Abstract
Background:
Awareness for the importance of psychological and spiritual needs in patients with terminal diseases has increased in recent years, but randomized trials on the effects of psychosocial interventions are still rare.
Aim:
To investigate the efficacy of the “Song of Life” music therapy intervention regarding the emotional and psycho-spiritual dimensions of quality of life.
Design:
Patients were randomly assigned to either “Song of Life” or a relaxation intervention. “Song of Life” is a novel three-session music therapy intervention working with a biographically meaningful song. Primary outcome was the improvement in psychological quality of life. Secondary outcomes included spiritual well-being, ego-integrity, momentary distress, and global quality of life and the explorative assessment of treatment satisfaction (patient and family member version). Intention-to-treat analysis was conducted including adjustment for multiple testing in secondary outcomes.
Setting/participants:
Between December 2018 and August 2020, 104 patients receiving specialized palliative care were recruited from two palliative care wards.
Results:
No significant differences were found regarding psychological and global quality of life, but “Song of Life” participants reported significantly higher spiritual well-being (p = 0.04) and ego-integrity (p < 0.01), as well as lower distress (p = 0.05) than patients in the control group. Both patients’ and family members’ treatment satisfaction was higher after “Song of Life” with large between-group effect sizes on items asking for meaningfulness (d = 0.96) and importance (d = 1.00).
Conclusions:
Our findings provide evidence that “Song of Life” is an effective and meaningful biographical music therapy intervention to facilitate psycho-spiritual integration in terminally ill patients.
Trial Registration:
German Clinical Trials Register (DRKS)—DRKS00015308 (date of registration: September 7th 2018).
Keywords: Music therapy, palliative care, cancer, randomized controlled trial, end-of-life, quality of life, spiritual well-being, distress, ego-integrity
What is already known about the topic:
Patients nearing the end of life report high needs for emotional and spiritual support.
Although the use of psychosocial interventions including life review and creative arts-based techniques is immensely valued in clinical practice, recent guidelines, reviews, and reports have repeatedly called for high-quality studies on their efficacy.
What this paper adds:
Findings show that biographical music therapy can effectively facilitate psycho-spiritual integration of past life events.
The intervention was further effective in reducing patients’ momentary distress and was perceived as meaningful and important by both patients and family members.
Implications for practice, theory or policy:
Together with previous findings, music therapy has been shown to be effective with regard to a number of clinically relevant outcomes including pain, quality of life, and spiritual well-being.
The present study therefore marks an important step towards an evidence-based rationale for the use of music therapy in palliative care.
The “Song of Life” intervention should be recommended to address emotional and existential needs in terminally ill patients nearing the end of life.
Background
The diagnosis and course of a terminal disease is one of the most distressing life events with a detrimental impact on the physical, emotional, spiritual, and social well-being of the individual and their relatives. 1 While medical interventions effectively treat physical symptoms like pain, 2 the mission of palliative care is to provide holistic support of patients on all levels of well-being. 3 For instance, one third of palliative care patients suffer from depression, adjustment, or anxiety disorders. 4 Therefore, psychosocial interventions have emerged to specifically address emotional difficulties and spiritual concerns regarding meaning in life, 5 including cognitive-behavioral therapy, mindfulness, life review or meaning-centered interventions, and creative arts-based therapies.6–8 Research on these treatments provides evidence for improvements in depression and quality of life, particularly in advanced cancer patients.9–12 However, the majority of these interventions were designed for patients in non-final stages of the disease requiring a session number that is hard to achieve in patients nearing the end of life. Palliative care settings often deal with unique conditions necessitating respective adjustments in intervention protocols. 13
A recent meta-analysis summarized studies using brief interventions with four sessions or less showing improvements in quality of life and reductions in emotional and existential distress. 14 Most of these studies focused on life review techniques or music therapy. The common therapeutic focus of life review interventions (e.g. dignity therapy15–17) lies on the patient’s biography and the attempt to create a legacy,7,18 as generativity and ego-integrity (i.e. achieving a sense of meaning and acceptance of past life events) were postulated as important developmental tasks at the end of life.19,20 While a recent meta-analysis provided evidence for improvements in psychological well-being, efficacy trials revealed inconsistent findings concerning quality of life and dignity. 21
Creative arts therapies offer an alternative way for terminally ill patients to regulate emotions and integrate life experiences on a psycho-spiritual level. 22 Music therapy has been a substantial part of palliative care since its beginnings 23 and aims at the improvement of quality of life by alleviating physical and emotional burden as well as through enabling communication and spiritual experiences. 24 Common definitions of music therapy emphasize the importance of the therapeutic relationship combined with musical and verbal techniques, and thereby contrast music listening interventions which do not require the presence of a trained therapist. 25 Music therapy techniques encompass receptive (e.g. music and imagery), creative (e.g. songwriting), recreative (e.g. instrument playing), and combined (e.g. musical life review) methods, 26 which usually are customized to the individual’s needs. 27 Previous trials on the efficacy of music therapy in palliative care reported beneficial effects regarding the improvement of quality of life, general well-being,28,29 and spiritual well-being,30,31 as well as the reduction of pain 32 and anxiety. 33 No study has systematically evaluated biographical music therapy in a clinical trial in palliative care yet.
Therefore, the aim of the present study was to investigate the efficacy of the newly developed, pilot-tested 34 biographical music therapy technique “Song of Life” (SOL) with palliative care patients. Working with a biographically meaningful song, SOL integrates elements of life review interventions and creative arts therapies. Hence, we hypothesized the SOL to have more beneficial effects on the psychological and spiritual domain of quality of life than a non-specific psychosocial control treatment.
