ABSTRACT
Background: A safe and effective vaccine against COVID-19 has become a public health priority. However, little is known about the public willingness to accept a future COVID-19 vaccine in China. This study aimed to understand the willingness and determinants for the acceptance of a COVID-19 vaccine among Chinese adults.
Methods: A cross-sectional survey using an online questionnaire was conducted in an adult population in China. Chi-square tests were used to identify differences for various intentions regarding COVID-19 vaccination. The t test was used to identify differences among vaccine hesitancy scores. Multivariable logistic regression was used to analyze the predicated factors associated with the willingness to receive a COVID-19 vaccine.
Results: Of the 3195 eligible participants, 83.8% were willing to receive a COVID-19 vaccine, and 76.6% believed the vaccine would be beneficial to their health; however, 74.9% expressed concerns or a neutral attitude regarding its potential adverse effects. Of the participants, 76.5% preferred domestically manufactured vaccines and were more willing to be vaccinated than those who preferred imported vaccines. Multivariable logistic regression indicated that lack of confidence, complacency in regard to health, risk of the vaccine, and attention frequency were the main factors affecting the intention to receive a COVID-19 vaccine.
Conclusion: Our study indicated that the respondents in China had a high willingness to accept a COVID-19 vaccine, but some participants also worried about its adverse effects. Information regarding the efficacy and safety of an upcoming COVID-19 vaccine should be disseminated to ensure its acceptance and coverage.
KEYWORDS: COVID-19, SARS-CoV-2, vaccine, willingness, attitude
Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) pandemic continues to threaten public health worldwide, and more than 42 million confirmed cases have been reported. During the COVID-19 pandemic, governments have taken a series of strong interventions to prevent and control it, including city lockdown, travel bans, quarantine, mask mandates, and social distancing policies.1 These measures have effectively slowed the spread of the epidemic, but severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is still increasing worldwide. In some cities and regions where the spread of the virus was previously effectively controlled, the COVID-19 outbreak has begun to rebound as control measures were loosened. Therefore, some people worry that there will be a cycle of “City lockdown – Case reduction – City opening – Case rebound – City relockdown”.2 As one of the most powerful weapons against infectious diseases, a safe and effective vaccine is expected to eventually end the COVID-19 pandemic. Impressively, a race to develop a coronavirus vaccine is in full swing. Hundreds of vaccine candidates are being developed against SARS-CoV-2 using different technologies, ranging from traditional inactivated vaccines and subunit vaccines to recombinant DNA vaccines, mRNA vaccines, and viral-vectored vaccines. Among them, several candidates show promise for testing in phase III clinical trials. It is no exaggeration to say that COVID-19 vaccine development has been progressing at a historic speed from bench research to clinical trials, in which vaccines are already being injected into healthy human volunteers for clinical testing or emergency use after several months instead of several years, as is typical for vaccine development.
Before the COVID-19 vaccine is ready for public inoculation, much work undoubtedly needs to be done to ensure that it is safe and effective through the use of preclinical and clinical evidence.3 Meanwhile, plans should be made to disseminate the upcoming COVID-19 vaccine to large populations. To date, only a few studies have investigated vaccination intentions. For instance, 85.8% of 3741 participants from Australia, 73.9% of 7664 participants from Europe and 68.5% of 2006 participants from the United States stated that they would be willing to be vaccinated against COVID-19.4,5 Very recently, Wang et al. reported that the willingness to receive a COVID-19 vaccine was 91.3% (1879/2058) during the COVID-19 pandemic in China.6 In this work, we aimed to further assess the acceptance of a COVID-19 vaccine during the remission period of this pandemic, and we also focused on understanding who was hesitant about vaccination, what concerns they had, and how to increase their willingness to accept a vaccine. It is expected that this work will provide guidance to make regulations and policies for the upcoming COVID-19 vaccination plan in this large population.
Methods
Design and sample
This survey is a cross‐sectional study with a convenience sample of the adult population in China. Data were collected from all 34 provincial administrative regions in China through an online anonymous questionnaire from May to June 2020.7,8 We used wenjuan.com, an online survey platform, to publish the questionnaire and generate the answer URL link and quick response (QR) code, which were spread by snowball sampling using social software. The interviewees visited the URL or scanned the QR code on their mobile phones to answer the questionnaire. The inclusion criteria were individuals who (1) were at least 18 years old; (2) able to read and complete the self-administered questionnaire independently; and (3) voluntarily agreed to participate in this survey.
Sample size and enrollment
The initial minimum sample size of participants was calculated by the following formula based on an α error of 0.05 and maximum permissible error δ equaling 0.02:9
| (1) |
A minimum sample size of 2401 participants was estimated, and considering invalid questionnaires (~10%), we increased the sample size to 3383. To assure the reliability of the self-reported data obtained from the self-administered questionnaires, we processed the data using the following cleaning procedure: (1) when exporting data, the screening conditions were set to be over 18 years old, the answer time was more than 30 s, and the quality control question need to be answered correctly; (2) the questionnaires in which all items in the scale were answered with the same option (except neutral/unknown) were excluded, and were defined these participants as inattentive or unmotivated participants; and (3) logically contradicted data were also deleted. Finally, a total of 3195 of 3383 questionnaires were considered valid (effective rate = 94.4%). Given that the elderly population is thought to be a high-risk group for SARS-COV-2 infection and that the proportion of this group using smartphones is relatively small, we also conducted an on-the-spot survey of people over 50 years old.
Measures
This study used an anonymous, population-based, structured questionnaire. The following three parts were included in this questionnaire: (1) demographic and health information; (2) questions evaluating participants’ knowledge and attitudes regarding COVID-19 and a COVID-19 vaccine; and (3) items measuring the vaccination hesitancy variable. A 5-point Likert scale (strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree) was used to assess the related items.
The draft of the questionnaire was developed based on previous studies10,11 and revised according to the 10 items of the Vaccine Hesitancy Scale (VHS) developed by the WHO Strategic Advisory Group on Experts (SAGE) Working Group,12 considering the specific research and development of COVID-19 vaccines and the characteristics of the COVID-19 epidemic situation. Preinvestigation was performed to further improve the quality of this questionnaire. To ensure content validity, the questionnaire was improved based on reviews by five public health scholars. Moreover, to improve the credibility of the scale, we added several reversed questions to the scale to make the direction of all the items In consistent, and the values of these questions were flipped when analyzing them. Therefore, higher scores indicated a more negative attitude toward COVID-19 vaccination.
