Abstract
Overweight and obesity are well-known independent risk factors for stroke in the general population although uncertain in the case of the elderly, according to the obesity paradox. Little is known about underlying mechanisms. Our study aims to assess whether there is a relationship between excess body weight (measured as waist circumference) and poor cerebral hemodynamics (measured by transcranial Doppler parameters: basal, mean flow velocity (MFV), and dynamic, cerebrovascular reserve (CvR) in the right middle cerebral artery (RMCA)). A possible underlying molecular mechanism was analyzed via plasma leptin, adiponectin, TNF-α, IL-6, VCAM, and CRP levels. One hundred sixty-five subjects were included. Bivariate and multivariate regression showed a linear correlation between waist circumference and hemodynamics in RMCA, with clear gender effects: MFV (global NS, men β − 0.26 p < 0.01; women NS), CvR (global: β − 0.15 p < 0.01; men: β − 0.29 p < 0.01, women: β − 0.19 p < 0.09). For subjects above 65 years, there is no significant relationship between AbP and cerebral hemodynamics. In multivariate regression models, only leptin correlated independently with MFV in RMCA (β 7.24, p < 0.01) and CvR (β − 0.30, p < 0.01). In both cases, waist circumference remains significantly related to both parameters. There is an inverse linear correlation between excess body weight and cerebral hemodynamics, independent of other vascular risk factors and clearly influenced by gender. This relation disappears in the elderly population. Leptin might play a role in this relationship. Nevertheless, there must be another associated mechanism, not identified in this study.
Keywords: Obesity, Overweight, Age, Sex, Adipokine, Cerebral hemodynamics, Cerebrovascular reserve, Transcranial Doppler
Introduction
Obesity and being overweight are a major problem worldwide. Both have a high prevalence in most populations. In 2016, there were more than 700 million obese people worldwide, with an overall prevalence among adults of 12%. This prevalence is increasing in almost all countries [1].
Overweight is a major public health problem because it is associated with a higher incidence of mortality and disability (morbidity) [2]. In fact, it is estimated that there are between 2.8 and 4 million deaths from overweight and obesity worldwide [3], accounting for up to 7.0% of all deaths. This mortality is caused by many diseases, especially vascular diseases such as stroke [1, 4, 5]. Accordingly, overweight and obesity can be associated with 2.7 million of deaths related to vascular diseases [1].
Within this clear association between obesity and morbimortality, there is a striking exception corresponding to the elderly population. Although these phenomena are well described in the general population, neither the epidemiology nor the physiology seems to be the same in elderly people. Over the years, several studies have described the lack of a negative relationship between excess weight and cardiovascular mortality in the elderly, which has been called the “obesity paradox” [6–8]. The underlying mechanisms are not clear. One of the possible reasons being the fact that in elderly people it is especially important to evaluate body composition rather just volume in terms of fat and muscle mass [9, 10].
The link between weight excess and vascular events has two important features. First, risk is proportional to excess weight and follows a linear model, starting at overweight and continuing on to morbid obesity [2, 11, 12]. Secondly, even excess weight produces a higher incidence of vascular risk factors, which is related per se to a higher incidence of vascular events [13]. Therefore, obesity should be associated with intrinsic mechanisms which promote vascular pathology. There are many studies showing different mechanisms explaining how excess adipose tissue induces functional and structural damage in the peripheral vascular system [14, 15]. Adipose tissue is metabolically very active, producing a host of circulating factors, the so-called adipokines (leptin, adiponectin, ghrelin), and induces the production of other cytokines such as IL6, TNF, or VCAM in other organs. In obesity, seemingly related to abnormal production of adipokines and probably because of resistance to them, several processes are activated [16, 17]. These include entering a proinflammatory state, endothelial dysfunction, and insulin resistance. All these phenomena are known to eventually induce vascular damage in the form of atherosclerosis [16, 18, 19].
However, the physiology of the cerebral vascular system is different and, in many respects, independent to its peripheral counterpart, especially due to its capacity for autocontrol of local flow, driven primarily by the phenomenon of arteriole-mediated vasoreactivity. Thus, the literature provides hardly any specific information about the mechanisms by which excess weight is associated with cerebrovascular pathology [20]. To date, there have been very few studies in animals [21] and almost none in humans [22, 23]. The hypothesis in our study is that in cases of weight excess, there is a concomitant disorder in cerebral hemodynamics, proportional to increasing weight and mediated by adipokines. This relationship could disappear in the case of elderly subjects. The objective of this work is to analyze if increasing nutritional grade worsens cerebral hemodynamics, and to identify whether or not, in fact, it exists, which model it follows, and if it is independent from the presence of other vascular risk factors, and finally, in case of an independent relationship, to know if there is any molecular mediator derived from the adipose tissue that might explain this relationship.
Material and methods
Design
An observational study of prevalence and cross-association was performed in a population covering the whole spectrum of nutritional status.
Subjects were systematically and consecutively recruited from patients and population in the proximity of a nutrition outpatient clinic in the Endocrinology Department of the Complejo Hospitalario Universitario de Albacete (CHUA). Inclusion criteria were age > 18 years, BMI ≥ 18, temporal acoustic window for ultrasonography, and informed consent signed. Exclusion criteria were detection of intra- or extracranial stenosis (> 50%) and diseases that could modify cerebral hemodynamics (previous stroke, diabetes mellitus, heart failure, or thyrotoxicosis). The proportion of patients with morbid obesity (BMI > 40) was limited to 5% in order to minimize any problems with collinearity, given the frequent association of these patients with all vascular risk factors.
This study was funded by a research grant from the Foundation for Research of Castilla-La Mancha (FISCAM).
Protocol of work
In the initial visit, baseline data were collected; blood tests and all hemodynamic studies were conducted. The basal data included age, sex, hypertension, diabetes, dyslipidemia, smoking, and alcohol consumption. Anthropometric values collected were weight, height, body mass index (BMI), and abdominal perimeter (AbP).
Hemodynamic study
Basal brain hemodynamics
The ultrasonographic study consisted of a cervical duplex study (Esaote MyLab70, Genoa, Italy) in order to rule out cervical arterial stenosis, and a transcranial Doppler (DWL Box, Singen, Germany). A manual 2-MHz pulsed probe was employed for basal study and another probe attached to a helmet for continuous monitoring to collect the data from the right middle cerebral artery (MCA). The basal hemodynamic study values collected were mean flow velocity (MFV) and pulsatility index (PI). For the dynamic hemodynamical study, vasoreactivity measured as cerebrovascular reserve (CvR) was calculated using the carbogen inhalation technique [24], aided by the specific software provided by the transcranial Doppler equipment. The patient was placed in a supine position on a comfortable stretcher, in a quiet darkened room. In all patients, blood pressure was monitored by measuring it immediately before and after the ultrasonographic study. Those values were included in the bivariate and multivariate analysis. MFV in MCA and partial pressure of CO2 in blood (Smiths Medical capnograph, Capnocheck Plus model, Ashford, UK) were monitored. Once basal MFV had stabilized, a high-flux mask with carbogen (O2 95%, CO2 5%) was placed in situ. Within a few seconds, slight hypercapnia (42–55 mmHg) was induced. This was maintained until the new velocity had stabilized. The CvR was measured by dividing the difference between the maximal MFV in hypercapnia and basal MFV by basal MFV (CvR = ((MFVhypercapnia − MFVbasal) / MFVbasal) × 100) [24].
Blood tests included plasma levels of total cholesterol, LDL, HDL, hemoglobin, T4, and thyrotropin. Plasma levels of adipokines (leptin, adiponectin, TNF-α, IL-6, soluble portion of the VCAM (sVCAM), and CRP) were measured by means of ELISA. Plasma insulin levels were determined by chemiluminescence. The HOMA index was calculated using an established formula (HOMA = (glucose (mg/dL) × insulinemia (μU/mL)/405).