Methods
Study design
This multicenter randomized controlled trial compared the effects of the SOL music therapy intervention plus usual care as the experimental group with a relaxation intervention (RELAX) plus usual care as the control group in a parallel design. Patients in both groups participated in three sessions of 20–30 min duration. We additionally recruited family members for participation in an assessment of treatment satisfaction. The trial was preregistered at the German Clinical Trials Registry (DRKS00015308) and received approval by the local ethics committees. Methods and procedures have been published in a study protocol. 35
Setting
Study sites were the University Palliative Care Unit at St. Vincentius Hospital, Heidelberg University Hospital, Germany, and the Interdisciplinary Palliative Care Unit at the University Medical Center of the Johannes Gutenberg University of Mainz, Germany.
Randomization, masking, and blinding
Randomization to one of the two study arms was based on a computer-based block randomization sequence (block size = 8) stratified by study site, which was created by a researcher not involved in recruitment, assessment, or treatment. Sequentially numbered opaque envelopes were opened after the patient had provided informed consent and completed baseline assessment. Adhering to recommendations regarding blinding of participants, we (a) used an active control group without the patient knowing which one was the experimental group and (b) implemented an expectancy measure at baseline, 36 assessed via the item “I expect the study intervention to be helpful to me” (agreement, 1–5). While patients were blind to the study hypothesis, blinding of therapists and outcome assessors was not feasible.
Participants
Patients from these palliative care wards were included if they (a) received palliative treatment according to OPS 8-982/OPS 8-98e (German modification of International Classification of Procedures in Medicine; ICPM) or had an estimated life expectancy of <12 months, 37 (b) were ⩾18 years old, and (c) were able to provide informed consent. Patients were excluded if they (d) did not speak German language, (e) had a clinical estimation of life expectancy <1 week, or (e) showed cognitive or auditory impairments, or psychiatric symptoms. Patients were asked to name a family member or another close person to be included in an evaluation of treatment satisfaction. Family members were included if they (a) were ⩾18 years old and (b) spoke German language.
Sampling and recruitment
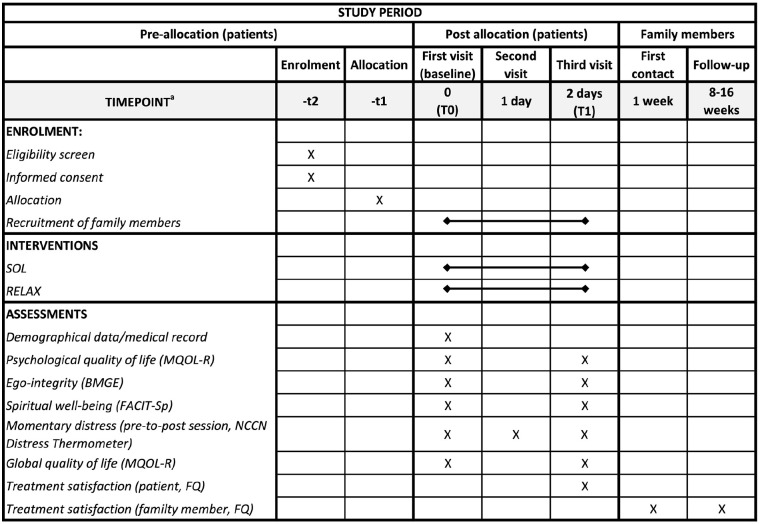
Based on the medical record and information from the physician, eligible patients from the two palliative care units were contacted at bedside consecutively between December 2018 and August 2020. All patients were informed about the study goals, procedures, risks, and benefits and were asked to provide written informed consent. Family members were contacted after allocation of the patient to one of the interventions and were also asked to provide informed consent before inclusion in the study (Figure 1).
Figure 1.
Figure 2 SPIRIT figure: schedule of enrolment, interventions and assessments.
SPIRIT: standard protocol items: recommendations for interventional trials; SOL: “Song of Life” music therapy; RELAX: relaxation intervention; MQOL-R: McGill quality of life questionnaire–revised); BMGE: brief measure of generativity and ego-integrity; FACIT-Sp: functional assessment of chronic illness therapy-spiritual well-being; NCCN: national comprehensive cancer network; FQ: feedback questionnaire.
aDeviations from the schedule were possible.
Interventions
The SOL intervention was a new pilot-tested 34 music therapy technique, in which therapist and patient explored and identified a biographically meaningful and emotionally arousing song in the first session. This song was played live to the patient in the second session by the therapist in a lullaby style (i.e. 3/4 or 6/8 rhythm, slow tempo) with guitar or e-piano and voice, while the session was audio-recorded. A CD or flash drive containing the edited recording was handed over to the patient as a possible legacy in the third session. Both patient and therapist listened to the recording and reflected on feelings and memories, guided by pre-defined questions. Conversations in the last session were again audio-recorded.
Sessions in the control group consisted of three standardized relaxation interventions focusing on (a) muscle relaxation, (b) breathing, and (c) imaginary journey, plus a brief inquiry at the end of each session. Relaxation and mindfulness exercises were chosen as they proved to be feasible, safe, and potentially effective in seriously ill patients, 10 but were non-specific with regard to psycho-spiritual integration processes targeted in the SOL intervention. Hence, exercises did not contain any biographical, spiritual, or musical content, and were delivered in person by the study therapists. Detailed intervention manuals are presented in Appendix A.
In both groups, sessions were preferably carried out on three consecutive days, but deviations from this schedule were possible (e.g. for organizational reasons or if wished by the patient). The two study therapists were trained music therapists with a wide range of experience and were employed at the two participating palliative care wards. The study therapists participated in a 36-h training program conveying all intervention procedures. Moreover, study therapists were asked to rate their perception of adherence to the intervention protocol for each patient and of the musical realization of the SOL (e.g. using rhythm, tempo, and dynamics in accordance with the training and manual; see Appendix A) on a scale from 1 (“not at all”) to 5 (“very good”). Moreover, audio recordings in the experimental group (sessions 2 and 3) were rated by a research assistant for protocol adherence (e.g. interview topics covered; see Appendix A) on a self-developed treatment integrity scale (1–5). Further, study therapists received supervision by the principal investigator after 25%, 50%, and 75% of recruitment completion to maintain high treatment fidelity, where therapists were asked to describe cases, treatment progress, or difficulties and received feedback by the supervisor.
