Abstract
Objective
In Japan, many otolaryngologists provide primary care for patients with coronavirus disease 2019 (COVID-19). The purpose of this study was to analyze the characteristics of otorhinolaryngological findings in order to improve COVID-19 diagnostic systems in a primary care setting.
Methods
A total of 351 patients (mean age, 36.0 ± 15.4 years) diagnosed with COVID-19 by otolaryngologists who belong to the Japan Otorhinolaryngologists Association were included in the study. A web-based questionnaire was used to collect information regarding the timing of positive identification of COVID-19, the route of infection, symptoms, and findings in the tonsils, nasal cavity, pharynx, ear, and neck. A modified Centor score was calculated for cases in which age, symptoms, and tonsil and neck findings were described.
Results
Symptoms included fever (56%), olfactory disturbance (46%), and a sore throat (56%). Of the individuals considered, 63% had ordinary rhinoscopic findings, 21% experienced watery rhinorrhea, and 12% had observable mucosal redness. Further, 87% had ordinary tonsillar findings, 13% displayed tonsillar redness, with enlargement and white mucus observe in 2% and 1% of participants, respectively. A total of 193 patients had a calculated Centor score of 3 points in 2%, and scores of the remaining participants were ≤2 points.
Conclusion
Of all patients considered, 40% had nasal findings and 4% had purulent nasal discharge. In contrast, only 13% of the patients had tonsillar findings, and no patients had Centor scores ≥4 points. Symptom differentiation from that of bacterial infections is difficult. In areas where COVID-19 is prevalent, the disease should be considered in patients presenting with fever, olfactory disturbances, and sore throat with minimal or no clinical findings in the nasal cavity and pharynx.
Keywords: COVID-19, Olfactory disturbances, Otolaryngological findings, Centor score
1. Introduction
In Japan, ear, nose and throat (ENT) clinics accounted for 5,828 (5.7%) of the 101,471 medical clinics operating in October of 2017 [1]. In most developed countries, general practitioners or family physicians provide primary care for upper respiratory tract infections. However, in Japan, under the universal health insurance system, patients have the option to choose the department they visit based on subjective symptoms by paying 10–30% of their medical costs, a value that depends on income and age. In addition, since ENT clinics provide local treatment to alleviate symptoms of the nasal cavity and pharynx, such as nasal and laryngeal procedures and nebulizer therapy, many patients who present with symptoms of an upper respiratory tract infection first visit ENT clinics.
COVID-19 is a disease that develops from upper respiratory tract infection symptoms. Under the healthcare system described above, many ENT clinics in Japan provide primary care for COVID-19 and play a role in its diagnosis. Otolaryngologists can evaluate local findings in great detail using specialized medical equipment such as rhinoscopes, laryngoscopes, and endoscopes, which require a deep understanding of local anatomy and the pathophysiology of the nasal cavity and pharynx. Therefore, with the aim of improving the diagnostic system of COVID-19 in primary care settings, we analyzed the characteristics of otolaryngological findings in patients diagnosed with COVID-19 in ENT clinics in Japan.
2. Materials and methods
In December 2020, we conducted a web-based survey titled "Nationwide survey of COVID-19 patients" among 7,254 members of the Japan Otorhinolaryngologists Association. A Google form was used for the survey, and all confirmed cases of COVID-19 at each institution were included. Personal information was anonymized at the time of registration at each facility; thus no individuals were identifiable.
The contents of the survey included the age and sex of COVID-19 positive patients. The reason why the patient visited the clinic when each diagnosis was confirmed, the type of test used for diagnosis, site of testing, route of infection, symptoms, and findings in the tonsils, nose, pharynx, ears, and neck were also recorded. In cases where age, symptoms, tonsillar findings, and neck findings were all present, a modified Centor score was calculated [2]. This study was approved by the Ethics Committee of the institution to which the first author is affiliated, and all researchers involved in this study acted in accordance with the latest Declaration of Helsinki and Ethical Guidelines for Medical Research Involving Human Subjects.
