Abstract
Turmeric, the rhizome of Curcuma longa plant belonging to the ginger family Zingiberaceae, has a history in Ayurvedic and traditional Chinese medicine for treatment of chronic diseases, including metabolic and cardiovascular diseases (CVD). This parallels a prevalence of age- and lifestyle-related diseases, especially CVD and type 2 diabetes (T2D), and associated mortality which has occurred in recent decades. While the chemical composition of turmeric is complex, curcuminoids and essential oils are known as two major groups that display bioactive properties. Curcumin, the most predominant curcuminoid, can modulate several cell signaling pathways involved in the etiology and pathogenesis of CVD, T2D, and related morbidities. Lesser bioactivities have been reported from other curcuminoids and essential oils. This review examines the chemical compositions of turmeric, and related bioactive constituents. A focus was placed on the cellular and molecular mechanisms that underlie the protective effects of turmeric and turmeric-derived compounds against diabetes and CVD, compiled from the findings obtained with cell-based and animal models. Evidence from clinical trials is also presented to identify potential preventative and therapeutic efficacies. Clinical studies with longer intervention durations and specific endpoints for assessing health outcomes are warranted in order to fully evaluate the long-term protective efficacy of turmeric.
Keywords: Curcumin, Curcuminoids, Turmeric oil, Diabetes, Cardiovascular diseases, Human clinical trials
Introduction
Curcuma longa Linn. (Syn. Curcuma domestica Valeton) belongs to the ginger family Zingiberaceae, a perennial plant that grows in tropical and humid climates and originates from the Indian Subcontinent and Southeast Asia [1, 2]. The term longa refers to the elongated shape of the rhizome, where turmeric is derived from the rhizome of the plant having a characteristic orange-yellow color. The term for turmeric varies among languages, but most often it refers to “yellow colour” or “bright colour” [3]. The Latin word curcuma is believed to be derived from the Arabic root kurkum meaning “saffron,” in reference to similar coloring properties [4]. Turmeric is also known as “Indian saffron.”
The history of using turmeric dates back to more than 4000 years during the Vedic age of India, where it was initially used as a dye and a culinary spice, due to its bright yellow color and aromatic flavor [2, 3]. Turmeric also has a spiritual significance, where with the Hindu religion, turmeric was connected with South East Asian countries by 700 AD, migrating later to West and East African countries during 800 to 1200 AD [2, 3]. Turmeric has become a commonly cultivated seed in many of these countries and regions. Along with the history of use, turmeric has had an important role in folk medicine, especially Ayurveda and traditional Chinese medicine where it was used as a remedy for various diseases that range from simple ailments to more complex chronic illnesses, such as digestive (e.g., abdominal pain and bloating, dyspepsia), cardiovascular (e.g., heart burning, heart pain), respiratory (e.g., runny nose, sinusitis, asthma), and hepatic disorders [1, 5–8]. On the other hand, turmeric although arriving in Europe in the 13th century by Arab traders currently remains a minor spice in Western countries. Until more recently, turmeric has been recognized, and since gained popularity as a dietary supplement and a nutraceutical thus becoming one of the most successful natural health products sold in the US since 2013 [9]. Recent studies that have also shown therapeutic potential of turmeric against coronavirus disease 2019 (COVID-19) [10] and the potential to modulate cytokine storm in COVID-19 patients [11] have produced formidable renewed interest in this herb.
Notwithstanding the long history of using turmeric in traditional medicine to treat various diseases, the mechanism or scientific basis for its bioactivity has remained unclear, until more recently when pharmacological assessments demonstrated safe use for modern medicine [3]. Curcuminoids and essential oils (mainly terpenoids) are two major components present in turmeric, the former being responsible for the orange-yellow color of the herb and the latter accounting for the aromatic flavor [12]. These components also possess a wide range of bioactivities (Table 1), for which evidence has been substantiated at all levels of inquiry that range from in vitro and in vivo experiments to human clinical studies [12, 13]. Curcumin, a principal and abundant curcuminoid in turmeric, has been extensively studied for bioactivity in pharmaceutical studies [14]. Albeit a majority of preclinical and clinical studies have focused on the efficacy of turmeric extracts and isolated curcumin, relatively less information exists on bioactivity of other curcuminoids and essential oils present from turmeric for potential use in modern-day medicinal and nutraceutical industries [12].
Table 1.
Major bioactivities of turmeric and its bioactive constituents that relate to specific health disorders
| Health disorder | Reported bioactivity | References |
|---|---|---|
| Oxidative stress | Antioxidant | [15–18] |
| Inflammation and inflammatory diseases |
Anti-inflammatory Immunomodulatory |
[19–21] |
| Allergy | Anti-allergic | [22–24] |
| Cardiovascular diseases |
Hypolipidemic Atheroprotective Cardioprotective |
[25–28] |
| Diabetes |
Hypoglycemic Antiglycation Antidiabetic |
[29–32] |
| Cancer |
Antitumor Pro-apoptotic Antimetastatic Anticancer |
[33–36] |
| Neurodegenerative diseases | Neuroprotective | [37–39] |
| Depression | Antidepressant | [40–42] |
| Liver diseases | Hepatoprotective | [43–45] |
Among the various bioactivities possessed by turmeric and its bioactive components listed in Table 1 [15–45], the antidiabetic and cardioprotective effects have attracted pronounced attention from numerous researchers with a common interest in understanding the role of turmeric and related bioactives in the protection against cardiovascular diseases (CVD), that currently exists as a leading cause of mortality worldwide. Diabetes is also one of the top 10 causes of death and is often associated with onset of CVD [46]. Although a number of therapeutic strategies for diabetes and CVD have been developed and tested, there are limited applications because of the high costs, low accessibility, and complications [14].
This review provides an overview on the complex chemical composition of turmeric and its bioactive constituents that are involved in metabolic health benefits. Furthermore, we review mechanistic preclinical (in vitro and in vivo) evidence on the antidiabetic and cardioprotective effects attributed to turmeric constituents. A comprehensive discussion on the cellular and molecular mechanisms that corroborates the beneficial outcomes observed from human clinical trials is given.
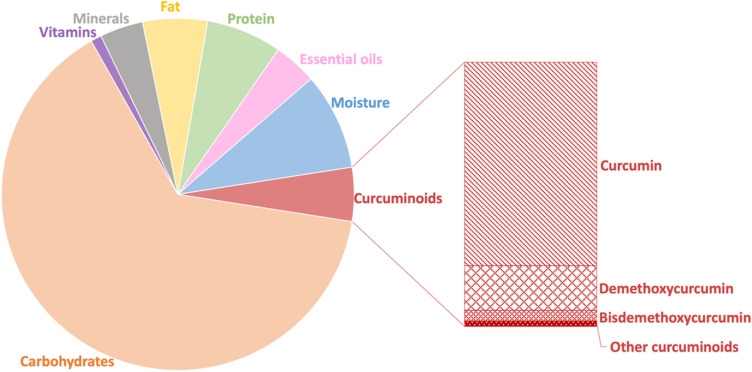
Chemical composition of turmeric
Proximate analysis (Fig. 1) of turmeric reveals that the herb contains 6–13% moisture, with 60–70% carbohydrate, 6–8% protein, 5–10% fat, 3–7% minerals (potassium, sodium, calcium, iron, phosphorus), and trace amounts of vitamins [47–49]. Essential oils obtained by steam distillation represent 3–7% of the turmeric rhizome and mainly consist of terpenoids, including sesquiterpenoids (e.g., α-phellandrene, zingiberene), monoterpenoids (e.g., sabinene, cineol), and norsesquiterpenoids [12, 49]. There is also 3–5% curcuminoids, which comprises more than 50 structurally related compounds; the three principal ones being curcumin, demethoxycurcumin, and bisdemethoxycurcumin [47]. In general, turmeric composition varies according to the soil conditions used in cultivation, with Indian turmeric being regarded as having superior quality and high curcumin content [3]. Curcuminoids and essential oils are classified as secondary metabolites produced by Curcuma plants, with well-defined bioactivity [50].
Fig. 1.
Curcuminoids
Curcuminoids are bioactive phenolic compounds and consist of more than 100 individual curcuminoids that have been isolated and identified from genus Curcuma, about 50 of which are present in C. longa (turmeric). Turmeric contains three major curcuminoids: curcumin (CUR; 77%), demethoxycurcumin (DMC; 17%), and bisdemethoxycurcumin (BMC; 3–6%) [12, 47].
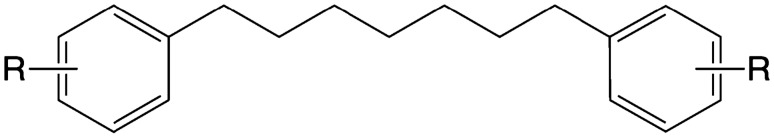
Strictly speaking, curcuminoids only refer to linear diphenylheptanoids with a skeleton structure that has two aromatic rings linked by a heptane chain (Fig. 2) [51]. By this definition, there are 15 curcuminoids isolated and identified in turmeric (C. longa).
Fig. 2.
Skeleton structure of diphenylheptanoids
The definition of curcuminoids has expanded to include any orange-yellow-colored compounds present in turmeric that are structurally related to the principal constituent curcumin [51]. Specifically, there must be two aryl groups (aromatic rings) linked by an aliphatic chain, which is usually a heptane (7C) chain (Compounds 1–15), or a pentane (5C) chain (Compounds 16–18). Alternatively, a cyclic chain structure exists (Compounds 19–21). Cyclization of the heptane chain leads to the formation of a furanone ring, as shown in curcumalongin A and B (Compounds 20, 21), or a pyrone ring present in cyclcocurcumin (Compound 22). These are generally not common and found only in C. longa. The structures and names of these compounds are presented in Table 2 [52–56]. More recently, uncommon structures of curcuminoids that are conjugated with monoterpenes or sesquiterpenes have been isolated from turmeric and have been termed terpecurcuminoids or terpenoid-conjugated curcuminoids [57].
Table 2.
Unconjugated curcuminoids present in the rhizome of C. longa
| No. | Compound name | Structure | Reference |
|---|---|---|---|
| 1 | Curcumin |

|
[52] |
| 2 | Demethoxycurcumin (DMC) | ||
| 3 | Bisdemethoxycurcumin (BDMC) | ||
| 4 | (1E,6E)-1-(3,4-dihydroxyphenyl)-7-(4- hydroxyphenyl)-1,6-heptadiene-3,5-dione | [53] | |
| 5 |
(1E,6E)-1,7-Bis(3,4-dihydroxyphenyl)-1, 6-heptadiene-3,5-dione (Didemethyl curcumin) |
[54] | |
| 6 |
(1E,6E)-1-(3,4-dihydroxyphenyl)-7- (4-hydroxy-3-methoxyphenyl)-1, 6-heptadiene-3,5-dione (Monodemethylcurcumin) |
[53, 55] | |
| 7 | Curcumalongin C | [54] | |
| 8 |
(1E,6E)-1-(4-hydroxy-3,5-dimethoxyphenyl)-7-(4-hydroxy-3-methoxyphenyl)- 1,6-heptadiene-3,5-dione (5′-methoxycurcumin) |
[55] | |
| 9 | (1E,4E,6E)-1,7-bis(4-hydroxyphenyl)-1,4,6-heptatrien-3-one |
|
[55] |
| 10 | (4Z,6E)-5-hydroxy-1,7-bis-(4-hydroxyphenyl)-4,6-heptadien-3-one |
|
[53] |
| 11 | (6E)-3-hydroxy-1,7-bis (4-hydroxyphenyl)-6-heptene-1,5-dione |
|
[53] |
| 12 | (4Z,6E)-1,5-dihydroxy-1,7-bis-(4-hydroxyphenyl)-4,6-heptadien-3-one |

|
[53] |
| 13 | (4Z,6E)-1,5-dihydroxy-1-(4-hydroxyphenyl)-7-(4-hydroxy-3-methoxyphenyl)- 4,6-heptadien-3-one | ||
| 14 | (4Z,6E)-1,5-dihydroxy-1-(4-hydroxy-3-methoxyphenyl)-7-(4-hydroxyphenyl)- 4,6-heptadien-3-one | ||
| 15 | (4Z,6E)-1,5-dihydroxy-1,7-bis(4-hydroxy-3- methoxyphenyl)-4,6-heptadien-3-one | ||
| 17 | 1,5-Bis(4-hydroxyphenyl)-1,4-pentadiene-3-one |
|
[52] |
| 18 | (1E,4E)-1-(4-hydroxy-3-methoxyphenyl)-5-(4-hydroxyphenyl)-1,4-pentadien-3-one | ||
| 19 | (1E,4E)-1,5-bis(4-hydroxy-3- methoxyphenyl)-penta-1,4-dien-3-one | ||
| 20 | Curcumalongin A |
|
[54] |
| 21 | Curcumalongin B | ||
| 22 | Cyclocurcumin |
|
[56] |
Curcuminoids are readily soluble in polar organic solvents, such as dimethyl sulfoxide (DMSO), acetone, methanol, and ethanol, but are poorly soluble in water, lipids, and hydrocarbons, like cyclohexane and hexane [47, 58]. The 1,3-diketone group in curcumin and some curcuminoids (Compounds 1–8) exhibit keto–enol tautomerism, and therefore exist in keto and enol tautomeric forms (Fig. 3). The diketo form predominates in crystal curcumin or in acidic and neutral solutions, whereas the keto–enol form is exclusively present in alkaline conditions [47–49]. Water solubility increases under alkaline conditions when curcuminoids assume ionic forms upon dissociation of enolic and phenolic protons [47].
Fig. 3.
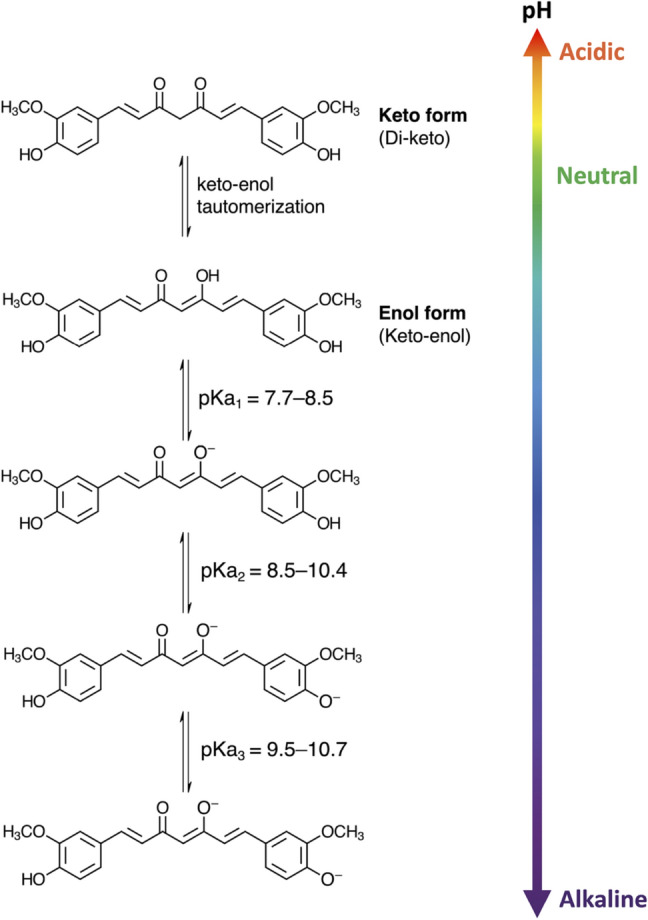
Different forms of curcumin depending on pH conditions
Curcuminoids are subject to chemical degradation in aqueous-organic solutions, especially under alkaline pH, or in dilute solutions of curcuminoids. Binding to macromolecules, such as albumins, lipids, and liposomes, will increase curcuminoid stability [59, 60]. Although the degradation mechanism is not fully understood, it is generally believed that hydrolysis of the α,β-unsaturated β-diketone moiety, which is a common structure in curcuminoids, is involved in the reaction. Major degradation products of curcuminoids that have been identified include vanillin, vanillic acid, ferulic acid, ferulic aldehyde, and others [60].
