Abstract
Background
While left-sided congenital heart defects have been well described in females with Turner syndrome (45, X), the literature is scarce regarding arrhythmias in this patient population.
Case summary
A full-term neonate referred to cardiology was found to have a non-apex forming left ventricle and partial anomalous pulmonary venous return. During the echocardiogram, she developed atrial flutter, followed by orthodromic reentrant supraventricular tachycardia (SVT). She was started on propranolol and eventually switched to sotalol due to breakthrough SVT. A genetics evaluation revealed Turner syndrome with complete monosomy X (45, X). The patient is now 18 months old and has not had any further arrhythmias.
Discussion
We present a rare case of atrial flutter followed by supraventricular tachycardia in a neonate with Turner syndrome and left-sided heart defects. This case highlights the importance of early and precise investigation of cardiac abnormalities in neonatal patients, especially among females with Turner syndrome given their relatively higher risk of cardiovascular disease compared to the general population.
Keywords: Turner syndrome, Atrial flutter, Supraventricular tachycardia, Arrhythmia, Congenital heart disease, Case report
Learning points
Left-sided congenital heart defects are common in females with Turner syndrome (45, X), but arrhythmias are not well described in this patient population.
As soon as Turner syndrome is suspected or confirmed, investigation of cardiac abnormalities is recommended given their higher risk of cardiovascular disease.
Introduction
In females with Turner syndrome (45, X), left-sided congenital heart defects are well described. However, the literature is scarce regarding arrhythmias. A common electrocardiographic abnormality in Turner syndrome is a prolonged QT interval, which may be associated with ventricular tachyarrhythmias.1,2 While a case of supraventricular tachycardia (SVT) has been previously described in an adult with Turner syndrome, there are no cases describing multiple atrial arrhythmias in Turner syndrome.3 We describe the first case of a neonate with Turner syndrome, presenting with left-sided heart defects and atrial flutter followed by SVT.
Timeline
| Days of age | Clinical findings |
|---|---|
| 3 | Apneic episode with hypoxia upon feeding. Transferred to neonatal intensive care unit for monitoring. Screening electrocardiogram showed normal sinus rhythm, northwest axis, right ventricular hypertrophy with strain, possible left ventricular hypertrophy, and T-wave inversion in lateral leads. |
| 4 | Discharged with plan for outpatient cardiology follow-up. |
| 5 | Seen by primary care provider. Heart rate variability noted during feeding. |
| 8 | Electrocardiogram in cardiology clinic revealed sinus tachycardia, northwest axis, right ventricular hypertrophy with strain, paucity of left ventricular forces, and QTc 447 ms. Echocardiogram revealed a non-apex forming left ventricle with increased trabeculations, low normal left ventricular systolic function, and partial anomalous pulmonary venous return. During the echocardiogram, she developed atrial flutter followed by supraventricular tachycardia (SVT). Admitted to pediatric intensive care unit (PICU). She had two breakthrough episodes of SVT. |
| 13 | Discharged home. |
| 19 | Brought to the emergency department due to SVT. Readmitted to PICU. Switched medications. Discharged home after no-repeat events. |
| Current | Seen by cardiologist every 1–2 month(s) as outpatient. Weaned off the antiarrhythmic medication by 12 months of age without any reoccurrence of SVT to date. |
Case presentation
A full-term, non-dysmorphic 3-day-old female in the newborn nursery had an apneic episode with hypoxia upon feeding, most likely due to aspiration, and was transferred to the neonatal intensive care unit. Her screening electrocardiogram showed normal sinus rhythm at 124 beats per minute (bpm.), a northwest axis, right ventricular hypertrophy with strain pattern, possible left ventricular hypertrophy, and T-wave inversion in the lateral leads. There was no family history of arrhythmias or congenital heart disease. She was feeding well with no further apneic episodes, therefore was discharged home at 4 days of age with plan for outpatient cardiology follow-up.
The baby was seen by her primary care provider at 5 days. Heart rate variability from 97 to 120 bpm was noted during feeding without further apnoea. She was otherwise doing well without cyanosis, sweating, or tachypnoea during feeds.