3. Results
3.1. Patient characteristics
A total of 353 patients were enrolled in the study, of these 351 had a confirmed diagnosis of COVID-19. The mean age was 36.0 ± 15.4 years (median age, 33 years), and the study included 175 males, 175 females, and 1 patient of unknown sex.
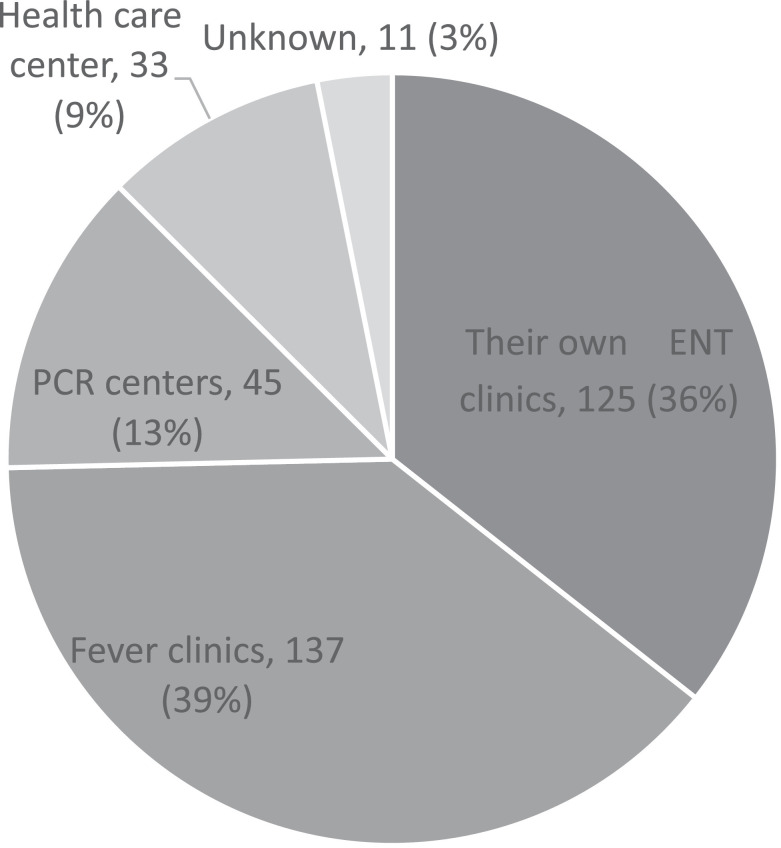
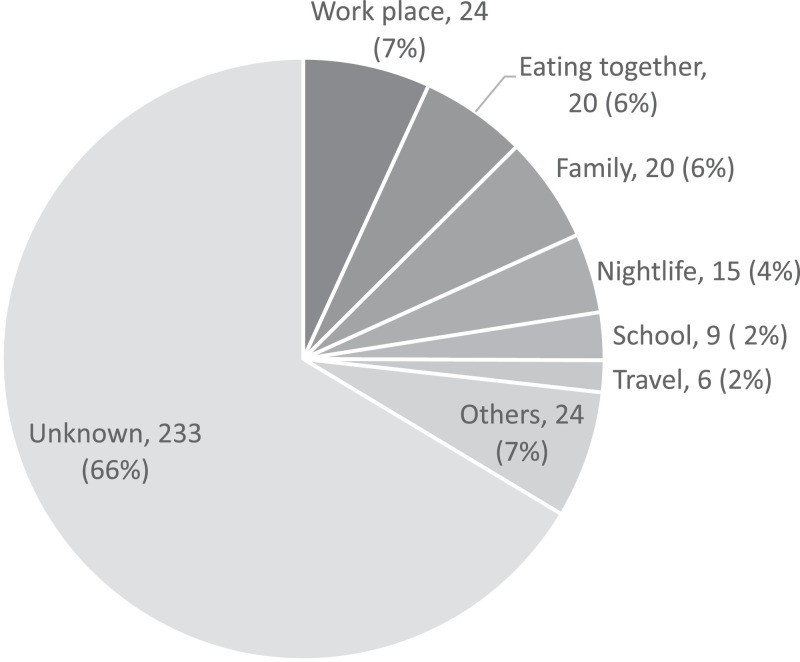
For 125 (36%) patients, COVID-19 was diagnosed at their own ENT hospital, 137 (39%) at fever outpatient clinics, 45 (13%) at centers that performed the polymerase chain reaction (PCR), 33 (9%) at public health centers, and 11 (3%) at unknown locations (Fig. 1 ). Routes of infection, identified at the time of the first visit, were as follows: 24 (7%) cases from workplace exposure, 20 (6%) cases from eating with an infected individual, 15 (4%) cases from nightlife exposure, 9 (2%) cases from school, and 6 (2%) cases from travel. A total of 233 (66%) cases were of unknown origin, or the infection route was not reported at the time of the patient's initial examination (Fig. 2 ).