Then, we used confirmatory factor analysis (CFA) and exploratory factor analysis (EFA)13 to evaluate the reliability and construct validity of the instrument based on the 10-item scales for COVID-19 vaccination. The reliability of each scale construct was evaluated according to Cronbach’s coefficient, which was 0.81, 0.79, and 0.80 for lack of confidence, complacency and risk, respectively (Supplementary Table 1-Table 3).
Statistical analysis
For descriptive analyses, chi-square tests were used to evaluate the associations between participants’ willingness to receive a COVID-19 vaccine and sociodemographic characteristics, cognition, and attitudes. The differences in the vaccination hesitancy scores between those participants who intended to receive the vaccine and those who had no intention of receiving the vaccine were determined by t tests. Subsequently, we employed multivariable logistic regression to identify the possible factors affecting intention. Only the single factors (Chi-square test or t-test) that were statistically significant and professionally considered meaningful were included in the multivariable regression model. For the above regression, OR and the respective 95% CI were estimated. All analyses were performed using SPSS26.0 (IBM Corporation, New York, NY, United States). The alpha level was set at 0.05, and p < .05 was considered statistically significant.
Ethical approval
This study was approved by the Ethics Committee of the School of Public Health (Shenzhen), Sun Yat-sen University (Approval number: SYSU-PHS-IACUC-2020 − 029).
Results
Participant characteristics
A total of 3383 respondents were recruited in this survey, and 3195 questionnaires were considered valid (effective rate = 94.4%) (Table 1). The geographical distribution of the population involved in this survey was roughly the same as that in provinces in China (Supplementary Figure 1). Based on population distribution data among provinces in China, Guangdong Province has the largest population, and the other provinces with the top ten largest populations are Shandong, Henan, Sichuan, Jiangsu, Hebei, Hunan, Anhui, Hubei and Zhejiang. Consistent with these data, most participants in our survey were from Guangdong Province, followed by Hunan, Hebei, Inner Mongolia, Fujian, Henan, Jiangsu, Anhui, Sichuan, Shandong and Hubei Provinces.
Table 1.
Descriptive characteristics of various populations by willingness to receive a COVID-19 vaccine in China
| Variables | N% | Willingness to receive vaccine |
P | |
|---|---|---|---|---|
| Yes N (%) | No and unsure N (%) | |||
| Whole sample | 3195 (100.0) | 2676 (83.8) | 519 (16.2) | |
| Gender | ||||
| Male | 1163 (36.4) | 991 (85.2) | 172 (14.8) | 0.092 |
| Female | 2032 (63.6) | 1685 (82.9) | 347 (17.1) | |
| Age | ||||
| 18–25 | 1503 (47.1) | 1282 (85.3) | 221 (14.7) | 0.049* |
| 26–44 | 1260 (39.4) | 1045 (82.9) | 215 (17.1) | |
| ≥45 | 432 (13.5) | 349 (80.8) | 83 (19.2) | |
| Ethnicity | ||||
| The Han nationality | 3048 (95.4) | 2564 (84.1) | 484 (15.9) | 0.011* |
| Other | 147 (4.6) | 112 (76.2) | 35 (23.8) | |
| Educational level | ||||
| ≤High school | 342 (10.7) | 301 (88.0) | 41 (12.0) | <0.001* |
| Bachelor | 1812 (56.7) | 1540 (85.0) | 272 (15.0) | |
| Master and above | 1041 (32.6) | 835 (80.2) | 206 (19.8) | |
| Occupation | ||||
| Students | 1320 (41.3) | 1130 (85.6) | 190 (14.4) | 0.33 |
| Company employees | 440 (13.8) | 356 (83.0) | 75 (17.0) | |
| Professional technicians | 404 (12.6) | 325 (80.4) | 79 (19.6) | |
| Health care professionals | 345 (10.8) | 284 (82.3) | 61 (17.7) | |
| Public servants | 252 (7.9) | 206 (81.7) | 46 (18.3) | |
| Freelancers | 229 (7.2) | 194 (84.7) | 35 (15.3) | |
| Self-employed | 106 (3.3) | 90 (84.9) | 16 (15.1) | |
| Retirees | 67 (2.1) | 54 (80.6) | 13 (19.4) | |
| Others | 32 (1.0) | 28 (87.5) | 4 (12.5) | |
| Monthly income | ||||
| <2000 RMB | 1071 (33.5) | 918 (85.7) | 153 (14.3) | 0.035* |
| 2001–5000 RMB | 871 (27.3) | 723 (83.0) | 148 (17.0) | |
| 5001–10000 RMB | 581 (18.2) | 495 (85.2) | 86 (14.8) | |
| 10001–20000 RMB | 429 (13.4) | 342 (79.7) | 87 (20.3) | |
| >20000 RMB | 243 (7.6) | 198 (81.5) | 45 (18.5) | |
| Health | ||||
| Good | 2811 (88.0) | 2366 (84.2) | 445 (15.8) | 0.214 |
| General | 371 (11.6) | 300 (80.9) | 71 (19.1) | |
| Poor | 13 (0.4) | 10 (76.9) | 3 (23.1) | |
| Chronic disease or not | ||||
| Yes | 333 (10.4) | 66 (19.8) | 267 (80.2) | 0.062 |
| No | 2862 (89.6) | 453 (15.8) | 2409 (84.2) | |
Among the participants, 86.5% were aged between 18 and 44 years old. The proportion of male and female participants in this survey was 36.4:63.6. In this online survey, 56.7% of the respondents had a university/college degree. The respondents’ economic status was also determined. To investigate the susceptible population at high-risk for SARS-CoV-2 infection, 432 (13.5%) participants were over 45 years old, 57 (1.9%) were over 60 years old, and 333 (10.4%) suffered from chronic diseases. Of note, 3 patients with SARS-CoV-2 infection were included in this survey.
In our survey, the majority (2676, 83.8%) of participants were willing to receive a COVID-19 vaccine, 84 (2.6%) were not, and the remaining 435 (13.6%) were unsure (Table 1). In the subsequent analysis, the factors of age, ethnicity, education level, and monthly income were statistically correlated with willingness to receive a COVID-19 vaccine.
