ABSTRACT
Background: Millions of children in developing countries remained unvaccinated and under-vaccinated. This study was aimed to determine the pooled full vaccination coverage and associated factors in Ethiopia.
Methods: This review and meta-analysis were included observational studies conducted from 2013 to 2020. The international online databases as well as gray literatures were retrieved from April 15 to 30/2020. The quality of each study was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOS). Data were extracted using Microsoft excel 2016 and analyzed using STATA 11.0 statistical software. Heterogeneity among studies was assessed using the Cochran Q statistics and I2 test. The pooled effect sizes were determined using pooled proportion for the full vaccination coverage and odds ratios for the associated factors with the corresponding 95% confidence interval.
Result: Sixteen studies with 8305 children aged 12–23 months were included. The overall pooled full vaccination coverage was 65% (95% CI: 56%-74%). Institutional delivery (OR: 2.12, 95% CI: 1.78–2.52), travel to vaccination site for <2 hours (OR: 2.43, 95%CI: 1.97–3.00), received at least one antenatal (ANC) visit (OR: 3.2, 95%CI: 2.46–4.1), good maternal knowledge of immunization (OR: 3.63, 95%CI: 2.82–4.67), being informed on immunization schedule (OR: 2.54, 95%CI: 2.02–3.2), living in urban areas (OR: 2, 95% CI: 1.54–2.6), and a household visit by health-care providers during the postnatal period (OR: 2.23, 95%CI: 1.22–4.09) were the independent predictors of full immunization coverage among children age 12–23 months.
Conclusion: The study showed that the pooled full immunization coverage is still far from the national target (90%). Therefore, the government should strengthen both the outreach and facility-based immunization services.
KEYWORDS: Vaccination, immunization, systematic review, meta-analysis, Ethiopia
Background
Immunization is the process whereby a person is made immune or resistant to an infectious disease by the administration of an antigen called vaccine.1,2 Full immunization coverage is a powerful public health strategy for improving child survival and the prevention of morbidity and mortality associated with common childhood illnesses.3 Although the global immunization coverage has been increased during the past decades, it has however remained stagnant in recent years.4–6 According to the report from the World Health Organization (WHO), an estimated 22 million infants remained unvaccinated globally.7 Moreover, global reports showed that millions of children did not receive their full course of vaccinations every year.2,5,8 Furthermore, a significant number of children in Low- and Middle-Income countries (LMICs) remaining unvaccinated, under-vaccinated, and still dying from vaccine-preventable diseases.9–11
Tremendous progress has been made in expanding immunization in African countries over the last four decades. However, about 20–30% of children remained unvaccinated in these countries.11 Besides, the full immunization coverage in LMICs remained between 56% and 69%. An estimated 4.3 million unimmunized infants are located only in four African countries; the Democratic Republic of the Congo, Ethiopia, Nigeria, and South Africa.12,13 Moreover, close to 19% of children aged 12–23 months did not receive any vaccination in Ethiopia. Studies in Ethiopia revealed that full immunization coverage varied greatly in the country ranging from 22.9% to 91.7%.6,14–19 Therefore, the pooled estimate of vaccination coverage from this study will provide more reliable information regarding the vaccination coverage in the country.
Several studies conducted across the globe identified different factors associated with full immunization coverage. Wealth index, educational status, ANC, birthplace, and residence were among the major predictors.6,17,18 Furthermore, maternal knowledge of immunization, maternal age, maternal education, type of pregnancy, and a household visit by health-care workers were other factors of full immunization coverage in Ethiopia.14–16,19 However, limited and inconclusive studies have been conducted to determine the full immunization coverage and associated factors in Ethiopia. Therefore, this review and meta-analysis were aimed to estimate the pooled full immunization coverage and associated factors in Ethiopia.
Methods and materials
Study setting and period
This systematic review and meta-analysis were conducted in Ethiopia from March 1 to August 30, 2020. Ethiopia is a multiethnic, multilingual, and multicultural country in east Africa with a total population of more than 109 million. The country has a total area of 1.1 million square kilometers with a border of Eritrea to the North, Djibouti to the Northeast, Somalia to the East, Kenya to the South, South Sudan to the West, and Sudan to the Northwest.20
Study design
A systematic review and meta-analysis of observational studies were conducted to determine the pooled vaccination coverage and its determinants among children age 12–23 months in Ethiopia. The review and analysis were registered with PROSPERO/International Prospective Register of Systematic Reviews (CRD42020157887)/https://www.crd.york.ac.uk/prospero/
Search strategy
Appropriate and comprehensive searches for international databases: Public Medline (PubMed), Health Inter-Network Access to Research Initiative (HINARI), google scholar, Excerpta Medica Database (EMBASE), Cumulative Index of Nursing and Allied Health Literature (CINAHL), Scopus, African Journal of Online (AJOL), and the Cochran library were conducted. Additional studies were also identified from reference lists of the retrieved articles, gray literature (Academic Open Access Repositories, WorldWideScience, Mednar, and pre-print articles), and manual searching of relevant publications. A Medical Subject Headings (MeSH) thesaurus and keyword terms and phrases were used both in separation and in combination using the Boolean operators “OR” and “AND” to search for eligible articles. The authors were used the following search strategies to find all the necessary databases in PubMed: ((“full Immunization” OR “full Vaccination”) AND (Coverage OR Proportion OR Magnitude OR Prevalence) AND (Determinants OR Predictors OR “Risk factors” OR Causes) AND (children OR “under 2 years” OR “12–23 months” OR toddlers) AND (Ethiopia OR Ethio)). The literature search was restricted to the English language and human study groups and also records were managed using the EndNote X8 reference manager.
Inclusion and exclusion criteria
The inclusion criteria were: 1) Studies among 12–23 months old child conducted in Ethiopia; 2) Observational studies (cross-sectional, case-control, cohort studies); 3) Studies reported the full vaccination coverage; 4) English language articles published in a peer-reviewed journal from 2013 to 2020 (Starting from the introduction of PCV and Rota vaccines to 2020). Whereas articles that were not fully accessed or failed to contact the primary author, case reports, and expert opinions were excluded.