Fig. 1.
Facility where patients were diagnosed with coronavirus disease. For 125 (36%) patients, COVID-19 was diagnosed at their own ENT hospitals, 137 (39%) at fever outpatient clinics, 45 (13%) at PCR centers, 33 (9%) at public health centers, and 11 (3%) at unknown locations.
Fig. 2.
Route of infection identified at the time of initial diagnosis. Routes of infection identified at the time of the first visit were as follows: 24 (7%) cases from workplace exposure, 20 (6%) cases from eating with an infected individual, 15 (4%) cases from nightlife exposure, 9 (2%) cases from school, and 6 (2%) cases from travel. A total of 233 (66%) cases were of unknown origin, or the infection route was not reported at the time of the patient's initial examination.
3.2. Basis of diagnosis
The types of tests used to positively confirm the presence of SARS-CoV-2 infection were (with some duplication): PCR (nasopharynx), 179 (51%) cases; PCR (saliva), 57 (16%) cases; PCR (nasal cavity), 16 (5%) cases; antigen qualitative test, 69 (20%) cases; antigen quantitative test, 12 (3%) cases; and unknown, 25 (7%) cases.
3.3. Clinical symptoms
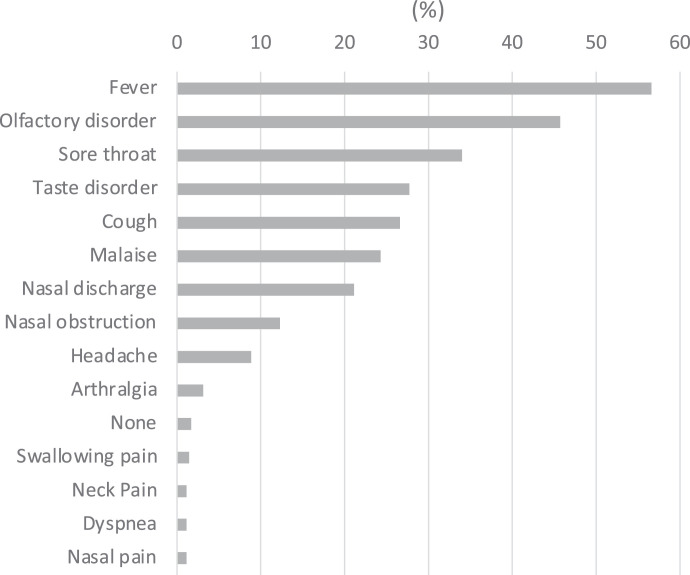
Of the 350 cases considered, the chief complaint (with duplication) was: fever, 198 (56%) cases; olfactory disturbance, 160 (46%) cases; sore throat, 119 (34%) cases; taste disturbance, 97 (28%) cases; cough, 93 (27%) cases; malaise, 85 (24%) cases; nasal discharge, 74 (21%) cases; nasal obstruction, 43 (12%) cases; headache, 31 (9%) cases; arthralgia, 11 (3%) cases; no symptoms, 6 (2%) cases; pain when swallowing, 5 (1%) cases; neck pain, 4 (1%) cases; respiratory distress, 4 (1%) cases; intranasal pain, 4 (4%) cases; diarrhea, 3 c (1%) cases; sputum, 3 (1%) cases; hearing impairment, 2 (1%) cases; otalgia, 2 (1%) cases; nasal obstruction, 2 (1%) cases; posterior rhinorrhea, 2 (1%) cases (Fig. 3 ).