Vaccination willingness and hesitancy
The distribution of responses for each item on the vaccine hesitancy scale (VHS) was analyzed (Figure 1). Most believed that a vaccine was beneficial if it was recommended by the government (80.0%, item 8) or professionals (70.1%, item 9). Though a high proportion of participants were willing to receive a COVID-19 vaccine, 33.2% of participants were concerned and 41.7% held a neutral attitude regarding the adverse effects of a COVID-19 vaccine (item L7). Meanwhile, 20.5% of participants doubted the safety of a COVID-19 vaccine, and 40.7% had a neutral attitude (item L6).
Figure 1.
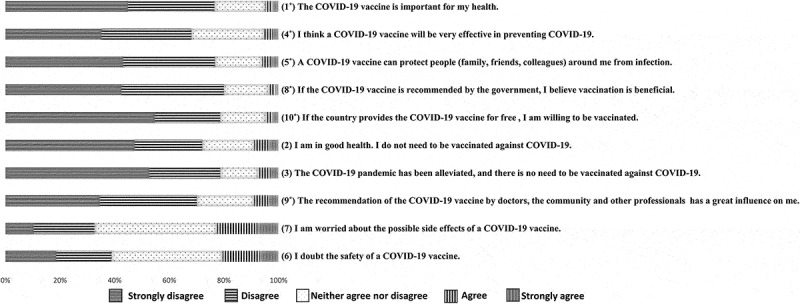
Distribution of the responses to ten items of the vaccine hesitancy scale (VHS) in China
To determine the relationship between COVID-19 vaccination willingness and vaccine hesitancy, ten items of the VHS were analyzed, as shown in above figure. These items were developed by the WHO Strategic Advisory Group on Experts (SAGE) Working Group. To improve the credibility of this scale, several reversed questions were added, and the values of these questions (marked with *) were flipped when analyzing them. As a result, all the indicated higher scores represented a more negative attitude toward COVID-19 vaccination in this Figure.
We further analyzed the differences in VHS between participants who intended to receive the COVID-19 vaccine and those who had no intention of receiving the vaccine, and the results demonstrated that participants who had more confidence, less complacency and less worry about risks were more likely to accept a COVID-19 vaccine (p < .001) (Table 2).
Table 2.
Total values of VHS measures by intention to receive a COVID-19 vaccine
| Scale | Willing to be vaccinated |
Unsure and unwilling to be vaccinated |
t test (P value) | Cohen’s d | ||
|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | |||
| Lack of confidence | 2676 | 1.77 (0.59) | 519 | 2.60 (0.76) | <0.001 | 1.12 |
| Complacency | 2676 | 1.72 (0.90) | 519 | 2.57 (0.98) | <0.001 | 0.88 |
| Risk | 2676 | 2.77 (0.97) | 519 | 3.50 (0.98) | <0.001 | 0.75 |
Attitudes toward the COVID-19 pandemic and a COVID-19 vaccine
We also addressed the public’s attitudes toward the COVID-19 pandemic and a COVID-19 vaccine with eight questions in our survey (Table 3). An overwhelming majority of participants (98.7%) thought that COVID-19 was a somewhat or strongly serious disease, 76.6% of participants were worried that they might be infected with SARS-CoV-2, and 94.7% of participants believed that a future COVID-19 vaccine would effectively control the spread of the COVID-19 epidemic. In particular, 3 COVID-19 patients participated in this study, and they were all willing to receive a COVID-19 vaccine. Of note, 10.4% of the participants reported that they paid little or no attention to the related information about COVID-19 vaccine development, while the vaccination willingness (66.3%) of this population was significantly lower than that of others (85.8%) (p < .001).
Table 3.
Participants’ attitudes toward COVID-19 and COVID-19 vaccines
| Willingness to receive vaccine |
|||||
|---|---|---|---|---|---|
| Variable | Classification | N (%) | Yes N (%) |
No and unsure N (%) |
P |
| Views on COVID-19 | Serious | 1767 (55.3) | 1524 (86.2) | 243 (13.8) | <0.001 |
| Moderate | 1375 (43.0) | 1115 (81.1) | 260 (18.9) | ||
| Mild and no idea | 53 (1.7) | 37 (69.8) | 16 (30.2) | ||
| Worry degree of COVID-19 | Very worried | 807 (25.3) | 727 (90.1) | 80 (9.9) | <0.001 |
| Somewhat worried | 1640 (51.3) | 1369 (83.5) | 271 (16.5) | ||
| A little worried | 649 (20.3) | 510 (78.6) | 139 (21.4) | ||
| Not at all | 99 (3.1) | 70 (70.7) | 29 (29.3) | ||
| Attention frequency | Often | 1290 (40.4) | 1164 (90.2) | 126 (9.8) | <0.001 |
| Sometimes | 1573 (49.2) | 1292 (82.1) | 281 (17.9) | ||
| Rarely | 294 (9.2) | 201 (68.4) | 93 (31.6) | ||
| Never | 38 (1.2) | 19 (50.0) | 19 (50.0) | ||
| Maximum affordable price | Free | 605 (18.9) | 490 (81.0) | 115 (19.0) | 0.054 |
| 1–100 RMB | 898 (28.1) | 766 (85.3) | 132 (14.7) | ||
| 101–500 RMB | 1218 (38.1) | 1017 (83.5) | 201 (16.5) | ||
| 501–1000 RMB | 302 (9.5) | 265 (87.7) | 37 (12.3) | ||
| 1001–2000 RMB | 101 (3.2) | 79 (78.2) | 22 (16.9) | ||
| >2000 RMB | 71 (2.2) | 59 (83.1) | 12 (16.9) | ||
| Priority vaccination population | Health care professionals and other high-risk groups | 1386 (43.4) | 1186 (85.6) | 200 (14.4) | <0.001 |
| Elderly and other susceptible groups | 528 (16.5) | 439 (83.1) | 89 (16.9) | ||
| No distinction and voluntary | 1032 (32.3) | 819 (79.4) | 213 (20.6) | ||
| No distinction and mandatory for all | 225 (7.0) | 217 (96.4) | 8 (3.6) | ||
| Other | 24 (0.8) | 15 (62.5) | 9 (37.5) | ||
| Time to market of vaccine | Within half a year | 505 (15.8) | 446 (88.3) | 59 (11.7) | <0.001 |
| 6 months – 1 year | 1475 (46.2) | 1287 (87.3) | 188 (12.7) | ||
| 1–5 years | 868 (27.2) | 680 (78.3) | 188 (21.7) | ||
| > 5 years | 49 (1.5) | 32 (65.3) | 17 (34.7) | ||
| I do not know | 298 (9.3) | 231 (77.5) | 67 (22.5) | ||
In our survey, 59.9% of participants thought that the high-risk population, such as health care workers and elderly people, should be given COVID-19 vaccination priority. Interestingly, among the participants who were willing or hesitant to be vaccinated, 76.8% preferred to receive a domestic COVID-19 vaccine, and only 23.2% of the participants preferred to receive an imported COVID-19 vaccine. We also found that those who preferred a domestic COVID-19 vaccine had a higher willingness to be vaccinated (88.8%) than those who preferred an imported COVID-19 vaccine (76.9%) (p < .001) (Supplementary Table 4).