Outcome measurements
The primary outcome of this systematic review and meta-analysis was the pooled full immunization coverage. Full immunization coverage is the percentage of target populations (12–23 months) who have received all the full course of recommended vaccines in the national immunization schedule of Ethiopia (A single dose of Bacillus Calmette–Guérin (BCG); three doses of polio vaccine; three doses of pneumococcal conjugate vaccine (PCV); two doses of rotavirus; three doses of pentavalent vaccines (diphtheria, tetanus, pertussis, hepatitis B and Haemophilus influenzae type B vaccine (DTP-HepBHib)) and a single dose of measles vaccine). Secondarily the associated factors of full immunization coverage were considered in the review and meta-analysis. These predictors of full vaccination coverage were determined using the log odds ratio.
Data extraction
Relevant data were extracted using Microsoft excel 2016 computer program. Pilot testing the extraction form prior to the commencement of the review was done. Two different investigators (GB & AW) extract data from each study independently based on the study objectives; thereafter, the extracted data were exported to STATA 11 statistical software for analysis. Disagreements were resolved by discussion; however, if failed to reach consensus, a third reviewer (SM) was consulted. For each included article; the first author name, year of publication, the study setting, study design, study period, sample size, response rate, outcome definition, comparison group, and the effect estimate were recorded.
Risk of bias
The quality of each study was assessed using the NOS adapted for meta-analysis. Studies were assessed for representativeness of sample size, non-respondents, ascertainment of exposure, comparability, assessment of the outcome, and statistical test. We assigned stars to evaluate study quality, with 9–10 stars indicating “very good” quality, 7–8 stars indicating “good” quality, 5–6 stars indicating “satisfactory” quality, and 0–4 stars indicating “unsatisfactory” quality. Two authors (SM and GB) assessed the quality appraisal independently and the average assessment scale of the two authors was used for the final decision.21
Publication bias and heterogeneity
Statistical heterogeneity was determined and quantified using Cochran’s Q statistic and the I2 test statistic. A p-value less than 0.05 of the Cochran’s Q statistic was used to declare heterogeneity and the I2 test statistics of 25%, 50%, and 75% were declared as low, moderate, and high heterogeneity, respectively. The possible risk of publication bias was examined by the inspection of the funnel plot, Begg’s correlation, and Egger’s regression test. Subgroup analysis was conducted by region and sample size to minimize random variation among studies. Lastly, a sensitivity analysis was performed to examine the influence of a single study on the overall estimate.
Analysis
After defining the included studies, relevant data from each primary studies were extracted using Microsoft excel 2016 computer program. Then, the extracted data were exported into STATA 11 statistical software for analysis. A random-effect model was used to estimate the pooled prevalence of full vaccination coverage whereas a fixed effect model was applied for the analysis of the associated factors. Further statistical analyses like subgroup analysis, publication bias, and sensitivity analysis were performed.
Results
Study screening process
In the initial search, a total of 1244 records were identified; 1127 records from online databases and 117 records from other sources (WorldWideScience, Mednar, and pre-print articles, Academic Open Access Repositories). After importing all the retrieved articles to the EndNote X8, 784 articles were excluded due to duplications. The title of 460 articles was checked and 300 articles were removed due to unrelated title. Then, the abstract of 160 articles was reviewed and 120 articles were removed by reason. Finally, the full text of 40 articles was reviewed and 16 were selected based on the inclusion criteria. The list of all included articles was prepared for data extraction and further analysis. The Preferred Reporting Item for Systematic Review and Meta-analysis (PRISMA) flow diagram was applied to summarize and synthesize the selection process of the included articles (Figure 1).22
Figure 1.
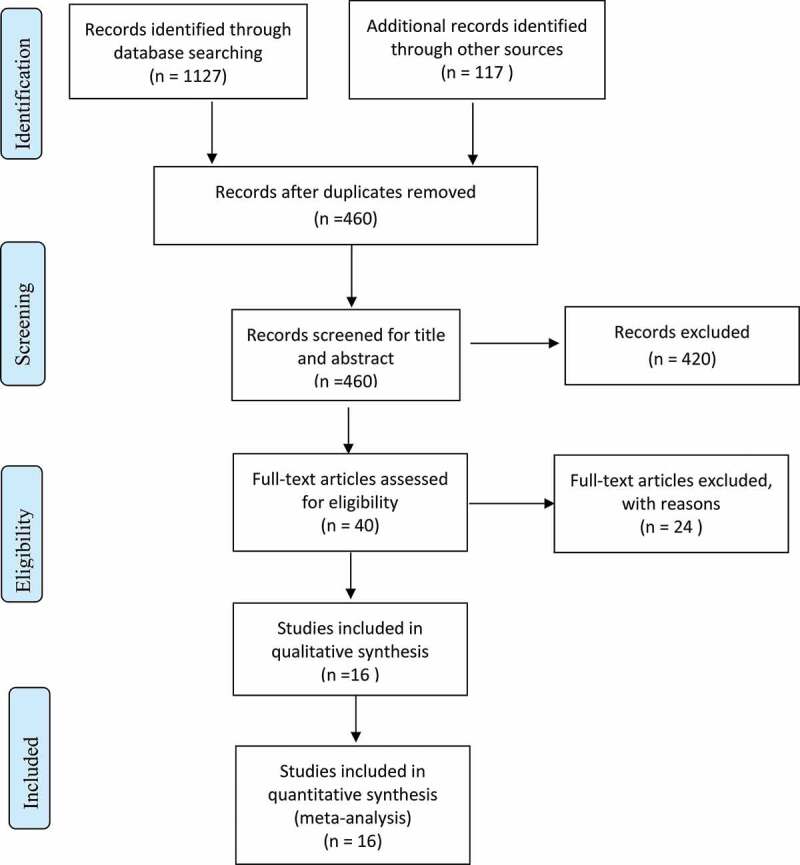
Flow chart illustrating the process of search and selection of studies included in the present systematic review and meta-analysis
Study characteristics
From the total of 16 included studies; 4 studies were conducted in Oromia region,23–26 6 in Amhara region,4,27–31 5 in South Nation Nationality and People (SNNP)15,32–35 and 1 in Somalia region.19 All the studies were cross-sectional in design with the minimum and maximum sample sizes of 173 and 846, respectively. The highest full vaccination coverage was reported in Amhara region (91.7%),29 whereas the lowest coverage was reported in Oromia region (22.9%)25 (Table 1).
