Abstract
In low‐ and middle‐income countries (LMICs), access to water, sanitation and hygiene (WASH) is associated with nutritional status including stunting, which affects 144 million children under 5 globally. Despite the consistent epidemiological association between WASH indicators and nutritional status, the provision of WASH interventions alone has not been found to improve child growth in recent randomized control trials. We conducted a literature review to develop a new conceptual framework that highlights what is known about the WASH to nutrition pathways, the limitations of certain interventions and how future WASH could be leveraged to benefit nutritional status in populations. This new conceptual framework will provide policy makers, program implementors and researchers with a visual tool to bring into perspective multiple levels of WASH and how it may effectively influence nutrition while identifying existing gaps in implementation and research.
Keywords: child growth, hygiene, infections, nutritional status, sanitation, stunting, water supply
Key messages.
WASH is strongly associated with nutritional status of children and women in LMICs, and improvements in WASH could significantly reduce disease and nutritional deficits.
The WASH to nutrition conceptual framework presented here provides policy makers, program implementors and researchers with a comprehensive tool to design and implement WASH interventions at multiple levels.
Evidence for effective low‐cost WASH interventions and their impact on nutritional status is lacking; additional investments in ‘transformative WASH’ are warranted.
Incremental, systems‐level improvements in drinking water and sanitation services are likely to have the most meaningful impact on population nutritional status and health in LMICs.
1. INTRODUCTION
In low‐ and middle‐income countries (LMICs), poor nutrition among women and children remains a persistent problem that has far reaching consequences for population health and human capital (Black et al., 2013; UNICEF, WHO, & World Bank Group, 2020; Victora et al., 2008). The association of poor nutritional status with diverse and interconnected determinants has led to a global call for multisectoral approaches to combat nutritional issues (Reinhardt & Fanzo, 2014). For decades, epidemiologic studies have revealed how household level access to and quality of water, sanitation and hygiene (WASH) facilities are associated with child stunting, wasting and maternal and child micronutrient deficiencies (Checkley et al., 2004; Danaei et al., 2016; Esrey, 1996). The significant improvements in population health and child mortality that were correlated with WASH advancements in the late 19th and early 20th centuries further support the potential for WASH interventions in LMICs to improve nutritional status and health (Alsan & Goldin, 2019; Cain & Rotella, 2001; Cutler & Miller, 2005; Kesztenbaum & Rosenthal, 2014; Ogasawara et al., 2018).
WASH interventions are theorized to improve nutritional status by breaking the transmission of pathogens from the environment to the individual, thus reducing the nutrient needs required to combat infections and increasing their availability for growth and development (Mbuya & Humphrey, 2016). Strategies to achieve this have included the development of intervention packages with technological inputs and behaviour change communication delivered at the household or community level to reduce exposure to pathogens (Prendergast & Kelly, 2016). However, the current randomized control trial literature suggests such interventions are not effective in reducing enteropathogenic exposure to a level that impacts child growth in low‐income country settings (Humphrey et al., 2019; Luby et al., 2018; Null et al., 2018). These recent findings of the null effects of household‐level WASH interventions on child nutritional status has resulted in a challenge for policy makers, program implementors and the broader nutrition community in determining the role of WASH in multisectoral nutrition programs.
The aim of this paper is to present a conceptual framework for the WASH to nutrition pathways in LMICs. The nutrition community would benefit from a new framework that expands the view on WASH implementation beyond household level interventions, proposes new strategies and pathways that leverage WASH in nutrition programming and aligns with the Sustainable Development Goals (SDG) and the Joint Monitoring Program for Water Supply, Sanitation, and Hygiene (JMP) indicators. We sought to ground the framework in the current literature and to reconcile the findings from new randomized control trial evidence with the established observational and historical research.
2. METHODS
The framework was developed in three phases: (1) review of the literature, (2) technical document review and (3) expert consultation.
We started with a peer‐reviewed literature search to identify any papers that explore the role of water, sanitation and/or hygiene on nutritional outcomes among children and women of reproductive age in LMICs.
We searched the PubMed database for studies with WASH key words, nutrition terms and LMIC terms within the title or abstract (Table A1). We scanned titles and abstracts for relevancy and included papers that described a link between WASH and nutrition in LMICs. We excluded papers for the following reasons: (1) The measures of WASH were not relevant to maternal and child nutrition; (2) nutritional outcomes were not described; (3) studies did not involve human subjects (i.e., animal research); or (4) were not conducted in LMICs. Papers were categorized according to type: epidemiological or cross‐sectional associations, randomized control trials and conceptual or review papers. During the full text review, common themes and components emerged, and levels of organization were informed by previous frameworks. Specifically, the UNICEF framework for undernutrition (United Nations Children's Fund, 1998) was used as a basis for formulating a socioecological model for the multilevel linkages between WASH and nutrition that were revealed through the literature review.
In addition to the peer‐reviewed literature, we expanded our search to include technical documents that described the implementation of WASH services in LMIC settings. These included WHO and UNICEF materials that provided information on upstream factors, such as policy, governance, infrastructure and implementation of water and sanitation systems (World Health Organization, 2006, 2017, 2018; World Health Organization, UNICEF, & USAID, 2015; World Health Organization & United Nations Children's Fund, 2018). After incorporating these elements into the framework, we continued reviewing papers, iteratively adjusting the framework until reaching saturation, that is, when no new themes or components were found.
We convened a meeting of nutrition experts in October 2019 to gather feedback and comments on our new framework. We subsequently reached out to several academic and UN‐affiliated professionals to garner more feedback, but responses were disappointingly low. With help from two academic WASH and nutrition experts, subsequent iterations of the framework were developed that aligned the content and language with the current movements in the WASH‐nutrition field. We received constructive feedback on the inclusion of behaviour change communication strategies, on narrowing the breadth of upstream factors into more digestible components and in targeting to our selected audience.
3. RESULTS
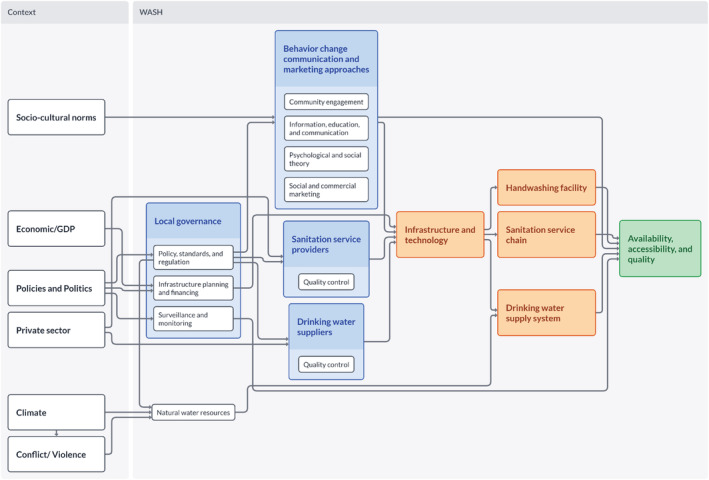
Figure 1 presents the high‐level visualization of our proposed WASH to nutrition conceptual framework. It follows a socioecological model, where elements within different levels of influence feed into each subsequent level, ultimately impacting the individual level outcomes. The broader context of a country, such as economy and policies, shapes the WASH sector at both the national and regional levels. While we refer to this level as the WASH sector, water and sanitation systems are generally separate entities but have the following commonalities: (1) require capacity/human resources, (2) utilize technologies and processes (i.e., service/supply chains) and (3) provide available, accessible, and quality services to consumers. The WASH domains influence the underlying causes of nutritional status, including health behaviours and exposure to pathogens. These in turn impact food intake and disease, labelled as immediate causes, which directly affect nutritional status and subsequently, morbidity and mortality. Sub‐elements and links are detailed in Figure S1. The scope of the framework was limited to the relationship between WASH and nutrition; however, we acknowledge the numerous contributors to nutritional status outside of WASH and the existence of WASH‐related outcomes beyond nutrition. We will take a deeper dive into the conceptual framework by starting on the right‐hand side, with the immediate causes, and move our way left towards the underlying, WASH and contextual contributors.
FIGURE 1.
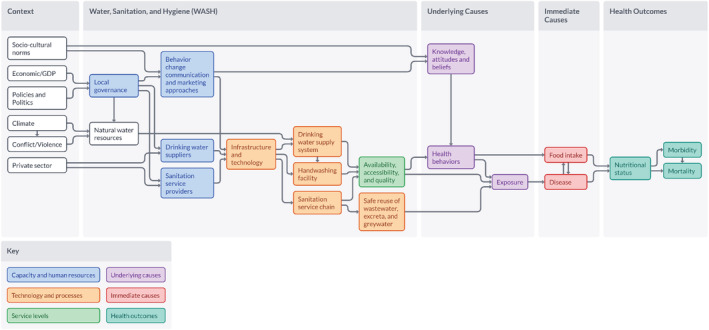
Water, sanitation and hygiene (WASH) to nutrition conceptual framework
The justification for improving WASH for nutrition is based on the theory that WASH improves nutritional status through the direct prevention of infection and disease. WASH is thought to influence nutritional status via three main disease pathways: diarrhoea, environmental enteric dysfunction (EED) and helminth infections (Figure 2). Twenty‐five per cent of stunting in children at 24 months of age is attributable to having experienced ≥5 diarrhoeal episodes in their first 2 years of life, and persistent diarrhoea (lasting more than 14 days) is, among all other forms of diarrhoea, the greatest contributor of stunting (Checkley et al., 2008; Lima et al., 2000). The pathogens most responsible for diarrhoeal episodes in children in LMICs include Shigella, rotavirus, adenovirus 40/41, Escherichia coli, Cryptosporidium and Campylobacter and are transmitted through the faecal‐oral route or through infected water (Liu et al., 2016). When pathogenic bacteria are present in the environment due to contaminated water, lack of sanitation and/or insufficient hygiene, this facilitates a high or ubiquitous exposure in young children and consequently, frequent infections and coinfections. Intermittent diarrhoeal episodes in children are associated with poor growth, predominantly through chronic inflammation and reduced insulin‐like growth factor 1 (IGF‐1) (Jones et al., 2015).
FIGURE 2.
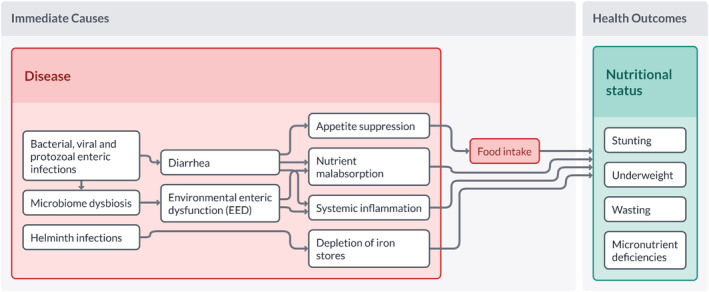
Water, sanitation and hygiene (WASH)‐related disease and nutritional status
Even in the absence of diarrhoea, an environment with high microbial exposure may cause a far more omnipresent subclinical disorder, referred to as EED (Humphrey, 2009). EED is characterized by intestinal inflammation, villous atrophy, malabsorption and gut permeability (Prendergast & Kelly, 2016). EED is thought to impair growth in children through chronic immune activation that diverts nutrients away from growth and through the overproduction of proinflammatory cytokines that decrease IGF‐1 and inhibit the process of bone remodelling necessary for long bone growth (Mbuya & Humphrey, 2016). While EED biomarkers are difficult to measure, asymptomatic enteric infections are believed to be the predominant way enteric infections cause growth failure and poor cognitive development (Harper et al., 2018). Subclinical and non‐diarrhoeal infections that have been associated with significant decreases in growth in children under two years include Shigella, enteroaggregative E. coli, Campylobacter and Giardia (Rogawski et al., 2018).
