Abstract
Background The COVID-19 pandemic led to dramatic increases in telemedicine use to provide outpatient care without in-person contact risks. Telemedicine increases options for health care access, but a “digital divide” of disparate access may prevent certain populations from realizing the benefits of telemedicine.
Objectives The study aimed to understand telemedicine utilization patterns after a widespread deployment to identify potential disparities exacerbated by expanded telemedicine usage.
Methods We performed a cross-sectional retrospective analysis of adults who scheduled outpatient visits between June 1, 2020 and August 31, 2020 at a single-integrated academic health system encompassing a broad range of subspecialties and a large geographic region in the Upper Midwest, during a period of time after the initial surge of COVID-19 when most standard clinical services had resumed. At the beginning of this study period, approximately 72% of provider visits were telemedicine visits. The primary study outcome was whether a patient had one or more video-based visits, compared with audio-only (telephone) visits or in-person visits only. The secondary outcome was whether a patient had any telemedicine visits (video-based or audio-only), compared with in-person visits only.
Results A total of 197,076 individuals were eligible (average age = 46 years, 56% females). Increasing age, rural status, Asian or Black/African American race, Hispanic ethnicity, and self-pay/uninsured status were significantly negatively associated with having a video visit. Digital literacy, measured by patient portal activation status, was significantly positively associated with having a video visit, as were Medicaid or Medicare as payer and American Indian/Alaskan Native race.
Conclusion Our findings reinforce previous evidence that older age, rural status, lower socioeconomic status, Asian race, Black/African American race, and Hispanic/Latino ethnicity are associated with lower rates of video-based telemedicine use. Health systems and policies should seek to mitigate such barriers to telemedicine when possible, with efforts such as digital literacy outreach and equitable distribution of telemedicine infrastructure.
Keywords: telemedicine, health care disparities, ambulatory care
Background and Significance
The COVID-19 pandemic generated national interest in telemedicine as a means of providing safe, effective health care without the risks of in-person contact. Telemedicine is defined by the World Health Organization as “the delivery of health care services using information and communication technologies for the exchange of valid information for diagnosis, treatment, and prevention of disease and injuries.” 1 2 The pandemic led to rapid expansion in both scale and scope of telemedicine services. According to a brief from the U.S. Department of Health and Human Services, 43.5% of Medicare primary care visits were conducted via telemedicine in April 2020, compared with 0.1% before the pandemic in February 2020. 3
Available evidence shows telemedicine is effective for chronic disease management, teleradiology, counseling, and mental health care. 4 5 Despite the potential of telemedicine to increase health care access options for all, the large-scale deployment of telemedicine may paradoxically exacerbate health care disparities. Socioeconomic status, digital literacy, language, and racial/ethnic access disparities may contribute to a “digital divide” of disparate technology utilization for health care purposes. 6 7 8
Rural Americans have more limited health care access and variable levels of insurance coverage, and face cultural and financial constraints when seeking care. 9 Furthermore, 23 million (38%) of rural Americans, as well as 1.6 million (41%) of all Americans living on tribal lands, lack access to broadband speed benchmarks set by the Federal Communications Commission, compared with 4% of urban Americans. 10 These data suggest barriers to telemedicine adoption (particularly video-based telemedicine) by rural patients. 11
Poor patients and people of color experience disproportionate levels of many chronic diseases. 12 Socioeconomic disadvantage, rurality, and race/ethnicity interact to influence health care outcomes. For example, the effects of poverty are compounded in rural populations due to a scarcity of resources and infrastructure. 13 Rural populations are thus more likely to experience socioeconomic disparities than their urban counterparts. 9 13
Video-based telemedicine provides a richer clinical experience than phone based, 14 15 but may require higher digital literacy 16 and access to more advanced technologies such as broadband and newer devices. Advances in health care technology could potentially facilitate health equity by increasing access to care. 17 However, factors producing unequal use and implementation of technology may in fact exacerbate social inequalities in health. 18 Understanding differences in utilization of telemedicine across demographic groups will ensure that further adoption of telemedicine does not inadvertently create or widen disparities. Furthermore, understanding factors associated with lower telemedicine utilization can support the allocation of resources and outreach to communities facing these barriers.
Wisconsin is uniquely suited for analyses of health disparities in telemedicine. First, it has both densely populated urban areas and large swaths of rural land. By U.S. census definitions, 30% of Wisconsinites live in rural areas. 19 Wisconsin has also experienced growing income inequality in recent years. 2 Finally, though over 90% of the population is White, most racial and ethnic groups are represented, including the American Indian Nations and tribal communities of Wisconsin. 19
Previous studies presented changes in the scale and applications of telemedicine use during the first wave of the pandemic, which occurred around March to May of 2020, 20 21 22 23 24 25 as well as the utility of telemedicine in treating cases of suspected COVID-19. 24 26 27 Few studies thus far have examined telemedicine utilization patterns after May 2020, as outpatient telemedicine delivery grew more widespread. Existing work has also demonstrated connections between decreased telemedicine use and older age, non-White race, and non-English language preference. 8 Some have highlighted disparities in health care and technology infrastructure in rural populations likely to place them risk for decreased telemedicine adoption. 11 Thus, we chose to include these variables in our analysis, as well as those likely to influence or confound their effects, including health care payer and area-level disadvantage.
Objectives
We examined how patient characteristics affected telemedicine utilization in 3 months following a governor-issued stay-at-home order in effect March to late April 2020. We identified two subgroups for particular attention: a rural subgroup and a subgroup at the greatest risk of disadvantage based on Area Deprivation Index (ADI) above the 80th percentile to further elucidate determinants of telemedicine utilization within these groups.
Methods
This study was exempted from the University of Wisconsin Institutional Review Board review. This study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guideline.
Study Design/Setting
We conducted a retrospective, observational study within UW Health, the integrated health system of University of Wisconsin-Madison. UW Health serves over 600,000 patients yearly throughout Wisconsin and neighboring states in the Upper Midwest and includes a tertiary referral center among its seven hospitals and over 80 outpatient sites. The UW Health electronic health record (EHR) vendor was Epic (Epic Systems; Verona, Wisconsin, United States).
Our center such as the nation at large was compelled to expand its telemedicine program rapidly: the distribution of provider visits moved from nearly 100% in-person pre-pandemic to 72% telemedicine visits in May 2020. This mirrors similar swift transitions in health systems across the United States. 28 Prior to the pandemic, an infrastructure existed for outpatient telemedicine only for highly specific use cases, such as providing care for incarcerated persons. UW Health expanded its telemedicine program to all clinical specialties and locations, including both video visits (audio and visual capabilities) and telephone visits (audio-only), by mid-May 2020. Further information regarding technologic requirements, telemedicine vendor, and telemedicine workflows at our center are detailed in Appendix A . Patient portal activation was not required to conduct a video visit.