Fig. 3.
Symptoms of coronavirus disease present at the initial visit.
3.4. Otolaryngological findings
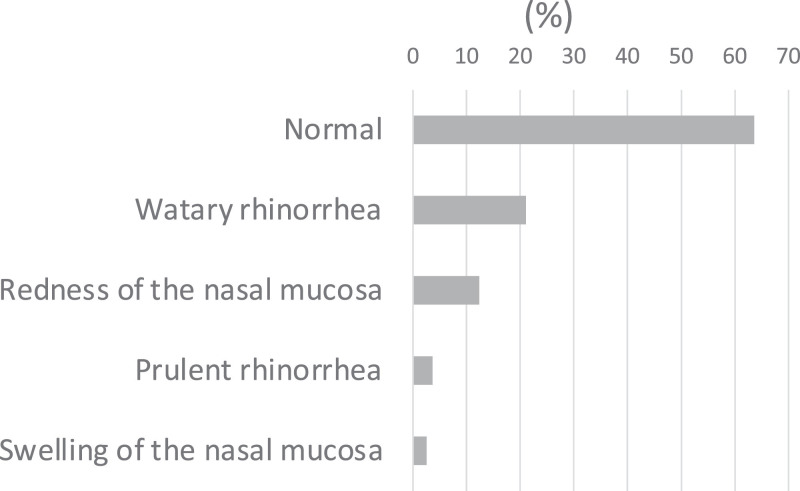
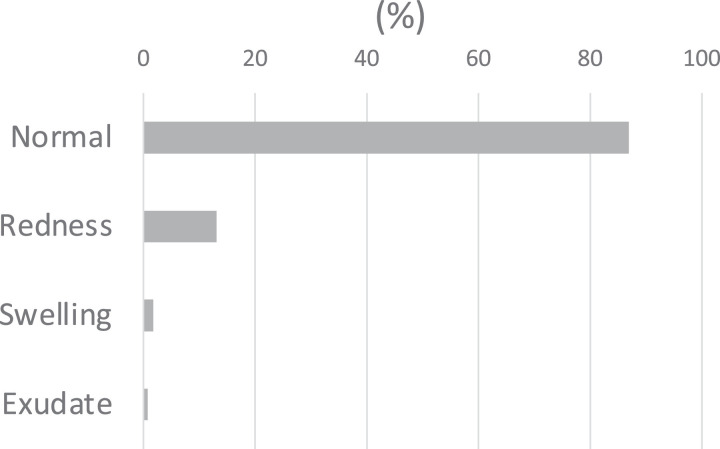
Otolaryngological findings were specified as either otoscopic, rhinoscopic, tonsillar, pharyngeal, or neck. Otoscopic findings were reported for 142 cases. An affected otitis media was found in one case; however, the remaining 141 cases were normal. Rhinoscopic findings were reported for 275 patients. Of these, 175 (63%) patients had no abnormalities, 58 (21%) had watery nasal discharge, 34 (12%) had mucosal redness, 10 (4%) had purulent nasal discharge, and 7 (3%) had nasal mucosal swelling (Fig. 4 ). Tonsillar findings were ordinary in 245 patients (87%), and redness was observed in 37 (13%) patients, enlargement was found in 5 (2%) patients, and exudate was present in 2 patients (1%) (Fig. 5 ). Pharyngeal findings were reported in 284 patients. Among these, 173 (61%) displayed no abnormalities, 110 (39%) had redness, and 1 (0.4%) had stomatitis. In comparison, regarding palatine tonsil findings, 81 (32%) cases had redness in the pharynx but no abnormalities in the tonsils, and 30 (11%) cases had redness in both the pharynx and tonsils. No pharyngeal or tonsillar findings were reported for 156 patients (61%). Neck findings were reported in 194 cases. Of these, no abnormalities were observed in 187 (96%) cases and lymphadenopathy occurred in 7 (4%) cases.