Soil‐transmitted helminth infections (STHs), such as hookworm or schistosomiasis, increase the burden of anaemia and stunting and are associated with poor WASH environments (Echazú et al., 2015; Kassebaum, 2016). A 2014 meta‐analysis found a 33% reduction in odds of STH infection with any WASH practice or access, suggesting that WASH plays an important role in reducing helminth infections and subsequent nutritional deficiencies (Strunz et al., 2014).
These three disease pathways result from transmission of pathogens from the environment to the human host, most often by oral ingestion, but also through skin in the case of STHs. When food, fingers, flies, water, soil and surfaces are contaminated due to presence of pathogens in the environment, this facilitates frequent transmission and subsequent infection (Figure 3) (Wagner & Lanoix, 1958). Assessment of the ‘local exposure landscape’, that is, how the pathogens enter the environment, is crucial in determining what WASH inputs will best address the enteric disease burden in a given setting. While open defecation is a significant contributor to faecal contamination in the environment, other factors, such as animal faeces or faeces‐derived fertilizer run‐off from fields could also contribute to pathogen load in drinking water and home environments (Kumwenda et al., 2017; Ngure et al., 2013). Where this might be the case, 100% coverage of latrines would not prevent all exposures and disease burden could remain substantial. Acknowledging all the potential sources of pathogens in context will help determine what type and combination of WASH efforts are needed. WASH interventions can only be expected to influence nutritional outcomes if they either (1) significantly reduce the level of pathogens in the environment or (2) break the transmission from the environment to the host.
FIGURE 3.
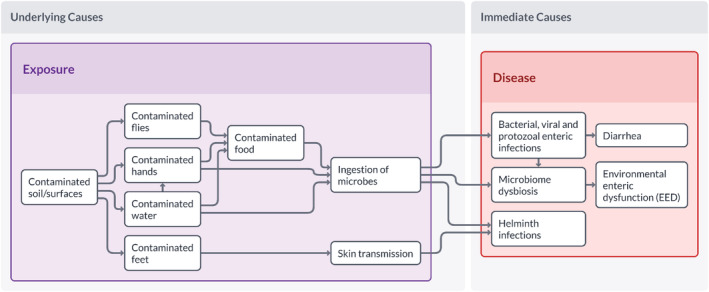
Modes of transmission of pathogens from the environment to the host and disease consequences
The hygiene element of WASH encompasses the health behaviors performed by individuals with the aim of breaking transmission. For example, handwashing at key times does not influence the level of pathogens in the environment, but it is an effective behavior in reducing the risk of transmission when performed regularly and with the essentials of water and soap or disinfectant (Ejemot‐Nwadiaro et al., 2015; Luby et al., 2010). These hygiene behaviors are influenced by individual and societal knowledge, attitudes and beliefs regarding hygiene, as well as the availability, accessibility and quality of the WASH services (Curtis et al., 2011; Hirai et al., 2016; Nizame et al., 2013; Schmidt et al., 2009). Other health behaviors, such as latrine use and removal of animal faeces from living spaces, aim to reduce the level of pathogens in the environment by removing the source of those pathogens. While seemingly more upstream, these behaviors also require knowledge, attitudes and beliefs and access to sanitation services (Jenkins & Scott, 2007; Water and Sanitation Program & United Nations Children's Fund (UNICEF), 2015). Herein lie the two predominant strategies of WASH interventions in nutrition programming: behavior change communication and marketing (BCCM) and the provision of WASH hardware.
BCCM strategies for WASH behavior uptake are essential, as the provision of hardware does not ensure uptake, or the appropriate and sustained use of the hardware (Garn et al., 2017). Point of use (POU) water treatment technology, which places a high demand on users, fails to have health benefits unless strictly adhered to. This has not been achieved without daily to biweekly personal contact with a behavior change promoter (Pickering, Null, et al., 2019). Various strategies exist for BCCM, and the combination of multiple strategies may be adopted to best address the barriers within context (Figure S2) (Dreibelbis et al., 2013). Conversely, behavior change in the absence of hardware is not successful as people are unlikely to use a latrine if they do not have a safe one or to wash their hands when they lack sufficient water (Oswald et al., 2008; Pickering & Davis, 2012).
The WASH benefits and SHINE trials conducted in Bangladesh, Kenya and Zimbabwe were designed to test this combination of BCCM and hardware through the provision of latrines and sani‐scoops, conveniently located handwashing stations with soap or soapy water, chlorine tablets or dispensers for water treatment and frequent contact with BCC promoters (Arnold et al., 2013; Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Team et al., 2015). In all three trials, the WASH interventions had no impact on linear growth, and only the Bangladesh trial found beneficial effects on diarrhoea (Humphrey et al., 2019; Luby et al., 2018; Null et al., 2018). The authors concluded that these findings do not disprove the theory of improved WASH impacting nutrition but rather that the specific WASH interventions implemented in these trails did not reduce the level of faecal contamination in the environment substantially enough to reduce infection and influence child growth (Cumming et al., 2019; Pickering, Swarthout, et al., 2019).
In high‐income and increasingly in middle‐income countries, WASH infrastructure encompasses more than tippy taps, POU water treatment and latrines and instead is characterized by piped drinking water and comprehensive sewage systems. Historically, improvements in water and sanitation supply systems in the late 1800s and early 1900s have been associated with significant reductions in child mortality (Alsan & Goldin, 2019; Cutler & Miller, 2005; Kesztenbaum & Rosenthal, 2014). More recently, municipal water chlorination in Mexico led to steady improvements in child diarrhoeal mortality but had the greatest effect in cities where the piping infrastructure was well maintained and sanitation services were available (Bhalotra et al., 2017). In rural India, the provision of piped drinking water and pit latrines installed in every household resulted in significant reductions in diarrhoeal disease in the participating villages (Duflo et al., 2015). In Brazil, access to sanitation services was a significant contributor to the reduction in child stunting (Monteiro et al., 2009). This evidence supports the need to expand WASH infrastructure in LMICs to more developed and effective systems as seen in high‐income settings for the improvement of child health and nutrition.
WHO technical documents provide detailed guidance on the implementation of safe sanitation service chains and clean drinking water supply systems. Figure 4 outlines the steps in each system, which encompasses the technologies, infrastructure and the processes required at every level. To ensure human excreta is safely disposed of in the sanitation service chain, the steps required are toilet/latrine, containment, conveyance, treatment and end use (World Health Organization, 2018). In the drinking water supply system, the factors include a safe water source, catchment, treatment and distribution (World Health Organization, 2017). The technologies within each of these steps vary according to the local landscape, population needs and available resources. For example, in a highly industrialized or urban area equipped with sewage systems, the user interface may look like a pedestal toilet with a water flush and nearby handwashing station with piped water. In these settings, the sanitation occurs ‘off‐site’ as the sewerage systems immediately transport human excreta away from the user interface and towards a wastewater treatment plant, reducing the risk of exposure to pathogens at the user level. In a rural or urban space without sewerage, the user interface may be a pit latrine with a slab, where human excreta is stored in an open bottom tank underground. Such catchment systems are not fully enclosed and can lead to leachate entering nearby groundwater or overflowing at the surface level if not regularly maintained and emptied. Other sanitation technologies include septic tanks, which help channel human excreta away from the user interface and more securely contain the sludge in an enclosed tank, but regular maintenance and emptying are required to ensure leakages do not occur. These ‘on‐site’ sanitation systems increase the risk of exposure to pathogens through overflowing tanks, spillage of faecal sludge at the time of emptying and, in some settings, dumping of sludge directly into water bodies when treatment plants are not available. While large infrastructure projects such as sewerage and piped drinking water may be considered too expensive or unfeasible in remote areas, the trade‐off is having technologies and processes that carry more risk of pathogenic exposure along the supply chain and require regular maintenance. Different technologies also require different health behaviors for proper use and safety. For example, piped drinking water on plot facilitates handwashing practices, the cleaning of sanitation facilities, and the washing of fruits and vegetables, as the water is in proximity, requires only the manual turning of a tap, and often provides a greater quantity of water than alternatives. Other technologies, such as boreholes or wells, may require fetching if not on plot, and POU treatment, such as chlorination tablets. These technologies require more manual labour to get the water on plot, may limit the amount of water that can be available at one time and require additional inputs for treatment, all of which increase user burden and subsequently reduce compliance to hygiene and health behaviors. While it is possible to develop safe drinking water and sanitation systems with different technologies that meet local needs and resource levels, it is important to acknowledge that certain technologies favour the uptake of health behaviors more than others.
FIGURE 4.
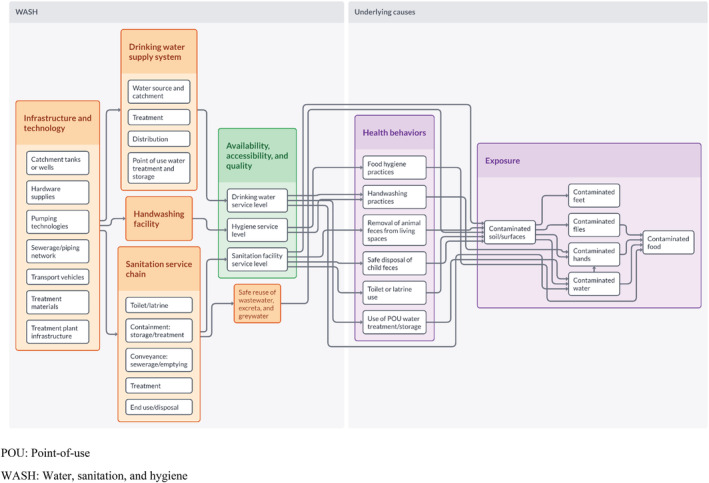
Linkages between water, sanitation and hygiene (WASH) infrastructure and service levels to health behaviours and exposure to pathogens
As highlighted previously, the availability, accessibility, and quality of the technologies along the supply chain are important factors in ensuring safe and convenient systems for the users as well as the water and sanitation workers. The JMP service ladder indicators provide a way to measure the availability, accessibility and quality of these services within household level surveys (World Health Organization & United Nations Children's Fund, 2018). The service levels have been included as a part of the framework to stress the importance of accessibility and quality when evaluating water and sanitation services and to highlight these indicators for measuring WASH within nutrition‐related programmatic efforts. Other household indicators, such as the household water insecurity experiences (HWISE) scale, may provide additional insights into water availability, accessibility, use and stability and how water insecurity affects child nutrition and health (Young et al., 2019, 2021).
Whether the systems are largely informal, such as independent water vendors, or formal, such as municipal treatment and distribution, water and sanitation systems require capacity and human resources (Figure 5). Sanitation and water supply services are delivered by service providers, which may be government workers or private entities. The local government sets standards based on health targets, finances large infrastructure developments, such as treatment plants or piping networks, and monitors and evaluates WASH service levels. In addition, the local government is responsible for implementing BCCM programs, in coordination with the health and education sectors locally (World Health Organization, 2017, 2018).
FIGURE 5.
Influence of context and role of capacity and human resources in water, sanitation and hygiene (WASH) systems
Contextual factors such as sociocultural norms, economic conditions, national level policies and politics, the role of the private sector, climate conditions and conflict impact WASH resources at various levels. For example, climate change is causing a stress on the natural resources for drinking water, which directly impacts supply and may fuel conflict, further exacerbating water scarcity and the public health consequences (Allouche, 2011; DeNicola et al., 2015). Separately, understanding sociocultural norms and incorporating them into BCCM interventions has been found to be integral to their success, as different cultural drivers may more readily influence behaviour uptake (Biran et al., 2014; De Buck et al., 2017). More research on the effects of contextual factors on WASH implementation, coverage and effectiveness is warranted.