Table 1.
Summary of relevant characteristics of the main findings of the included studies among children 12–23 months from 2013 to 2020 in Ethiopia
| Authors, Year | Region | Study design | Sample Size | Event | Prevalence | Response Rate | Quality Score |
|---|---|---|---|---|---|---|---|
| Worku A. et al, 2014 | Oromia | Cross sectional | 630 | 461 | 73.2 | 100% | 9 |
| Wolde Facha, 2015 | SNNP | Cross sectional | 210 | 112 | 53.3 | 100% | 7 |
| Melkamu B. et al, 2015 | Amhara | Cross sectional | 757 | 571 | 76 | 99% | 8 |
| Tadesse D. et al, 2019 | Amhara | Cross sectional | 629 | 657 | 72.6 | 98.7 | 8 |
| Tenaw G. et al, 2017 | Amhara | Cross sectional | 298 | 264 | 91.7 | 96.6 | 7 |
| Yemesrach A. et al,2018 | SNNP | Cross sectional | 541 | 297 | 61 | 90 | 8 |
| Robera O. et al, 2019 | SNNP | Cross sectional | 173 | 130 | 75.4 | 100 | 6 |
| Abdi Nur M. et al, 2014 | Somali | Cross sectional | 582 | 434 | 74.6 | 100 | 7 |
| Ayal Debie, 2014 | Oromia | Cross sectional | 497 | 245 | 49.3 | 100 | 8 |
| Alemayehu Gonie, 2019 | Amhara | Cross sectional | 566 | 428 | 75.6 | 98.8 | 7 |
| Asrat Meleko, 2017 | SNNP | Cross sectional | 322 | 136 | 42.2 | 100 | 8 |
| Tadesse Dagget, 2018 | Amhara | Cross sectional | 846 | 494 | 58.4 | 98.11 | 9 |
| Hussen M. et al, 2013 | Oromia | Cross sectional | 694 | 159 | 22.9 | 98.7 | 6 |
| Elias L. et al, 2015 | SNNP | Cross sectional | 606 | 454 | 76.8 | 98.5 | 8 |
| Abadi G et al, 2019 | Amhara | Cross sectional | 623 | 480 | 77.4 | 99.5 | 7 |
| Takele T. et al, 2019 | Oromia | Cross sectional | 331 | 215 | 64.8 | 100 | 5 |
Pooled full immunization coverage
In this review and meta-analysis, a total of 16 studies with 8305 children aged 12–23 months were included. The overall pooled full immunization coverage was 65% (95% CI: 56%, 74%). High heterogeneity was observed among the included studies (I2 = 98.9%, p < .001). Due to the heterogeneity of included studies, subgroup analysis was done by region and sample size. The random-effect model was applied for reporting the pooled estimate of full immunization coverage whereas a fixed effect model was used for analyzing the associated factors (Figure 2).
Figure 2.
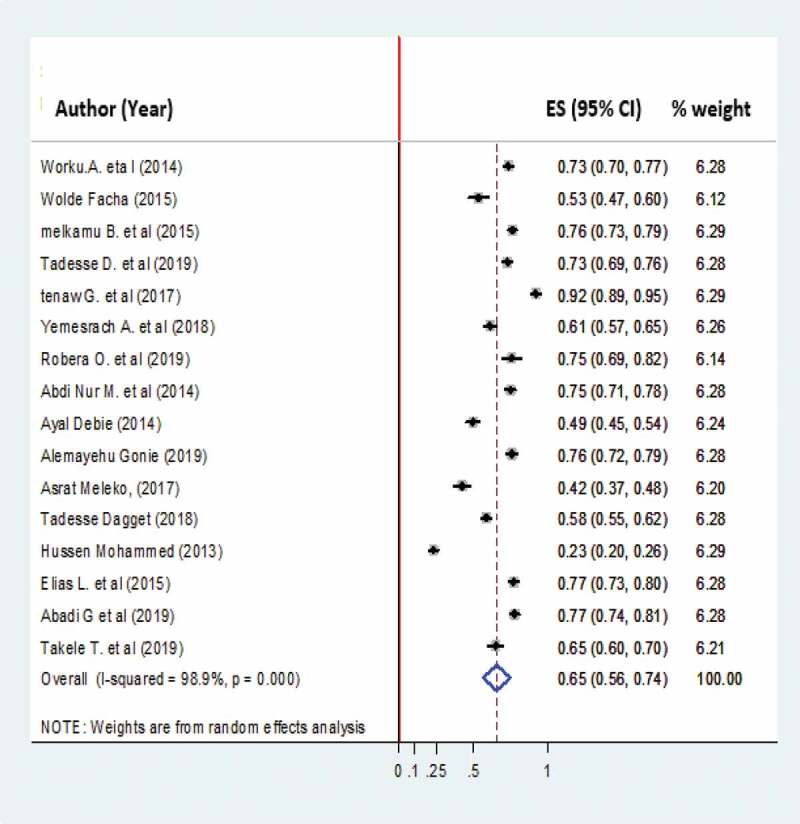
Pooled full immunization coverage among children 12–23 months in Ethiopia from 2013 to 2020
Subgroup analysis
Subgroup analysis was conducted based on region and sample size. Northern Ethiopia had the highest prevalence of pooled full vaccination coverage (75%) followed by southern Ethiopia (62%) and eastern Ethiopia (57%). Subgroup analysis regarding the sample size indicated that the prevalence of pooled full vaccination coverage was almost similar between categories with 65% for sample size <380 and 66% for sample size >380. Studies with a sample size of more than 380 had the highest weight (69.04%), the possible reason for this might be the number of studies (Figs3&4)
Figure 3.
