Abstract
Entrapment neuropathy around elbow is a common cause of disability across all age groups. The major nerves that traverse the elbow are ulnar, median and radial nerves and their branches. Cubital tunnel syndrome leading to ulnar nerve compression can often present with significant pain, paresthesia or weakness. Median and Radial nerve compression around the elbow, albeit less frequent, can also lead to significant morbidity and must be kept in the differential diagnosis when dealing with patients complaining of persistent pain around the elbow and weakness of forearm/hand muscles. Electrodiagnostic studies can be a useful adjunct to clinical examination, to help localize the site and quantify the grade of compression. Management should involve a trial of conservative treatment and failing that, surgical treatment should be considered. We hereby provide an overview of nerve entrapments around the elbow including their applied anatomy, etiology, clinical assessment and overview of the current concepts in surgical treatment.
Keywords: Nerve entrapment, Elbow, Radial tunnel syndrome, Cubital tunnel
1. Introduction
Ulnar nerve compression is the second most frequent site for nerve entrapment in the upper limb but all nerves traversing the elbow are at risk of entrapment including radial, posterior interosseous, median and anterior interosseous nerve.1 Patients initially present with sensory symptoms and/or pain that can gradually progress to motor weakness resulting in significant disability.
This article aims to review the various entrapment neuropathies around the elbow and their management.
1.1. Ulnar nerve(Cubital tunnel syndrome)
Compression of the ulnar nerve at the elbow joint is often referred to as cubital tunnel syndrome.
1.1.1. Anatomy
The ulnar nerve lies behind the brachial artery in the anterior compartment of the upper half of the arm. It pierces the medial intermuscular septum, about two-thirds of the way down the arm to enter the posterior compartment, where it lies adjacent to triceps muscle. It then travels on the posterior aspect of the medial epicondyle of the humerus, where it is subcutaneous in location. The cubital tunnel is a fibro-osseous tunnel with olecranon process laterally, posterior cortex medially, elbow joint capsule and posterior bundle of medial collateral ligament anteriorly and the ligament of Osborne posteriorly. In the forearm, the nerve passes through two heads of the Flexor Carpi Ulnaris (FCU) running deep to the muscle alongside the ulna.
1.1.2. Etiology
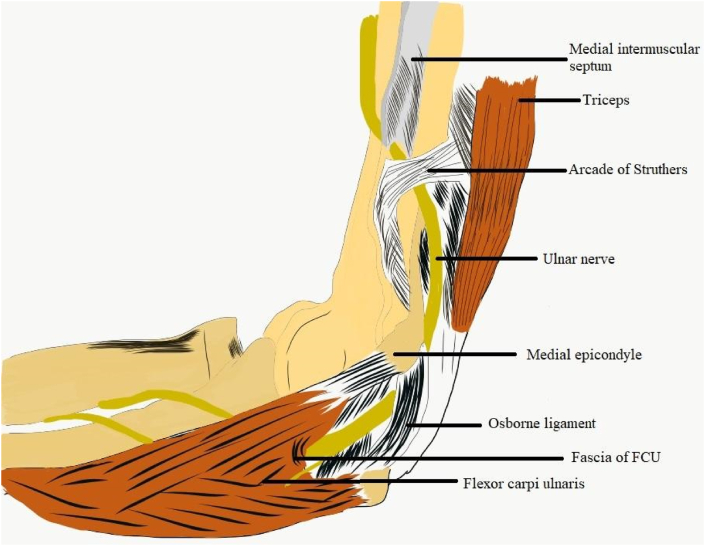
The ulnar nerve can be compressed at five potential sites around the elbow (Fig. 1):
-
●
Medial intermuscular septum, when it enters from anterior to posterior compartment
-
●
Arcade of Struthers-a fibrous band consisting of medial head of triceps and its expansion extending into the medial intermuscular septum, 6–10 cm proximal to medial epicondyle
-
●
Exostoses or osteophytes over the medial epicondyle
-
●
Osborne ligament/fascia (fibrous band between ulnar and humeral heads of FCU that forms the roof of the cubital tunnel)
-
●
Two heads of FCU muscle/FCU aponeurosis
Fig. 1.
Ulnar nerve entrapment sites around elbow.
Ulnar nerve can also be compressed by valgus deformity/olecranon bursitis or synovitis around medial epicondyle in patients of rheumatoid arthritis of elbow.
