Abstract
Purpose
To examine the perceptions and opinions of orthopedic surgeons on new medical technology for patient-specific three-dimensional (3D) bone models in the diagnosis and treatment of orthopedic diseases related to the hip joint.
Materials and Methods
A total of 75 doctors who were trained in orthopedic surgery or were current residents in the Republic of Korea were surveyed via questionnaires. Eight questions were included regarding the utility and current issues in the diagnosis and treatment of orthopedic disease using a customized 3D bone model made from s patient's computed tomography (CT) image. In addition to the questionnaire, the simple plain radiography and 3D CT image of the patient and 3D printed models of two actual patients were presented for comparison.
Results
An average of 92.7% of the orthopedic surgeons answered “very much” or “yes” to questions regarding the effectiveness of diagnosis, treatment, education, and simulation of surgery using the patient-specific 3D bone model. To the question, “Do you think you must have medical insurance to provide better medical services by using a new patient-specific 3D bone model medical technology for simulated surgery?” 93.3% of orthopedic surgeons answered either “very much” or “yes”.
Conclusion
Patient-specific 3D bone models of new medical technology can provide breakthrough support in the diagnosis, treatment, and education of orthopedic diseases in the field of hip joints. Therefore, it seems that efforts should be made to change governmental policy for coverage of patient-specific 3D bone modeling.
Keywords: Patient-specific modeling, Three-dimensional, Printing
INTRODUCTION
Three-dimensional (3D) printing technology is advancing day by day and is being introduced into the medical industry1). Simulation surgery using 3D-printed bone models has been mainly used in the reconstruction and cosmetic surgery of the maxillofacial area in dentistry and plastic surgery and is also effectively used in orthopedic surgery in advanced countries2,3,4,5).
The pelvic bone and hip joints have a complex 3D structure, which makes operation on these structures difficult. In particular, surgery for complex acetabular fractures, total hip arthroplasty in patients with anatomical deformity, and revision of the hip joint in patients with severe bone defects are technically challenging and many complications occur during surgery6,7). Therefore, efforts to combine 3D printing technology with pelvic and hip surgery have been conducted, and research results have shown that the actual surgery can be effectively performed by creating an anatomical model, performing simulation surgery, and establishing a plan8,9). This technique can dramatically improve the outcome of surgery while reducing side effects and complications. However, despite these advantages and positive results reported within the academic community, 3D modeling is currently not designated as a medical care expense, making it difficult to apply it widely in clinical practice. The authors evaluated the concepts and opinions of orthopedic surgeons regarding the use of patient-specific 3D bone models via questionnaires distributed among orthopedic surgeons along with a simple plain radiograph, a 3D computed tomography (CT) image of the patient, and 3D printed models of two actual patients. The questionnaire included information such as whether the surgeon had any experience with 3D bone models, whether they find them useful, and if there are limitations to their use.
MATERIALS AND METHODS
From June 1, 2020 to June 30, 2020, questionnaires were distributed to 75 orthopedic surgeons in Korea which included 50 orthopedic specialists and 25 residents. The survey was created by our institution (Table 1), and the questionnaire was given to the doctors along with the simple plain radiography and 3D CT image of a patient, and the 3D printed models of two actual patients for comparison (Fig. 1, 2). As shown in Table 1 the questionnaire includes as following; the experience of using the bone models, usefulness for diagnosing the disease, the effect of the model on the decision of treatment method, usefulness for actual patient treatment, usefulness for explanations to the patient or the medical team, and obstacles for using the bone model. Based on the responses, we determined the usefulness or limitations of 3D bone models (Fig. 3, 4, 5, 6, 7, 8, 9).
Table 1. Questionnaire about Patient-specific Three-dimensional Bone Models to Orthopedic Surgeons in Korea.
| 1. Do you know any information on patient-specific 3D bone models for simulated surgery? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
| 2. Have you ever used a patient-specific 3D bone model for simulated surgery? | |||||
| ① None | ② 1-5 years | ③ Over 5 years | |||
| 3. Do you think that a patient-specific 3D bone model for simulated surgery can help orthopedic surgeons to diagnose a patient’s disease? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
| 4. Do you think that a patient-specific 3D bone model for simulated surgery has a positive effect on the decision for the patient’s treatment method? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
| 5. Do you think that a patient-specific 3D bone model for simulated surgery is helpful for orthopedic surgeons to treatment? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
| 6. Do you think that a patient-specific 3D bone model for simulated surgery is helpful in explaining surgical methods to patients, doctors, and surgery teams? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
| 7. Please indicate all the things that you think are a major obstacle in using a patient-specific 3D bone model for simulated surgery. | |||||
| ① Lack of bone model manufacturers | |||||
| ② Expenses needed to receive bone model | |||||
| ③ Lack of experience with bone models | |||||
| ④ The problem of time it takes to make a bone model | |||||
| ⑤ Other ( ) | |||||
| 8. Do you think medical insurance should be provided in order to provide better medical service by using a patient-specific 3D bone model for simulated surgery? | |||||
| ① Very much | ② Yes | ③ Neutral | ④ No | ⑤ Never | |
Fig. 1. Simple plain radiography (A) and 3-dimensional (3D) computed tomography (B, C), and 3D printed models (D) of actual patients underwent Girdlestone operation in order to help for the questionnaire survey.