Sample size
A sample size calculation was made based on the results of our own group and on the normal values of the Apnea Test in the study of the healthy population, given that the CvR values with this technique and those of carbogen inhalation are superimposed [25]. Likewise, we consider an improvement of over 25% in the CvR test to be a relevant difference, as it seems clinically significant and in accordance with the recommendations of epidemiology in evidence-based medicine. Considering this difference as relevant, the variation of 25% in the test, the sample size for a statistical power (1 − β = 90) and a α = 0.05, the sample size was estimated for 57 subjects. Taking into account a 10% loss or dropout, the minimum sample size was set at 63 patients.
Therefore, considering the three main variables of the study, the minimum necessary sample size was 63 cases and 63 controls. However, due to the possibility of having to use at least 8 variables in the linear regression analysis, it was decided to increase the final sample size to a figure of 160 subjects.
Statistical analysis
All statistical tests presented below were performed using SPSS software version 22.0. For the description of the results, the usual dispersion measures were used: mean and standard deviation for the continuous quantitative variables, and percentages for ordinal and qualitative variables. Bivariate analysis was calculated by linear regression because all variables were quantitative. This was expressed by the regression coefficient beta (β), its degree of significance (p), and the linear correlation coefficient (r). Additionally, a scatter plot of points in which the linear regression line overlaps was also produced. Multivariate analysis was completed in two steps; firstly, a linear regression model was performed including covariables to evaluate independence of the relation between AbP and cerebral hemodynamics. The clinical covariables considered for the model were those with significant correlation to dependent variables or those with clinical relevance. Secondly, a new linear regression model was performed including plasma adipokine levels in order to determine whether some of those variables explain the relationship between AbP and cerebral hemodynamics.
The final inclusion of covariables in each model was made manually, with the aim of identifying the model with the maximum coefficient of determination (R2). The model finally selected established both the degree of relationship that existed (coefficient β) and the significance (p) for each dependent variable.
The presence of collinearity was also analyzed, especially between AbP and adipokines. If present, the covariable value used in each case was in effect z scores, according to residual analysis.
We looked for variables that, like age, can modulate the relationship between abdominal perimeter and cerebral hemodynamics. We performed a univariate analysis by subgroups according to age and other variables that could influence the relationship found in the bivariate and multivariate analysis.
Results
A total of 171 subjects were recruited. Of these, 2 (1.1%) were discarded for either presenting a previously undeclared DM or failure to detect the MCA in the neurosonological study due to absence of an ultrasonographic temporal window 4 (2.3%). No patient was excluded because of a significant arterial stenosis.
Basal results
Specimen characteristics
The baseline characteristics of the study population are shown in Table 1 and Fig. 1.
Table 1.
Values of the baseline characteristics by subgroup according to nutritional state. The last column shows the significance of the differences according to groups, evaluated by an ANOVA study. SD standard deviation
| BMI 18–24.9 | BMI 25–29.9 | BMI ≥ 30 | p | |
|---|---|---|---|---|
| Age (mean ± SD) | 44.4 (9.3) | 47.8 (11.9) | 49.2 (13.0) | 0.02 |
| Sex (% women) | 72.7 | 57.1 | 54.7 | 0.09 |
| Hypertension (%) | 7.3 | 14.8 | 37.2 | < 0.01 |
| Hypercholesterolemia (%) | 16.4 | 23.1 | 28.2 | 0.27 |
| Hypertriglyceridemia (%) | 3.6 | 19.2 | 11.8 | 0.08 |
| Smoking (%) | 28.3 | 36 | 17.4 | 0.10 |
| Sleep apnea (%) | 4 | 4 | 16 | 0.04 |
Fig. 1.
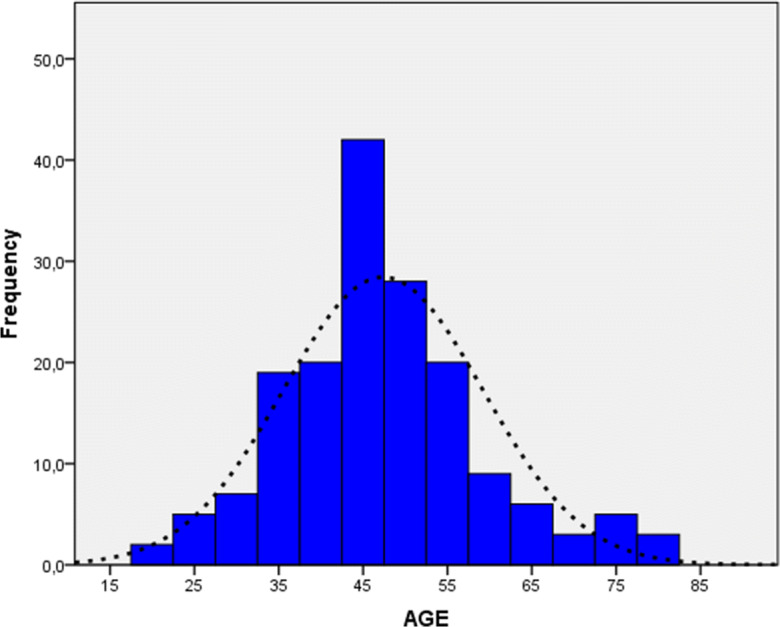
Age distribution among subjects
Anthropometric variables
The mean anthropometric values of this group are shown in Table 2.
Table 2.
Anthropometric values of the group studied and distribution of the weight state of the sample according to the criterion defined by the BMI. BMI body mass index, AbP abdominal perimeter, SD standard deviation
| Anthropometric values (Global) | Weight (kg) | BMI (kg/m2) | AbP (cm) |
| 81.8 SD: 20.1 (45–133) | 29.8 SD: 6.8 (18.2–47.5) | 99.1 SD: 17.4 (60–140) | |
| BMI distribution |
Normal (BMI 18–24.9) |
Overweight (25–29.9) |
Obesity (> 30) |
| 32.50% | 16.60% | 50.90% | |
| AbP distribution |
AbP excess (global) |
Women (AbP > 80 cm) |
Men (AbP > 94 cm) |
| 59.80% | 61.20% | 57.60% |
Hemodynamic and ultrasonographic variables
Cerebral hemodynamic variables in the middle cerebral artery are shown in Table 3:
Table 3.
Cerebral hemodynamics of the global population and segmented sample according to gender and nutritional status. MCA right middle cerebral artery, MFV mean flow velocity, PI pulsatility index, CvR cerebrovascular reserve, BMI body mass index, SD standard deviation
| MFV | PI | CvR (%) | ||
|---|---|---|---|---|
| Total | 55.1 SE: 12.9 (24.7–94.3) | 0.8 SE: 0.13 (0.54–1.56) | 39.9 SE: 12.3 (5.5–110.3) | |
| Sex | Women (103) | 58.7** | 0.78* | 41.4* |
| Men (66) | 49.2 | 0.83 | 37.5 | |
| BMI | 18–24.9 (55) | 58.1 | 0.82 | 43.7 |
| 25–29.9 (28) | 54.3 | 0.77 | 40.7 | |
| ≥ 30 (86) | 53.5 | 0.8 | 37.1** |
*< 0.05; **< 0.01
Normality of the variables
Applying the Kolmogorov-Smirnov and Shapiro-Wilk tests and using the Q-Q plot charts, the normality of cerebral hemodynamics and blood pressure, as well as anthropometric and molecular variables, was studied. This test showed normality for all of the variables used except for PI.