Among these, the most common site of compression is between the two heads of FCU.2
The ulnar nerve becomes taut in flexion and continues to be stretched as the area in the cubital tunnel decreases beyond 90° of flexion.3 When the elbow is bent, tensile load on the nerve increases and pressure within the cubital tunnel can be as high as 20 times of that at rest.4 Baseball pitchers, truck divers or office workers whose job involve repetitive or prolonged flexion of elbow, are more likely to develop ulnar neuropathy.5 Keeping the arm under the head during sleep with shoulder abducted and elbow acutely flexed, can decrease nerve conduction velocity and cause paresthesias in the ulnar nerve distribution in the hand.6
Ulnar nerve subluxation has been reported as a risk factor for nerve entrapment, but without any conclusive evidence. However, some surgeons advocate anterior transposition if nerve instability is noted intra-operatively.7,8
1.1.3. Clinical features
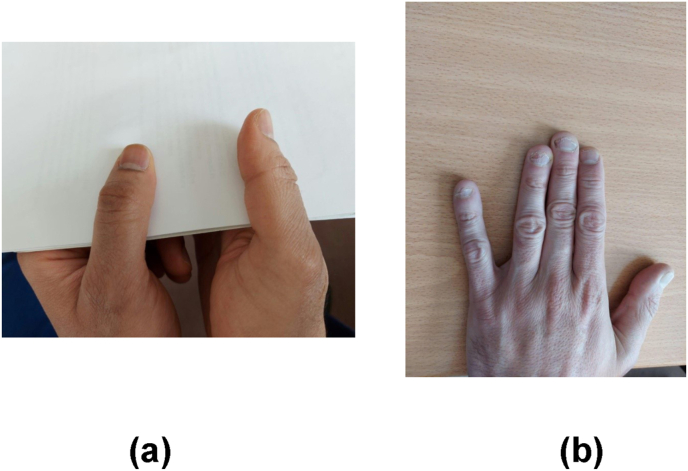
Patients initially present with sensory symptoms such as paresthesia, numbness and pain along the distribution of the nerve, predominantly in the little finger and ulnar border of the ring finger. If left untreated, it can progress to weakness and complete loss of sensation distal to the site of compression. Hypoesthesia in the ulnar nerve distribution and positiveTinel's test over the cubital tunnel are helpful in establishing the diagnosis. Motor involvement manifests as wasting of first dorsal interosseous and clawing of little and ring fingers which is suggestive of severe compression.9 Froment's sign (Fig. 2a) tests the power of adductor pollicis and first dorsal interosseous. It is elicited by asking the patient to grasp a paper between the ulnar border of thumb and radial border of index finger. Inability to hold the paper with adducted thumb and flexion of thumb interphalangeal joint (IPJ) due to flexor pollicis longus recruitment signifies a positive test. Wartenberg's sign (Fig. 2b) is an involuntary abduction (abduction posture) of little finger when asked to hold fingers together, caused by unopposed action of extensor digitiminimi due to weakness of ulnar nerve innervated intrinsic hand muscles-in particular the palmar interossei muscle to the little finger.
Fig. 2.
(a) Froment's sign- FPL recruitment (Left thumb) to grasp paper due to weakness of adductor pollicis and first dorsal interossei(b) Wartenburgsign-abduction of little finger due to unopposed action of extensor digitiminimi.
The ulnar paradox is:the more distal the lesion, the worse is the clawing.10 It occurs due to sparing of the flexor digitorum profundus in more distal lesions.
1.1.4. Investigations
Nerve conduction studies (NCS) and Electromyography (EMG) are useful investigations to confirm the diagnosis. Motor Nerve Conduction Velocity (NCV) less than 50 m/s and a decrease in compound muscle action potential (CMAP) peak amplitude (less than 20% of the normal contralateral limb)using moderate elbow flexion between 70 and 90°, are suggestive of ulnar nerve entrapment.11
Ultrasound imaging in real-time flexion and extension is a dynamic investigation to evaluate nerve motion and its relation to surrounding muscles and tendons such as the medial head of triceps.12 Nerve swelling seen in ultrasound as compared to control subjects, is a reliable diagnostic tool indicating nerve derangement.13, 14, 15 Ulnar nerve in the opposite elbow should be scanned in the same degree of flexion before reaching a conclusion.
Plain radiographs in anteroposterior, lateral and cubital views to assess osteophytic narrowing of the cubital tunnel are useful. Magnetic Resonance Imaging (MRI) in elbow flexion would be helpful if a space occupying lesion is suspected. It can also diagnose a snapping ulnar nerve.16 A signal hyperintensity on T2 weighted images in MRI and nerve swelling represents a symptomatic ulnar nerve caused due to compression. However, some studies show that 60% of asymptomatic elbows also show signal hyperintensity in the ulnar nerve in MRI.17
1.1.5. Treatment
1.1.5.1. Nonoperative treatment
Patients with mild to moderate symptoms often respond well to nonoperative management including patient education, non-steroidal anti-inflammatory drugs (NSAIDS), night splints and activity modification.18,19
Svernolov et al. managed 3 groups of patients nonoperatively: the first group was provided a nightsplint, the second group was treated with nerve gliding exercises and the third group was educated for activity modification. They found that 89.5% of patients experienced improvement in symptoms with no difference between the three groups.20
Avoidance of provocative activities such as prolonged periods of elbow flexion has shown spontaneous recovery of mild and/or intermediate symptoms.21
1.1.5.2. Surgical treatment
Indications for surgery include failure of nonoperative management, presence of muscle weakness/wasting and evidence of severe compression on NCS. Decompression of the nerve has been described using open, mini open or endoscopic techniques.