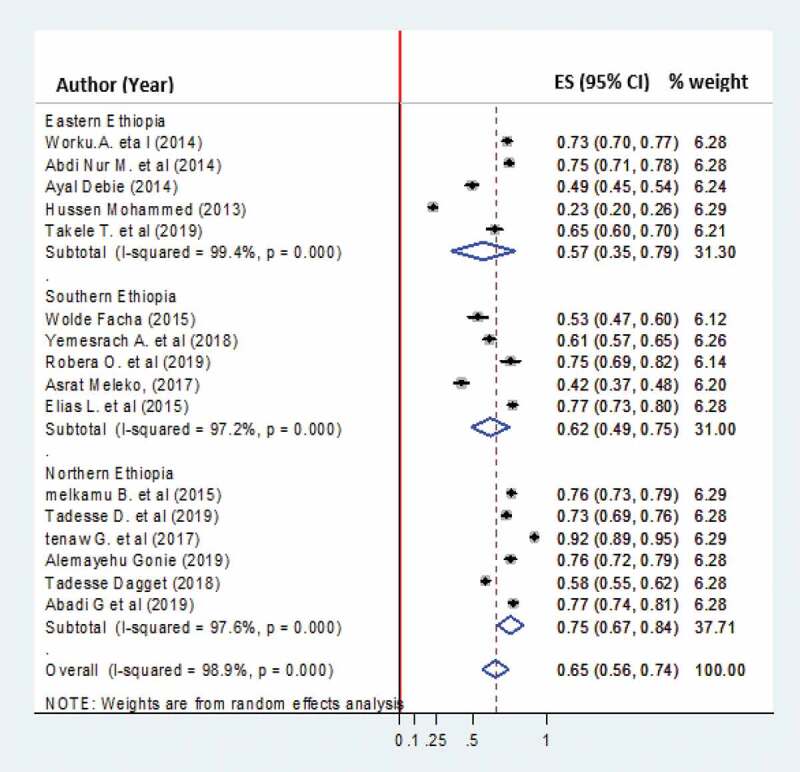
The forest plot of subgroup analysis of the study full immunization coverage among 12–23 month child based on regions in Ethiopia
Figure 4.
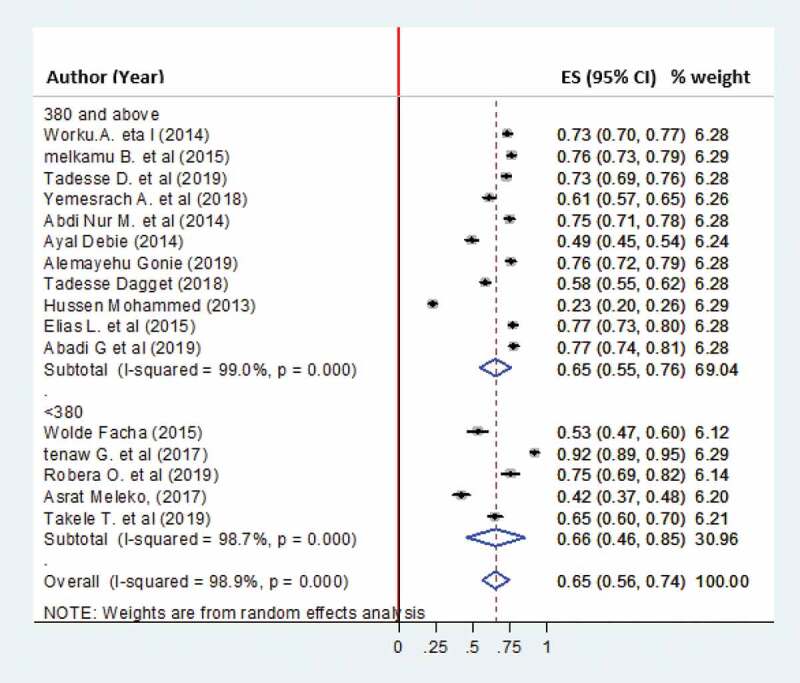
The forest plot of subgroup analysis of the study full immunization coverage among 12–23 month child based on sample size in Ethiopia
Meta-regression and sensitivity analysis
Meta-regression with a random effect model was conducted by considering publication year and sample size as covariates. The result showed that no heterogeneity was observed by sample size (p = .928) and publication year (p = .168). Furthermore, a sensitivity analysis was performed with the random effect model to see the effect of a single study on the overall estimate of full immunization coverage. However, the sensitivity analysis showed no evidence for the influence of a single study on the overall estimate of full immunization coverage (Figure 5).
Figure 5.