Participants
We examined outpatient visits between June 1, 2020 and August 31, 2020. This date range encompasses a period shortly after the statewide stay-at-home order ended, and UW Health resumed most standard services. 29 Patients were included in the analysis if they completed at least one outpatient visit (video, audio or in-person) during the study period. UW Health's EHR was queried for all encounters meeting the criteria specified, and all unique patients were identified and included in the study population.
Data Source and Variables
For patients meeting criteria, baseline characteristics and demographics were extracted from the UW Health instance of Epic's Clarity and Caboodle databases.
Independent Variables
These included age, sex, race, ethnicity, preferred language, and marital status. Patient portal activation status, payer category, and the types of visits (video, audio, or in-person) were also extracted. All values were assumed to stay constant throughout the study period and were designated as those recorded in the EHR at the time of extraction in October 2020.
Rurality was determined by using each patient's documented county and state to derive a 2013 Rural-Urban Continuum Code (RUCC) designation, with RUCC codes of 4 or greater designating nonmetropolitan, more rural counties. 30 Charlson Comorbidity Index (CCI) was calculated for each patient based on age and the presence of up to 17 comorbid conditions, based on diagnosis codes documented up to a year before the start of the study period. Higher CCI indicates higher likelihood of mortality or resource use within 10 years. 31 Area Deprivation Index (ADI), a measure of neighborhood disadvantage based on income, education, employment, and housing quality (higher values correspond to increased disadvantage) was determined by using each patient's 9-digit zip code, when available, or else geocoded address. 32
Groupings for race and preferred language were chosen based on the most frequent categories of these variables. Patients were dichotomized into urban (RUCC codes = 1–3) and rural (RUCC codes = 4–9). CCI was treated as a continuous variable. ADI was stratified by quintile. Patient payer was classified based on broader categories of health care coverage common in the United States according to the following scheme: local HMO/commercial, fee-for-service/commercial, Medicare, Medicaid, or self-pay/none.
Outcomes
For each patient, the highest level of technology used in an encounter was determined ( Fig. 1 ). The “video visit” group consisted of patients who had at least one video-based telemedicine encounter. Similarly, the “audio visit” group consisted of patients who had an audio visit, but no video visits. The remainder of patients had only in-person visits and were designated the “in-person” group. Our primary outcome measure was whether each patient had at least one video visit compared with audio or in-person visits only. Our secondary outcome measure was whether the patient had any telemedicine visit (either a video or audio visit) compared with in-person visits only.
Fig. 1.
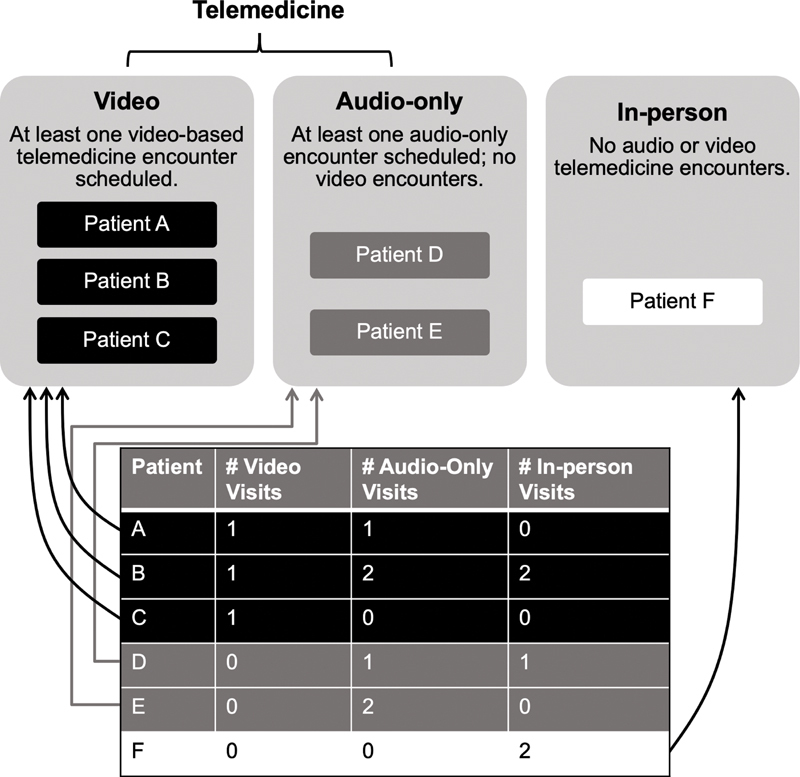
Patients were assigned to video, audio-only, and in-person groups based on the highest level of technology used for an outpatient visit. The telemedicine group comprises the video and audio-only groups combined.
Statistical Analysis
Means, standard deviations, and proportions were calculated for continuous and categorical variables ( Table 1 ). The Chi-square test and one-way ANOVA were used to assess risk factors associated with rural versus urban status, as well as for the highest level of technology used. A q-value ( p -value adj ) corrected for false discovery rate of 0.05 using the Storey method was considered statistically significant. 33 We assessed the relationship between the likelihood of having at least one video visit (video vs. audio or in-person) and at least one telemedicine visit (video or audio vs. in-person) with each of the input variables using a multivariable logistic regression model. Select two-way interactions terms between these variables were also included in the model. Data analysis was done with the R statistical software version R 4.0.1. (R Foundation for Statistical Computing, Vienna, Austria).
Table 1. Characteristics of study population.
