Abstract
Background and aims
The COVID-19 pandemic continues to challenge us. Despite several strides in management, steroids remain the mainstay for treating moderate to severe disease and with it arises challenges such as hyperglycemia. The review aims to enhance awareness amongst physicians on steroid use and hyperglycemia.
Methods
An advisory document describing various strategies for hyperglycemia management was prepared in the public interest by DiabetesIndia.
Results
The review provides awareness on steroids and hyperglycemia, adverse outcomes of elevated blood glucose levels and, advice at the time of discharge.
Conclusions
The article emphasizes enhancing awareness on effective management of hyperglycemia during COVID-19.
Keywords: Steroids, Diabetes, Pharmacotherapy, Blood glucose, COVID-19
1. Introduction
The COVID-19 pandemic continues to challenge us. Despite several strides in management, steroids remain the cornerstone for treatment of severe disease and with it come challenges like immunosuppression and hyperglycemia. Management of acute hyperglycemia in critically ill and non-critically ill individuals to improve recovery rates from acute infection and reduce mortality is of paramount importance. Managing hyperglycemia in this setting requires different skills, with a greater theoretical and practical knowledge of insulin therapy. This article aims to increase awareness amongst physicians for effective management of hyperglycemia.
1.1. Steroid induced hyperglycemia-getting it under control
Steroids are medications used for treatment of several diseases, including COVID-19 [1,2]. While it is lifesaving in several individuals with COVID-19 infection (from moderate to severe), its pharmacological action increases blood glucose and poses additional challenges in the management. There is also an ongoing concern on inappropriate timing, dosing and duration of steroid use in COVID-19 among certain sections of the medical fraternity [[3], [4], [5]]. Hence it is important to understand the risk benefit ratio and learn how to manage rising blood glucose when steroids are used.
As per International Diabetes Federation, India has the challenge of:
-
1.
77 million people with diabetes
-
2.
25.2 million people with pre-diabetes (with Impaired Fasting Glucose or Impaired Glucose Tolerance)
-
3.
43.9 million people who are undiagnosed, as diabetes is often asymptomatic.
This document aims to increase awareness on the impact of steroids on blood sugar levels among all the 3 groups mentioned above and will provide an overview and guidance on monitoring and control of blood sugar levels.
1.2. How does steroid use during COVID – 19 infection increase blood glucose?
Steroids increase the blood sugar levels by various mechanisms.
-
1.
Increase the hepatic gluconeogenesis or production of glucose from the liver by enhancing the effect of counter regulatory hormones [6].
-
2.
Block the action of insulin and increase insulin resistance.
-
3.
Reduce uptake of glucose by the muscles and adipose tissue [7,8].
-
4.
May even reduce the action of Beta cells directly [9].
-
5.
Elevations in the levels of inflammatory cytokines as seen in COVID-19 further worsen insulin resistance [10].
-
6.
Stress of illness and fear of death can increase stress hormone response and can elevate blood glucose.
Note: Point No 5 & 6 are strictly not related to Steroid use but contribute to Hyperglycemia.
2. Diagnosis
Monitoring of blood glucose is thus very important in anyone diagnosed with COVID -19. This is advisable even if steroids have not been prescribed, as COVID -19 can cause new onset diabetes in high risk and susceptible population and can worsen blood sugar control in those with preexisting diabetes. Treatment of high blood glucose is necessary and must be immediate as good control can improve recovery rates and reduce risk of complications.
2.1. Looking for hyperglycemia in patients -know the facts
Stress, infection and steroids play a role in causing hyperglycemia. There are broadly 3 types of situations one could fall under:
2.1.1. Stress hyperglycemia
Is a condition of temporary rise in blood glucose in individuals without diabetes. In such cases the HbA1c is <5.7%, but high blood glucose are recorded during the acute illness.
Medications to control the blood glucose are necessary to improve recovery rates and it is possible to stop medications once the patient recovers in most. Very few progresses to develop diabetes.