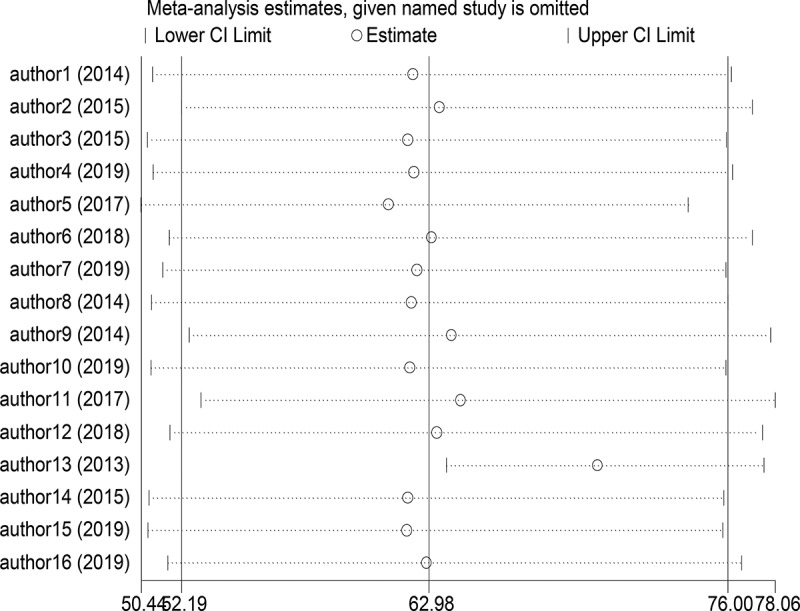
Sensitivity analysis for the study full immunization coverage and associated factors among 12–23 month child in Ethiopia
Publication bias
The likely of publication bias across studies was evaluated using observation of funnel plot and p-values of begs correlation and Egger’s regression test. The visual inspection of the funnel plot was symmetrical which indicates no publication bias. In addition, Begg’s correlation and Egger’s regression tests showed that there was no statistically significant publication bias across the included articles (p-value = 0.053 and 0.496, respectively) (Figure 6).
Figure 6.
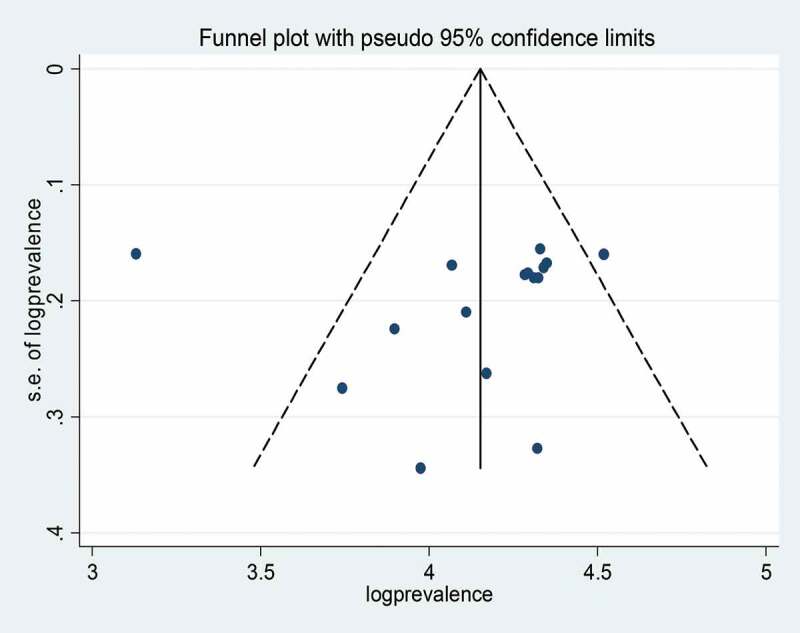
Funnel plot of effect estimate against the standard error of log estimate
Factors associated with full immunization coverage (Table 1Table 2)
Table 2.
Meta-analysis finding showing factors associated with full immunization coverage in Ethiopia (n = 8305)
| Variables | OR, 95%CI | Heterogeneity | No of studies |
|---|---|---|---|
| Institutional delivery | 2.12 (1.78–2.52) | I2 = 0.0%, p = .811 | 8 |
| Distance to vaccination site ≤1 hr | 2.43 (1.97–3.00) | I2 = 0.0%, p = .793 | 7 |
| Received at least one ANC follow up | 3.20 (2.46–4.10) | I2 = 0.0%, p = .863 | 7 |
| Good maternal knowledge of immunization | 3.63 (2.82–4.67) | I2 = 57.1%, p = .053 | 5 |
| Being informed about Immunization schedule | 2.54 (2–02-3.20) | I2 = 63.3%, p = .043 | 4 |
| Urban Residency | 2 (1.54–2.6) | I2 = 0.0%, p = .938 | 4 |
| Received home visit by health care workers | 2.23 (1.22–4.09) | I2 = 0.0%, p = .883 | 3 |
Place of delivery and full immunization coverage
In this meta-analysis, the association of place of delivery with full immunization coverage was examined using eight studies.4,19,23–25,31,32,35 The finding showed that children born at the health facilities were 2 times more likely to be fully vaccinated compared to those children born outside of the health institution [OR: 2.12, 95% CI: 1.78,2.52, I2 = 0.0%, P = .811].
Distance from immunization site and full immunization coverage
The statistical test of association between distance from the immunization site and full immunization coverage was assessed using seven studies.4,15,28–31,33 The result showed that mothers who reside near to the immunization site (less than 2 hours travel) were 2.4 times more likely to get their child vaccinated compared to mothers residing far from the health institution (>2 hours travel) [OR: 2.43, 95%CI: 1.97–3, I2 = 0.0%, p = .79].
Antenatal visit and full immunization coverage
Similarly, seven primary studies were used to determine the association between maternal ANC visit and Full Immunization Coverage.4,15,28,29,31–33 Pregnant mothers having at least one ANC visit were 3 times more likely to get their child vaccinated compared to mothers with no ANC visit [OR: 3.2, 95%CI: 2.46–4.10, I2 = 0.0%, p = .86].
Maternal knowledge and full immunization coverage
The effect of maternal knowledge on full immunization coverage was examined using five studies.15,24,25,31,35 The test result showed that the odds of full immunization was 3.6 times higher among children born to mothers with better knowledge of immunization [OR: 3.63, 95%CI: 2.82–4.67, I2 = 57%, P = .053].