| Persons, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Visit group | Rurality | |||||||
| Telemedicine | ||||||||
| Characteristic | Total 19,7076 b | Video 46,751 b |
Audio 35,605 b |
In-person 114,720 b |
p -Value adj | Urban 163,616 b |
Rural 33,460 b |
p -Value adj |
| Age, mean (SD) a | 46 (24) | 42 (22) | 55 (21) | 44 (25) | <0.001 | 45 (24) | 51 (24) | <0.001 |
| Sex c | <0.001 | <0.001 | ||||||
| Female | 110,360 (56) | 27,594 (59) | 20,157 (57) | 62,609 (55) | 92,297 (56) | 18,063 (54) | ||
| Race d | <0.001 | <0.001 | ||||||
| White | 175,400 (91) | 41,840 (91) | 32,032 (92) | 101,528 (91) | 143,641 (90) | 31,759 (97) | ||
| Black/African American | 9,979 (5.2) | 2,119 (4.6) | 1,904 (5.4) | 5,956 (5.3) | 9,589 (6.0) | 390 (1.2) | ||
| Asian | 5,707 (3.0) | 1,396 (3.1) | 714 (2.0) | 3,597 (3.2) | 5,546 (3.5) | 161 (0.5) | ||
| American Indian or Alaska Native | 1,435 (0.7) | 318 (0.7) | 281 (0.8) | 836 (0.7) | 1,191 (0.7) | 244 (0.7) | ||
| Native Hawaiian or other Pacific Islander | 351 (0.2) | 93 (0.2) | 47 (0.1) | 211 (0.2) | 313 (0.2) | 38 (0.1) | ||
| Ethnicity e | <0.001 | <0.001 | ||||||
| Hispanic/Latino | 8,792 (4.5) | 1,854 (4.0) | 1,335 (3.8) | 5,603 (5.0) | 7,851 (4.9) | 941 (2.9) | ||
| Not Hispanic/Latino | 18,552 (94) | 44,187 (95) | 33,865 (95) | 5,603 (4.9) | ||||
| RUCC | <0.001 | |||||||
| Urban | 163,616 (83) | 40,903 (87) | 28,070 (79) | 94,643 (82) | ||||
| Rural | 33,460 (17) | 5,848 (13) | 7,535 (21) | 20,077 (18) | ||||
| Language | <0.001 | <0.001 | ||||||
| English | 193,102 (98) | 46,246 (99) | 34,852 (98) | 112,004 (98) | 159,992 (98) | 33,110 (99) | ||
| Spanish | 2,559 (1.3) | 268 (0.6) | 498 (1.4) | 1,793 (1.6) | 2,318 (1.4) | 241 (0.7) | ||
| Other | 1,074 (0.5) | 204 (0.4) | 170 (0.5) | 700 (0.6) | 997 (0.6) | 77 (0.2) | ||
| Hmong | 208 (0.1) | 17 (<0.1) | 64 (0.2) | 127 (0.1) | 200 (0.1) | 8 (<0.1) | ||
| American sign language | 133 (<0.1) | 16 (<0.1) | 21 (<0.1) | 96 (<0.1) | 109 (<0.1) | 24 (<0.1) | ||
| Patient portal activation f | 140,007 (71) | 39,174 (84) | 23,500 (66) | 77,333 (68) | <0.001 | 122,045 (75) | 17,962 (54) | <0.001 |
| CCI, Mean (SD) a | 76 (34) | 80 (31) | 61 (40) | 79 (32) | <0.001 | 78 (33) | 67 (37) | <0.001 |
| ADI quintile | <0.001 | <0.001 | ||||||
| 1 | 35,730 (18) | 9,918 (22) | 5,161 (15) | 20,651 (18) | 35,578 (22) | 152 (0.5) | ||
| 2 | 79,641 (41) | 19,539 (42) | 13,643 (39) | 46,459 (41) | 73,020 (45) | 6,621 (20) | ||
| 3 | 52,726 (27) | 11,478 (25) | 10,632 (30) | 30,616 (27) | 36,804 (23) | 15,922 (48) | ||
| 4 | 20,150 (10) | 3,822 (8.3) | 4,453 (13) | 11,875 (11) | 11,095 (6.9) | 9,055 (28) | ||
| 5 | 5,828 (3.0) | 1,235 (2.7) | 1,192 (3.4) | 3,401 (3.0) | 4,746 (2.9) | 1,082 (3.3) | ||
| Payer g | <0.001 | <0.001 | ||||||
| Local HMO/commercial | 70,950 (36) | 20,340 (44) | 9,562 (27) | 41,048 (36) | 64,826 (40) | 6,124 (18) | ||
| Medicare | 52,584 (27) | 8,850 (19) | 14,800 (42) | 28,934 (25) | 39,852 (24) | 12,732 (38) | ||
| Fee-for-service/ commercial | 49,531 (25) | 12,340 (26) | 6,975 (20) | 30,216 (26) | 39,634 (24) | 9,897 (30) | ||
| Medicaid | 17,928 (9.1) | 4,076 (8.7) | 3,275 (9.2) | 10,577 (9.2) | 14,246 (8.7) | 3,682 (11) | ||
| Self-pay/none | 6,010 (3.1) | 1,136 (2.4) | 968 (2.7) | 3,906 (3.4) | 4,990 (3.1) | 1,020 (3.0) | ||
| Visit | <0.001 | |||||||
| In-person | 114,720 (58) | 94,643 (58) | 20,077 (60) | |||||
| Video | 46,751 (24) | 40,903 (25) | 5,848 (17) | |||||
| Audio | 35,605 (18) | 28,070 (17) | 7,535 (23) | |||||
Abbreviations: ADI, Area Deprivation Index; CCI, Charlson Comorbidity Index; HMO, Health Maintenance Organization; RUCC, rural-urban continuum code; y, years.
Age and CCI were continuous variables; the remainder were treated as categorical variables.
Statistical tests performed: one-way ANOVA; Chi-square test of independence.
Study population includes a small number (<10) of nonbinary individuals.
Race was unavailable for 4,240 (2.1%).
Ethnicity was unavailable for 2,757 (1.5%).
Patient portal activation status was unknown for 452 (0.2%).
Payer was unspecified for 73 (<0.1%).
We planned two subgroup analyses: (1) the subgroup of patients with rural status and (2) the subgroup of patients above the 80th percentile for ADI (corresponding to the most disadvantaged group) to determine drivers of telemedicine access within this population. Based on literature, we hypothesized that White race, lower corresponding to lower comorbidity (CCI), younger age, patient portal activation, and urban status would be associated with a higher likelihood of completing a video visit, while older, rural patients living in areas of disadvantage (higher ADI) would be likelier to utilize audio or in-person visits.
Results
Demographics
A total of 197,076 unique individuals (504,464 visits) were eligible for inclusion in the analysis. Table 1 displays patient characteristics. However, 96% of patient-level records had no fields missing, and all were included in the analysis. The proportion of established patients (having any previous encounter within 3 years of the study period start) were similar at 97.5, 94.9, and 98.5% for the video, audio, and in-person groups, respectively. During the study period, cumulative confirmed COVID-19 cases rose from 18,543 to 75,603, and a more rapid “surge” occurred a month afterward.
Differences in sex, race, ethnicity, ADI, and payer between the three groups were statistically significant, but small. The audio visit group was on average over a decade older than either the video or in-person groups. Patients with video visits more frequently had their EHR patient portal activated (84%) compared with audio (66%) or in-person only (68%; p < 0.001). Overall comorbidity status differed between groups, reflected in a mean (SD) CCI of 80 (31), 61 (40), and 79 (32) ( p < 0.001) for video, audio, and in-person groups, respectively, indicating that the audio group had the lowest 10-year mortality risk overall. Finally, payer type differed among the three groups. Only 19% of the video group had Medicare listed as payer, compared with 42% of the audio group and 25% of the in-person group.