The open technique is carried out by a 10 cm longitudinal incision along the course of the ulnar nerve between the medial epicondyle and olecranon, usually starting 5 cm above medial epicondyle. Structures released from proximal to distal are medial intermuscular septum, arcade of Struthers, Osborne's ligament and FCU fascia. Care should be taken to only release the superficial fascia over the nerve and the vascular bed of the nerve should not be disturbed. The nerve is examined for subluxation at the end of the procedure and significant instability on flexion can be an indication for anterior transposition, especially in patients with muscle atrophy.
The mini open technique is more popularand is the senior author's treatment of choice. Various authors have published their clinical outcomes demonstrating excellent results using a small skin incision but ensuring a complete deep release of the nerve.22,23 Main advantages of this technique is a shorter scar with reduced surgical site tenderness.
Endoscopic release of the nerve has been reported with satisfactory outcomes. Smeraglia et al.24 conducted a systematic review and concluded that the main advantages of the endoscopic technique are shorter time to return to work and better cosmetic appearance of the scar. However, increased risk of postoperative haematoma formation has been reported with this technique.1
Anterior transposition of the nerve is also a well described surgical technique, but of doubtful additional benefit. Simple decompression of ulnar nerve provides excellent results in relieving symptoms without disturbing its blood supply. A meta-analysis of studies comparing simple decompression versus simple decompression and transposition found no difference in outcomes. A Cochrane review has also shown no difference between simple decompression and transposition of the ulnar nerve for both clinical and neurophysiological improvement.1 It also found an increased risk of superficial and deep wound infections in patients who had transposition. The main indication for transposition is the presence of ulnar nerve instability noted intra-operatively, especially in patients with muscle atrophy and presence of medial epicondyle osteophytes/osteoarthritic changes. Anterior transposition can be performed using subcutaneous, intramuscular or submuscular techniques. No significant difference in outcomes has been found between the three techniques. Subcutaneous transposition in slim patients can be associated with a visible, palpable and irritable ulnar nerve. Intramuscular and submuscular approaches are associated with a risk of recurrent compression by the muscle or its fascial bands.25,26
Medial epicondylectomy is another technique which has been described, with a view to theoretically eliminate traction of the nerve and reduce strain during elbow flexion with satisfactory outcomes. However, complications such as medial elbow pain, nerve subluxation, flexor-pronator weakness, flexion contracture and medial elbow instability due to injury to anterior band of MCLhave been reported. To avoid these complications, a partial medial epicondylectomy has been advocated which did not show any case of instability in a series of 80 patients27
Outcomes of surgery are excellent in patients with mild to moderate compression. However, the results can be disappointing in patients with prolonged or advanced nerve compression. Unrealistic patient expectations can contribute to poor outcomes of surgery. Patients should be warned that the recovery of pain, paresthesia, pinch and grip strength can be a slow and gradual process and the improvement may continue for 12 months.28 Tong et al. reported that patients with severe compression and absent sensory nerve action potential had worse outcomes.29
Failure of decompression surgery can be due to late presentation, advanced compression, inadequate release, ulnar nerve instability, double crush or iatrogenic nerve injury. Recurrence of cubital tunnel syndrome can be due to secondary compression, perineurial scarring, elbow stiffness/osteoarthritis and ulnar nerve instability.30 Revision surgery for failure or recurrence often includes neurolysis±anterior transposition depending on the cause. Outcomes of revision surgery can be unpredictable, and most patients report ongoing symptoms. Grandizio et al. reported improvement in pain and paresthesia following revision decompression. Patients with severe motor neuropathy and older age have unfavourable prognosis.30
1.2. Radial nerve
Whilst the ulnar nerve is most commonly involved, both the radial nerve and the posterior interosseous nerves (PIN) are also susceptible to compression around the elbow.
1.2.1. Anatomy
The radial nerve arises from the posterior cord of the brachial plexus. In the lower arm, it passes through the lateral intermuscular septum from the posterior to the lateral compartment of the arm between the brachialis and brachioradialis muscles. The nerve then passes anterior to the lateral epicondyle into the cubital fossa and forearm. It divides into the PIN which is a motor branch passing within the heads of the supinator muscle and innervates the muscles of the posterior compartment of the forearm(Fig. 2). The superficial branch follows the radial artery distally to the wrist where it terminates into sensory branches.