Data collection
After obtaining written informed consent, research staff initiated baseline assessment (T0) of outcome measures listed below and afterwards opened an envelope with the group assignment. Each of the three intervention sessions contained a pre-to-post single-item assessment of momentary distress. Post-intervention outcome data (T1) was immediately assessed after session 3.
Family members who provided informed consent completed a brief evaluation of treatment satisfaction after the intervention (T1) and again after 8–16 weeks (T2) either in person or by phone. The rationale of these follow-up assessments was to gather indirect information on the endurance of treatment effects, as previous trials showed that time spans for patient outcome assessments of more than 1 week were not feasible in palliative care research. 31 Figure 1 gives an overview of the assessment procedures.
Outcome measures
The working mechanism of the SOL intervention was assumed to include the emotional and spiritual processing and integration of past life events. Outcomes have been chosen in accordance with this assumption and a detailed rationale for the selection of study outcomes can be found in the study protocol. 35
The primary study outcome was the pre-to-post change (T0-T1) in psychological quality of life (range: 0–10) as measured by the psychological subscale of the validated McGill Quality of Life Questionnaire – Revised (MQOL-R), 38 which contains four items asking for anxiety and depression in the past 2 days.
Secondary outcomes included the 5-item ego-integrity subscale (1–5) of the validated Brief Measure of Generativity and Ego-Integrity 20 (BMGE) for the assessment of acceptance and the sense of meaning regarding one’s past life. Changes in non-religious aspects of spiritual well-being were measured by the validated 8-item meaning/peace-scale (0–32) of the Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being (FACIT-Sp), which is commonly used in palliative care research.39,40 Due to the intervention duration of 3 days, the item time frame was reduced from 7 to 3 days. Moreover, we assessed patient’s momentary distress before and after each session by use of the modified version of the validated single-item (0–10) NCCN Distress Thermometer asking for acute distress.41,42 For consistency with other outcome measures, we analyzed the two distress scores before the first session and after the last. The MQOL-R’s single item (0–10) on global quality of life during the past 2 days additionally served as a secondary endpoint. 38
Outcome assessment was complemented by modified versions of the Feedback Questionnaire (FQ), in the patient 16 and family member 43 version. The FQ is a non-validated retrospective measure frequently used in research on biographical interventions in palliative care. Both versions used eight items (agreement from 1 to 5) to cover the perception of treatment satisfaction (T1: patients and family members, T2: family members only). All questionnaires were delivered by research assistants who were not involved in the treatment process. The timing of assessments is displayed in Figure 1.
Statistical analyses
A priori calculations with G*Power 44 assuming a medium-sized effect of Cohen’s d = 0.50 45 on the primary outcome, statistical power of (1–ß) = 0.8, a type-I error probability of α = 0.05, a correlation between covariate and outcome of ρ = 0.6, and an attrition rate of 25% revealed an optimal sample size of N = 104 patients for this study. The rationale for the estimation of parameters has been discussed in the study protocol. 35
Hypotheses were tested by intention to treat 46 in the statistical environment R. 47 We first calculated analyses of covariance (ANCOVA) with a multiply imputed dataset (MI), using the baseline score as a covariate, treatment and study site 48 as fixed factors, and the post-intervention score as the outcome. We created 20 imputations and combined the statistical results using the R package “mice.” 49 Effect sizes (Cohen’s d) and 95% confidence intervals (CI) were computed according to Morris’ 50 formula for pretest-posttest-control-group designs and were visualized with the funnel plot function in the “metaphor” 51 package. Next, sensitivity analysis with all available data (AAD) was calculated by multilevel modeling using the “lme4” package. 52 We chose to conduct analyses with both ANCOVA (MI) and multilevel modeling (AAD) as different approaches to handle missing data and expected similar results. Parameters were obtained via restricted maximum likelihood (REML) estimation. We computed a random-intercept model including the pre- and post-intervention scores as the outcome, and time, treatment, time × treatment, and study site as fixed factors. Concerning the analyses of secondary outcomes, we accounted for the false discovery rate (FDR) in multiple comparisons employing the Benjamini-Hochberg correction and report adjusted p-values. 53 Both α and the FDR were set on 0.05. Group differences on the FQ were exploratively analyzed on an item level 16 using Cohen’s d and 95 % CIs calculated with the “effectsize” 54 package, as this non-validated measure does not allow for calculation of a composite score.
Results
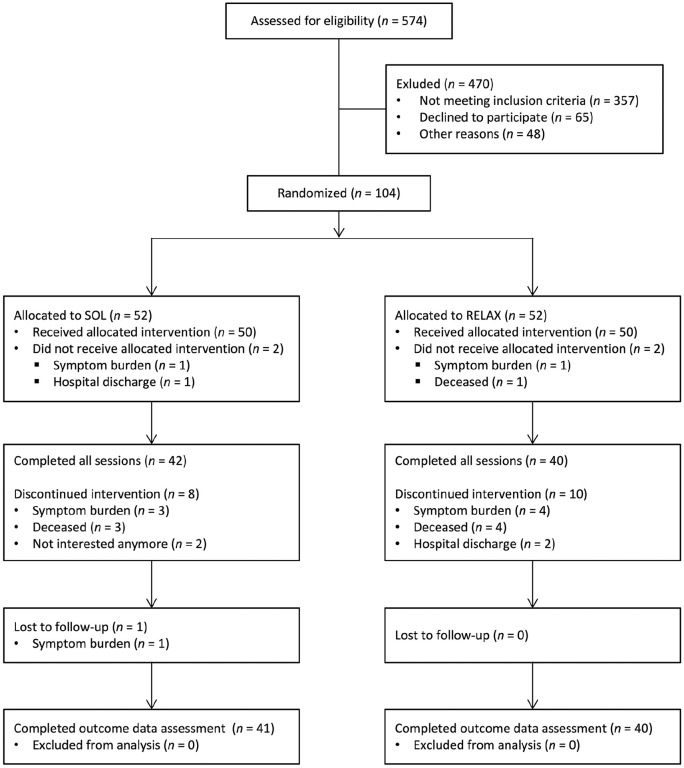
Of the 574 patients assessed for eligibility between December 2018 and August 2020, N = 104 consented to participate and were randomly assigned to either SOL (n = 52) or RELAX (n = 52). Among those included, n = 100 patients (98.0%) completed session 1, n = 89 completed session 2 (85.6%), and n = 82 (78.8%) completed the entire intervention protocol. Eighty-one patients (77.9%) provided complete outcome data, hence, the attrition rate in the present study was 22.1%. The patient flow chart is shown in Figure 2.