Rural patients were older (51 [24] vs. 45 [24], p < 0.001) and less likely to have activated their patient portal (54 vs. 75%, p < 0.001). Differences existed between urban and rural patients in ADI distribution–a larger proportion of rural patients lived in neighborhoods of greater disadvantage. Rural patients were less likely to have local HMO/commercial listed as payer and more likely to have Medicare. Rural patients comprised 17% of total visits, 15% of video visits, 21% of audio visits, and 18% of in-person visits ( p < 0.001). Utilization of telemedicine type differed, with rural patients less likely than urban patients to use video (17 vs. 25%, p < 0.001) and more likely to use audio (23 vs. 17%, p < 0.001).
Logistic Regression Analyses
In all logistic regression models, ADI and RUCC were highly correlated; thus, ADI was not added to the model.
Video Visits versus Audio or In-Person Visits
Older patients were less likely to have a video visit compared with an audio or in-person visit ( Table 2 ; Fig. 2 ). Other factors associated with lower likelihood of having a video visit were self-pay/uninsured status, rural RUCC, Spanish language, Hispanic/Latino ethnicity, Black/African American or Asian race, and increasing CCI. Variables positively associated with having a video visit were Medicaid or Medicare as payer, patient portal activation, and American Indian/Alaskan Native race. The interaction of increasing age with Asian race, Black/African American race, and Hispanic/Latino ethnicity were each positively associated with a video visit, while the latter three variables individually were negatively associated. Other significant interaction terms are shown in Table 2 and Fig. 2 .
Table 2. Logistic regression for video versus audio or in-person visits.
| Characteristic a | Log odds | 95% CI | p -Value adj | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | −0.005 | −0.006 | −0.004 | 0.000 |
| Fee-for-Service/commercial | −0.006 | −0.061 | 0.048 | 0.822 |
| Medicaid | 0.126 | 0.050 | 0.202 | 0.001 |
| Medicare | 1.223 | 1.077 | 1.370 | 0.000 |
| Self-pay/none | −0.199 | −0.352 | −0.046 | 0.011 |
| American Indian/Alaska Native | 0.343 | 0.060 | 0.626 | 0.017 |
| Asian | −0.442 | −0.561 | −0.324 | 0.000 |
| Black/African American | −0.446 | −0.550 | −0.342 | 0.000 |
| Hispanic/Latino | −0.240 | −0.348 | −0.132 | 0.000 |
| Rural | −0.253 | −0.285 | −0.222 | 0.000 |
| Patient portal activation | 0.854 | 0.825 | 0.882 | 0.000 |
| CCI | −0.002 | −0.003 | −0.002 | 0.000 |
| American sign language | 0.382 | −0.568 | 1.331 | 0.431 |
| Hmong | 0.241 | −0.841 | 1.323 | 0.663 |
| Language, other | 0.439 | 0.133 | 0.745 | 0.005 |
| Spanish | −0.314 | −0.569 | −0.059 | 0.016 |
| Age: Fee-for-service/commercial | −0.002 | −0.003 | 0.000 | 0.011 |
| Age: Medicaid | −0.004 | −0.006 | −0.001 | 0.001 |
| Age: Medicare | −0.024 | −0.026 | −0.021 | 0.000 |
| Age: Self-Pay/None | 0.000 | −0.003 | 0.004 | 0.894 |
| Age: American Sign Language | −0.033 | −0.058 | −0.007 | 0.012 |
| Age: Hmong | −0.027 | −0.049 | −0.005 | 0.015 |
| Age: Language - Other | −0.015 | −0.022 | −0.008 | 0.000 |
| Age: Spanish | −0.012 | −0.018 | −0.005 | 0.000 |
| Age: American Indian/Alaska Native | −0.008 | −0.014 | −0.001 | 0.024 |
| Age: Asian | 0.010 | 0.007 | 0.013 | 0.000 |
| Age: Black/African American | 0.009 | 0.007 | 0.011 | 0.000 |
| Age: Hispanic/Latino | 0.007 | 0.005 | 0.010 | 0.000 |
Abbreviations: CI, confidence interval; CCI, Charlson Comorbidity Index.
The references classes used were: White (race), not Hispanic (ethnicity), no patient portal activation (patient portal activation status), and urban (rural vs. urban).
Note: Interaction terms are represented by a colon (“:”) between terms; for example, “age: fee-for-service/commercial.”
Fig. 2.
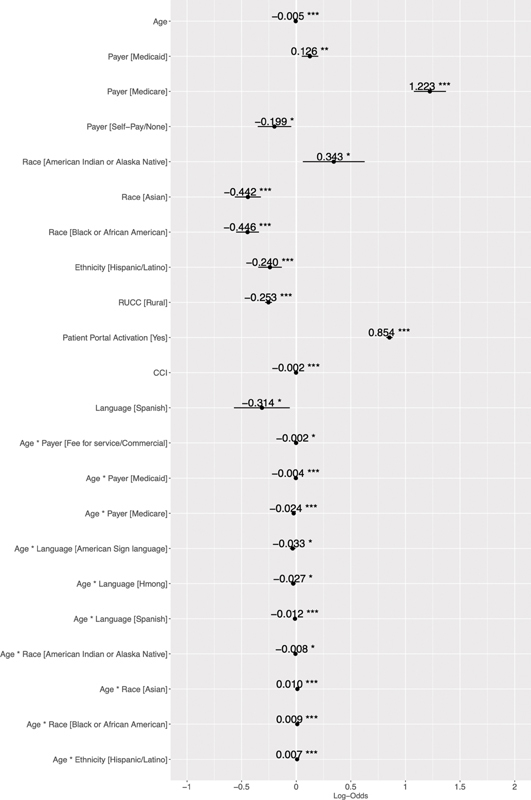
The forest plot presents a visualization of the results (logistic regression results for video versus audio or in-person visits). Variables to the right are positively associated with the outcome, and values to the left are negatively associated. The bar represents the 95% confidence interval. Only statistically significant variables are shown in the forest plot; * p < 0.001, ** p < 0.01, *** p < 0.05. CCI, Charlson Comorbidity Index.
Telemedicine versus In-person Visits
For the telemedicine (video or audio vs. in-person) outcome, rural RUCC, self-pay/uninsured status, Hispanic/Latino ethnicity, Black/African American or Asian race and increasing CCI were negatively associated with having any telemedicine visit ( Table 3 ; Fig. 3 ). Increasing age, Medicaid or Medicare as payer, and patient portal activation were positively associated. Once again, the interaction of increasing age with Asian race, Black/African American race, and Hispanic/Latino ethnicity were each positively associated with a telemedicine visit, while the latter three variables individually were negatively associated. Other significant interaction terms are shown in Table 3 and Fig. 3 .
