Abstract
BACKGROUND:
We investigated whether the use of a specially designed visual estimation tool may improve accuracy in quantifying blood volumes related to surface spreading.
METHODS:
A prospective, paired-control, single-blinded experimental study was performed at a medical university. Anesthesiologists and emergency medical personnel estimated various blood volumes on surfaces with varying absorptivity (carpet, towel, polyvinyl chloride, wooden flooring) in an experimental setting. We assessed the sensitivity of training blood volume quantification using a self-designed visual estimation tool by comparing the accuracy of visual blood volume estimations before and after practical training with the tool.
RESULTS:
A total of 352 estimations by 44 participants were evaluated. Accurate estimations improved significantly from pre-training to post-training (P<0.05). The sensitivity of blood volume quantification was 33.0% after training with the visual estimation tool. Estimations did not depend on age, profession, gender or years of the estimator’s professional experience.
CONCLUSIONS:
Training with a visual estimation tool by professional rescuers can improve the estimation accuracy of blood volumes spread on surfaces with varying absorptivity.
Keywords: Academic training, Emergency medicine, Hemorrhage control, Major bleeding
INTRODUCTION
Precise estimation of blood loss has a direct impact on the extent of volume and coagulation therapy as both, and volume overload and delayed volume therapy may be harmful to patients. Appropriate and timely treatment is particularly important when children, very old or sick patients, and obstetric patients are involved.[1-4] However, visual estimation of external blood loss in pre- and in-hospital emergencies based on the assessment of blood puddle areas is difficult and frequently inaccurate independent of experience and qualification of professionals.[3-5] Overestimation of blood loss at low volumes and underestimation of blood loss at high volumes are commonly observed.[6] Quantification of external blood loss may be further hampered by spreading blood on surfaces with various degrees of absorptivity.[6] Dynamics of vital signs and clinical parameters further influence visual estimation and alter quantification of blood loss.[7] Using pictorial nomograms,[5] pictorial guidelines,[8] drapes[4] or one’s fist to determine external blood loss[9] was reported to improve the accuracy of visual estimation.
The objective of this trial is to assess the significance of blood volume quantification after training with a visual estimation tool.
METHODS
A prospective, paired-control, single-blinded experimental study was conducted at the training center of the Medical University of Innsbruck. Anonymized participation of attendees was facilitated by encoding test results. Using convenience sampling technique participation was voluntary and based on the understanding that the results will be published in scientific journals. The experimental study corresponds to the STARD 2015 guidelines for reporting diagnostic accuracy studies.[10]
Study population
Eligible participants from the Department of Anesthesiology and Intensive Care Medicine, Innsbruck Medical University Hospital and from Innsbruck Emergency Medical Service (EMS), Red Cross Tyrol were contacted.
Inclusion criteria were: specialists and specialist trainees in anesthesiology, emergency physicians, emergency technicians, emergency assistants, voluntary participation, and written informed consent.
Exclusion criteria were: incomplete participation during the study phase, and lack of written informed consent.
Study design
On day 1, participants were asked to estimate the volume of blood puddles spread on four different surfaces in the examination room. The investigation was conducted without any previous supply of information to the attendees (pre-training). Then, participants were taught how to estimate the area of spread blood when using the visual estimation tool (training).
On day 2 and day 14 after the initial assessment and training, participants again had to estimate four randomly assigned blood volumes on identical surfaces. In order to assess the training effect, attendees were not allowed to use the visual estimation tool (post-training).
Experimental setting
Human packed red cell concentrates, anticoagulated with citrate phosphate glucose and hematocrit ranging between 33.0% and 42.0%, were poured slowly from 5 cm distance on the test surface. Four different test materials were used: carpet (loop fitted, 8 mm height, 100% polyamide), cotton towel, polyvinyl chloride (PVC) flooring, and wooden flooring (raw spruce board for timber piling). The investigation was performed indoors under dry conditions at room temperature with no wind or air conditioning to counteract the speed of evaporation. Materials were horizontally positioned. Surfaces were brightly colored, without pattern, with no grooves or gaps.
Visual estimation tool and questionnaire
In the current study, training was performed with a self-designed visual estimation tool in the shape of a DIN A4 sheet of paper (Figure 1). The tool can be folded either along the continuous line to provide one and two-thirds of the reference surface or along the dotted line to provide half of the reference surface for comparison of blood puddle sizes. For estimation of circular type blood puddles, the formula for calculation of the area of a circle was provided.
Figure 1.