Fig. 4.
Nasal findings associated with coronavirus disease present at the initial visit.
Fig. 5.
Tonsillar findings associated with coronavirus disease present at the initial visit.
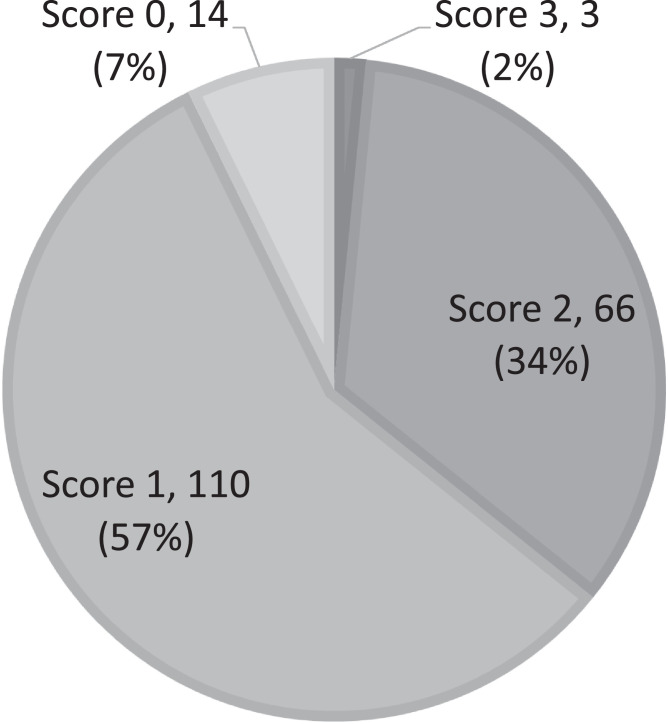
There were 193 cases with complete age, symptom, tonsillar and neck finding data. Of these the modified Centor score calculated was 3 (2%), 2 (34%), 1 (57%), and 0 (7%) for 3, 66, 110, and 14 cases, respectively (Fig. 6 ).
Fig. 6.
Centor score determined for coronavirus disease-positive patients with a description of associated tonsillar and neck findings present at the initial visit (n = 193). The Centor score calculated was 3 (2%), 2 (34%), 1 (57%), and 0 (7%) for 3, 66, 110, and 14 cases, respectively.
4. Discussion
The provision of treatment for upper respiratory tract infection, including COVID-19, by otolaryngologists is advantageous because they may diagnostically assess local findings in detail and with a high degree of accuracy using specialized medical equipment, such as the specific optical devices used for rhinoscopy, laryngoscopy, and endoscopy. Further, otolaryngologists are able to respond quickly and accurately to diseases that require emergency treatment such as peritonsillar abscess or acute epiglottitis. Therefore, it is important for otolaryngologists to clarify local findings of COVID-19 to differentiate COVID-19 from other diseases at the time of initial diagnosis, enabling practitioners to respond sufficiently and quickly for effective treatment and infection control.