Figure 2.
Patient flow chart.
SOL: “Song of Life” music therapy; RELAX: relaxation intervention.
The majority of patients was female (n = 77, 74.0%) and all but n = 2 patients were primarily diagnosed with advanced cancer (n = 102, 98.1%). The mean age was M = 66.1 years (SD = 12.0). As Table 1 shows, study groups were comparable with regard to age, sex, diagnosis, functional status, and treatment expectancy. On average, therapists rated their subjective overall adherence to the treatment protocols at 3.52 (SD = 0.82) in the experimental group and 3.74 (SD = 0.94) in the control group. In the experimental group, the musical adherence in session 2 received an average rating of M = 3.50 (SD = 0.90) by the therapists and of M = 4.47 (SD = 0.67) by the research assistant. Adherence to the interview guidelines in session 3 (SOL) was rated 3.36 (0.90) by the research assistant. The majority of chosen songs were associated with a meaningful life phase, close relationships, or important life event, while other songs represented the lifelong companionship and consolation through music in the patient’s biography.
Table 1.
Baseline sample characteristics.
| Characteristic | SOL | RELAX |
|---|---|---|
| Participants per site (n, %) | ||
| Study site 1 | 24 (23.1%) | 24 (23.1%) |
| Study site 2 | 28 (26.9%) | 28 (26.9%) |
| Age (M, SD, years) | 67.75 (11.5) | 64.46 (12.37) |
| Sex (n, % female) | 41 (78.8%) | 36 (69.2%) |
| Cancer type (%, n) | ||
| Gastrointestinal | 30.8% (16) | 26.9% (14) |
| Gynecologic | 28.8% (15) | 26.9% (14) |
| Skin | 9.6% (5) | 9.6% (5) |
| Lymphatic | 5.8% (3) | 9.6% (5) |
| Thoracic | 9.6% (5) | 15.4% (8) |
| Other | 13.5% (7) | 9.6% (5) |
| Non-cancer | 1.9% (1) | 1.9% (1) |
| Karnofsky performance status scale (M, SD, 0–100) | 42.88 (15.51) | 48.46 (20.71) |
| Treatment expectancy (M, SD, 1–5) | 3.74 (0.69) | 3.81 (0.60) |
SOL: “Song of Life” music therapy (experimental group); RELAX: relaxation intervention (control group); M: mean; SD: standard deviation.
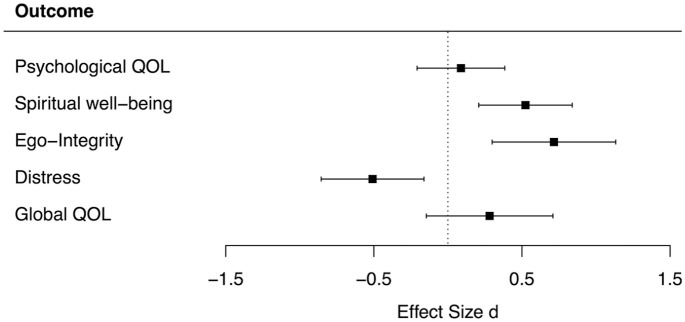
ANCOVA showed no statistically significant differences between groups in the primary outcome psychological quality of life (F = 0.13, p = 0.72, Table 2). With regard to secondary outcomes, patients reported significantly higher spiritual well-being (F = 5.53, p = 0.04) and ego-integrity (F = 16.03, p < 0.01) after SOL than after RELAX. Effect sizes were medium to large for both spiritual well-being (d = 0.52) and ego-integrity (d = 0.72, Figure 3). Further, momentary distress was significantly lower after SOL (F = 4.49, p = 0.05), with a medium effect size of d = −0.51. Findings with regard to global quality of life showed a small between-group effect favoring the SOL (d = 0.28), but differences were not statistically significant (F = 0.71, p = 0.40). Sensitivity analyses using multilevel modeling with AAD yielded identical test results (Table 2).
Table 2.
Results for primary and secondary outcomes.