Analytical study
Overview
Statistical analysis of the continuous variables was commenced by testing several non-linear models of dispersion, which did not show a better fit than the linear model. Subsequently, linear models were applied to both bivariate and multivariate studies.
When analyzing the results obtained, we found that the variable “sex” acted as a modifier of the effect of body size on all dependent variables. In other words, the effect that the independent variables had on each of the dependent variables studied was very different in men and women. The results are presented for the general population and stratified by sex.
Bivariate study
With respect to the MFV in the MCA, a significant correlation with AbP was identified. This correlation is also significant in both sexes, but with different values. In males (β − 0.24: for each cm of AbP, the MCA is lowered by 0.24 cm/s), it is clearly higher than that in females, in which this correlation is almost non-existent (β 0.08) (Table 4).
Table 4.
Bivariate analysis between the variables of cerebral and systemic hemodynamics and abdominal perimeter. MFV mean flow velocity, PI pulsatility index, CvR cerebrovascular reserve, β regression coefficient beta, r linear correlation coefficient
| MFV | PI | CvR (%) | ||||
|---|---|---|---|---|---|---|
| r | β | r | β | r | β | |
| Total | − 0.27 | − 0.20** | 0.06 | < 0.01 | − 0.29 | − 0.20** |
| Women | − 0.11 | − 0.08* | 0.12 | < 0.01 | − 0.26 | − 0.19* |
| Men | − 0.29 | − 0.24* | − 0.15 | < 0.01 | − 0.25 | − 0.18* |
*p < 0.05; **p < 0.01
Regarding the MCA pulsatility index (MCA PI), in our group, there is no significant correlation with AbP, neither in women nor in men.
When the CvR in MCA is considered, there is a significant correlation with AbP. This correlation is similar in both sexes (women β 0.19, men β − 0.18: for each cm of AbP, the CvR in the MCA is lowered 0.19% in women and 0.18% in men) (Table 4).
Elderly people
There was a linear negative relationship between age and cerebral hemodynamics in terms of MFV and PI, but not in CvR. The subgroup of subjects above 65 years had lower MFV in MCA and higher PI in right MCA (Table 5). This relationship seems to be independent to other risk factors (Table 6).
Table 5.
Relationship of age with cerebral hemodynamics. First row: Student t test comparing the mean cerebral hemodynamic values in subgroups of subjects up to and above 65 years. Second row: linear univariate regression analysis between age and cerebral hemodynamics. MFV mean flow velocity in right middle cerebral artery, PI pusatility index, CvR cerebrovascular reserve, β regression coefficient beta, r linear correlation coefficient
| MFV | PI | CvR (%) | |||||
|---|---|---|---|---|---|---|---|
| t Student |
≤ 65 years (155) |
56.5 cm/s** | 0.79** | 40.3 | |||
|
> 65 years (14) |
40.5 cm/s | 0.95 | 35.2 | ||||
| Bivariate | r 0.44 | β − 0.47** | r 0.23 | β 0.003* | r 0.058 | β − 0.06 | |
*p < 0.05; **p < 0.001
Table 6.
Univariate linear regression between abdominal perimeter and cerebral hemodynamics in terms of mean flow velocity (MFV), pulsatility index (PI), and cerebrovascular reserve (CvR). β regression coefficient beta, r linear correlation coefficient. First row: all subjects. Second row: population up to 65 years. Third row: population above 65 years
| MFV | PI | CvR (%) | ||||
|---|---|---|---|---|---|---|
| r | β | r | β | r | β | |
| Total | 0.27 | − 0.20** | 0.06 | 0 | 0.29 | − 0.20** |
| ≤ 65 | 0.23 | − 0.16** | 0.02 | 0 | 0.28 | − 0.19** |
| > 65 | 0.20 | 0.17 | 0.39 | − 0.01 | 0.28 | − 0.22 |
**p < 0.001
Considering the relation between cerebral hemodynamics and AbP in elderly people, the bivariate linear regression analysis was repeated by splitting the sample into two subgroups: subjects up to 65 years in one group and above 65 in the other. In the subgroup of subjects up to 65 years, there is a significant negative relationship between AbP and the variables MFV in right MCA and CvR, which is linear in form, whereas there is no identifiable relationship in the subgroup of subjects over 65 years of age (Table 6).
Multivariate study
A multivariate analysis was performed for each dependent variable that had a correlation with AbP in the univariate analysis (MFV and CvR). The model included AbP and all covariates with clinical relationships as independent variables. They were included in a manual fashion, in order to find the model which can explain such dependent variables most convincingly according to the highest R2 value.
Regarding the mean flow velocity in the MCA, we found AbP remained significantly linked in the male group with β 0.26 (Table 7). The covariables that were independently associated according to our results were age and smoking. This correlation indicates that for each extra centimeter of waist measured, the MFV in MCA is 0.26 cm/s smaller.
Table 7.
Multiple linear regression analysis of the mean flow velocity and cerebrovascular reserve in the right MCA
| Multiple linear regression | |||||
|---|---|---|---|---|---|
| Mean flow velocity in R MCA | Cerebrovascular reserve in R MCA | ||||
| Women | Men | Global | Women | Men | |
| Coefficient β | |||||
| Age | − 0.24* | − 0.50* | − 0.09 | 0.12 | 0.04 |
| Hypertension | 0.69 | 1.28 | − 5.4* | − 8.74* | − 0.07 |
| Smoking | 0.57 | 6.71* | 0.11 | 0.15 | 0.16 |
| Abdominal perimeter | − 0.01 | − 0.26* | −0.15* | − 0.19 (p 0.09) | − 0.29* |
| Systolic blood pressure | 0.00 | 0.15* | − 0.67 | − 0.15 | − 0.16 |
| HOMA (≤ 2.53) | 1.12 | 3.86 | − 0.71 | − 0.14 | − 0.13 |
| Cholesterolemia (< 200 mg/dL) | − 7.42 | 3.64 | 0.035 | − 0.04 | 0.15 |
| Adjusted R2 | 0.08 | 0.38 | 0.12 | 0.06 | 0.38 |
*p < 0.05
Inspection of the CvR of the MCA in the global group reveals that abdominal perimeter has a statistically significant association with the CvR. For each centimeter that the AbP increases, there is a decrease of 0.19% of the CvR of the MCA.
In the female group, AbP is bordering on significance. A history of hypertension is independently associated with CvR (β − 8.74). In the male group, AbP was significantly associated with the CvR independently of other factors included in the model. For each centimeter of waist circumference, the CvR of the MCA decreases 0.29%.
Participation of circulating factors
Molecule levels had a high correlation with AbP, so the risk of multicollinearity was high.
Due to this, a further multivariate model was performed in case of a significant relationship between AbP and the dependent variable (MFV in men, CvR global and CvR in men). In each case, the molecule residual value (z score) was included in the same manual fashion, thus identifying the variables which adequately explained the dependent variable (maximum R2).
When examining the MFV of the R MCA, it is seen that there is a statistical association with leptin residual values. Since the beta coefficient for AbP was maintained, the relationship of AbP with MFV is likely to be in part leptin-mediated, but there is also an independent effect on this molecule (Table 8).
Table 8.
