Abstract
Background
The majority of ventricular tachycardias (VTs) occurs in patients with structural heart disease and is associated with an increased risk of sudden cardiac death. These VT are scar-related and may develop in patients with ischaemic or non-ischaemic cardiomyopathies.
Case summary
We describe a 44-year-old patient without any pre-existing cardiovascular disease, presenting with the first documentation of a haemodynamically unstable sustained fast VT with a cycle length of 250 ms. He reported a suicidal attempt with a self-made handgun aged 16 when he had shot himself in the thorax and had injured the myocardium. After presenting with the VT coronary artery disease was excluded through cardiac catheterization. A cardiovascular magnetic resonance study showed a localized myocardial scar in the left ventricular free wall starting from the subepicardium and correlating to the scar described 28 years ago by the thoracic surgeons. In an electrophysiological study, non-sustained VT were easily inducible. Presuming a causal relationship between the fast VT and the epicardial scar, a single-chamber implantable cardioverter-defibrillator was implanted and beta-blocker therapy was initiated.
Discussion
Scar-related VT often occur many years after an acute event, e.g. an acute myocardial infarction. This case highlights, that any cardiac trauma, even a superficial epicardial projectile-related damage with subsequent scarring, may cause a VT after many years and to our knowledge for the first time describes the occurrence of a VT due to mechanical damage to the myocardium by a gunshot.
Keywords: Ventricular tachycardia, Case report, Gunshot
For the podcast associated with this article, please visit https://academic.oup.com/ehjcr/pages/podcast
Learning points
Any cardiac trauma with subsequent scarring may act as a substrate for ventricular tachycardia even after many years.
The need for an implantable cardioverter-defibrillator is difficult to predict in these cases with a single arrhythmic event of uncertain origin and a circumscribed non-ischaemic scar in the presence of a preserved ventricular function.
Introduction
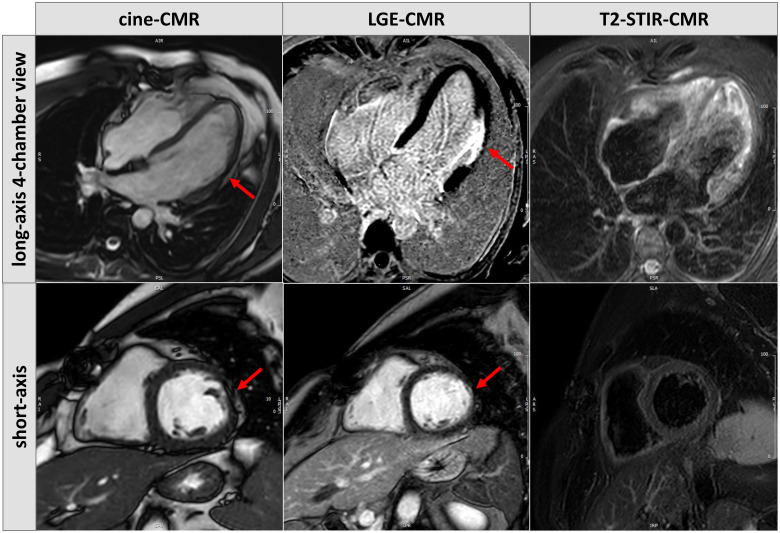
Structural heart disease is the most common cause for ventricular tachycardia (VT) and is associated with an increased risk of sudden cardiac death. VTs are often scar-related, may develop in patients with ischaemic or non-ischaemic cardiomyopathies and are associated with an increased risk of sudden cardiac death. To the best of our knowledge, we here present the first case of a bullet-associated VT that occurred 28 years after a failed suicide attempt with a self-made handgun (Timeline).