The electrocardiogram in the cardiology clinic at 8 days of life showed sinus tachycardia at 182 bpm, a northwest axis, right ventricular hypertrophy with strain pattern, paucity of left ventricular forces, and a borderline QT interval (Figure 1A). Her corrected QT interval (QTc) was 448 msec. An echocardiogram revealed a non-apex forming left ventricle with increased trabeculations (Video 1, Figure 2), low normal left ventricular systolic function, and partial anomalous pulmonary venous return (PAPVR) of the right upper pulmonary vein with no evidence of right heart dilation (Figures 3 and 4). Notably, the baby had a normal trileaflet aortic valve, no evidence of coarctation of the aorta, and no gradient in the blood pressures between the right arm and right leg. While undergoing her echocardiogram, she developed atrial flutter with an atrial rate of 320 bpm and 2:1 atrioventricular conduction (Video 2) associated with mottling and cyanosis. The rhythm transitioned to SVT at a rate of 350 bpm (Figure 1B) that was terminated by the application of ice to the face. She was admitted to the pediatric intensive care unit (PICU) and started on oral propranolol at 1 mg/kg/day spread over 3 doses per day. She had two breakthrough episodes of SVT (Figure 5) that required intravenous adenosine (0.2 mg/kg) and titration of propranolol up to 3 mg/kg/day. She was hemodynamically stable during all episodes of SVT. She had no further events and was discharged home with a 24-hour Holter monitor at 13 days of age.
Figure 1.
(A) Baseline electrocardiogram in cardiology clinic at 8 days of age showing sinus tachycardia with a heart rate of 182 beats per minute, a northwest axis, and right ventricular hypertrophy with strain pattern. (B) Electrocardiogram one hour later showing orthodromic reentrant supraventricular tachycardia with retrograde conduction at 350 beats per minute. The retrograde p-waves are noted with arrows.
Figure 2.
Apical four-chamber view showing a non-apex forming (arrow) mildly hypoplastic left ventricle with increased trabeculations (*). LV, left ventricle; RV, right ventricle.
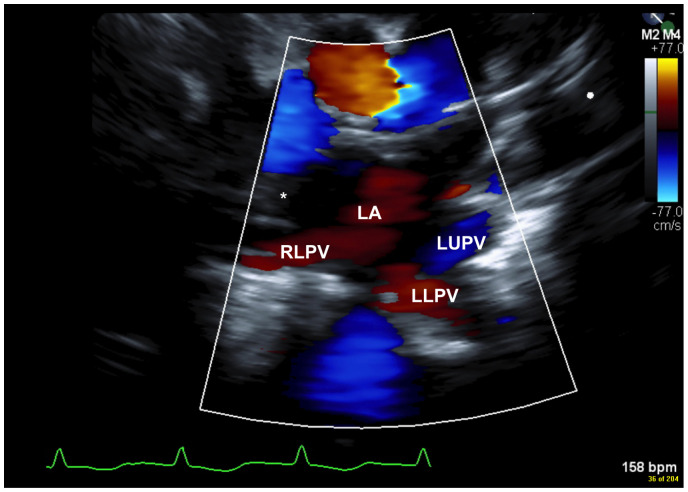
Figure 3.
Suprasternal notch view showing the normal drainage of the right lower (RLPV), left upper (LUPV), and left lower pulmonary veins (LLPV) into the left atrium (LA). The absence of the right upper pulmonary vein (RUPV) is shown with the *, suggestive of partial anomalous pulmonary venous return (PAPVR) of the RUPV.
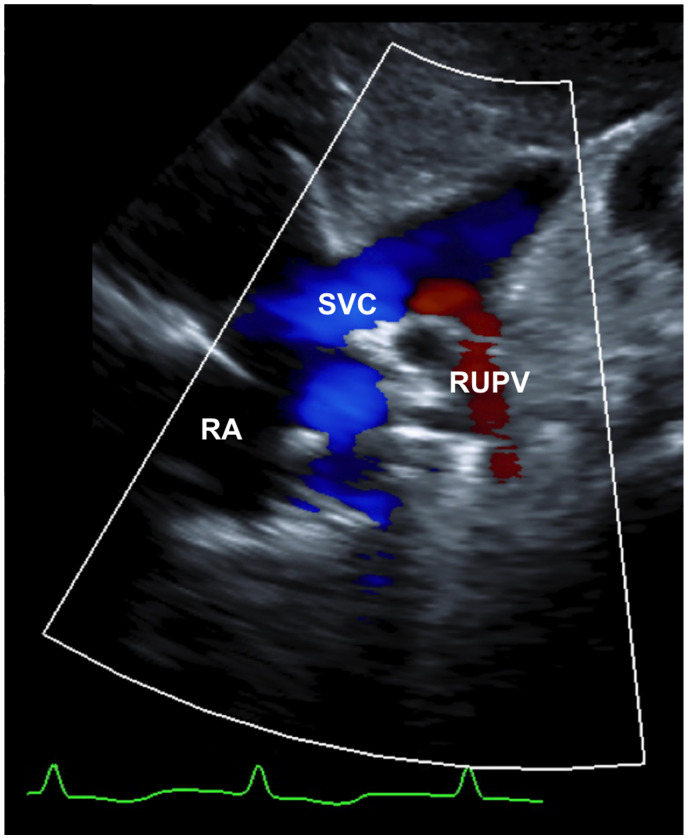
Figure 4.