An even more significant and rapid degradation of curcuminoids occurs when exposed to photooxidation, as is the case when curcuminoids are exposed to sunlight. Photochemical degradations of curcuminoids occur in both solid form and in solution [58, 60]. The products of photodegradation are almost identical to those that are produced from chemical degradation, thereby indicating similar decomposition pathways. Photodegradation is initiated by photoexcitation resulting in the formation of triplet excited states of curcuminoids, which subsequently act as principal photosensitizers of singlet oxygen. The curcuminoids in turn undergo self-photosensitization, a reaction that is not dependent on the presence of oxygen [60, 61]. To prevent photodegradation of curcuminoids from ultraviolet light sources, commercial products are typically packaged in brown or amber containers for shelf-storage.
Besides degradation, bioavailability of phytochemicals is also an important factor limiting pharmaceutical applications. The efficacy of curcumin toward antioxidant, anti-inflammatory, and anti-angiogenic activities is governed by factors that limits bioavailability, or accelerates metabolism and elimination. Low bioavailability of curcumin, due to its poor water solubility, has received considerable attention to find ways to enhance bioavailability using novel encapsulation delivery strategies that include liposomes, polymeric micelles, micro-emulsions, and nano-particle technologies [62–64]. Moreover, improved gastrointestinal absorption and bioavailability of curcumin has been observed using other plant bioactive components, such as piperine [65], and genistein [66] as adjuvants to increase permeability of curcumin, whereas tea catechins, namely, epigallocatechin-3-gallate-EGCG, are known to counteract certain curcumin activities [67].
Turmeric oil (essential oils)
Turmeric oil (TO) is a group of essential oils which mainly consists of more than 250 diverse terpenoids, identified from Curcuma species [68]. TO represents another major group of bioactive compounds in turmeric. Table 3 summarizes the major and most commonly reported terpenoids isolated from turmeric (C. longa) [69–88], which have been categorized into sesquiterpenoids (Compounds 22–81), monoterpenoids (Compounds 82–86), norsesquiterpenoids (Compounds 87–89), and norditerpenes (Compound 90) [12].
Table 3.
Terpenoids present in the rhizome of C. longa
| No. | Compound | Reference |
|---|---|---|
| Sesquiterpenoids | ||
| Bisabolane-type sesquiterpenes | ||
| 22 | α-turmerone | [69] |
| 23 | β-turmerone | [69] |
| 24 | Aromatic (ar)-turmerone | [70] |
| 25 | ar-dihydroturmerone | [71] |
| 26 | β-sesquiphellandrene | [72] |
| 27 | ar-curcumene | [73] |
| 28 | Curlone | [74] |
| 29–32 | Curculonone A–D | [75] |
| 33 | β-atlantone | [75] |
| 34–35 | (Z)/(E)-α-atlantone | [76] |
| 36 | (6S,7R)-bisabolone | [76] |
| 37 | (6R,7R)-bisabolone | [77] |
| 38 | β-bisabolene | [72] |
| 39 | α-zingiberene | [72] |
| 40 | 2-methoxy-5-hydroxybisabola-3,10-diene-9-one | [78] |
| 41 | 2,8-epoxy-5-hydroxybisabola-3,10-diene-9-one | [78] |
| 42 | 4-methylene-5-hydroxybisabola-2,10-diene-9-one | [78] |
| 43 | Bisacurone | [79] |
| 44–46 | Bisacurone A–C | [78] |
| 47 | (6S)‐2‐hydroxy‐6‐(4‐hydroxy‐3‐methylphenyl)‐2‐methylheptan‐4‐one | [80] |
| 48 | (6S)‐6‐(4‐hydroxy‐3‐methylphenyl)‐2‐methoxy‐2‐methylheptan‐4‐one | [80] |
| Bisabolane-type sesquiterpenoids | ||
| 49–50 | (5α/5β)-hydroxyl-1β-bisabolon-9-one | [81] |
| 51–52 | Turmeronol A–B | [82] |
| 53 | (6S)-2‐methyl‐6‐(4‐hydroxyphenyl)‐2‐hepten‐4‐one | [83] |
| 54–57 | Turmerone A–D | [84] |
| 58 | Turmerone Q | [85] |
| 59 | Bisabola-3,10-diene-2-one | [79] |
| 60 | 2,5-dihydroxybisabola-3,10-diene | [79] |
| 61 | 4,5-dihydroxybisabola-2,10-diene | [79] |
| 62 | ar-tumerol (bisacumol) | [79] |
| 63, 64 | Longpene C, D | [86] |
| 65 | Intermedin B | [86] |
| Guaiane-type sesquiterpenoids | ||
| 66 | Curcumenol | [79] |
| 67 | Procurcumadiol | [79] |
| 68 | Procurcumenol | [79] |
| 69 | Isoprocurcumenol | [79] |
| 70 | Epiprocurcumenol | [79] |
| 71 | Zedoaronediol | [79] |
| 72 | 1,10-dehydro-10-deoxy-9-oxozedoarondiol | [75] |
| Germacrane-type sesquiterpenoids | ||
| 73 | Dehydrocurdione | [79] |
| 74 | Germacrone-13-al | [79] |
| 75 | (4S,5S)-germacrone-4,5-epoxide | [79] |
| Carane-type sesquiterpenoid | ||
| 76 | Curcumenone | [79] |
| Elemane-type sesquiterpenoid | ||
| 77 | Curzerenone | [86] |
| Spironolactone-type sesquiterpenoid | ||
| 78 | 6α-hydroxycurcumanolide A | [75] |
| Other sesquiterpenoids | ||
| 79 | Bicycloturmeronol | [87] |
| 80 | Longpene B | [86] |
| Novel sesquiterpene with new skeleton | ||
| 81 | (6S)-2‐methyl‐6‐(4‐hydroxy‐3‐methylphenyl)‐2‐hepten‐4‐one | [83] |
| Monoterpenoids | ||
| Linear monoterpene | ||
| 82 | (Z)-β-ocimene | [88] |
| Monocyclic monoterpene | ||
| 83 | 2-(2,5-dihydroxy-4-methylcyclohex-3-enyl)-propanoic acid | [78] |
| 84 | p-cymene | [77] |
| Monocyclic monoterpenoid | ||
| 85 | 1,8-cineole | [77] |
| Bicyclic monoterpenoid | ||
| 86 | α-pinene | [77] |
| Norsesquiterpenoids | ||
| 87 | 4-hydroxybisabola-2,10-diene-9-one | [79] |
| 88 | 4-methoxy-5-hydroxybisabola-2, 10-diene-9-one | [79] |
| 89 | (6R)-[(1R)-1,5-dimethylhex-4-enyl]-3-methylcyclohex-2-en-1-one | [75] |
| Norditerpene | ||
| 90 | Longpene A | [86] |
Monoterpenes, with a molecular formula C10H16, consist of two isoprene units existing in either linear (acyclic) or ring structure (mono- or bi-cyclic) forms. Monoterpenoid derivatives are produced through modification, such as oxygenation or demethylation [51]. Sesquiterpenes, with a molecular formula C15H24, and associated sesquiterpenoid derivatives consist of three isoprenoid units. As is the case with monoterpenes and monoterpenoids, sesquiterpenes and sesquiterpenoids also exist in either acyclic or cyclic form [68]. Sesquiterpenoids are the dominant group of terpenoids in the turmeric rhizome and are further sub-categorized into several types; the major three being bisabolane, guaiane, and germacrane types, and the minor ones being carane, elemane, spironolactone types, and others [12]. Turmerones (α, β, and aromatic) that fall into the bisabolane-type sesquiterpene category are the predominant constituents that contribute to approximately 50% of the total TO [68]. A broad spectrum of biological activities has been reported in all the sesquiterpenoid classes.
Terpecurcuminoids (terpenoid-conjugated curcuminoids)
Terpecurcuminoids are a minor group of bioactive compounds recovered from turmeric and are distinguished by having a curcuminoid moiety that is conjugated with a terpenoid moiety [89–93]. Out of the 29 identified terpecurcuminoids (Compounds 91–119), 20 compounds have a curcumin moiety, while others possess DMC, BDMC, and curcuminoid derivatives; bisabolene-type sesquiterpenoids are the most common terpenoid moiety, existing in 24 terpecurcuminoids (Table 4). The curcuminoid and terpenoid moieties in 17 of these compounds are conjugated via one or two C–C bonds, while in 12 compounds they are conjugated via C–O–C bonds [92, 93].
Table 4.
Terpecurcuminoids in the rhizome of C. longa
| No | Compound | Curcuminoid moiety | Terpenoid moiety | Reference |
|---|---|---|---|---|
| C–C conjugation | ||||
| 91 | Bisabocurcumin | Curcumin | Bisabolane-type sesquiterpenoid | [92] |
| 92, 93 | Terpercurcumin H, I | [89] | ||
| 94–100 | Terpercurcumin L–P, R, T | [90] | ||
| 101 | Terpercurcumin Q | Curcumin | Other sesquiterpenoid | [90] |
| 102 | Terpercurcumin X | Tetrahydrocurcumin | Bisabolane-type sesquiterpenoid | [91] |
| 103 | Terpercurcumin Y | Cyclocurcumin | Bisabolane-type sesquiterpenoid | [91] |
| 104, 105 | Terpercurcumin J, K | Dihydro-BDMC | Other sesquiterpenoid | [90] |
| 106, 107 | Terpercurcumin V, W | Curcumin | Monocyclic monoterpenoid | [90] |
| C–O–C conjugation | ||||
| 108 | Bisabolocurcumin ether | Curcumin | Bisabolane-type sesquiterpenoid | [93] |
| 109–114 | Terpercurcumin A–F | [89] | ||
| 115 | Demethoxybisabolo-curcumin ether | DMC | Bisabolane-type sesquiterpenoid | [93] |
| 116 | Terpercurcumin G | [89] | ||
| 117 | Terpercurcumin U | [91] | ||
| 118 | Didemethoxybisabolo-curcumin ether | BDMC | Bisabolane-type sesquiterpenoid | [93] |
| 119 | Terpercurcumin S | [91] | ||
The terpecurcuminoids show cytotoxicity against various human cancer cell lines (e.g., human breast cancer cell lines MDA-MB-231 and MCF-7, human liver cancer cell line HepG2, and human lung cancer cell line A549), and some have exhibited greater cytotoxic potency compared to curcumin, thereby suggesting a promising anti-cancer activity of these compounds that requires more investigation on clinical efficacies [89, 90].
Bioactivities of turmeric and its constituents against diabetes and CVD
Cellular and molecular mechanisms of the bioactivities of turmeric and several constituents reported from both in vitro (Table 5) and in vivo studies (Table 6) point to chemoprotection against onset of chronic diseases, such as diabetes and CVD. Human clinical trials (Table 7) have also provided positive evidence to recognize clinical efficacy of turmeric and turmeric-derived compounds. Table 8 summarizes the few current meta-analyses that reported on clinical effects of these compounds against CVD and related conditions.
Table 5.