| Descriptive statistics and effect sizes (AAD) | ANCOVA (MI) | MLM (AAD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SOL | RELAX | d (CI) a | |||||||||
| N | M | SD | N | M | SD | F | p b Value | b | p b Value | ||
| Psychological quality of life (MQOL-R, range = 0–10) | |||||||||||
| Baseline (T0) | 52 | 5.22 | 2.25 | 52 | 5.50 | 2.74 | |||||
| Post-intervention (T1) | 41 | 5.46 | 2.07 | 40 | 5.51 | 2.44 | 0.09 (−0.21, 0.38) | 0.13 | 0.721 | 0.07 | 0.859 |
| Meaning/peace (FACIT-Sp, range = 0–32) | |||||||||||
| Baseline (T0) | 50 | 20.40 | 4.45 | 50 | 22.70 | 4.32 | |||||
| Post-intervention (T1) | 41 | 22.32 | 5.09 | 40 | 22.30 | 5.17 | 0.52 (0.21, 0.84) | 5.53 | 0.039* | 2.45 | 0.006* |
| Ego-integrity (BMGE, range = 1–5) | |||||||||||
| Baseline (T0) | 51 | 3.20 | 0.52 | 52 | 3.34 | 0.66 | |||||
| Post-intervention (T1) | 41 | 3.58 | 0.57 | 40 | 3.29 | 0.59 | 0.72 (0.30, 1.13) | 16.03 | <0.001* | 0.47 | 0.001* |
| Distress (NCCN distress thermometer, range = 0–10) | |||||||||||
| Baseline (T0) | 50 | 5.66 | 2.50 | 50 | 4.82 | 2.54 | |||||
| Post-intervention (T1) | 42 | 3.33 | 2.43 | 40 | 3.78 | 2.54 | -0.51 (-0.86, -0.16) | 4.49 | 0.046* | −1.18 | 0.017* |
| Global quality of life (MQOL-R, range = 0–10) | |||||||||||
| Baseline (T0) | 52 | 4.50 | 2.10 | 52 | 4.92 | 2.46 | |||||
| Post-intervention (T1) | 41 | 5.73 | 2.05 | 40 | 5.50 | 2.32 | 0.28 (-0.15, 0.71) | 0.71 | 0.401 | 0.61 | 0.254 |
SOL: “Song of Life” music therapy; RELAX: relaxation intervention; ANCOVA: analysis of covariance; MLM: multilevel modeling; MI: multiple imputation; AAD: all available data; M: mean; SD: standard deviation; MQOL-R: McGill quality of life questionnaire–revise); FACIT-Sp: functional assessment of chronic illness therapy-spiritual well-Being; BMGE: brief measure of generativity and ego-integrity; NCCN: national comprehensive cancer network.
Effect size variant of Cohen’s d for pretest-posttest-control group designs. 55
p-Values were adjusted by the Benjamini-Hochberg correction in secondary outcomes. 48
Statistically significant (p < 0.050).
Figure 3.
Effect sizes and 95% confidence intervals for primary and secondary outcomes.
QOL: quality of life; d: effect size according to Morris; 50 positive effect size indicates higher increase in SOL than in RELAX.
Table 3 lists results of the explorative analyses for the FQ. Overall, patients and family members reported a positive impact of both interventions. Effect sizes between groups were medium to large or large, all favoring SOL over RELAX. In the patient version, large effect sizes were found on the items “Participating in the intervention made me feel that life was more meaningful” (d = 0.96) and “. . . was important to me” (d = 1.00). For family members, large between-group effect sizes were identified for the items “. . . made me feel something lasts from the patient” (d = 2.03) and “. . .will be helpful and comforting to our family” (d = 1.14), both immediately after the intervention (T1) and at follow-up (T2).
Table 3.
Explorative results for feedback questionnaire.
| Participating in the intervention… | Post-intervention (T1, AAD) | Follow-up (T2, AAD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SOL | RELAX | SOL | RELAX | |||||||
| Patient evaluation | n | M (SD) | n | M (SD) | d [95% CI] | n | M (SD) | N | M (SD) | d [95% CI] |
| . . . was helpful to me | 40 | 4.30 (0.69) | 40 | 3.80 (0.88) | 0.63 [0.18, 1.08] | – | – | – | ||
| . . . was satisfactory | 40 | 4.55 (0.71) | 40 | 3.98 (0.80) | 0.76 [0.30, 1.21] | – | – | – | ||
| . . . made me feel that life was more meaningful | 40 | 3.60 (0.98) | 40 | 2.58 (1.15) | 0.96 [0.49, 1.42] | – | – | – | ||
| . . . met my expectations | 36 | 4.22 (0.72) | 39 | 3.64 (0.93) | 0.69 [0.23, 1.16] | – | – | – | ||
| . . . was or will be of help to my family | 39 | 3.56 (0.99) | 39 | 2.69 (1.24) | 0.78 [0.32, 1.24] | – | – | – | ||
| . . . helped me to accept the way things are | 40 | 3.70 (0.79) | 40 | 3.05 (1.11) | 0.68 [0.22, 1.13] | – | – | – | ||
| . . . was important to me | 40 | 4.35 (0.70) | 40 | 3.53 (0.93) | 1.00 [0.53, 1.47] | – | – | – | ||
| . . . is something I would recommend to others | 40 | 4.70 (0.52) | 39 | 4.33 (0.58) | 0.67 [0.22, 1.12] | – | – | – | ||
| Family member evaluation | ||||||||||
| . . . was helpful to the patient | 23 | 4.52 (0.59) | 19 | 3.58 (0.90) | 1.26 [0.59, 1.93] | 17 | 4.59 (0.51) | 9 | 3.67 (0.87) | 1.42 [0.52, 2.32] |
| . . . was satisfactory to the patient | 23 | 4.61 (0.50) | 19 | 3.63 (1.01) | 1.26 [0.60, 1.93] | 16 | 4.38 (0.50) | 9 | 3.44 (1.13) | 1.19 [0.31, 2.08] |
| . . . made the patient feel life was meaningful | 23 | 3.43 (1.12) | 20 | 2.60 (1.14) | 0.74 [0.12, 1.36] | 16 | 3.13 (1.02) | 9 | 2.00 (1.00) | 1.11 [0.23, 1.98] |
| . . . helped to alleviate the patient’s suffering | 22 | 4.23 (0.75) | 20 | 3.20 (0.89) | 1.25 [0.58, 1.91] | 17 | 4.12 (0.70) | 9 | 3.22 (1.20) | 1.00 [0.14, 1.85] |
| . . . was helpful to me | 23 | 3.78 (1.04) | 19 | 2.95 (1.31) | 0.71 [0.09, 1.34] | 17 | 3.76 (1.15) | 9 | 2.44 (1.24) | 1.12 [0.25, 1.99] |
| . . . will be helpful and comforting to our family | 22 | 3.86 (1.04) | 19 | 2.53 (1.31) | 1.14 [0.48, 1.81] | 17 | 3.82 (1.19) | 9 | 2.00 (1.12) | 1.57 [0.65, 2.49] |
| . . . made me feel something lasts from patient | 23 | 3.91 (1.16) | 19 | 1.89 (0.74) | 2.03 [1.28, 2.78] | 17 | 3.82 (1.07) | 9 | 1.67 (0.87) | 2.14 [1.13, 3.14] |
| . . . is something I would recommend to others | 23 | 4.83 (0.39) | 20 | 4.15 (0.88) | 1.02 [0.39, 1.66] | 17 | 4.88 (0.33) | 9 | 4.22 (0.83) | 1.20 [0.32, 2.07] |
Range = 1–5 (agreement); SOL: “Song of Life” music therapy; RELAX: relaxation intervention; AAD: all available data; M: mean; SD: standard deviation; d: effect size Cohen’s d; CI: confidence interval. 56
Discussion
Main findings/results of the study