Immunization schedule and full immunization coverage
Four primary studies were used to assess the association between immunization schedule and full vaccination coverage.4,23,27,32 Women being informed of all the national immunization programs were 2.5 times more likely to get their child fully vaccinated compared to mothers with no information regarding to the national immunization schedule [OR: 2.54, 95%CI: 2.02–3.20, I2 = 63%, p = .043].
Maternal residence and full immunization coverage
In this review and meta-analysis, four individual studies were included to the examine the association between maternal residence and full immunization coverage.4,19,24,27 The test had revealed significant association between maternal residence and full immunization coverage [OR: 2, 95%CI: 1.54–2.60, I2 = 0.0%, p = .94].
Household visit and full immunization coverage
Three individual studies were included to determine the association between a household visits by the health-care providers and full immunization coverage.19,24,25 Young children who visited by health-care professionals were nearly 2 times more likely to get full immunization compared to children who did not visited by health-care workers [OR: 2.23, 955 CI: 1.22–4.09, I2 = 0.0%, p = .88].
Discussion
This systematic review and meta-analysis were the first to systematically explore and integrate the evidences available on full vaccination coverage and its associated factors in Ethiopia. Through gathering and summarizing all available facts about full immunization coverage and associated factors, we came up with strong evidence regarding full immunization coverage and associated factors. The knowledge derived from this review and meta-analysis could help policymakers and program managers to design the appropriate strategies and interventions to improve childhood immunization in the country.
In this study, the overall pooled full immunization coverage was 65% (95% CI: 56%-74%). The finding was comparable with the global immunization coverage (57.8%),36 pooled full vaccination coverage in Ethiopia (60%),37 Demographic and Health Survey (DHS) report in Kenya (67.2%),38 South Africa (61%)39 and India 62%.40 The similarity could be due to the implementation of similar child health programs including immunization services by the world health organization and other non-governmental organizations across the globe and a similar program is implemented in Ethiopia.
However, the finding was higher than the Ethiopian and Demographic and Health Survey (EDHS) reports of 2016 (39%)6 and the EDHS report of 2019 (43%).17 The discrepancy could be explained that the EDHS survey involves large-scale areas including the unreached area of the country which may underestimate the report. Besides the finding was higher than the studies in LMICs (36%)41 and a similar finding in Nigeria (34.4%).42 The difference might be due to variation in the implementation and achievement of the immunization program across the regions.
The report from this meta-analysis was lower than the global report (86%),43 study in Eritrea (83%),44 and the finding in Malaysia (86.3)%.45 The possible reason for the difference could be explained the quality of health services and population differences in developed countries contributed to the higher achievement of full immunization. Moreover, Eretria won an award for the better achievement of childhood immunization program. In this meta-analysis, women having good knowledge of immunization were more likely to get their child fully immunized. The finding was similar to the study in Ethiopia,46 Sub-Saharan African (SSA),47 Malaysia,48 Nigeria,42 and England.49 This might be best explained that maternal knowledge regarding the importance of immunization improves their attitude toward the national immunization program and are more likely to vaccinate their child.
This study revealed that mothers who had ANC visit for the index child, children delivered at health facilities, and mothers who were informed about the schedule of immunization were more likely to vaccinate their children compared to their counterparts. The finding was similar to the study in Ethiopia.46 Women having ANC visits during pregnancy and gave birth at health facilities could have adequate counseling about the importance of childhood vaccination and could be more adhere to the immunization schedules.
In this study, children who were living near to the immunization site (less than 2 hours) were more likely to be fully vaccinated than those children who were living far away from the immunization center. The finding was similar to the studies conducted in Ethiopia,46 Nigeria,50 and SSA.47 This could be because parents who reside far from health institutions may not bring their child for immunization due to lack of transportation or lack of access to information regarding the immunization program.
Limitation of the study
The first limitation of this systematic review and meta-analysis was the involvement of articles published in the English language only. Besides, the current study was included studies conducted from 2013 to 2020 since rota and PCV vaccines were started in 2013 in Ethiopia.
Conclusion
The full immunization coverage of Ethiopia was lower than the 2020 target. Several factors were responsible for the low achievement of full immunization coverage in the country. Therefore, the government should strengthen the expansion of immunization services by giving a focus for outreach programs to reach hard-to-reach areas of the country. Besides, health-care workers should integrate child vaccination services with other health services like maternal health-care services.
Acknowledgments
We would like to acknowledge Wollo University librarian and ICT complex staffs for availing an uninterrupted internet connection for searching important resources for this systematic review and meta-analysis. We would also like to thank all our colleagues for their unreserved help during the write up of this systematic review and meta-analysis.
Abbreviations
- ANC
Ant-natal Care.
- EDHS
Ethiopian Demographic Health.
- LMICs
Low and Middle-Income Countries.
- MeSH
Medical Subject Headings.
- NOS
Newcastle Ottawa Scale.
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-Analysis.
- SNNP
South Nation Nationality and Peoples.
- SSA
Sub-Saharan Countries
- WHO
World Health Organization
Disclosure of potential conflicts of interest
The authors have declared that there are no competing interests.
Authors contribution
GB conceived and designed the protocol. AW and MT wrote the first draft of the protocol. All authors wrote and developed the protocol. SM and MT designed a search strategy and conduct the quality assessment. GB and AW read and approved the final protocol, conduct data extraction, and analysis. All authors were involved in the final write up of the systematic review and meta-analysis. All authors read and approved the final draft of the review and meta-analysis.
