Abstract
Introduction
Spinal tuberculosis is a chronic destructive disease with long-term morbidity. Patients are usually young especially from a poor socioeconomic background. Destruction of the intervertebral disk space and the adjacent vertebral bodies is the characteristic lesion. The dorsal spine is the most affected region with multi-level noncontiguous involvement being detected more frequently. Patients usually present with chronic back pain associated with spinal tenderness, paraplegia, spinal deformities, as well as with constitutional symptoms. Magnetic resonance imaging has proved to be more sensitive and specific for its diagnosis, but availability and affordability of this investigation remain a problem in developing countries. Anti-tuberculous drug therapy has revolutionized the treatment of this debilitating disease. Surgery is still required in selected cases especially with evolving neurological deficit, progressive deformity, intractable pain and lack of response to drug therapy. With early diagnosis and effective treatment, prognosis is generally good.
Materials/Methods: After getting permission from the clinical governance department, We collected the retrospective data of 305 patients with diagnosed spinal tuberculosis, who underwent surgical intervention.
Results
There was no significant difference in incidence among males and females. Housewives were the most affected. Lower dorsal spinal was the commonest site involved but our study didn't confirm the incidence of multi-level disease process. Anterior decompression along with Cage fixation was most frequently performed procedure.
Conclusion
Despite the availability of highly effective antituberculous drugs, advanced surgical procedure, the spinal tuberculosis still maintains its demographic profile. There has been no change in characteristics of spinal presentation of this chronic debilitating disease. Patients continue to suffer the same way as they were suffering decades ago.
Keywords: Spinal tuberculosis, Pott's disease, Cage fixation, Antituberculous drugs, Anterior decompression
Highlights
-
•
Spinal tuberculosis is a chronic destructive disease with long-term morbidity.
-
•
The dorsal spine is the most affected region with multi-level involvement being detected.
-
•
Analysis of data of 305 patients with diagnosed spinal tuberculosis, who underwent surgical intervention.
-
•
Despite the availability of highly effective drugs, and surgical procedure, the spinal tuberculosis still maintains its demographic profile.
-
•
There has been no change in characteristics of spinal presentation of this chronic debilitating disease.
1. Introduction
Spinal involvement in tuberculosis is a frequently extrapulmonary manifestation of the disease. In developing nations, the incidence of spinal tuberculosis is high mainly because of poverty, unhygienic living conditions and poor access to good quality healthcare. Resurgence in all forms of tuberculosis, including spinal tuberculosis, has been observed because of the recent increase in acquired immunodeficiency caused by human immunodeficiency virus. (see Table 1, Table 2, Table 3, Table 4, Table 5)
Table 1.
Patients socio-demographic characteristics (N = 305).
| Variable | Frequency (N) | Percent (%) |
|---|---|---|
| Gender | ||
| Male | 168 | 55.1 |
| Female | 137 | 44.9 |
| Age Group | ||
| <16 | 34 | 11.1 |
| 16–30 | 85 | 27.9 |
| 31–45 | 83 | 27.2 |
| 45–60 | 65 | 21.3 |
| >60 | 38 | 12.5 |
| Job Type | ||
| Student | 79 | 25.9 |
| Housewife | 97 | 31.8 |
| Office Worker | 10 | 3.3 |
| Laborer | 47 | 15.4 |
| Shopkeeper | 38 | 12.5 |
| Retired | 21 | 6.9 |
| Teacher | 13 | 4.3 |
| Residence | ||
| Urban | 34 | 11.1 |
| Rural | 271 | 88.9 |
| Socioeconomic Class | ||
| Lower | 244 | 80.0 |
| Middle | 61 | 20.0 |
| High | 0 | 0.0 |
Table 2.
Primary complains/symptoms of tuberculosis (N = 305).
| Symptoms | Yes (%) | No (%) |
|---|---|---|
| Lower Back Pain | 302 (99) | 3 (1) |
| Weight Loss | 295 (96.7) | 10 (3.3) |
| Appetite Loss | 289 (94.8) | 16 (5.2) |
| Fever | 176 (57.7) | 129 (42.3) |
| Neck Pain | 2 (0.7) | 303 (99.3) |
| Lower Limb Weakness | 2 (0.7) | 303 (99.3) |
| Upper Limb Weakness | 2 (0.7) | 303 (99.3) |
| Deformity | 3 (1) | 302 (99) |
Table 3.