Factors associated with COVID-19 vaccination intention
Finally, the model of multivariable logistic regression in our study was matched with the Hosmer and Leme showed goodness‐of‐fit test (χ2 = 8.21, df = 8, p = .41), implying that this model had a good fitting degree (Table 4). The populations who had higher scores for lack of confidence (adjusted odds ratio [aOR] = 0.16, 95% confidence interval [CI] = 0.14–0.19, p < .001), complacency (aOR = 0.45, 95% CI = 0.40–0.49, p < .001) and risks (aOR = 0.46, 95% CI = 0.41–0.51, p < .001) were less likely to accept a COVID-19 vaccine. High frequency attention to relevant COVID-19 information (aOR = 2.11, 95%CI = 1.52–2.92, p < .001) was positively correlated with willingness to receive a COVID-19 vaccine. However, the perceived views of the severity of COVID-19 disease and the degree of concern regarding the COVID-19 pandemic were not significantly correlated with the dependent variable.
Table 4.
Logistic regression to identify factors affecting vaccination willingness of various populations
| Unadjusted odds ratio |
Adjusted odds ratio |
||||||
|---|---|---|---|---|---|---|---|
| Variables | Classification | ORa | 95%CI | P | aORb | 95%CI | P |
| VHS | Lack of confidence | 0.16 | 0.14–0.19 | <0.001 | 0.22 | 0.18–0.27 | <0.001 |
| Complacency | 0.45 | 0.40–0.49 | <0.001 | 0.58 | 0.52–0.66 | <0.001 | |
| Risks | 0.46 | 0.41–0.51 | <0.001 | 0.53 | 0.46–0.60 | <0.001 | |
| Attitudes and behavior | |||||||
| Views on COVID-19 | More perceived COVID-19 severity | 1.50 | 1.24–1.82 | <0.001 | 1.09 | 0.86–1.37 | 0.48 |
| Worry degree of COVID-19 | More worried about infection | 1.73 | 1.41–2.12 | <0.001 | 1.14 | 0.87–1.48 | 0.35 |
| Attention frequency | More attention | 3.07 | 2.39–3.95 | <0.001 | 2.11 | 1.52–2.92 | <0.001 |
| Sociodemographic characteristics | |||||||
| Gender | Male | 1.19 | 0.97–1.45 | 0.092 | 1.35 | 1.05–1.74 | 0.019 |
| Female | Ref | Ref | |||||
| Age | 18–25 | 1.38 | 1.04–1.82 | 0.024 | 1.17 | 0.74–1.90 | 0.52 |
| 26–44 | 1.16 | 0.87–1.53 | 0.31 | 1.11 | 0.70–1.65 | 0.63 | |
| ≥45 | Ref | Ref | |||||
| Ethnicity | The Han nationality | 1.66 | 1.12–2.45 | 0.012 | 1.96 | 1.21–3.17 | 0.007 |
| Other | Ref | Ref | |||||
| Educational level | High school and below | 1.81 | 1.26–2.60 | 0.001 | 2.19 | 1.22–3.91 | 0.009 |
| Bachelor | 1.40 | 1.14–1.71 | 0.001 | 1.22 | 0.92–1.62 | 0.17 | |
| Master and above | Ref | Ref | |||||
| Occupation | Students | 1.28 | 0.93–1.75 | 0.13 | 1.14 | 0.72–1.90 | 0.59 |
| Company employees | 1.05 | 0.72–1.52 | 0.82 | 0.98 | 0.61–1.62 | 0.92 | |
| Professional technicians | 0.88 | 0.61–1.28 | 0.51 | 0.75 | 0.47–1.19 | 0.22 | |
| Health care professionals | Ref | Ref | |||||
| Public servants | 0.96 | 0.63–1.47 | 0.86 | 0.96 | 0.56–1.63 | 0.88 | |
| Freelancers | 1.19 | 0.76–1.88 | 0.45 | 1.07 | 0.58–1.97 | 0.84 | |
| Self-employed | 1.21 | 0.66–2.20 | 0.54 | 0.80 | 0.34–1.86 | 0.60 | |
| Retirees | 0.89 | 0.46–1.74 | 0.74 | 0.70 | 0.28–1.75 | 0.45 | |
| Others | 1.50 | 0.51–4.44 | 0.46 | 1.32 | 0.39–4.46 | 0.65 | |
| Monthly income | <2000 RMB | 1.36 | 0.95–1.97 | 0.10 | 0.63 | 0.34–1.14 | 0.13 |
| 2001–5000 RMB | 1.11 | 0.77–1.61 | 0.58 | 0.54 | 0.31–0.91 | 0.022 | |
| 5001–10000 RMB | 1.31 | 0.88–1.95 | 0.18 | 0.85 | 0.50–1.97 | 0.53 | |
| 10001–20000 RMB | 0.89 | 0.60–1.33 | 0.58 | 0.77 | 0.46–1.29 | 0.32 | |
| >20000 RMB | Ref | Ref | |||||
| Health | Good | 1.60 | 0.44–5.82 | 0.48 | 0.84 | 0.09–7.43 | 0.87 |
| General | 1.27 | 0.34–4.73 | 0.72 | 0.87 | 0.10–7.87 | 0.90 | |
| Poor | Ref | Ref | |||||
| Chronic disease or not | Yes | 0.76 | 0.57–1.01 | 0.062 | 0.80 | 0.54–1.16 | 0.24 |
| No | Ref | Ref | |||||
OR, odds ratio; a Unadjusted odds ratio, b Adjusted odds ratio; The following variables were included in the multivariate logistic regression model: lack of confidence, complacency, risks, attention frequency, gender, ethnicity, educational level.
