Abstract
Background/purpose
Because the anatomy and the nature of the bone tissue between the mandible and maxilla are largely different, more site-specific studies are required to improve the healing rate on medication-related osteonecrosis of the jaw (MRONJ). The present study assessed maxillary MRONJ that was treated by surgery to understand its clinical characteristics, and to identify critical factors that influenced outcomes.
Materials and methods
The medical records of 54 patients with maxillary MRONJ who underwent surgery were retrospectively reviewed. Variables related to the prognosis of MRONJ were extracted from the medical records and imaging, and were statistically analyzed. We also evaluated the concomitant maxillary sinusitis (MS) after the surgical treatment of MRONJ, based on CT evaluation and change of symptoms.
Results
The healing rate of surgery for maxillary MRONJ was 85.2%, which suggested that surgical treatment is an effective strategy for treating maxillary MRONJ. Multivariate analysis revealed that postoperative residual necrotic bone was a poor prognosticator for maxillary MRONJ. Among 10 patients who did not obtain healing of MS postoperatively, 8 patients showed an improvement.
Conclusion
Our results indicate that surgical treatment is an appropriate strategy for maxillary MRONJ and complete resection of necrotic bone (i.e., extensive surgery) is needed to obtain complete healing of maxillary MRONJ. Concomitant MS tends to be healed or improved clinically in combination with the healing of maxillary MRONJ.
Keywords: Medication-related osteonecrosis of the jaw, Maxilla, Necrotic bone, Extensive surgery, Maxillary sinusitis
Introduction
Antiresorptive agents such as bisphosphonate (BP) and denosumab (Dmab) are widely used to manage osteoporosis, skeletal-related events associated with bone metastases from malignancies, and multiple myeloma. However, medication-related osteonecrosis of the jaw (MRONJ), which is caused by the administration of those drugs, is a growing problem. This adverse event can interfere with the treatment of malignant diseases such as bone metastasis and influence the patient's quality of life. MRONJ is defined as the presence of exposed necrotic jawbone that does not resolve over 8 weeks in a patient taking antiresorptive agents and who has not had radiotherapy of the jaw.1 To date, several strategies for treating MRONJ have been reported; however, its treatment remains challenging.2,3 A previous study revealed the significance of extensive surgery, which includes the removal of surrounding sclerotic bone with sequestrum and/or osteolysis, compared to conservative surgery for the resolution of MRONJ.4 Conservative surgery is defined as the removal of only the necrotic bone (i.e., sequestrectomy) and extensive surgery is defined as removal of the necrotic and its surrounding bone which is associated with infection from sequestrum (i.e., partial maxillectomy).4 However, the anatomy and the nature of the bone tissue between the mandible and maxilla are largely different. Therefore, more site-specific studies are required to improve the healing rate on MRONJ. In cases of maxillary MRONJ, the teeth and alveolar bone are close to the maxillary sinus, especially in cases with molar lesions. Therefore, maxillary MRONJ is often accompanied with maxillary sinusitis (MS).5 Although identifying factors associated with the failed treatment of concomitant MS is important, how concomitant MS in patients with maxillary MRONJ can be treated has not been reported. In the present study, including concomitant MS evaluation, we retrospectively analyzed patients with maxillary MRONJ to clarify the clinical characteristics, to identify critical factors associated with treatment outcomes, and to determine appropriate surgical strategies for maxillary MRONJ.
Materials and methods
Patients and variables
The authors retrospectively reviewed the medical records of 54 patients with maxillary MRONJ that was treated by conservative or extensive surgery between January 2011 and July 2018 in participating hospitals. All patients were postoperatively followed up with panoramic radiography and/or computed tomography (CT) over at least 14 days. The follow-up continued at least until a complete healing was achieved. The clinical findings and the surgical procedures were reviewed. Sex, age (<75 or ≥75 years), staging of MRONJ,1 primary disease (malignancy or other; bone metabolism disorders), type of agents (BP or Dmab, used at the time of onset of maxillary MRONJ), administration period of BP and/or Dmab (<4 or ≥4 years), duration of BPs and/or Dmab holiday (≤90 or >90 days), presence of diabetes mellitus (DM), and administration of steroids were statistically analyzed for their associations with outcomes of surgery. BP deposits in the bone long after the blood concentration decreases.6 In contrast, Dmab has no binding affinity for bone matrices and, unlike BP, the antiresorptive effects of Dmab should dissipate within 6 months of drug discontinuation.1 Therefore, we included the type of agent in the analysis. Other, antibiotics were administered as needed.