Diagnosis and treatment for Skeletal Tuberculosis in Patients.
| Variable | Frequency (N) | Percent (%) | |
|---|---|---|---|
| Duration of Symptoms | |||
| <6 months | 70 | 23 | |
| 6–12 months | 231 | 75.7 | |
| >12 months | 4 | 1.3 | |
| Duration of Treatments | |||
| <3 months | 1 | 0.3 | |
| 3–6 months | 3 | 1.0 | |
| 6–12 months | 300 | 98.4 | |
| >12 months | 1 | 0.3 | |
| How Diagnosis made | |||
| Radiographs | 147 | 48.2 | |
| MRI | 158 | 51.8 | |
| Fixation Level | |||
| Cervical | 13 | 4.3 | |
| Upper Dorsal | 36 | 11.8 | |
| Lower Dorsal | 128 | 42.0 | |
| Dorsolumbar Junction | 29 | 9.5 | |
| Lumbar | 93 | 30.5 | |
| Lumbosacral Junction | 6 | 2.0 | |
| Fused Segments | |||
| 1 segment | 264 | 86.6 | |
| 2-3 segment | 36 | 11.8 | |
| >3 segment | 5 | 1.6 | |
| Treatment | Yes (%) | No (%) | |
| Cage Fixation | 280 (91.8) | 25 (8.2) | |
| Anterior Decompression | 201 (65.9) | 104 (34.1) | |
| Pedicular Screw Fixation | 22 (7.2) | 283 (92.8) | |
| Posterior Fusion | 6 (2) | 299 (98) | |
Table 4.
Bivariate analysis.
| Job | Socioeconomic Class |
||
|---|---|---|---|
| Lower | Middle | P value | |
| Student | 58 (19) | 21 (6.9) | 0.00* |
| Housewife | 85 (27.9) | 12 (3.9) | |
| Office Worker | 1 (0.3) | 9 (3) | |
| Laborer | 47 (15.4) | 0 (0) | |
| Shopkeeper | 33 (10.8) | 5 (1.6) | |
| Retired | 7 (2.3) | 14 (4.6) | |
| Teacher | 13 (4.3) | 0 (0) | |
Table 5.
Level of disease.
| Age Groups | Fixation Level |
||||||
|---|---|---|---|---|---|---|---|
| Cervical | Upper Dorsal | Lower Dorsal | Dorsolumbar Junction | Lumbar | Lumbosacral Junction | P value | |
| <16 | 2 (0.7) | 8 (2.6) | 12 (3.9) | 2 (0.7) | 10 (3.3) | 0 (0) | 0.373 |
| 16–30 | 4 (1.3) | 7 (2.3) | 37 (12.1) | 8 (2.6) | 28 (9.2) | 1 (0.3) | |
| 31–45 | 5 (1.6) | 6 (2) | 36 (11.8) | 8 (2.6) | 27 (8.9) | 1 (0.3) | |
| 45–60 | 0 (0) | 9 (3) | 31 (10.2) | 4 (1.3) | 18 (5.9) | 3 (1) | |
| >60 | 2 (0.7) | 6 (2) | 12 (3.9) | 7 (2.3) | 10 (3.3) | 1 (0.3) | |
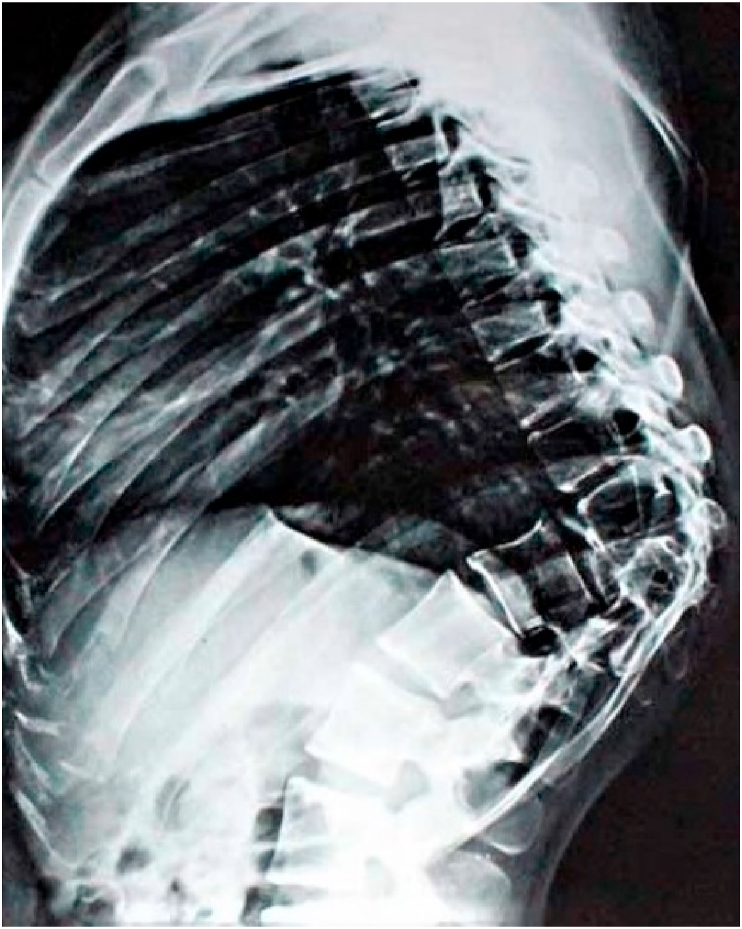