1.2.2. Etiology
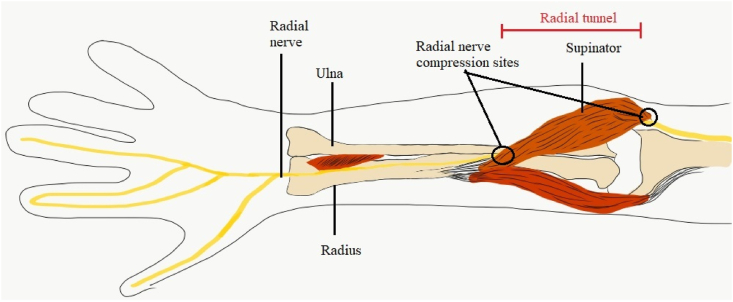
Proximal to the elbow, the radial nerve can be compressed by overuse, direct trauma and/or haematoma. Additionally, the fibrous arch of the long head or lateral head of triceps can cause the entrapment of radial nerve above the elbow. More commonly, it is compressed just proximal to supinator muscle or in the radial tunnel (Fig. 3).
Fig. 3.
Radial nerve entrapment:Common sites: proximal to supinator muscle and in the radial tunnel.
1.2.3. Clinical features
Patients present with gradual sensory loss/alteration over the dorsal aspect of the fingers and hand, the dorsal first web space (autonomous zone) and weakness of wrist and finger extension. Patients with severe compression can develop a wrist drop. Assessment of motor function can be done by examining for resisted dorsiflexion of the wrist while palpating the tendons of extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) which inserts to the base of second and third metacarpal, respectively. Brachioradialis (BR) is tested by flexing a semi prone forearm against resistance.
1.2.4. Investigations
Diagnosis can be confirmed by EMG studies. MRI is useful in detecting nerve changes and diagnosing small tumors, masses, aneurysms or compressive synovitis.
1.2.5. Treatment
A trial of nonoperativetreatment using splints/activitymodification/NSAIDS should be tried initially.31,32 Surgical exploration and decompression should be considered if nonoperative treatment is unsuccessful. The return of function follows a pattern with brachioradialis and ECRL recovering first, followed by extensor pollicis longus and extensor Indicis.33
1.3. Posterior interosseous nerve(PIN)/radial tunnel syndrome(RTS)
PIN syndrome and RTS are often described as interchangeable terms but in the senior author's opinion, RTS usually refers to Radial nerve/PIN compression at the proximal part of the radial tunnel and presents predominantly with lateral elbow pain. PIN syndrome, on the other hand, is usually associated with neurological symptoms and signs.
1.3.1. Etiology
The anatomic radial tunnel extends from the radial head to the inferior border of the supinator muscle. The causes ofPIN syndrome include trauma, space occupying lesions like lipomas, synovitis (eg.in rheumatoid arthritis), brachial neuritis and spontaneous compression from muscle hypertrophy in bodybuilders. Compression of the posterior interosseous nerve can occur at one of the following locations within the radial tunnel:
-
●
Fibrous bands/osteophytes between the brachioradialis muscle and joint capsule at the level of radial head
-
●
Leash of Henry, an arcade of anastomosing branches of the radial Recurrent artery, distal to the radial head
-
●
Tendinous edge of the overlying ECRBmuscle
-
●
Arcade of Frohse along the proximal and distal aspect of the Supinatormuscle.
Above cause can be summarized in the mnemonic (FREAS).34
1.3.2. Clinical features
Radial tunnel symptoms (RTS) can mimic lateral epicondylitis (burning sensation over the lateral aspect of the forearm). Tenderness 2–3 cm distal to the radial head in line with the radial nerve and not over the lateral epicondyle, can help differentiate RTS from lateral epicondylitis. In RTS, the pain is in the region of Arcade of Frohse, is continuous and aching in nature causing discomfort during fine movements like writing. Sarhadi et al.35 suggested that the diagnosis of radial tunnel syndrome included at least two of the three objective signs: resisted supination causing pain, resisted middle finger extension and pressure along the radial tunnel reproducing patient symptoms. Diagnosis is confirmed by resolution of these signs after infiltration of local anesthetic solution in the tender area.
PIN syndrome is associated with pain as well as weakness of thumb and finger extensors. Thumb extension is tested by asking the patient to do a ‘hitchhiker’ sign which involves flexion of all fingers and hyperextension of thumb. Inability to extend the thumb indicates a PIN palsy.
1.3.3. Investigations
EMG studies are diagnostic for PIN syndrome but are often normal in RTS. Radiographs are useful to rule out fracture, healing callus or bone tumour. Ultrasound can help to visualise injured nerves with axonal swelling, hypoechogenicity of the nerve, loss of continuity of the nerve bundle, neuroma formation and partial laceration of the nerve. MRI is useful in detecting nerve changes and diagnosing small tumors, masses, aneurysms or compressive synovitis.