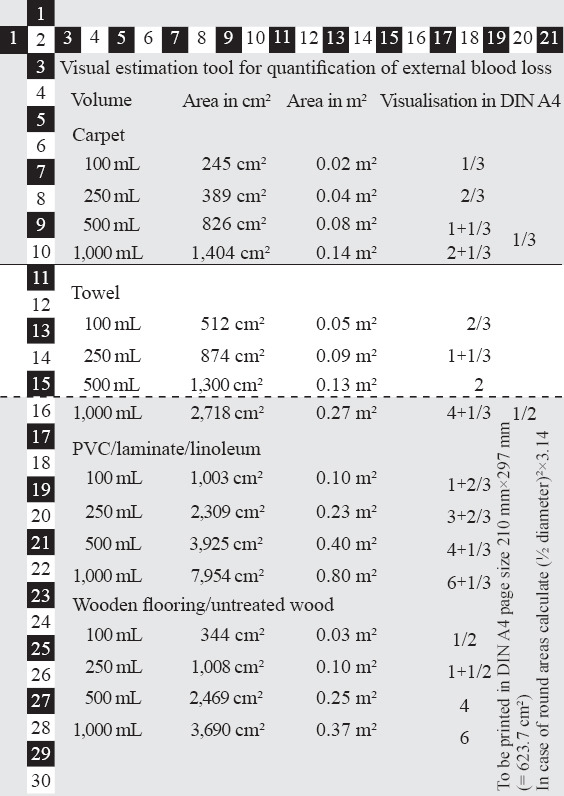
The visual estimation tool modified by converting areas of blood puddles to proportions of the standardized sheet of DIN A4.
For measurement of blood puddle diameters, two tape lines in cm units were perpendicularly arranged on the margins of the tool. Specific information with respect to absorbing properties of four common materials (carpet, towel, wood, PVC) at four common volumes was provided in the center of the tool. The reference surfaces were expressed as proportions of the surface area of a sheet of paper (standard DIN A4: 210 mm×297 mm=623.7 cm²). Areas indicated in this tool were based on results of a previous study,[11] in which the spread of pre-defined blood volumes on the surface of different everyday objects was analyzed.
The questionnaire contained three questions regarding certainty, experience, and need for training in the estimation of external blood loss, and five questions regarding the content, comprehensibility efficiency, complexity, and importance of the training program (each item provided a Likert-type scale with five response levels).
Study endpoints and null hypothesis
The primary study endpoint was to assess the pre- and post-training differences in percent error of estimated blood volume (accurate visual estimation of blood volume) when using the visual estimation tool. The secondary study endpoint was to compare the frequency of accurate visual estimation and various characters including age, profession, gender, and years of professional experience. The null hypothesis of the study was that the detection rate (significance) of actual blood volumes dispersed on different subsoils in an experimental setting does not differ between pre- and post-training.
Statistical analysis
The percent error of estimated blood volume was calculated as ([estimated blood volume–actual blood volume]/actual blood volume×100). Accurate estimation was defined as assessment within a deviation of 20% of actual blood volume. Consequently, overestimation and underestimation were defined as >+20% and <–20% of actual blood volume, respectively. Clinical experience was categorized as 0–5 years, >5–10 years, >10–15 years, or >15 years after graduation from a medical or professional school.
Data were entered into a Microsoft Excel spreadsheet Version 7.0.25 (Microsoft Corporation, Redmond, Washington, USA). Data were not normally distributed as assessed by Shapiro-Wilk test; results were expressed as median and range. The Wilcoxon signed-rank test was used to compare pre- and post-training results. To compare two independent groups, the Mann-Whitney U-test or the Kruskal-Wallis test was used if more than two groups were analyzed. For frequency analysis, Fisher’s exact or the Chi-square test was performed, and correlations were calculated with Spearman’s Rho. The tendency to overestimate or underestimate a series of blood volumes was assessed with the Jonckheere-Terpstra test. The significance level was defined as P<0.05.
RESULTS
Overall, 57 persons responded and participated in the pre-training assessment, but 13 persons did not attend the post-training assessment (inclusion rate 77.2%). Of 44 participants enrolled in the study, 18 (40.9%) were female, 34 (77.3%) were physicians, and 10 (22.7%) were EMS personnel. The median age was 32 years (range 18–56 years), and the median professional experience was six years (range 1–25 years).
Pre-training assessment
On PVC flooring, 28 (63.6%) estimations were exceeding 20% deviation, whereas on wood 27 (61.4%) estimations were below –20% deviation of actual blood volume. On carpet, 39 (88.7%) estimations were below –20% deviation, and on towel 22 (50.0%) estimations were exceeding 20% deviation of actual blood volume (Table 1, Figure 2). There was no association between the estimation results or estimation errors and age, profession, gender, and years of professional experience.
Table 1.