In Japan, symptoms of COVID-19 recorded at the initial visit to ENT departments were fever (56%), olfactory disturbance (46%), sore throat (34%), taste disturbance (28%), cough (27%), nasal discharge (21%), nasal obstruction (12%), and headache (9%). However, symptoms of COVID-19 patients from European countries with mild to moderate disease included headache (70%), olfactory disturbance (70%), nasal obstruction (67.8%), dysgeusia (63%), and nasal discharge (60%) [3], and those reported for patients from Turkey were cough (32%), nasal obstruction (10%), nasal discharge (3%), sore throat (15%), olfactory disturbance (47%), and dysgeusia (44%) [4]. Assessing general comparisons between Japan and other countries is not possible, because in other countries, most COVID-19 patients are diagnosed by family physicians. As a result, differences arise since some patients do not experience subjective otolaryngological symptoms, and methods used for assessing symptoms differ. However, in patients with COVID-19 who were first examined at an ENT clinic in Japan, where a high proportion of ENT symptoms are expected to be detected, the incidence of olfactory taste disorder was lower than of other countries. This result is likely due to the fact that this study reviewed symptoms present at the time of the first visit and included cases in which olfactory and gustatory disturbances may have occurred later on as the disease progressed, however, in agreement the incidences of olfactory and gustatory disturbances in COVID-19 in Japan is low. Although virus differences, due to the presence of mutations and host genetic factors, have been identified as potential causes of the high and low incidences of olfactory and gustatory disorders in Western and Asian regions, respectively, the precise features that underlie regional differences remain unclear [5]. It should be noted that in Japan, the number of typical COVID-19 cases presenting with acute olfactory and gustatory disturbances is lower than that of Western countries, and many patients present with only general upper respiratory tract infection symptoms.
Rhinoscopic findings were ordinary in 63% of cases considered. However, cases of acute rhinitis were observed, which were characterized by the presence of a watery nasal discharge in 21% of cases, mucosal redness in 12%, and purulent nasal discharge in 4% of cases. Purulent rhinorrhea and posterior rhinorrhea are characteristic findings of bacterial rhinosinusitis [6]. However, recent reports suggest that antimicrobial agents are not necessarily effective, even in acute rhinosinusitis with purulent rhinorrhea [7,8]. Therefore, during the SARS-CoV-2 epidemic, it has remained difficult to differentiate between SARS-CoV-2 and bacterial infections, even in patients presenting with purulent nasal discharge due to acute rhinosinusitis. Symptomatic treatment and guidance on infection control should be provided to those in contact with an infected patient. If symptoms persist for 10 days post-symptom onset, the initiation of antimicrobial therapy is re-commended.
Tonsillar findings were ordinary in 87% of patients considered. However, redness was observed in 13%, enlargement in 2%, and exudate in 1% of patients. Neck lymph node findings showed that only 4% of patients had enlarged neck lymph nodes. To date, no single parameter has been identified that distinguishes viral from bacterial tonsillitis; nevertheless, the modified Centor score has been used as an excellent screening method for acute tonsillitis caused by streptococci and recommends the use of rapid tests and culture tests for patients with scores ≥3, since streptococcal infection is suspected. Fever (> 38°C), absence of cough, neck lymphadenopathy, and the presence of enlarged tonsils and exudates are assigned 1 point each, patients aged 3–14 years are given 1 point, patients 15–44 receive 0 points, and those aged ≥ 45 years receive -1 point [2,9]. The possibility of streptococcal infection for Centor scores ≤ 2 points, 3 points, and ≥ 4 points is ≤ 17%, ≤ 35%, and > 50%, respectively [2,10]. Among the 193 patients with reported pharyngeal and neck findings who were first diagnosed with COVID-19 in this study, only 2% had a Centor score of 3, and none had a score ≥ 4. Centor scores could be calculated in 55% of all cases and the remaining cases were prioritized for pathogen examination. Briefly explained, Centor scores could not be calculated for cases in which COVID-19 was more strongly suspected than bacterial inflammation, such as fever type, presence of cough or sick contact, and may have been biased to increase the probability of bacterial infections relative to all eligible cases. Therefore, when clinical findings are suggestive of a bacterial infection, as represented by a high Centor score, symptoms are not likely to due to a SARS-CoV-2 infection, and the initiation of treatment with antimicrobial agents is recommended. However, if the patient complains of a sore throat and cough despite the absence of abnormal findings from visual examinations, COVID-19 should be considered.