Overall, our findings provide evidence that the innovative SOL technique has a positive impact on emotional and spiritual components of palliative care patients’ quality of life. In particular, we found significant treatment benefits with medium effect sizes regarding higher spiritual well-being and ego-integrity in the SOL group. Since patients nearing the end of life name existential fears regarding meaning in life as a fundamental challenge, 55 these results suggest that SOL provides relief through facilitating the experience of a sense of connectedness with life and oneself. Corroborating research on other life review techniques, the present study adds to the promising potential of biographical interventions with terminally ill patients pointing to personal meaningful music as a valuable legacy. In addition, the significant reduction of distress through SOL music therapy hints at an acute relief of burden as well. Patients at the end of life commonly report a high level of psychological distress involving unpleasant emotional experiences, so even a short-term decrease might be of clinical importance to alleviate the patients’ suffering.57,58 Similar to other studies investigating psychosocial interventions with advanced cancer patients, we found no significant differences between the study groups with regard to more general outcomes. 16 As our primary outcome contained items on general depression and anxiety, the measurement might not depict the actual content and goals of SOL (i.e. psycho-spiritual integration processes). Additionally, without a third study arm receiving usual care only, we cannot make conclusions about the effects of either SOL or RELAX on the MQOL-R domains in comparison to no add-on treatment. Further, as patient-reported outcomes may depend on the individual interpretation of items, future research may include external assessments, for example, by clinicians, as well. Regarding the explorative evaluation of treatment satisfaction (FQ), patients and family members in the SOL group rated the intervention more favorably on all items. Single-item effect sizes point to a profound personal relevance and perceived meaningfulness of the SOL. Family members, in particular, considered SOL benefits to be enduring and helpful to the whole family. The large between-groups effect sizes at both T1 and T2 on the item “. . . made me feel something lasts from the patient” highlights the important difference that the created legacy (SOL recording) might have made for the (bereaved) family member.
Limitations
With regard to the selection of an appropriate comparator for the experimental intervention, the Declaration of Helsinki demands the effects of a new intervention to be tested against those of the best proven intervention. 59 Usual-care-only groups may therefore be considered unethical in palliative care research and may also threaten the internal validity of a study through attention bias and lack of blinding. 36 Therefore, we decided to compare two active psychosocial therapies which may partially explain the non-significant findings regarding psychological and global quality of life. Moreover, the generalizability of findings may be limited as 74% of participants were female. Ad-hoc analysis of sex differences in the observed treatment effects showed that effect sizes for the increase in spiritual well-being were larger in women while the observed distress reductions were more pronounced in men. This finding is consistent with previous research suggesting that women may be more open to development in gratitude and compassion, while men may have a stronger disease- or health-related focus. 58 Further, the patient assessment only contained two measurement times, as long-term assessment plans were proven to be unfeasible considering an average hospital stay of less than 2 weeks.31,60 The present attrition rate of 22.1% is comparable to other studies and we addressed the issue of missing data integrating findings from different statistical approaches. 61 We implemented the T2 family member follow-up to evaluate the endurance of effects, but also faced recruitment challenges and high attrition rates increasing the likelihood of selection bias in these results. At T2 among the family members that participated, only 28.6% of patients were alive. Of note, there was a great amount of family members who declined to participate at T2 due to the recent loss of their loved one.
What this study adds
Findings from this multicenter RCT suggest that SOL music therapy can serve as an effective psychosocial treatment in palliative care to facilitate psycho-spiritual integration and reduce distress in patients nearing the end of life. Future studies may continue to explore optimal study outcomes and should address the importance of patient characteristics (e.g. sex, cultural background) in order to tailor biographical interventions to the individual’s situation and needs.
Supplemental Material
Supplemental material, sj-docx-1-pmj-10.1177_02692163211010394 for “Song of Life”: Results of a multicenter randomized trial on the effects of biographical music therapy in palliative care by Marco Warth, Friederike Koehler, Martin Brehmen, Martin Weber, Hubert J Bardenheuer, Beate Ditzen and Jens Kessler in Palliative Medicine
Acknowledgments
We would like to thank the study therapists Gisela Platzbecker and Sung-Eun Lee and the research assistants Theresa Schöche and Natalie Hess for their outstanding commitment in this study. We would also like to thank Josien van Kampen and Corina Aguilar-Raab who contributed to the development of intervention protocols and to the therapist training. Finally, we would like to thank our study participants and their families who put their time and effort into this project.
Footnotes
Author contributions: MWA and FK analyzed the data and drafted the manuscript. JK, HJB, MWE and BD contributed significantly to the design and conception of the study. MB and FK collected data. MWA, FK, MWE, MB, HJB, BD, and JK critically revised the present version of the manuscript. MWA, FK, MWE, MB, HJB, BD, and JK gave final approval of the version to be published. All authors declare that they had full access to the data in the study and accept responsibility to submit for publication.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study received funding by the “H.W. & J. Hector Stiftung” and by “Sonnen-Blau. Gemeinnützige Morgott-Schupp-Stiftung für frühkindliche Erziehung und Palliativversorgung.”
Data management and patient consent: This study was conducted in accordance with the Declaration of Helsinki and the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. The trial was approved by the Ethics Committee of the Medical Faculty of Heidelberg University on July 5th 2018 (S-398/2018) and by the Landesärztekammer Rheinland-Pfalz on August 30th 2018 (2018–13496). Participants were only included if they provided written informed consent.