Spinal tuberculosis is chronic debilitating disease with long term morbidity yet there are no straightforward guidelines for the diagnosis and treatment. Neurological compromise and spinal deformity (Fig. 1 & Fig. 2) are main complications of no treatment. To prevent the development of permanent neurological disability and to minimize the spinal deformity, early diagnosis and prompt treatment is necessary [1,2].
Fig. 1.
Patient with tubercolosis of thoracic spine.
Fig. 2.
Patient with deformity due to tubercolosis thoracic spine.
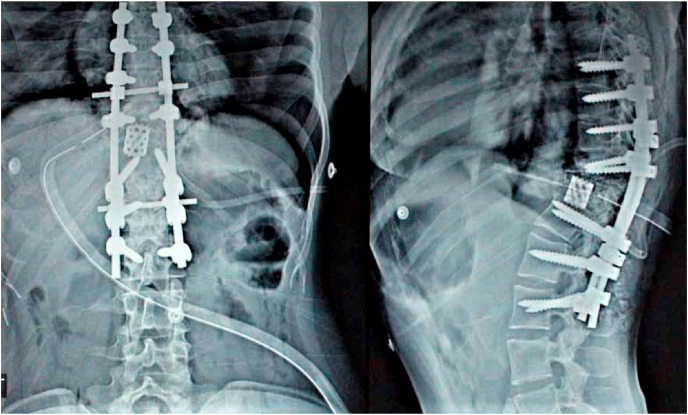
The development of multidrug resistance in Mycobacterium Tuberculosis, increased incidence of immunodeficient patients with tuberculosis, availability of advanced imaging modalities (Fig. 3, Fig. 4) and development of specialized spinal reconstructive techniques (Fig. 5) have all changed the management of this disease [3].
Fig. 3.
X ray showing tubercolosis of thoracic spine.
Fig. 4.
X ray showing tubercolosis of thoracic spine.
Fig. 5.
Screw+ cage fixation thoracic spine+ lumbar spine post therapy.
In Pakistan, the incidence of immunodeficiency, especially in children, caused by human immunodeficiency virus is on the rise [4]. New multidrug resistant strains of mycobacterium have also been detected in our country [5]. Both factors have sparked a flurry of activity towards the prevention and treatment of this disease [6].
Methods of diagnosis and quality of treatment have shown great advances in recent years, but tuberculosis remains a global public health problem. According to World Health Organization, “the disease burden of tuberculosis is falling globally but not fast enough” and around 10 million people developed clinical symptomatic tuberculosis in 2017 [7].
Pakistan, being a developing country with slow economic growth programs for prevention and control of tuberculosis started late.
A lot of research publication [8,9], local as well as international, about tuberculosis are available but there are few studies with large number of patients suffering from spinal tuberculosis and its management. That's why the level of spine affected by this disease and trend of surgical management are not clear.