In addition, among the respondents, the willingness of men (aOR = 1.35, 95% CI = 1.05–1.74, p = .019) to be vaccinated against COVID-19 was higher than that of women. Moreover, high-income respondents had a more positive attitude toward COVID-19 vaccination (>20000 RMB as the control; 2001–5000 aOR = 0.54, 95% CI = 0.31–0.91, p = .022), and the respondents with a lower education level (high school or below: aOR = 2.19; 95% CI = 1.22–3.91, p = .009) showed greater vaccination acceptance.
Discussion
In our survey, the percentage of subjects willing to accept a future COVID-19 vaccine was 83.8%, much higher than that for other vaccines in China, such as influenza vaccine (50.8%-59.9%)14,15 and HPV vaccine (58.6%).16 This phenomenon might result from the fact that the COVID-19 outbreak had a serious impact on the public’s daily life, including the inability to resume work and school, strict travel restrictions, and huge economic losses. The vaccination intention (83.8%) in this study was slightly lower than that in another recent survey in China, in which 91.3% of Chinese adults stated a willingness to receive COVID-19 vaccination.6 Several studies have indicated that the willingness to receive vaccination might be different in various regions and in different stages of the pandemic.5,17 Consequently, as the COVID-19 pandemic continues, it will be important to monitor the dynamic changes in the public’s vaccination willingness.
Compared with other countries, Chinese attitudes toward a COVID-19 vaccine appear to be more positive than reported in France in March (74.0%), in Europe in April (73.9%),4 in the United States in May (68.5%), and similar to that in Australia in April (85.8%),5,17,18 which might reflect the degree of trust in the government. Notably, a previous work indicated that despite a strong parental preference (83.4%) for the administration of an influenza vaccine to their children, the actual vaccination rate was much lower (3.1%).11 Thus, the willingness reported in the survey might not represent the actual rate of vaccination when a vaccine is clinically available.
More than half of participants (62.0%) believed that a vaccine would be on the market within one year, which showed that the participants were eager for a COVID-19 vaccine to be available and might also be partly attributable to the impressive performance of the Chinese government during this pandemic. We also found an obvious association between the perception of vaccine development time and the willingness to be vaccinated (Table 2). We investigated the preference for imported vaccines or domestic vaccines at the same price. Our results showed that participants had more confidence in domestic COVID-19 vaccines, and the people who trusted domestic vaccines showed a greater willingness to accept a COVID-19 vaccine, implying that the quality of domestic vaccines was increasingly recognized. The “2020 Trust Barometer” released by Edelman, the world’s largest public relations consulting company, showed that the trust of people in the Chinese government ranked first in the world (90%), significantly above the world average (49%).19 Consistent with these data, in our present study, if the government recommended a COVID-19 vaccine, less than 4% of the 3195 respondents reported reluctance to be vaccinated. Therefore, a highly trusted government would be a powerful measure to improve vaccination coverage.
Nearly half of the respondents thought that high-risk groups, such as health care personnel and scientific researchers, should be given priority if a vaccine became available. Participants expressed that health care personnel and scientific researchers, who risk their lives on the front lines fighting against this epidemic, need to be vaccinated preferentially. A booster vaccination may be required to ensure sufficient levels of population protection to achieve herd immunity, particularly in asymptomatic individuals, individuals who have recovered from COVID-19 but generated poor immunity or who have experienced a rapid waning of immunity, and individuals who received a rapidly developed ‘pandemic’ vaccine that provided suboptimal protection or rapidly waning immune responses.20
Less than half of the participants indicated that they would pay out-of-pocket for a COVID-19 vaccine (101–500 RMB, 1 RMB ≈ 0.15 USD, 38.1%). In China, 18.9% of participants hoped to receive the vaccine for free, while 30% of participants in the United States hoped to be vaccinated free of charge.17 Previous studies have shown that the majority of individuals were not willing to pay the market price for vaccines against high-burden diseases in China,21 while the immunization intention and coverage of those self-paid vaccines could be improved by China’s Expanded Program on Immunization (EPI).22 Therefore, the government should consider incorporating the COVID-19 vaccine into the EPI.
The efforts of the scientific community to search for a vaccine against COVID-19 may be hampered by vaccine hesitancy.23 According to a previous study, three dimensions of the VHS (lack of confidence, complacency, and risks) were related to vaccination intention.12,24 Consistent with these studies, we found that lack of confidence (aOR = 0.22) was the most important factor affecting COVID-19 vaccination intention, followed by risks (aOR = 0.53) and complacency (aOR = 0.58). Confidence means the trust in vaccines, the entire health care system, and immunization decision-makers.25 Compared with the average, those who refused to be vaccinated reported lower confidence in a COVID-19 vaccine. Therefore, public health institutions and the scientific community should make a serious effort to maintain and enhance the feeling of mutual trust and cooperation with the public.26 Risks refer to the safety and side effects of a vaccine, which are essential factors to be considered. In the group that intended to be vaccinated, 16.6% and 28.5% were concerned with the safety and side effects of vaccines, respectively, while 44.6% and 57.1% were concerned with those who did not intend to get vaccinated. A previous study also reported that the side effects and safety of vaccines were the most common reasons for influenza vaccination hesitancy.27 Hence, vaccine providers still need to work on addressing public misconceptions about vaccine safety and side effects. In addition to the lack of confidence and risks, complacency also contributes to vaccine hesitancy. Complacency refers to the perception that the risks of vaccine-preventable diseases are low, and therefore, vaccination is not deemed a necessary preventive action.28 Our work indicated that 20.3% of participants had almost no fear of COVID-19 infection, and 3.1% did not worry about infection at all, while their vaccination intentions were 78.6% and 70.7%, respectively, below the average of 83.8%.