4. DISCUSSION
We propose this new conceptual framework to provide policy makers, implementors and researchers alike as a resource to visualize the complex WASH–nutrition relationship and how the current evidence may inform future WASH programming. In constructing this framework, some important findings came through in the literature:
First, there are various biological pathways by which exposure to pathogens may result in poor nutritional status of children and women in LMICs. EED and microbiome dysbiosis are likely to be important contributors to poor growth, although the exact mechanisms remain unclear and better diagnostics are required to measure EED and its pathogen‐specific causes (Harper et al., 2018).
Second, water and sanitation coverage continue to be strong predictors of nutritional status, especially among children but improving household level access to latrines, tippy taps and water treatment hardware has not been found to have any impact on child nutritional status in highly controlled randomized trials. The WASH interventions implemented in these trials did not achieve a significant enough reduction in exposure to pathogens to have a meaningful impact on nutritional status, indicating a need for more effective interventions.
Third, in response to these findings, researchers have called for new and innovative interventions to address these challenges, or ‘transformative WASH’ (Pickering, Null, et al., 2019). Further, all interventions should be assessed for effectiveness based on the intervention's ability to reduce the pathogenic load in the target population. JMP indicators may be helpful in determining whether WASH services are available, of good quality, and accessible, but ultimately WASH interventions need to be assessed by their ability to reduce enteropathogenic load in the human population. Implementing this kind of surveillance will allow health officials and researchers to know whether the WASH interventions are likely to reduce infection and improve nutrition and health.
Fourth, a return to the historical and observational literature provides consistent evidence that comprehensive piped drinking water and sewage systems are established and effective solutions for improving health in populations, including nutrition. Policy makers and programme implementors in the nutrition field must extend beyond WASH as a component of a household nutrition intervention ‘package’ and, instead, work collaboratively with water and sanitation leaders to improve WASH at higher levels, as indicated by the framework. With improvements in technology and infrastructure and greater capacity of governing bodies to make meaningful changes in the drinking water supply and sanitation systems, less burden will fall on poor communities to ensure they have safe WASH, and hygiene behaviors may become more accessible. Researchers have suggested the incremental changes in the water and sanitation systems in LMICs are the most promising strategies for reducing disease and improving nutrition, as demonstrated by countries such as Brazil (Monteiro et al., 2009). More evidence on the cost‐effectiveness of large WASH infrastructure projects on population health and nutrition are required.
The conceptual framework described above has several limitations. First, the exact biological pathways linking poor water and sanitation to nutritional status are not fully understood. Second, it is difficult to capture all the potential sources of pathogen exposure, and important sources in a given context may be missing. Third, the various WASH technologies that currently exist and are continuously evolving are not fully encapsulated in this framework. Finally, the graded nature of governance and regional organization is not captured in this visualization, but WASH efforts at every level of organization are necessary, much like the health system.
Despite these limitations, this framework has several advantages. It provides an encompassing view of all the pathways by which water and sanitation affect nutrition, highlighting the need to incorporate multilevel WASH measures in multisectoral nutrition planning and programming. Much like how the health and education sectors have important linkages to nutrition, improvements in WASH could accelerate nutrition gains in LMICs, while reducing disease more broadly (King et al., 2021; Xu et al., 2021). This framework brings together the various roles of policy makers, program implementors, engineers and researchers engaged in WASH and highlights gaps that need to be addressed to have a measurable effect on nutrition. The nutrition community may use this framework to advocate for WASH policies, programmes and research that strives to meet SDG6: clean water and sanitation for all (United Nations, 2015). Finally, the framework has the potential to be adapted as new developments arise and provide guidance as to how interventions may be designed and incorporated into existing systems to impact nutritional status.
5. CONCLUSION
Using this framework as a guide, more comprehensive WASH strategies may be incorporated into multisectoral nutrition policies and programming. However, to have a significant impact on nutritional status, the global agenda must primarily focus on interrupting the transmission of pathogens to the human host. This will require greater investments in large‐scale water supply and sanitation systems where possible; increased coordination between the bodies responsible for providing WASH services and ensuring their safety, including increasing capacity; and funding of research for effective, lower cost interventions that have a meaningful impact on pathogenic load and ultimately, nutritional status and health.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.
CONTRIBUTIONS
EZ conducted the literature review and drafted the first version of the manuscript. SEK, TSL and TR guided the methodology and helped outline the manuscript. All contributed to multiple revisions of the manuscript and read and approved the final version.
Supporting information
Figure S1 Detailed WASH to nutrition conceptual framework
Figure S2 WASH BCCM for health behaviour change and reduction of pathogenic exposure.
ACKNOWLEDGMENTS
We gratefully acknowledge Dr. Jean Humphrey, Dr. Robert Dreibelbis and Yvonne Yiru Xu for their critical feedback and suggestions on the early versions of the conceptual framework. Global Affairs Canada, under the project ‘Real Accountability: Data Analysis for Results’ Johns Hopkins University grant 90067950.
In this appendix, we provide details on our search strategy indicating our specific search terms (Table A1) and from what sources evidence was drawn from to inform the different levels of the conceptual framework (Table A2).
TABLE A1.
Search terms and strategy
| A. WASH specific terms |
| (‘water’[Title/Abstract] OR ‘hygiene’[Title/Abstract] OR ‘sanitation’[Title/Abstract] OR ‘enteric’[Title/Abstract] OR ‘latrine’[Title/Abstract] OR ‘waste’[Title/Abstract] OR ‘handwashing’[Title/Abstract] OR ‘diarrhea’[Title/Abstract] OR ‘acute disease’[Title/Abstract] OR ‘drinking water’[Title/Abstract] OR ‘defecation’[Title/Abstract] OR ‘toilet’[Title/Abstract] OR ‘pit latrine’[Title/Abstract] OR ‘Soap’[Title/Abstract] OR ‘detergent’[Title/Abstract] OR ‘well’[Title/Abstract] OR ‘pumps’[Title/Abstract] OR ‘taps’[Title/Abstract] OR ‘borehole’[Title/Abstract] OR ‘potable’[Title/Abstract] OR ‘contaminant’[Title/Abstract] OR ‘contaminants’[Title/Abstract] OR ‘toilets’[Title/Abstract] OR ‘latrines’[Title/Abstract] OR ‘acute diseases’[Title/Abstract] OR ‘EED’[Title/Abstract] OR ‘pathogens’[Title/Abstract] OR ‘WASH’[Title/Abstract] OR ‘treatment’[Title/Abstract] OR ‘chlorine’[Title/Abstract] OR ‘water‐borne’[Title/Abstract] OR ‘waterborne’[Title/Abstract] OR ‘bacteria’[Title/Abstract] OR ‘bacterium’[Title/Abstract] OR ‘communicable’[Title/Abstract] OR ‘infection’[Title/Abstract] OR ‘pathogen’[Title/Abstract] OR ‘E.Coli’[Title/Abstract] OR ‘cholera’[Title/Abstract] OR ‘disinfectant’[Title/Abstract] OR ‘chlorination’[Title/Abstract] OR ‘infections’[Title/Abstract] OR ‘infect’[Title/Abstract] OR ‘Soap’[Title/Abstract]) AND (1950:2019[pdat]) (8,488,291) |