Median estimation and percent error of estimated blood volume from actual blood quantities
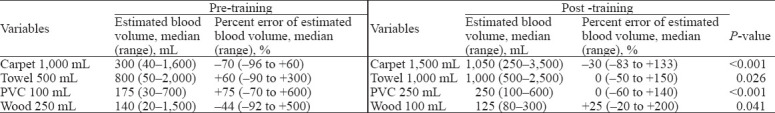
Figure 2.
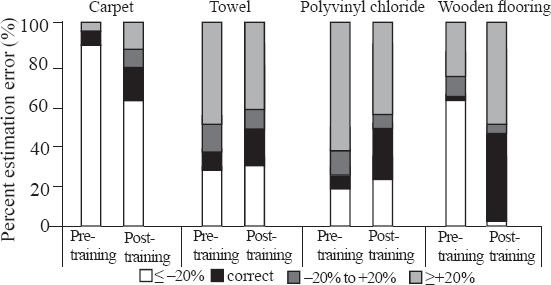
Changes in percent estimation error between pre-training and post-training assessments on various surfaces.
Post-training assessment
After being instructed on the application of the visual estimation tool, the percentage of accurate estimations within 20% deviation rose from 26 of 176 estimations to 58 of 176 estimations (P<0.001). The accuracy of estimation significantly improved regarding all four surfaces tested. Overall significance of blood volume quantification after training with the visual estimation tool was 33.0%. There was no association between the estimation results or estimation errors and age, profession, gender, or years of professional experience.
Questionnaire
Twenty-five (56.8%) participants stated that they had little or very little experience in estimating blood loss and 42 (95.5%) quoted the need to be trained in blood loss estimation. Forty-three (97.7%) participants reported a good to very positive training effect and considered the training content to be comprehensible to very comprehensible. Twenty-three (52.4%) participants reported that they had learned much or very much, and 27 (61.4%) participants ranked the level of difficulty of the training program between low and mean. In sum, 36 (83.7%) participants graded the training program very good or good.
DISCUSSION
The results of our experimental study underline that training with a tool for visual estimation has a lasting effect and may improve the estimation accuracy of blood volumes spread on surfaces with varying absorptivity. Such training has education value for prehospital providers. As emergency cases with blood scattered on various surfaces are rare, even the very experienced emergency physicians and technicians have difficulties in the quantification of external blood losses.[1-4] Estimated volumes differed considerably regardless of age, profession, gender, or years of professional experience during the pre-training assessment. Overestimations of up to about 11 folds (1,500 mL vs. 140 mL) on wood and underestimations of up to 16 folds (50 mL vs. 800 mL) on the towel were observed (Table 1). Interestingly, there were 63.6% overestimations regarding blood on PVC flooring but 61.4% underestimations regarding blood on wood although both materials have minimally absorbent surfaces. Similar, there were 50.0% overestimations regarding blood on the towel but 88.7% underestimations regarding blood on carpet although both materials are highly absorbent. However, it is still a question of debate whether the accuracy of measuring blood loss has direct effects on outcomes.[12]
Majority of participants quoted that the comprehensible training increased their subjective certainty concerning how to estimate external blood loss. There was an impressive training effect in this and in similar studies.[13-15] Pre-hospital assessment of blood loss relies on visual estimation and clinical parameters such as heart rate, blood pressure, capillary refill time, characteristics of the pulse wave in oxygraphy, turgor, and venous filling status. This differs substantially from the in-hospital assessment of blood loss focusing on laboratory results such as hemoglobin, hematocrit, clotting factor concentrations, and coagulation intervals. The results of our study corresponded with the improved estimation of external blood loss when training was performed with a nomogram, as reported recently.[5]
Presumably, the estimation may be even more precise using a cell-phone-based software for planimetry of blood puddles in dependency of surface properties corrected with a specific coefficient. When considering age and weight of the patient, the amount of blood loss can even be assessed as percentage of circulating blood.
The limitations of this study are numerous. The study population was small although the results were within the range of similar studies.[5,12,13,16] Selection bias cannot be excluded as the majority of participants quoted the need to be trained in blood loss estimation. Factors that may influence blood puddle sizes were blood viscosity, coagulation, air humidity, temperature, and evaporation. In addition, surface characteristics may vary substantially, e.g., the thickness and absorbability of carpets, unevenness, and dimples may change area and expansiveness of blood puddles.[5] Accuracy of visual blood volume estimation may be further influenced by optical illusion arising from the color or pattern of surfaces.
The quantity of scattered blood on various surfaces is still difficult to estimate, but training with the visual estimation tool might help to consider the varying degrees of absorption into the overall assessment.
CONCLUSIONS
Training with a visual estimation tool by professional rescuers can improve the estimation accuracy of blood volumes spread on surfaces with varying absorptivity.
ACKNOWLEDGMENTS
The authors thank all participants for their attendance and for having contributed valuable feedback.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board and the Ethics Committee of the Medical University of Innsbruck and complied with the Declaration of Helsinki.