The perceived severity of the pandemic affects the public’s perception of risk. Despite the fact that more than half (55.3%) of the respondents thought COVID-19 was a very serious infectious disease, only a small number (25.3%) worried about the likelihood of contracting COVID-19. This finding indicated that public risk perception needs to be enhanced, as the perception of high risk translates into preventive actions in many infectious disease outbreaks and has been found to enhance epidemic control.29
In this survey, it was found that less educated participants were more willing to be vaccinated, while those with higher monthly earnings were also more willing to be vaccinated. This observation seemed to be contradictory, a high education level is not always correlated with high income. One possible reason for this observation might be the high proportion of highly educated people in our survey, a considerable proportion of whom are still college students or graduate students with a high level of education but a low income.
We also observed that education level was negatively associated with willingness to be vaccinated. Further analysis showed that populations with high levels of education were more optimistic about their health condition, less confident about the vaccine’s effect, and more easily influenced by the opinions of others, including social media, colleagues and friends. In addition, a previous study indicated that highly educated individuals absorbed and responded to health information more quickly than others,30 and another study reported that the majority of people, especially highly educated individuals, agreed that new vaccines carried more risks than older vaccines.24 The COVID-19 vaccine is an unmarketed vaccine, and people with a higher education level may require more precise information than those with a lower education level. The results of our study suggest that vaccination providers should offer patients who have completed tertiary education more scientific evidence that the vaccine works well.
Our study has some limitations. The survey method is easy to perform, provides access to large and diverse samples, and produces timely results.31 However, this approach also has inherent limitations and recruitment biases.32 Obviously, some individuals are not exposed to social media, especially elderly people or those without internet access. To some degree, this bias can be adjusted by providing a directed invitation to a specific community, and we also sought responses from older individuals though the use of face-to-face questionnaires in a community park. In the present study, the respondents were relatively young and highly educated compared to the whole society, which seems in accordance with the social media-based recruitment mechanism that we employed. Moreover, our conclusions from heterogeneous populations using convenience sampling survey tools in this study make it difficult to extrapolate them to the actual population. A more representative sampling method will be required to investigate the actual population’s perspectives on the willingness to receive a COVID-19 vaccine in the future. Finally, we did not investigate how well each participant understood each question, so it is possible that not every participant fully understood the meaning of the questions. These issues may influence the data quality, and therefore, our results should be interpreted with some caution.
Conclusions
Overall, our study demonstrated that there was a high willingness to accept a future COVID-19 vaccine in China, even though the pandemic has been under control; additionally, certain participants expressed concern about its potential safety. The lack of confidence, the risk of vaccines, complacency in health, and attention frequency toward the COVID-19 vaccine were the major factors contributing to this vaccine hesitancy. Accordingly, we suggest that dissemination of information regarding the efficacy and safety of the upcoming COVID-19 vaccine may ensure its acceptance and coverage.
Supplementary Material
Acknowledgments
CJS conceived and designed this project; MSC, YJL, JSC, ZYW performed this project and analyzed the data; CXF, HCZ, YLS, LC, FLF contributed the resources and discussion; CJS, MSC, YJL, JSC drafted the manuscript, and all authors reviewed the final manuscript.
Survey of Public Vaccination Willingness for a COVID-19 Vaccine.
Dear friends: We are a survey team from Sun Yat-sen University, China. The purpose of this survey is to inquire about the public’s views regarding vaccination willingness for an upcoming COVID-19 vaccine. The survey is answered anonymously and does not involve personal privacy information; please rest assured and answer objectively as much as possible.
Background: Currently, millions of people are infected with COVID-19 worldwide, and vaccines, as the ultimate weapon against the global pandemic, are expected. At present, a number of scientific research institutions and pharmaceutical companies around the world are accelerating their efforts to develop a COVID-19 vaccine.
Basic Information
- What’s your gender? [single choice]
- Male
- Female
- How old are you? [single choice]
- <18
- 18–25
- 26-44
- 45–59
- ≥60
- What’s your ethnicity? [single choice]
- The Han nationality
- Other
What province do you often live in?[completion]
- What’s your education background (including the degree you are currently pursuing)? [single choice]
- Junior middle school and below
- Junior high school
- Bachelor (including associate)
- Master and above
- What do you do? [single choice]
- Students (turn to 7.)
- Health care professionals
- Public servants
- Professional technicians (teachers, lawyers, engineering technicians, etc.)
- Company employees
- Self-employed
- Retirees
- Freelancers
- Others, please fill in
- * What is your major? [single choice]
- Medicine
- Humanities
- Science and engineering
- Agronomy
- Physical education
- Art
- Others, please fill in
- Your personal average monthly income last year (including social benefits, living expenses from other people, etc.)? [single choice]
- <2000 RMB
- 2001–5000 RMB
- 5001–10000 RMB
- 10001–20000 RMB
- >20000 RMB
- How is your current state of health? [single choice]
- Good
- General
- Poor
- Have you ever suffered from any of the following diseases? [multiple choice]
- Cardiovascular disease
- Chronic tumor
- Chronic respiratory disease
- Immunodeficiency disease
- Other chronic diseases
- COVID-19
- None二, Attitudes and Behavior
- What do you think about COVID-19? [single choice]
- A very serious and severe infectious disease
- An infectious disease of some severity
- It is similar to a common respiratory disease
- No idea
- Have any of your family members, relatives, neighbors, friends or colleagues been infected with COVID-19? [single choice]
- Yes
- No
- Are you concerned that you will be infected (or reinfected) with COVID-19? [single choice]
- Very worried
- Worried
- A little worried
- Not worried at all
- How often do you think about the development of a COVID-19 vaccine? [single choice]
- Often
- Sometimes
- Rarely
- Never
- How do you get information about the COVID-19 vaccine initiative? [multiple choice]
- Internet
- Communication with friends and family
- TV programs
- Expert lectures
- Others, please fill in
- According to your perception, how long will it take for a COVID-19 vaccine to be on the market? [single choice]
- Within 6 months
- 6 months – 1 year
- 1–5 years
- 5 years
- I do not know
- Following the release of a COVID-19 vaccine, how do you think it should be implemented? [single choice]
- Priority should be given to relevant health care professionals, scientific researchers and other high-risk groups.
- Priority should be given to the elderly, people with underlying diseases and other susceptible groups.