In vitro studies on antidiabetic and cardioprotective effects of turmeric and turmeric-derived bioactive compounds
| Disease/bioactivity | Model | Treatment | Dose | Main outcomes | Reference |
|---|---|---|---|---|---|
| Diabetes | |||||
| High glucose-induced insulin resistance | Rat insulinoma cell line INS-1 | Curcumin | 5–15 μM |
⬆ Expression of: insulin, GSIS, GCK, PDX-1, GLUT2; ⬆ Phosphorylation of: IR, IRS1, PI3K, Akt |
[32] |
| High glucose-induced oxidative stress and pancreatic β-cell apoptosis | Min-6 mouse pancreatic β-cells | Curcumin | 1–10 μM |
⬇ ROS, MDA, ⬆ SOD levels; ⬇ CHOP, ⬆ PGC-1α; ⬇ p-ERK1/2 |
[30] |
| Leptin-stimulated increase in intracellular glucose | Rat hepatic stellar cells (HSCs) and immortalized human hepatocytes | Curcumin | 20 μM |
⬇ Glucose level; ⬇ GLUT4 translocation to membrane; ⬇ Phosphorylation of: IRS-1, PI3K, Akt; ⬆ Glucokinase activity; ⬆ G6P levels |
[94] |
| Akt signaling pathway and glucose uptake | 3T3-L1 adipocytes | Curcumin |
10–75 μM (dose response); 50 μM (time response) |
[Dose-dependent] ⬇ Akt protein levels; ⬇ GLUT4 plasma membrane expression; ⬇ Glucose uptake; ⬆ LC3-II protein; ⬆ LC3-II/LC3-I ratio |
[95] |
| Glucose uptake in GLUT1-expressing cells | L929 mouse fibroblast cells, HK2 human kidney cells, immortalized human corneal-limbal epithelial (HCLE) cells | Curcumin | 25–200 μM |
[Dose-dependent] ⬇ 2DG uptake (all three cell types); ⬇ Cytochalasin B binding (L929 cells) |
[96] |
| Glucagon-like peptide-1 secretion | GLUTag L cells | Curcumin | 25 μM |
⬆ GLP-1 secretion (the effect diminished by GW1100) |
[31] |
| Human adipocyte differentiation and peroxisome proliferator-activated receptor gamma (PPAR-γ) ligand-binding activity | Human preadipocytes |
Turmeric extract (ethanol), curcumin, DMC, BDMC, ar-turmerone |
Turmeric extract: 2–20 μg mL−1 Others: 2–5 μg mL−1 |
[Dose-dependent] ⬆ adipocyte differentiation (turmeric extract); ⬆ PPAR-γ ligand-binding activity (all treatments) |
[101] |
| Human adipocyte differentiation and PPAR-γ ligand-binding activity | Human preadipocytes |
Turmeric extracts (ethanol: E-ext; hexane: H-ext; ethanol extraction from hexane extraction residue: HE-ext), curcumin, DMC, BDMC, ar-turmerone |
[Adipocyte differentiation] E-ext: 2–20 mg L−1 [GAL4-PPAR-γ chimera assay] Turmeric ext: 5–10 mg L−1 Others: 2–5 mg L−1 |
[Dose-dependent] ⬆ adipocyte differentiation (E-ext); ⬆ PPAR-γ ligand-binding activity (all treatments) |
[102] |
| Sterol regulatory element-binding protein (SREBP) pathway |
Luciferase-expressing cancer cells Huh-7/SRE-Luc, rat heptaocytes CRL-1601 |
Curcumin |
0.1–40 μM (Huh-7/SRE-Luc) 10 μM (CRL-1601) |
[Dose-dependent] ⬇ Luciferase activity (in Huh-7/SRE-Luc cells); ⬇ Intracellular cholesterol, TG; ⬇ Expression of mRNA: SREBP-1, SREBP-2; ⬇ Expression of endogenous nuclear: SREBP-1, SREBP-2; (in CRL-1601 cells) |
[107] |
| Inhibition of α-amylase and α-glucosidase |
Chemical assays: α-amylase inhibition, α-glucosidase inhibition |
Turmeric oil from fresh (FTO) and dried (DTO) rhizomes; ar-tumerone |
0.1–100 μg mL−1 |
Inhibition of: α-amylase, α-glucosidase, (ar-tumerone > DTO > FTO > acarbose) |
[99] |
| In vitro antidiabetic potential |
Chemical assays: α-amylase inhibition, α-glucosidase inhibition, antiglycation activity |
Turmeric rhizome extracts using ethyl acetate (EtOAc Ex), methanol (MeOH Ex), and water (Water Ex) | 0–600 μg mL−1 |
Inhibition of: α-amylase (EtOAc Ex > MeOH Ex > acarbose > Water Ex), α-glucosidase (EtOAc Ex > MeOH Ex > Water Ex > acarbose) Antiglycation activity: (EtOAc Ex > MeOH Ex > Water Ex) |
[97] |
| Inactivation of human pancreatic α-amylase (HPA) | Chemical assays (α-amylase inhibition, α-glucosidase inhibition) | BDMC | 2–15 μg mL−1 | Inhibition of HPA (IC50 = 0.025 mM; Acarbose IC50 = 0.015 mM) | [98] |
| CVD | |||||
| Monocyte adhesion to TNF-α-stimulated endothelial cells | Primary human umbilical vein endothelial cells (HUVECs), human monocytic cell line U937 | Curcumin | 0.1–1 μM |
[Dose-dependent] ⬇ Monocyte adhesion to HUVECs; ⬇ VCAM-1 gene expression |
[123] |
| Cholesterol accumulation in foam cells | Mouse macrophage cell line J774.A1 | Curcumin | 5–40 μM |
[Dose-dependent] ⬇ oxLDL-induced intracellular cholesterol accumulation; ⬇ Dil-oxLDL binding; ⬇ SR-A expression; ⬆ SR-A turnover; ⬆ SR-A–ubiquitin–VCP complex formation; ⬆ ApoAI-mediated cholesterol efflux; ⬆ ABCA1 expression (Curcumin’s effect on ABCA1 abolished by LXRα inhibition.) |
[28] |
| Lipid accumulation in monocyte/macrophage | Human acute monocytic leukemia THP-1 cells | Curcumin | 1–20 μM |
[Dose-dependent] In THP-1 and THP-1 differentiated macrophages: ⬆ Lipid accumulation; ⬆ CD36 and aP2 protein expression; ⬆ FOXO3a phosphorylation |
[125] |
| TLR4 expression and NF-κB activation | Mouse peritoneal macrophages (MPMs) | Curcumin | 10–25 μM |
[Dose-dependent] ⬇ TLR4 mRNA level; ⬇ NF-κB activation |
[27] |
| Hypoxia-induced cardiomyocyte apoptosis | Mouse cardiac myocytes (MCMs) | Curcumin | 10 μM |
⬆ miR-7a/b expression; ⬇ SP1 expression and cell apoptosis (the effect diminished by miR-7a/b inhibitors) |
[129] |
| TLR2 and MCP-1 expression | Neonatal rat cardiomyocyte | Curcumin | 10 μM |
⬇ TLR2 and MCP-1 (otherwise by TNF-α, PGN and H/R) |
[130] |
| p300-HAT inhibitory activity | In vitro HAT assay | Curcumin, DMC, BDMC | 20–60 μM |
[Dose-dependent] ⬇ p300-induced acetylation of histone H3K9; Inhibitory activity at 20 μM: CUR > BDMC > DMC; at 60 μM: CUR ≈ DMC ≈ BDMC |
[135] |
| Cardiac fibrosis | Cardiac fibroblasts (CFs) | Curcumin | 5–15 μM |
[Dose-dependent] ⬇ Ang II-induced expression of: collagen I, collagen III, and TGF-β1; ⬇ MMP-2 activity; ⬇ Ang II-induced CF cell proliferation and migration (All above effects of curcumin diminished by SIRT1 siRNA.) |
[133] |
| Phenylephrine-induced cardiomyocyte hypertrophy | Primary neonatal rat cardiomyocytes | Curcumin, DMC, BDMC | 10 μM |
⬇ Phenylephrine-induced: acetylation of histone H3K9, myocardial cell-surface area increase, ANF and BNP expression (CUR ≈ DMC ≈ BDMC) None of the compounds changed morphology of cardiomyocytes |
[135] |
| Noradrenaline‐induced cardiomyocyte hypertrophy | Heart‐derived H9C2 cardiomyoblast cells, primary neonatal rat cardiomyocytes | Curcumin | 8 μM |
⬇ Noradrenaline-stimulated increases in: cell size, protein concentration, ANF expression, nuclear localization of GATA4, DNA-binding activity of GATA4 |
[137] |
| Phenylephrine-induced cardiomyocyte hypertrophy | Primary neonatal rat cardiomyocytes | Curcumin | 5–10 μM |
⬇ Phenylephrine (PE)- or p300-induced increases in: cell surface area, ANF and β-MHC promoter activities, p300-GATA4 association, GATA4 acetylation, GATA4-DNA binding; ⬇ p300-induced increases in: cell surface area, ANF and β-MHC promoter activities |
[136] |
Table 6.
In vivo animal studies on antidiabetic and cardioprotective effects of turmeric and turmeric-derived bioactive compounds
| Disease/condition | Model | Treatment | Dose, administration manner; duration | Main outcomes | Reference |
|---|---|---|---|---|---|
| Diabetes | |||||
| Glycemic response | KK-Ay mice/Ta mice | Turmeric extract (ethanol) |
0.2–1.0 g/100 g diet, ad libitum; 4 weeks |
[Dose-dependent] ⬇ Blood glucose |
[101] |
| Glycemic response | KK-Ay mice/Ta mice |
Turmeric extracts (ethanol: E-ext; hexane: H-ext; ethanol extraction from hexane extraction residue: HE-ext) |
H-ext or HE-ext: 0.1–0.5 g/100 g diet E-ext: 0.2–1.0 g/100 g diet; 4 weeks |
⬇ Blood glucose (H-ext and HE-ext at 0.5 g/100 g diet; E-ext at 0.2 and 1.0 g/100 g diet) |
[102] |
| Glycemic response | Alloxan-induced diabetic mice | C. longa extract (ethanol:water = 70:30 v/v) |
5–15 mg kg−1, i.p.; before alloxan i.p |
[Dose-dependent] ⬇ Blood glucose |
[103] |
| T2D-assocaited liver complications | Wild-type and db/db mice | Curcumin |
0.75% w/w in diet, ad libitum; 8 weeks |
⬇ NF-κB p65 expression; ⬆ AMPK and PPAR-γ expressions |
[104] |
| Glucose tolerance and GLP-1 secretion | Sprague–Dawley rats | Theracurcumin | 5 mg kg−1 (= 1.5 mg kg−1 curcumin equivalent), p.o.; before glucose i.p |
⬇ Serum glucose concentration (effect diminished by GW1100); ⬆ Serum levels of: insulin, total & active GLP-1 |
[31] |
| High-fat diet-induced obesity and SREBP pathway | C57BL/6 mice | Curcumin |
40–80 mg kg−1 day−1 in high-fat diet (HFD), p.o.; 12 weeks |
⬆ Energy expenditure; ⬇ Body weight gain; ⬇ Serum TC, TG and LDL-c; ⬇ Hepatic TC and TG; ⬇ Lipid droplets accumulation in liver [High dose (80 mg kg−1)] ⬇ Epididymal fat weigh and adipocyte diameter in white adipose tissue; ⬇ Blood glucose; ⬇ Serum insulin; ⬇ Hepatic expression of: SREBP-1, SREBP-2; ⬆ Tyrosine phosphorylation of: IRS-1, IRS-2; ⬆ Serine 473 phosphorylation of Akt |
[107] |
| CVD | |||||
| Atherosclerosis | ApoE–/– mice | Curcumin |
0.1% w/w in HFD, p.o.; 16 weeks |
⬇ Macrophage infiltration and TLR4 expression in atherosclerosis plaque; ⬇ Aortic NF-κB activation; ⬇ VCAM-1 and ICAM-1 expressions; ⬇ Serum IL-1β and TNF-α levels; ⬇ Aortic sinus plaque area |
[27] |
| Atherosclerosis | ApoE–/– mice | Curcumin |
20 mg kg−1 day−1, p.o.; 4 weeks |
⬇ Atherosclerotic lesion area in aortic roots; ⬇ Serum levels of: IL-6, TNF-α, MCP-1, TC, TG, non-HDL-c; ⬆ Serum HDL-c; ⬆ Aortic ABCA1 level; ⬇ Aortic SR-A level |
[28] |
| Atherosclerosis | ApoE–/– mice | Curcumin |
0.2% w/w in diet, p.o.; 4 months |
⬇ Atherosclerotic lesion size; ⬇ Macrophage number in atherosclerotic lesions; ⬆ Aortic IκB expression; Modulated 1,670 genes expression in aorta (1,022 ⬆, 648 ⬇) |
[123] |
| Lipid accumulation in macrophage | LDL receptor knockout (LDL-R–/–) mice | Curcumin |
500–1500 mg kg−1 HFD, p.o.; 4 months |
⬇ Lipid accumulation in peritoneal macrophages; ⬇ mRNA expressions of: aP2, ABCA1 (all otherwise ⬆ by HFD.) |
[125] |
| Altered gene expression in MI | Sprague–Dawley rats | Curcumin |
75 mg kg−1 day−1, p.o.; 3 days |
⬆ Cardiac function; ⬇ Cardiac infarct size; ⬇ LDH and CK-MB activities Altered expression of genes in particular the one involved in cytokine–cytokine receptor interaction, JAK/STAT pathway, ECM-receptor interaction |
[127] |
| Cardiac ischemia/reperfusion (I/R) injury | Sprague–Dawley rats | Curcumin |
10–30 mg kg−1 day−1, p.o.; 20 days before I/R injury |
[Dose-dependent] ⬆ Cardiac function; ⬇ Cardiac infarction size; ⬇ Myocardial MDA level; ⬆ Myocardial SOD, CAT, GSH-Px, GR activities; ⬇ Myocardial LDH, CK-MB activities; ⬇ Myocardial Bax and Caspase-3; ⬆ Myocardial Bcl-2 level; ⬆ JAK2 and STAT3 phosphorylation |
[25] |
| Cardiac I/R injury | Sprague–Dawley rats | Curcumin |
300 mg kg−1 day−1, p.o.; 7 days before and 14 days after I/R injury |
⬇ TLR2 mRNA and protein expressions; ⬇ Macrophage infiltration (CD68); ⬇ cardiac fibrosis (otherwise ⬆ by I/R); ⬆ Cardiac contractility; ⬆ Cardiac function parameters (otherwise ⬇ by I/R.) |
[130] |
| Cardiomyocyte apoptosis | Sprague–Dawley rats | Curcumin |
150 mg kg−1 day−1, p.o.; 4 weeks |
⬇ Morphological changes and apoptosis index of myocardial cells; ⬇ NF-κB p65 expression; ⬆ PPAR-γ and Bcl-2 expressions |
[128] |
| Cardiomyocyte apoptosis | C57BL/6 mice | Curcumin |
50 mg kg−1 day−1, p.o.; 4 weeks |
⬇ Myocardial infarct size; ⬆ LDH release; ⬆ miR-7a and miR-7b levels; ⬇ SP1 mRNA and protein levels |
[129] |
| MI and cardiac fibrosis | C57BL/6 J mice | Curcumin |
100 mg kg−1 day−1, p.o.; 4 weeks |
⬇ Interstitial fibrosis; ⬇ Myocardial expressions of: collagen I, collagen III, TGF-β1; ⬇ Infarct size; (otherwise ⬆ by MI) ⬆ SIRT1 in heart tissues (otherwise ⬇ by MI) |
[133] |
| Hypertension- and MI-induced heart failure |
Salt-sensitive/resistant Dahl (DS/DR) rats, MI rats |
Curcumin |
50 mg kg−1 day−1, p.o.; 7 weeks |
In DS rats: ⬇ Hypertension-induced heart failure; ⬇ GATA4 acetylation; ⬇ p300/GATA4 complex In MI rats: Prevented MI-deteriorated left ventricular systolic function |
[136] |
Table 7.
Double-blind RCTs on antidiabetic and cardioprotective effects of turmeric and turmeric-derived bioactive compounds
| Disease/condition | Sample population (n = sample size) | Duration | Treatment | Dose, administration manner | Outcome | Reference |
|---|---|---|---|---|---|---|
| Diabetes | ||||||
| Anthropometric parameters and serum lipid profile | Hyperlipidemic T2D patients (n = 72) | 8 weeks | Turmeric rhizome powder | 2100 mg day−1, p.o |
Compared to baseline: ⬇ Body weight; ⬇ Serum TG; ⬇ Serum LDL-c Compared to control: ⬇ BMI; ⬇ Serum TG; ⬇ Serum TC |
[112] |
| Serum lipid profile and inflammation status |
T2D patients (n = 44) |
10 weeks |
Curcumin capsule (69.4% curcumin, 16.8% DMC, 1.8% BDMC, and 7.6% TO) |
1500 mg day−1, p.o |
Compared to baseline: ⬇ Serum TG Compared to control: ⬇ Serum hs-CRP |
[113] |
| Serum lipid profile |
T2D patients (n = 118) |
12 weeks | Curcuminoids + piperine |
1000 mg day−1 curcuminoids + 10 mg day−1 piperine, p.o |
Compared to control: ⬇ Serum TC; ⬇ Serum non-HDL-c; ⬇ Serum Lp(a); ⬆ Serum HDL-c |
[114] |
| Diabetic sensorimotor polyneuropathy (DSPN) |
T2D patients (n = 80) |
8 weeks | Nano-curcumin | 80 mg day−1, p.o |
⬇ Glycemic indices: HbA1c, FBS; ⬇ DSPN severity: total score of neuropathy, total symptom score, total reflex score |
[29] |
| Metabolic syndrome (MetS) |
Apparently healthy males screened positive for MetS (n = 250) |
8 weeks | Turmeric | 2.4 g day−1, p.o |
At 4 weeks: ⬇ BMI; ⬇ WC; ⬇ %BF At 8 weeks: ⬇ LDL-c; CRP |
[109] |
| MetS | Individuals with MetS (n = 120) | 6 weeks | Curcumin (native or phospholipidated) | 1 g day−1, p.o |
⬆ Serum PAB (native curcumin, but not phospholipidated curcumin) |
[18] |
| MetS | Individuals with MetS (n = 120) | 6 weeks | Curcumin (native or phospholipidated) | 1 g day−1, p.o | No significant effects on serum anti-Hsp 27 concentrations | [138] |
| MetS | Individuals with MetS (n = 120) | 6 weeks | Curcumin (native or phospholipidated) | 1 g day−1, p.o |
⬆ Serum Zn; ⬆ Serum Zn/Cu ratio Phospholipidated curcumin resulted in higher increases than native curcumin |
[110] |
| MetS | Individuals with MetS (n = 117) | 8 weeks | Curcuminoids + piperine | 1000 mg day−1 curcuminoids + 10 mg day−1 piperine, p.o |
⬆ Serum SOD activity; ⬇ Serum MDA; ⬇ Serum CRP |
[111] |
| CVD | ||||||
| Atherogenic risk |
T2D patients (n = 117) |
6 months | Curcuminoid | 750 mg day−1, p.o |
⬇ Pulse wave velocity; ⬇ Serum leptin; ⬆ Serum adiponectin |
[126] |
| Acute myocardial infarction (MI) associated with coronary artery bypass grafting (CABG) |
Patients undergoing CABG without valve surgery (n = 121)z |
8 days | Curcuminoid | 4 g day−1, p.o |
⬇ In-hospital MI incidence; ⬇ Postoperative levels of: CRP, MDA, NT–pro-BNP |
[26] |
Table 8.