Surgery and treatment outcome
The surgical wound was primarily closed or opened with or without a prosthesis. In primary closure cases, the Schneiderian mucosa was preserved and the wound was closed by using the buccal and palatal mucosa as much as possible.7 Surgical procedures were divided into three groups, based on the height of the bone resection level with regard to the height of the apex of the related tooth: below the apex, at the height of the apex, and above the apex. In the analysis, the “at the height of the apex” group data were combined with the “below the apex” group data. In addition, critical cause (e.g., tooth extraction or other), history of maxillary sinus radical operation (Caldwell-Luc operation), sequestration, sclerotic bone reaction, periosteal reaction, postoperative residual necrotic bone, and wound procedures (primary suture or open healing) were also statistically analyzed for their associations with the outcomes of surgery.
The postoperative follow-up interval of the patients was set for each case. In cases of patients just after discharge were examined per 1or 2 weeks. Then, those with a good clinical course ranged from 1 month to 3 months. Treatment outcome was defined as clinical evaluations and/or as imaging (panoramic radiograph and/or CT) assessments. The outcomes of surgery are divided into two categories: (1) complete healing, which is the resolution of all clinical symptoms, including bone exposure, and (2) not healing, which is a reduction, no change, or increased clinical stage but some symptoms are remained and/or infection is out of control.
Concomitant MS was also followed up postoperatively and clinically evaluated by using CT imaging and change of symptoms.
Statistical analysis
Associations between the variables and outcomes of surgical treatment were analyzed by using Cox proportional hazards regression analysis, followed by multivariate logistic regression analysis by using SPSS software (version 25.0; Japan IBM Co., Tokyo, Japan). Variables with confounders were excluded from the multivariate analysis models. Two-tailed p values < 0.05 were statistically significant.
Ethics
This study conformed to the tenets of the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board of each institution (reference number of our hospital: 16020827-2).
Results
The study included 17 men and 37 women, whose mean age was 73.0 years (range, 48–89 years). The median follow-up period was 37.0 ± 158.8 days (range, 14–723 days). With regards to the clinical classification of maxillary MRONJ, 1, 36, and 17 patients were classified as having Stage 1 MRONJ (i.e., no infectious symptoms), Stage 2 MRONJ (i.e., infectious symptoms), and Stage 3 MRONJ (i.e., extensive disease), respectively. The primary diseases were 26 malignancies and 28 bone metabolism disorders. The type of agent was BPs in 34 patients and Dmab in 20 patients. Twenty-three patients were medicated with BPs and/or Dmab for ≥4 years and 31 patients were medicated with those agents for <4 years. Thirty-three patients had no drug holiday or a drug holiday of <90 days, and 21 patients had a drug holidays of ≥90 days. Six patients had DM. Fourteen patients were medicated with steroids during the administration of BPs or Dmab. There were no significant anamnestic variables to relate the healing of maxillary MRONJ via univariate analysis (Table 1).
Table 1.
Univariate analysis of anamnestic variables associated with the complete healing of maxillary MRONJ.
| Variable | Category | Outcome |
Total | p-value | |
|---|---|---|---|---|---|
| Healing | Not healing | ||||
| Age (years) | <75 | 25 | 4 | 29 | 0.512 |
| ≥75 | 21 | 4 | 25 | ||
| Sex | Male | 15 | 2 | 17 | 0.437 |
| Female | 31 | 6 | 37 | ||
| Stage | 1, 2 | 34 | 3 | 37 | 0.202 |
| 3 | 12 | 5 | 17 | ||
| Primary disease | Osteoporosis | 28 | 0 | 28 | 0.067 |
| Malignancy | 18 | 8 | 26 | ||
| Type of agent | BP | 30 | 4 | 34 | 0.671 |
| Dmab | 16 | 4 | 20 | ||
| Drug administration duration | <4 years | 27 | 4 | 31 | 0.838 |
| ≥4 years | 19 | 4 | 23 | ||
| Drug holiday | No, <90 days | 28 | 5 | 33 | 0.285 |
| Yes, ≥90 days | 18 | 3 | 21 | ||
| DM | No | 42 | 6 | 48 | 0.301 |
| Yes | 4 | 2 | 6 | ||
| Steroid administration | No | 33 | 7 | 40 | 0.781 |
| Yes | 13 | 1 | 14 | ||
MRONJ, medication-related osteonecrosis of the jaw; BP, bisphosphonate; Dmab, denosumab; DM, diabetes mellitus.