1.3.4. Treatment
Conservative treatment entails avoidance of prolonged elbow flexion and pronation of wrist alongwith splints/activity modification and NSAIDS.31,32 In Sarhadi et al.‘s series, 16 of 26 cases resolved with conservative management and 9 underwent decompression surgery; 78% of total patients reported complete pain relief.35Success rates can be as high as 90% in 3–4 months with nonoperative management. Steroid infiltration into the pronator region and local anaesthetic administered in the radial tunnel has shown good results in relieving symptoms.34 One single injection of 2 ml of 1% lidocaine and 40 mg triamcinolone achieved a pain relief in 72% patients after 6 weeks and in 64% patients for a period of more than 2 years.35
Surgical decompression is indicated after failure of non-operative treatment. The posterior interosseous nerve can be accessed anteriorly or posteriorly using either the dorsal Henry approach (between ECRB and extensor digitorum) or transmuscular (brachioradialis splitting) approach through the interval between the ECRL and BR. Nerve proximal to the compression may be swollen (pseudoneuroma).36 Care must be taken to ensure decompression of both posterior interosseous nerve and superficial branch of radial nerve.37 Decompression surgery has shown good outcomes in cases of isolated RTS.32,38
1.4. Median nerve
Median nerve compression at the elbow can lead to pronator syndrome oranterior interosseous nerve syndrome (Kiloh-Nevin's syndrome).
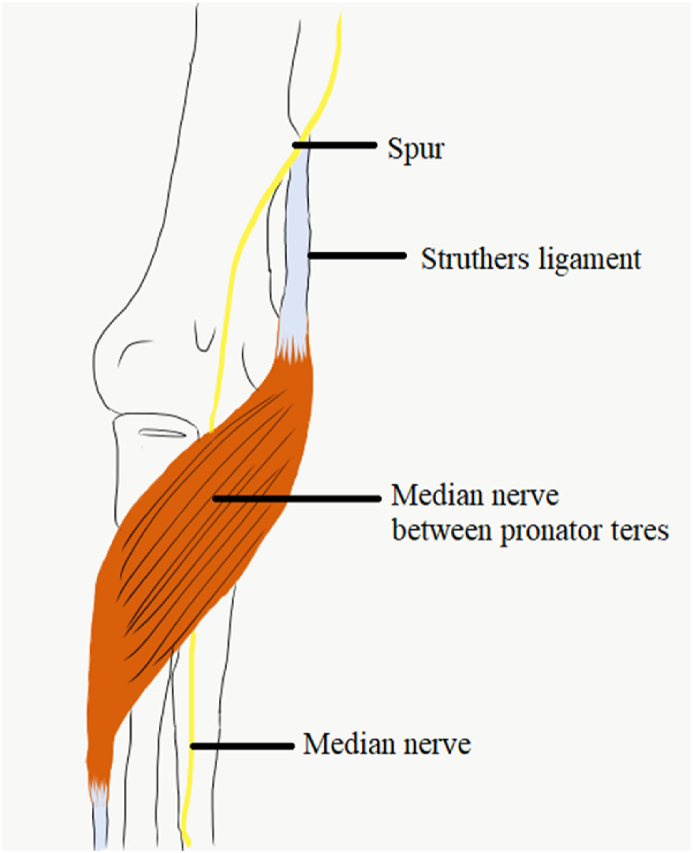
1.4.1. Sites of compression
Pronator syndrome can occur at one of five locations:(a) supracondylar process on distal medial humerus, (b)ligament of Struthers which extends from the anteromedial aspect of distal humerus to the medial epicondyle(c)thickened biceps aponeurosis (lacertus fibrosus) in proximal elbow, (d) between the superficial and deep heads of pronator teres and by a (e) thickened edge of Flexor digitorum superficialis in proximal forearm(Fig. 4).
Fig. 4.
The course of Median nerve in relation to pronator teres.
Anterior interosseous nerve (AIN) can be compressed by the deep head of pronator teres or the fibrous arch of Flexor digitorum superficialis. It is important to distinguish this from Parsonage Turner syndrome which is preceded by a viral prodrome and sometimes intense shoulder pain.39
1.4.2. Clinical features
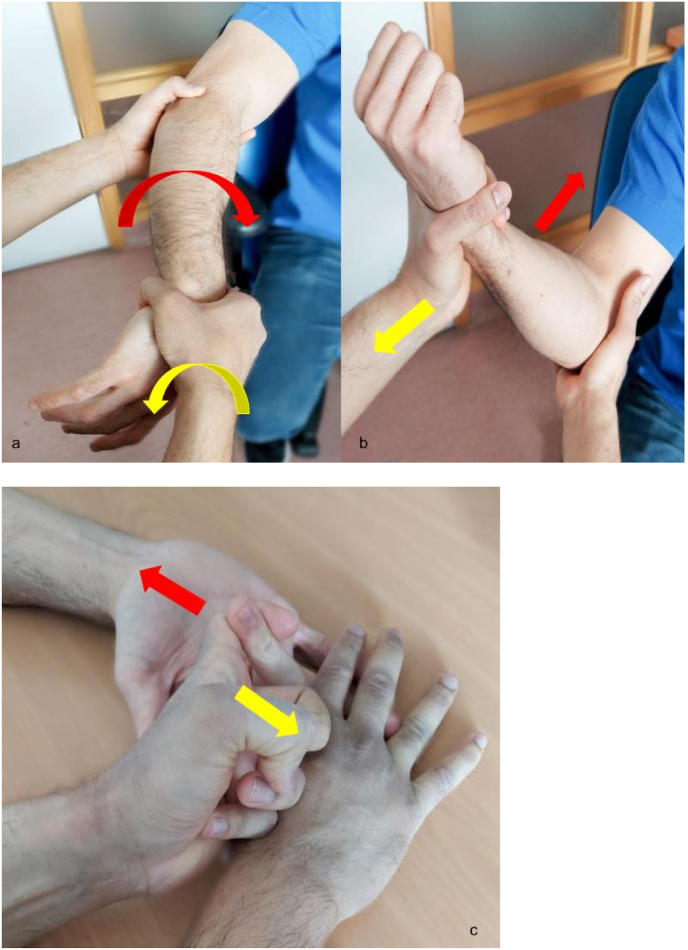
Pronator syndrome usually presents with pain & paresthesia in the flexor aspect of the elbow and forearm. Thumb, index, middle and ring finger can have reduced sensations which maybe misinterpreted as carpal tunnel syndrome. Provocative tests include pain on resisted pronation with elbow extended, pain on resisted elbow flexion and forearm supination and pain on resisted middle finger proximal interphalangeal (PIP) joint flexion (Fig. 5).