Table 3. Logistic regression for video or audio versus in-person visits.
| Characteristic a | Log odds | 95% CI | p -Value adj | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 0.003 | 0.002 | 0.003 | 0.000 |
| Fee-for-service/commercial | −0.029 | −0.079 | 0.021 | 0.257 |
| Medicaid | 0.110 | 0.043 | 0.177 | 0.001 |
| Medicare | 1.768 | 1.646 | 1.891 | 0.000 |
| Self-pay/none | −0.071 | −0.199 | 0.057 | 0.276 |
| American Indian or Alaska Native | 0.214 | −0.028 | 0.457 | 0.083 |
| Asian | −0.378 | −0.482 | −0.273 | 0.000 |
| Black/African American | −0.375 | −0.463 | −0.286 | 0.000 |
| Native Hawaiian/Other Pacific Islander | 0.196 | −0.237 | 0.629 | 0.375 |
| Hispanic/Latino | −0.268 | −0.357 | −0.180 | 0.000 |
| Rural | −0.078 | −0.104 | −0.053 | 0.000 |
| Patient portal activation | 0.450 | 0.428 | 0.472 | 0.000 |
| CCI | −0.009 | −0.009 | −0.008 | 0.000 |
| Age: Fee-for-Service/Commercial | −0.001 | −0.002 | 0.000 | 0.032 |
| Age: Medicaid | 0.003 | 0.001 | 0.005 | 0.001 |
| Age: Medicare | −0.029 | −0.031 | −0.027 | 0.000 |
| Age: Self-Pay/None | −0.003 | −0.006 | 0.000 | 0.023 |
| Age: American Indian or Alaska Native | −0.004 | −0.009 | 0.002 | 0.178 |
| Age: Asian | 0.006 | 0.003 | 0.008 | 0.000 |
| Age: Black/African American | 0.009 | 0.007 | 0.011 | 0.000 |
| Age: Native Hawaiian or Other Pacific Islander | −0.004 | −0.015 | 0.006 | 0.389 |
| Age: Hispanic/Latino | 0.005 | 0.003 | 0.007 | 0.000 |
Abbreviations: CI, confidence interval; CCI, Charlson Comorbidity Index.
The references classes used were: White (race), not Hispanic (ethnicity), no patient portal activation (patient portal activation status), and urban (rural vs. urban).
Note: Interaction terms are represented by a colon (“:”) between terms; for example, “age: fee-for-service/commercial.”
Fig. 3.
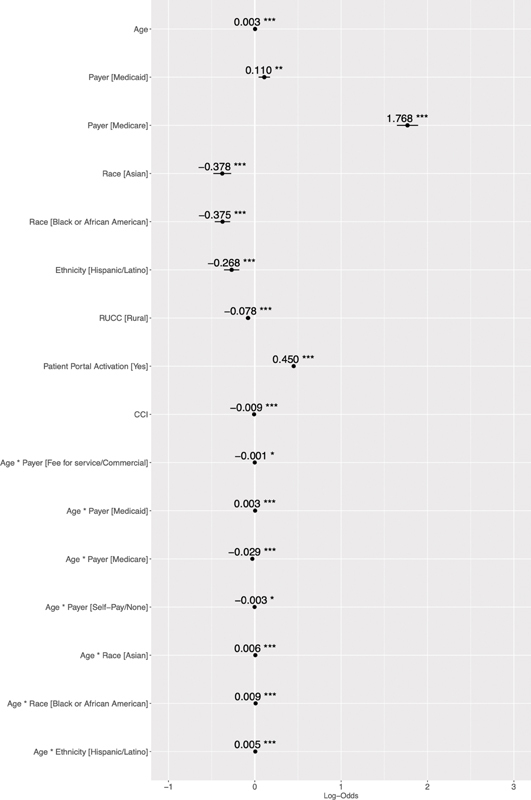
The forest plot presents a visualization of the results (logistic regression results for video or audio versus in-person visits). Variables to the right are positively associated with the outcome, and values to the left are negatively associated. The bar represents the 95% confidence interval. Only statistically significant variables are shown in the forest plot; * p < 0.001, ** p < 0.01, *** p < 0.05. CCI, Charlson Comorbidity Index.
Rural Subgroup Analysis
In the subgroup of patients with rural residence based on RUCC codes (4–9), increasing age and CCI, and Hispanic/Latino ethnicity were negatively associated with having a video visit, while Medicare as payer and patient portal activation were positively associated ( Table 4A ). In this population, Black/African American race, Hispanic/Latino ethnicity, and increasing CCI were negatively associated with having any telemedicine visit, while Medicare payer, American Indian/Alaskan Native or Asian race, and patient portal activation were positively associated ( Table 4B ). Significant interaction terms are also shown in Table 4 .
Table 4. Subgroup analysis (rural population).
| Logistic regression for video vs. audio or in-person visits | ||||
|---|---|---|---|---|
| Characteristic a | Log odds | 95% CI | p -Value adj | |
| Lower | Upper | |||
| Age | −0.017 | −0.021 | −0.014 | 0.000 |
| Fee-for-Service/commercial | 0.085 | −0.079 | 0.249 | 0.311 |
| Medicaid | 0.167 | −0.023 | 0.358 | 0.086 |
| Medicare | 1.082 | 0.726 | 1.437 | 0.000 |
| Self-pay/none | −0.411 | −0.848 | 0.026 | 0.065 |
| Hispanic/Latino | −0.548 | −0.854 | −0.242 | 0.000 |
| Patient Portal Activation | 0.612 | 0.481 | 0.742 | 0.000 |
| CCI | −0.003 | −0.004 | −0.001 | 0.000 |
| Age: Fee-for-service/commercial | −0.005 | −0.008 | −0.001 | 0.019 |
| Age: Medicaid | −0.003 | −0.008 | 0.002 | 0.225 |
| Age: Medicare | −0.023 | −0.029 | −0.017 | 0.000 |
| Age: Self-pay/none | 0.001 | −0.008 | 0.010 | 0.806 |
| Age: Patient portal activation | 0.007 | 0.004 | 0.010 | 0.000 |
| Age: Hispanic/Latino | 0.011 | 0.003 | 0.019 | 0.009 |
| Logistic regression for video or audio vs. in-person visits | ||||
| Characteristic a | Log odds | 95% CI | p -Value adj | |
| Lower | Upper | |||
| Age | −0.001 | −0.003 | 0.002 | 0.662 |
| Fee-for-service/commercial | 0.087 | −0.060 | 0.234 | 0.248 |
| Medicaid | 0.283 | 0.115 | 0.450 | 0.001 |
| Medicare | 1.601 | 1.336 | 1.865 | 0.000 |
| Self-pay/none | −0.141 | −0.485 | 0.202 | 0.420 |
| American Indian or Alaska Native | 0.307 | 0.048 | 0.566 | 0.020 |
| Asian | 0.315 | 0.000 | 0.630 | 0.050 |
| Black/African American | −0.060 | −0.271 | 0.150 | 0.575 |
| Native Hawaiian/Other Pacific Islander | 0.257 | −0.399 | 0.912 | 0.443 |
| Hispanic/Latino | −0.637 | −0.896 | −0.378 | 0.000 |
| Patient portal activation | 0.429 | 0.382 | 0.476 | 0.000 |
| CCI | −0.009 | −0.010 | −0.008 | 0.000 |
| Age: Medicaid | −0.002 | −0.006 | 0.002 | 0.309 |
| Age: Medicare | −0.027 | −0.031 | −0.023 | 0.000 |
| Age: Self-pay/none | −0.004 | −0.011 | 0.003 | 0.223 |
| Age: Hispanic/Latino | 0.010 | 0.004 | 0.016 | 0.001 |
Abbreviations: CI, confidence interval; CCI, Charlson Comorbidity Index.