References
- 1.Subaiya S, Dumolard L, Lydon P, Gacic-Dobo M, Eggers R, Conklin L.. Global routine vaccination coverage, 2014. Morbidity Mortality Weekly Rep. 2015;64(44):1252–55. doi: 10.15585/mmwr.mm6444a5. [DOI] [PubMed] [Google Scholar]
- 2.Vakili R, Ghazizadeh Hashemi A, Khademi G, Ajilian Abbasi M, Saeidi M. Immunization coverage in WHO regions: a review article. Int J Pediatr. 2015;3:111–18. [Google Scholar]
- 3.VanderEnde K, Gacic-Dobo M, Diallo MS, Conklin LM, Wallace AS. Global Routine Vaccination Coverage-2017. MMWR. 2018;67(45):1261. doi: 10.15585/mmwr.mm6745a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tesfaye TD, Temesgen WA, Kasa AS. Vaccination coverage and associated factors among children aged 12–23 months in Northwest Ethiopia. Human Vaccines Immuno-Therapeutics. 2018;14(10):2348–54. doi: 10.1080/21645515.2018.1502528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feldstein LR, Mariat S, Gacic-Dobo M, Diallo MS, Conklin LM, Wallace AS. Global routine vaccination coverage, 2016. MMWR. 2017;66(45):1252. doi: 10.15585/mmwr.mm6645a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Central Statistical Agency (CSA) [Ethiopia] and ICF . Ethiopia Demographic and Health Survey 2016. Addis Ababa (Ethiopia): CSA and ICF; 2016. [Google Scholar]
- 7.Brown DW, Burton A, Gacic-Dobo M, Karimov RI, Vandelaer J, Okwo-Bele JM. A mid-term assessment of progress towards the immunization coverage goal of the Global Immunization Vision and Strategy (GIVS). BMC Public Health. 2011;11(1):806. doi: 10.1186/1471-2458-11-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris JB, Gacic-Dobo M, Eggers R, Brown DW, Sodha SV. Global routine vaccination coverage, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:1055. [PMC free article] [PubMed] [Google Scholar]
- 9.Mihigo R, Anya B, Okeibunor J, Poy A, Machingaidze S, Wiysonge C. Routine immunization in the WHO African Region: progress, challenges, and way forward. Afr Health Monit. 2015;19:2–4. [Google Scholar]
- 10.Nshimirimana D, Mihigo R, Clements CJ. Routine immunization services in Africa: back to basics. J Vaccines Immun. 2013;1:6–12. doi: 10.14312/2053-1273.2013-2. [DOI] [Google Scholar]
- 11.Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle-income countries: findings from a systematic review of the published literature, 1999–2009. Vaccine. 2011;29(46):8215–21. doi: 10.1016/j.vaccine.2011.08.096. [DOI] [PubMed] [Google Scholar]
- 12.Restrepo-Méndez MC, Barros AJ, Wong KL, Johnson HL, Pariyo G, França GV, Wehrmeister FC, Victora CG. Inequalities in full immunization coverage: trends in low-and middle-income countries. Bull World Health Organ. 2016;94(11):794. doi: 10.2471/BLT.15.162172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farzad F, Reyer JA, Yamamoto E, Hamajima N. Socio-economic and demographic determinants of full immunization among children of 12–23 months in Afghanistan. Nagoya J Med Sci. 2017;79(2):179. doi: 10.18999/nagjms.79.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abebe AM, Kassaw MW, Birara A. Coverage, Opportunity, and Challenges of expanded Program on Immunization among 12-23 Months old Children in Woldia Town, Northeast Ethiopia, 2018. BioMed Research International. 2019 Dec 31;2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Legesse E, Dechasa W. An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia. BMC Pediatr. 2015;15(1):31. doi: 10.1186/s12887-015-0345-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lakew Y, Bekele A, Biadgilign S. Factors influencing full immunization coverage among 12–23 months of age children in Ethiopia: evidence from the national demographic and health survey in 2011. BMC Public Health. 2015;15(1):728. doi: 10.1186/s12889-015-2078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF . Ethiopia Mini Demographic and Health Survey 2019: key Indicators. Rockville (Maryland): EPHI and ICF; 2019. [Google Scholar]
- 18.Dessie DB, Negeri MA. Determining factors of full immunization of children among 12-23 months old in rural Ethiopia. Am J Public Health. 2018;6:160–65. [Google Scholar]
- 19.Mohamud AN, Feleke A, Worku W, Kifle M, Sharma HR. Immunization coverage of 12–23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health. 2014;14(1):1–9. doi: 10.1186/1471-2458-14-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Federal Democratic Republic of Ethiopia Ministry of Health (FDRE-MoH) [Ethiopia] . 2010. Health Sector Development Program IV, 2010/11—2014/15.