Study of the multiple linear regression models with and without circulating factors corresponding to the dependent variables mean flow velocity and cerebrovascular reserve in right middle cerebral artery
| Multiple linear regression | ||||
|---|---|---|---|---|
| Mean flow velocity in R MCA | Cerebrovascular reserve in R MCA | |||
| With circulating factors | Without circulating factors | With circulating factors | Without circulating factors | |
| Coefficient β | ||||
| Age | − 0.50* | − 0.44 | 0.04 | 0.04 |
| Hypertension | 1.28* | 1.19* | − 0.07 | − 0.07 |
| Smoking | 6.71* | 7.29* | 0.16 | 0.16 |
| Abdominal perimeter | − 0.26 | − 0.26 * | − 0.29** | − 0.29** |
| Systolic blood pressure | 0.15* | 0.18 | − 0.16 | − 0.16 |
| HOMA (≤ 2.53) | 3.86 | 3.12 | − 0.13 | 0.12 |
| Cholesterolemia (< 200 mg/dL) | 3.64 | 3.75 | 0.15 | 0.15 |
| Leptin (4th quartile) | 7.24* | − 0.30* | ||
| Adjusted R2 | 0.38 | 0.43 | 0.15 | 0.15 |
*p < 0.05; **p < 0.01
Finally, with respect to the CvR in the MCA, it is also apparent that there is a statistical association with the leptin residual value. Once again, the beta coefficient for AbP was maintained thus indicating that the relationship of AbP with CvR is in part leptin-mediated, but there is also an independent effect on this molecule.
Discussion
As discussed in the main hypothesis of this study, we have been able to verify that excess weight is associated with worse cerebral hemodynamics, apparent as a lower MFV in the MCA (male group) and a lower CvR. In addition, within the secondary objectives, we have been able to demonstrate that this relationship is mediated by leptin, rather than the other circulating factors analyzed. The relationship disappears in the subgroup of subjects older than 65 years. Finally, the demonstration of a clear modulating effect of sex on the relationship between waist circumference and cerebral hemodynamics was not expected at the beginning. Thus, hemodynamic damage in males is higher than that in females in cases of equal weight excess.
With regard to the main hypothesis of the study, it has been demonstrated that weight excess is related to poor cerebral hemodynamics, with both a worse MFV in the main cranial arteries (although this has only been demonstrated for males) and reduced capacity to dilate in response to a vasodilator stimulus (CvR).
In addition, and according to our proposal, the relationship between waist circumference and cerebral hemodynamics conforms to a linear model, with worsening of such being proportional to excess weight, with overweight being the starting point. Of note, the relation of waist circumference and risk of stroke follows the same linear pattern [11, 12, 26].
Similarly, as proposed in the hypotheses of the study, the association of abdominal circumference with worse cerebral hemodynamics is independent of common vascular risk factors, according to multivariate analysis. This is relevant because most obese patients are both hypertensive, hyperlipidemic, or diabetic. Again, the relationship between weight excess and risk for stroke is independent of their vascular risk factors [26–29].
Therefore, there should be mechanisms inherent to weight excess that cause damage which affects cerebral hemodynamics. As we have already mentioned, these mechanisms, which are well characterized in the systemic circulation, remain hypothetical when applied to the cerebral vascular bed [20, 30].
According to these results, with respect to lower MFV and CvR, we consider that the damage is most likely preferentially confined to small caliber arteries, be it functional or structural in nature.
In the case of normal intracranial pressure, a decrease in the blood flow velocity of the great cerebral arteries, such as the MCA, is fundamentally due to three circumstances: a change in the luminal diameter of that artery, a decrease of global blood flow to the brain, or an increase in the distal resistance of the artery studied.
It has already been observed by means of MRI that in weight excess, the diameter of the MCA remains unchanged [22]. Likewise, we can reasonably rule out the presence of heart failure in our patients because of the absence of either prior history, symptoms, or abnormal BP, thus accounting for decreased global blood flow to the brain.
The third option corresponds to an increase in peripheral cerebral resistance, at the level of arterioles, which is the most plausible possibility in the context of the rest of the findings.
The presence of lower MFV and CvR in the MCA in weight excess supports the hypothesis that global hemodynamic changes are secondary to an intrinsic property of cerebral arteries. Specifically, CvR damage reinforces the idea that alteration of cerebral vasculature in obesity does not predominate in the arteries of the circle of Willis but rather is located in the most distal portions of the arterial system. Cerebral arterioles are those that determine vascular resistance [20, 31]; they are also the effectors of changes that allow dynamic regulation of cerebral flow. Although arteriolar lesions are usually associated with a higher pulsatility index, we did not see such a relationship in our study because this parameter has a very small range of values, so a very high statistical power would be required to be able to find any differences. In effect, we postulate that in obesity there is an increase in cerebral peripheral resistance derived from structural alteration of the cerebral arteriolar tree.
Animal models support the theory of damage in arterioles. Moreover, they suggest that this change corresponds to structural modifications in the wall of the artery, and not functional changes. These correspond to remodeling rather than atheromatosis [21, 32, 33]: these models show evidence of migration, muscle proliferation, and change in the extracellular matrix [34] (which undergoes increased collagen and metalloprotease activity).
Arterial remodeling is described as those structural changes of the arteries in response to atheromatosis or any hemodynamic alterations that are intended to maintain surface stress within the vessel lumen. These changes correspond to modifications of the intima (development of neointima) and most probably with modifications of the middle layer as well. This layer shows anomalies of myocyte growth and proliferation, but also alterations in the composition of the extracellular matrix, mainly by means of an increase in collagen.
These findings, as predicted, are associated with worse arterial vasodilatation and major cerebral infarctions in animal models of ischemia [32]. Our work, like previous works [22, 23], has found altered CvR in the obese. And our hypothesis, which has not been previously raised, is that these alterations are at least partly due to a process of cerebral vascular remodeling. Another reason to think that there is arterial remodeling in the obese is the finding in our sample that the relationship of waist circumference to MFV in MCA and CvR is modulated by the action of leptin. Previous studies have shown that this molecule is involved in changes in arterial wall structure in obesity [35].
Whatever structural or functional change the cerebral vascular bed may undergo in the obese, in any case, it is necessary to investigate the mechanism by which these alterations can occur. Both functional alteration and structural changes in cerebral arteriolar remodeling in obesity should be mediated by mechanisms that act at a distance, since there is no adipose tissue in the nervous system. The molecular analysis obtained in this work has allowed us to identify leptin as the only substance analyzed involved in the relationship between abdominal circumference and cerebral vascular damage. We cannot exclude completely some level of relationship between any of the other circulating factors studied and cerebral vasculature, because of a potential lack of statistical power linked to sample size. If this is indeed the case, relation is presumably very weak. Collinearity and use of residual values are complex statistical procedures and require careful interpretation. In any case, it is the methodologically correct way to handle closely related variables. As a result, we have drawn more valuable conclusions about the role of inflammation, endothelial function, insulin resistance, and indeed the role of adipokines themselves.
Regarding inflammation, it is known that obesity promotes a proinflammatory state, with local formation of inflammatory cytokines, specially CRP, TNF-α, and IL-6 [36], clearly related to vascular damage in obesity [16, 37, 38]. However, in the present study, although we found elevated levels of these cytokines, we found no association with cerebral hemodynamic damage. It should be noted that all these cytokines act in a paracrine mode [36, 39], by local release of these circulating factors into the vasa vasorum, and not per se as hormones [40]. By extension, it could be inferred that in cerebral territories, and since the cerebral arteries do not have perivascular adipose tissue [20, 41], there would be no vascular damage mediated by cytokines [42].
Overweight has also been associated with systemic endothelial dysfunction [30], mediated by free fatty acids, insulin, and adipokines. To date, there are no in vivo techniques validated in humans to assess the endothelial function of cerebral arteries. We relied on an indirect approach to assess endothelial function, based on sVCAM levels. However, multivariate models in our study did not show any relationship between sVCAM levels or any of the parameters analyzed for cerebral hemodynamics in our cohort of overweight patients. These observations therefore contradict, once again, the participation of endothelial dysfunction in cerebral arterial damage in obesity, in mechanistic terms at least.
