Abstract
Background:
Multimorbidity, the co-occurrence of two or more chronic diseases, is more common than having a single chronic disease, especially among persons age 65 years and older. The routine measurement of multimorbidity can facilitate a better understanding of potential causes and interactions and promote more effective treatment and improved outcomes.
Objectives:
To present a multimorbidity research framework and identify gaps in the research literature related to multimorbidity.
Design:
In preparation for an expert panel workshop convened in September 2018, planning committee members reviewed the literature and developed a guiding framework that informed the selection of topics and speakers.
Results:
The framework, grounded in a patient-centered approach, incorporates the concept of concordant and discordant comorbidity, and includes potential causes, interactions, and outcomes. This work informed workshop presentations and discussion related to identifying and selecting the best available multimorbidity instruments and determining future research needs.
Conclusions:
Multimorbidity research can be advanced by addressing gaps in study design and target populations, and by increasing attention to universal outcome measurement.
Multimorbidity, the co-occurrence of two or more chronic diseases, increases with aging and is found in the majority of persons age 65 years and older.1 Considerable research has been conducted on concordant comorbid conditions, such as diabetes and hypertension, which may have shared care goals and risk management.2 More recently, attention has drawn to discordant conditions, not directly related in either their pathogenesis or management and without an underlying predisposing factor. For example, research into the co-occurrence of physical and mental illness, such as diabetes and depression, has begun to flourish. After noting that people had worse treatment outcomes for both co-occurring diabetes and depression, the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institute of Mental Health held an international conference in 2012, which developed a research agenda for the combined conditions. NIH initiated drug treatment trials in this population along with basic studies of the underlying biology and pathophysiology. The series of trials ultimately led to a collaborative care model, which improved outcomes of depression, controlled blood glucose, blood pressure and low-density lipoproteins.3
While many of the NIH Institutes and Centers (ICs) focus on specific diseases and much of the research has been targeting single diseases, recent efforts signal an ongoing shift to increasing research on multimorbidity. Program officials from several NIH ICs have begun to discuss common interests related to multimorbidity. They recognized the need to evaluate the current state of research on measuring multimorbidity, and identified the lack of a framework organizing the research. They began to develop a research agenda on the topic, which was refined based on the presentations and discussion that took place during an NIH-convened multimorbidity measurement workshop in 2018.
Methods
In 2017, several NIH ICs—including the National Institute on Aging, Office of Disease Prevention, National Cancer Institute, National Institute on Minority Health and Health Disparities, and Office of Behavioral and Social Sciences Research—formed a committee to plan an expert panel workshop entitled, “Measuring Multimorbidity: Matching the Instrument and the Purpose”, held on September 25–26, 2018. The committee, comprised of NIH staff with expertise in multimorbidity, chronic disease prevention, epidemiology, and behavioral science, met monthly for a year prior to the workshop. Committee activities included reviewing relevant literature and developing a guiding framework that informed the selection of workshop topics and speakers. The workshop speakers provided further expertise in multimorbidity, chronic disease treatment, geriatrics, pediatrics, clinical medicine, informatics, and statistics.
Results
The research framework (Figure 1) developed by the NIH IC planning committee incorporates the concept of concordant and discordant comorbidity, and includes potential causes, interactions, and outcomes. The patient with multimorbidities is at the center of the framework, represented by a large circle. Within the large circle are smaller colored circles representing the patient’s multiple chronic conditions. The framework depicts the influence of multiple factors that may cause, increase risk for, or exacerbate each condition including environmental, biological, physiological, behavioral, and social and life course or aging factors. Understanding the influence of these factors on each disease and interactions with comorbid conditions may inform prevention strategies that could have substantial public health impact. Interactions among the treatments and co-occurring conditions may worsen universal and disease-specific outcomes (e.g., functional status, quality of life, and mortality), shown at right. Drugs (or other therapies) may interact with comorbid diseases and worsen the disease outcomes, known as therapeutic competition.4 Nutritional factors may also affect onset of and may interact with the disease, and sometimes treatment. Nutritional intake is especially important for certain types of multimorbidity prevention and can also be essential in the management of multimorbidity. The framework is grounded in a patient-centered approach. It illustrates that prevention strategies (e.g., smoking cessation, increasing physical activity) may be applied to the causative factors, while treatment strategies may impact both disease interactions and health outcomes. Multimorbidity may be a focus of primary prevention (to prevent development of multimorbidity in the first place) and secondary prevention (to prevent poor outcomes of multimorbidity after it has developed).
Figure 1.