- No distinction and voluntary
- No distinction but mandatory for all
- Others, please fill in
- What impact do you think the COVID-19 vaccine will have on the pandemic? [single choice]
- An immediate effect, the virus will be eradicated immediately
- Mitigation of the epidemic, but the virus will not be eliminated entirely
- No effect
- I do not know
- Which is the most effective measure to prevent COVID-19? [single choice]
- Wearing a mask
- Drinking
- Smoking
- Sauna, sweat steaming
- Would you like to be vaccinated, if a COVID-19 vaccine is available in the future? [single choice]
- I would like to
- I would be grudgingly will
- I would be hesitant
- I would refuse
- The highest total price of COVID-19 vaccine you can afford is ?[single choice]
- Free of charge
- 1 ~ 100 RMB
- 101 ~ 500 RMB
- 501 ~ 1000 RM
- 1001 ~ 2000 RMB
- >2000 RMB
- Do you prefer to be vaccinated with a domestic or imported COVID-19 vaccine if offered at the same price? [single choice]
- Domestic vaccine.
- Imported vaccine
三, Vaccine hesitation scale
Each question has five options: 1. strongly disagree 2. disagree 3. neither agree nor disagree 4. agree 5. strongly agree.
Question:
The COVID-19 vaccine is important for my health.
I am in good health. I do not need to be vaccinated against COVID-19.
The COVID-19 pandemic has been alleviated, and there is no need to be vaccinated against COVID-19.
I think a COVID-19 vaccine will be very effective in preventing COVID-19.
A COVID-19 vaccine can protect people (family, friends, colleagues) around me from infection.
I doubt the safety of a COVID-19 vaccine.
I am worried about the possible side effects of a COVID-19 vaccine.
If the COVID-19 vaccine is recommended by the government, I believe vaccination is beneficial.
The recommendation for the COVID-19 vaccine by doctors, the community and other professionals has a great influence on me.
If the country provides the COVID-19 vaccine for free, I am willing to be vaccinated.
Appendix. 新型冠状病毒疫苗公众接种意愿调查
卷首语:您好!我们是来自中山大学公共卫生学院 (深圳) 的调查小组, 非常感谢您参与本次调查。此次调查目的是了解公众对终将到来的新冠疫苗接种的真实看法与接种意愿; 调查均为匿名填写, 不涉及个人隐私, 请您放心并尽可能客观回答。
背景知识:在全球新冠病毒感染人数累计超过数百万人的今天, 疫苗作为抵御病毒全球大流行的终极武器, 被人们寄予厚望。目前, 全球各大科研机构和制药企业都在快马加鞭的进行新型冠状病毒疫苗 (以下简称新冠疫苗) 的开发。
一、基本信息
1, 您的性别是:[单选题]
A. 男
B. 女
2, 您的年龄是:[单选题]
A. <18
B. 18-25
C. 26-44
D. 45-59
E. ≥60
3, 您的民族是: [单选题]
A. 汉族
B. 少数民族
4, 请问您经常居住的省份为?[下拉填空题]
5, 您的最高教育水平 (含目前在读) 是:[单选题]
A. 初中及以下
B. 高中 (含中专)
C. 大学 (含大专)
D. 硕士及以上
6, 您的职业是: [单选题]
A. 学生 (转第7题)
B. 医疗卫生人员
C. 国家机关, 事业单位人员
D. 专业技术人员 (教师, 律师, 工程技术人员等专业人员)
E. 公司职员
F. 个体经营者
G. 退休人员
H. 自由职业者
I. 其他, 请填写
7, 请问您的专业是?[单选题]
A. 医科类
B. 文史类
C. 理工类
D. 农学类
E. 体育类
F. 艺术类
G. 其他, 请填写
8, 您去年的个人平均月收入水平 (含社会补助金, 来自其他人的生活费等各种来源) ?[单选题]
A. <2000元
B. 2001-5000元
C. 5001-10000元
D. 10001-20000元
E. >20000元
9, 您目前健康状况如何?[单选题]
A. 良好
B. 一般
C. 较差
10, 您是否患有或曾患有以下疾病?[多选题]
A. 心血管疾病
B. 慢性肿瘤
C. 慢性呼吸道疾病
D. 免疫缺陷性疾病
E. 其他慢性疾病
F. 新冠肺炎
G. 以上均无
二、新冠疫苗相关行为与认知
11, 您如何看待新冠肺炎这种疾病? [单选题]
A. 是一种很严重的烈性传染病
B. 有一定严重性的传染病
C. 和普通的呼吸道疾病差不多
D. 没有想法
12, 您周边 (如家人, 亲戚, 邻居, 朋友或同事) 是否出现过新冠肺炎病例?[单选题]
A. 是
B. 否
13, 您是否担心会感染 (或曾经感染痊愈后再次感染) 新冠肺炎这种疾病?[单选题]
A. 非常担心
B. 有些担心
C. 一般
D. 完全不担心
14, 您近期对新冠疫苗研发的关注频率是?[单选题]
A. 经常 (转15)
B. 偶尔 (转15)
C. 很少 (转15)
D. 从不 (转16)
15, 您平时通过什么途径主动了解新冠疫苗的相关信息?[多选题]
A. 网络信息
B. 亲友交流
C. 电视节目
D. 专家讲座
E. 其他, 请写出
16, 根据您的了解, 您认为新冠疫苗还需要多久会上市?[单选题]
A. 半年内
B. 半年-1年
C. 1-5年
D. >5年
E. 不清楚
17, 新冠疫苗问世后, 您认为应 [单选题]
A. 优先给相关的医护工作者, 科研工作者等易感人群使用
B. 优先给老人, 有基础疾病等高危人群使用
C. 无差别但自愿地给所有人推广接种
D. 无差别但强制性给所有人接种
E. 其他情况, 请填写
18, 新冠疫苗上市后, 您认为对疫情有何影响?[单选题]
A. 立竿见影, 新冠病毒被消灭
B. 减轻疫情, 但不会消灭病毒
C. 没有影响
D. 不清楚
19, 目前预防新冠肺炎的有效措施有 [单选题]
A. 戴口罩
B. 饮酒
C. 吸烟
D. 桑拿, 汗蒸
20, 新冠疫苗将来上市后, 您是否会接种?[单选题]
A. 愿意
B. 勉强愿意
C. 犹豫不决
D. 拒绝
21, 您可负担的新冠疫苗全程接种的总价格最高为 [单选题]
A. 免费
B. 1 ~ 100元
C. 101 ~ 500元
D. 501 ~ 1000元
E. 1001 ~ 2000元
F. >2000元
22, 同等价格您更倾向于接种国产还是进口新冠疫苗?[单选题]
A. 国产疫苗
B. 进口疫苗
三、疫苗犹豫量表
每题均为5个选项, 从左至右分别表示:1.非常不赞同 2.不赞同 3.中立/不知道 4.赞同 5.非常赞同。[打分题:请填写数字1-5进行打分]
问题:
. 接种新冠疫苗对我的健康非常重要
. 我的身体很好, 不需要接种新冠疫苗
. 新冠疫情目前已经缓解, 不需要接种新冠疫苗
. 我觉得接种新冠疫苗对预防新冠肺炎非常有效
. 接种新冠疫苗可以保护我周围的人 (家人, 朋友, 同事) 不受感染
. 我怀疑新冠疫苗的安全性
. 我担心新冠疫苗可能带来的副作用
. 如果政府推荐接种新冠疫苗, 我相信接种是有益的
. 医生, 社区等专业人士对新冠疫苗的推荐对我影响很大
. 如果国家免费提供新冠疫苗, 我愿意接种
Funding Statement
This work was supported by the National Natural Science Foundation of China (81971927), the National Science and Technology Major Project of China (2018ZX10731101-002), and Science and Technology Planning Project of Shenzhen City (20190804095916056, JSGG20200225152008136).