2.1.2. Newly diagnosed diabetes
Prediabetes or susceptible individuals without previous history of diabetes, may get diagnosed with new onset diabetes based on the presence of one of the following:
Fasting blood glucose (FBG) ≥ 126 mg/dl
Post prandial sugar (PPBS) ≥ 180 mg/dl
Random blood sugar (RBS) ≥200 mg/dl
HbA1c ≥ 6.5%
2.1.3. Uncontrolled diabetes
Those with known diagnosis of diabetes present with high blood glucose despite taking their prescribed medications.
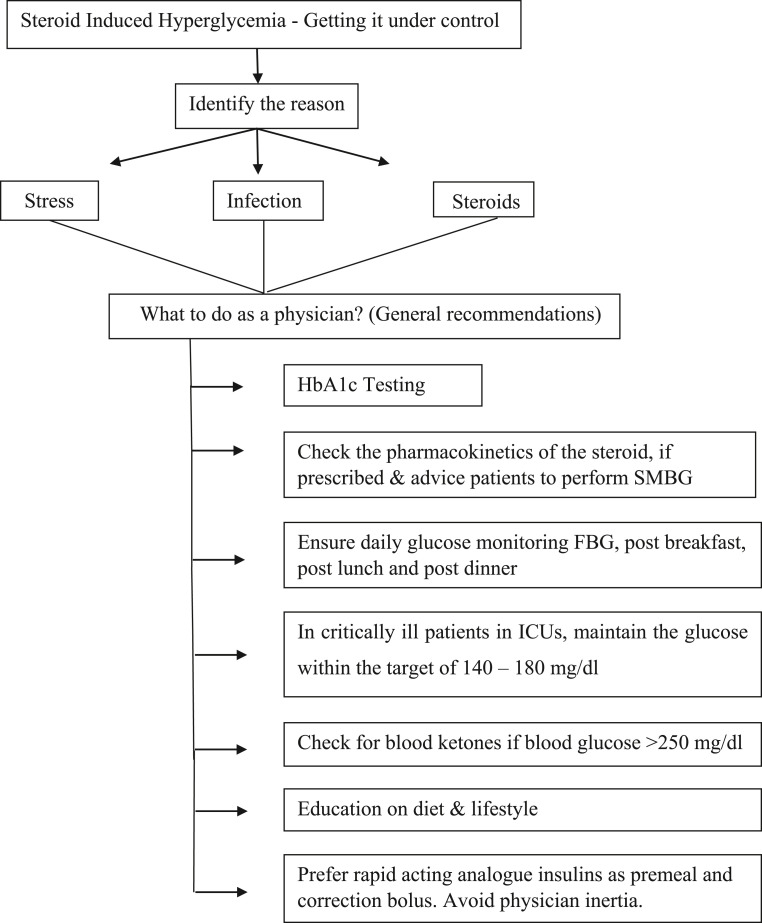
3. Things to do as a treating physician
-
1.
Get HbA1c done with High performance liquid chromatography (HPLC) method in all patients with COVID -19 infection at baseline.
-
2.
Rise in blood glucose depends on the time at which the steroid is dosed. Check the pharmacokinetics of the steroid being used and advise the patient on timing of self- monitoring of blood glucose (SMBG) (Fig. 1).
Fig. 1.
General recommendation for hyperglycemia control in COVID-19 patients.
In those on morning steroids, blood glucose rise post lunch and begin to fall post dinner. In those with long acting steroids or multiple doses of short acting steroids, hyperglycemia may be encountered throughout the day.
-
3.
Monitor FBG, post breakfast, post lunch and post dinner using a glucose meter daily.
-
4.
Try to maintain FBG< 130 mg/dl and all Prandial glucose <180 mg/dl. However, the targets can be relaxed in elderly and people with comorbid conditions.
-
5.
In critically ill patients in ICUs, maintain the glucose within the target of 140–180 mg/dl.
-
6.
Check for ketones in the blood if blood glucose are >300 mg/dl using capillary blood ketone strips. However, if euglycemic Diabetic ketoacidosis (DKA) is suspected, check for ketones if blood glucose cross 250 mg/dl. Urinary ketones values are not reliable and may get altered in patients taking Vitamin C.
-
7.
Diet and Lifestyle changes are a must and all patients must be educated in this aspect along with self-monitoring of blood glucose.
-
8.