Fig. 5.
(a)Resisted pronation of forearm. (b) Resisted flexion with forearm supinated. (c) Resisted middle finger flexion at proximal interphalangeal joint.
Some patients can develop mild weakness and wasting of the median nerve innervated muscles. The pronator teres is spared as it is innervated by the median nerve before it pierces into the muscle. Muscles involved are abductor polllicisbrevis (APB) and flexor pollicis longus (FPL) with occasional involvement of flexor digitorum profundus (FDP) and opponens pollicis (OP).40
AINsyndrome is manifested by weakness and inability to pinch the thumb and index finger together (‘OK’ sign) due to weakness of FDP slip to index and middle finger and FPL. The patients can lose the ability to button their shirts or turn on their car keys. Involvement of proprioceptive fibers can lead to deep forearm discomfort. A positive Tinel sign over the elbow and proximal forearm can sometimes be elicited on clinical examination.
1.4.3. Investigations
Nerve conduction studies are helpful to confirm the diagnosis. A supracondylar process may be seen on a plain radiograph and should be excluded. An EMG study to confirm the involvement of the FPL or pronator quadratus should be performed in suspected anterior interosseous nerve syndrome.
1.4.4. Treatment
Non operative treatment is usually successful in relieving symptoms in a majority of cases. Rodner et al. recommended decompression surgery if there are persistent symptoms for >6 months in patients with Pronator Syndrome or a minimum of 12 months with no signs of motor improvement in AIN syndrome.41
Decompression surgery can be performed with a “lazy-S”-shaped skin incision from 3 cm distal to the medial epicondyle over the flexor/pronator muscles. Bicipital aponeurosis is released, and the median nerve exposed after splitting pronator teres. Distal to the elbow, AIN is the only nerve that branches off the radial side of the median nerve which makes it easier to identify it intra-operatively.42
Hagert et al. described a modified open procedure with the patient awake, without a tourniquet, in which a 2–3 cm transverse incision is madein the region of cubital fossa along the flexion crease. Landmarks for incision are from 1 cm medial of biceps tendon to 2 cm lateral of the medial epicondyle. Fascia of the pronator teres is released to expose the lacertus fibrosus. FPL and FDP are tested intraoperatively in an awake patient to detect improvement in the weakness which may or may not be evident at this stage.43 Thorough decompression of all median nerve branches should be performed. Meticulous haemostasis is done to prevent post-operative haematoma.
Author statement
Arjun Ajith Naik and Akshdeep Bawa were involved in literature search and paper writing, Anand Arya and Abhinav Gulihar were involved in expert opinion, practical aspects of surgeries and paper editing.