Note: Interaction terms are represented by a colon (“:”) between terms; for example, “age: fee-for-service/commercial.”
The references classes used were: White (race), not Hispanic (ethnicity), no patient portal activation (patient portal activation status), and urban(rural vs. urban).
Most Disadvantaged Subgroup Analysis
In the subgroup of patients in the highest quintile of ADI, increasing age, Medicaid payer, and increasing CCI were negatively associated with having a video visit, while Medicare payer and patient portal activation were positively associated ( Table 5A ). Increasing CCI was negatively associated with a telemedicine visit, while Medicare as payer and patient portal activation were positively associated ( Table 5B ). Significant interaction terms are also shown in Table 5 .
Table 5. Subgroup analysis of most disadvantaged (Area Deprivation Index > 80th percentile).
| Logistic regression for video vs. audio or in-person visits | ||||
|---|---|---|---|---|
| Characteristic a | Log odds | 95% CI | p -Value adj | |
| Lower | Upper | |||
| Age | −0.024 | −0.033 | −0.014 | 0.000 |
| Fee-for-service/commercial | −0.008 | −0.409 | 0.393 | 0.969 |
| Medicaid | −0.561 | −0.974 | −0.149 | 0.008 |
| Medicare | 1.027 | 0.286 | 1.768 | 0.007 |
| Self-pay/none | −0.263 | −0.950 | 0.424 | 0.453 |
| Patient portal activation | 0.454 | 0.170 | 0.737 | 0.002 |
| CCI | −0.003 | −0.006 | −0.001 | 0.018 |
| Age: Fee-for-service/commercial | −0.005 | −0.015 | 0.006 | 0.364 |
| Age: Medicaid | 0.007 | −0.005 | 0.018 | 0.240 |
| Age: Medicare | −0.021 | −0.034 | −0.008 | 0.002 |
| Age: Self-pay/none | 0.000 | −0.017 | 0.017 | 0.983 |
| Age: Patient portal activation | 0.011 | 0.004 | 0.018 | 0.001 |
| Logistic regression for video or audio vs. in-person visits | ||||
| Characteristic a | Log odds | 95% CI | p -Value adj | |
| Lower | Upper | |||
| Age | −0.005 | −0.012 | 0.002 | 0.160 |
| Fee-for-service/commercial | −0.105 | −0.468 | 0.259 | 0.572 |
| Medicaid | −0.350 | −0.707 | 0.007 | 0.054 |
| Medicare | 1.613 | 0.998 | 2.228 | 0.000 |
| Self-pay/none | −0.030 | −0.605 | 0.544 | 0.918 |
| Patient portal activation | 0.518 | 0.405 | 0.631 | 0.000 |
| CCI | −0.009 | −0.011 | −0.007 | 0.000 |
| Age: Fee-for-service/commercial | −0.001 | −0.010 | 0.008 | 0.880 |
| Age: Medicaid | 0.012 | 0.002 | 0.021 | 0.013 |
| Age: Medicare | −0.025 | −0.036 | −0.015 | 0.000 |
| Age: Self-pay/none | −0.006 | −0.019 | 0.007 | 0.358 |
Abbreviations: CI, confidence interval; CCI, Charlson Comorbidity Index.
Note: Interaction terms are represented by a colon (“:”) between terms; for example, “age: fee-for-service/commercial.”
The references classes used were: White (race), not Hispanic (ethnicity), no patient portal activation (patient portal activation status), and urban (rural vs. urban).
Discussion
Rural, uninsured individuals of Asian and Black/African American race, and Hispanic/Latino ethnicity were all significantly less likely to have a video visit and to use telemedicine in general. The effects of Black/African American race and Hispanic/Latino ethnicity persisted within the rural subgroup. Increasing comorbidity (as measured by CCI) was negatively associated with having a video visit or any telemedicine visit; however, the effect of CCI was small. Patients with fewer comorbidities may more frequently have elected to utilize audio-only visits, as their queries might be addressed easily using an audio-only format.
Older age was positively associated with overall telemedicine use, but negatively associated with use of video visits. Older patients may have preferred to avoid the risks of in-person visits but struggled with digital literacy or technology access. We found somewhat surprisingly that Medicare payer type was positively associated with video telemedicine use, in spite of the negative association with age. A post hoc subgroup analysis of the Medicare patients redemonstrated a negative association between age and video telemedicine use (log odds = 0.023, 95% confidence interval: 0.028–0.018, p < 0.001). In addition, the interaction between age and Medicare payer type has a significant negative association with video telemedicine use. Thus, the negative association between age and video telemedicine use persists regardless of Medicare payer type.
Patient portal activation, which we believe to be a fair indicator of digital literacy and technology access (itself likely linked to the demographic factors we examined), was positively associated with both video visits and telemedicine in general. There was a significant positive association between American Indian or Alaska Native race and video use. Of note, the Indian Health Service—an early adopter of telemedicine technology—has sought to improve Native American health care access through remote technology since the 1970s, with significant improvements to multiple Native American health outcomes, which may relate to our findings. 34
Taken together, our findings reinforce previous data demonstrating older age, lower socioeconomic status (as evidenced by uninsured status in this analysis), certain non-English language speakers, and people of color may have decreased access to telemedicine. 8 21 In particular, we replicated the finding that Black/African American race, Asian race, and Hispanic/Latino ethnicity were independently associated with lower telemedicine use. However, the interaction terms between increasing age and Asian or Black/African American race and Hispanic/Latino ethnicity were positively associated both with having a video visit and using telemedicine in general, suggesting older patients within these racial and ethnic groups were more likely to utilize telemedicine, and that this racial divide primarily existed among younger individuals. This is an unexpected pattern that warrants further investigation.