Fig. 2. Simple plain radiography (A) and 3-dimensional (3D) computed tomography (B, C), and 3D printed models (D) of another patients underwent total hip arthroplasty in order to help for the questionnaire survey.

Fig. 3. Do you know any information on patient-specific 3D bone models for simulated surgery? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.

Fig. 4. Have you ever used a patient-specific 3D bone model for simulated surgery? 1: none, 2: 1-5 years, 3: over 5 years.

Fig. 5. Do you think that a patient-specific 3D bone model for simulated surgery can help orthopedic surgeons to diagnose a patient's disease? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.

Fig. 6. Do you think that a patient-specific 3D bone model for simulated surgery has a positive effect on the decision for the patient's treatment method? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.
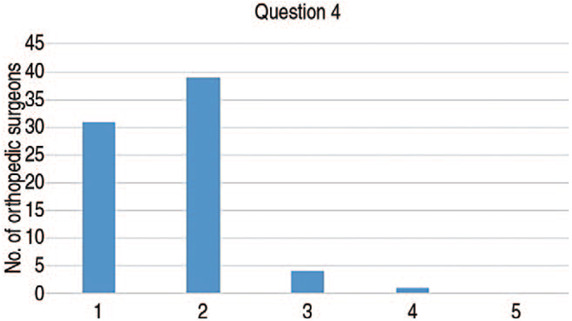
Fig. 7. Do you think that a patient-specific 3D bone model for simulated surgery is helpful for orthopedic surgeons to treatment? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.

Fig. 8. Do you think that a patient-specific 3D bone model for simulated surgery is helpful in explaining surgical methods to patients, doctors, and surgery teams? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.

Fig. 9. Do you think medical insurance should be provided in order to provide better medical service by using a patient-specific 3D bone model for simulated surgery? 1: very much, 2: yes, 3: neutral, 4: no, 5: never.