Check liver function (LFT), Renal function and Cardiac function (in those with cardiac symptoms or history of cardiovascular disease or heart failure). Modify treatment of diabetes medications based on LFT and eGFR (estimated glomerular filtration rate).
-
9.
Continue daily SMBG monitoring and up titration of medications as glucose rise and down titration later during recovery or as steroids as tapered.
-
10.
As premeal and correction bolus, rapid acting analogue insulins are preferred due to its rapid action, short duration and with minimal risk of hypoglycemia (Aspart, Lispro, Glulisine) compared to older regular human insulin. Initiate insulin when indicated and overcome physician inertia. Do not use sliding scale insulin as the practice is outdated and unscientific.
4. Pharmacotherapy
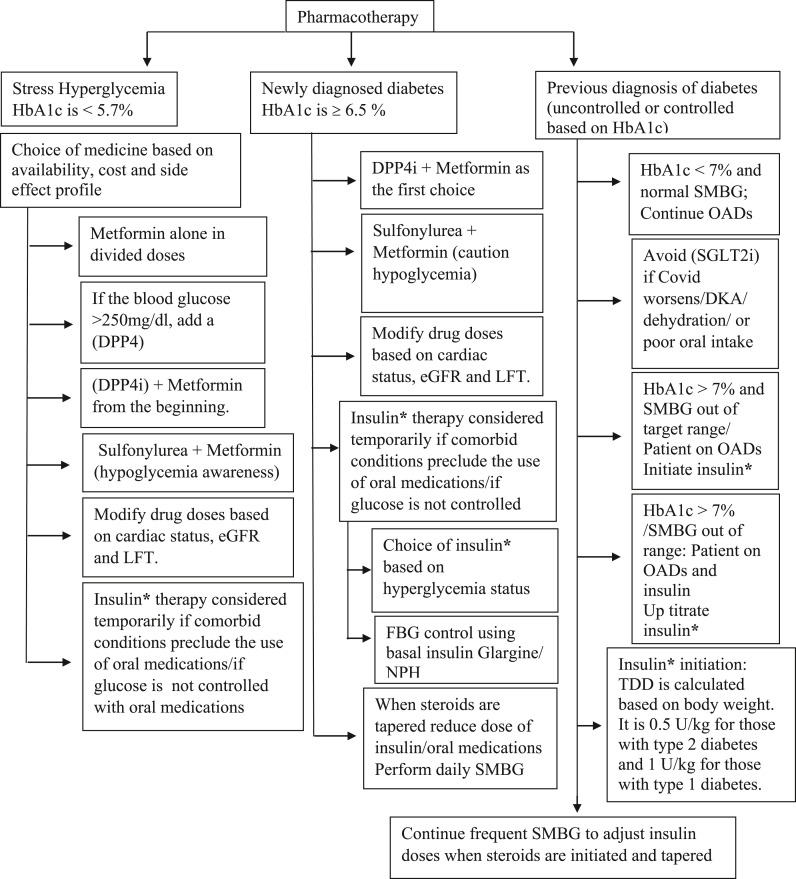
4.1. Scenario 1:Stress hyperglycemia where HbA1c is <5.7%
-
1.
Any medication prescribed must be used with proper prior knowledge of each molecule. Several options are available, and choice depends on availability, cost and side effect profile.
-
2.
Metformin alone in divided doses can control hyperglycemia. However, if the blood glucose is in excess of 250 mg/dl, adding a Dipeptidyl peptidase-4 inhibitor (DPP4i) help faster reduction of blood sugar.
-
3.
One can also start a combination of Dipeptidyl peptidase inhibitor (DPP4i) + Metformin right at the beginning. Choice of DPP4i is left to the treating physician.
-
4.
A Sulfonylurea + Metformin can also be used. The threat/possibility of hypoglycemia must be kept in mind.
-
5.
In several situations, drug doses need to be modified based on cardiac status, eGFR and LFT. Continuous monitoring every 2–3 days is often necessary in critically ill or hospitalized patients.
-
6.
Insulin therapy can be considered temporarily if comorbid conditions preclude the use of oral medications or if glucose are not controlled with oral medications.
-
7.