| B. Nutrition specific terms |
| (‘nutritional’[Title/Abstract] OR ‘nutrition’[Title/Abstract] OR ‘dietary’[Title/Abstract] OR ‘diet’[Title/Abstract] OR ‘food’[Title/Abstract] OR ‘fortified’[Title/Abstract] OR ‘nutrients’[Title/Abstract] OR ‘fortification’[Title/Abstract] OR ‘feeding’[Title/Abstract] OR ‘breastfeeding’[Title/Abstract] OR ‘hunger’[Title/Abstract] OR ‘complementary’[Title/Abstract] OR ‘nutritive’[Title/Abstract] OR ‘supplements’[Title/Abstract] OR ‘nutritive value’[Title/Abstract] OR ‘eating’[Title/Abstract] OR ‘micronutrients’[Title/Abstract] OR ‘malnutrition’[Title/Abstract] OR ‘undernourish’[Title/Abstract] OR ‘undernutrition’[Title/Abstract] OR ‘overnutrition’[Title/Abstract] OR ‘nutrient’[Title/Abstract] OR ‘nourish’[Title/Abstract] OR ‘nutrients’[Title/Abstract] OR ‘nutriture’[Title/Abstract] OR ‘nourishment’[Title/Abstract] OR ‘stunting’[Title/Abstract] OR ‘wasting’[Title/Abstract] OR ‘underweight’[Title/Abstract] OR ‘overweight’[Title/Abstract]) AND (1950:2019/10/15[pdat]) (1,423,116) |
| C. LMIC terms |
| (‘developing country’[tiab] OR ‘developing countries’[tiab] OR ‘developing nation’[tiab] OR ‘developing nations’[tiab] OR ‘developing population’[tiab] OR ‘developing populations’[tiab] OR ‘developing world’[tiab] OR ‘less developed country’[tiab] OR ‘less developed countries’[tiab] OR ‘less developed nation’[tiab] OR ‘less developed nations’[tiab] OR ‘less developed population’[tiab] OR ‘less developed populations’[tiab] OR ‘less developed world’[tiab] OR ‘lesser developed country’[tiab] OR ‘lesser developed countries’[tiab] OR ‘lesser developed nation’[tiab] OR ‘lesser developed nations’[tiab] OR ‘lesser developed population’[tiab] OR ‘lesser developed populations’[tiab] OR ‘lesser developed world’[tiab] OR ‘under developed country’[tiab] OR ‘under developed countries’[tiab] OR ‘under developed nation’[tiab] OR ‘under developed nations’[tiab] OR ‘under developed population’[tiab] OR ‘under developed populations’[tiab] OR ‘under developed world’[tiab] OR ‘underdeveloped country’[tiab] OR ‘underdeveloped countries’[tiab] OR ‘underdeveloped nation’[tiab] OR ‘underdeveloped nations’[tiab] OR ‘underdeveloped population’[tiab] OR ‘underdeveloped populations’[tiab] OR ‘underdeveloped world’[tiab] OR ‘middle income country’[tiab] OR ‘middle income countries’[tiab] OR ‘middle income nation’[tiab] OR ‘middle income nations’[tiab] OR ‘middle income population’[tiab] OR ‘middle income populations’[tiab] OR ‘low income country’[tiab] OR ‘low income countries’[tiab] OR ‘low income nation’[tiab] OR ‘low income nations’[tiab] OR ‘low income population’[tiab] OR ‘low income populations’[tiab] OR ‘lower income country’[tiab] OR ‘lower income countries’[tiab] OR ‘lower income nation’[tiab] OR ‘lower income nations’[tiab] OR ‘lower income population’[tiab] OR ‘lower income populations’[tiab] OR ‘underserved country’[tiab] OR ‘underserved countries’[tiab] OR ‘underserved nation’[tiab] OR ‘underserved nations’[tiab] OR ‘underserved population’[tiab] OR ‘underserved populations’[tiab] OR ‘underserved world’[tiab] OR ‘under served country’[tiab] OR ‘under served countries’[tiab] OR ‘under served nation’[tiab] OR ‘under served nations’[tiab] OR ‘under served population’[tiab] OR ‘under served populations’[tiab] OR ‘under served world’[tiab] OR ‘deprived country’[tiab] OR ‘deprived countries’[tiab] OR ‘deprived nation’[tiab] OR ‘deprived nations’[tiab] OR ‘deprived population’[tiab] OR ‘deprived populations’[tiab] OR ‘deprived world’[tiab] OR ‘poor country’[tiab] OR ‘poor countries’[tiab] OR ‘poor nation’[tiab] OR ‘poOR nations’[tiab] OR ‘poor population’[tiab] OR ‘poor populations’[tiab] OR ‘poor world’[tiab] OR ‘poorer country’[tiab] OR ‘poorer countries’[tiab] OR ‘poorer nation’[tiab] OR ‘poorer nations’[tiab] OR ‘poorer population’[tiab] OR ‘poorer populations’[tiab] OR ‘poorer world’[tiab] OR ‘developing economy’[tiab] OR ‘developing economies’[tiab] OR ‘less developed economy’[tiab] OR ‘less developed economies’[tiab] OR ‘lesser developed economy’[tiab] OR ‘lesser developed economies’[tiab] OR ‘under developed economy’[tiab] OR ‘under developed economies’[tiab] OR ‘underdeveloped economy’[tiab] OR ‘underdeveloped economies’[tiab] OR ‘middle income economy’[tiab] OR ‘middle income economies’[tiab] OR ‘low income economy’[tiab] OR ‘low income economies’[tiab] OR ‘lower income economy’[tiab] OR ‘lower income economies’[tiab] OR ‘low gdp’[tiab] OR ‘low gnp’[tiab] OR ‘low gross domestic’[tiab] OR ‘low gross national’[tiab] OR ‘lower gdp’[tiab] OR ‘lower gnp’[tiab] OR ‘lower gross domestic’[tiab] OR ‘lower gross national’[tiab] OR ‘lmic’[tiab] OR ‘lmics’[tiab] OR ‘third world’[tiab] OR ‘lami country’[tiab] OR ‘lami countries’[tiab] OR ‘transitional country’[tiab] OR ‘transitional countries’[tiab] OR ‘developing country’[ot] OR ‘developing countries’[ot] OR ‘developing nation’[ot] OR ‘developing nations’[ot] OR ‘developing population’[ot] OR ‘developing populations’[ot] OR ‘developing world’[ot] OR ‘less developed country’[ot] OR ‘less developed countries’[ot] OR ‘less developed nation’[ot] OR ‘less developed nations’[ot] OR ‘less developed population’[ot] OR ‘less developed populations’[ot] OR ‘less developed world’[ot] OR ‘lesser developed country’[ot] OR ‘lesser developed countries’[ot] OR ‘lesser developed nation’[ot] OR ‘lesser developed nations’[ot] OR ‘lesser developed population’[ot] OR ‘lesser developed populations’[ot] OR ‘lesser developed world’[ot] OR ‘under developed country’[ot] OR ‘under developed countries’[ot] OR ‘under developed nation’[ot] OR ‘under developed nations’[ot] OR ‘under developed population’[ot] OR ‘under developed populations’[ot] OR ‘under developed world’[ot] OR ‘underdeveloped country’[ot] OR ‘underdeveloped countries’[ot] OR ‘underdeveloped nation’[ot] OR ‘underdeveloped nations’[ot] OR ‘underdeveloped population’[ot] OR ‘underdeveloped populations’[ot] OR ‘underdeveloped world’[ot] OR ‘middle income country’[ot] OR ‘middle income countries’[ot] OR ‘middle income nation’[ot] OR ‘middle income nations’[ot] OR ‘middle income population’[ot] OR ‘middle income populations’[ot] OR ‘low income country’[ot] OR ‘low income countries’[ot] OR ‘low income nation’[ot] OR ‘low income nations’[ot] OR ‘low income population’[ot] OR ‘low income populations’[ot] OR ‘lower income country’[ot] OR ‘lower income countries’[ot] OR ‘lower income nation’[ot] OR ‘lower income nations’[ot] OR ‘lower income population’[ot] OR ‘lower income populations’[ot] OR ‘underserved country’[ot] OR ‘underserved countries’[ot] OR ‘underserved nation’[ot] OR ‘underserved nations’[ot] OR ‘underserved population’[ot] OR ‘underserved populations’[ot] OR ‘underserved world’[ot] OR ‘under served country’[ot] OR ‘under served countries’[ot] OR ‘under served nation’[ot] OR ‘under served nations’[ot] OR ‘under served population’[ot] OR ‘under served populations’[ot] OR ‘under served world’[ot] OR ‘deprived country’[ot] OR ‘deprived countries’[ot] OR ‘deprived nation’[ot] OR ‘deprived nations’[ot] OR ‘deprived population’[ot] OR ‘deprived populations’[ot] OR ‘deprived world’[ot] OR ‘poor country’[ot] OR ‘poor countries’[ot] OR ‘poor nation’[ot] OR ‘poor nations’[ot] OR ‘poor population’[ot] OR ‘poor populations’[ot] OR ‘poor world’[ot] OR ‘poorer country’[ot] OR ‘poorer