The main purpose of our study is to give insight and literature to better provide antituberculosis therapy and further understand the epidemiological characteristics, diagnosis, and status of spinal level of disease and treatment of spinal tuberculosis in our region of world at this moment. Spinal tuberculosis has been reported in published literature to involve lower dorsal and upper lumbar regions than other portions of the spine [4]. The idea for the study came when surgeons and doctors at 1 spinal center observed that the case presentations and level of pathology was contradicting the research and literature given in most cases. This study intends to retrospectively analyse the clinical data of the patients with spinal tuberculosis in a tertiary care teaching hospital in Lahore, Pakistan.
2. Materials and methods
After noticing a change in current trend of the disease, we discussed the project with clinical governance in our hospital and registered it as a quality improvement project in the trust. After getting access to the data, We retrospectively reviewed patients, who were treated with surgery from January 2020 to June 2020 in a tertiary care teaching hospital in Pakistan, to see the exact level of pathology and compare it with given literature and figures to see if the disease is following trend or not. Variables kept for the study were age, gender, job, residence socioeconomic class, duration of symptoms, primary site, how diagnosis was made, medical therapy and definitive management. All patients, who were managed conservatively, were excluded. Patient notes and radiology were reviewed to calculate variables and patient sensitive data was omitted. All data was recorded in Microsoft excel sheets and analyzed via IBM SPSS® (v.25).
3. Results
3.1. Demographic
In present study, 305 patients were evaluated and 302 were diagnosed with skeletal TB of which 168 (55.1%) are male and 137 (44.9%) female patients. Majority of the patients (27.9%) were 16–30 years old and (31.8%) are housewives. In addition, 89% patients suffering from skeletal TB were from rural area and (80%) of them belong to lower socioeconomic class.
3.2. Presenting complaints
Majority of patients (90%) had reported primary complains or symptoms of lower back pain, weight loss and appetite loss and (57.7%) had fever symptom and no significant number of patients had shown symptoms of neck pain, lower limb weakness, upper limb weakness and deformity.
3.3. Diagnosis and treatment
Maximum duration of illness or symptoms of TB in 231 (75%) patients lasts for 6–12 months and 300 (98%) patients had gone through 6–12 months of treatment. To determine the spread of the disease, diagnosis was performed by MRI of 158 patients and radiographs of 147 patients. Fixation was done on lower dorsal in 128 (42%) patients and on Lumbar in 93 (30%) patients. The development of skeletal TB was 264 (86.6%) for one fused segment. Most of the patients underwent cage fixation in 280 (91.8%) and anterior decompression in 201 (65.9%).
3.4. Socioeconomic status
In bivariate analysis, Job type and socioeconomic class are statistically significant at p value of 0.00 (<0.05). According to this study, highest number of skeletal TB cases 85 (27.9%) are in housewives and they belong to lower socioeconomic class. After housewives, prevalence of skeletal tuberculosis cases is in students (58, 19%) and laborers (47, 15.4%)
3.5. Level of disease
Maximum Fixation done on lower Dorsal in 37 (12.1%) patients who were from age group of 16–30 years and 36 (11.8%) were from 31 to 45 years. Fixation on Lumbar in 28 (9.2%) patients were from 16 to 30 years of age group and 27 (8.9%) were from 31 to 45 years.
4. Discussion
Percival Pott described the spinal involvement in tuberculosis in 1782, and this presentation of the disease still holds his name [10]. It accounts for almost 50% of the cases of skeletal tuberculosis [11]. It mostly involves dorsal and lumbar spine as a whole and is one of the leading causes of spinal deformity and paralysis [12].
Being the most common form of skeletal involvement, spinal tuberculosis follows the same increasing trend in incidence as is the tuberculosis trend overall [13].
In accordance with many studies [14], the largest number of patients in our study were the 16–30 years old (27.9%). At the time of diagnosis, 12.5% of our patients were older than 60 years.
Like pulmonary tuberculosis, spinal involvement is also chronic and slowly progressive disease. But unlike pulmonary tuberculosis, spinal disease has different symptoms profile. It is not usually accompanied by symptoms such as productive cough, fever, weight loss or night sweats. That's why it's very easy to be misdiagnosed as compared to its pulmonary counterpart.
Similar to other studies (3), back pain was the most common presenting symptom, followed by weight loss with limb weakness being the least common symptom.