In the case of insulin resistance, the relationship between diabetes mellitus and arterial damage is already well known, although it is not clear in models of insulin resistance without diabetes [43, 44]. In our sample, up to 25% of the subjects scored highly on the HOMA index, indicating insulin resistance. Despite this, the multivariate models did not prove that insulin resistance was involved in the relation of weight excess to alterations in cerebral hemodynamics. Our conclusions in this regard must be tempered with caution and limited to patients with non-diabetic weight excess. In those individuals, the presence of insulin resistance probably does not confer a deleterious effect upon the cerebral arteries. We are not able to assure that this mechanism plays a role in patients who are both obese and diabetic.
It is important to note that patients with diabetes were not included in the study because such a variable, so strongly associated with vascular damage, may underestimate the effect of obesity on the pathology examined. Therefore, diabetic patients were not included due to two reasons: mainly because it is a disease that significantly alters all cerebral parameters studied [45]. Because there is a preponderance of patients who are both obese and diabetic, inclusion of such patients in a consecutive fashion directly from an Endocrinology outpatient clinic would skew the study population. This would undoubtedly greatly limit multivariate analysis because of the risk of collinearity between the anthropometric variables and the presence of diabetes [35]. In previous studies of the vascular relevance of obesity, this problem has already been seen. In those studies, diabetes has not been considered, or when included in multivariate models, it significantly modifies the effect of the anthropometric variable on vascular disease [46]. We firmly believe that with the design of our study, the results are more easily extrapolated to estimate the specific cerebrovascular effect of obesity, rather than the effect of vascular risk factors to which it is associated.
Finally, main adipokines (leptin, adiponectin, and resistin) have been linked to the systemic vascular changes [36]. With respect to adiponectin, in our study, there was no relation with cerebral hemodynamic parameters. We should point out that, although low levels of adiponectin have been previously associated with good prognosis in case of stroke [47], recent meta-analysis did not support that contention [48, 49]. Other clinical studies also failed to find a relationship with small vessel disease [36, 50].
On the contrary, in the case of leptin, our work points to a substantial participation of this molecule in relation to weight excess and lower MFV in MCA, and worse CvR.
Leptin is known to participate in multiple pathophysiological processes that bring about vascular damage at the systemic level [36]: production in macrophages of other proinflammatory and vasoactive circulating factors like CCL-3, CL-4, and CCL-5. It also induces the release of oxygen reactive substances from activated inflammatory cells with consequent local oxidative stress. Its excess is associated with the development of endothelial dysfunction [51], arterial hypertension [52], and finely accumulated vascular cholesterol and atheromatosis [53]. More interesting and related to our results is that there are studies which demonstrate that hyperleptinemia is involved in processes of functional and/or structural alteration of the cerebral arterioles. Leptin is implicated in mechanisms that can modify the tone and regulation of arteriolar diameter, which could generate arteriolar dysfunction without structural modification [51]. In addition, as previously mentioned, control of CvR is multifactorial, but one element that is certainly relevant is vegetative control, both sympathetic and parasympathetic [20, 54]. Leptin has been shown to be a potent activator of the sympathetic system at a systemic level [52], but also at the cerebral level [55, 56]. On the other hand, there are multiple studies showing that hyperleptinemia causes arterial remodeling at the systemic level: increased arterial stiffness measured by ultrasound [57], pulse pressure velocity, and increased intima media thickness [35]. In addition, there are studies that demonstrate the development of neointima [58] and the proliferation of smooth muscle cells in the arterial wall mediated by leptin [59]. All this supports the observations in our sample and therefore allows us to suggest that leptin might be involved in the relationship between weight excess and worse cerebral hemodynamics. Nevertheless, further studies are warranted to confirm the hypothesis of a causal relationship. In turn, worsening of cerebral hemodynamics would, in whole or in part, cause arterial and arteriolar remodeling. Our study has not investigated all other potential participants in the relationship between waist circumference and cerebral hemodynamics. In this respect, we cannot rule out the participation of other circulating factors, such as resistin, C1q/TNF-related proteins, omentin [60], CCL-2, PAI-1, free fatty acids, or the recently newly described myokines, which are tightly related to adipokines and fat tissue metabolism [61, 62]. Indeed, this role of myokines could help to understand why sarcopenia is a better marker of vascular damage, rather than AbP in elderly people. Likewise, there are studies that also suggest the presence of an adipocyte-dependent vasodilator factor (ADVF), not characterized to date [39]. In addition to other molecular mediators, it is necessary to mention the potential influence of additional factors that have also remained outside the field studied in this work, such as sleep apnea, a vascular risk factor recently related to cerebral arterial damage [63, 64]. Although there was no history of OSAHS in our sample, there were no specific tests that corroborated or refuted this possibility.
In our population, there is no relation between AbP and cerebral hemodynamics in elderly people. Age remains a clearly related variable with a poorer MFV and PI in the right MCA, with an overall negative linear trend being evident. The worsening of hemodynamics along the years is well described, so that the normality values of the MFV and IP are currently described according to age [65]. However, there is no relation between AbP and cerebral hemodynamics in elderly people.
Regarding the role of age in the relationship between weight excess and cerebral hemodynamics, this study showed different results for elderly people compared to the general population. Above 65 years, AbP is not related to MFV nor CvR in the MCA. These findings match the obesity paradox, insofar that typical biomarkers, such as BMI or AbP, are bad predictors of vascular diseases in terms of incidence and mortality in older populations [6]. There are two main reasons which explain why AbP does not allow estimation of the real relationship between adipose tissue and cerebral hemodynamics. Both are related to the process of muscle tissue loss or sarcopenia, which is quite frequent and intense in older population. Firstly, in the non-elderly population, usual weight indicators such as BMI and AbP markers accurately reflect excess adipose tissue, and in the case of BP, visceral adipose tissue. However, in the older population, their value is poorer because the loss of muscle mass significantly modifies their value independent to the volume of adipose tissue. Secondly, in the elderly, the process of muscle tissue loss has a relevant impact on multiple pathological processes, including vascular pathology and probably also on cerebrovascular pathology [6]. The metabolic changes related to muscle loss conceivably include modification in the production of some adipokines such us leptin and adiponectin [61]. Moreover, in this population, the effects of sarcopenia are much more intense than those caused by the accumulation of adipose tissue. Therefore, in the case of the elderly population, a specific design is needed to analyze the role of each tissue type in brain hemodynamics [9].
In our results, we found subject sex to be a modulator of the relationship between waist circumference and cerebral hemodynamics. It is known that the incidence of cerebrovascular disease and its severity is different between the two sexes. At the vascular level, cerebral hemodynamics is also different between men and women, at least until menopause. Cerebral vessels do not have the same functional and/or structural situation, but in previous works studying relations between obesity and cerebral or cervical hemodynamics included no descriptive analysis regarding sex [22, 23, 66]. It is noteworthy that between the previous studies regarding the relation between cerebral hemodynamics and weight, only one considered the influence of sex. Several articles have found different amounts of perivascular and epicardial adipose tissue depending on sex and also different activities in the production of adipokines (adiponectin and leptin) and inflammatory circulating factors between the two sexes [67, 68]. There can also be different metabolic responses to the same external stimuli (metabolic flexibility) between the sexes [69]. Finally, several studies showed a sexual dimorphism in terms of different plasma levels of adipokines (higher in men) and especially in their effect. Indeed, it is postulated that there is some degree of resistance to the effects of leptin in women [70, 71]. It would be interesting in future studies to consider the presence of sexual dimorphism in the female group all along the age range or just until menopause. Therefore, we could postulate by way of conclusion that in men, not only would there be a greater frequency of visceral fat accumulation, but perhaps there would also be a different perivascular distribution and, in any case, the repercussions caused by each centimeter of increase in the abdominal perimeter could mean a substantial increase in metabolic activity.
