cantley L. C. AKT/PKB signaling: navigating downstream. Cell. 2007;129(7):1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Meroni S. B., Galardo M. N., Rindone G., Gorga A., Riera M. F., Cigorraga S. B. Molecular mechanisms and signaling pathways involved in sertoli cell proliferation. Frontiers in Endocrinology. 2019;10:p. 224. doi: 10.3389/fendo.2019.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu P., Wang Z., Wei W. Phosphorylation of Akt at the C-terminal tail triggers Akt activation. Cell Cycle. 2014;13(14):2162–2164. doi: 10.4161/cc.29584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fan Y., Liu Y., Xue K., et al. Diet-induced obesity in male C57BL/6 mice decreases fertility as a consequence of disrupted blood-testis barrier. PloS One. 2015;10:p. e0120775. doi: 10.1371/journal.pone.0120775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lin N., Xu L.-F., Sun M. The protective effect of trefoil factor 3 on the intestinal tight junction barrier is mediated by toll-like receptor 2 via a PI3K/Akt dependent mechanism. Biochemical and Biophysical Research Communications. 2013;440(1):143–149. doi: 10.1016/j.bbrc.2013.09.049. [DOI] [PubMed] [Google Scholar]
- 71.Liu X., Zhang X., Ma K., et al. Matrine alleviates early brain injury after experimental subarachnoid hemorrhage in rats: possible involvement of PI3K/Akt-mediated NF-kappaB inhibition and Keap1/Nrf2-dependent HO-1 inductionn. Cellular and Molecular Biology (Noisy-Le-Grand, France) 2016;62:38–44. [PubMed] [Google Scholar]
- 72.Mao B., Mruk D., Lian Q., et al. Mechanistic insights into PFOS-mediated sertoli cell injury. Trends in Molecular Medicine. 2018;24(9):781–793. doi: 10.1016/j.molmed.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Deng Q., Zhang Z., Wu Y., et al. Non-genomic action of androgens is mediated by rapid phosphorylation and regulation of androgen receptor trafficking. Cellular Physiology and Biochemistry. 2017;43(1):223–236. doi: 10.1159/000480343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the conclusions of this article are included within the article.