Early diagnosis is of paramount importance for prevention of possible complications as it allows rapid therapeutic interventions. Disk space narrowing and vertebral body endplate destruction are the most common initial radiological findings, however these changes are hard to detect on plain radiographs especially in the earlier stages of disease. That formed the bases of MRI scans in 51.8% of our patients. Like other studies [9,15], the dorsal (58.1%) and lumbar spines (42%) were the spinal segments most affected.
The management of spinal tuberculosis consists of supportive care, drugs in the form of antituberculous chemotherapy, and surgical intervention. Antituberculous chemotherapy remains the mainstay of therapy throughout the treatment process of the disease for a duration of 6–9 months [16].
Compliance to therapy is a big problem because of long duration of therapy and serious adverse reaction to drugs. This has resulted in emergence of multi drug resistant strains [17]. Also, chemotherapy alone, can't correct the anatomical deformity caused by bony destruction. That's why, Surgical intervention still holds an important role the management of spinal tuberculosis. At the same time, surgery cannot be assumed to work as sole treatment modality. Therefore, antituberculous chemotherapy and surgical intervention work symbiotically, as adequate antitubercular chemotherapy combined with surgical treatment is important to save the spinal cord function and avoid neurological dysfunction.
Surgical debridement provides local control of disease, decompresses the spinal cord and nerves, corrects deformity, and reshapes the stability of involved spinal segment [18].
Advanced surgical techniques including anterior, posterior, and combined approaches and fixation with cage or pedicular screws have revolutionized the surgical correction of spinal alignment and sagittal and coronal balance [19,20]. Surgery is most commonly performed for intractable pain, progressive neurological compromise and deformity, and ineffective antituberculous chemotherapy. Our patient population also underwent surgical intervention for these same indications.
5. Conclusion
Despite changing time and availability of highly effective antituberculous chemotherapy and advancement in surgical modalities, spinal tuberculosis still maintains its demographic profile in terms of population distribution as well as involvement of spinal segment level. Spine is still the most favorite site of skeletal manifestation of this centuries old debilitating disease. More research is needed to detect factors responsible for persistent prevalence of spinal tuberculosis to device the strategic plan for reduction in incidence of this disease.
Please state any conflicts of interest
Nil
Please state any sources of funding for your research
Nil
Conflict of interest
There are no conflict of interests for this study amongst authors or any organization.
Ethical approval
Retrospective study looking at patient notes so no ethical approval needed.
Sources of funding
Nil.
Author statement
Mr Mohammad Noah H Khsn: lead author idea and write up.
Dr Abdul Basit Jamal: data analysis and collection.
Dr Auzair Hafeez: Data collection.
Marium Sadiq: data analysis.
Dr Umar Rasool: proof reading and corrections of statistics.
Registration of research studies
Name of the registry:
Unique Identifying number or registration ID:
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Mohammad Noah H Khan corresponding author.
Consent
All data anonymised.
Declaration of competing interest
Nil.
Contributor Information
Mohammad Noah Hasan Khan, Email: noah_khan@hotmail.com.
Abdul Basit Jamal, Email: dr.basit@live.com.
Auzair Hafeez, Email: Auzair.hafeez964@gmail.com.
Marium Sadiq, Email: mariumsadiq1319@gmail.com.
Muhammad Umer Rasool, Email: muhammadumerrasool90@gmail.com.
References
- 1.Jain A.K., Dhammi I.K. Tuberculosis of the spine: a review. Clin. Orthop. 2007;460:39–49. doi: 10.1097/BLO.0b013e318065b7c3. Jul. [DOI] [PubMed] [Google Scholar]
- 2.Jain A.K. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br. 2010;92(7):905–913. doi: 10.1302/0301-620X.92B7.24668. Jul. [DOI] [PubMed] [Google Scholar]
- 3.Turgut M. Spinal tuberculosis (Pott's disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg. Rev. 2001;24(1):8–13. doi: 10.1007/pl00011973. Mar. [DOI] [PubMed] [Google Scholar]
- 4.WHO | HIV cases–Pakistan [internet]. WHO. World health organization; [cited 2021 Mar 30]. Available from: http://www.who.int/csr/don/03-july-2019-hiv-cases-pakistan/en/.