Meta-analyses of RCTs on cardioprotective effects of turmeric and turmeric-derived bioactive compounds
| Disease/condition | No. of Articles included | Sample population (n = total sample size) |
Duration | Treatment | Dose | Outcomea | Reference |
|---|---|---|---|---|---|---|---|
| Blood lipid profile | 7 |
Subjects with CVD risk factors, e.g., dyslipidemia, T2D, prediabetes, MetS, hypertension, prehypertension, or obesity (n = 649) |
4 weeks–6 months | Purified curcumin/curcuminoids, turmeric powder, turmeric extract | 70–1890 mg day−1 curcuminoid equivalent, or 2–2.4 g day−1 turmeric powder, p.o |
⬇ Serum LDL-c (SMD = − 0.340 [− 0.530, − 0.150]); |
[118] |
|
⬇ Serum TG (SMD = − 0.214 [− 0.369, − 0.059]) | |||||||
| MetS | 8 |
Subjects with MetS (n = 562) |
2–12 weeks | Purified or standardized preparations with known amounts of curcumin/curcuminoids | 80 mg day−1–6 g day−1, p.o |
⬇ Serum CRP (WMD = − 2.20, [− 3.96, − 0.44]) |
[111] |
| Atherosclerosis and CVD | 6 |
Diverse subjects (n = 312) |
6 days–3 months | Purified or standardized preparations with known amounts of curcumin/curcuminoids | 80 mg day−1–6 g day−1, p.o |
⬇ Serum CRP (WMD = − 6.44, [− 10.77, − 2.11]) |
[119] |
| Stronger effect in subgroups that used bioavailability-improved preparations, and had intervention duration ≥ 4 weeks |
aSMD standardized mean difference; WMD weighted mean difference; numbers in square brackets represent the 95% confidence interval
Hypoglycemic and antidiabetic activities
Curcumin and other related bioactive compounds present in turmeric have been proposed to protect against type 2 diabetes (T2D) through different mechanisms that involve a hypoglycemic effect attributed to upregulation of insulin, enhanced insulin sensitivity, and lower cellular uptake of glucose.
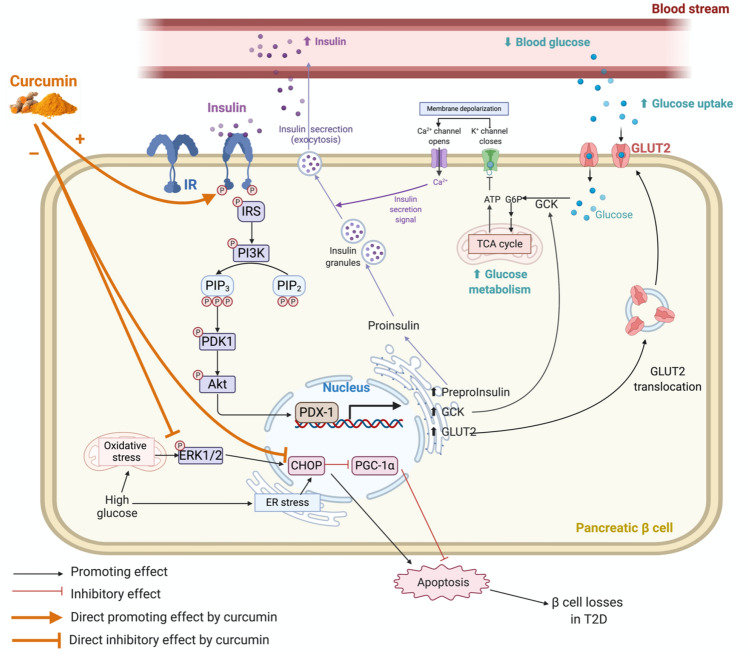
The mechanism of which curcumin evokes hypoglycemic and antidiabetic effects involves the pancreatic β-cells (Fig. 4). Curcumin attenuates high glucose-induced insulin resistance in cultured rat insulinoma cells, INS-1, a model by which insulin secretion by pancreatic β-cells has been studied [32]. The underlying mechanism therein is the increased expression and secretion of insulin by activating the phosphatidylinositol-3-kinase/protein kinase B/glucose transporter 2 (PI3K/Akt/GLUT2) signaling pathway. In this pathway, curcumin acts to upregulate phosphorylation of the insulin receptor (IR), insulin receptor substrate (IRS)-1, PI3K, and Akt, all of which in turn increase the expression of pancreatic and duodenal homeobox-1 (PDX-1) and subsequent insulin mRNA. This effect is linked to increased levels of GLUT2 and glucokinase (GCK) activity, which are both required to regulate cellular glucose uptake and metabolism [32]. These processes are otherwise suppressed in the presence of a high glucose concentration. Curcumin is effective at attenuating oxidative stress that is induced by high glucose levels and which triggers apoptosis in a dose-dependent manner, and observation made using in mouse pancreatic β-cells [30]. This occurs by both a downregulated expression of C/EBP homologous protein (CHOP) and an upregulated expression of peroxisome proliferator-activated receptor-γ coactivator-1α (PGC-1α), along with a suppressing effect on phosphorylation of extracellular signal-regulated kinase 1/2 (ERK1/2) [30].
Fig. 4.
Pancreatic β-cell signaling mechanisms involved in hypoglycemic and antidiabetic events attributed to curcumin (created with https://BioRender.com). Abbreviations are given below
In adipocytes and hepatocytes, curcumin reduces glucose uptake by inhibiting the translocation of GLUT4 from the cytosol to plasma membrane, and by interfering with the IRS/PI3K/Akt signaling pathway [94, 95]. Curcumin has also been shown to directly inhibit GLUT1, thus lowering glucose uptake in GLUT1-expressing cells. It is noteworthy that the selective binding of curcumin to GLUT1 overlaps with the binding site of cytochalasin B, a mycotoxin that also has been shown to inhibit glucose transport [96].
The in vitro antidiabetic potentials of the turmeric extract, BDMC [97, 98], TO, and its major component ar-turmerone [99] have in common a capacity to inhibit the activities of α-amylase and α-glucosidase, two key enzymes involved in glucose digestion and also linked to T2D. These enzymes are the targets for specific antidiabetic drugs that control postprandial increase of blood glucose. Regardless of the forms of which turmeric is administered, for example, TO recovered from both fresh and dried rhizomes, turmeric extracts using different solvents, and the isolated ar-turmerone, there is sufficient evidence that these compounds show inhibitory effects on both glucose digestion enzymes; in fact they are relatively stronger than the standard antidiabetic drug, acarbose, an inhibitor of both α-amylase and α-glucosidase that reduces the breakdown of complex carbohydrates to glucose [97–99]. In addition, the turmeric extract also has notable antiglycation effects [97]. Protein glycation is the formation of advanced glycation end-products (AGEs) resulting in structurally and functionally altered proteins that contribute to various metabolic complications; the process could be accelerated by high levels of reducing sugars, such as glucose [97]. Antiglycation activity refers to delaying production of AGEs by suppressing oxidation of Amadori products and metal-catalyzed glucose oxidation [100].
Ethanol-derived turmeric extracts yield both curcuminoids and sesquiterpenoids, whereas hexane extracts yield mainly sesquiterpenoids. Further extraction of the hexane extraction with ethanol has been successful to improve recovery of DMC, BDMC, and ar-turmerone. These components were also effective at significantly increasing peroxisome proliferator-activated receptor gamma (PPAR-γ) ligand-binding activity, whereas the turmeric ethanolic extract stimulated human adipocyte proliferation in vitro [101, 102]. In vivo studies using genetically diabetic KK-Ay mice showed that turmeric extracts suppressed diet-induced increases in blood glucose level [101, 102]. Similarly, in alloxan-induced diabetic mice, a hydroethanolic extract of turmeric was effective to control blood glucose levels [103].
In genetically diabetic db/db mice, upregulation of PPAR-γ expression by dietary curcumin occurs in the liver and is associated with the upregulation of 5′ adenosine monophosphate-activated protein kinase (AMPK) expression and downregulation of p65 Nuclear factor kappa B (NF-κB). These effects are regarded as being beneficial to reduce T2D complications [104]. In other studies conducted in mice, curcumin improved glucose tolerance by stimulating secretion of the glucagon-like peptide-1 (GLP-1), and also incretin from enteroendocrine L (GLUTag L) cells [31]. These activities are connected to the stimulated proliferation of β-cells and glucose-dependent insulin secretion, both of which are important for T2D treatment and prevention. Kato et al. [31] reported a similar finding regarding curcumin stimulation of GLP-1 secretion in GLUTag L cells in vitro. G-protein-coupled receptors (GPRs) are a group of free fatty acid receptors (FFARs) on the surface of β-cells, among which GPR 40 and GRP 120 are important for β-cells in the mediation of insulin secretion upon stimulation by long-chain fatty acids [105]. Both in vivo and in vitro studies have confirmed that activation of the GPR 40/120 pathway is involved in the GLP-1-stimulating effect of curcumin; this conclusion was reached by the observation that this effect was also reduced when cells were treated with GW1100, a GPR 40/120 antagonist [31].
Obesity is a major co-morbidity of T2D, and strategies that have been developed to treat this disorder by inhibiting the sterol regulatory element-binding protein (SREBP) pathway, important for regulating gene expressions that stimulate fatty acid, triacylglyceride, and cholesterol biosynthesis [106]. Ding et al. [107] reported that curcumin was an active inhibitor of triacylglyceride and cholesterol synthesis by downregulating expressions of both SREBP-1 and SREBP-2, respectively. Curcumin also has been shown to improve glucose homeostasis and insulin sensitivity by upregulating the phosphorylation of IRS-1, IRS-2, and Akt in these mice [107].
Metabolic syndrome (MetS), a term that refers to the co-occurrence of morbidities that increase the risk of heart attack, stroke, and T2D, engages several dysfunctional metabolic outcomes that include excess fat around the waist, insulin resistance, hyperglycemia, atherogenic dyslipidemia, and hypertension [108]. Randomized clinical trial (RCT) studies conducted with MetS subjects reported that turmeric, curcumin, and curcuminoids are effective at improving pertinent anthropometric and biochemical-metabolic parameters in these patients. Turmeric improves body mass index (BMI), waist circumference (WC), and the percent body fat (%BF) and also lowers serum low-density lipoprotein cholesterol (LDL-c) and C-reactive protein (CRP) levels in MetS patients [109]. Curcumin significantly increases the serum pro-oxidant-antioxidant balance (PAB) and the zinc-to-copper (Zn/Cu) ratio, and in addition will also increase serum Zn/Cu ratios without affecting PAB [18, 110]. Short-term supplementation with a curcuminoid-piperine combination also improves oxidative stress and inflammatory status in MetS patients, as evidenced by increased serum superoxide dismutase (SOD) activity and a decrease in serum malondialdehyde (MDA) and CRP levels [111]. Piperine, a pungent alkaloid recovered from black pepper, enhances bioavailability of curcuminoids [111]. The CRP-lowering effect observed in MetS patients fed various purified or standardized preparations of curcumin or curcuminoids leads to a final conclusion derived from a meta-analysis [111]. By alleviating MetS, turmeric and related curcuminoids actively prevented the development of T2D. Notwithstanding this, similar results that pointed to improved metabolic parameters due to curcumin treatment were also reported in patients with existing T2D. Three double-blind RCTs [112–114], involving 44 to 118 T2D patients supplemented with turmeric rhizome powder, a curcumin capsule consisting of curcuminoids and TO, or a curcuminoid-piperine combination over an 8- to 12-week treatment duration, showed similar improvements in anthropometric parameters. These parameters included lowered body weight and BMI, and positive changes in serum lipid profiles that included reduced triglyceride (TG), total cholesterol (TC), LDL-c, and lipoprotein a [Lp(a)], and increased high-density lipoprotein cholesterol (HDL-c). In addition, the inflammation status was amended by a reduction in serum high-sensitivity CRP levels [112–114]. A systematic review and meta-analysis of RCTs [115] has recently reported that curcumin or curcuminoids preparations are effective at lowering body weight and BMI in subjects with obesity or T2D. Nano-curcumin, a nano-formulation of curcumin with enhanced bioavailability, can also improve glycemic indices in T2D subjects. This finding was based on observed reductions in serum glycated hemoglobin (HbA1c) and fasting blood sugar (FBS), and improved severity of diabetic sensorimotor polyneuropathy (DSPN), known to be a common T2D complication [29]. Taken together, the data are very convincing as to the benefits of turmeric and curcumin to improve both the serum lipid profile, glycemic indices, hemoglobin glycation, and inflammatory conditions of T2D patients.
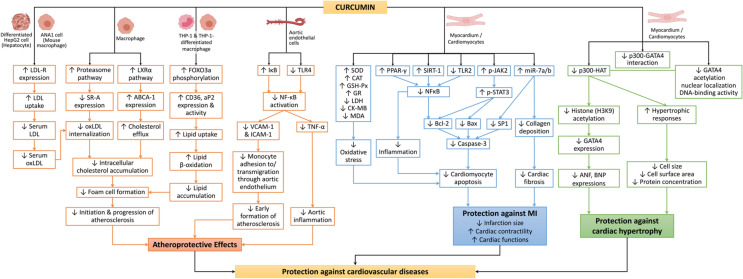
Hypolipidemic, atheroprotective, and cardioprotective activities
Studies conducted in vitro, in vivo, and also in human clinical trials have collected considerable evidence to indicate that turmeric and associated bioactive components, especially curcumin, can protect against CVD; albeit underlying mechanisms can differ (Fig. 5). A very strong line of evidence for protection has been attributed to the antioxidant and anti-inflammatory effects of curcumin that involve the regulation cell signaling pathways, such as mitogen-activated protein kinase (MAPK), NF-κB, and nuclear factor erythroid 2-related factor 2–Kelch-like ECH-associated protein 1 (Nrf2-Keap1). These molecular redox signaling pathways combat oxidative stress and inflammation—two highly recognized factors associated with the etiology and pathogenesis of CVDs [116, 117]. In addition, the onset of MetS, as discussed previously in T2D subjects, is another risk factor for the development of CVD which curcumin was effective to mitigate. Of particular interest is that turmeric, curcumin, and curcuminoids are all effective in preventing CVD in both healthy individuals, as well as those individuals that have underlying CVD risk factors. The biomarkers that have been used to indicate these outcomes include reductions in serum LDL cholesterol, TG, and CRP [118, 119].