References
- 1.Caliandro P., La Torre G., Padua R., Giannini F., Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2016;11 doi: 10.1002/14651858.CD006839.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Posner M.A. Compressive neuropathies of the ulnar nerve at the elbow and wrist. Instr Course Lect. 2000;49:305–317. [PubMed] [Google Scholar]
- 3.James J., Sutton L.G., Werner F.W., Basu N., Allison M.A., Palmer A.K. Morphology of the cubital tunnel: an anatomical and biomechanical study with implications for treatment of ulnar nerve compression. J Hand Surg Am. 2011;36(12):1988–1995. doi: 10.1016/j.jhsa.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Gellman H. Compression of the ulnar nerve at the elbow: cubital tunnel syndrome. Instr Course Lect. 2008;57:187–197. [PubMed] [Google Scholar]
- 5.Descatha A., Leclerc A., Chastang J.-F., Roquelaure Y., Study Group on Repetitive Work Incidence of ulnar nerve entrapment at the elbow in repetitive work. Scand J Work Environ Health. 2004;30(3):234–240. doi: 10.5271/sjweh.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu K., Robinson L.R. Effect of shoulder and elbow position on ulnar nerve conduction. Muscle Nerve. 2019;60(1):88–90. doi: 10.1002/mus.26489. [DOI] [PubMed] [Google Scholar]
- 7.DeGeorge B.R., Kakar S. Decision-making factors for ulnar nerve transposition in cubital tunnel surgery. J Wrist Surg. 2019;8(2):168–174. doi: 10.1055/s-0038-1665548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang P. The blocking flap for ulnar nerve instability after in situ release: technique and a grading system of ulnar nerve instability to guide treatment. Tech Hand Up Extrem Surg. 2017;21(4):137–142. doi: 10.1097/BTH.0000000000000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutts S. Cubital tunnel syndrome. Postgrad Med. 2007;83(975):28–31. doi: 10.1136/pgmj.2006.047456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strohl A.B., Zelouf D.S. Ulnar tunnel syndrome, radial tunnel syndrome, anterior interosseous nerve syndrome, and pronator syndrome. J Am Acad Orthop Surg. 2017;25(1):e1–e10. doi: 10.5435/JAAOS-D-16-00010. [DOI] [PubMed] [Google Scholar]
- 11.Landau M.E., Campbell W.W. Clinical features and electrodiagnosis of ulnar neuropathies. Phys Med Rehabil Clin. 2013;24(1):49–66. doi: 10.1016/j.pmr.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Jacobson J.A., Jebson P.J., Jeffers A.W., Fessell D.P., Hayes C.W. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography--report of three cases. Radiology. 2001;220(3):601–605. doi: 10.1148/radiol.2202001723. [DOI] [PubMed] [Google Scholar]
- 13.Kim S., Choi J.-Y., Huh Y.-M. Role of magnetic resonance imaging in entrapment and compressive neuropathy - what, where, and how to see the peripheral nerves on the musculoskeletal magnetic resonance image: part 1. Overview and lower extremity. Eur Radiol. 2007;17(1):139–149. doi: 10.1007/s00330-006-0179-4. [DOI] [PubMed] [Google Scholar]
- 14.Thoirs K., Williams M.A., Phillips M. Ultrasonographic measurements of the ulnar nerve at the elbow: role of confounders. J Ultrasound Med. 2008;27(5):737–743. doi: 10.7863/jum.2008.27.5.737. [DOI] [PubMed] [Google Scholar]
- 15.Yoon J.S., Walker F.O., Cartwright M.S. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve. 2008;38(4):1231–1235. doi: 10.1002/mus.21094. [DOI] [PubMed] [Google Scholar]
- 16.Spinner R.J., Hayden F.R., Hipps C.T., Goldner R.D. Imaging the snapping triceps. AJR Am J Roentgenol. 1996;167(6):1550–1551. doi: 10.2214/ajr.167.6.8956595. [DOI] [PubMed] [Google Scholar]
- 17.Husarik D.B., Saupe N., Pfirrmann C.W.A., Jost B., Hodler J., Zanetti M. Elbow nerves: MR findings in 60 asymptomatic subjects--normal anatomy, variants, and pitfalls. Radiology. 2009;252(1):148–156. doi: 10.1148/radiol.2521081614. [DOI] [PubMed] [Google Scholar]
- 18.Elhassan B., Steinmann S.P. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007;15(11):672–681. doi: 10.5435/00124635-200711000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Hong C.Z., Long H.A., Kanakamedala R.V., Chang Y.M., Yates L. Splinting and local steroid injection for the treatment of ulnar neuropathy at the elbow: clinical and electrophysiological evaluation. Arch Phys Med Rehabil. 1996;77(6):573–577. doi: 10.1016/s0003-9993(96)90297-x. [DOI] [PubMed] [Google Scholar]
- 20.Svernlöv B., Larsson M., Rehn K., Adolfsson L. Conservative treatment of the cubital tunnel syndrome. J Hand Surg Eur Vol. 2009;34(2):201–207. doi: 10.1177/1753193408098480. [DOI] [PubMed] [Google Scholar]
- 21.Palmer B.A., Hughes T.B. Cubital tunnel syndrome. J Hand Surg Am. 2010;35(1):153–163. doi: 10.1016/j.jhsa.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Jeon I.-H., Micić I., Lee B.-W., Lee S.-M., Kim P.-T., StojiljkovićP Simple in situ decompression for idiopathic cubital tunnel syndrome using minimal skin incision. Med Pregl. 2010;63(9-10):601–606. doi: 10.2298/mpns1010601j. [DOI] [PubMed] [Google Scholar]