In most cases, blood glucose will return to normal in 4–6 weeks and no medication will be needed. Patients may be encouraged to continue lifestyle changes.
-
8.
In some cases, blood glucose may not return to normal values and this could be termed as ‘new onset diabetes’ and treatment would need to be continued (Fig. 2 ).
Fig. 2.
Pharmacotherapy of hyperglycemia in COVID-19.
∗Newer analogue insulins Glargine, Degludec (basal), Aspart, Lispro, Glulisine (rapid acting) have lesser chances for hypoglycemia and superior PK PD profile in the presence of organ derangement.
4.2. Scenario 2: Newly diagnosed diabetes where HbA1c is ≥ 6.5%
-
1.
Start a combination of DPP4i + Metformin as the first choice.
-
2.
A sulfonylurea + Metformin can also be used but the risk of hypoglycemia must be kept in mind. The patient must be educated well regarding all aspects of preventing, recognizing and treating hypoglycemia.
-
3.
In several situations, drug doses need to be modified based on cardiac status, eGFR and LFT. Continuous monitoring of FBG, post breakfast, post lunch and post dinner is often necessary in critically ill or hospitalized patients.
-
4.
Insulin therapy should be considered temporarily if comorbid conditions preclude the use of oral medications or if glucose is not controlled with oral medications.
4.2.1. Choice of insulin
This depends on when the patient has hyperglycemia and if there is hyperglycemia at just one time point or throughout the day. Monitoring all pre & post prandial glucose helps to identify this problem. It is thus necessary to understand pharmacological properties of different insulins to know which insulin is indicated based on when the blood sugar rises.
SLIDING SCALE is outdated and unscientific and should never be practiced in ICU, hospital care or at discharge.
-
1.
To control FBG use a basal insulin like Glargine or Neutral Protamine Hagedorn (NPH). Glargine works for 24 h and can be dosed either in the morning or at night but needs to be taken at the same time daily. NPH works for about 12 h and may need to be dosed twice-a-day (BID) if 24-h coverage is required.
-
2.
If the patient has a morning steroid dose, with rising glucose post lunch, NPH can be administered in the morning. This enables the peak of NPH to coincide with the rise in blood glucose levels.
-
3.
If the patient shows hyperglycemia both during fasting and after all the 3 meals (Breakfast (BF), Lunch & Dinner), basal bolus insulin therapy is indicated. In this situation a basal insulin like Glargine is administered once a day (morning or night) to control the FBG and a short acting or rapid acting insulin given at mealtime to cover post prandial spikes.
Note the following about Insulins:
-
1.
A short acting human insulin (regular insulin) needs to be given 30 min before the meal.
-
2.
A rapid acting analog (Aspart, Lispro, Glulisine) can be given 15 min before the meal.
-
3.
Ultrafast acting aspart can be dosed 2 min before or even up to 20 min after the start of the meal. Post meal dosing can be advantageous if the oral intake is unpredictable and the dose can be adjusted based on the food intake.
Blood glucose fluctuates a lot and if one is not sure as to how the glucose may fluctuate, it is best to use basal bolus therapy as it is flexible. The basal insulin can prevent ketogenesis and control the fasting glucose, and 1–3 mealtime boluses can be initiated based on the prandial values.
4.2.2. Monitoring of blood glucose levels and adjustment of insulin
-
1.
SMBG 4 times a day – fasting and post each meal in recommended.
-
2.
Adjust the basal insulin to control the FBG. Increase by 2–3 units daily to target a FBG< 130 mg/dl if NPH is used and dosed in the morning, adjust dose based on pre-dinner glucose.
-
3.
Adjust the corresponding mealtime insulin to control the PPBS< 180 mg/dl. As an example, if the post lunch glucose is high, increase the bolus given with lunch by 2–3 units the following day. Adjust the pre-dinner dose of mealtime insulin, to control PPBS post dinner. Adjust the pre-breakfast dose of mealtime insulin, to control the PPBS post breakfast.
-
4.
Advise monitoring whenever there are symptoms of hypoglycemia and at 2 or 3 a.m. to detect nocturnal hypoglycemia. Correct hypoglycemia with 15–20 g glucose or intravenous dextrose if hypoglycemia is severe. Change and adjust insulin dose if there is hypoglycemia. If there is hypoglycemia, reduce the following day the insulin dose given before hypo by 3–4 U. Do not skip subsequent doses of insulin if there is a hypoglycemia.