Fig. 5.
A schematic of mechanisms that have been attributed to the protective effects of curcumin against etiology of CVD. Abbreviations are given below
Atherosclerosis associated with CVD involves the narrowing or hardening of coronary arteries due to the deposition of cholesterol plaques initiated by an increase in serum oxidized low-density lipoproteins (oxLDL) [120]. Curcumin activates increased expression of low-density lipoprotein (LDL) receptors, both in cultured human liver cancer cell line HepG2 [121] and mouse macrophage [122], thus contributing to increased LDL uptake, an important step in protection against atherosclerosis. In the apolipoprotein E knockout (ApoE–/–) mouse model, dietary curcumin prevented the incidence and progression of atherosclerosis [27, 28, 123]. Coban et al. [123] reported that curcumin was effective at inducing significant changes in aortic gene expression, in particular those associated with monocyte adhesion to aortic endothelial cells and transmigration through to the aortic endothelium. Curcumin also downregulated the expression of vascular cell adhesion molecule-1 (VCAM-1) and intercellular cell adhesion molecule-1 (ICAM-1) in vitro [123] and in vivo [27]. VCAM-1 and ICAM-1 have important roles in the adhesion of monocytes to aortic endothelial cells in the early formation of atherosclerosis, and both are upregulated by NF-κB [124]. Correspondingly, curcumin increases inhibitor of NF-κB (IκB) expression [123], while also decreasing NF-κB activation and tumor necrosis factor α (TNF-α) [27], in aortic tissue. Expression of toll-like receptor 4 (TLR4), an upstream mediator of NF-κB, was shown to be suppressed by curcumin [27]. Serum levels of NF-κB-associated inflammatory cytokines were also significantly reduced by curcumin treatment in ApoE–/– mice [27, 28]. These researchers found that the atheroprotective capacity of curcumin was due to an affinity to reduce oxLDL-stimulated foam cell development, a crucial step in the initiation and progression of atherosclerosis. Curcumin suppresses intracellular cholesterol accumulation in macrophages by decreasing both oxLDL internalization and increasing cholesterol efflux. Furthermore, molecular studies revealed that these two effects are attributed to downregulation of scavenger receptor class A (SR-A) expression, via proteasome activation, and upregulation of adenosine triphosphate (ATP)-binding cassette transporter A1 (ABCA1) expression, via liver X receptor α (LXRα) pathway, respectively [28].
The affinity of curcumin to upregulate Forkhead box O3a (FOXO3a) activity, a central transcription factor that regulates lipid transport genes in macrophage LDL, and recovered from LDL receptor knockout (LDL-R–/–) mice fed a high-fat diet [125], is important for recognizing its potential role to prevent atherosclerosis. Curcumin improves the serum lipid profile of ApoE–/– mice by reducing TC, TG, non-HDL-cholesterol, and increased HDL-cholesterol [28]. These activities correspond to an early retarded progression of atherosclerosis by alleviating oxidation and inflammation and by supporting cholesterol homeostasis through stabilizing the serum lipid profile and preventing endothelial dysfunction. Although human clinical trials designed to show the efficacy of curcumin/curcuminoids to treat atherosclerosis have not yet been established, a daily intake of curcuminoids at 750 mg effectively reduced atherogenic risk in T2D patients in a 6-month double-blind RCT [126].
Myocardial infarction (MI) is frequently associated with underlying atherosclerotic conditions, due to a sudden diminished supply of oxygenated blood caused by narrowing of blood vessels [120]. Hong et al. [127], using an experimental MI rat model, demonstrated numerous benefits of curcumin that included significant protection of cardiac function and reduced cardiac infarction size. Connected with these observations were anti-inflammatory responses related to regulation of genes involved in cytokine–cytokine receptor interaction, extracellular matrix (ECM) receptor interaction, and Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway [127]. In particular, the activation of JAK2/STAT3 signaling pathway by curcumin is associated with reduced infarction size in rats injured with cardiac ischemia/reperfusion (I/R) and curcumin induced reduction in oxidative stress, inflammation, and cardiomyocyte apoptosis [25]. The anti-apoptotic effect of curcumin on cardiomyocytes was also reported to be mediated through the downregulation of NF-κB expression and upregulation of expression PPAR-γ and B-cell lymphoma-2 (Bcl-2), an apoptotic factor [128]. Others have reported that curcumin induced upregulation of microRNA-7a/b (miR-7a/b), while also downregulating specific protein 1 (SP1) [129]. Kim et al. [130] reported that curcumin was able to protect cardiac contractibility and cardiac function in I/R-injured rats, and this effect could be mediated by decreasing toll-like receptor 2 (TLR2) expression and macrophage infiltration. TLR2, a key mediator of the innate immune system, is involved in MI by activating the NF-κB pathway that results in cardiomyocyte inflammation and contractile dysfunction [131, 132]. An in vitro model of neonatal rat cardiomyocytes treated with curcumin confirmed the downregulation of TLR2 expression, when MI cells were challenged with hypoxia/reoxygenation (H/R) to mimic the in vivo I/R process [130]. Post-MI cardiac fibrosis was prevented by curcumin, restoring MI-induced downregulation of nicotinamide adenine dinucleotide (NAD)-dependent deacetylase sirtuin-1 (SIRT-1) expression, and collagen deposition in heart tissues [133]. Taken together, these findings show that the capacity of curcumin to ameliorate MI and MI-induced injury is by attenuating oxidative stress, inflammatory status, cardiomyocyte apoptosis, and collagen deposition in the infarcted area, all of which contribute to a reduced infarction size and improved cardiac function. An RCT study reported that curcuminoid administration at 4 g day−1 for 3 days before coronary artery bypass grafting (CABG) surgery and 5 days after the surgery, significantly reduced the incidence of in-hospital MI events associated with CABG [26]. In this study, postoperative levels of CRP, MDA, and N-terminal pro-B-type natriuretic peptide were also improved. These biomarkers indicate a direct involvement of antioxidant and anti-inflammatory effects of curcuminoids in the protection against CABG-associated MI. The efficacy of curcuminoids, or other turmeric bioactives, on prevention and treatment of MI in a more general population has not yet been established.
Cardiac hypertrophy is characterized by abnormal enlargement or thickening of heart muscle caused by increased cardiomyocyte size. The more intensive sarcomere is an adaptive response to hemodynamic stresses that results from various pro-hypertrophic stimuli [134]. Although it is compensatory to improve cardiac performance under a stress-induced condition, persisted hypertrophy can cause cardiac decompensation and contractile dysfunction, which will eventually lead to heart failure [134]. Curcumin, DMC, and BDMC have protective effects against cardiac hypertrophy, and one of the most critical mechanisms involves the inhibition of p300-specific histone acetyltransferase (HAT) activity [135]. p300-HAT is a transcriptional coactivator of several transcription factors, e.g., GATA-binding factor 4 (GATA4), critically important for both the development and differentiation of cardiomyocytes, which precede the progression of cardiac hypertrophy and heart failure. Indeed, histone acetylation is a notable transcriptional modification that mediate the activation of these transcription factors. Inhibition of p300-HAT activity was associated with reduced histone acetylation and hypertrophic responses in rat cardiomyocytes [135]. Curcumin, DMC, and BDMC had positive effects on p300-HAT inhibitory activity and anti-hypertrophic effects to a similar extent. In cardiomyocyte models, curcumin inhibited not only p300-HAT but also the nuclear localization and DNA-binding activity of GATA4 [136, 137], and p300-GATA4 interaction [136]. These effects were associated with repressed hypertrophic responses of the cardiomyocytes, and prevention of heart failure in both hypertension-induced and MI-induced heart failure rat models [136].
Associated with these protective effects of curcumin on molecular signaling of myocardial health is the observation that curcuminoid supplementation reduced circulating CRP levels, a chronic inflammatory biomarker that predicts risk to atherothrombosis and CVD in both normal healthy individuals and individuals with chronic health conditions [119]. However, more human clinical evidence for turmeric having protective and therapeutic efficacies against CVD, in particular, is needed. Furthermore, well-designed and longer-term RCTs with specific CVD outcome measures are required to confirm the potential health benefits of curcumin in lowering incidence of CVD.
Conclusion
This review summarized the complex chemical composition and specific bioactivities of turmeric and turmeric-derived constituents, such as curcumin, DMC, BMC, and TO. A focus was placed on describing cellular and molecular mechanisms that underlie the etiology and pathogenesis of diabetes, and CVD disorders, and how the protective properties of turmeric and its constituents can lessen these chronic disease conditions. Favorable results generated from human RCTs on the efficacies of these bioactives that mitigate risk factors for the aforementioned health conditions further support the use of turmeric constituents as ingredients in functional food and nutraceutical preparations. To fully evaluate the long-term preventative and therapeutic efficacies of these compounds, RCTs with subjects from a more general population, having longer intervention durations and a specific endpoint for reduction in disease outcomes are warranted.
Acknowledgements
HZ was funded from a Natural Sciences and Engineering Research Council (NSERC) Discovery Grant to DDK [No. RGPIN2019-04130].
Abbreviations
- 2DG
2-Deoxyglucose
- ABCA-1
Adenosine triphosphate (ATP)-binding cassette transporter A1
- AGE
Advanced glycation end-product
- Akt
Protein kinase B
- AMPK
5′ Adenosine monophosphate-activated protein kinase
- ANF
Atrial natriuretic factor
- Ang II
Angiotensin II
- aP2
Adipocyte Protein 2 (aka. fatty acid-binding protein 4, FABP4)
- ApoAI
Apolipoprotein AI
- ApoE–/–
Apolipoprotein E knockout
- ATP
Adenosine triphosphate
- Bax
Bcl-2-associated X protein
- Bcl-2
B-cell lymphoma-2
- BDMC
Bisdemethoxycurcumin
- β-MHC
Beta-myosin heavy chain
- BMI
Body mass index
- BNP
Brain natriuretic peptide
- CABG
Coronary artery bypass grafting
- CAT
Catalase
- CD36
Cluster of differentiation 36
- CD68
Cluster of differentiation 68
- C/EBP
CCAAT/enhancer-binding protein
- CHOP
C/EBP homologous protein
- CK-MB
Creatine kinase-MB
- CRP
C-reactive protein
- CVD
Cardiovascular diseases
- DMC
Demethoxycurcumin
- DSPN
Diabetic sensorimotor polyneuropathy
- ECM
Extracellular matrix
- ER
Endoplasmic reticulum
- ERK1/2
Extracellular signal-regulated kinase 1/2
- FBS
Fasting blood sugar
- FFAR
Free fatty acid receptor
- FOXO3a
Forkhead box O3a
- G6P
Glucose 6-phosphate
- GATA4
GATA-binding factor 4
- GCK
Glucokinase
- GLP-1
Glucagon-like peptide -1
- GLUT
Glucose transporter
- GPR
G-protein-coupled receptor
- GR
Glutathione reductase
- GSH-Px
Glutathione peroxidase
- GSIS
Glucose-stimulated insulin secretion
- HAT
Histone acetyltransferase
- HbA1c
Hemoglobin A1c (glycated hemoglobin)
- HDL-c
High-density lipoprotein cholesterol
- HFD
High-fat diet
- H/R
Hypoxia/reoxygenation
- hs-CRP
High-sensitivity C-reactive protein
- ICAM-1
Intercellular cell adhesion molecule-1
- IκB
Inhibitor of NF-κB
- IL
Interleukin
- i.p.
Intraperitoneal injection
- IR
Insulin receptor
- I/R
Ischemia/reperfusion
- IRS
Insulin receptor substrate
- JAK
Janus kinase
- Keap1
Kelch-like ECH-associated protein 1
- LC3
Microtubule-associated protein 1 light chain 3
- LDH
Lactate dehydrogenase
- LDL
Low-density lipoproteins
- LDL-c
Low-density lipoprotein cholesterol
- LDL-R
Low-density lipoprotein receptor
- Lp(a)
Lipoprotein a
- LXRα
Liver X receptor α
- MAPK
Mitogen-activated protein kinase
- MCP-1
Mast cell protease 1
- MDA
Malondialdehyde
- MetS
Metabolic syndrome
- MI
Myocardial infarction
- miR-7a/b
MicroRNA-7a/b
- MMP-2
Matrix metalloproteinase-2
- NAD
Nicotinamide adenine dinucleotide
- NF-κB
Nuclear factor kappa B
- Nrf2
Nuclear factor erythroid 2-related factor 2
- NT-pro-BNP
N-terminal pro-B-type natriuretic peptide
- oxLDL
Oxidized low-density lipoproteins
- PAB
Pro-oxidant-antioxidant balance
- PDK1
3-Phosphoinositide-dependent protein kinase-1
- PDX-1
Pancreatic and duodenal homeobox-1
- p-ERK1/2
Extracellular signal-regulated kinase 1/2
- PGC-1α
Peroxisome proliferator-activated receptor-γ coactivator-1α
- PGN
Peptidoglycan
- PI3K
Phosphatidylinositol-3-kinase
- PIP2
Phosphatidylinositol-4,5-bisphosphate
- PIP3
Phosphatidylinositol-3,4,5-trisphosphate
- p.o.
Oral administration (Latin per os)
- PPAR-γ
Peroxisome proliferator-activated receptor-γ
- RCT
Randomized clinical trials
- SIRT-1
Sirtuin-1
- SOD
Superoxide dismutase
- SP1
Specific protein 1
- SR-A
Scavenger receptor class A
- SREBP
Sterol regulatory element-binding protein
- STAT
Signal transducer and activator of transcription
- T2D
Type 2 diabetes
- TC
Total cholesterol
- TG
Triglyceride
- TGF-β1
Transforming growth factor beta 1
- TLR
Toll-like receptor
- TNF-α
Tumor necrosis factor α
- VCAM-1
Vascular cell adhesion molecule-1
- VCP
Valosin-containing protein
- WC
Waist circumference
- %BF
Percent body fat
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Huiying Amelie Zhang, Email: amelie.huiying.zhang@ubc.ca.