Disclosure of stakeholder investments (CONSORT SPI extension): MW developed the SOL intervention (together with Josien van Kampen) and was also involved in the design, analysis, and reporting of the trial. He was not involved in the assessments and study therapies.
ORCID iD: Marco Warth  https://orcid.org/0000-0003-3277-5516
https://orcid.org/0000-0003-3277-5516
Data management and sharing: The dataset for this study is accessible in the heiDATA repository under the following identifier: https://doi.org/10·11588/data/Z4XZQ7.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Holland JC, Breitbart WS, Jacobsen PB, et al. Psycho-oncology. New York: Oxford University Press, 2010. [Google Scholar]
- 2. Potter J, Hami F, Bryan T, et al. Symptoms in 400 patients referred to palliative care services: prevalence and patterns. Palliat Med 2003; 17: 310–314. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. WHO definition of palliative care; http://www.who.int/cancer/palliative/definition/en (2015, accessed 30 April 2015).
- 4. Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011; 12: 160–174. [DOI] [PubMed] [Google Scholar]
- 5. Rodin G. Research on psychological and social factors in palliative care: an invited commentary. Palliat Med 2013; 27: 925–931. [DOI] [PubMed] [Google Scholar]
- 6. Kumar S, Morse M, Zemenides P, et al. Psychotherapies for psychological distress in the palliative care setting. Psychiatr Ann 2012; 42: 133–137. [Google Scholar]
- 7. Teo I, Krishnan A, Lee GL. Psychosocial interventions for advanced cancer patients: a systematic review. Psycho Oncol 2019; 28: 1394–407. [DOI] [PubMed] [Google Scholar]
- 8. Rodin G, An E, Shnall J, et al. Psychological interventions for patients with advanced disease: implications for oncology and palliative care. J Clin Oncol 2020; 38: 885–904. [DOI] [PubMed] [Google Scholar]
- 9. Uitterhoeve RJ, Vernooy M, Litjens M, et al. Psychosocial interventions for patients with advanced cancer-a systematic review of the literature. Br J Cancer 2004; 91: 1050–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zimmermann FF, Burrell B, Jordan J. The acceptability and potential benefits of mindfulness-based interventions in improving psychological well-being for adults with advanced cancer: a systematic review. Complement Ther Clin Pract 2018; 30: 68–78. [DOI] [PubMed] [Google Scholar]
- 11. Breitbart W, Rosenfeld B, Pessin H, et al. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. J Clin Oncol 2015; 33: 749–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rodin G, Lo C, Rydall A, et al. Managing Cancer and Living Meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J Clin Oncol 2018; 36: 2422–2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. von Blanckenburg P, Leppin N. Psychological interventions in palliative care. Curr Opin Psychiatry 2018; 31: 389–395. [DOI] [PubMed] [Google Scholar]
- 14. Warth M, Kessler J, Koehler F, et al. Brief psychosocial interventions improve quality of life of patients receiving palliative care: a systematic review and meta-analysis. Palliat Med 2019; 33: 332–345. [DOI] [PubMed] [Google Scholar]
- 15. Martinez M, Arantzamendi M, Belar A, et al. ‘Dignity therapy’, a promising intervention in palliative care: a comprehensive systematic literature review. Palliat Med 2017; 31: 492–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chochinov HM, Kristjanson LJ, Breitbart W, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol 2011; 12: 753–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mai SS, Goebel S, Jentschke E, et al. Feasibility, acceptability and adaption of dignity therapy: a mixed methods study achieving 360 degrees feedback. BMC Palliat Care 2018; 17: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang CW, Chow AY, Chan CL. The effects of life review interventions on spiritual well-being, psychological distress, and quality of life in patients with terminal or advanced cancer: a systematic review and meta-analysis of randomized controlled trials. Palliat Med 2017; 31: 883–894. [DOI] [PubMed] [Google Scholar]
- 19. Erikson JM. The life cycle completed: Extended version with new chapters on the ninth stage of development. New York, NY: W. W. Norton & Company, 1998. [Google Scholar]
- 20. Vuksanovic D, Dyck M, Green H. Development of a brief measure of generativity and ego-integrity for use in palliative care settings. Palliat Support Care 2015; 13: 1411–1415. [DOI] [PubMed] [Google Scholar]
- 21. Xiao J, Chow KM, Liu Y, et al. Effects of dignity therapy on dignity, psychological well-being, and quality of life among palliative care cancer patients: a systematic review and meta-analysis. Psycho Oncol 2019; 28: 1791–802. [DOI] [PubMed] [Google Scholar]
- 22. Salmon D. Music therapy as psychospiritual process in palliative care. J Palliat Care 2001; 17: 142–146. [PubMed] [Google Scholar]
- 23. Munro S, Mount B. Music therapy in palliative care. Can Med Assoc J 1978; 119: 1029–1034. [PMC free article] [PubMed] [Google Scholar]
- 24. McConnell T, Porter S. Music therapy for palliative care: a realist review. Palliat Support Care 2017; 15: 454–464. [DOI] [PubMed] [Google Scholar]
- 25. Bruscia KE. Defining music therapy. 2nd ed. Gilsum, NH: Barcelona Publishers, 1998. [Google Scholar]
- 26. Clements-Cortes A. Development and efficacy of music therapy techniques within palliative care. Complement Ther Clin Pract 2016; 23: 125–129. [DOI] [PubMed] [Google Scholar]
- 27. Koehler F, Martin Z-S, Hertrampf R-S, et al. Music therapy in the psychosocial treatment of adult cancer patients: a systematic review and meta-analysis. Front Psychol 2020; 11: 651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Warth M, Kessler J, Hillecke TK, et al. The effectiveness of receptive music therapy in palliative care: results of a randomized, controlled trial. Nord J Music Ther 2016; 25: 82–83. [Google Scholar]