RESULTS
Of the 75 orthopedic surgeons surveyed, 65 orthopedic surgeons (86.7%) answered that they had never used new medical technology with a patient-specific 3D bone model. After comparing the 3D printing models of two patients to the same simple radiography and 3D CT, 67 orthopedic surgeons (89.3%) answered that the patient-specific 3D bone model helped to diagnose the patient's disease. A total of 70 orthopedic surgeons (93.3%) answered that the model had a positive effect on the treatment method decision and that they found the model helpful. Of the 75 surveyed orthopedic surgeons, 71 (94.7%) responded that the patient-specific 3D bone models were helpful in explaining the surgical method to patients, doctors, and surgical teams. However, 32 orthopedic surgeons (42.7%) felt that there are not enough manufacturers to make patient-specific 3D bone models, 53 orthopedic surgeons (70.7%) thought that the expense required to manufacture bone models is a problem, 40 (53.3%) responded that they have insufficient experience with 3D bone models, and 32 orthopedic surgeons (42.7%) had concerns over the amount of time that it takes to manufacture bone models. A total of 75 orthopedic surgeons, 70 (93.3%) answered that medical insurance should cover the costs associated with creating and using patient-specific 3D bone models.
DISCUSSION
Diagnosing and treating diseases using 3D CT and simple radiographic examination has become essential for evaluating orthopedic disease. Though 3D CT is helpful in diagnosis and treatment compared to simple radiographic examination, it is often different from what surgeons encounter in the actual operating field as the 3D reconstruction of the patient's current state must still be viewed in two dimensions. There are more differences in patients with a serious deformity or bone defect, comminuted fractures, and revision surgery. If the actual operating field differs from the preoperative examination or plan, treatment may have to be altered in the operating room and outcomes will depend solely on the experience and judgment of the surgeon. This can be innovatively solved through the use of patient-specific 3D bone models. The patient-specific 3D bone model reconstructs the current state of the patient in 3D allowing the surgeon to easily recognize defects or deformities that are difficult to judge in 2D. Prior to surgery, a doctor can practice in advance the methods and techniques to be used in the actual operating field through simulated surgery. Additionally, when inserting an implant or prosthesis in patients with severe deformities, bone defects, or comminuted fractures, often the outline does not match with the implant making it is difficult to insert the implant or prosthesis. This may increase the operation time, and complications may arise due to improper insertion. These problems can be addressed through the use of a patient-specific 3D bone model.
There are many existing cases where patient-specific 3D bone models are used in other countries. In 2019, Chen et al.10) performed surgery on a total of 52 patients with pelvic fractures. For 28 of the 52 patients, the operation was performed using a metal plate that had been outlined prior to surgery using 3D printing technology while a conventional method of matching the outline of the metal plate while operating was used for the remaining patients. Findings indicated that the bleeding amount and the operation time were shorter in the group that operated with a metal plate that was outlined in advance using 3D printing technology compared to surgeries where conventional methods were used.
In 2014, Small et al.11) performed total hip arthroplasty in 36 patients where half the patients (18 patients) were operated on using conventional total hip arthroplasty and patient-specific total hip arthroplasty was performed on the remaining patients (18 patients). Preoperative and postoperative CT scans were used to compare the differences between the preoperative plan and the actual outcome. Findings indicate that the differences between the preoperative plan and the actual postoperative acetabular cup inclination and anteversion angle were significantly lower in the patient group who underwent patient-specific total hip arthroplasty compared to the patient group who underwent conventional total hip arthroplasty. This suggests that the patient-specific total hip arthroplasty was performed exactly as planned before surgery. In 2013, Won et al.12) performed total hip arthroplasty in 21 patients where preoperative planning and simulation were performed using the 3D printing rapid prototype (RP) model. In 80.9% of patients, the acetabular cup was within 2 mm of the expected size, and in all patients bone ingrowth and stability could be confirmed without abrasion or osteolysis at the final follow-up. Through this, they reported that the 3D printing RP model enables simulated surgery before surgery and that the shape, size, and location of the implants can be determined before surgery in total hip arthroplasty.