With regard to clinical characteristics, critical causes were tooth extraction in 24 patients and other causes in 30 patients. The history of maxillary sinus radical operation had in 6 patients. Sequestration, sclerotic bone reaction, and periosteal reaction was detected in 12, 34, and 5 patients, respectively. The bone resection levels; below the apex, at the height of the apex, and above the apex, were 5, 6, and 43 patients, respectively. The number of patients with postoperative residual necrotic bone were 8. The number of patients who performed surgical treatment with primary suture were 49. Among 54 patients, 46 patients achieved complete healing (85.2%). Multivariate analysis with Cox proportional hazards regression analysis revealed that postoperative residual necrotic bone were poor prognosticators for the complete healing of maxillary MRONJ (Table 1, Table 2, Table 3). Its odds ratio was 0.392 and 95% confidence interval was 0.151–1.018 (Table 3).
Table 2.
Univariate analysis of clinical variables associated with the complete healing of maxillary MRONJ.
| Variable | Category | Outcome |
Total | p-value | |
|---|---|---|---|---|---|
| Healing | Not healing | ||||
| Critical cause of MRONJ | Tooth extraction | 19 | 5 | 24 | 0.386 |
| Other | 27 | 3 | 30 | ||
| History of a maxillary sinus radical operation | No | 40 | 8 | 48 | 0.144 |
| Yes | 6 | 0 | 6 | ||
| Sequestration | No | 34 | 8 | 42 | 0.396 |
| Yes | 12 | 0 | 12 | ||
| Sclerotic reaction | No | 19 | 1 | 20 | 0.052 |
| Yes | 27 | 7 | 34 | ||
| Periosteal reaction | No | 43 | 6 | 49 | 0.192 |
| Yes | 3 | 2 | 5 | ||
| Bone resection level | Under the apex | 9 | 2 | 11 | 0.209 |
| Over the apex | 37 | 6 | 43 | ||
| Postoperative residual necrotic bone | No | 41 | 5 | 46 | 0.047 |
| Yes | 5 | 3 | 8 | ||
| Wound procedure | Primary suture | 43 | 6 | 49 | 0.512 |
| Open healing | 3 | 2 | 5 | ||
MRONJ, medication-related osteonecrosis of the jaw.
Table 3.
Multivariate analysis of variables in upper MRONJ patients.
| Variable | OR | 95% CI |
|---|---|---|
| Postoperative residual necrotic bone | 0.392 | 0.151–1.018 |
MRONJ, medication-related osteonecrosis of the jaw; OR, odds ratio; CI, confidence interval.
Eight patients did not achieve complete healing. Three and 5 patients were classified as having Stage 2 and Stage 3, respectively. The primary disease for all of those patients were malignancies. Among those 8 patients, the postoperative courses of 3, 4, and 1 patient were improvement, no change, and progression in maxillary MRONJ. With regard to the resection levels, 1, 1, and 6 patients were resected below the apex, at the height of the apex, and above the apex. Also, 1, 3, and 1 patient obtained complete healing, improvement, and no change in concomitant MS (Table 4).
Table 4.
Details of the patients who did not achieve the healing of the maxillary MRONJ.