- 5.Hasan R., Jabeen K., Ali A., Rafiq Y., Laiq R., Malik B. Extensively drug-resistant tuberculosis, Pakistan. Emerg. Infect. Dis. 2010;16(9):1473–1475. doi: 10.3201/eid1609.100280. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang J., Zhang H., Zeng K., Gao Q. The clinical outcomes of surgical treatment of noncontiguous spinal tuberculosis: a retrospective study in 23 cases. PloS One. 2014;9(4) doi: 10.1371/journal.pone.0093648. Apr 3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Organization WH. Global tuberculosis report 2018 [internet]. World health organization. 2018. https://apps.who.int/iris/handle/10665/274453 [cited 2021 Mar 30]. Available from:
- 8.Schlesinger N., Lardizabal A., Rao J., Rao J., McDonald R. Tuberculosis of the spine: experience in an inner city hospital. JCR J Clin Rheumatol. 2005;11(1):17–20. doi: 10.1097/01.rhu.0000152144.91206.0c. Feb. [DOI] [PubMed] [Google Scholar]
- 9.Wang H., Li C., Wang J., Zhang Z., Zhou Y. Characteristics of patients with spinal tuberculosis: seven-year experience of a teaching hospital in Southwest China. Int. Orthop. 2012;36(7):1429–1434. doi: 10.1007/s00264-012-1511-z. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gorse G.J., Pais M.J., Kusske J.A., Cesario T.C. Tuberculous spondylitis: a report OF six cases and a review OF the literature. Medicine (Baltim.) 1983;62(3):178. May. [PubMed] [Google Scholar]
- 11.Moon M.-S., Kim S.-S., Moon H.-L., Kim D.-H. Mycobacterium tuberculosis in spinal tuberculosis. Asian Spine J. 2017;11(1):138–149. doi: 10.4184/asj.2017.11.1.138. Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung W.Y., Luk K.D.K. Clinical and radiological outcomes after conservative treatment of TB spondylitis: is the 15 years' follow-up in the MRC study long enough? Eur. Spine J. 2013;22(4):594–602. doi: 10.1007/s00586-012-2332-x. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trecarichi E., Meco E., Mazzotta V., Fantoni M. Tuberculous spondylodiscitis: epidemiology, clinical features, treatment, and outcome. Eur. Rev. Med. Pharmacol. Sci. 2012;(16 Suppl 2):58–72. Apr 1. [PubMed] [Google Scholar]
- 14.Shi T., Zhang Z., Dai F., Zhou Q., He Q., Luo F. Retrospective study of 967 patients with spinal tuberculosis. Orthopedics. 2016;39(5):e838–e843. doi: 10.3928/01477447-20160509-03. Sep. 1. [DOI] [PubMed] [Google Scholar]
- 15.Danchaivijitr N., Temram S., Thepmongkhol K., Chiewvit P. Diagnostic accuracy of MR imaging in tuberculous spondylitis. J. Med. Assoc. Thai. 2007;90(8):1581. Aug 1. [PubMed] [Google Scholar]
- 16.Jiang T., Zhao J., He M., Wang K., Fowdur M., Wu Y. Outcomes and treatment of lumbosacral spinal tuberculosis: a retrospective study of 53 patients. Cardona P.-J., editor. PloS One. 2015;10(6) doi: 10.1371/journal.pone.0130185. Jun 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jain A.K., Jaggi K.R., Bhayana H., Saha R. Drug-resistant spinal tuberculosis. Indian J. Orthop. 2018;52(2):100–107. doi: 10.4103/ortho.IJOrtho_306_17. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karaeminogullari O., Aydinli U., Ozerdemoglu R., Ozturk C. Tuberculosis of the lumbar spine: outcomes after combined treatment of two-drug therapy and surgery. Orthopedics. 2007;30(1):55–59. doi: 10.3928/01477447-20070101-15. Jan. [DOI] [PubMed] [Google Scholar]
- 19.Issack P.S., Boachie-Adjei O. Surgical correction of kyphotic deformity in spinal tuberculosis. Int. Orthop. 2012;36(2):353–357. doi: 10.1007/s00264-011-1292-9. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapoor S., Kapoor S., Agrawal M., Aggarwal P., Jain B.K. Thoracoscopic decompression in Pott's spine and its long-term follow-up. Int. Orthop. 2012;36(2):331–337. doi: 10.1007/s00264-011-1453-x. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]