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
References
- 1.Tian H, Liu Y, Li Y, Wu CH, Chen B, Kraemer MUG, Li B, Cai J, Xu B, Yang Q, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–42. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M.. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860-+. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang S. Don’t rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020;579:321. doi: 10.1038/d41586-020-00751-9. [DOI] [PubMed] [Google Scholar]
- 4.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ, Ayre J, Batcup C, Copp T, Cornell S, Dakin T. Sydney health literacy lab C-g. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2020. doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 Pandemic in China. Vaccines (Basel). 2020;8. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hays RD, Liu HH, Kapteyn A. Use of Internet panels to conduct surveys. Behav Res Methods. 2015;47:685–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eysenbach G, Wyatt J. Using the Internet for surveys and health research. J Med Internet Res. 2002;4:ARTN e13. doi: 10.2196/jmir.4.2.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang J. Statistical methods for biomedical research. 1th ed. Beijing (China): Higher Education Press; 2007. [Google Scholar]
- 10.Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, Verger P. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Euro Surveill. 2018;23. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeng Y, Yuan Z, Yin J, Han Y, Chu CI, Fang Y. Factors affecting parental intention to vaccinate kindergarten children against influenza: A cross-sectional survey in China. Vaccine. 2019;37:1449–56. doi: 10.1016/j.vaccine.2019.01.071. [DOI] [PubMed] [Google Scholar]
- 12.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33:4165–75. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 13.Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, Perez S, Rosberger Z. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36:660–67. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 14.Wu S, Su J, Yang P, Zhang H, Li H, Chu Y, Hua W, Li C, Tang Y, Wang Q, et al. Willingness to accept a future influenza A(H7N9) vaccine in Beijing, China. Vaccine. 2018;36:491–97. doi: 10.1016/j.vaccine.2017.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.You D, Han L, Li L, Hu J, Zimet GD, Alias H, Danaee M, Cai L, Zeng F, Wong L. Human Papillomavirus (HPV) vaccine uptake and the willingness to receive the HPV vaccination among female college students in china: a multicenter study. Vaccines (Basel). 2020;8. doi: 10.3390/vaccines8010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ren J, AL W, Zheng A, Sun X, ML B, Huang Z, Zikmund-Fisher BJ. The demographics of vaccine hesitancy in Shanghai, China. PloS One. 2018;13:e0209117. doi: 10.1371/journal.pone.0209117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38:6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Group TC. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20:769–70. doi: 10.1016/s1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.2020 Edelman Trust Barometer. Chicago: Edelman Public Relations Worldwide; 2020 Jan 19 [accessed 2020 Aug 20] . https://www.edelman.com/trustbarometer [Google Scholar]
- 20.Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z. Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol. 2020;20:615–32. doi: 10.1038/s41577-020-00434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hou Z, Jie C, Yue D, Fang H, Meng Q, Zhang Y. Determinants of willingness to pay for self-paid vaccines in China. Vaccine. 2014;32:4471–77. doi: 10.1016/j.vaccine.2014.06.047. [DOI] [PubMed] [Google Scholar]
- 22.Zhou L, Su QR, Xu Z, Feng A, Jin H, Wang SY, Feng Z. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12). PloS One. 2013;8:ARTN e73724. doi: 10.1371/journal.pone.0073724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35:785–88. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith MJ. Promoting vaccine confidence. Infect Dis Clin North Am. 2015;29:759–69. doi: 10.1016/j.idc.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Chen SC, Hawkins G, Aspinall E, Patel N. Factors influencing uptake of influenza A (H1N1) vaccine amongst healthcare workers in a regional pediatric centre: lessons for improving vaccination rates. Vaccine. 2012;30:493–97. doi: 10.1016/j.vaccine.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 26.Provenzi L, Barello S. The science of the future: establishing a citizen-scientist collaborative agenda after Covid-19. Front Public Health. 2020;8:ARTN 282. doi: 10.3389/fpubh.2020.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lau AYS, Sintchenko V, Crimmins J, Magrabi F, Gallego B, Coiera E. Impact of a web-based personally controlled health management system on influenza vaccination and health services utilization rates: a randomized controlled trial. J Am Med Inform Assn. 2012;19:719–27. doi: 10.1136/amiajnl-2011-000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 29.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vacc Immunother. 2020;16:2204–14. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang LV. Information, education, and health behaviors: evidence from the MMR vaccine autism controversy. Health Econ. 2018;27:1043–62. doi: 10.1002/hec.3645. [DOI] [PubMed] [Google Scholar]
- 31.Mo PK, Lau JT. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: the application of the Health Belief Model. Health Educ Res. 2015;30:706–18. doi: 10.1093/her/cyv038. [DOI] [PubMed] [Google Scholar]
- 32.Steiner M, Vermeulen LC, Mullahy J, Hayney MS. Factors influencing decisions regarding influenza vaccination and treatment: a survey of healthcare workers. Infect Control Hospital Epidemiol. 2002;23:625–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