Timeline
Case presentation
In August 2020, a 44-year-old male patient presented after the first occurrence and documentation of a haemodynamically unstable sustained fast VT with a cycle length of 250 ms. The patient’s history revealed no pre-existing cardiovascular disease, he was not taking any medications or drugs of abuse. He only reported a suicide attempt with a self-made handgun aged 16 when he had shot himself in the thorax. At that time, he had undergone emergency cardiac surgery. The cardiac surgeons documented that a bullet had perforated the pericardium and touched on the anterolateral aspect of the left ventricle. The patient survived, underwent psychiatric therapy and has lived a healthy life thereafter. No psychiatric drugs were taken by the patient at any point. The patient exercises several times a week.
At the day of the initial admission, the patient was on a bike ride and suddenly experienced palpitations and fatigue. The patient rode back home slowly, where he laid down and tried to rest. Mild dyspnoea but no chest pain was reported. Because the symptoms persisted upon resting, the patient called an ambulance.
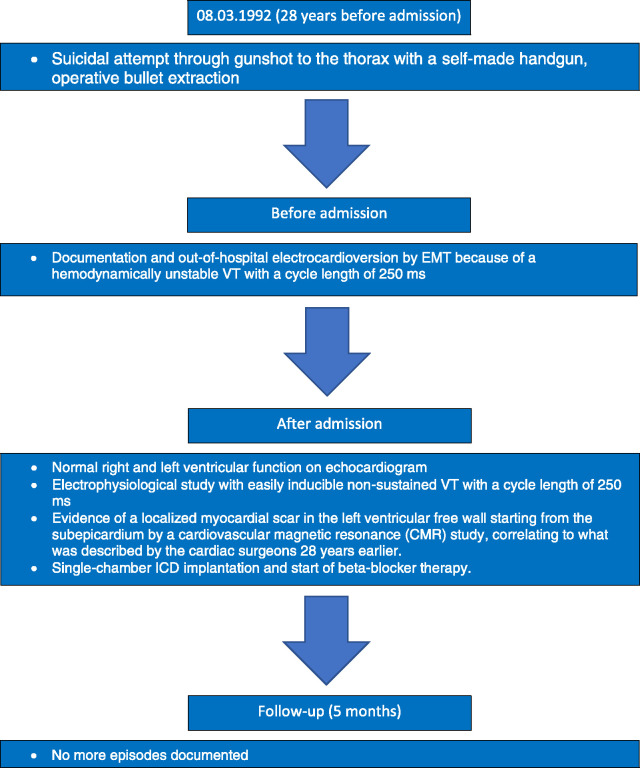
When the emergency medical team (EMT) arrived, a wide-complex tachycardia with a cycle length of 250 ms was documented and electrically cardioverted two times. VT was described by the EMT as haemodynamically relevant (Figure 1).
Figure 1.
EMT-documentation of a sustained ventricular tachycardia with a cycle length of 250 ms.
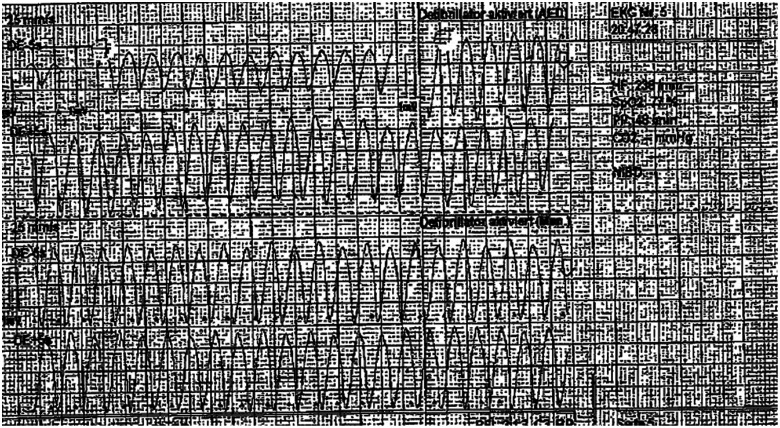
On admission in our clinic, the patient was asymptomatic and in stable sinus rhythm. Physical and cardiovascular examinations were inconspicuous. Blood tests showed an elevated Troponin (187 pg/mL; normal range: <14 pg/mL) with normal CK levels (149 U/L; normal range: <190 U/L), other than that they were unremarkable. Electrocardiogram showed a stable sinus rhythm with flattened or inverted T-waves in I, II, aVL, and V5–V6 (Figure 2).