countries’[ot] OR ‘poorer nation’[ot] OR ‘poorer nations’[ot] OR ‘poorer population’[ot] OR ‘poorer populations’[ot] OR ‘poorer world’[ot] OR ‘developing economy’[ot] OR ‘developing economies’[ot] OR ‘less developed economy’[ot] OR ‘less developed economies’[ot] OR ‘lesser developed economy’[ot] OR ‘lesser developed economies’[ot] OR ‘under developed economy’[ot] OR ‘under developed economies’[ot] OR ‘underdeveloped economy’[ot] OR ‘underdeveloped economies’[ot] OR ‘middle income economy’[ot] OR ‘middle income economies’[ot] OR ‘low income economy’[ot] OR ‘low income economies’[ot] OR ‘lower income economy’[ot] OR ‘lower income economies’[ot] OR ‘low gdp’[ot] OR ‘low gnp’[ot] OR ‘low gross domestic’[ot] OR ‘low gross national’[ot] OR ‘lower gdp’[ot] OR ‘lower gnp’[ot] OR ‘lower gross domestic’[ot] OR ‘lower gross national’[ot] OR ‘lmic’[ot] OR ‘lmics’[ot] OR ‘third world’[ot] OR ‘lami country’[ot] OR ‘lami countries’[ot] OR ‘transitional country’[ot] OR ‘transitional countries’[ot] OR ‘Africa’[tiab] OR ‘Asia’[tiab] OR ‘Caribbean’[tiab] OR ‘West Indies’[tiab] OR ‘South America’[tiab] OR ‘Latin America’[tiab] OR ‘Central America’[tiab] OR ‘Afghanistan’[tiab] OR ‘Albania’[tiab] OR ‘Algeria’[tiab] OR ‘Angola’[tiab] OR ‘Antigua’[tiab] OR ‘Barbuda’[tiab] OR ‘Argentina’[tiab] OR ‘Armenia’[tiab] OR ‘Armenian’[tiab] OR ‘Aruba’[tiab] OR ‘Azerbaijan’[tiab] OR ‘Bahrain’[tiab] OR ‘Bangladesh’[tiab] OR ‘Barbados’[tiab] OR ‘Benin’[tiab] OR ‘Byelarus’[tiab] OR ‘Byelorussian’[tiab] OR ‘Belarus’[tiab] OR ‘Belorussian’[tiab] OR ‘Belorussia’[tiab] OR ‘Belize’[tiab] OR ‘Bhutan’[tiab] OR ‘Bolivia’[tiab] OR ‘Bosnia’[tiab] OR ‘Herzegovina’[tiab] OR ‘Hercegovina’[tiab] OR ‘Botswana’[tiab] OR ‘Brasil’[tiab] OR ‘Brazil’[tiab] OR ‘Bulgaria’[tiab] OR ‘Burkina Faso’[tiab] OR ‘Burkina Fasso’[tiab] OR ‘Upper Volta’[tiab] OR ‘Burundi’[tiab] OR ‘Urundi’[tiab] OR ‘Cambodia’[tiab] OR ‘Khmer Republic’[tiab] OR ‘Kampuchea’[tiab] OR ‘Cameroon’[tiab] OR ‘Cameroons’[tiab] OR ‘Cameron’[tiab] OR ‘Cape Verde’[tiab] OR ‘Central African Republic’[tiab] OR ‘Chad’[tiab] OR ‘Chile’[tiab] OR ‘China’[tiab] OR ‘Colombia’[tiab] OR ‘Comoros’[tiab] OR ‘Comoro Islands’[tiab] OR ‘Comores’[tiab] OR ‘Mayotte’[tiab] OR ‘Congo’[tiab] OR ‘Zaire’[tiab] OR ‘Costa Rica’[tiab] OR ‘Cote dIvoire’[tiab] OR ‘Ivory Coast’[tiab] OR ‘Croatia’[tiab] OR ‘Cuba’[tiab] OR ‘Cyprus’[tiab] OR ‘Czechoslovakia’[tiab] OR ‘Czech Republic’[tiab] OR ‘Slovakia’[tiab] OR ‘Slovak Republic’[tiab] OR ‘Djibouti’[tiab] OR ‘French Somaliland’[tiab] OR ‘Dominica’[tiab] OR ‘Dominican Republic’[tiab] OR ‘East Timor’[tiab] OR ‘East Timur’[tiab] OR ‘TimOR Leste’[tiab] OR ‘Ecuador’[tiab] OR ‘Egypt’[tiab] OR ‘United Arab Republic’[tiab] OR ‘El Salvador’[tiab] OR ‘Eritrea’[tiab] OR ‘Estonia’[tiab] OR ‘Ethiopia’[tiab] OR ‘Fiji’[tiab] OR ‘Gabon’[tiab] OR ‘Gabonese Republic’[tiab] OR ‘Gambia’[tiab] OR ‘Gaza’[tiab] OR ‘Georgia Republic’[tiab] OR ‘Georgian Republic’[tiab] OR ‘Ghana’[tiab] OR ‘Gold Coast’[tiab] OR ‘Greece’[tiab] OR ‘Grenada’[tiab] OR ‘Guatemala’[tiab] OR ‘Guinea’[tiab] OR ‘Guam’[tiab] OR ‘Guiana’[tiab] OR ‘Guyana’[tiab] OR ‘Haiti’[tiab] OR ‘Honduras’[tiab] OR ‘Hungary’[tiab] OR ‘India’[tiab] OR ‘Maldives’[tiab] OR ‘Indonesia’[tiab] OR ‘Iran’[tiab] OR ‘Iraq’[tiab] OR ‘Isle of Man’[tiab] OR ‘Jamaica’[tiab] OR ‘Jordan’[tiab] OR ‘Kazakhstan’[tiab] OR ‘Kazakh’[tiab] OR ‘Kenya’[tiab] OR ‘Kiribati’[tiab] OR ‘Korea’[tiab] OR ‘Kosovo’[tiab] OR ‘Kyrgyzstan’[tiab] OR ‘Kirghizia’[tiab] OR ‘Kyrgyz Republic’[tiab] OR ‘Kirghiz’[tiab] OR ‘Kirgizstan’[tiab] OR ‘Lao PDR’[tiab] OR ‘Laos’[tiab] OR ‘Latvia’[tiab] OR ‘Lebanon’[tiab] OR ‘Lesotho’[tiab] OR ‘Basutoland’[tiab] OR ‘Liberia’[tiab] OR ‘Libya’[tiab] OR ‘Lithuania’[tiab] OR ‘Macedonia’[tiab] OR ‘Madagascar’[tiab] OR ‘Malagasy Republic’[tiab] OR ‘Malaysia’[tiab] OR ‘Malaya’[tiab] OR ‘Malay’[tiab] OR ‘Sabah’[tiab] OR ‘Sarawak’[tiab] OR ‘Malawi’[tiab] OR ‘Nyasaland’[tiab] OR ‘Mali’[tiab] OR ‘Malta’[tiab] OR ‘Marshall Islands’[tiab] OR ‘Mauritania’[tiab] OR ‘Mauritius’[tiab] OR ‘Agalega Islands’[tiab] OR ‘Mexico’[tiab] OR ‘Micronesia’[tiab] OR ‘Middle East’[tiab] OR ‘Moldova’[tiab] OR ‘Moldovia’[tiab] OR ‘Moldovian’[tiab] OR ‘Mongolia’[tiab] OR ‘Montenegro’[tiab] OR ‘Morocco’[tiab] OR ‘Ifni’[tiab] OR ‘Mozambique’[tiab] OR ‘Myanmar’[tiab] OR ‘Myanma’[tiab] OR ‘Burma’[tiab] OR ‘Namibia’[tiab] OR ‘Nepal’[tiab] OR ‘Netherlands Antilles’[tiab] OR ‘New Caledonia’[tiab] OR ‘Nicaragua’[tiab] OR ‘Niger’[tiab] OR ‘Nigeria’[tiab] OR ‘Northern Mariana Islands’[tiab] OR ‘Oman’[tiab] OR ‘Muscat’[tiab] OR ‘Pakistan’[tiab] OR ‘Palau’[tiab] OR ‘Palestine’[tiab] OR ‘Panama’[tiab] OR ‘Paraguay’[tiab] OR ‘Peru’[tiab] OR ‘Philippines’[tiab] OR ‘Philipines’[tiab] OR ‘Phillipines’[tiab] OR ‘Phillippines’[tiab] OR ‘Poland’[tiab] OR ‘Portugal’[tiab] OR ‘Puerto Rico’[tiab] OR ‘Romania’[tiab] OR ‘Rumania’[tiab] OR ‘Roumania’[tiab] OR ‘Russia’[tiab] OR ‘Russian’[tiab] OR ‘Rwanda’[tiab] OR ‘Ruanda’[tiab] OR ‘Saint Kitts’[tiab] OR ‘St Kitts’[tiab] OR ‘Nevis’[tiab] OR ‘Saint Lucia’[tiab] OR ‘St Lucia’[tiab] OR ‘Saint Vincent’[tiab] OR ‘St Vincent’[tiab] OR ‘Grenadines’[tiab] OR ‘Samoa’[tiab] OR ‘Samoan Islands’[tiab] OR ‘NavigatOR Island’[tiab] OR ‘NavigatOR Islands’[tiab] OR ‘Sao Tome’[tiab] OR ‘Saudi Arabia’[tiab] OR ‘Senegal’[tiab] OR ‘Serbia’[tiab] OR ‘Montenegro’[tiab] OR ‘Seychelles’[tiab] OR ‘Sierra Leone’[tiab] OR ‘Slovenia’[tiab] OR ‘Sri Lanka’[tiab] OR ‘Ceylon’[tiab] OR ‘Solomon Islands’[tiab] OR ‘Somalia’[tiab] OR ‘Sudan’[tiab] OR ‘Suriname’[tiab] OR ‘Surinam’[tiab] OR ‘Swaziland’[tiab] OR ‘Syria’[tiab] OR ‘Tajikistan’[tiab] OR ‘Tadzhikistan’[tiab] OR ‘Tadjikistan’[tiab] OR ‘Tadzhik’[tiab] OR ‘Tanzania’[tiab] OR ‘Thailand’[tiab] OR ‘Togo’[tiab] OR ‘Togolese Republic’[tiab] OR ‘Tonga’[tiab] OR ‘Trinidad’[tiab] OR ‘Tobago’[tiab] OR ‘Tunisia’[tiab] OR ‘Turkey’[tiab] OR ‘Turkmenistan’[tiab] OR ‘Turkmen’[tiab] OR ‘Uganda’[tiab] OR ‘Ukraine’[tiab] OR ‘Uruguay’[tiab] OR ‘USSR’[tiab] OR ‘Soviet Union’[tiab] OR ‘Union of Soviet Socialist Republics’[tiab] OR ‘Uzbekistan’[tiab] OR ‘Uzbek’ OR ‘Vanuatu’[tiab] OR ‘New Hebrides’[tiab] OR ‘Venezuela’[tiab] OR ‘Vietnam’[tiab] OR ‘Viet Nam’[tiab] OR ‘West Bank’[tiab] OR ‘Yemen’[tiab] OR ‘Yugoslavia’[tiab] OR ‘Zambia’[tiab] OR ‘Zimbabwe’[tiab] OR ‘Rhodesia’[tiab] OR ‘Africa’[ot] OR ‘Asia’[ot] OR ‘Caribbean’[ot] OR ‘West Indies’[ot] OR ‘South America’[ot] OR ‘Latin America’[ot] OR ‘Central America’[ot] OR ‘Afghanistan’[ot] OR ‘Albania’[ot] OR ‘Algeria’[ot] OR ‘Angola’[ot] OR ‘Antigua’[ot] OR ‘Barbuda’[ot] OR ‘Argentina’[ot] OR ‘Armenia’[ot] OR ‘Armenian’[ot] OR ‘Aruba’[ot] OR ‘Azerbaijan’[ot] OR ‘Bahrain’[ot] OR ‘Bangladesh’[ot] OR ‘Barbados’[ot] OR ‘Benin’[ot] OR ‘Belarus’[ot] OR ‘Belize’[ot] OR ‘Bhutan’[ot] OR ‘Bolivia’[ot] OR ‘Bosnia’[ot] OR ‘Herzegovina’[ot] OR ‘Botswana’[ot] OR ‘Brasil’[ot] OR ‘Brazil’[ot] OR ‘Bulgaria’[ot] OR ‘Burkina Faso’[ot] OR ‘Upper Volta’[ot] OR ‘Burundi’[ot] OR ‘Cambodia’[ot] OR ‘Khmer Republic’[ot] OR ‘Kampuchea’[ot] OR ‘Cameroon’[ot] OR ‘Cape Verde’[ot] OR ‘Central African Republic’[ot] OR ‘Chad’[ot] OR ‘Chile’[ot] OR ‘China’[ot] OR ‘Colombia’[ot] OR ‘Comoros’[ot] OR ‘Comoro Islands’[ot] OR ‘Mayotte’[ot] OR ‘Congo’[ot] OR ‘Zaire’[ot] OR ‘Costa Rica’[ot] OR ‘Cote dIvoire’[ot] OR ‘Ivory Coast’[ot] OR ‘Croatia’[ot] OR ‘Cuba’[ot] OR ‘Cyprus’[ot] OR ‘Czechoslovakia’[ot] OR ‘Czech Republic’[ot] OR ‘Slovakia’[ot] OR ‘Slovak Republic’[ot] OR ‘Djibouti’[ot] OR ‘French Somaliland’[ot] OR ‘Dominica’[ot] OR ‘Dominican Republic’[ot] OR ‘East Timor’[ot] OR ‘East Timur’[ot] OR ‘Timor Leste’[ot] OR ‘Ecuador’[ot] OR ‘Egypt’[ot] OR ‘United Arab Republic’[ot] OR ‘El Salvador’[ot] OR ‘Eritrea’[ot] OR ‘Estonia’[ot] OR ‘Ethiopia’[ot] OR ‘Fiji’[ot] OR ‘Gabon’[ot] OR ‘Gabonese Republic’[ot] OR ‘Gambia’[ot] OR ‘Gaza’[ot] OR ‘Georgia Republic’[ot] OR ‘Georgian