Right parasternal view showing the anomalous venous drainage of the right upper pulmonary vein (RUPV) into the right superior vena cava (SVC). RA, right atrium.
Figure 5.
Supraventricular tachycardia at 266 beats per minute that converted to sinus rhythm after administration of intravenous adenosine 0.2 mg/kg in the pediatric intensive care unit. Note the retrograde p-waves (arrows), consistent with orthodromic retrograde conduction.
At 19 days of age, she was brought back to the emergency department after a 3-hour episode of SVT at 288 bpm was noted on her Holter monitor (Figure 6). Upon arrival, she was found to be in SVT, which again terminated with application of ice to the face. She was readmitted to the PICU, and propranolol was switched to sotalol (54 mg/m2/day). After a few days of monitoring with no-repeat events, she was discharged home.
Figure 6.
Supraventricular tachycardia at 288 beats per minute with spontaneous resolution noted on Holter monitoring. The retrograde p-waves are noted with arrows.
The patient has been seen every 1–2 months in the cardiology outpatient clinic without breakthrough episodes of SVT or increase in her QTc. Due to the patient’s cardiac findings, a genetics evaluation was pursued. Chromosomal microarray revealed Turner syndrome with complete monosomy X (45, X). The infant was successfully weaned off of sotalol at 12 months of age and remains hemodynamically stable without further arrhythmias to date.
Discussion
Cardiac arrhythmias in neonates have an approximate incidence of 24.4 per 100 000 live births and may present with or without congenital heart disease.4 Among arrhythmias in neonates, the most common is SVT, with an incidence of 1 per 250–1,000 paediatric patients.5,6 Atrial flutter occurs less often, with an incidence of 2.1 per 100,000 live births, and typically does not reoccur after treatment.4,6 While one study of 44 neonates with atrial flutter showed that 25% had a second atrial arrhythmia, none of them had an underlying genetic syndrome.7 Our case is the first to illustrate a newborn with Turner syndrome having atrial flutter followed by SVT.
Turner syndrome occurs in 1/2500 live female births and is caused by the complete or partial absence of one X chromosome.8 About 45% of cases are caused by monosomy X (45, X), while the remainder is due to mosaicism (45, X/45, XX or 45, X/47, XXX) or X chromosome abnormalities (i(Xq) or i(Xp)).8 Compared to the general population, females with Turner syndrome have a three times higher risk of early death from cardiovascular disease.1 The incidence and severity of congenital heart disease are higher in females with monosomy X compared to those with mosaicism or other X chromosome abnormalities.9 This difference may be attributable to unknown gene(s) located on Xp, which has been found to be involved in normal cardiovascular development of the aortic valve and aortic arch.10 The absence of a second X chromosome has been linked to increased atherogenic lipids, and monosomy for a maternally inherited X chromosome has been associated with increased risk of visceral fat accumulation and dyslipidemia.11
Congenital structural heart abnormalities are present in up to 50% of females with Turner syndrome (45, X), and are typically left-sided.1 These include bicuspid aortic valve (15–30%), coarctation of the aorta (7–18%), mitral valve abnormalities including mitral prolapse and/or regurgitation (21%), hypoplastic left heart syndrome (2%), and PAPVR (3.8–13%).1,12,13 The left-sided lesions seen in this patient are consistent with the prior literature.
Both pediatric and adult females with Turner syndrome have an increased likelihood of electrocardiographic abnormalities.14 Reported abnormalities include a shortened PR interval, left posterior fascicular block, right axis deviation, T-wave changes, and accelerated atrioventricular conduction.15 Females with Turner syndrome also have significantly longer QT intervals when compared to age-matched controls.11,13 A prolonged QT interval is associated with ventricular tachyarrhythmias, specifically torsades de pointes, and predisposition to sudden cardiac death in the general population.2 Thus, females with Turner syndrome may have a higher risk for ventricular arrhythmias if they have a prolonged QTc.1 While SVT has been previously described in one adult with Turner syndrome, this is the first report of SVT in a neonate with Turner syndrome.3 To date, there are no known associations between Turner syndrome and the development of atrial flutter with or without SVT. Although atrial arrhythmias secondary to right atrial dilation from left to right shunting in PAPVR are possible, our patient did not have right atrial dilation from the single anomalous pulmonary venous connection. Therefore, our patient’s structural heart defects were not likely to account for the arrhythmias seen.