-
5.
Adjustment of insulin needs to be taught to every patient prior to discharge.
-
6.
When steroids are tapered, insulin requirement is bound to drop, and hence the dose of insulin or even oral medications (like sulfonylureas) may need to be reduced to avoid hypoglycemia. Perform daily SMBG to adjust insulin doses when steroids are initiated and tapered.
-
7.
Continuous Glucose Monitoring (CGM) has been approved by the Food and Drug Administration (FDA) for use in Intensive Care Unit (ICU) settings but Libre can be used under expert guidance in outpatient setting also.
-
8.
For eligible patients getting treated at home/hospital, CGM with Freestyle Libre can help easily maintain glucose targets with frequent doses of rapid/ultra-rapid analogue insulin eliminating both hypoglycemia and hyperglycemia.
4.3. Scenario 3: A person with a previous diagnosis of diabetes (uncontrolled or controlled based on HbA1c)
-
1.
HbA1c < 7% and normal SMBG: Patient only on oral antidiabetic medications (OADs) Continue OADs as before. Avoid Sodium-glucose co transporter 2 inhibitors (SGLT2i) if Covid worsens, patient has DKA, dehydration or if there is poor oral intake. Plan to initiate insulin as explained in scenario 2 if glucose goes above the target range.
-
2.
HbA1c < 7% and normal SMBG: Patient on OADs and insulin continue previous baseline medications. Avoid SGLT2i if Covid worsens, patient has DKA, dehydration or if there is poor oral intake. Titrate insulin as explained in scenario 2 if glucose go above the target range. It is likely that those on steroids require 2–4 times the amount of insulin compared to baseline.
-
3.
HbA1c > 7% and SMBG out of target range: Patient on OADs initiate insulin as explained in scenario 2 and titrate the dosage.
-
4.
HbA1c > 7% and SMBG out of range: Patient on OADs and insulin uptitrate the insulin regimen. It is likely that those on steroids require 2–4 times the amount of insulin compared to baseline. The requirement may be higher for those uncontrolled at baseline.
4.3.1. Choice of insulin and regimens
-
1.
If the patient is on twice daily 30/70 premix insulin, increase dosage by 10–20% when steroids are started.
-
2.
If post lunch glucose continues to be high, consider switching to three injections a day with a short acting insulin given with breakfast and lunch, and a 30/70 premix insulin given with dinner.
-
3.
In many cases, further titration to 4 injections a day may be necessary. So basal bolus insulin can be initiated on hospitalization or when high dose steroids are prescribed, and dose altered based on SMBG. For those already on 4 injections a day, it is likely that basal bolus insulin with a higher dose than baseline will be required to control the hyperglycemia.
-
4.
In case of Hypoglycemia at any time, reduce the dose given before hypoglycemia by 3–4 units the following day. Take the necessary action and administer 15–20g glucose and correct the hypoglycemia.
-
5.
In most cases, blood glucose will settle down as soon as the steroids are tapered and stopped, and doses may need to be reduced. Thus, continuing SMBG is critical to preventing hypoglycemia during recovery of 2–6 weeks post discharge. Perform daily SMBG to adjust insulin doses when steroids are initiated and tapered.
-
6.Those with Type 1 Diabetes:
-
1.It is essential to ensure that insulin is not stopped. SMBG frequency at 4–6 times per day must be continued and blood monitored for blood ketone levels.
-
2.A basal insulin must always be given as it helps to prevent ketogenesis with 3 mealtime shots given before the meals. Principles to adjust insulin therapy remain the same as in those with type 2 diabetes.
-
3.Hydration must be maintained orally or with intravenous fluids.
-
7.Diabetic ketoacidosis/Hyperglycemic hyperosmolar syndrome (DKA/HHS – If the patient is diagnosed with Diabetic ketoacidosis or hyperosmolar hyperglycemic state, IV insulin therapy is indicated). Each hospital is advised to develop standard protocols for IV insulin for use in such situations.