Republic’[ot] OR ‘Ghana’[ot] OR ‘Gold Coast’[ot] OR ‘Greece’[ot] OR ‘Grenada’[ot] OR ‘Guatemala’[ot] OR ‘Guinea’[ot] OR ‘Guam’[ot] OR ‘Guiana’[ot] OR ‘Guyana’[ot] OR ‘Haiti’[ot] OR ‘Honduras’[ot] OR ‘Hungary’[ot] OR ‘India’[ot] OR ‘Maldives’[ot] OR ‘Indonesia’[ot] OR ‘Iran’[ot] OR ‘Iraq’[ot] OR ‘Isle of Man’[ot] OR ‘Jamaica’[ot] OR ‘Jordan’[ot] OR ‘Kazakhstan’[ot] OR ‘Kazakh’[ot] OR ‘Kenya’[ot] OR ‘Kiribati’[ot] OR ‘Korea’[ot] OR ‘Kosovo’[ot] OR ‘Kyrgyzstan’[ot] OR ‘Kirghizia’[ot] OR ‘Kyrgyz Republic’[ot] OR ‘Lao PDR’[ot] OR ‘Laos’[ot] OR ‘Latvia’[ot] OR ‘Lebanon’[ot] OR ‘Lesotho’[ot] OR ‘Liberia’[ot] OR ‘Libya’[ot] OR ‘Lithuania’[ot] OR ‘Macedonia’[ot] OR ‘Madagascar’[ot] OR ‘Malagasy Republic’[ot] OR ‘Malaysia’[ot] OR ‘Malaya’[ot] OR ‘Malay’[ot] OR ‘Sabah’[ot] OR ‘Sarawak’[ot] OR ‘Malawi’[ot] OR ‘Nyasaland’[ot] OR ‘Mali’[ot] OR ‘Malta’[ot] OR ‘Marshall Islands’[ot] OR ‘Mauritania’[ot] OR ‘Mauritius’[ot] OR ‘Agalega Islands’[ot] OR ‘Mexico’[ot] OR ‘Micronesia’[ot] OR ‘Middle East’[ot] OR ‘Moldova’[ot] OR ‘Mongolia’[ot] OR ‘Montenegro’[ot] OR ‘Morocco’[ot] OR ‘Mozambique’[ot] OR ‘Myanmar’[ot] OR ‘Burma’[ot] OR ‘Namibia’[ot] OR ‘Nepal’[ot] OR ‘Netherlands Antilles’[ot] OR ‘New Caledonia’[ot] OR ‘Nicaragua’[ot] OR ‘Niger’[ot] OR ‘Nigeria’[ot] OR ‘Northern Mariana Islands’[ot] OR ‘Oman’[ot] OR ‘Muscat’[ot] OR ‘Pakistan’[ot] OR ‘Palau’[ot] OR ‘Palestine’[ot] OR ‘Panama’[ot] OR ‘Paraguay’[ot] OR ‘Peru’[ot] OR ‘Philippines’[ot] OR ‘Poland’[ot] OR ‘Portugal’[ot] OR ‘Puerto Rico’[ot] OR ‘Romania’[ot] OR ‘Rumania’[ot] OR ‘Roumania’[ot] OR ‘Russia’[ot] OR ‘Russian’[ot] OR ‘Rwanda’[ot] OR ‘Ruanda’[ot] OR ‘Saint Kitts’[ot] OR ‘St Kitts’[ot] OR ‘Nevis’[ot] OR ‘Saint Lucia’[ot] OR ‘St Lucia’[ot] OR ‘Saint Vincent’[ot] OR ‘St Vincent’[ot] OR ‘Grenadines’[ot] OR ‘Samoa’[ot] OR ‘Samoan Islands’[ot] OR ‘NavigatOR ‘Island’[ot] OR ‘NavigatOR Islands’[ot] OR ‘Sao Tome’[ot] OR ‘Saudi Arabia’[ot] OR ‘Senegal’[ot] OR ‘Serbia’[ot] OR ‘Montenegro’[ot] OR ‘Seychelles’[ot] OR ‘Sierra Leone’[ot] OR ‘Slovenia’[ot] OR ‘Sri Lanka’[ot] OR ‘Ceylon’[ot] OR ‘Solomon Islands’[ot] OR ‘Somalia’[ot] OR ‘Sudan’[ot] OR ‘Suriname’[ot] OR ‘Surinam’[ot] OR ‘Swaziland’[ot] OR ‘Syria’[ot] OR ‘Tajikistan’[ot] OR ‘Tadzhikistan’[ot] OR ‘Tanzania’[ot] OR ‘Thailand’[ot] OR ‘Togo’[ot] OR ‘Togolese Republic’[ot] OR ‘Tonga’[ot] OR ‘Trinidad’[ot] OR ‘Tobago’[ot] OR ‘Tunisia’[ot] OR ‘Turkey’[ot] OR ‘Turkmenistan’[ot] OR ‘Turkmen’[ot] OR ‘Uganda’[ot] OR ‘Ukraine’[ot] OR ‘Uruguay’[ot] OR ‘USSR’[ot] OR ‘Soviet Union’[ot] OR ‘Union of Soviet Socialist Republics’[ot] OR ‘Uzbekistan’[ot] OR ‘Uzbek’ OR ‘Vanuatu’[ot] OR ‘New Hebrides’[ot] OR ‘Venezuela’[ot] OR ‘Vietnam’[ot] OR ‘Viet Nam’[ot] OR ‘West Bank’[ot] OR ‘Yemen’[ot] OR ‘Yugoslavia’[ot] OR ‘Zambia’[ot] OR ‘Zimbabwe’[ot] OR ‘Rhodesia’[ot] OR ‘Developing Countries’[Mesh:noexp] OR ‘Africa’[Mesh:noexp] OR ‘Africa, Northern’[Mesh:noexp] OR ‘Africa South of the Sahara’[Mesh:noexp] OR ‘Africa, Central’[Mesh:noexp] OR ‘Africa, Eastern’[Mesh:noexp] OR ‘Africa, Southern’[Mesh:noexp] OR ‘Africa, Western’[Mesh:noexp] OR ‘Asia’[Mesh:noexp] OR ‘Asia, Central’[Mesh:noexp] OR ‘Asia, Southeastern’[Mesh:noexp] OR ‘Asia, Western’[Mesh:noexp] OR ‘Caribbean Region’[Mesh:noexp] OR ‘West Indies’[Mesh:noexp] OR ‘South America’[Mesh:noexp] OR ‘Latin America’[Mesh:noexp] OR ‘Central America’[Mesh:noexp] OR ‘Afghanistan’[Mesh:noexp] OR ‘Albania’[Mesh:noexp] OR ‘Algeria’[Mesh:noexp] OR ‘American Samoa’[Mesh:noexp] OR ‘Angola’[Mesh:noexp] OR ‘Antigua and Barbuda’[Mesh:noexp] OR ‘Argentina’[Mesh:noexp] OR ‘Armenia’[Mesh:noexp] OR ‘Azerbaijan’[Mesh:noexp] OR ‘Bahrain’[Mesh:noexp] OR ‘Bangladesh’[Mesh:noexp] OR ‘Barbados’[Mesh:noexp] OR ‘Benin’[Mesh:noexp] OR ‘Byelarus’[Mesh:noexp] OR ‘Belize’[Mesh:noexp] OR ‘Bhutan’[Mesh:noexp] OR ‘Bolivia’[Mesh:noexp] OR ‘Bosnia‐Herzegovina’[Mesh:noexp] OR ‘Botswana’[Mesh:noexp] OR ‘Brazil’[Mesh:noexp] OR ‘Bulgaria’[Mesh:noexp] OR ‘Burkina Faso’[Mesh:noexp] OR ‘Burundi’[Mesh:noexp] OR ‘Cambodia’[Mesh:noexp] OR ‘Cameroon’[Mesh:noexp] OR ‘Cape Verde’[Mesh:noexp] OR ‘Central African Republic’[Mesh:noexp] OR ‘Chad’[Mesh:noexp] OR ‘Chile’[Mesh:noexp] OR ‘China’[Mesh:noexp] OR ‘Colombia’[Mesh:noexp] OR ‘Comoros’[Mesh:noexp] OR ‘Congo’[Mesh:noexp] OR ‘Costa Rica’[Mesh:noexp] OR ‘Cote dIvoire’[Mesh:noexp] OR ‘Croatia’[Mesh:noexp] OR ‘Cuba’[Mesh:noexp] OR ‘Cyprus’[Mesh:noexp] OR ‘Czechoslovakia’[Mesh:noexp] OR ‘Czech Republic’[Mesh:noexp] OR ‘Slovakia’[Mesh:noexp] OR ‘Djibouti’[Mesh:noexp] OR ‘Democratic Republic of the Congo’[Mesh:noexp] OR ‘Dominica’[Mesh:noexp] OR ‘Dominican Republic’[Mesh:noexp] OR ‘East Timor’[Mesh:noexp] OR ‘Ecuador’[Mesh:noexp] OR ‘Egypt’[Mesh:noexp] OR ‘El Salvador’[Mesh:noexp] OR ‘Eritrea’[Mesh:noexp] OR ‘Estonia’[Mesh:noexp] OR ‘Ethiopia’[Mesh:noexp] OR ‘Fiji’[Mesh:noexp] OR ‘Gabon’[Mesh:noexp] OR ‘Gambia’[Mesh:noexp] OR ‘Georgia (Republic)’[Mesh:noexp] OR ‘Ghana’[Mesh:noexp] OR ‘Greece’[Mesh:noexp] OR ‘Grenada’[Mesh:noexp] OR ‘Guatemala’[Mesh:noexp] OR ‘Guinea’[Mesh:noexp] OR ‘Guinea‐Bissau’[Mesh:noexp] OR ‘Guam’[Mesh:noexp] OR ‘Guyana’[Mesh:noexp] OR ‘Haiti’[Mesh:noexp] OR ‘Honduras’[Mesh:noexp] OR ‘Hungary’[Mesh:noexp] OR ‘India’[Mesh:noexp] OR ‘Indonesia’[Mesh:noexp] OR ‘Iran’[Mesh:noexp] OR ‘Iraq’[Mesh:noexp] OR ‘Jamaica’[Mesh:noexp] OR ‘Jordan’[Mesh:noexp] OR ‘Kazakhstan’[Mesh:noexp] OR ‘Kenya’[Mesh:noexp] OR ‘Korea’[Mesh:noexp] OR ‘Kosovo’[Mesh:noexp] OR ‘Kyrgyzstan’[Mesh:noexp] OR ‘Laos’[Mesh:noexp] OR ‘Latvia’[Mesh:noexp] OR ‘Lebanon’[Mesh:noexp] OR ‘Lesotho’[Mesh:noexp] OR ‘Liberia’[Mesh:noexp] OR ‘Libya’[Mesh:noexp] OR ‘Lithuania’[Mesh:noexp] OR ‘Macedonia’[Mesh:noexp] OR ‘Madagascar’[Mesh:noexp] OR ‘Malaysia’[Mesh:noexp] OR ‘Malawi’[Mesh:noexp] OR ‘Mali’[Mesh:noexp] OR ‘Malta’[Mesh:noexp] OR ‘Mauritania’[Mesh:noexp] OR ‘Mauritius’[Mesh:noexp] OR ‘Mexico’[Mesh:noexp] OR ‘Micronesia’[Mesh:noexp] OR ‘Middle East’[Mesh:noexp] OR ‘Moldova’[Mesh:noexp] OR ‘Mongolia’[Mesh:noexp] OR ‘Montenegro’[Mesh:noexp] OR ‘Morocco’[Mesh:noexp] OR ‘Mozambique’[Mesh:noexp] OR ‘Myanmar’[Mesh:noexp] OR ‘Namibia’[Mesh:noexp] OR ‘Nepal’[Mesh:noexp] OR ‘Netherlands Antilles’[Mesh:noexp] OR ‘New Caledonia’[Mesh:noexp] OR ‘Nicaragua’[Mesh:noexp] OR ‘Niger’[Mesh:noexp] OR ‘Nigeria’[Mesh:noexp] OR ‘Oman’[Mesh:noexp] OR ‘Pakistan’[Mesh:noexp] OR ‘Palau’[Mesh:noexp] OR ‘Panama’[Mesh:noexp] OR ‘Papua New Guinea’[Mesh:noexp] OR ‘Paraguay’[Mesh:noexp] OR ‘Peru’[Mesh:noexp] OR ‘Philippines’[Mesh:noexp] OR ‘Poland’[Mesh:noexp] OR ‘Portugal’[Mesh:noexp] OR ‘Puerto Rico’[Mesh:noexp] OR ‘Romania’[Mesh:noexp] OR ‘Russia’[Mesh:noexp] OR ‘Russia (Pre‐1917)’[Mesh:noexp] OR ‘Rwanda’[Mesh:noexp] OR ‘Saint Kitts and Nevis’[Mesh:noexp] OR ‘Saint Lucia’[Mesh:noexp] OR ‘Saint Vincent and the Grenadines’[Mesh:noexp] OR ‘Samoa’[Mesh:noexp] OR ‘Saudi Arabia’[Mesh:noexp] OR ‘Senegal’[Mesh:noexp] OR ‘Serbia’[Mesh:noexp] OR ‘Montenegro’[Mesh:noexp] OR ‘Seychelles’[Mesh:noexp] OR ‘Sierra Leone’[Mesh:noexp] OR ‘Slovenia’[Mesh:noexp] OR ‘Sri Lanka’[Mesh:noexp] OR ‘Somalia’[Mesh:noexp] OR ‘South Africa’[Mesh:noexp] OR ‘Sudan’[Mesh:noexp] OR ‘Suriname’[Mesh:noexp] OR ‘Swaziland’[Mesh:noexp] OR ‘Syria’[Mesh:noexp] OR ‘Tajikistan’[Mesh:noexp] OR ‘Tanzania’[Mesh:noexp] OR ‘Thailand’[Mesh:noexp] OR ‘Togo’[Mesh:noexp] OR ‘Tonga’[Mesh:noexp] OR ‘Trinidad and Tobago’[Mesh:noexp] OR ‘Tunisia’[Mesh:noexp] OR ‘Turkey’[Mesh:noexp] OR ‘Turkmenistan’[Mesh:noexp] OR ‘Uganda’[Mesh:noexp] OR ‘Ukraine’[Mesh:noexp] OR ‘Uruguay’[Mesh:noexp] OR ‘USSR’[Mesh:noexp] OR ‘Uzbekistan’[Mesh:noexp] OR ‘Vanuatu’[Mesh:noexp] OR ‘Venezuela’[Mesh:noexp] OR ‘Vietnam’[Mesh:noexp] OR ‘Yemen’[Mesh:noexp] OR ‘Yugoslavia’[Mesh:noexp] OR ‘Zambia’[Mesh:noexp] OR ‘Zimbabwe’[Mesh:noexp]) AND (1950:2019/10/15[pdat]) (1,307,784) |
| Search strategy: (A) AND (B) AND (C) – 46,165 |
TABLE A2.