Regarding the weaknesses of the study, first, due to the different waist circumference-cerebral hemodynamics relationships according to the sex of the subject, it was necessary to split the sample. Statistical power could be diminished. Positive results can be considered reliable, but false negatives can exist, especially in the female group. Another potential methodological weakness lies in the selection of the sample, since patients with diabetes were not included. If this is the case, there is a risk that this variable, so strongly associated with vascular damage, may underestimate the effect of obesity on the pathology examined. Therefore, diabetic patients were not included due to two reasons: mainly because it is a disease that significantly alters all cerebral parameters studied. Because there is a preponderance of patients who are both obese and diabetic, inclusion of such patients in a consecutive fashion directly from an Endocrinology outpatient clinic would skew the study population. This would undoubtedly greatly limit multivariate analysis, with a high risk of collinearity between the anthropometric variables and the presence of diabetes. In previous studies of the cardiovascular relevance of obesity, diabetes has not been considered, or when included in multivariate models, significantly modifies the effect of the anthropometric variable on cardiovascular disease. Collinearity and use of residual values can reduce the statistical power and therefore could produce false negatives in molecule analysis. Again, it does not influence positive results regarding the role of leptin in the relationship of waist circumference-cerebral hemodynamics. Although it is a complex statistical procedure and requires careful interpretation, it is the methodologically correct way to handle closely related variables. As a result, we have drawn more valuable conclusions about the role of inflammation, endothelial function, and insulin resistance or the role of adipokines themselves.
Regarding the strengths of the study, the methodology used in this work to measure cerebral hemodynamics, it should be noted that systemic and cerebral ultrasonography were used for the assessment, ultrasonography being a simple and valid technique, that compares favorably to other more complex methods, which are less accessible and require a greater period of time to conduct [24]. This technique allows us to analyze basal (MFV, PI) and dynamic parameters of the cerebral vasculature (CvR). Although brain ultrasonography may show inter- and even intraobserver variability, a homogeneous evaluation of the subjects could be made by systematization of the procedure and the completion of all the studies by the same observer, who also had previously acquired a high level of ultrasonographic skill. Finally, the inclusion of parameters of systemic vascular dysfunction and of the analytical values of the secreted circulating factors also allowed us to suggest the mechanisms that drive this relationship. Similar studies published previously have shown results equivalent to those of this study [22, 23]. In comparison, there are some similarities in terms of cerebral hemodynamics, but this study gives additional information about the molecular mechanisms underlying the relationship and shows the important effect of gender on this relationship. In addition, the study was carried out with a large sample size and a wide variety of variables analyzed, which allowed for a sufficiently complete multivariate analysis for an adequate study of the hypotheses of this work. The breadth of the analyzed variables also made it possible to clarify one of the main questions raised in this study, which is the independent effect of weight excess from the other vascular risk factors that are usually associated with this problem.
In summary, our work shows that excess body weight is related to worse cerebral hemodynamics independent of other vascular risk factors and that leptin is a fundamental mediator in this relationship, which is also clearly influenced by the gender of the patient. These findings reinforce the need for public health measures to prevent overweight, mainly in men. However, since this is a cross-sectional study, it is mainly a hypothesis generator and should lead to subsequent work that tries to corroborate our findings. Future studies should aim to both confirm our findings and explore the potential reversibility of cerebral hemodynamic alterations after weight loss, as has been seen to occur in other systemic vascular beds [72, 73]. Finally, in the future, a better understanding of the mechanisms underlying cerebrovascular damage linked to obesity may serve to develop treatment and prevention strategies for these patients, which unfortunately are becoming increasingly common in our societies.
Acknowledgments
We thank Dr. J Ahmad BSc (Hons) MBBS Ph.D. for their expert advice in the translation process.
Authors’ contribution
OAM participated in the design of the project, recruiting process, physical exam of the subjects, ultrasonographic studies, and statistical analysis and wrote the article.
MGH and IGF participated in the design of the project, recruiting process, measuring vital signs, taking blood samples, and helping in ultrasonographic procedures and revised the text of the article.
CAF participated in the design of the project and laboratory analysis and wrote the article.
CL, JJAM, and FB participated in the design of the project and recruiting process and wrote the article.
JGG, FHF, and TM participated in the design of the project, recruiting process, and statistical analysis and wrote the article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: official grant from the regional Health Service of Castilla-La Mancha, Spain (Exp. Number PI 2006/39-2008).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethics Committee of Complejo Hospitalario Universitario de Albacete as well as by the Research Commission of the Centre, according to the Helsinki declaration. Written informed consent was obtained from each volunteer prior to participation.
Footnotes
NEW & NOTEWORTHY
This study provides evidence of the relationship between excess weight and inferior cerebral hemodynamics in humans, in terms of lower arterial flow velocity and cerebrovascular reserve. The relationship is linear, progressing from overweight to any grade of obesity. In subjects older than 65 years, no association between abdominal perimeter and cerebral hemodynamics was found. Sexual dimorphism is evident, with worse hemodynamic values in males compared to females for the same weight excess. Molecular analysis suggests leptin plays a key role, possibly by facilitating dynamic or structural (remodeling) changes in the arterioles.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Oscar Ayo-Martin, Email: oayo@sescam.jccm.es, Email: oscarayo@gmail.com.
Jorge García-García, Email: jggpillarno@hotmail.com.
Francisco Hernández-Fernández, Email: fco.hdez.fdez@gmail.com.
Mercedes Gómez-Hontanilla, Email: mercegonta@gmail.com.
Isabel Gómez-Fernández, Email: gomezfernandezisabel@gmail.com.
Carolina Andrés-Fernández, Email: carolanfer@hotmail.com.
Cristina Lamas, Email: cristinalamas72@hotmail.com.
José Joaquín Alfaro-Martínez, Email: jalfaro@sescam.jccm.es.
Francisco Botella, Email: fbotellar@sescam.jccm.es.
Tomás Segura, Email: tseguram@gmail.com.