There are some limitations to the current study. First, the number of orthopedic surgeons who participated in the survey is small and some participants were not experienced. Second, because the survey is limited to the field of hip joints, it is difficult to extend it to the entire field of orthopedic surgery. Third, since the 3D printing products used in the survey are provided in a completed form, there is a limit to assessing the difficulty in actually manufacturing and designing the models.
Patient-specific 3D bone models can be useful in clinical practice, as indicated by responses from Korean orthopedic surgeons who are aware of the effectiveness and usefulness of patient-specific 3D bone models. However, due to issues of cost treatment using a patient-specific 3D bone model is often not possible, which may to the patient not receiving the best possible treatment. Specifically, in the case of reoperation or complex fracture, if adequate surgical treatment is not performed due to severe bone defects or deformities, several additional surgical treatments may be required which is a substantial burden on the patient both physically and mentally. The results of the current survey demonstrate that though surgeons are aware of this technology they are hindered by cost and that they feel regret over not being able to provide the best treatment possible. The utility and necessity of using a patient-specific 3D bone model is gradually being demonstrated as a technology that must be introduced for the development of the medical field in the future.
CONCLUSION
Patient-specific 3D bone models of new medical technology can provide breakthrough support in the diagnosis, treatment, and education of orthopedic diseases in the field of hip joints. However, due to issues of cost treatment using a patient-specific 3D bone model is often not possible, which may to the patient not receiving the best possible treatment. Therefore, it seems that efforts should be made to change governmental policy for coverage of patient-specific 3D bone modeling.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Furlow B. Medical 3-D printing. Radiol Technol. 2017;88:519CT–537CT. [PubMed] [Google Scholar]
- 2.Kalman L. 3D printing of a novel dental implant abutment. J Dent Res Dent Clin Dent Prospects. 2018;12:299–303. doi: 10.15171/joddd.2018.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dawood A, Marti Marti B, Sauret-Jackson V, Darwood A. 3D printing in dentistry. Br Dent J. 2015;219:521–529. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 4.Hsieh TY, Dedhia R, Cervenka B, Tollefson TT. 3D printing: current use in facial plastic and reconstructive surgery. Curr Opin Otolaryngol Head Neck Surg. 2017;25:291–299. doi: 10.1097/MOO.0000000000000373. [DOI] [PubMed] [Google Scholar]
- 5.Bauermeister AJ, Zuriarrain A, Newman MI. Three-dimensional printing in plastic and reconstructive surgery: a systematic review. Ann Plast Surg. 2016;77:569–576. doi: 10.1097/SAP.0000000000000671. [DOI] [PubMed] [Google Scholar]
- 6.Gamradt SC, Lieberman JR. Bone graft for revision hip arthroplasty: biology and future applications. Clin Orthop Relat Res. 2003;(417):183–194. doi: 10.1097/01.blo.0000096814.78689.77. [DOI] [PubMed] [Google Scholar]
- 7.Brubaker SM, Brown TE, Manaswi A, Mihalko WM, Cui Q, Saleh KJ. Treatment options and allograft use in revision total hip arthroplasty the acetabulum. J Arthroplasty. 2007;22(7 Suppl 3):52–56. doi: 10.1016/j.arth.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Li YT, Hung CC, Chou YC, et al. Surgical treatment for posterior dislocation of hip combined with acetabular fractures using preoperative virtual simulation and three-dimensional printing model-assisted precontoured plate fixation techniques. Biomed Res Int. 2019;2019:3971571. doi: 10.1155/2019/3971571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woo SH, Sung MJ, Park KS, Yoon TR. Three-dimensional-printing technology in hip and pelvic surgery: current landscape. Hip Pelvis. 2020;32:1–10. doi: 10.5371/hp.2020.32.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen K, Yang F, Yao S, et al. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019;105:877–884. doi: 10.1016/j.otsr.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Small T, Krebs V, Molloy R, Bryan J, Klika AK, Barsoum WK. Comparison of acetabular shell position using patient specific instruments vs. standard surgical instruments: a randomized clinical trial. J Arthroplasty. 2014;29:1030–1037. doi: 10.1016/j.arth.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Won SH, Lee YK, Ha YC, Suh YS, Koo KH. Improving preoperative planning for complex total hip replacement with a Rapid Prototype model enabling surgical simulation. Bone Joint J. 2013;95:1458–1463. doi: 10.1302/0301-620X.95B11.31878. [DOI] [PubMed] [Google Scholar]