| Case | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Sex/Age | F/65 | M/77 | M/86 | F/81 | F/81 | F/68 | F/52 | F/60 |
| Stage | 3 | 3 | 2 | 3 | 3 | 2 | 2 | 3 |
| Primary disease | Malignancy | Malignancy | Malignancy | Malignancy | Malignancy | Malignancy | Malignancy | Malignancy |
| Type of drug | Dmab | BP | BP | Dmab | Dmab | BP | Dmab | BP |
| Drug administration period (y) | <4 | <4 | ≥4 | ≥4 | ≥4 | ≥4 | <4 | <4 |
| Steroid administration | Yes | No | No | No | No | No | No | No |
| DM | Yes | Yes | No | No | No | No | No | No |
| Periosteal reaction | No | No | No | Yes | Yes | No | No | No |
| Resection level | At the height of the apex | Above the apex | Above the apex | Above the apex | Above the apex | Above the apex | Above the apex | Below the apex |
| Residual necrotic bone | Yes | Yes | Yes | No | No | No | No | No |
| Sinus procedure | None | Open | None | Open | None | None | None | ESS |
MRONJ, medication-related osteonecrosis of the jaw; BP, bisphosphonate; Dmab, denosumab; DM, diabetes mellitus; F, female; M, male; ESS, endoscopic sinus surgery.
Among 10 patients without healing of concomitant MS postoperatively, 8 patients showed an improvement, based on CT evaluation and change of symptoms. Among 5 patients underwent endoscopic sinus surgery (ESS) to treat concomitant MS, 4 patients did not achieve healing of MS.
Discussion
Recent studies indicate that surgical treatment significantly increases the healing rate in patients with MRONJ compared to conservative therapy.4,8 Furthermore, the treatment outcome was better in patients undergoing major surgery than in patients undergoing minimal surgery.9 Other previous articles also support those results.4,10,11 However, those reports included many mandibular cases. The anatomical and histological differences between maxilla and mandible may influence the disease dynamics and the treatment of MRONJ. Here, the present study subjected to analyze focusing on maxillary surgical cases, and multivariate analysis revealed that postoperative residual necrotic bone were poor prognosticators for the surgical treatment of maxillary MRONJ. Considering the healing rate of the surgery for maxillary MRONJ was 85.2% (46/54 patients), we demonstrate that surgical treatment can be an appropriate strategy for treating maxillary MRONJ. According to the present analysis, clinicians should consider the complete resection of necrotic bone to obtain complete healing of maxillary MRONJ. For this purpose, a surgeon should plan the resection height of the alveolar bone surrounding the necrotic area. In the 46 patients with complete healing, 37 patients were resected above the apex of the involved teeth, indicated that extensive surgery, including the apex, is generally recommended. Considering that the sclerotic reaction tended to be detected in not healing group (7/8 cases), osteotomy height would also be estimated including the sclerotic reaction area on CT imaging.
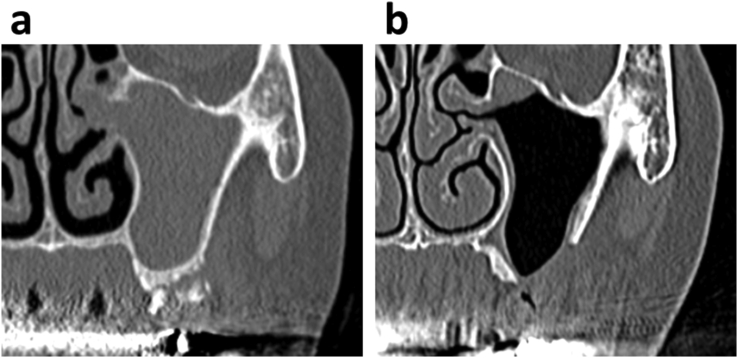
The maxilla has an intricate anatomy, and its specificity makes maxillary bone surgery difficult. Maxillary alveolar infection easily spreads to the maxillary sinus because the bone between these structures is sparse and thin. With regard to the surgery for maxillary MRONJ, the authors preserved the mucous membrane of maxillary sinus as much as possible. The sinus membrane has an abundant blood flow; it demonstrates adequate regenerative capacity (Fig. 1). In case that the improvement of concomitant MS is not obtained postoperatively, additional surgical treatment for MS should be considered (i.e., ESS). However, the significance of the ESS for the treatment of concomitant MS in patients with maxillary MRONJ will be revealed after the accumulation of more cases in the future.
Figure 1.
a. Representative image of the isolation of the left maxillary sequestrum and concomitant maxillary sinusitis. b. In the same patient, maxillary sinusitis healed after the resection of the necrotic bone of the maxilla. The natural hole on the left maxillary sinus is also allowed.