In conclusion, we describe the novel combination of a neonate with Turner syndrome, PAPVR, and mildly hypoplastic left ventricle, presenting with atrial flutter followed by SVT. Early and precise investigation of such cardiac abnormalities is important to reduce morbidity and mortality, especially given their higher risk of cardiovascular disease relative to the general population.
Lead author biography

Dr Meena Bolourchi is an assistant professor of Pediatrics at Boston University and a general pediatric cardiologist at Boston Medical Center and Boston Children’s Hospital. She completed her fellowship in Pediatric Cardiology at Columbia University in 2019 and her residency in Pediatrics at the University of California, Irvine in 2016. She obtained her medical doctorate degree from Tufts University School of Medicine in 2013. She is passionate about the diagnosis and management of pediatric arrhythmias, particularly in children with congenital heart disease.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing these cases and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient's legal guardian in line with COPE guidelines.
Conflict of interest: None declared.
Funding: None declared.
Data availability
No new data were generated or analysed in support of this research.
Supplementary Material
References
- 1.Silberbach M, Roos-Hesselink JW, Andersen NH, Braverman AC, Brown N, Collins RT, et al. ; On behalf of the American Heart Association Council on Cardiovascular Disease in the Young; Council on Genomic and Precision Medicine; and Council on Peripheral Vascular Disease. Cardiovascular health in turner syndrome: a scientific statement from the American Heart Association. Circ Genom Precis Med 2018;11: 10.1161/HCG.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 2.Tse G, Chan YWF, Keung W, Yan BP.. Electrophysiological mechanisms of long and short QT syndromes. Int J Cardiol Heart Vasc 2017;14:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forgosh LB, Conetta DA.. Cardiac assessment in Turner’s syndrome: a case for the inclusion of coronary angiography. J Am Soc Echocardiogr 1992;5:281–284. [DOI] [PubMed] [Google Scholar]
- 4.Turner CJ, Wren C.. The epidemiology of arrhythmia in infants: a population-based study: epidemiology of arrhythmia in infants. J Paediatr Child Health 2013;49:278–281. [DOI] [PubMed] [Google Scholar]
- 5.Srinivasan C, Balaji S.. Neonatal supraventricular tachycardia. Indian Pacing Electrophysiol J 2019;19:222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ban J-E.Neonatal arrhythmias: diagnosis, treatment, and clinical outcome. Korean J Pediatr 2017;60:344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Texter KM, Kertesz NJ, Friedman RA, Fenrich AL.. Atrial flutter in infants. J Am Coll Cardiol 2006;48:1040–1046. [DOI] [PubMed] [Google Scholar]
- 8.Cui X, Cui Y, Shi L, Luan J, Zhou X, Han J.. A basic understanding of Turner syndrome: incidence, complications, diagnosis, and treatment. Intractable Rare Dis Res 2018;7:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gotzsche CO, Krag-Olsen B, Nielsen J, Sorensen KE, Kristensen BO.. Prevalence of cardiovascular malformations and association with karyotypes in Turner’s syndrome. Arch Dis Childhood 1994;71:433–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bondy C, Bakalov VK, Cheng C, Olivieri L, Rosing DR, Arai AE.. Bicuspid aortic valve and aortic coarctation are linked to deletion of the X chromosome short arm in Turner syndrome. J Med Genet 2013;50:662–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bondy CA.Congenital cardiovascular disease in Turner syndrome: aortic aneurysm, aortic coarctation, aortic dissection. Congenital Heart Disease 2008;3:2–15. [DOI] [PubMed] [Google Scholar]
- 12.Dulac Y, Pienkowski C, Abadir S, Tauber M, Acar P.. Cardiovascular abnormalities in Turner’s syndrome: what prevention? Arch Cardiovasc Dis 2008;101:485–490. [DOI] [PubMed] [Google Scholar]
- 13.Poprawski K, Michalski M, Ławniczak M, Łacka K.. Cardiovascular abnormalities in patients with Turner syndrome according to karyotype: own experience and literature review. Pol Arch Med Wewn 2009;119:453–460. [PubMed] [Google Scholar]
- 14.Bondy CA, Ceniceros I, Van PL, Bakalov VK, Rosing DR.. Prolonged rate-corrected QT interval and other electrocardiogram abnormalities in girls with Turner syndrome. Pediatrics 2006;118:e1220–5. [DOI] [PubMed] [Google Scholar]
- 15.Bondy CA, Van PL, Bakalov VK, Sachdev V, Malone CA, Ho VB. et al. Prolongation of the cardiac QTc interval in Turner syndrome. Medicine 2006;85:75–81. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analysed in support of this research.