References
- 1.GBD 2015 Obesity Collaborators A. Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO | 10 facts on obesity. https://www.who.int/features/factfiles/obesity/en/
- 4.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26- year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5):968–977. doi: 10.1161/01.CIR.67.5.968. [DOI] [PubMed] [Google Scholar]
- 5.Rexrode KM. Abdominal adiposity and coronary heart disease in women. JAMA J Am Med Assoc. 1998;280:1843–1848. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 6.Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. 2019. 10.1007/s40519-019-00815-4. [DOI] [PubMed]
- 7.Chang VW, Langa KM, Weir D, Iwashyna TJ. The obesity paradox and incident cardiovascular disease: a population-based study. PLoS One. 2017;12:e0188636. doi: 10.1371/journal.pone.0188636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc. 2014;62(2):253–260. doi: 10.1111/JGS.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanada K, Chen R, Willcox B, et al. Association of sarcopenic obesity predicted by anthropometric measurements and 24-y all-cause mortality in elderly men: the Kuakini Honolulu Heart Program. Nutrition. 2018;46:97–102. doi: 10.1016/J.NUT.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Batsis JA, Mackenzie TA, Barre LK, Lopez-Jimenez F, Bartels SJ. Sarcopenia, sarcopenic obesity and mortality in older adults: results from the National Health and Nutrition Examination Survey III. Eur J Clin Nutr. 2014;68(9):1001–1007. doi: 10.1038/EJCN.2014.117. [DOI] [PubMed] [Google Scholar]
- 11.Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 13.Strazzullo P, D’Elia L, Cairella G, et al. Excess body weight and incidence of stroke: meta-analysis of prospective studies with 2 million participants. Stroke. 2010;41(5):e418–26. 10.1161/STROKEAHA.109.576967. [DOI] [PubMed]
- 14.Kalil GZ, Haynes WG. Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens Res. 2012;35:4–16. doi: 10.1038/hr.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tripathy D, Mohanty P, Dhindsa S, et al. Elevation of free fatty acids induces inflammation and impairs vascular reactivity in healthy subjects. Diabetes. 2003;52:2882–2887. doi: 10.2337/diabetes.52.12.2882. [DOI] [PubMed] [Google Scholar]
- 16.Bastard J-P, Maachi M, Lagathu C, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17:4–12. [PubMed] [Google Scholar]
- 17.Beltowski J, Wojcicka G, Gorny D, Marciniak A. The effect of dietary-induced obesity on lipid peroxidation, antioxidant enzymes and total plasma antioxidant capacity. J Physiol Pharmacol. 2000;51:883–896. [PubMed] [Google Scholar]
- 18.Fantuzzi G, Theodore M, Mazzone T. Adipose tissue and atherosclerosis: exploring the connection. Arterioscler Thromb Vasc Biol. 2007;27:996–1003. doi: 10.1161/ATVBAHA.106.131755. [DOI] [PubMed] [Google Scholar]
- 19.Ruscica M, Baragetti A, Catapano AL, Norata GD. Translating the biology of adipokines in atherosclerosis and cardiovascular diseases: gaps and open questions. Nutr Metab Cardiovasc Dis. 2017;27(5):379–395. doi: 10.1016/J.NUMECD.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Dorrance AM, Matin N, Pires PW. The effects of obesity on the cerebral vasculature. Curr Vasc Pharmacol. 2014;12:462–472. doi: 10.2174/1570161112666140423222411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu F, Beard DA, Frisbee JC. Computational analyses of intravascular tracer washout reveal altered capillary-level flow distributions in obese Zucker rats. J Physiol. 2011;589:4527–4543. doi: 10.1113/jphysiol.2011.209775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Selim M, Jones R, Novak P, et al. The effects of body mass index on cerebral blood flow velocity. Clin Auton Res. 2008;18:331–338. doi: 10.1007/s10286-008-0490-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willeumier KC, Taylor DV, Amen DG, et al. Elevated BMI is associated with decreased blood flow in the prefrontal cortex using SPECT imaging in healthy adults. Obesity (Silver Spring) 2011;19:1095–1097. doi: 10.1038/oby.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ringelstein EB, Sievers C, Ecker S, et al. Noninvasive assessment of CO2-induced cerebral vasomotor response in normal individuals and patients with internal carotid artery occlusions. Stroke. 1998;19:963–969. doi: 10.1161/01.STR.19.8.963. [DOI] [PubMed] [Google Scholar]
- 25.Jiménez-Caballero PE, Segura T, Jimńez-Caballero PE, T. S. Valores de normalidad de la reactividad vasomotora cerebral mediante el test de apnea voluntaria. Rev Neurol. 2006;43:598–602. [PubMed] [Google Scholar]
- 26.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurth T, Gaziano JM, Berger K, et al. Body mass index and the risk of stroke in men. Arch Intern Med. 2002;162:2557–2562. doi: 10.1001/archinte.162.22.2557. [DOI] [PubMed] [Google Scholar]
- 28.Suk S-HH, Sacco RL, Boden-Albala B, et al. Abdominal obesity and risk of ischemic stroke: the Northern Manhattan Stroke Study. Stroke. 2003;34:1586–1592. doi: 10.1161/01.STR.0000075294.98582.2F. [DOI] [PubMed] [Google Scholar]
- 29.Hu G, Tuomilehto J, Silventoinen K, et al. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch Intern Med. 2007;167:1420–1427. doi: 10.1001/archinte.167.13.1420. [DOI] [PubMed] [Google Scholar]
- 30.Pires A, Castela E, Sena C, Seiça R. Obesity: paradigm of endothelial dysfunction in paediatric age groups. Acta Medica Port. 2015;28:233–239. doi: 10.20344/amp.5202. [DOI] [PubMed] [Google Scholar]
- 31.Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2:161–192. [PubMed] [Google Scholar]
- 32.Osmond JM, D. MJ. Brian D, et al. Obesity increases blood pressure, cerebral vascular remodeling, and severity of stroke in the Zucker rat. Hypertension. 2009;53:381–386. doi: 10.1161/HYPERTENSIONAHA.108.124149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deutsch C, Portik-Dobos V, Smith AD, et al. Diet-induced obesity causes cerebral vessel remodeling and increases the damage caused by ischemic stroke. Microvasc Res. 2009;78:100–106. doi: 10.1016/j.mvr.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weisbrod RM, Shiang T, Al Sayah L, et al. Arterial stiffening precedes systolic hypertension in diet-induced obesity. Hypertension. 2013;62:1105–1110. doi: 10.1161/hypertensionaha.113.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ciccone M, Vettor R, Pannacciulli N, et al. Plasma leptin is independently associated with the intima-media thickness of the common carotid artery. Int J Obes Relat Metab Disord. 2001;25:805–810. doi: 10.1038/sj.ijo.0801623. [DOI] [PubMed] [Google Scholar]
- 36.Molica F, Morel S, Kwak BR, et al. Adipokines at the crossroad between obesity and cardiovascular disease. Thromb Haemost. 2015;113:553–566. doi: 10.1160/th14-06-0513. [DOI] [PubMed] [Google Scholar]
- 37.Festa A, D’Agostino RJ, Williams K, et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord. 2001;25:1407–1415. doi: 10.1038/sj.ijo.0801792. [DOI] [PubMed] [Google Scholar]
- 38.Chudek J, Wiecek A. Adipose tissue, inflammation and endothelial dysfunction. Pharmacol Rep. 2006;58(Suppl):81–88. [PubMed] [Google Scholar]
- 39.Rajsheker S, David M, Al B, et al. Crosstalk between perivascular adipose tissue and blood vessels. Curr Opin. 2010;10:191–196. doi: 10.1016/j.coph.2009.11.005.Crosstalk. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phillips CM. Metabolically healthy obesity: definitions, determinants and clinical implications. Rev Endocr Metab Disord. 2013;14:219–227. doi: 10.1007/s11154-013-9252-x. [DOI] [PubMed] [Google Scholar]