This report analyzed nasal and pharyngeal findings associated with COVID-19 from the particular perspective of otolaryngological specialists due to the characteristics of the Japanese medical system, which has an important role in the differentiation of COVID-19 from bacterial disease based on the findings. At the time this report was compiled, the SARS-CoV-2 pandemic showed no signs of ending. Due to Japan's healthcare delivery system, otolaryngologists must continue to provide safe and reliable information regarding acute upper respiratory tract infections, which involves COVID-19 and non-COVID-19-associated diseases.
5. Conclusion
We analyzed the clinical characteristics of 351 patients that were diagnosed with COVID-19 in ENT clinics in Japan. Olfactory and gustatory disturbances were relatively rare when compared with reports from Western countries. Nasal findings were not always easy to distinguish from bacterial infections, as nasal findings were observed in approximately 40% of cases and purulent nasal discharge was reported in 4% of cases. In terms of pharyngeal findings, only 13% of cases had findings that were reported. Further, no case had a Centor score of ≥ 4 points, indicating that COVID-19 is unlikely to be present in cases with typical pharyngeal findings of a bacterial infection. The limitations of this study include the unavailability of resources, small sample size, and flawed methodology. In areas where COVID-19 is prevalent, symptoms such as fever, olfactory disturbances, and sore throat without any clinically abnormal nasal or pharyngeal findings should be addressed with COVID-19 infection in mind.
Declaration of Competing Interest
The authors declare no conflicts of interest associated with this manuscript.
Acknowledgement
We would like to express our gratitude to all members of the Japan Otorhinolaryngology Association who partook in this survey.
References
- 1.Ministry of Health, Labor and Welfare. Overview of the 2017 medical facilities (static and dynamic) survey and hospital reports. 2020 https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/17/dl/09gaikyo29.pdf.
- 2.McIsaac W.J., Goel V., To T., Low D.E. The validity of a sore throat score in family practice. Can Med Assoc J. 2000;163:811–815. [PMC free article] [PubMed] [Google Scholar]
- 3.Lechien J.R., Chiesa-Estomba C.M., Place S., Laethem Y.V., Cabaraux P., Mat Q. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 2020;288:335–344. doi: 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avcı H., Karabulut B. The relation between otolaryngology-specific symptoms and computed tomography findings in ambulatory care COVID-19 patients. Ear Nose Throat J. 2021;100:79–85. doi: 10.1177/0145561320975508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butowt R., Bilinska K., Von Bartheld C.S. Chemosensory dysfunction in COVID-19: integration of genetic and epidemiological data points to D614G spike protein variant as a contributing factor. ACS Chem Neurosci. 2020;11:3180–3184. doi: 10.1021/acschemneuro.0c00596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young J., De Sutter A.I.M., Merenstein D., van Essen G.A., Kaiser L. Antibiotics for adults with clinically diagnosed acute rhinosinusitis: a meta-analysis of individual patient data. Lancet. 2008;371 doi: 10.1016/S0140-6736(08)60416-X. 908–14. [DOI] [PubMed] [Google Scholar]
- 7.Kenealy T., Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev. 2013;6 doi: 10.1002/14651858.CD000247.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van den Broek M.F., Gudden C., Kluijfhout W.P., Stam-Slob M.C., Aarts M.C., Kaper N.M. No evidence for distinguishing bacterial from viral acute rhinosinusitis using symptom duration and purulent rhinorrhea: a systematic review of the evidence base. Otolaryngol Head Neck Surg. 2014;150:533–537. doi: 10.1177/0194599814522595. [DOI] [PubMed] [Google Scholar]
- 9.ESCMID Sore Throat Guideline Group Guideline for the management of acute sore throat. Clin Microbiol Infect. 2012;18(Suppl 1):1–28. doi: 10.1111/j.1469-0691.2012.03766.x. [DOI] [PubMed] [Google Scholar]
- 10.McIsaac W.J., Kellner J.D., Aufricht P., Vanjaka A., Low D.E. Empirical validation of guidelines for the management of pharyngitis in children and adults. JAMA. 2004;291:1587–1595. doi: 10.1001/jama.291.13.1587. [DOI] [PubMed] [Google Scholar]