David D. Kitts, Email: david.kitts@ubc.ca
References
- 1.Kocaadam B, Şanlier N. Curcumin, an active component of turmeric (Curcuma longa), and its effects on health. Crit Rev Food Sci Nutr. 2017;57(13):2889–2895. doi: 10.1080/10408398.2015.1077195. [DOI] [PubMed] [Google Scholar]
- 2.Nair KPP. 1—turmeric: origin and history. In: Nair KPP, editor. The agronomy and economy of turmeric and ginger. Oxford: Elsevier; 2013. pp. 1–5. [Google Scholar]
- 3.Prasad S, Aggarwal BB. Turmeric, the golden spice: from traditional medicine to modern medicine. In: Benzie IFF, Wachtel-Galor S, editors. Herbal medicine: biomolecular and clinical aspects. 2. Boca Raton: CRC Press/Taylor & Francis; 2011. pp. 263–288. [PubMed] [Google Scholar]
- 4.Solymosi K, Latruffe N, Morant-Manceau A, Schoefs B. 1—food colour additives of natural origin. In: Scotter MJ, editor. Colour additives for foods and beverages. Woodhead Publishing Series in Food Science, Technology and Nutrition. Oxford: Woodhead Publishing; 2015. pp. 3–34. [Google Scholar]
- 5.Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: the Indian solid gold. In: Aggarwal BB, Surh Y-J, Shishodia S, editors. The molecular targets and therapeutic uses of curcumin in health and disease. Advances in experimental medicine and biology. Boston: Springer US; 2007. pp. 1–75. [DOI] [PubMed] [Google Scholar]
- 6.Portincasa P, Bonfrate L, Scribano MLL, Kohn A, Caporaso N, Festi D, Campanale MC, Di Rienzo T, Guarino M, Taddia M, Fogli MV, Grimaldi M, Gasbarrini A. Curcumin and fennel essential oil improve symptoms and quality of life in patients with irritable bowel syndrome. J Gastrointest Liver Dis. 2016;25(2):151–157. doi: 10.15403/jgld.2014.1121.252.ccm. [DOI] [PubMed] [Google Scholar]
- 7.Sanidad KZ, Sukamtoh E, Xiao H, McClements DJ, Zhang G. Curcumin: recent advances in the development of strategies to improve oral bioavailability. Annu Rev Food Sci Technol. 2019;10(1):597–617. doi: 10.1146/annurev-food-032818-121738. [DOI] [PubMed] [Google Scholar]
- 8.Verma RK, Kumari P, Maurya RK, Kumar V, Verma RB, Singh RK. Medicinal properties of turmeric (Curcuma longa L.): a review. Int J Chem Stud. 2018;6(4):1354–1357. [Google Scholar]
- 9.Smith T, Gillespie M, Eckl V, Knepper J, Reynolds CM (2019) Herbal supplement sales in US increase by 9.4% in 2018. Am Bot Counc. http://cms.herbalgram.org/herbalgram/issue123/files/HG123-HMR.pdf. Accessed 03 Dec 2020
- 10.Emirik M. Potential therapeutic effect of turmeric contents against SARS-CoV-2 compared with experimental COVID-19 therapies: in silico study. J Biomol Struct Dyn. 2020 doi: 10.1080/07391102.2020.1835719. [DOI] [PubMed] [Google Scholar]
- 11.Valizadeh H, Abdolmohammadi-Vahid S, Danshina S, Ziya Gencer M, Ammari A, Sadeghi A, Roshangar L, Aslani S, Esmaeilzadeh A, Ghaebi M, Valizadeh S, Ahmadi M. Nano-curcumin therapy, a promising method in modulating inflammatory cytokines in COVID-19 patients. Int Immunopharmacol. 2020;89(Pt B):107088. doi: 10.1016/j.intimp.2020.107088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meng F-C, Zhou Y-Q, Ren D, Wang R, Wang C, Lin L-G, Zhang X-Q, Ye W-C, Zhang Q-W. Chapter 10—turmeric: a review of its chemical composition, quality control, bioactivity, and pharmaceutical application. In: Grumezescu AM, Holban AM, editors. Natural and artificial flavoring agents and food dyes. Cambridge: Academic Press; 2018. pp. 299–350. [Google Scholar]
- 13.Amalraj A, Pius A, Gopi S, Gopi S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives—a review. J Tradit Complement Med. 2017;7(2):205–233. doi: 10.1016/j.jtcme.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kunnumakkara AB, Bordoloi D, Padmavathi G, Monisha J, Roy NK, Prasad S, Aggarwal BB. Curcumin, the golden nutraceutical: multitargeting for multiple chronic diseases. Br J Pharmacol. 2017;174(11):1325–1348. doi: 10.1111/bph.13621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akter J, Hossain MA, Takara K, Islam MZ, Hou D-X. Antioxidant activity of different species and varieties of turmeric (Curcuma spp): isolation of active compounds. Comp Biochem Physiol Part C: Toxicol Pharmacol. 2019;215:9–17. doi: 10.1016/j.cbpc.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Alizadeh M, Kheirouri S. Curcumin reduces malondialdehyde and improves antioxidants in humans with diseased conditions: a comprehensive meta-analysis of randomized controlled trials. Biomedicine. 2019;9(4):10–22. doi: 10.1051/bmdcn/2019090423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dall'Acqua S, Stocchero M, Boschiero I, Schiavon M, Golob S, Uddin J, Voinovich D, Mammi S, Schievano E. New findings on the in vivo antioxidant activity of Curcuma longa extract by an integrated 1H NMR and HPLC–MS metabolomic approach. Fitoterapia. 2016;109:125–131. doi: 10.1016/j.fitote.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Ghazimoradi M, Saberi-Karimian M, Mohammadi F, Sahebkar A, Tavallaie S, Safarian H, Ferns GA, Ghayour-Mobarhan M, Moohebati M, Esmaeili H, Ahmadinejad M. The effects of curcumin and curcumin-phospholipid complex on the cerum pro-oxidant-antioxidant balance in subjects with metabolic syndrome. Phytother Res. 2017;31(11):1715–1721. doi: 10.1002/ptr.5899. [DOI] [PubMed] [Google Scholar]
- 19.Edwards RL, Luis PB, Nakashima F, Kunihiro AG, Presley S-H, Funk JL, Schneider C. Mechanistic differences in the inhibition of NF-κB by turmeric and its curcuminoid constituents. J Agric Food Chem. 2020;68(22):6154–6160. doi: 10.1021/acs.jafc.0c02607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rana M, Reddy SS, Maurya P, Singh V, Chaturvedi S, Kaur K, Agarwal H, Ahmad H, Naqvi A, Dwivedi AK, Dikshit M, Barthwal MK. Turmerone enriched standardized Curcuma longa extract alleviates LPS induced inflammation and cytokine production by regulating TLR4–IRAK1–ROS–MAPK–NFκB axis. J Funct Foods. 2015;16:152–163. doi: 10.1016/j.jff.2015.04.034. [DOI] [Google Scholar]
- 21.White CM, Pasupuleti V, Roman YM, Li Y, Hernandez AV. Oral turmeric/curcumin effects on inflammatory markers in chronic inflammatory diseases: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2019;146:104280. doi: 10.1016/j.phrs.2019.104280. [DOI] [PubMed] [Google Scholar]
- 22.Fu M, Fu S, Ni S, Wang D, Hong T. Inhibitory effects of bisdemethoxycurcumin on mast cell-mediated allergic diseases. Int Immunopharmacol. 2018;65:182–189. doi: 10.1016/j.intimp.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Wu S, Xiao D. Effect of curcumin on nasal symptoms and airflow in patients with perennial allergic rhinitis. Ann Allergy Asthma Immunol. 2016;117(6):697–702.e691. doi: 10.1016/j.anai.2016.09.427. [DOI] [PubMed] [Google Scholar]
- 24.Zhang N, Li H, Jia J, He M. Anti-inflammatory effect of curcumin on mast cell-mediated allergic responses in ovalbumin-induced allergic rhinitis mouse. Cell Immunol. 2015;298(1):88–95. doi: 10.1016/j.cellimm.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Liu T, Zhang L, Joo D, Sun S-C. NF-κB signaling in inflammation. Signal Transduct Target Ther. 2017;2(1):1–9. doi: 10.1038/sigtrans.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wongcharoen W, Jai-aue S, Phrommintikul A, Nawarawong W, Woragidpoonpol S, Tepsuwan T, Sukonthasarn A, Apaijai N, Chattipakorn N. Effects of curcuminoids on frequency of acute myocardial infarction after coronary artery bypass grafting. Am J Cardiol. 2012;110(1):40–44. doi: 10.1016/j.amjcard.2012.02.043. [DOI] [PubMed] [Google Scholar]
- 27.Zhang S, Zou J, Li P, Zheng X, Feng D. Curcumin protects against atherosclerosis in apolipoprotein e-knockout mice by inhibiting toll-like receptor 4 expression. J Agric Food Chem. 2018;66(2):449–456. doi: 10.1021/acs.jafc.7b04260. [DOI] [PubMed] [Google Scholar]
- 28.Zhao J-F, Ching L-C, Huang Y-C, Chen C-Y, Chiang A-N, Kou YR, Shyue S-K, Lee T-S. Molecular mechanism of curcumin on the suppression of cholesterol accumulation in macrophage foam cells and atherosclerosis. Mol Nutr Food Res. 2012;56(5):691–701. doi: 10.1002/mnfr.201100735. [DOI] [PubMed] [Google Scholar]
- 29.Asadi S, Gholami MS, Siassi F, Qorbani M, Khamoshian K, Sotoudeh G. Nano curcumin supplementation reduced the severity of diabetic sensorimotor polyneuropathy in patients with type 2 diabetes mellitus: a randomized double-blind placebo- controlled clinical trial. Complement Ther Med. 2019;43:253–260. doi: 10.1016/j.ctim.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 30.Hou K, Chen Y, Zhu D, Chen G, Chen F, Xu N, Barakat K, Zheng J, Xie X, Chen R. Curcumin inhibits high glucose oxidative stress and apoptosis in pancreatic beta cells via CHOP/PCG-1a and pERK1/2. Front Biosci (Landmark Ed) 2020;25:1974–1984. doi: 10.2741/4858. [DOI] [PubMed] [Google Scholar]
- 31.Kato M, Nishikawa S, Ikehata A, Dochi K, Tani T, Takahashi T, Imaizumi A, Tsuda T. Curcumin improves glucose tolerance via stimulation of glucagon-like peptide-1 secretion. Mol Nutr Food Res. 2017;61(3):1600471. doi: 10.1002/mnfr.201600471. [DOI] [PubMed] [Google Scholar]
- 32.Song Z, Wang H, Zhu L, Han M, Gao Y, Du Y, Wen Y. Curcumin improves high glucose-induced INS-1 cell insulin resistance via activation of insulin signaling. Food Funct. 2015;6(2):461–469. doi: 10.1039/C4FO00608A. [DOI] [PubMed] [Google Scholar]
- 33.Kuttikrishnan S, Siveen KS, Prabhu KS, Khan AQ, Ahmed EI, Akhtar S, Ali TA, Merhi M, Dermime S, Steinhoff M, Uddin S. Curcumin induces apoptotic cell death via inhibition of PI3-kinase/AKT pathway in B-precursor acute lymphoblastic leukemia. Front Oncol. 2019 doi: 10.3389/fonc.2019.00484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li M, Yue GG-L, Tsui SK-W, Fung K-P, Lau CB-S. Turmeric extract, with absorbable curcumin, has potent anti-metastatic effect in vitro and in vivo. Phytomedicine. 2018;46:131–141. doi: 10.1016/j.phymed.2018.03.065. [DOI] [PubMed] [Google Scholar]
- 35.Ramasamy TS, Ayob AZ, Myint HHL, Thiagarajah S, Amini F. Targeting colorectal cancer stem cells using curcumin and curcumin analogues: insights into the mechanism of the therapeutic efficacy. Cancer Cell Int. 2015;15:96. doi: 10.1186/s12935-015-0241-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang X-P, Wang Q-X, Lin H-P, Chang N. Anti-tumor bioactivities of curcumin on mice loaded with gastric carcinoma. Food Funct. 2017;8(9):3319–3326. doi: 10.1039/c7fo00555e. [DOI] [PubMed] [Google Scholar]
- 37.Bhat A, Mahalakshmi AM, Ray B, Tuladhar S, Hediyal TA, Manthiannem E, Padamati J, Chandra R, Chidambaram SB, Sakharkar MK. Benefits of curcumin in brain disorders. BioFactors. 2019;45(5):666–689. doi: 10.1002/biof.1533. [DOI] [PubMed] [Google Scholar]
- 38.Forouzanfar F, Read MI, Barreto GE, Sahebkar A. Neuroprotective effects of curcumin through autophagy modulation. IUBMB Life. 2020;72(4):652–664. doi: 10.1002/iub.2209. [DOI] [PubMed] [Google Scholar]
- 39.Huang L, Chen C, Zhang X, Li X, Chen Z, Yang C, Liang X, Zhu G, Xu Z. Neuroprotective effect of curcumin against cerebral ischemia-reperfusion via mediating autophagy and inflammation. J Mol Neurosc. 2018;64(1):129–139. doi: 10.1007/s12031-017-1006-x. [DOI] [PubMed] [Google Scholar]
- 40.Al-Karawi D, Al Mamoori DA, Tayyar Y. The role of curcumin administration in patients with major depressive disorder: mini meta-analysis of clinical trials. Phytother Res. 2016;30(2):175–183. doi: 10.1002/ptr.5524. [DOI] [PubMed] [Google Scholar]
- 41.Ng QX, Koh SSH, Chan HW, Ho CYX. Clinical use of curcumin in depression: a meta-analysis. J Am Med Dir Assoc. 2017;18(6):503–508. doi: 10.1016/j.jamda.2016.12.071. [DOI] [PubMed] [Google Scholar]
- 42.Wang Z, Zhang Q, Yuan L, Wang S, Liu L, Yang X, Li G, Liu D. The effects of curcumin on depressive-like behavior in mice after lipopolysaccharide administration. Behav Brain Res. 2014;274:282–290. doi: 10.1016/j.bbr.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 43.Goodarzi R, Sabzian K, Shishehbor F, Mansoori A. Does turmeric/curcumin supplementation improve serum alanine aminotransferase and aspartate aminotransferase levels in patients with nonalcoholic fatty liver disease? A systematic review and meta-analysis of randomized controlled trials. Phytother Res. 2019;33(3):561–570. doi: 10.1002/ptr.6270. [DOI] [PubMed] [Google Scholar]
- 44.Khan H, Ullah H, Nabavi SM. Mechanistic insights of hepatoprotective effects of curcumin: therapeutic updates and future prospects. Food Chem Toxicol. 2019;124:182–191. doi: 10.1016/j.fct.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Naik RS, Mujumdar AM, Ghaskadbi S. Protection of liver cells from ethanol cytotoxicity by curcumin in liver slice culture in vitro. J Ethnopharmacol. 2004;95(1):31–37. doi: 10.1016/j.jep.2004.06.032. [DOI] [PubMed] [Google Scholar]
- 46.World Health Organization (2018) The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 03 Dec 2020