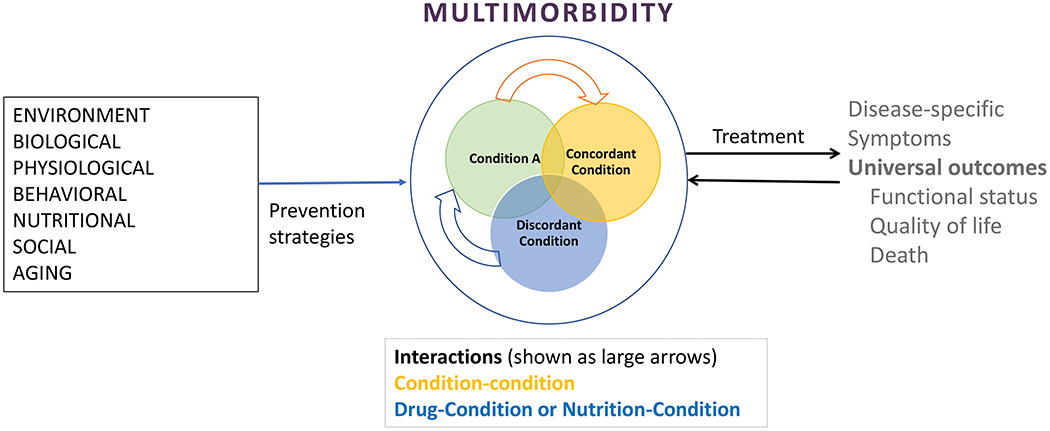
Conceptual model and research framework for multimorbidity, depicting relationships among causal factors, disease conditions and interactions, and outcomes of multimorbidity.
The NIH IC planning committee also identified relevant literature in preparation for the workshop; this literature informed workshop discussions and the identification of research gaps and future directions (Table 1). Highlighted areas included gaps in study design such as the need for relevant epidemiological and longitudinal studies, gaps in disparity or age-based studies, and gaps in intervention studies and health outcomes research. The workshop focused on pragmatic measurement approaches that are currently in use such as personal self-report measures in surveys; diagnostic codes in billing records; and more elaborate clinical methods in dedicated (mainly single-disease focused) studies. Expert panel members also endorsed the need for improved infrastructure to measure multimorbidity in clinical practice such as linking patients’ electronic health records to other records of health interventions and drug treatment (e.g., pharmacy records). Guidance on multimorbidity instrument selection to match the study purpose and data source is published elsewhere.5
Table 1:
Selected research gaps in the measurement of multimorbidity
| 1. Gaps in study design |
| • Rigorous measurement of multiple diseases in epidemiological or mechanistic studies |
| • Longitudinal studies to examine onset and/or fluctuation in multimorbidity |
| • Expansion of single-disease-focused studies or dominant conditions to include measurement of multimorbidity and disease severity |
| 2. Gaps in disparity or age-based studies |
| • Studies of multimorbidity in diverse, underserved, and vulnerable populations |
| • Studies of a variety of rare disease combinations of multimorbidity in children |
| • Inclusion of geriatric syndromes, including dementia (and its causes) among older adults |
| 3. Gaps in Intervention Studies and health outcomes research |
| • Development of person-centered approaches to the care of persons with multimorbidity, including contextual targeting (including age, gender, social context, economics, and dominant health conditions) |
| • Advancing universal outcome measurement and matching outcome measurement to the purpose of measuring multimorbidity |
| • Use of modeling and simulations to improve multimorbidity measurement in systems of care |
Discussion
In addition to the benefits of multimorbidity measurement outlined in the research framework, routine measurement of multimorbidity in studies can facilitate comparison with available population data, make assessment of the applicability of the evidence developed feasible, and be used to judge whether and how the findings might be generalized to a population. In a randomized trial, multimorbidity balance is important to exclude the potential for confounding. Further, the identification of a subgroup with multimorbidity can be an exploratory approach to further investigation. In population studies, consistent measurement of multimorbidity can be used to examine trends. It is important to consider whether measuring the disease and multimorbidity is sufficient, or whether the disease severity also needs to be measured. Disease severity is included in some but not all multimorbidity measurement tools.5
Basic biology studies should include measurement of multimorbidity to check for novel mechanisms or pathways that might explain disease clustering. Epidemiological studies can elucidate combinations occurring more frequently than might be expected by chance alone. Late stage treatment studies should enroll persons with multimorbidity and consider whether the efficacy or effectiveness differs among those with and without multimorbidity. Understanding why disparities in multimorbidity occur and why earlier onset is observed in some racial and ethnic populations needs further study.
Multimorbidity measurement is needed in research on new models of care for patients with multiple chronic conditions. Improved and highly effective person-centered care is paramount, particularly for primary care and geriatrics. The coordination of care for multimorbidity is particularly needed for the discordant conditions as well as for persons whose care is managed by multiple specialists. Disease-specific guidelines should consider and explain how to modify care for persons with common multimorbid combinations.