- 23.Taniguchi Y., Takami M., Takami T., Yoshida M. Simple decompression with small skin incision for cubital tunnel syndrome. J Hand Surg. 2002;27(6):559–562. doi: 10.1054/jhsb.2002.0821. [DOI] [PubMed] [Google Scholar]
- 24.Smeraglia F., Del Buono A., Maffulli N. Endoscopiccubital tunnel release: a systematicreview. Br Med Bull. 2015;116:155–163. doi: 10.1093/bmb/ldv049. [DOI] [PubMed] [Google Scholar]
- 25.Gervasio O., Gambardella G., Zaccone C., Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(1):108–117. doi: 10.1227/01.neu.0000145854.38234.81. discussion 117. [DOI] [PubMed] [Google Scholar]
- 26.Nabhan A., Ahlhelm F., Kelm J., Reith W., Schwerdtfeger K., Steudel W.I. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg. 2005;30(5):521–524. doi: 10.1016/j.jhsb.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Efstathopoulos D.G., Themistocleous G.S., Papagelopoulos P.J., Chloros G.D., Gerostathopoulos N.E., Soucacos P.N. Outcome of partial medial epicondylectomy for cubital tunnel syndrome. Clin Orthop Relat Res. 2006;444:134–139. doi: 10.1097/01.blo.0000201153.36948.29. [DOI] [PubMed] [Google Scholar]
- 28.Ido Y., Uchiyama S., Nakamura K. Postoperative improvement in DASH score, clinical findings, and nerve conduction velocity in patients with cubital tunnel syndrome. Sci Rep. 2016;6:27497. doi: 10.1038/srep27497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tong J.-S., Dong Z., Xu B., Zhang C.-G., Gu Y.-D. Surgical treatment for severe cubital tunnel syndrome with absent sensory nerve conduction. Neural Regen Res. 2019;14(3):519–524. doi: 10.4103/1673-5374.245479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grandizio L.C., Maschke S., Evans P.J. The management of persistent and recurrentcubital tunnel syndrome. J Hand Surg Am. 2018;43(10):933–940. doi: 10.1016/j.jhsa.2018.03.057. [DOI] [PubMed] [Google Scholar]
- 31.Cleary C.K. Management of radial tunnel syndrome: a therapist's clinical perspective. J Hand Ther. 2006;19(2):186–191. doi: 10.1197/j.jht.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 32.Lee J.-T., Azari K., Jones N.F. Long term results of radial tunnel release--the effect of co-existing tennis elbow, multiple compression syndromes and workers' compensation. J Plast ReconstrAesthetSurg. 2008;61(9):1095–1099. doi: 10.1016/j.bjps.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 33.Gragossian A, Varacallo M. Radial nerve injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing. [PubMed]
- 34.Moradi A., Ebrahimzadeh M.H., Jupiter J.B. Radial tunnel syndrome, diagnostic and treatment dilemma. Arch Bone Jt Surg. 2015;3(3):156–162. doi: 10.22038/abjs.2015.4110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarhadi N.S., Korday S.N., Bainbridge L.C. Radial tunnel syndrome: diagnosis and management. J Hand Surg. 1998;23(5):617–619. doi: 10.1016/s0266-7681(98)80015-6. [DOI] [PubMed] [Google Scholar]
- 36.Naam N.H., Nemani S. Radial tunnel syndrome. Orthop Clin N Am. 2012;43(4):529–536. doi: 10.1016/j.ocl.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 37.De Smet L., Van Raebroeckx T., Van Ransbeeck H. Radial tunnel release and tennis elbow: disappointing results? Acta Orthop Belg. 1999;65(4):510–513. [PubMed] [Google Scholar]
- 38.Lawrence T., Mobbs P., Fortems Y., Stanley J.K. Radial tunnel syndrome. A retrospective review of 30 decompressions of the radial nerve. J Hand Surg. 1995;20(4):454–459. doi: 10.1016/s0266-7681(05)80152-4. [DOI] [PubMed] [Google Scholar]
- 39.Schollen W., Degreef I., De Smet L. Kiloh-Nevin syndrome: a compression neuropathy or brachial plexus neuritis? Acta Orthop Belg. 2007;73(3):315–318. [PubMed] [Google Scholar]
- 40.Dididze M., Tafti D., Sherman Al. StatPearls. StatPearls Publishing; Treasure Island (FL): 2021 Jan. Pronator teres syndrome. Updated 2021 Mar 17. Internet. [PubMed] [Google Scholar]
- 41.Rodner C.M., Tinsley B.A., O'Malley M.P. Pronator syndrome and anterior interosseous nerve syndrome. J Am Acad Orthop Surg. 2013;21(5):268–275. doi: 10.5435/JAAOS-21-05-268. [DOI] [PubMed] [Google Scholar]
- 42.Ulrich D., Piatkowski A., Pallua N. Anterior interosseous nerve syndrome: retrospective analysis of 14 patients. Arch Orthop Trauma Surg. 2011;131(11):1561–1565. doi: 10.1007/s00402-011-1322-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hagert E. Clinical diagnosis and wide-awake surgical treatment of proximal median nerve entrapment at the elbow: a prospective study. Hand (N Y) 2013;8(1):41–46. doi: 10.1007/s11552-012-9483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]