- 21.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–05. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Animaw W, Taye W, Merdekios B, Tilahun M, Ayele G. An Expanded program of immunization coverage and associated factors among children age 12–23 months in Arba Minch town and Zuria District, Southern Ethiopia, 2013. BMC Public Health. 2014;14(1):464. doi: 10.1186/1471-2458-14-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Debie A, Taye B. Assessment of full vaccination coverage and associated factors among children aged 12–23 months in Mecha District, North West Ethiopia: a cross-sectional study. Sci J Public Health. 2014;2(4):342–48. doi: 10.11648/j.sjph.20140204.26. [DOI] [Google Scholar]
- 25.Mohammed H, Atomsa A. Assessment of child immunization coverage and associated factors in Oromia regional state, eastern Ethiopia. Sci Technol Arts Res J. 2013;2(1):36–41. doi: 10.4314/star.v2i1.98842. [DOI] [Google Scholar]
- 26.Tiki T, Likassa T, Endalew D, Tolessa A. Immunization coverage and associated factors among children in Bila Town, West Wellega Zone, Oromia Regional State, Western Ethiopia. Acta Sci Med Sci. 2019;3(11):54–58. doi: 10.31080/ASMS.2019.03.0440. [DOI] [Google Scholar]
- 27.Kassahun MB, Biks GA, Teferra AS. Level of immunization coverage and associated factors among children aged 12–23 months in Lay Armachiho District, North Gondar Zone, Northwest Ethiopia: a community-based cross-sectional study. BMC Res Notes. 2015;8(1):1–10. doi: 10.1186/s13104-015-1192-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Desalegn T, Shiferaw MB, Tesfahun E, Moges A, Semunigus T. Vaccination coverage and associated factors among children in Debre Berhan Town, Ethiopia. Recent Adv Biol Med. 2019;5(2019):11536. doi: 10.18639/RABM.2019.961845. [DOI] [Google Scholar]
- 29.Gualu T, Dilie A. Vaccination coverage and associated factors among children aged 12–23 months in Debre Markos town, Amhara regional state, Ethiopia. Adv Public Health. 2017;2017. doi: 10.1155/2017/5352847. [DOI] [Google Scholar]
- 30.Mekonnen AG, Bayleyegn AD, Ayele ET. Immunization coverage of 12–23 months old children and its associated factors in Minjar-Shenkora district, Ethiopia: a community-based study. BMC Pediatr. 2019;19(1):1–8. doi: 10.1186/s12887-019-1575-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Girmay A, Dadi AF. Full immunization coverage and associated factors among children aged 12-23 months in the hard-to-reach areas of Ethiopia. Int J Pediatr. 2019;2019. doi: 10.1155/2019/1924941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Facha W. Vaccination coverage and associated factors among children aged 12 to 23 months in Arba Minch Zuriya Woreda, Southern Ethiopia. J Pharm Alternat Med. 2015;v7:16–25. [Google Scholar]
- 33.Tefera YA, Wagner AL, Mekonen EB, Carlson BF, Boulton ML. Predictors and barriers to full vaccination among children in Ethiopia. Vaccines. 2018;6(2):22. doi: 10.3390/vaccines6020022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fite RO, Hailu LD. Immunization coverage of 12 to 23 months old children in Ethiopia. J Public Health Epidemiol. 2019;11(1):31–37. doi: 10.5897/JPHE2018.1071. [DOI] [Google Scholar]
- 35.Meleko A, Geremew M, Birhanu F. Assessment of child immunization coverage and associated factors with full vaccination among children aged 12–23 months at Mizan Aman town, Bench Maji zone, Southwest Ethiopia. Int J Pediatr. 2017;2017. doi: 10.1155/2017/7976587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Forshaw J, Gerver SM, Gill M, Cooper E, Manikam L, Ward H. The global effect of maternal education on complete childhood vaccination: a systematic review and meta-analysis. BMC Infect Dis. 2017;17(1):801. doi: 10.1186/s12879-017-2890-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ketema DB, Assemie MA, Alamneh AA, Alene M, Chane KY, Alamneh YM, Birhanu MY, Alebel A. Full vaccination coverage among children aged 12–23 months in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20:1–10. doi: 10.1186/s12889-020-08940-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Demographic K: Health Survey 2014: key indicators . Kenya National Bureau of Statistics (KNBS) and ICF Macro 2014. 8, 166–206.
- 39.National Development of Health (NDoH), Statistics South Africa (Stats SA), South African Medical Research Council (SAMRC), and ICF . South Africa Demographic Health and Survey 2016: key Indicators. Pretoria (South Africa): NDoH, Stats SA, SAMRC, and ICF; 2017. [Google Scholar]
- 40.International Institute for Population Sciences (IIPS) and ICF . National Family Health Survey (NFHS-4), 2015-16: Mumbai (India): IIPS; 2017. [Google Scholar]
- 41.Lukusa LA, Ndze VN, Mbeye NM, Wiysonge CS. A systematic review and meta-analysis of the effects of educating parents on the benefits and schedules of childhood vaccinations in low and middle-income countries. Hum Vaccin Immunother. 2018;14(8):2058–68. doi: 10.1080/21645515.2018.1457931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adeloye D, Jacobs W, Amuta AO, Ogundipe O, Mosaku O, Gadanya MA, Oni G. Coverage and determinants of childhood immunization in Nigeria: a systematic review and meta-analysis. Vaccine. 2017;35(22):2871–81. doi: 10.1016/j.vaccine.2017.04.034. [DOI] [PubMed] [Google Scholar]
- 43.Peck M, Gacic-Dobo M, Diallo MS, Nedelec Y, Sodha SS, Wallace AS. Global routine vaccination coverage, 2018. MMWR. 2019;68(42):937. doi: 10.15585/mmwr.mm6842a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kibreab F, Lewycka S, Tewelde A. Impact of mother’s education on full immunization of children aged 12–23 months in Eritrea: population and health survey 2010 data analysis. BMC Public Health. 2020;20(1):1–10. doi: 10.1186/s12889-020-8281-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lim K, Chan Y, Ani AN, Rohani J, Norfadhilah ZS, Santhi M. Complete immunization coverage and its determinants among children in Malaysia: findings from the National Health and Morbidity Survey (NHMS) 2016. Public Health. 2017;153:52–57. doi: 10.1016/j.puhe.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 46.Eshete A, Shewasinad S, Hailemeskel S. Immunization coverage and its determinant factors among children aged 12–23 months in Ethiopia: a systematic review, and meta-analysis of cross-sectional studies. BMC Pediatr. 2020;20(1):1–13. doi: 10.1186/s12887-020-02163-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bangura JB, Xiao S, Qiu D, Ouyang F, Chen L. Barriers to childhood immunization in sub-Saharan Africa: A systematic review. BMC Public Health. 2020;20(1):1–15. doi: 10.1186/s12889-020-09169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nor Afiah MZ, Mohammad FR, Juni MH. Adherence among parents on under-five childhood immunization schedule: a review. Int J Public Health Clin Sci. 2016;3:11–34. [Google Scholar]
- 49.Smith LE, Amlôt R, Weinman J, Yiend J, Rubin GJ. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35(45):6059–69. doi: 10.1016/j.vaccine.2017.09.046. [DOI] [PubMed] [Google Scholar]
- 50.Sato R. Association between access to a health facility and continuum of vaccination behaviors among Nigerian children. Hum Vaccin Immunother. 2020;16(5):1215–20. doi: 10.1080/21645515.2019.1678360. [DOI] [PMC free article] [PubMed] [Google Scholar]