- 41.Szasz T, Webb RC, Clinton WR. Perivascular adipose tissue: more than just structural support. Clin Sci (Lond) 2012;122:1–12. doi: 10.1042/CS20110151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheranov SY, Jaggar JH. TNF-alpha dilates cerebral arteries via NAD(P)H oxidase-dependent Ca2+ spark activation. Am J Physiol Cell Physiol. 2006;290:C964–C971. doi: 10.1152/ajpcell.00499.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Henry RMA, J. KP. M. DJ et al. Carotid arterial remodeling: a maladaptive phenomenon in type 2 diabetes but not in impaired glucose metabolism: the Hoorn study. Stroke. 2004;35:671–676. doi: 10.1161/01.STR.0000115752.58601.0B. [DOI] [PubMed] [Google Scholar]
- 44.Institoris A, Lenti L, Domoki F, et al. Cerebral microcirculatory responses of insulin-resistant rats are preserved to physiological and pharmacological stimuli. Microcirculation. 2012;19:749–756. doi: 10.1111/j.1549-8719.2012.00213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Siró P, Molnár C, Katona É, et al. Carotid intima-media thickness and cerebrovascular reactivity in long-term type 1 diabetes mellitus. J Clin Ultrasound. 2009;37:451–456. doi: 10.1002/jcu.20617. [DOI] [PubMed] [Google Scholar]
- 46.Schunkert H, Susanne M, Jens H, et al. The correlation between waist circumference and ESC cardiovascular risk score: data from the German metabolic and cardiovascular risk project (GEMCAS) Clin Res Cardiol. 2008;97:827–835. doi: 10.1007/s00392-008-0694-1. [DOI] [PubMed] [Google Scholar]
- 47.Efstathiou SP, Tsioulos DI, Tsiakou AG, et al. Plasma adiponectin levels and five-year survival after first-ever ischemic stroke. Stroke. 2005;36:1915–1919. doi: 10.1161/01.STR.0000177874.29849.f0. [DOI] [PubMed] [Google Scholar]
- 48.Bloemer J, Pinky PD, Govindarajulu M, et al. Role of adiponectin in central nervous system disorders. Neural Plast. 2018. 10.1155/2018/4593530. [DOI] [PMC free article] [PubMed]
- 49.Gorgui J, Gasbarrino K, Georgakis MK, et al. Circulating adiponectin levels in relation to carotid atherosclerotic plaque presence, ischemic stroke risk, and mortality: a systematic review and meta-analyses. Metabolism. 2017;69:51–66. doi: 10.1016/j.metabol.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 50.Kohara K, Ochi M, Okada Y, et al. Clinical characteristics of high plasma adiponectin and high plasma leptin as risk factors for arterial stiffness and related end-organ damage. Atherosclerosis. 2014;235:424–429. doi: 10.1016/j.atherosclerosis.2014.05.940. [DOI] [PubMed] [Google Scholar]
- 51.Korda M, Kubant R, Patton S, Malinski T. Leptin-induced endothelial dysfunction in obesity. Am J Physiol Heart Circ Physiol. 2008;295:H1514–H1521. doi: 10.1152/ajpheart.00479.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aizawa-Abe M, Ogawa Y, Masuzaki H, et al. Pathophysiological role of leptin in obesity-related hypertension. J Clin Invest. 2000;105:1243–1252. doi: 10.1172/JCI8341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Beltowski J. Leptin and atherosclerosis. Atherosclerosis. 2005;189:47–60. doi: 10.1016/j.atherosclerosis.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 54.Hamner JW, Tan CO, Ozan TC. Relative contributions of sympathetic, cholinergic, and myogenic mechanisms to cerebral autoregulation. Stroke. 2014;45:1771–1777. doi: 10.1161/strokeaha.114.005293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barnes MJ, McDougal DH. Leptin into the rostral ventral lateral medulla (RVLM) augments renal sympathetic nerve activity and blood pressure. Front Neurosci. 2014;8:232. doi: 10.3389/fnins.2014.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hay-Schmidt A, Helboe L, Larsen PJ. Leptin receptor immunoreactivity is present in ascending serotonergic and catecholaminergic neurons of the rat. Neuroendocrinology. 2001;73:215–226. doi: 10.1159/000054638. [DOI] [PubMed] [Google Scholar]
- 57.Singhal A, Farooqi IS, Cole TJ, et al. Influence of leptin on arterial distensibility: a novel link between obesity and cardiovascular disease? Circulation. 2002;106:1919–1924. doi: 10.1161/01.CIR.0000033219.24717.52. [DOI] [PubMed] [Google Scholar]
- 58.Schäfer K, Martin H, Colin G, et al. Leptin promotes vascular remodeling and neointimal growth in mice. Arterioscler Thromb Vasc Biol. 2004;24:112–117. doi: 10.1161/01.ATV.0000105904.02142.e7. [DOI] [PubMed] [Google Scholar]
- 59.Schroeter MR, Eschholz N, Herzberg S, et al. Leptin-dependent and leptin-independent paracrine effects of perivascular adipose tissue on neointima formation. Arter Thromb Vasc Biol. 2013;33:980–987. doi: 10.1161/atvbaha.113.301393. [DOI] [PubMed] [Google Scholar]
- 60.Shibata R, Ouchi N, Ohashi K, Murohara T. The role of adipokines in cardiovascular disease. J Cardiol. 2017;70:329–334. doi: 10.1016/j.jjcc.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 61.Li F, Li Y, Duan Y, et al. Myokines and adipokines: involvement in the crosstalk between skeletal muscle and adipose tissue. Cytokine Growth Factor Rev. 2017;33:73–82. doi: 10.1016/j.cytogfr.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 62.Chung HS, Choi KM. Adipokines and myokines: a pivotal role in metabolic and cardiovascular disorders. Curr Med Chem. 2018;25:2401–2415. doi: 10.2174/0929867325666171205144627. [DOI] [PubMed] [Google Scholar]
- 63.Jiménez Caballero PE, Coloma Navarro R, Ayo Martín O, Segura MT. Cerebral hemodynamic changes at basilar artery in obstructive sleep apnea syndrome after continuous positive airway pressure treatment. J Stroke Cerebrovasc Dis. 2012;22:1–6. doi: 10.1016/j.jstrokecerebrovasdis.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 64.Jiménez Caballero PE, Coloma Navarro R, Segura Martín T, Ayo MO. Cerebral hemodynamic changes at basilar artery in patients with obstructive sleep apnea syndrome. A case-control study. Acta Neurol Scand. 2014;129:80–84. doi: 10.1111/ane.12156. [DOI] [PubMed] [Google Scholar]
- 65.Segura T, Serena J, Plaza I, et al. Normal values for transcranial doppler studies in our medium. Neurologia. 1999;14:437–443. [PubMed] [Google Scholar]
- 66.Alosco ML, Spitznagel MB, Raz N, et al. Obesity interacts with cerebral hypoperfusion to exacerbate cognitive impairment in older adults with heart failure. Cerebrovasc Dis Extra. 2012;2:88–98. doi: 10.1159/000343222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ferreira I, Beijers HJ, Schouten F, et al. Clustering of metabolic syndrome traits is associated with maladaptive carotid remodeling and stiffening: a 6-year longitudinal study. Hypertension. 2012;60:542–549. doi: 10.1161/HYPERTENSIONAHA.112.194738. [DOI] [PubMed] [Google Scholar]
- 68.Iglesias MJ, Eiras S, Pineiro R, et al. Gender differences in adiponectin and leptin expression in epicardial and subcutaneous adipose tissue. Findings in patients undergoing cardiac surgery. Rev Esp Cardiol. 2006;59:1252–1260. doi: 10.1157/13096596. [DOI] [PubMed] [Google Scholar]
- 69.Sparks LM, Pasarica M, Sereda O, et al. Effect of adipose tissue on the sexual dimorphism in metabolic flexibility. Metabolism. 2009;58:1564–1571. doi: 10.1016/j.metabol.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 70.Licinio J, Negrão AB, Mantzoros C, et al. Sex differences in circulating human leptin pulse amplitude: clinical implications. J Clin Endocrinol Metab. 1998;83:4140–4147. doi: 10.1210/jcem.83.11.5291. [DOI] [PubMed] [Google Scholar]
- 71.Luque-Ramírez M, Martínez-García MÁ, Montes-Nieto R, et al. Sexual dimorphism in adipose tissue function as evidenced by circulating adipokine concentrations in the fasting state and after an oral glucose challenge. Hum Reprod. 2013;28:1908–1918. doi: 10.1093/humrep/det097. [DOI] [PubMed] [Google Scholar]
- 72.Petersen KS, Blanch N, Keogh JB, Clifton PM. Effect of weight loss on pulse wave velocity: systematic review and meta-analysis. Arterioscler Thromb Vasc Biol. 2015;35(1):243–252. doi: 10.1161/ATVBAHA.114.304798. [DOI] [PubMed] [Google Scholar]
- 73.Montero D, Roberts CK, Vinet A, et al. Effect of aerobic exercise training on arterial stiffness in obese populations : a systematic review and meta-analysis. Sports Med. 2014;44(6):833–843. doi: 10.1007/s40279-014-0165-y. [DOI] [PubMed] [Google Scholar]