- 47.Kotha RR, Luthria DL. Curcumin: biological, pharmaceutical, nutraceutical, and analytical aspects. Molecules. 2019;24(16):2930. doi: 10.3390/molecules24162930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nelson KM, Dahlin JL, Bisson J, Graham J, Pauli GF, Walters MA. The essential medicinal chemistry of curcumin. J Med Chem. 2017;60(5):1620–1637. doi: 10.1021/acs.jmedchem.6b00975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prasad S, Gupta SC, Tyagi AK, Aggarwal BB. Curcumin, a component of golden spice: from bedside to bench and back. Biotechnol Adv. 2014;32(6):1053–1064. doi: 10.1016/j.biotechadv.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 50.Lee J, Jung Y, Shin J-H, Kim HK, Moon BC, Ryu DH, Hwang G-S. Secondary metabolite profiling of Curcuma species grown at different locations using GC/TOF and UPLC/Q-TOF MS. Molecules. 2014;19(7):9535–9551. doi: 10.3390/molecules19079535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jacob JN. Chapter 4—comparative studies in relation to the structure and biochemical properties of the active compounds in the volatile and nonvolatile fractions of turmeric (C. longa) and ginger (Z. officinale) In: Atta-ur-Rahman, editor. Studies in natural products chemistry, vol 48. Amsterdam, Netherlands: Elsevier; 2016. pp. 101–135. [Google Scholar]
- 52.Masuda T, Jitoe A, Isobe J, Nakatani N, Yonemori S. Anti-oxidative and anti-inflammatory curcumin-related phenolics from rhizomes of Curcuma domestica. Phytochemistry. 1993;32(6):1557–1560. doi: 10.1016/0031-9422(93)85179-U. [DOI] [Google Scholar]
- 53.Li W, Wang S, Feng J, Xiao Y, Xue X, Zhang H, Wang Y, Liang X. Structure elucidation and NMR assignments for curcuminoids from the rhizomes of Curcuma longa. Magn Reson Chem. 2009;47(10):902–908. doi: 10.1002/mrc.2478. [DOI] [PubMed] [Google Scholar]
- 54.Dao TT, Nguyen PH, Won HK, Kim EH, Park J, Won BY, Oh WK. Curcuminoids from Curcuma longa and their inhibitory activities on influenza A neuraminidases. Food Chem. 2012;134(1):21–28. doi: 10.1016/j.foodchem.2012.02.015. [DOI] [Google Scholar]
- 55.Nakayama R, Tamura Y, Yamanaka H, Kikuzaki H, Nakatani N. Two curcuminoid pigments from Curcuma domestica. Phytochemistry. 1993;33(2):501–502. doi: 10.1016/0031-9422(93)85548-6. [DOI] [Google Scholar]
- 56.Kiuchi F, Goto Y, Sugimoto N, Akao N, Kondo K, Tsuda Y. Nematocidal activity of turmeric: synergistic action of curcuminoids. Chem Pharm Bull. 1993;41(9):1640–1643. doi: 10.1248/cpb.41.1640. [DOI] [PubMed] [Google Scholar]
- 57.Shang Z-P, Xu L-L, Lu Y-Y, Guan M, Li D-Y, Le Z-Y, Bai Z-L, Qiao X, Ye M. Advances in chemical constituents and quality control of turmeric. World J Tradit Chin Med. 2019;5(2):116. doi: 10.4103/wjtcm.wjtcm_12_19. [DOI] [Google Scholar]
- 58.Priyadarsini KI. The chemistry of curcumin: from extraction to therapeutic agent. Molecules. 2014;19(12):20091–20112. doi: 10.3390/molecules191220091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Price LC, Buescher RW. Kinetics of alkaline degradation of the food pigments curcumin and curcuminoids. J Food Sci. 1997;62(2):267–269. doi: 10.1111/j.1365-2621.1997.tb03982.x. [DOI] [Google Scholar]
- 60.Priyadarsini KI. Photophysics, photochemistry and photobiology of curcumin: studies from organic solutions, bio-mimetics and living cells. J Photochem Photobiol C: Photochem Rev. 2009;10(2):81–95. doi: 10.1016/j.jphotochemrev.2009.05.001. [DOI] [Google Scholar]
- 61.Tønnesen HH, Karlsen J, van Henegouwen GB. Studies on curcumin and curcuminoids VIII. Photochemical stability of curcumin. Z Lebensm Unters Forch. 1986;183(2):116–122. doi: 10.1007/BF01041928. [DOI] [PubMed] [Google Scholar]
- 62.Sasaki H, Sunagawa Y, Takahashi K, Imaizumi A, Fukuda H, Hashimoto T, Wada H, Katanasaka Y, Kakeya H, Fujita M, Hasegawa K, Morimoto T. Innovative preparation of curcumin for improved oral bioavailability. Biol Pharm Bull. 2011;34(5):660–665. doi: 10.1248/bpb.34.660. [DOI] [PubMed] [Google Scholar]
- 63.Kharat M, Aberg J, Dai T, McClements DJ. Comparison of emulsion and nanoemulsion delivery systems: the chemical stability of curcumin decreases as oil droplet size decreases. J Agric Food Chem. 2020;68(34):9205–9212. doi: 10.1021/acs.jafc.0c01877. [DOI] [PubMed] [Google Scholar]
- 64.Arvapalli DM, Sheardy AT, Allado K, Chevva H, Yin Z, Wei J. Design of curcumin loaded carbon nanodots delivery system: enhanced bioavailability, release kinetics, and anticancer activity. ACS Appl Bio Mater. 2020;3(12):8776–8785. doi: 10.1021/acsabm.0c01144. [DOI] [PubMed] [Google Scholar]
- 65.Suresh D, Srinivasan K. Studies on the in vitro absorption of spice principles—curcumin, capsaicin and piperine in rat intestines. Food Chem Toxicol. 2007;45(8):1437–1442. doi: 10.1016/j.fct.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 66.Verma SP, Salamone E, Goldin B. Curcumin and genistein, plant natural products, show synergistic inhibitory effects on the growth of human breast cancer MCF-7 cells induced by estrogenic pesticides. Biochem Biophys Res Commun. 1997;233(3):692–696. doi: 10.1006/bbrc.1997.6527. [DOI] [PubMed] [Google Scholar]
- 67.Eckert RL, Crish JF, Efimova T, Balasubramanian S. Opposing action of curcumin and green tea polyphenol in human keratinocytes. Mol Nutr Food Res. 2006;50(2):123–129. doi: 10.1002/mnfr.200500125. [DOI] [PubMed] [Google Scholar]
- 68.Afzal A, Oriqat G, Khan MA, Jose J, Afzal M. Chemistry and biochemistry of terpenoids from Curcuma and related species. J Biol Act Prod Nat. 2013;3(1):1–55. doi: 10.1080/22311866.2013.782757. [DOI] [Google Scholar]
- 69.Golding BT, Pombo-Villar E. Structures of α- and β-turmerone. J Chem Soc Perkin Trans. 1992;1(12):1519–1524. doi: 10.1039/P19920001519. [DOI] [Google Scholar]
- 70.Ferreira LAF, Henriques OB, Andreoni AAS, Vital GRF, Campos MMC, Habermehl GG, de Moraes VLG. Antivenom and biological effects of ar-turmerone isolated from Curcuma longa (Zingiberaceae) Toxicon. 1992;30(10):1211–1218. doi: 10.1016/0041-0101(92)90437-A. [DOI] [PubMed] [Google Scholar]
- 71.Jantan I, Saputri FC, Qaisar MN, Buang F. Correlation between chemical composition of curcuma domestica and Curcuma xanthorrhiza and their antioxidant effect on human low-density lipoprotein oxidation. Evid Based Complement Altern Med. 2012 doi: 10.1155/2012/438356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hwang K-W, Son D, Jo H-W, Kim CH, Seong KC, Moon J-K. Levels of curcuminoid and essential oil compositions in turmerics (Curcuma longa L.) grown in Korea. Appl Biol Chem. 2016;59(2):209–215. doi: 10.1007/s13765-016-0156-9. [DOI] [Google Scholar]
- 73.Liju VB, Jeena K, Kuttan R. An evaluation of antioxidant, anti-inflammatory, and antinociceptive activities of essential oil from Curcuma longa L. Indian J Pharmacol. 2011;43(5):526–531. doi: 10.4103/0253-7613.84961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kiso Y, Suzuki Y, Oshima Y, Hikino H. Stereostructure of curlone, a sesquiterpenoid of Curcuma longa rhizomes. Phytochemistry. 1983;22(2):596–597. doi: 10.1016/0031-9422(83)83057-X. [DOI] [Google Scholar]
- 75.Chen J-J, Tsai C-S, Hwang T-L, Shieh P-C, Chen J-F, Sung P-J. Sesquiterpenes from the rhizome of Curcuma longa with inhibitory activity on superoxide generation and elastase release by neutrophils. Food Chem. 2010;119(3):974–980. doi: 10.1016/j.foodchem.2009.07.060. [DOI] [Google Scholar]
- 76.Braga MEM, Leal PF, Carvalho JE, Meireles MAA. Comparison of yield, composition, and antioxidant activity of turmeric (Curcuma longa L.) extracts obtained using various techniques. J Agric Food Chem. 2003;51(22):6604–6611. doi: 10.1021/jf0345550. [DOI] [PubMed] [Google Scholar]
- 77.Ferreira FD, Kemmelmeier C, Arrotéia CC, da Costa CL, Mallmann CA, Janeiro V, Ferreira FMD, Mossini SAG, Silva EL, Machinski M. Inhibitory effect of the essential oil of Curcuma longa L. and curcumin on aflatoxin production by Aspergillus flavus Link. Food Chem. 2013;136(2):789–793. doi: 10.1016/j.foodchem.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 78.Li W, Feng J-T, Xiao Y-S, Wang Y-Q, Xue X-Y, Liang X-M. Three novel terpenoids from the rhizomes of Curcuma longa. J Asian Nat Prod Res. 2009;11(6):569–575. doi: 10.1080/10286020902939182. [DOI] [PubMed] [Google Scholar]
- 79.Ohshiro M, Kuroyanagi M, Ueno A. Structures of sesquiterpenes from Curcuma longa. Phytochemistry. 1990;29(7):2201–2205. doi: 10.1016/0031-9422(90)83038-3. [DOI] [Google Scholar]
- 80.Li J, Wang H-F, Chen G, Huang S-D, Zhang W-Y, Hua H-M, Pei Y-H. Structure determination of two new bisabolane-type sesquiterpenes from the rhizomes of Curcuma longa by NMR spectroscopy. Magn Reson Chem. 2015;53(7):536–538. doi: 10.1002/mrc.4215. [DOI] [PubMed] [Google Scholar]
- 81.Zhang W-Y, Wang H-F, Chen G, Zhang O, Bai S, Pei Y-H. Two new bisabolane sesquiterpenoids from Curcuma longa. J Asian Nat Prod Res. 2014;16(3):271–274. doi: 10.1080/10286020.2013.875010. [DOI] [PubMed] [Google Scholar]
- 82.Imai S, Morikiyo M, Furihata K, Hayakawa Y, Seto H. Turmeronol A and turmeronol B, new inhibitors of soybean lipoxygenase. Agric Biol Chem. 1990;54(9):2367–2371. doi: 10.1080/00021369.1990.10870290. [DOI] [Google Scholar]
- 83.Zeng Y, Qiu F, Takahashi K, Liang J, Qu G, Yao X. New sesquiterpenes and calebin derivatives from Curcuma longa. Chem Pharm Bull. 2007;55(6):940–943. doi: 10.1248/cpb.55.940. [DOI] [PubMed] [Google Scholar]
- 84.Wen J, Qiu T-Y, Yan X-J, Qiu F. Four novel bisabolane-type sesquiterpenes from Curcuma longa. J Asian Nat Prod Res. 2018;20(10):928–933. doi: 10.1080/10286020.2017.1367769. [DOI] [PubMed] [Google Scholar]
- 85.Yuan T, Zhang C, Qiu C, Xia G, Wang F, Lin B, Li H, Chen L. Chemical constituents from Curcuma longa L. and their inhibitory effects of nitric oxide production. Nat Prod Res. 2018;32(16):1887–1892. doi: 10.1080/14786419.2017.1354185. [DOI] [PubMed] [Google Scholar]
- 86.Xu J, Ji F, Kang J, Wang H, Li S, Jin D-Q, Zhang Q, Sun H, Guo Y. Absolute configurations and NO inhibitory activities of terpenoids from Curcuma longa. J Agric Food Chem. 2015;63(24):5805–5812. doi: 10.1021/acs.jafc.5b01584. [DOI] [PubMed] [Google Scholar]
- 87.Del Prete D, Millán E, Pollastro F, Chianese G, Luciano P, Collado JA, Munoz E, Appendino G, Taglialatela-Scafati O. Turmeric sesquiterpenoids: expeditious resolution, comparative bioactivity, and a new bicyclic turmeronoid. J Nat Prod. 2016;79(2):267–273. doi: 10.1021/acs.jnatprod.5b00637. [DOI] [PubMed] [Google Scholar]
- 88.Awasthi PK, Dixit SC. Chemical composition of Curcuma longa leaves and rhizome oil from the plains of Northern India. J Young Pharm. 2009;1(4):312. doi: 10.4103/0975-1483.59319. [DOI] [Google Scholar]
- 89.Lin X, Ji S, Li R, Dong Y, Qiao X, Hu H, Yang W, Guo D, Tu P, Ye M. Terpecurcumins A-I from the rhizomes of Curcuma longa: absolute configuration and cytotoxic activity. J Nat Prod. 2012;75(12):2121–2131. doi: 10.1021/np300551g. [DOI] [PubMed] [Google Scholar]
- 90.Lin X, Ji S, Qiao X, Hu H, Chen N, Dong Y, Huang Y, Guo D, Tu P, Ye M. Density functional theory calculations in stereochemical determination of terpecurcumins J–W, cytotoxic terpene-conjugated curcuminoids from Curcuma longa L. J Org Chem. 2013;78(23):11835–11848. doi: 10.1021/jo401859u. [DOI] [PubMed] [Google Scholar]
- 91.Qiao X, Lin X-h, Ji S, Zhang Z-x, Bo T, Guo D-a, Ye M. Global profiling and novel structure discovery using multiple neutral loss/precursor ion scanning combined with substructure recognition and statistical analysis (MNPSS): characterization of terpene-conjugated curcuminoids in Curcuma longa as a case study. Anal Chem. 2016;88(1):703–710. doi: 10.1021/acs.analchem.5b02729. [DOI] [PubMed] [Google Scholar]
- 92.Xiao YC, Xie J, Yu M, Liu M, Ran J, Xi Z, Li W, Huang J. Bisabocurcumin, a new skeleton curcuminoid from the rhizomes of Curcuma longa L. Chin Chem Lett. 2011;22(12):1457–1460. doi: 10.1016/j.cclet.2011.09.002. [DOI] [Google Scholar]
- 93.Xiao YC, Lei J, Liu M, Yu M, Ran J, Xie J, Li W, Huang J. Three new bisabolocurcumin ethers from the rhizomes of Curcuma longa L. Helv Chim Acta. 2012;95(2):327–332. doi: 10.1002/hlca.201100273. [DOI] [Google Scholar]
- 94.Tang Y, Chen A. Curcumin prevents leptin raising glucose levels in hepatic stellate cells by blocking translocation of glucose transporter-4 and increasing glucokinase. Br J Pharmacol. 2010;161(5):1137–1149. doi: 10.1111/j.1476-5381.2010.00956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang D, Zhang Y, Ye M, Ding Y, Tang Z, Li M, Zhou Y, Wang C. Interference with Akt signaling pathway contributes curcumin-induced adipocyte insulin resistance. Mol Cell Endocrinol. 2016;429:1–9. doi: 10.1016/j.mce.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 96.Gunnink LK, Alabi OD, Kuiper BD, Gunnink SM, Schuiteman SJ, Strohbehn LE, Hamilton KE, Wrobel KE, Louters LL. Curcumin directly inhibits the transport activity of GLUT1. Biochimie. 2016;125:179–185. doi: 10.1016/j.biochi.2016.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lekshmi PC, Arimboor R, Nisha VM, Menon AN, Raghu KG. In vitro antidiabetic and inhibitory potential of turmeric (Curcuma longa L) rhizome against cellular and LDL oxidation and angiotensin converting enzyme. J Food Sci Technol. 2014;51(12):3910–3917. doi: 10.1007/s13197-013-0953-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ponnusamy S, Zinjarde S, Bhargava S, Rajamohanan PR, RaviKumar A. Discovering bisdemethoxycurcumin from Curcuma longa rhizome as a potent small molecule inhibitor of human pancreatic α-amylase, a target for type-2 diabetes. Food Chem. 2012;135(4):2638–2642. doi: 10.1016/j.foodchem.2012.06.110. [DOI] [PubMed] [Google Scholar]