Conflicts of interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: JK wrote the main body of the report. All authors approved the final version.
REFERENCES
- 1.Tall G, Wise D, Grove P, Wilkinson C. The accuracy of external blood loss estimation by ambulance and hospital personnel. Emerg Med (Fremantle) 2003;15(4):318–21. doi: 10.1046/j.1442-2026.2003.00469.x. [DOI] [PubMed] [Google Scholar]
- 2.Williams B, Boyle M. Estimation of external blood loss by paramedics:is there any point? Prehosp Disaster Med. 2007;22(6):502–6. doi: 10.1017/s1049023x0000532x. [DOI] [PubMed] [Google Scholar]
- 3.Maslovitz S, Barkai G, Lessing JB, Ziv A, Many A. Improved accuracy of postpartum blood loss estimation as assessed by simulation. Acta Obstet Gynecol Scand. 2008;87(9):929–34. doi: 10.1080/00016340802317794. [DOI] [PubMed] [Google Scholar]
- 4.Lertbunnaphong T, Lapthanapat N, Leetheeragul J, Hakularb P, Ownon A. Postpartum blood loss:visual estimation versus objective quantification with a novel birthing drape. Singapore Med J. 2016;57(6):325–8. doi: 10.11622/smedj.2016107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeung CY, Yim WW, Chan SY, Lo RSL, Leung LY, Hung KKC, et al. Improvement of blood loss volume estimation by paramedics using a pictorial nomogram:a developmental study. Injury. 2017;48(12):2693–8. doi: 10.1016/j.injury.2017.10.045. [DOI] [PubMed] [Google Scholar]
- 6.Donham B, Frondozo R, Petro M, Reynolds A, Swisher J, Knight RM. Clinical image:visual estimation of blood loss. J Spec Oper Med. 2017;17(1):68–71. doi: 10.55460/UUWG-H2J7. [DOI] [PubMed] [Google Scholar]
- 7.Frank M, Schmucker U, Stengel D, Fischer L, Lange J, Grossjohann R, et al. Proper estimation of blood loss on scene of trauma:tool or tale? J Trauma. 2010;69(5):1191–5. doi: 10.1097/TA.0b013e3181c452e7. [DOI] [PubMed] [Google Scholar]
- 8.Bose P, Regan F, Paterson-Brown S. Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG. 2006;113(8):919–24. doi: 10.1111/j.1471-0528.2006.01018.x. [DOI] [PubMed] [Google Scholar]
- 9.Merlin MA, Alter SM, Raffel B, Pryor PW., 2nd External blood loss estimation using the MAR method. Am J Emerg Med. 2009;27(9):1085–90. doi: 10.1016/j.ajem.2008.07.039. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies:explanation and elaboration. BMJ Open. 2016;6(11):e012799. doi: 10.1136/bmjopen-2016-012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kreutziger J, Haim A, Jonsson K, Wenzel V, Stark M, Nussbaumer W. Variation in size of blood puddles on different surfaces. Eur J Emerg Med. 2014;21(5):360–3. doi: 10.1097/MEJ.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 12.Yoong W, Karavolos S, Damodaram M, Madgwick K, Milestone N, Al-Habib A, et al. Observer accuracy and reproducibility of visual estimation of blood loss in obstetrics:how accurate and consistent are health-care professionals? Arch Gynecol Obstet. 2010;281(2):207–13. doi: 10.1007/s00404-009-1099-8. [DOI] [PubMed] [Google Scholar]
- 13.Dildy GA, 3rd, Paine AR, George NC, Velasco C. Estimating blood loss:can teaching significantly improve visual estimation? Obstet Gynecol. 2004;104(3):601–6. doi: 10.1097/01.AOG.0000137873.07820.34. [DOI] [PubMed] [Google Scholar]
- 14.Mbachu II, Udigwe GO, Ezeama CO, Eleje GU, Eke AC. Effect of on-site training on the accuracy of blood loss estimation in a simulated obstetrics environment. Int J Gynaecol Obstet. 2017;137(3):345–9. doi: 10.1002/ijgo.12133. [DOI] [PubMed] [Google Scholar]
- 15.Sukprasert M, Choktanasiri W, Ayudhya NI, Promsonthi P, O-Prasertsawat P. Increase accuracy of visual estimation of blood loss from education programme. J Med Assoc Thai. 2006;89(Suppl 4):S54–9. [PubMed] [Google Scholar]
- 16.Beer HL, Duvvi S, Webb CJ, Tandon S. Blood loss estimation in epistaxis scenarios. J Laryngol Otol. 2005;119(1):16–8. doi: 10.1258/0022215053222752. [DOI] [PubMed] [Google Scholar]