Evidence sources for framework components
| Peer‐reviewed articles | Technical documents | |
|---|---|---|
| Overall structure | King et al. (2021) and Xu et al. (2021) | The state of the world's children 1998. (United Nations Children's Fund, 1998) |
| Context | Allouche (2011), DeNicola et al. (2015), Biran et al. (2014), De Buck et al. (2017), Reinhardt and Fanzo (2014) and Cain and Rotella (2001) |
Guidelines on sanitation and health. (World Health Organization, 2018) Guidelines for drinking‐water quality. (World Health Organization, 2017) Transforming our world: The 2030 agenda for sustainable development. (United Nations, 2015) |
| Water, sanitation and hygiene | Alsan and Goldin (2019), Cutler and Miller (2005), Bhalotra et al. (2017), Duflo et al. (2015), Biran et al. (2014), Cain and Rotella (2001), Strunz et al. (2014), Garn et al. (2017), Pickering, Null, et al. (2019), Dreibelbis et al. (2013), Oswald et al. (2008), Pickering and Davis (2012), Arnold et al. (2013), Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Team et al. (2015) and Young et al. (2019) |
Guidelines for drinking‐water quality. (World Health Organization, 2017) Guidelines on sanitation and health. (World Health Organization, 2018) Guidelines for the safe use of wastewater, excreta and greywater (World Health Organization, 2006) Improving nutrition outcomes with better water, sanitation and hygiene: Practical solutions for policies and programmes. (World Health Organization, UNICEF,, & USAID, 2015) JMP Methodology 2017 Update & SDG Baselines. (World Health Organization & United Nations Children's Fund, 2018) |
| Underlying causes | Wagner and Lanoix (1958), Kumwenda et al. (2017), Ngure et al. (2013), Ejemot‐Nwadiaro et al. (2015), Luby et al. (2010), Curtis et al. (2011), Hirai et al. (2016), Nizame et al. (2013), Schmidt et al. (2009), Jenkins and Scott (2007) and Pickering, Swarthout, et al. (2019) | Management of child feces: current disposal practices. (Water and Sanitation Program & United Nations Children's Fund (UNICEF), 2015) |
| Immediate causes | Checkley et al. (2008), Lima et al. (2000), Liu et al. (2016), Jones et al. (2015), Humphrey (2009), Prendergast and Kelly (2016), Mbuya and Humphrey (2016), Harper et al. (2018), Rogawski et al. (2018), Echazú et al. (2015), Kassebaum (2016) and Cumming et al. (2019) | |
| Health outcomes | Bhalotra et al. (2017), Black et al. (2013), Humphrey et al. (2019), Luby et al. (2018), Null et al. (2018), Alsan and Goldin (2019), Cain and Rotella (2001), Cutler and Miller (2005), Kesztenbaum and Rosenthal (2014), Ogasawara et al. (2018), Monteiro et al. (2009), Danaei et al. (2016) and Esrey (1996) |
Zavala, E. , King, S. E. , Sawadogo‐Lewis, T. , & Roberton, T. (2021). Leveraging water, sanitation and hygiene for nutrition in low‐ and middle‐income countries: A conceptual framework. Matern Child Nutr. 2021;17:e13202. 10.1111/mcn.13202
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- Allouche, J. (2011). The sustainability and resilience of global water and food systems: Political analysis of the interplay between security, resource scarcity, political systems and global trade. Food Policy, 36, S3–S8. 10.1016/j.foodpol.2010.11.013 [DOI] [Google Scholar]
- Alsan, M. , & Goldin, C. (2019). Watersheds in child mortality: The role of effective water and sewerage infrastructure, 1880 to 1920. Journal of Political Economy, 127(2), 586–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold, B. F. , Null, C. , Luby, S. P. , Unicomb, L. , Stewart, C. P. , Dewey, K. G. , Ahmed, T. , Ashraf, S. , Christensen, G. , Clasen, T. , Dentz, H. N. , & Colford, J. M. (2013). Cluster‐randomised controlled trials of individual and combined water, sanitation, hygiene and nutritional interventions in rural Bangladesh and Kenya: The WASH Benefits study design and rationale. BMJ Open, 3(8). 10.1136/bmjopen-2013-003476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhalotra, S. R. , Diaz‐Cayeros, A. , Miller, G. , Miranda, A. , & Venkataramani, A. S. (2017). Urban water disinfection and mortality decline in developing countries (Working Paper No. 23239). National Bureau of Economic Research. 10.3386/w23239 [DOI] [Google Scholar]
- Biran, A. , Schmidt, W.‐P. , Varadharajan, K. S. , Rajaraman, D. , Kumar, R. , Greenland, K. , Gopalan, B. , Aunger, R. , & Curtis, V. (2014). Effect of a behaviour‐change intervention on handwashing with soap in India (SuperAmma): A cluster‐randomised trial. The Lancet Global Health, 2(3), e145–e154. 10.1016/S2214-109X(13)70160-8 [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , de Onis, M. , Ezzati, M. , Grantham‐McGregor, S. , Katz, J. , Martorell, R. , Uauy, R. , & Maternal and Child Nutrition Study Group . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet (London, England), 382(9890), 427–451. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- Cain, L. , & Rotella, E. (2001). Death and spending: Urban mortality and municipal expenditure on sanitation. Annales de demographie historique, no, 101(1), 139–154. [Google Scholar]
- Checkley, W. , Buckley, G. , Gilman, R. H. , Assis, A. M. , Guerrant, R. L. , Morris, S. S. , Mølbak, K. , Valentiner‐Branth, P. , Lanata, C. F. , Black, R. E. , & Childhood Malnutrition and Infection Network . (2008). Multi‐country analysis of the effects of diarrhoea on childhood stunting. International Journal of Epidemiology, 37(4), 816–830. 10.1093/ije/dyn099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkley, W. , Gilman, R. H. , Black, R. E. , Epstein, L. D. , Cabrera, L. , Sterling, C. R. , & Moulton, L. H. (2004). Effect of water and sanitation on childhood health in a poor Peruvian peri‐urban community. The Lancet, 363(9403), 112–118. 10.1016/S0140-6736(03)15261-0 [DOI] [PubMed] [Google Scholar]
- Cumming, O. , Arnold, B. F. , Ban, R. , Clasen, T. , Esteves Mills, J. , Freeman, M. C. , Gordon, B. , Guiteras, R. , Howard, G. , Hunter, P. R. , Johnston, R. B. , & Colford, J. M. (2019). The implications of three major new trials for the effect of water, sanitation and hygiene on childhood diarrhea and stunting: A consensus statement. BMC Medicine, 17(1), 173. 10.1186/s12916-019-1410-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis, V. , Schmidt, W. , Luby, S. , Florez, R. , Touré, O. , & Biran, A. (2011). Hygiene: New hopes, new horizons. The Lancet Infectious Diseases, 11(4), 312–321. 10.1016/S1473-3099(10)70224-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler, D. , & Miller, G. (2005). The role of public health improvements in health advances: The twentieth‐century United States. Demography, 42(1), 1–22. 10.1353/dem.2005.0002 [DOI] [PubMed] [Google Scholar]
- Danaei, G. , Andrews, K. G. , Sudfeld, C. R. , Fink, G. , McCoy, D. C. , Peet, E. , Sania, A. , Smith Fawzi, M. C. , Ezzati, M. , & Fawzi, W. W. (2016). Risk factors for childhood stunting in 137 developing countries: A comparative risk assessment analysis at global, regional, and country levels. PLoS Medicine, 13(11). 10.1371/journal.pmed.1002164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Buck, E. , Van Remoortel, H. , Hannes, K. , Govender, T. , Naidoo, S. , Avau, B. , … Young, T. (2017). Promoting handwashing and sanitation behaviour change in low‐ and middle‐income countries: A mixed‐method systematic review. London: International Initiative for Impact Evaluation (3ie). [Google Scholar]
- DeNicola, E. , Aburizaiza, O. S. , Siddique, A. , Khwaja, H. , & Carpenter, D. O. (2015). Climate change and water scarcity: The case of Saudi Arabia. Annals of Global Health, 81(3), 342–353. 10.1016/j.aogh.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Dreibelbis, R. , Winch, P. J. , Leontsini, E. , Hulland, K. R. S. , Ram, P. K. , Unicomb, L. , & Luby, S. P. (2013). The integrated behavioural model for water, sanitation, and hygiene: A systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure‐restricted settings. BMC Public Health, 13, 1015. 10.1186/1471-2458-13-1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duflo, E. , Greenstone, M. , Guiteras, R. , & Clasen, T. (2015). Toilets can work: Short and medium run health impacts of addressing complementarities and externalities in water and sanitation (Working Paper No. 21521). National Bureau of Economic Research. 10.3386/w21521 [DOI] [Google Scholar]
- Echazú, A. , Bonanno, D. , Juarez, M. , Cajal, S. P. , Heredia, V. , Caropresi, S. , Cimino, R. O. , Caro, N. , Vargas, P. A. , Paredes, G. , & Krolewiecki, A. J. (2015). Effect of poor access to water and sanitation as risk factors for soil‐transmitted helminth infection: Selectiveness by the infective route. PLoS Neglected Tropical Diseases, 9(9). 10.1371/journal.pntd.0004111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejemot‐Nwadiaro, R. I. , Ehiri, J. E. , Arikpo, D. , Meremikwu, M. M. , & Critchley, J. A. (2015). Hand washing promotion for preventing diarrhoea. Cochrane Database of Systematic Reviews, 9. 10.1002/14651858.CD004265.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esrey, S. A. (1996). Water, waste, and well‐being: A multicountry study. American Journal of Epidemiology, 143(6), 608–623. 10.1093/oxfordjournals.aje.a008791 [DOI] [PubMed] [Google Scholar]
- Garn, J. V. , Sclar, G. D. , Freeman, M. C. , Penakalapati, G. , Alexander, K. T. , Brooks, P. , … Clasen, T. F. (2017). The impact of sanitation interventions on latrine coverage and latrine use: A systematic review and meta‐analysis. International Journal of Hygiene and Environmental Health, 220(2 Pt B), 329–340. 10.1016/j.ijheh.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper, K. M. , Mutasa, M. , Prendergast, A. J. , Humphrey, J. , & Manges, A. R. (2018). Environmental enteric dysfunction pathways and child stunting: A systematic review. PLoS Neglected Tropical Diseases, 12(1). 10.1371/journal.pntd.0006205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirai, M. , Graham, J. P. , Mattson, K. D. , Kelsey, A. , Mukherji, S. , & Cronin, A. A. (2016). Exploring determinants of handwashing with soap in Indonesia: A quantitative analysis. International Journal of Environmental Research and Public Health, 13(9), 868. 10.3390/ijerph13090868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphrey, J. H. (2009). Child undernutrition, tropical enteropathy, toilets, and handwashing. The Lancet, 374(9694), 1032–1035. 10.1016/S0140-6736(09)60950-8 [DOI] [PubMed] [Google Scholar]
- Humphrey, J. H. , Mbuya, M. N. N. , Ntozini, R. , Moulton, L. H. , Stoltzfus, R. J. , Tavengwa, N. V. , Mutasa, K. , Majo, F. , Mutasa, B. , Mangwadu, G. , Chasokela, C. M. , & Makoni, T. (2019). Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: A cluster‐randomised trial. The Lancet Global Health, 7(1), e132–e147. 10.1016/S2214-109X(18)30374-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins, M. W. , & Scott, B. (2007). Behavioral indicators of household decision‐making and demand for sanitation and potential gains from social marketing in Ghana. Social Science & Medicine, 64(12), 2427–2442. 10.1016/j.socscimed.2007.03.010 [DOI] [PubMed] [Google Scholar]
- Jones, A. D. , Rukobo, S. , Chasekwa, B. , Mutasa, K. , Ntozini, R. , Mbuya, M. N. N. , … Prendergast, A. J. (2015). Acute illness is associated with suppression of the growth hormone axis in Zimbabwean infants. The American Journal of Tropical Medicine and Hygiene, 92(2), 463–470. 10.4269/ajtmh.14-0448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassebaum, N. J. (2016). The Global Burden of Anemia. Hematology/Oncology Clinics of North America, 30(2), 247–308. 10.1016/j.hoc.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Kesztenbaum, L. , & Rosenthal, J.‐L. (2014). Income versus sanitation; Mortality decline in Paris, 1880–1914. In PSE Working Papers (No. halshs‐01018594). HAL. Retrieved from HAL website: https://ideas.repec.org/p/hal/psewpa/halshs‐01018594.html