Black, Hispanic and Asian people have higher rates of infection, hospitalization, and death from COVID-19 compared with White people. 35 A cohort study of 11,210 hospitalized COVID-19 adults showed no difference in all-cause or in-hospital mortality between Black and White patients after adjusting for age, sex, insurance status, comorbidity, neighborhood deprivation, and site of care, 36 suggesting that the disproportionate harms caused to people of color are tied to these other factors, and that with equal access to equal care, the mortality differences might be expected to narrow as well. This further warrants the need for interventions to improve health equity for these communities, including equitable telemedicine access.
In addition, our data are consistent with a pattern of greater area-level disadvantage in the rural patient population (demonstrated by a disproportionate number of rural patients in higher quintiles of ADI), and lower digital literacy (suggested by decreased rates of patient portal activation compared with urban counterparts). Both would exacerbate the negative association demonstrated between rural residence and video telemedicine use. However, these factors do not explain why audio-only visits were not more commonly utilized. In this regard, differing sentiments regarding the necessity of social isolation (and hence telemedicine) might play a role. The negative effect of CCI may be partially attributable to the use of age in CCI calculation, but the additional negative effect of CCI on both video and audio visits suggests that the presence of more comorbidities may necessitate in-person visits in certain cases, even though increasing comorbidities would also make patients more vulnerable to COVID-19 complications.
Our analysis was not without limitations. This was a retrospective cross-sectional study capturing data over a limited time period. Our outcome measures were based on whether a patient was scheduled for a video, audio, or in-person visit, but not whether the visit proceeded using the scheduled modality (although patients were eligible only if they completed at least one visit of any kind). During our study period, the EHR did not have a system in place to reflect changes to the planned visit modality. We also cannot assess when patient characteristics might be modified by the presence of a caregiver (e.g., an older patient assisted by his or her adult child), or what effect implicit biases may have in offering a telemedicine visit to any given patient (e.g., a clinic might assume that an older, rural patient would be unlikely to accept a telemedicine visit and not offer one). Disease factors also undoubtedly play a role; for instance, a urologic or gynecologic complaint might necessitate an in-person exam. Finally, this was a single-center study, although it encompassed a large geographical area in which most demographics were represented.
Future areas of study should focus on refining analysis by subspecialty services and delving further into utilization patterns. For instance, a patient with one video visit and five in-person visits likely represents a distinct clinical scenario from a patient with one video visit and no in-person visits over the same time period, though their outcomes in this analysis would be equivalent. Additional studies quantifying effects on health outcomes and costs as a result of widespread implementation of telemedicine also will be informative, as remote encounters for outpatient care provision may become more common, and payers will make decisions about payment parity between video, audio, and in-person visits.
Conclusion
The COVID-19 pandemic created a strong impetus for the expansion of telemedicine infrastructure in most health care systems nationwide. Policymakers and health care administrators should be aware of the potential for disparities in access to telemedicine based on age, technologic literacy, rural status, socioeconomic disadvantage, race/ethnicity, and preferred language. Barriers to telemedicine access should be mitigated where possible, by identifying patient groups at risk, and ensuring the availability of video and audio language interpreters to reduce barriers arising due to language. Provisions for the rural community should include widely available broadband internet and devices compatible with video-based telemedicine. 37 As researchers outline best practices for telehealth delivery, health systems, payers, and policy makers should share responsibility for ensuring that telehealth is utilized costeffectively as an alternative to in-person visits, with appropriate patient incentives. For example, the Wisconsin legislature recently passed an act which requires health insurance policies to cover telehealth services without a greater deductible, copayment, or coinsurance. Policy makers should also invest in broadband access to improve access to both telehealth and the digital means to overcome other social determinants of health. Finally, appropriate community outreach and education should take place to ensure digital literacy and equitable telemedicine access.
Clinical Relevance Statement
Telemedicine offers a safe and effective means of health care delivery during a pandemic, but disparities may arise based on age, digital literacy, rural versus urban status, and race/ethnicity. Thus, health systems and policies should seek to mitigate barriers to telemedicine when possible.
Multiple Choice Questions
-
Which racial and ethnic groups were associated with lower use of video visits and telemedicine in general?
White race only.
Black race only.
Black race and Hispanic/Latino ethnicity only.
Black race, Asian race, and Hispanic/Latino ethnicity.
Correct Answer: The correct answer is option d. Our analysis replicates recent findings that Black race, Asian race, and Hispanic/Latino ethnicity are associated with lower use of video visits and telemedicine in general.
-
What are some possible barriers to video telemedicine adoption experienced by rural patients?
Decreased access to fast broadband connections.
Higher levels of digital and technologic literacy.
Cultural beliefs, but no other barriers are likely to exist.
Lower levels of comorbidity as measured by the Charlson Comorbidity Index.
Correct Answer: The correct answer is option is a. Rural patients disproportionately lack access to broadband speed benchmarks set by the Federal Communications Commission compared with urban counterparts (38 vs. 4%), which could pose a challenge to completing video telemedicine visits.
-
How can barriers to telemedicine access be mitigated by policymakers and hospital administrators?
Assuming disparities in telemedicine access will resolve over time on their own.
Community outreach and education for urban populations only.
Ensuring availability of video and audio language interpreters to reduce barriers arising due to language.
Upgrading platforms and technologic requirements for telemedicine use without ensuring compatible devices and Internet infrastructure are widely available.
Correct Answer: The correct answer is option c. We found that Spanish language was associated with a lower likelihood of having a video visit. Ensuring ease of access to interpreters could improve telemedicine access for non-English speakers.
Acknowledgments
The authors would like to thank Sang Thao, MPH, for his assistance in obtaining RUCC codes for subjects in this study.
Funding Statement
Funding This work was supported by the NCI Cancer Center Support Grant P30 CA014520, grant UL1TR000427 to UW ICTR from NIH/NCATS and grant T32 DC009401 from the NIH/NIDCD.
Conflict of Interest A.J.T. – Epic Systems (family member). The other authors report no conflict of interest.
Protection of Human and Animal Subject
This study was exempted from the University of Wisconsin Institutional Review Board (IRB) review.
Appendix A.
Technologic requirements, vendor, and workflows for use of telemedicine at UW health
During the study period, UW Health utilized a HIPAA-compliant video-enabled streaming telemedicine platform (Vidyo Telehealth Video Conferencing, Vidyo, Inc., Hackensack, New Jersey, United States) for ambulatory telemedicine visits. Though Vidyo offers integrated, context-aware linkage to the major electronic health record systems, UW Health implemented Vidyo as a standalone application due to the urgent need to offer a telemedicine solution when the pandemic began.