NIH is increasing its focus on measuring multimorbidity for purposes of comparative and evaluative research and to ensure that research is equitable. The NIH ICs are developing new collaborations to advance understanding of the biology, mechanisms and potential treatment approaches for prevalent multimorbidity. The All of Us program,6 a large-scale NIH research initiative that is collecting genetic and health data to advance individualized medical care, may be leveraged to enhance multimorbidity research into causes and personalization of treatments for specific disease combinations. The recent NIH inclusion policy,7 which calls for enrolling an increasing representation of study participants across the lifespan, will likely foster multimorbidity research among older adults and racial/ethnic minority groups. Yet, it may not achieve its scientific promise without an accompanying effort to characterize multimorbidity, which is only partially represented by the proxy measure of age. Innovative research to tease out the causal links that tie certain combinations of chronic conditions, develop interventions and put them into practice, will be needed to attain improvements in health outcomes.
Conclusions
Based on this workshop, NIH has developed a multi-institute initiative to expand research on the measurement, causes and consequences of multimorbidity. It will address the priorities of the multiple institutes, centers and offices, and indicates the wide scope and applicability of the topic. The initiative intends to also develop and evaluate interventions for multimorbidity treatment and prevention that address its widespread sequelae.8–9
Acknowledgements:
This manuscript is based on a research workshop funded in part by the National Institute on Aging; Office of Disease Prevention, NIH; National Cancer Institute; National Institute on Minority Health and Health Disparities; Office of Behavioral and Social Sciences Research, NIH. The Planning Committee members included Marcel E. Salive, Jerry Suls, Tilda Farhat, Carrie Klabunde, and Deborah Young-Hyman, who moderated sessions in the workshop. The workshop speakers, who had an opportunity to comment on this manuscript, are gratefully acknowledged, including Elizabeth A. Bayliss, Jay Berry, Arlene Bierman, Elizabeth Chrischilles, Lisa Cooper, Shanta Rishi Dube, Martin Fortin, Jerry Gurwitz, Gabi Kastenmüller, Siran Koroukian, Shari Ling, Kimberly Lochner, Ana Quinones, Walter Rocca, Shabnam Salimi, Jeffrey H. Silber, Michael Steinman, Theo Vos, Brian W. Ward, and Melissa Wei.
Footnotes
This material should not be interpreted as representing the viewpoint of the US Department of Health and Human Services, the National Institutes of Health, or its represented agencies.
No conflicts
Contributor Information
Marcel E. Salive, Geriatrics Branch, National Institute on Aging 7201 Wisconsin Ave, Suite 3W200, Bethesda, MD 20892-9205.
Jerry Suls, Behavioral Research Program, National Cancer Institute; Currently at Feinstein Institutes for Medical Research/Northwell Health, 130 East 59th Street, Suite 14C, New York City, NY 10022.
Tilda Farhat, Office of Science Policy, Planning, Evaluation, and Reporting, National Institute on Minority Health and Health Disparities, National Institutes of Health, 6707 Democracy Blvd., Suite 800, Bethesda, MD 20892.
Carrie N. Klabunde, Office of Disease Prevention, National Institutes of Health, 6100 Executive Drive, Room 2B03 MSC 7523, Bethesda, MD 20892.
References:
- 1.King DE, Xiang J, Pilkerton CS. Multimorbidity Trends in United States Adults, 1988–2014. Journal of the American Board of Family Medicine : JABFM. 2018;31(4):503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piette JD KE. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–731. [DOI] [PubMed] [Google Scholar]
- 3.Von Korff M, Katon WJ, Lin EH, et al. Functional outcomes of multi-condition collaborative care and successful ageing: results of randomised trial. BMJ (Clinical research ed). 2011;343:d6612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lorgunpai SJ, Grammas M, Lee DS, McAvay G, Charpentier P, Tinetti ME. Potential therapeutic competition in community-living older adults in the U.S.: use of medications that may adversely affect a coexisting condition. PloS one. 2014;9(2):e89447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suls J, Bayliss E, Bierman AS, Berry J, Chrischilles EA, Farhat T, et al. Measuring Multimorbidity: Selecting the Right Instrument for the Purpose and the Data Source. Medical Care. 2020:xxx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denny JC, Rutter JL, Goldstein DB, et al. The “All of Us” Research Program. The New England journal of medicine. 2019;381(7):668–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernard MA, Clayton JA, Lauer MS. Inclusion Across the Lifespan: NIH Policy for Clinical Research. JAMA. 2018;320(15):1535–1536. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health and Human Services. PAR 20–179: Advancing Research to Develop Improved Measures and Methods for Understanding Multimorbidity (R01 Clinical Trial Optional). Available at: https://grants.nih.gov/grants/guide/pa-files/par-20-179.html. Accessed on January 15, 2021.
- 9.Department of Health and Human Services. PAR 20–180: Identifying Innovative Mechanisms or Interventions that Target Multimorbidity and Its Consequences (R01 Clinical Trial Optional). Available at: https://grants.nih.gov/grants/guide/pa-files/par-20-180.html. Accessed on January 15, 2021.