The retrospective nature of the present study has some limitations such as the small number of patients, the impact of previous exposure to risk variables (past dental treatment, prosthesis, smoking, and drinking) which we could not extract from medical records, and antibiotics use (various types, doses, and periods). The point we emphasize the most in the present study is to validate the surgical management specialized in the maxillary cases. Now, MRONJ is not a rare disease, but cases which could undergo maxillary extensive surgery was not readily obtained constantly because of the physical conditions especially in the bony malignant patients (multiple myeloma or bone metastasis) who use BP and/or Dmab. Moreover, such patients could not always endure the general anesthesia and surgical invasion.
In conclusion, the findings in the present study suggested surgical treatment as an appropriate strategy for maxillary MRONJ. It also indicated that complete resection of necrotic bone (i.e., extensive surgery) is needed to obtain complete healing of maxillary MRONJ. Concomitant MS tended to be healed or improved clinically in combination with the healing of maxillary MRONJ.
Declaration of competing interest
The authors have no conflict of interest relevant to this article.
References
- 1.Ruggiero S.L., Dodson T.B., Fantasia J. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 2.Ristow O., Otto S., Troeltzsch M., Hohlweg-Majert B., Pautke C. Treatment perspectives for medication-related osteonecrosis of the jaw (MRONJ) J Cranio-Maxillo-Fac Surg. 2015;43:290–293. doi: 10.1016/j.jcms.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Ramaglia L., Guida A., Iorio-Siciliano V., Cuozzo A., Blasi A., Sculean A. Stage-specific therapeutic strategies of medication-related osteonecrosis of the jaws: a systematic review and meta-analysis of the drug suspension protocol. Clin Oral Invest. 2018;22:597–615. doi: 10.1007/s00784-017-2325-6. [DOI] [PubMed] [Google Scholar]
- 4.Hayashida S., Soutome S., Yanamoto S. Evaluation of the treatment strategies for medication-related osteonecrosis of the jaws (MRONJ) and the factors affecting treatment outcome: a multicenter retrospective study with propensity score matching analysis. J Bone Miner Res. 2017;32:2022–2029. doi: 10.1002/jbmr.3191. [DOI] [PubMed] [Google Scholar]
- 5.Wasserzug O., Kaffe I., Lazarovici T.S. Involvement of the maxillary sinus in bisphosphonate-related osteonecrosis of the jaw: radiologic aspects. Am J Rhinol Allergy. 2017;31:36–39. doi: 10.2500/ajra.2017.31.4395. [DOI] [PubMed] [Google Scholar]
- 6.Fleisch H.A. Bisphosphonates: preclinical aspects and use in osteoporosis. Ann Med. 1997;29:55–62. doi: 10.3109/07853899708998743. [DOI] [PubMed] [Google Scholar]
- 7.Voss P.J., Vargas Soto G., Schmelzeisen R. Sinusitis and oroantral fistula in patients with bisphosphonate-associated necrosis of the maxilla. Head Face Med. 2016;12:3. doi: 10.1186/s13005-015-0099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rupel K., Ottaviani G., Gobbo M. A systematic review of therapeutical approaches in bisphosphonates-related osteonecrosis of the jaw (BRONJ) Oral Oncol. 2014;50:1049–1057. doi: 10.1016/j.oraloncology.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Fliefel R., Tröltzsch M., Kühnisch J., Ehrenfeld M., Otto S. Treatment strategies and outcomes of bisphosphonate-related osteonecrosis of the jaw (BRONJ) with characterization of patients: a systematic review. Int J Oral Maxillofac Surg. 2015;44:568–585. doi: 10.1016/j.ijom.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 10.Stockmann P., Vairaktaris E., Wehrhan F. Osteotomy and primary wound closure in bisphosphonate-associated osteonecrosis of the jaw: a prospective clinical study with 12 months follow-up. Support Care Canc. 2010;18:449–460. doi: 10.1007/s00520-009-0688-1. [DOI] [PubMed] [Google Scholar]
- 11.Lopes R.N., Rabelo G.D., Rocha A.C., Carvalho P.A.G., Alves F.A. Surgical therapy for bisphosphonate-related osteonecrosis of the jaw: six-year experience of a single institution. J Oral Maxillofac Surg. 2015;73:1288–1295. doi: 10.1016/j.joms.2015.01.008. [DOI] [PubMed] [Google Scholar]