-
1.
4.4. Calculating total daily dose (TDD): if insulin needs to be initiated
-
1.
The TTD is calculated based on body weight. It is 0.5 U/kg for those with type 2 diabetes and 1 U/kg for those with type 1 diabetes.
-
2.
Half (50% of this is given as the basal insulin) and the other 50% is divided as 20% with breakfast, 20% with lunch and 10% with dinner as the mealtime bolus.
-
3.
Please note that the starting dose is calculated as given above for ease and will differ from patient to patient. Monitoring helps in titration of dose.
-
4.
Actual requirements may vary and may be much higher. Since insulin therapy is safe, it is important to titrate the insulin doses daily and achieve the SMBG targets.
-
5.Advice at the time of discharge
-
1.Comprehensive diabetes management including diet and lifestyle advise.
-
2.Risks associated with hyperglycemia and hypoglycemia.
-
3.Blood glucose monitoring at home and dosage adjustment as per patient requirement.
-
4.Self-Injection technique and site rotation.
-
5.Foot care and sick day rules.
-
6.Advice on reducing insulin as steroid dosage gets tapered.
-
7.Those with ‘Stress induced Diabetes’ to continue monitoring and to seek the help of the physician for future prevention of diabetes.
-
1.
5. Conclusion
The COVID-19 pandemic has opened our eyes on the importance of controlling hyperglycemia. The focus of diabetes management over the years has moved towards an individualized approach towards reduction of cardiovascular disease, kidney disease and microvascular complications. Uncontrolled diabetes a silent killer, needs timely appropriate management for better health care outcomes - both short and long term. In this situation, it is essential that we don't lose the war against diabetes, while we focus on winning the battle against COVID-19. It is one of those situations where we need a win-win!
References
- 1.Veronese N., Demurtas J., Yang L., Tonelli R., Barbagallo M., Lopalco P., et al. Use of corticosteroids in coronavirus disease 2019 pneumonia: a systematic review of the literature. Front. Clin. Med. 2020;7(170) doi: 10.3389/fmed.2020.00170. [Systematic Review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raju R., V P., Biatris P.S., SJUC J. Therapeutic role of corticosteroids in COVID-19: a systematic review of registered clinical trials. J. Pharmaceut. Sci. 2021;7(1):67. doi: 10.1186/s43094-021-00217-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yousefifard M., Mohamed Ali K., Aghaei A., Zali A., Madani Neishaboori A., Zarghi A., et al. Corticosteroids on the management of coronavirus disease 2019 (COVID-19): a systemic review and meta-analysis. Iran J Public Health. 2020;49(8):1411–1421. doi: 10.18502/ijph.v49i8.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W-j, Ni Z-y, Hu Y., Liang W-h, Ou C-q, He J-x, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alessi J., de Oliveira G.B., Schaan B.D., Telo G.H. Dexamethasone in the era of COVID-19: friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes. Diabetol Metab Syndrome. 2020;12(1):80. doi: 10.1186/s13098-020-00583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Venkatesan N., Lim J., Bouch C., Marciano D., Davidson M.B. Dexamethasone-induced impairment in skeletal muscle glucose transport is not reversed by inhibition of free fatty acid oxidation. Metab, Clin Exp. 1996;45(1):92–100. doi: 10.1016/s0026-0495(96)90205-x. [DOI] [PubMed] [Google Scholar]
- 8.Ruzzin J., Wagman A.S., Jensen J. Glucocorticoid-induced insulin resistance in skeletal muscles: defects in insulin signalling and the effects of a selective glycogen synthase kinase-3 inhibitor. Diabetologia. 2005;48(10):2119–2130. doi: 10.1007/s00125-005-1886-0. [DOI] [PubMed] [Google Scholar]
- 9.Hwang J.L., Weiss R.E. Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment. Diabetes Metabol Res Rev. 2014;30(2):96–102. doi: 10.1002/dmrr.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Esposito K., Nappo F., Marfella R., Giugliano G., Giugliano F., Ciotola M., et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans. Circulation. 2002;106(16):2067–2072. doi: 10.1161/01.cir.0000034509.14906.ae. [DOI] [PubMed] [Google Scholar]