Figure 2.
A 12-lead electrocardiogram at rest at time of admission (50 mm/s).
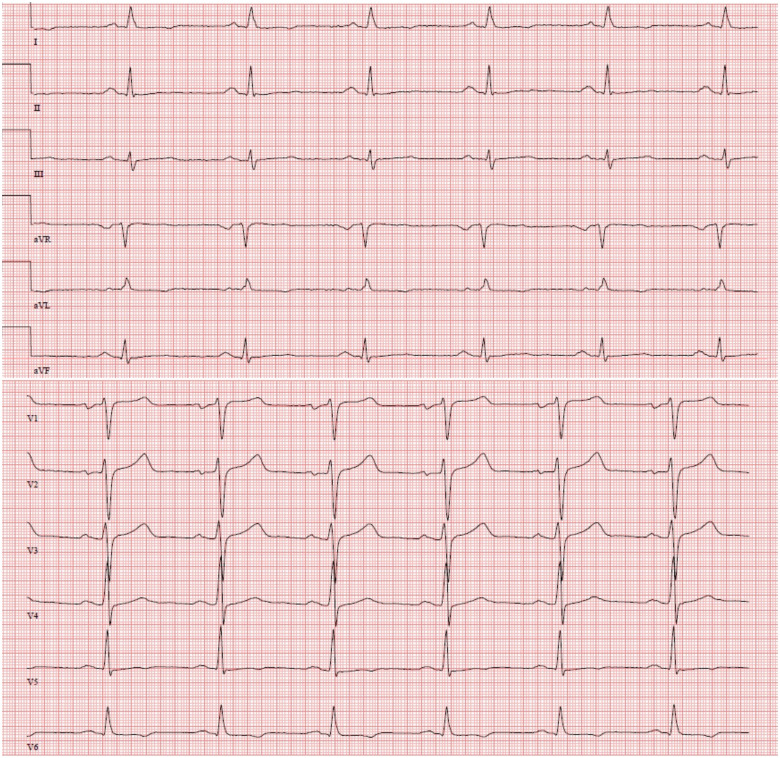
His echocardiogram revealed a normal right and left ventricular function. Cardiac catheterization excluded coronary artery disease. Though the timeline between the initial chest trauma and the occurrence of the VT was very long we were unable to detect a precipitating factor that triggered the VT. Besides, a cardiovascular magnetic resonance (CMR) study revealed a localized myocardial scar that correlated to the area that was described by cardiac surgery 28 years earlier (Figures 1 and 2). Other differential diagnoses (e.g. Sarcoidosis) were considered in this young patient presenting with VT and late gadolinium enhancement in CMR, but because of untypical patient history and findings, deemed quite unlikely (Figures 3 and 4).
Figure 3.
Cine-cardiovascular magnetic resonance images with a regional thinning in the midventricular left ventricular free wall (red arrow). Corresponding late gadolinium enhancement-cardiovascular magnetic resonance images depict a localized transmural myocardial scar in the area of myocardial thinning (red arrow). Since T2-weighted STIR images did not show any signal enhancement in the myocardium, there were no signs of myocardial oedema and consequently the observed myocardial scar is not in line with a myocarditis but rather reflects a chronic disease process.