- 99.Lekshmi PC, Arimboor R, Indulekha PS, Menon AN. Turmeric (Curcuma longa L.) volatile oil inhibits key enzymes linked to type 2 diabetes. Int J Food Sci Nutr. 2012;63(7):832–834. doi: 10.3109/09637486.2011.607156. [DOI] [PubMed] [Google Scholar]
- 100.Ramkissoon JS, Mahomoodally MF, Ahmed N, Subratty AH. Antioxidant and anti-glycation activities correlates with phenolic composition of tropical medicinal herbs. Asian Pac J Trop Med. 2013;6(7):561–569. doi: 10.1016/S1995-7645(13)60097-8. [DOI] [PubMed] [Google Scholar]
- 101.Kuroda M, Mimaki Y, Nishiyama T, Mae T, Kishida H, Tsukagawa M, Takahashi K, Kawada T, Nakagawa K, Kitahara M. Hypoglycemic effects of turmeric (Curcuma longa L. rhizomes) on genetically diabetic KK-Ay mice. Biol Pharm Bull. 2005;28(5):937–939. doi: 10.1248/bpb.28.937. [DOI] [PubMed] [Google Scholar]
- 102.Nishiyama T, Mae T, Kishida H, Tsukagawa M, Mimaki Y, Kuroda M, Sashida Y, Takahashi K, Kawada T, Nakagawa K, Kitahara M. Curcuminoids and sesquiterpenoids in turmeric (Curcuma longa L.) suppress an increase in blood glucose level in type 2 diabetic KK-Ay mice. J Agric Food Chem. 2005;53(4):959–963. doi: 10.1021/jf0483873. [DOI] [PubMed] [Google Scholar]
- 103.Mustafa SB, Akram M, Muhammad Asif H, Qayyum I, Hashmi AM, Munir N, Khan FS, Riaz M, Ahmad S. Antihyperglycemic activity of hydroalcoholic extracts of selective medicinal plants Curcuma longa, Lavandula stoechas, Aegle marmelos, and Glycyrrhiza glabra and their polyherbal preparation in alloxan-induced diabetic mice. Dose-Response. 2019 doi: 10.1177/1559325819852503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jiménez-Flores LM, López-Briones S, Macías-Cervantes MH, Ramírez-Emiliano J, Pérez-Vázquez V. A PPARγ, NF-κB and AMPK-dependent mechanism may be involved in the beneficial effects of curcumin in the diabetic db/db mice liver. Molecules. 2014;19(6):8289–8302. doi: 10.3390/molecules19068289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen Y, Cruzat VF, Newsholme P. Chapter 3—β-cell metabolism, insulin production and secretion: metabolic failure resulting in diabetes. In: Mauricio D, editor. Molecular nutrition and diabetes. San Diego: Academic Press; 2016. pp. 29–40. [Google Scholar]
- 106.Zhao X, Xiaoli ZH, Abdulla A, Yang EST, Wang Q, Ji J-Y, Pessin JE, Das BC, Yang F. Inhibition of SREBP transcriptional activity by a boron-containing compound improves lipid homeostasis in diet-induced obesity. Diabetes. 2014;63(7):2464–2473. doi: 10.2337/db13-0835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ding L, Li J, Song B, Xiao X, Zhang B, Qi M, Huang W, Yang L, Wang Z. Curcumin rescues high fat diet-induced obesity and insulin sensitivity in mice through regulating SREBP pathway. Toxicol Appl Pharmacol. 2016;304:99–109. doi: 10.1016/j.taap.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 108.Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5–6):231–237. doi: 10.1242/dmm.001180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Amin F, Islam N, Anila N, Gilani AH. Clinical efficacy of the co-administration of turmeric and black seeds (kalongi) in metabolic syndrome—a double blind randomized controlled trial—TAK-MetS trial. Complement Ther Med. 2015;23(2):165–174. doi: 10.1016/j.ctim.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 110.Safarian H, Parizadeh SMR, Saberi-Karimain M, Darroudi S, Javandoost A, Mohammadi F, Moammeri M, Ferns GA, Ghayour-Mobarhan M, Mohebati M. The effect of curcumin on serum copper and zinc and Zn/Cu ratio in individuals with metabolic syndrome: a double-blind clinical trial. J Diet Suppl. 2019;16(6):625–634. doi: 10.1080/19390211.2018.1472711. [DOI] [PubMed] [Google Scholar]
- 111.Panahi Y, Hosseini MS, Khalili N, Naimi E, Majeed M, Sahebkar A. Antioxidant and anti-inflammatory effects of curcuminoid-piperine combination in subjects with metabolic syndrome: a randomized controlled trial and an updated meta-analysis. Clin Nutr. 2015;34(6):1101–1108. doi: 10.1016/j.clnu.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 112.Adab Z, Eghtesadi S, Vafa M-R, Heydari I, Shojaii A, Haqqani H, Arablou T, Eghtesadi M. Effect of turmeric on glycemic status, lipid profile, hs-CRP, and total antioxidant capacity in hyperlipidemic type 2 diabetes mellitus patients. Phytother Res. 2019;33(4):1173–1181. doi: 10.1002/ptr.6312. [DOI] [PubMed] [Google Scholar]
- 113.Adibian M, Hodaei H, Nikpayam O, Sohrab G, Hekmatdoost A, Hedayati M. The effects of curcumin supplementation on high-sensitivity C-reactive protein, serum adiponectin, and lipid profile in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trial. Phytother Res. 2019;33(5):1374–1383. doi: 10.1002/ptr.6328. [DOI] [PubMed] [Google Scholar]
- 114.Panahi Y, Khalili N, Sahebi E, Namazi S, Reiner Ž, Majeed M, Sahebkar A. Curcuminoids modify lipid profile in type 2 diabetes mellitus: a randomized controlled trial. Complement Ther Med. 2017;33:1–5. doi: 10.1016/j.ctim.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 115.Mousavi SM, Milajerdi A, Varkaneh HK, Gorjipour MM, Esmaillzadeh A. The effects of curcumin supplementation on body weight, body mass index and waist circumference: a systematic review and dose-response meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2020;60(1):171–180. doi: 10.1080/10408398.2018.1517724. [DOI] [PubMed] [Google Scholar]
- 116.Banez MJ, Geluz MI, Chandra A, Hamdan T, Biswas OS, Bryan NS, Von Schwarz ER. A systemic review on the antioxidant and anti-inflammatory effects of resveratrol, curcumin, and dietary nitric oxide supplementation on human cardiovascular health. Nutr Res. 2020;78:11–26. doi: 10.1016/j.nutres.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 117.Li H, Sureda A, Devkota HP, Pittalà V, Barreca D, Silva AS, Tewari D, Xu S, Nabavi SM. Curcumin, the golden spice in treating cardiovascular diseases. Biotechnol Adv. 2020;38:107343. doi: 10.1016/j.biotechadv.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 118.Qin S, Huang L, Gong J, Shen S, Huang J, Ren H, Hu H. Efficacy and safety of turmeric and curcumin in lowering blood lipid levels in patients with cardiovascular risk factors: a meta-analysis of randomized controlled trials. Nutr J. 2017;16(1):68. doi: 10.1186/s12937-017-0293-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sahebkar A. Are curcuminoids effective c-reactive protein-lowering agents in clinical practice? Evidence from a meta-analysis. Phytother Res. 2014;28(5):633–642. doi: 10.1002/ptr.5045. [DOI] [PubMed] [Google Scholar]
- 120.Patel SS, Acharya A, Ray RS, Agrawal R, Raghuwanshi R, Jain P. Cellular and molecular mechanisms of curcumin in prevention and treatment of disease. Crit Rev Food Sci Nutr. 2020;60(6):887–939. doi: 10.1080/10408398.2018.1552244. [DOI] [PubMed] [Google Scholar]
- 121.Dou X, Fan C, Wo L, Yan J, Qian Y, Wo X. Curcumin up-regulates LDL receptor expression via the sterol regulatory element pathway in HepG2 cells. Planta Med. 2008;74(11):1374–1379. doi: 10.1055/s-2008-1081316. [DOI] [PubMed] [Google Scholar]
- 122.Fan C, Wo X, Qian Y, Yin J, Gao L. Effect of curcumin on the expression of LDL receptor in mouse macrophages. J Ethnopharmacol. 2006;105(1):251–254. doi: 10.1016/j.jep.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 123.Coban D, Milenkovic D, Chanet A, Khallou-Laschet J, Sabbe L, Palagani A, Berghe WV, Mazur A, Morand C. Dietary curcumin inhibits atherosclerosis by affecting the expression of genes involved in leukocyte adhesion and transendothelial migration. Mol Nutr Food Res. 2012;56(8):1270–1281. doi: 10.1002/mnfr.201100818. [DOI] [PubMed] [Google Scholar]
- 124.Galkina E, Ley K. Vascular adhesion molecules in atherosclerosis. Arterioscler Thromb Vasc Biol. 2007;27(11):2292–2301. doi: 10.1161/ATVBAHA.107.149179. [DOI] [PubMed] [Google Scholar]
- 125.Zingg J-M, Hasan ST, Cowan D, Ricciarelli R, Azzi A, Meydani M. Regulatory effects of curcumin on lipid accumulation in monocytes/macrophages. J Cell Biochem. 2012;113(3):833–840. doi: 10.1002/jcb.23411. [DOI] [PubMed] [Google Scholar]
- 126.Chuengsamarn S, Rattanamongkolgul S, Phonrat B, Tungtrongchitr R, Jirawatnotai S. Reduction of atherogenic risk in patients with type 2 diabetes by curcuminoid extract: a randomized controlled trial. J Nutr Biochem. 2014;25(2):144–150. doi: 10.1016/j.jnutbio.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 127.Hong D, Zeng X, Xu W, Ma J, Tong Y, Chen Y. Altered profiles of gene expression in curcumin-treated rats with experimentally induced myocardial infarction. Pharmacol Res. 2010;61(2):142–148. doi: 10.1016/j.phrs.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 128.Lv F-H, Yin H-L, He Y-Q, Wu H-M, Kong J, Chai X-Y, Zhang S-R. Effects of curcumin on the apoptosis of cardiomyocytes and the expression of NF-κB, PPAR-γ and Bcl-2 in rats with myocardial infarction injury. Exp Ther Med. 2016;12(6):3877–3884. doi: 10.3892/etm.2016.3858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Geng H-H, Li R, Su Y-M, Xiao J, Pan M, Cai X-X, Ji X-P. The circular RNA Cdr1as promotes myocardial infarction by mediating the regulation of miR-7a on its target genes expression. PLoS ONE. 2016;11(3):e0151753. doi: 10.1371/journal.pone.0151753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kim YS, Kwon JS, Cho YK, Jeong MH, Cho JG, Park JC, Kang JC, Ahn Y. Curcumin reduces the cardiac ischemia–reperfusion injury: involvement of the toll-like receptor 2 in cardiomyocytes. J Nutr Biochem. 2012;23(11):1514–1523. doi: 10.1016/j.jnutbio.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 131.Boyd JH, Mathur S, Wang Y, Bateman RM, Walley KR. Toll-like receptor stimulation in cardiomyoctes decreases contractility and initiates an NF-κB dependent inflammatory response. Cardiovasc Res. 2006;72(3):384–393. doi: 10.1016/j.cardiores.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 132.Zhu X, Bagchi A, Zhao H, Kirschning CJ, Hajjar RJ, Chao W, Hellman J, Schmidt U. Toll-like receptor 2 activation by bacterial peptidoglycan-associated lipoprotein activates cardiomyocyte inflammation and contractile dysfunction. Crit Care Med. 2007;35(3):886–892. doi: 10.1097/01.CCM.0000256723.37586.A2. [DOI] [PubMed] [Google Scholar]
- 133.Xiao J, Sheng X, Zhang X, Guo M, Ji X. Curcumin protects against myocardial infarction-induced cardiac fibrosis via SIRT1 activation in vivo and in vitro. Drug Des Dev Ther. 2016;10:1267–1277. doi: 10.2147/DDDT.S104925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Samak M, Fatullayev J, Sabashnikov A, Zeriouh M, Schmack B, Farag M, Popov A-F, Dohmen PM, Choi Y-H, Wahlers T, Weymann A. Cardiac hypertrophy: an introduction to molecular and cellular basis. Med Sci Monit Basic Res. 2016;22:75–79. doi: 10.12659/MSMBR.900437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sunagawa Y, Funamoto M, Sono S, Shimizu K, Shimizu S, Genpei M, Miyazaki Y, Katanasaka Y, Morimoto E, Ueno M, Komiyama M, Kakeya H, Wada H, Hasegawa K, Morimoto T. Curcumin and its demethoxy derivatives possess p300 HAT inhibitory activity and suppress hypertrophic responses in cardiomyocytes. J Pharmacol Sci. 2018;136(4):212–217. doi: 10.1016/j.jphs.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 136.Morimoto T, Sunagawa Y, Kawamura T, Takaya T, Wada H, Nagasawa A, Komeda M, Fujita M, Shimatsu A, Kita T, Hasegawa K. The dietary compound curcumin inhibits p300 histone acetyltransferase activity and prevents heart failure in rats. J Clin Investig. 2008;118(3):868–878. doi: 10.1172/JCI33160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ahuja S, Kohli S, Krishnan S, Dogra D, Sharma D, Rani V. Curcumin: a potential therapeutic polyphenol, prevents noradrenaline-induced hypertrophy in rat cardiac myocytes. J Pharm Pharmacol. 2011;63(12):1604–1612. doi: 10.1111/j.2042-7158.2011.01363.x. [DOI] [PubMed] [Google Scholar]
- 138.Mohammadi F, Ghazi-Moradi M, Ghayour-Mobarhan M, Esmaeili H, Moohebati M, Saberi-Karimian M, Safarian H, Tavallaie S, Ferns GA, Sahebkar A. The effects of curcumin on serum heat shock protein 27 antibody titers in patients with metabolic syndrome. J Diet Suppl. 2019;16(5):592–601. doi: 10.1080/19390211.2018.1472710. [DOI] [PubMed] [Google Scholar]