- 29. Hilliard RE. The effects of music therapy on the quality and length of life of people diagnosed with terminal cancer. J Music Ther 2003; 40: 113–137. [DOI] [PubMed] [Google Scholar]
- 30. Wlodarczyk N. The effect of music therapy on the spirituality of persons in an in-patient hospice unit as measured by self-report. J Music Ther 2007; 44: 113–122. [DOI] [PubMed] [Google Scholar]
- 31. Porter S, McConnell T, Graham-Wisener L, et al. A randomised controlled pilot and feasibility study of music therapy for improving the quality of life of hospice inpatients. BMC Palliat Care 2018; 17: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gutgsell KJ, Schluchter M, Margevicius S, et al. Music therapy reduces pain in palliative care patients: a randomized controlled trial. J Pain Symptom Manag 2013; 45: 822–831. [DOI] [PubMed] [Google Scholar]
- 33. Horne-Thompson A, Grocke D. The effect of music therapy on anxiety in patients who are terminally ill. J Palliat Med 2008; 11: 582–590. [DOI] [PubMed] [Google Scholar]
- 34. Warth M, Kessler J, van Kampen J, et al. ‘Song of Life’: music therapy in terminally ill patients with cancer. BMJ Support Palliat Care 2018; 8(2): 167–170. [DOI] [PubMed] [Google Scholar]
- 35. Warth M, Koehler F, Weber M, et al. “Song of Life (SOL)” study protocol: a multicenter, randomized trial on the emotional, spiritual, and psychobiological effects of music therapy in palliative care. BMC Palliat Care 2019; 18: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Munder T, Barth J. Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychother Res 2018; 28(3): 347–355. [DOI] [PubMed] [Google Scholar]
- 37. Hui D, Nooruddin Z, Didwaniya N, et al. Concepts and definitions for “actively dying,” “end of life,” “terminally ill,” “terminal care,” and “transition of care”: a systematic review. J Pain Asymptom Manag 2014; 47: 77–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cohen SR, Sawatzky R, Russell LB, et al. Measuring the quality of life of people at the end of life: the McGill Quality of Life Questionnaire-Revised. Palliat Med 2017; 31: 120–129. [DOI] [PubMed] [Google Scholar]
- 39. Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 1993; 11: 570–579. [DOI] [PubMed] [Google Scholar]
- 40. Peterman AH, Fitchett G, Brady MJ, et al. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 2002; 24: 49–58. [DOI] [PubMed] [Google Scholar]
- 41. Mehnert A, Müller D, Lehmann C, et al. Die deutsche version des NCCN distress-Thermometers. Zeitschrift für Psychiatrie Psychologie und Psychotherapie 2006; 54: 213–223. [Google Scholar]
- 42. Linehan K, Fennell KM, Hughes DL, et al. Use of the distress thermometer in a cancer helpline context: can it detect changes in distress, is it acceptable to nurses and callers, and do high scores lead to internal referrals? Eur J Oncol Nurs 2017; 26: 49–55. [DOI] [PubMed] [Google Scholar]
- 43. McClement S, Chochinov HM, Hack T, et al. Dignity therapy: family member perspectives. J Palliat Med 2007; 10: 1076–1082. [DOI] [PubMed] [Google Scholar]
- 44. Faul F, Erdfelder EL, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175–191. [DOI] [PubMed] [Google Scholar]
- 45. Cohen J. A power primer. Psychol Bull 1992; 112: 155–159. [DOI] [PubMed] [Google Scholar]
- 46. White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials 2012; 9: 396–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, https://www.R-project.org/ (2018, accessed July 24, 2020). [Google Scholar]
- 48. Feaster DJ, Mikulich-Gilbertson S, Brincks AM. Modeling site effects in the design and analysis of multi-site trials. Am J Drug Alcohol Abuse 2011; 37: 383–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by Chained Equations in R. J Stat Softw 2011; 45: 1–67. [Google Scholar]
- 50. Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods 2008; 11: 364–386. [Google Scholar]
- 51. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010; 36: 1–48. [Google Scholar]
- 52. Bates D, Mächler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Stat Softw 2015; 67: 1–48. [Google Scholar]
- 53. Benjamini Y, Heller R, Yekutieli D. Selective inference in complex research. Philos Trans A Math Phys Eng Sci 2009; 367: 4255–4271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ben-Shachar M, Makowski D, Lüdecke D. Compute and interpret indices of effect size. CRAN R package. 2020. [Google Scholar]
- 55. Grossman CH, Brooker J, Michael N, et al. Death anxiety interventions in patients with advanced cancer: a systematic review. Palliat Med 2018; 32: 172–184. [DOI] [PubMed] [Google Scholar]
- 56. Viechtbauer W. Confidence intervals for the amount of heterogeneity in meta-analysis. Stat Med 2007; 26: 37–52. [DOI] [PubMed] [Google Scholar]
- 57. Kelly B, McClement S, Chochinov HM. Measurement of psychological distress in palliative care. Palliat Med 2006; 20: 779–789. [DOI] [PubMed] [Google Scholar]
- 58. Luna MJ, Ameli R, Sinaii N, et al. Gender differences in psycho-social-spiritual healing. J Womens Health 2019; 28: 1513–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013; 310: 2191–2194. [DOI] [PubMed] [Google Scholar]
- 60. Ostgathe C, Alt-Epping B, Golla H, et al. Non-cancer patients in specialized palliative care in Germany: what are the problems? Palliat Med 2011; 25: 148–152. [DOI] [PubMed] [Google Scholar]
- 61. Hui D, Glitza I, Chisholm G, et al. Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer 2013; 119: 1098–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pmj-10.1177_02692163211010394 for “Song of Life”: Results of a multicenter randomized trial on the effects of biographical music therapy in palliative care by Marco Warth, Friederike Koehler, Martin Brehmen, Martin Weber, Hubert J Bardenheuer, Beate Ditzen and Jens Kessler in Palliative Medicine