The workflow for this system occurred as follows: patients were selected for in-person or telemedicine visits at the discretion of the provider. Patients scheduled for a telehealth visit were given both written and verbal instructions on the process and hardware/software requirements. Briefly, the requirements included a mobile device or computer with webcam, microphone, and speakers. Computers were required to use Google Chrome as the web browser. Mobile devices were required to have the VidyoConnect application installed. At least 48 hours prior to a scheduled visit, patients received an email with these requirements along with setup instructions. This email also contained the unique link with which to join the Vidyo visit virtual room. Patients without their own email address could also receive the link via text message. Patients who did not have the hardware or software requirements for a video visit were offered either telephone or in-person visits as the clinical scenario required. Further technical support was provided via UW Health schedulers, clinic staff, and the UW Health website.
References
- 1.Ryu S. Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth 2009 (global observatory for eHealth series, volume 2) Healthc Inform Res. 2012;18(02):153–155. [Google Scholar]
- 2.Wisconsin Budget Project Pulling apart 2017: focus on Wisconsin's 1%Accessed 2017 at:http://www.wisconsinbudgetproject.org/pulling-apart-2017-focus-on-wisconsins-1
- 3.Hosworth A, Ruhter J, Samson L W. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2020. Medicare Beneficiary Use of Telehealth Visits: Early Data from the Start of COVID-19 Pandemic. [Google Scholar]
- 4.Ekeland A G, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736–771. doi: 10.1016/j.ijmedinf.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med Inform Decis Mak. 2012;12(01):1. doi: 10.1186/1472-6947-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell U A, Chebli P G, Ruggiero L, Muramatsu N. The Digital divide in health-related technology use: the significance of race/ethnicity. Gerontologist. 2019;59(01):6–14. doi: 10.1093/geront/gny138. [DOI] [PubMed] [Google Scholar]
- 7.Khairat S, Haithcoat T, Liu S.Advancing health equity and access using telemedicine: a geospatial assessment J Am Med Inform Assoc 201926(8-9):796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nouri S, Khoong E C, Lyles C R, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal. 2020 doi: 10.1056/CAT.20.0123. [DOI] [Google Scholar]
- 9.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(06):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Federal Communications Commission . Washington, DC: 2016. 2016 Broadband Progress Report. [Google Scholar]
- 11.Hirko K A, Kerver J M, Ford S. Telehealth in response to the COVID-19 pandemic: implications for rural health disparities. J Am Med Inform Assoc. 2020;27(11):1816–1818. doi: 10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kind A JH, Buckingham W R. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blumenthal S J, Kagen J. MSJAMA. The effects of socioeconomic status on health in rural and urban America. JAMA. 2002;287(01):109–109. [PubMed] [Google Scholar]
- 14.Lion K C, Brown J C, Ebel B E. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr. 2015;169(12):1117–1125. doi: 10.1001/jamapediatrics.2015.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Viers B R, Lightner D J, Rivera M E. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68(04):729–735. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Manganello J, Gerstner G, Pergolino K, Graham Y, Falisi A, Strogatz D. The relationship of health literacy with use of digital technology for health information: implications for public health practice. J Public Health Manag Pract. 2017;23(04):380–387. doi: 10.1097/PHH.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 17.Pérez-Stable E J, Jean-Francois B, Aklin C F.Leveraging advances in technology to promote health equity Med Care 201957(Suppl 6 Suppl 2):S101–S103. [DOI] [PubMed] [Google Scholar]
- 18.Weiss D, Rydland H T, Øversveen E, Jensen M R, Solhaug S, Krokstad S. Innovative technologies and social inequalities in health: a scoping review of the literature. PLoS One. 2018;13(04):e0195447. doi: 10.1371/journal.pone.0195447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau . Washington, D.C.: U.S. Government Printing Office; 2012. Population and Housing Unit Counts, CPH-2–51, Wisconsin. [Google Scholar]
- 20.Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a U.S. survey of internet users from late March. J Am Med Inform Assoc. 2020 doi: 10.1093/jamia/ocaa221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eberly L A, Kallan M J, Julien H M. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640–e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hron J D, Parsons C R, Williams L A, Harper M B, Bourgeois F C. Rapid implementation of an inpatient telehealth program during the COVID-19 pandemic. Appl Clin Inform. 2020;11(03):452–459. doi: 10.1055/s-0040-1713635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ong S Y, Stump L, Zawalich M. Inpatient telehealth tools to enhance communication and decrease personal protective equipment consumption during disaster situations: a case study during the COVID-19 pandemic. Appl Clin Inform. 2020;11(05):733–741. doi: 10.1055/s-0040-1719180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon W J, Henderson D, DeSharone A. Remote patient monitoring program for hospital discharged COVID-19 patients. Appl Clin Inform. 2020;11(05):792–801. doi: 10.1055/s-0040-1721039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knighton A J, Ranade-Kharkar P, Brunisholz K D. Rapid implementation of a complex, multimodal technology response to COVID-19 at an integrated community-based health care system. Appl Clin Inform. 2020;11(05):825–838. doi: 10.1055/s-0040-1719179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chunara R, Zhao Y, Chen J. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(01):33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grange E S, Neil E J, Stoffel M. Responding to COVID-19: the UW medicine information technology services experience. Appl Clin Inform. 2020;11(02):265–275. doi: 10.1055/s-0040-1709715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehrotra A, Ray K, Brockmeyer D M, Barnett M L, Bender J A. Rapidly converting to “virtual practices”: outpatient care in the era of Covid-19. NEJM Catal. 2020 doi: 10.1056/CAT.20.0091. [DOI] [Google Scholar]
- 29.Wisconsin Department of Health Services COVID-19 (Coronavirus Disease)Accessed December 15, 2020 at:https://www.dhs.wisconsin.gov/covid-19/index.html
- 30.United States Department of Agriculture Rural-urban continuum codesAccessed 2020 at:https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- 31.Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(05):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 32.Area Deprivation IndexAccessed 2020 at:https://www.neighborhoodatlas.medicine.wisc.edu
- 33.Storey J D. False discovery rate. Int Encycloped Stat Sci. 2011;1:504–508. [Google Scholar]
- 34.Kruse C S, Bouffard S, Dougherty M, Parro J S. Telemedicine use in rural Native American communities in the era of the ACA: a systematic literature review. J Med Syst. 2016;40(06):145. doi: 10.1007/s10916-016-0503-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lopez L, III, Hart L H, III, Katz M H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(08):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 36.Yehia B R, Winegar A, Fogel R. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 US hospitals. JAMA Netw Open. 2020;3(08):e2018039–e2018039. doi: 10.1001/jamanetworkopen.2020.18039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(07):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]