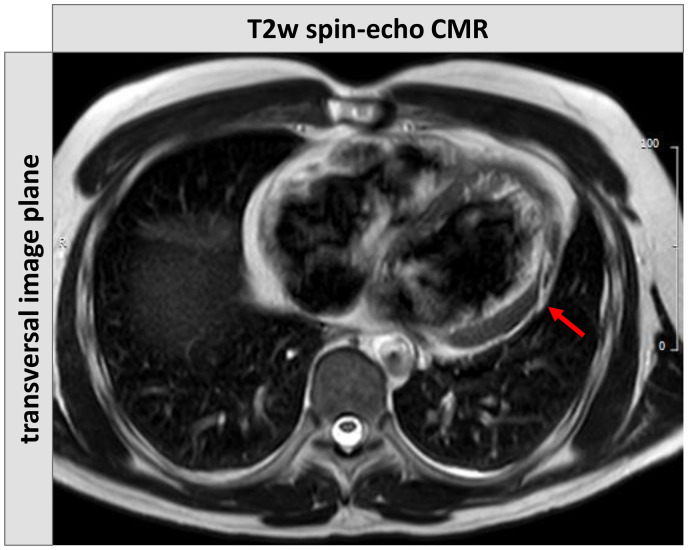
Figure 4.
Conventional T2-weighted spin-echo cardiovascular magnetic resonance images highlight the distribution pattern of myocardial damage in the left ventricular free wall that rather starts from the subepicardium and extends into the subendocardium, thereby consistent with a non-ischaemic process.
During an electrophysiological study with programmed electrical stimulation with up to three extra beats, non-sustained monomorphic VT were easily inducible at all basic cycle lengths with one or more extra beats (e.g. 500 ms, 430 ms, and 370 S2) without and in the presence of orciprenaline (0.25 mg) (Figure 5).
Figure 5.
Typical example of the non-sustained ventricular tachycardia-induced during the electrophysiological study at 370 S3.
In the presence of the fast haemodynamically relevant sustained VT, the patient’s history with the CMR findings and the results of the electrophysiological study, all therapeutic alternatives mainly VT ablation with endo- and epicardial substrate mapping/ablation and/or implantable cardioverter-defibrillator (ICD) implantation were extensively discussed with the patient and his family, who decided on ICD implantation. Therefore, the patient underwent single-chamber ICD implantation as secondary prophylaxis. Besides, beta-blocker therapy was started (bisoprolol 2.5 mg pd). During a follow-up of 5 months after discharge there were no other arrhythmic episodes documented.
Discussion
Scar-related VT often occurs many years after an acute event, e.g. an acute myocardial infarction. The reason for the often very long time periods between an acute event and a subsequent VT remains unknown but slowing of conduction and the occurrence of critically timed extra beats play an important role.1
There have been previously described cases of VT following mechanical trauma to the heart, e.g. after a blunt trauma to the chest.2 But to our knowledge, this case for the first time describes a monomorphic scar-related VT due to a penetrating mechanical damage to the myocardium by a gunshot.
The case nicely illustrates that any cardiac trauma even a superficial epicardial projectile with subsequent scarring may cause a VT after many years. It is hard to predict, whether the patient will suffer further VT episodes and/or will benefit from ICD therapy. Yet after an individual risk-benefit evaluation, we decided to implant a defibrillator as secondary prophylaxis because of the presentation with a fast VT, the easy induction of non-sustained VT during the electrophysiological study, and the presence of transmural scar in the left ventricular free wall on CMR.
Conclusion
It is known that VTs often occur many years after a remote acute myocardial event such as a myocardial infarction. To our knowledge, this is the first report of a monomorphic scar-related VT due to penetrating mechanical damage to the myocardium by a gun shot. The case highlights the role of cardiac trauma even after many years for the development of life-threatening VT.
Lead author biography

Dr. Florian Doldi graduated from the Medical University of Varna (Bulgaria) in 2019. He is currently specializing in Cardiology at the University Hospital Münster, Germany in the Department of Cardiology (Electrophysiology).
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patients in line with COPE guidance.
Conflict of interest: None declared.
Funding: None declared.
Supplementary Material
References
- 1.Stevenson WG. Ventricular scars and ventricular tachycardia. Trans Am Clin Climatol Assoc 2009;120:403–412. [PMC free article] [PubMed] [Google Scholar]
- 2.Casado-Arroyo R, Namdar M, Bayrak F, Sarkozy A, Meir ML, Brugada P.. The apple does not fall far from the tree: epicardial ventricular tachycardia due to blunt chest trauma. Eur Heart J 2012;33:1430. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.