- King, S. E. , Sawadogo‐Lewis, T. , Black, R. E. , & Roberton, T. (2021). Making the health system work for the delivery of nutrition interventions. Maternal & Child Nutrition, 17(1), e13056. 10.1111/mcn.13056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumwenda, S. , Msefula, C. , Kadewa, W. , Ngwira, B. , & Morse, T. (2017). Estimating the health risk associated with the use of ecological sanitation toilets in Malawi [Research Article]. 10.1155/2017/3931802 [DOI] [PMC free article] [PubMed]
- Lima, A. A. , Moore, S. R. , Barboza, M. S. , Soares, A. M. , Schleupner, M. A. , Newman, R. D. , Sears, C. L. , Nataro, J. P. , Fedorko, D. P. , Wuhib, T. , Schorling, J. B. , & Guerrant, R. L. (2000). Persistent diarrhea signals a critical period of increased diarrhea burdens and nutritional shortfalls: A prospective cohort study among children in northeastern Brazil. The Journal of Infectious Diseases, 181(5), 1643–1651. 10.1086/315423 [DOI] [PubMed] [Google Scholar]
- Liu, J. , Platts‐Mills, J. A. , Juma, J. , Kabir, F. , Nkeze, J. , Okoi, C. , Operario, D. J. , Uddin, J. , Ahmed, S. , Alonso, P. L. , Antonio, M. , & Houpt, E. R. (2016). Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: A reanalysis of the GEMS case‐control study. Lancet (London, England), 388(10051), 1291–1301. 10.1016/S0140-6736(16)31529-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby, S. P. , Kadir, M. A. , Sharker, M. A. Y. , Yeasmin, F. , Unicomb, L. , & Islam, M. S. (2010). A community‐randomised controlled trial promoting waterless hand sanitizer and handwashing with soap, Dhaka, Bangladesh. Tropical Medicine & International Health, 15(12), 1508–1516. 10.1111/j.1365-3156.2010.02648.x [DOI] [PubMed] [Google Scholar]
- Luby, S. P. , Rahman, M. , Arnold, B. F. , Unicomb, L. , Ashraf, S. , Winch, P. J. , Ahmed, T. , Jannat, K. K. , & Colford, J. M. (2018). Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: A cluster randomised controlled trial. The Lancet Global Health, 6(3), e302–e315. 10.1016/S2214-109X(17)30490-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbuya, M. N. N. , & Humphrey, J. H. (2016). Preventing environmental enteric dysfunction through improved water, sanitation and hygiene: An opportunity for stunting reduction in developing countries. Maternal & Child Nutrition, 12(S1), 106–120. 10.1111/mcn.12220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro, C. A. , Benicio, M. H. D. , Konno, S. C. , da Silva, A. C. F. , de Lima, A. L. L. , & Conde, W. L. (2009). Causes for the decline in child under‐nutrition in Brazil, 1996–2007. Revista De Saude Publica, 43(1), 35–43. 10.1590/s0034-89102009000100005 [DOI] [PubMed] [Google Scholar]
- Ngure, F. M. , Humphrey, J. H. , Mbuya, M. N. N. , Majo, F. , Mutasa, K. , Govha, M. , Mazarura, E. , Chasekwa, B. , Prendergast, A. J. , Curtis, V. , Boor, K. J. , & Stoltzfus, R. J. (2013). Formative research on hygiene behaviors and geophagy among infants and young children and implications of exposure to fecal bacteria. The American Journal of Tropical Medicine and Hygiene, 89(4), 709–716. 10.4269/ajtmh.12-0568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nizame, F. A. , Unicomb, L. , Sanghvi, T. , Roy, S. , Nuruzzaman, M. , Ghosh, P. K. , Winch, P. J. , & Luby, S. P. (2013). Handwashing before food preparation and child feeding: A missed opportunity for hygiene promotion. The American Journal of Tropical Medicine and Hygiene, 89(6), 1179–1185. 10.4269/ajtmh.13-0434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Null, C. , Stewart, C. P. , Pickering, A. J. , Dentz, H. N. , Arnold, B. F. , Arnold, C. D. , … Colford, J. M. (2018). Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: A cluster‐randomised controlled trial. The Lancet Global Health, 6(3), e316–e329. 10.1016/S2214-109X(18)30005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogasawara, K. , Shirota, S. , & Kobayashi, G. (2018). Public health improvements and mortality in interwar Tokyo: A Bayesian disease mapping approach. Cliometrica, Journal of Historical Economics and Econometric History, 1, 1–31. [Google Scholar]
- Oswald, W. E. , Hunter, G. C. , Lescano, A. G. , Cabrera, L. , Leontsini, E. , Pan, W. K. , Soldan, V. P. , & Gilman, R. H. (2008). Direct observation of hygiene in a Peruvian shantytown: Not enough handwashing and too little water. Tropical Medicine & International Health, 13(11), 1421–1428. 10.1111/j.1365-3156.2008.02177.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering, A. J. , & Davis, J. (2012). Freshwater availability and water fetching distance affect child health in sub‐Saharan Africa. Environmental Science & Technology, 46(4), 2391–2397. 10.1021/es203177v [DOI] [PubMed] [Google Scholar]
- Pickering, A. J. , Null, C. , Winch, P. J. , Mangwadu, G. , Arnold, B. F. , Prendergast, A. J. , Njenga, S. M. , Rahman, M. , Ntozini, R. , Benjamin‐Chung, J. , Stewart, C. P. , & Humphrey, J. H. (2019). The WASH Benefits and SHINE trials: Interpretation of WASH intervention effects on linear growth and diarrhoea. The Lancet Global Health, 7(8), e1139–e1146. 10.1016/S2214-109X(19)30268-2 [DOI] [PubMed] [Google Scholar]
- Pickering, A. J. , Swarthout, J. , Mureithi, M. , Mboya, J. , Arnold, B. F. , Wolfe, M. , Dentz, H. N. , Lin, A. , Arnold, C. D. , Rao, G. , Stewart, C. P. , & Null, C. (2019). Can individual and integrated water, sanitation, and handwashing interventions reduce fecal contamination in the household environment? Evidence from the WASH Benefits cluster‐randomized trial in rural Kenya. BioRxiv, 731992. 10.1101/731992 [DOI] [Google Scholar]
- Prendergast, A. , & Kelly, P. (2016). Interactions between intestinal pathogens, enteropathy and malnutrition in developing countries. Current Opinion in Infectious Diseases, 29(3), 229–236. 10.1097/QCO.0000000000000261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt, K. , & Fanzo, J. (2014). Addressing chronic malnutrition through multi‐sectoral, sustainable approaches: A review of the causes and consequences. Frontiers in Nutrition, 1. 10.3389/fnut.2014.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogawski, E. T. , Liu, J. , Platts‐Mills, J. A. , Kabir, F. , Lertsethtakarn, P. , Siguas, M. , Khan, S. S. , Praharaj, I. , Murei, A. , Nshama, R. , Mujaga, B. , & MAL‐ED Network Investigators . (2018). Use of quantitative molecular diagnostic methods to investigate the effect of enteropathogen infections on linear growth in children in low‐resource settings: Longitudinal analysis of results from the MAL‐ED cohort study. The Lancet. Global Health, 6(12), e1319–e1328. 10.1016/S2214-109X(18)30351-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial Team , Humphrey, J. H. , Jones, A. D. , Manges, A. , Mangwadu, G. , Maluccio, J. A. , Mbuya, M. N. , Moulton, L. H. , Ntozini, R. , Prendergast, A. J. , & Tielsch, J. M. (2015). The Sanitation Hygiene Infant Nutrition Efficacy (SHINE) trial: Rationale, design, and methods. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 61(Suppl 7), S685–S702. 10.1093/cid/civ844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, W.‐P. , Aunger, R. , Coombes, Y. , Maina, P. M. , Matiko, C. N. , Biran, A. , & Curtis, V. (2009). Determinants of handwashing practices in Kenya: The role of media exposure, poverty and infrastructure. Tropical Medicine & International Health, 14(12), 1534–1541. 10.1111/j.1365-3156.2009.02404.x [DOI] [PubMed] [Google Scholar]
- Strunz, E. C. , Addiss, D. G. , Stocks, M. E. , Ogden, S. , Utzinger, J. , & Freeman, M. C. (2014). Water, sanitation, hygiene, and soil‐transmitted helminth infection: A systematic review and meta‐analysis. PLoS Medicine, 11(3), e1001620. 10.1371/journal.pmed.1001620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF , WHO , & World Bank Group . (2020). UNICEF/WHO/The World Bank Group joint child malnutrition estimates: Levels and trends in child malnutrition: key findings of the 2020 edition. Retrieved November 5, 2020, from https://www.who.int/publications‐detail‐redirect/jme‐2020‐edition
- United Nations . (2015). Transforming our world: The 2030 agenda for sustainable development. New York, NY. [Google Scholar]
- United Nations Children's Fund . (1998). The state of the world's children 1998. New York, NY: UNICEF. [Google Scholar]
- Victora, C. G. , Adair, L. , Fall, C. , Hallal, P. C. , Martorell, R. , Richter, L. , & Sachdev, H. S. (2008). Maternal and child undernutrition: Consequences for adult health and human capital. The Lancet, 371(9609), 340–357. 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, E. G. , & Lanoix, J. N. (1958). Excreta disposal for rural areas and small communities. Monograph Series. World Health Organization, 39, 1–182. [PubMed] [Google Scholar]
- Water and Sanitation Program, & United Nations Children's Fund (UNICEF) . (2015). Management of child feces: Current disposal practices. The World Bank. [Google Scholar]
- World Health Organization . (2006). Guidelines for the safe use of wastewater, excreta and greywater—Volume 1. Geneva, Switzerland: World Health Organization. Retrieved from World Health Organization website. https://www.who.int/water_sanitation_health/sanitation‐waste/wastewater/wastewater‐guidelines/en/ [Google Scholar]
- World Health Organization . (2017). Guidelines for drinking‐water quality: Fourth edition incorporating the first addendum. Geneva, Switzerland: World Health Organization. Retrieved from World Health Organization website. https://apps.who.int/iris/bitstream/handle/10665/254637/9789241549950‐eng.pdf?sequence=1 [PubMed] [Google Scholar]
- World Health Organization . (2018). Guidelines on sanitation and health. Geneva, Switzerland: WHO: Retrieved from WHO website. https://apps.who.int/iris/bitstream/handle/10665/274939/9789241514705‐eng.pdf [Google Scholar]
- World Health Organization, UNICEF, & USAID . (2015). Improving nutrition outcomes with better water, sanitation and hygiene: Practical solutions for policies and programmes. Geneva: Switzerland. [Google Scholar]
- World Health Organization , & United Nations Children's Fund . (2018). JMP Methodology 2017 Update & SDG Baselines.
- Xu, Y. Y. , Sawadogo‐Lewis, T. , King, S. E. , Mitchell, A. , & Roberton, T. (2021). Integrating nutrition into the education sector in low‐ and middle‐income countries: A framework for a win‐win collaboration. Maternal & Child Nutrition, e13156. 10.1111/mcn.13156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, S. L. , Boateng, G. O. , Jamaluddine, Z. , Miller, J. D. , Frongillo, E. A. , Neilands, T. B. , Collins, S. M. , Wutich, A. , Jepson, W. E. , Stoler, J. , & Stoler, J. (2019). The household water insecurity experiences (HWISE) scale: Development and validation of a household water insecurity measure for low‐income and middle‐income countries. BMJ Global Health, 4(5), e001750. 10.1136/bmjgh-2019-001750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, S. L. , Frongillo, E. A. , Jamaluddine, Z. , Melgar‐Quiñonez, H. , Pérez‐Escamilla, R. , Ringler, C. , & Rosinger, A. Y. (2021). Perspective: The importance of water security for ensuring food security, good nutrition, and well‐being. Advances in Nutrition (Bethesda, Md.). 10.1093/advances/nmab003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Detailed WASH to nutrition conceptual framework
Figure S2 WASH BCCM for health behaviour change and reduction of pathogenic exposure.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.


